Abstract
Introduction:
Several studies have documented children gain more weight during the summer season. Despite high obesity rates, little research has included American Indian/Alaskan Native children and few studies have been longitudinal. This observational study examines seasonal weight variability over 3.5 years among ethnically diverse children including 2,184 American Indian/Alaskan Native children.
Methods:
Children’s height and weight were measured before and after the summer 2012–2015 and analyzed in 2019–2020, including children with ≥2 consecutive measurements (N=7,890, mean age=8.4 [SD=2.8] years). Mixed effects models tested whether percentage of the 95th BMI percentile and BMI differed by season (summer versus rest of year) and ethnicity.
Results:
American Indian/Alaskan Native (23.7%), Hispanic (19.8%), and Black (17.8%) children had significantly higher baseline obesity rates than White children (7.1%). The percentage of the 95th BMI percentile significantly increased during the summer compared with the rest of the year, with the strongest effects for children who were obese (b=2.69, 95% CI=1.35 to 4.03, p<0.001) or overweight (b=1.47, 95% CI=0.56, 2.35, p<0.01). In BMI units, summer BMI increase (versus rest of year) was 0.50 kg/m2 higher (obese model) and 0.27 kg/m2 higher (overweight). Seasonal effects were significantly less pronounced for American Indian/Alaskan Native children versus White children.
Conclusions:
Children gained significantly more weight during summer season, with the strongest effects for children who were obese. American Indian/Alaskan Native children had less seasonal variability than White children, but higher overall obesity rates. These data underscore summer as a critical time for obesity prevention among children who are overweight/obese, but suggest seasonal patterns may vary for American Indian/Alaskan Native children.
INTRODUCTION
Childhood obesity and sedentary behaviors are urgent health issues facing children worldwide, increasing their risk for early mortality, chronic conditions including diabetes and heart disease, poor mental health outcomes, and poor quality of life.1–6 Substantial disparities exist for children who are socioeconomically disadvantaged,7,8 and children of Black, Hispanic, and American Indian/Alaskan Native (AI/AN) background.9–12
Recent research has highlighted that weight gain in children is not consistent throughout the year; children disproportionately accelerate BMI over the summer months compared with other periods of the year.13–24 Several theories have proposed mechanisms underlying children’s seasonal variability in weight gain. The Structured Days Hypothesis posits that the structured environment of school days helps to limit obesogenic behaviors, such as sedentary behavior, increased caloric intake, increased screen time, and irregular sleep.19 Further, the impact of circadian rhythm and linked biological processes contribute to seasonal variability in weight gain as posited by the Circadian and Circannual Rhythm Model.20,25,26
Several factors have been associated with accelerated summer BMI gain, including SES, race/ethnicity, and weight status. Similar to the “summer setback” concept,15,27 the “health gap” hypothesis suggests that the obesity gap between children from households with low versus middle to upper income widens during summer.28 National studies have suggested that accelerated BMI during summer was most pronounced among Black and Hispanic children.13 Finally, children who were already overweight or obese have also been found to be at increased risk for summer excess weight gain.13,14,23
However, only a small amount of prior research has included AI/AN children, despite studies documenting that >50% of AI/AN children are overweight or obese by 5th grade10,11 and have up to 9 times the adolescent type 2 diabetes rates of non-Hispanic Whites.12 Disparities appear to be getting worse: Among children aged <5 years, in the past decade, low-income AI/AN children were the only population to see substantial increases in obesity rates.7 To date, only 3 studies have examined accelerated summer weight gain in AI/AN children, but have found inconsistent results.11,29,30 One study found lower weight velocity during summer compared with the school year,29 another found significant increases in BMI, but not in BMI z-scores during summertime,11 and 1 found no significant seasonal variation.30 These studies had modest AI/AN sample sizes (N=141, N=181, and N=440), 2 studies included only 1 summer of data, and only 1 compared AI/AN children to other ethnic groups.11,29,30
Given the limited research and inconsistent findings among AI/AN children, this study aims to gain deeper insight into the seasonal variability in weight gain among a diverse sample of almost 8,000 children including 2,184 AI/AN children. The data span 3.5 years and 7 measurements. It was hypothesized that all ethnic/racial groups would experience accelerated BMI during summertime, but given their high risk for overweight/obesity, effects would be more pronounced for children of AI/AN, Hispanic, and Black background, children in schools with lower SES, and children who were overweight/obese.
METHODS
Study Sample
A total of 10,648 students were measured between the fall of 2012 and fall of 2015 in 10 elementary and 2 middle schools in the Southwest U.S. as a district-wide health measurement. Data were analyzed in 2019–2020. The middle schools started measurements in fall 2013, leaving 5 measurements. Only students with ≥2 consecutive measurements were included, so that change between timepoints could be calculated (total N=7,890; flow diagram in Appendix Figure 1). Each student and school had a unique ID to allow tracking over time. If students moved within the district, a new ID was assigned, which was linked if it uniquely matched on date of birth, sex, ethnicity, non-consecutive measurement time, and plausible BMI range. The average number of measurements was 4.34 (SD=1.81), which was similar across sex and ethnicity and slightly lower among children who were overweight (4.14) and obese (4.10). Recruitment occurred on a rolling basis, and students with <7 measurements did not necessarily have missing data, but may have started in the school district at a later timepoint. A total of 78.2% of children had ≥3 consecutive measurements and 1,403 had all 7 timepoints. Measurements occurred 4–6 weeks before the end and start of the school year (start, mid-August; end, late May). Parents provided consent for their child to be measured and all procedures were approved by the IRBs of the school district, medical center, and academic institution.
Measures
A binary timepoint variable “season” was created to indicate a pre-summer measurement, on average April 28 (SD=18.4 days), and a post-summer measurement, on average September 30 (SD=15.1 days).
Demographics included sex (male/female), race and ethnicity (Hispanic, White, AI/AN, and Black) as reported by parents, and age (calculated from date of birth and categorized as ≤5, 6–11, 12–14 years). Only 1 ethnicity per child was indicated and mixed race was not an option. There were no missing values for ethnicity or sex. School SES was the proportion of children in the school who qualified for free or reduced lunch (range=13%–75%), with 4 schools with >50% of children who qualified, 4 schools between 40% and 48%, and 3 schools between 13% and 23%. Height and weight were collected at each school during the school day by a community outreach coordinator trained in research quality measurements, supported by the school nurse and volunteers. Children were asked to take shoes and jackets off and items out of their pockets. Height to the nearest quarter inch was measured twice with a Charder HM200P Portstad Portable Stadiometer. Weight was measured to the nearest 0.1 pounds with a Health o meter™ 752KL Heavy Duty Remote Display Digital Scale. Children’s first weight status was considered their baseline, with <5th BMI percentile for their age and sex considered underweight, 5th–85th percentile as healthy weight, 85th–95th percentile as overweight, and ≥95th percentile as obese.31
Findings are presented in both raw BMI (lbs * inches2 * 703) and percentage of the 95th percentile of BMI for age and sex (%BMIp95) as outcomes, rather than BMI z-score. Recent literature has suggested that BMI z-score has limitations in tracking over time, particularly children aged <10 years with severe obesity.32,33 Although still a proxy for adiposity, a more sensitive measure for tracking young high risk children over time is %BMIp95.32 Specifically, %BMIp95 was calculated using the childsds package in R34 as the ratio of individual BMI relative to the sex- and age-specific CDC 95th percentile BMI multiplied by 100, defining obesity by an individual having %BMIp95 >100%.35
Statistical Analysis
Data across timepoints were linked using student ID for longitudinal analysis. Changes in height and weight were tracked and clear actionable errors (e.g., typos) were corrected. Other implausible BMI values were removed (defined as ≥1.0-SD change in BMI z-score across 2 timepoints), resulting in removal of 29 values.
First, it was tested whether ethnicity was associated with obesity at baseline for the overall sample using ANOVA. To test the primary hypothesis that changes in %BMIp95 varied by season, linear mixed effects models with student’s change in %BMIp95 as the response variable, student ID and school ID as random factors, and season (summer versus rest of year) were fit, with covariates of age, sex, ethnicity, school SES, and a variable indicating whether measurement date was >4 weeks from the average. Interaction terms between season and ethnicity, sex, and SES were added to assess whether any seasonal differences varied by demographics. Models were run separately by children’s baseline weight status (underweight/healthy weight [Model 1], overweight [Model 2], and obese [model 3]) to address violations of the residual homoscedasticity linear model assumption across weight categories. Tukey–Kramer multiple comparison adjustments were made for pairwise comparisons. Tests were 2-sided with a 5% significance level using R packages lme4 and emmeans.36,37 Models for both BMI and %BMIp95 are presented to facilitate interpretation and comparison to prior research.
RESULTS
Student demographics are detailed in Table 1. Most children were aged 6–11 (63.5% of children) and 52.2% were male. A total of 56.5% of children were White (n=4,456), 27.7% AI/AN (n=2,184), 13.1% Hispanic (n=1,036), and 2.7% Black (n=214). A total of 27.3% of children were overweight (13.7%) or obese (13.6%). Average %BMIp95 was higher for older children and boys. AI/AN (40.9% overweight or obese), Hispanic (38.5% overweight/obese) and Black (34.1% overweight/obese) children had far higher overweight and obesity rates compared with White children (17.8%). Notably, almost a quarter (23.7%) of AI/AN children were obese (vs 7.1% for White children). AI/AN children represented 27.7% of the overall study sample, but almost half (48.1%) of all children who were obese.
Table 1.
Sex, Age, Ethnicity and %BMIp95 at Baseline (N=7,890)
| Variable | Characteristics n (%) | %BMIp95 Mean (SD) |
|---|---|---|
| Age group | ||
| 3–5 years | 1,971 (25.0) | 87.8 (10.7) |
| 6–11 years | 5,007 (63.5) | 84.6 (15.5) |
| 12–14 years | 912 (11.6) | 86.0 (19.8) |
| Sex | ||
| Male | 4,119 (52.2) | 87.2 (15.6) |
| Female | 3,771 (47.8) | 83.7 (14.4) |
| Ethnicity | ||
| Black | 214 (2.7) | 87.9 (14.9) |
| Hispanic | 1,036 (13.1) | 86.9 (17.8) |
| American Indian/Alaskan | 2,184 (27.7) | 91.3 (17.4) |
| Native | ||
| White | 4,456 (56.5) | 82.3 (12.0) |
| Weight status | ||
| Underweight | 252 (3.2) | 66.2 (5.7) |
| Healthy | 5,481 (69.5) | 79.1 (7.0) |
| Overweight | 1,081 (13.7) | 93.8 (3.5) |
| Obese | 1,076 (13.6) | 114.7 (13.8) |
One-way ANOVA (not shown in Table) confirmed that AI/AN (b=10.70, 95% CI=10.20, 11.20), Hispanic (b=5.91, 95% CI=5.34, 6.48), and Black (b=5.66, 95% CI=4.32, 6.99) children all had a significantly higher baseline %BMIp95 compared with White children (all p<0.001). Children in low-income schools (b=6.70, 95% CI=6.19, 7.21, p<0.001) and middle-income schools (estimated b=2.76, 95% CI=2.23, 3.28, p<0.001) had significantly higher %BMIp95 compared with children in high-SES schools.
To address the primary study hypothesis, that weight gain would be greater during the summer season relative to the rest of the year, a series of linear mixed effect models were fit including age, sex, ethnicity, SES, deviation from measurement date, and a season indicator by weight status (Table 2). Findings indicated that children who were obese at baseline (n=1,076) experienced significantly greater increases in %BMIp95 during the summer season compared with the rest of the year (b=2.69, 95% CI=1.35, 4.03, p<0.001). Children who were overweight at baseline (but not obese, n=1,081) also experienced significantly greater summer increases in %BMIp95 (b=1.47, 95% CI=0.56, 2.35, p<0.01), although the size of the estimate was smaller. The effect for children who were underweight/healthy weight at baseline was not significant. In terms of raw BMI (Table 2), children who were overweight and obese at baseline gained 0.27 kg/m2 (95% CI=0.06, 0.46, p=0.009) and 0.50 kg/m2 (95% CI=0.20, 0.80, p=0.001) more during the summer season. The findings for children who were obese at baseline compared with all children and by ethnicity are represented graphically in Figures 1 and 2.
Table 2.
Mixed Effect Models by Weight Status for the Outcomes of %BMIp95 and Raw BMI
| Effect | Model 1: Healthy weight/underweight (N=5,583) | Model 2: Overweight (N=1,081) | Model 3: Obese (N=1,076) |
|---|---|---|---|
| %BMIp95 Change (95% CI) | |||
| Season: Summer (vs rest of year) | 0.13 (−0.09, 0.35) | 1.47** (0.56, 2.35) | 2.69*** (1.35, 4.03) |
| Ethnicity (ref: White children) | – | – | – |
| Black | 0.18 (−0.20, 0.57) | −2.00** (−3.19, −0.78) | 1.33 (−0.14, 2.79) |
| Hispanic | 0.22* (0.03, 0.41) | 0.05 (−0.51, 0.65) | 0.80* (0.02, 1.58) |
| AI/AN | 0.44*** (0.29, 0.60) | 0.70** (0.22, 1.18) | 0.84* (0.20, 1.48) |
| Season* SES interactiona | −0.67** (−1.17, −0.17) | −0.28 (−2.07, 1.55) | −0.78 (−3.34, 1.79) |
| Season* Sex interaction | 0.27** (0.11, 0.45) | 0.13 (−0.46, 0.73) | 0.12 (−0.66, 0.90) |
| Season*Ethnicity interaction | |||
| Ref group: White children | – | – | – |
| Black | −0.41 (−0.97, 0.15) | 1.84* (0.06, 3.62) | −2.58* (−4.74, −0.42) |
| Hispanic | −0.38** (−0.66, −0.11) | −0.59 (−1.42, 0.22) | −1.35* (−2.49, −0.22) |
| AI/AN | −0.37** (−0.60, −0.15) | −1.20*** (−1.91, −0.52) | −1.56** (−2.48, −0.63) |
| BMI change kg/m2 (95% CI) Season: Summer (vs rest of year) | −0.04 (−0.09, 0.00) | 0.27** (0.06, 0.46) | 0.50** (0.20, 0.80) |
| Ethnicity (ref: White children) | – | – | – |
| Black | 0.05 (−0.04, 0.13) | −0.40** (−0.67, −0.13) | 0.30 (−0.03, 0.62) |
| Hispanic | 0.08*** (0.04, 0.12) | 0.02 (−0.10, 0.15) | 0.21* (0.05, 0.40) |
| AI/AN | 0.11***b (0.08, 0.15) | 0.16** (0.05, 0.27) | 0.22** (0.08, 0.37) |
| Season* SES interaction | −0.20*** (−0.31, −0.09) | −0.17 (−0.57, 0.23) | −0.32 (−0.89, 0.26) |
| Season* Sex interaction | 0.05** (0.01, 0.09) | 0.01 (−0.13, 0.14) | 0.01 (−0.16, 0.19) |
| Season*Ethnicity interaction | |||
| Reference group: White children | – | – | – |
| Black | −0.09 (−0.20, 0.04) | 0.37 (−0.03, 0.77) | −0.57* (−1.06, −0.09) |
| Hispanic | −0.13*** (−0.19, −0.07) | −0.15 (−0.34, 0.03) | −0.31* (−0.57, −0.06) |
| AI/AN | −0.08** (−0.14, −0.04) | −0.28***(−0.43, −0.12) | −0.35*** (−0.56, −0.15) |
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001). Data based on Linear Mixed Models adjusted for age, sex, SES and whether the measurement time was more than 4 weeks from average.
SES defined as % of children in the school who qualify for free/reduced lunch.
AI/AN significantly different from Hispanic.
AI/AN, American Indian/Alaskan Native.
Figure 1.
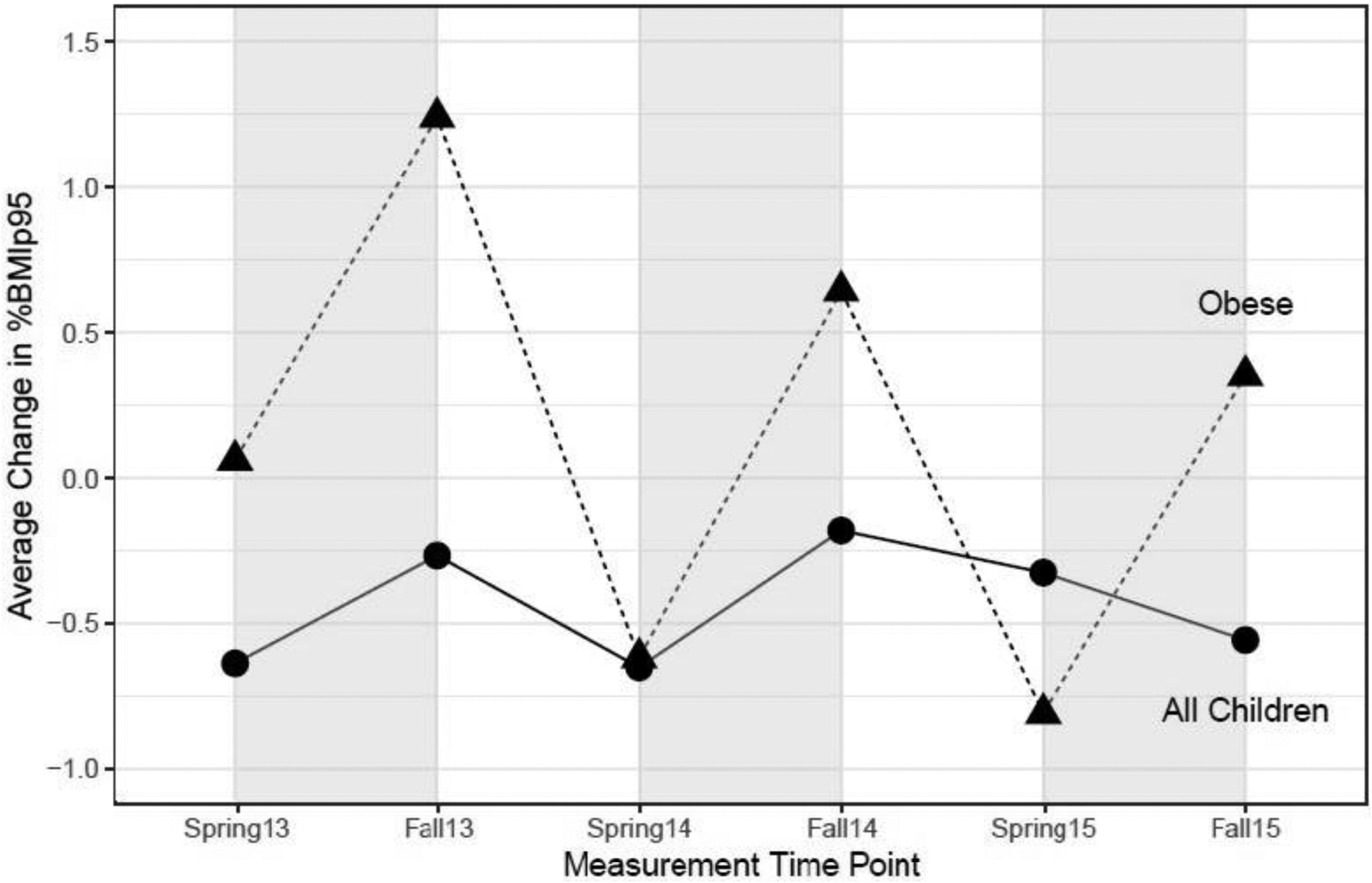
Average change in %BMIp95 over time by baseline obesity status.
Figure 2.
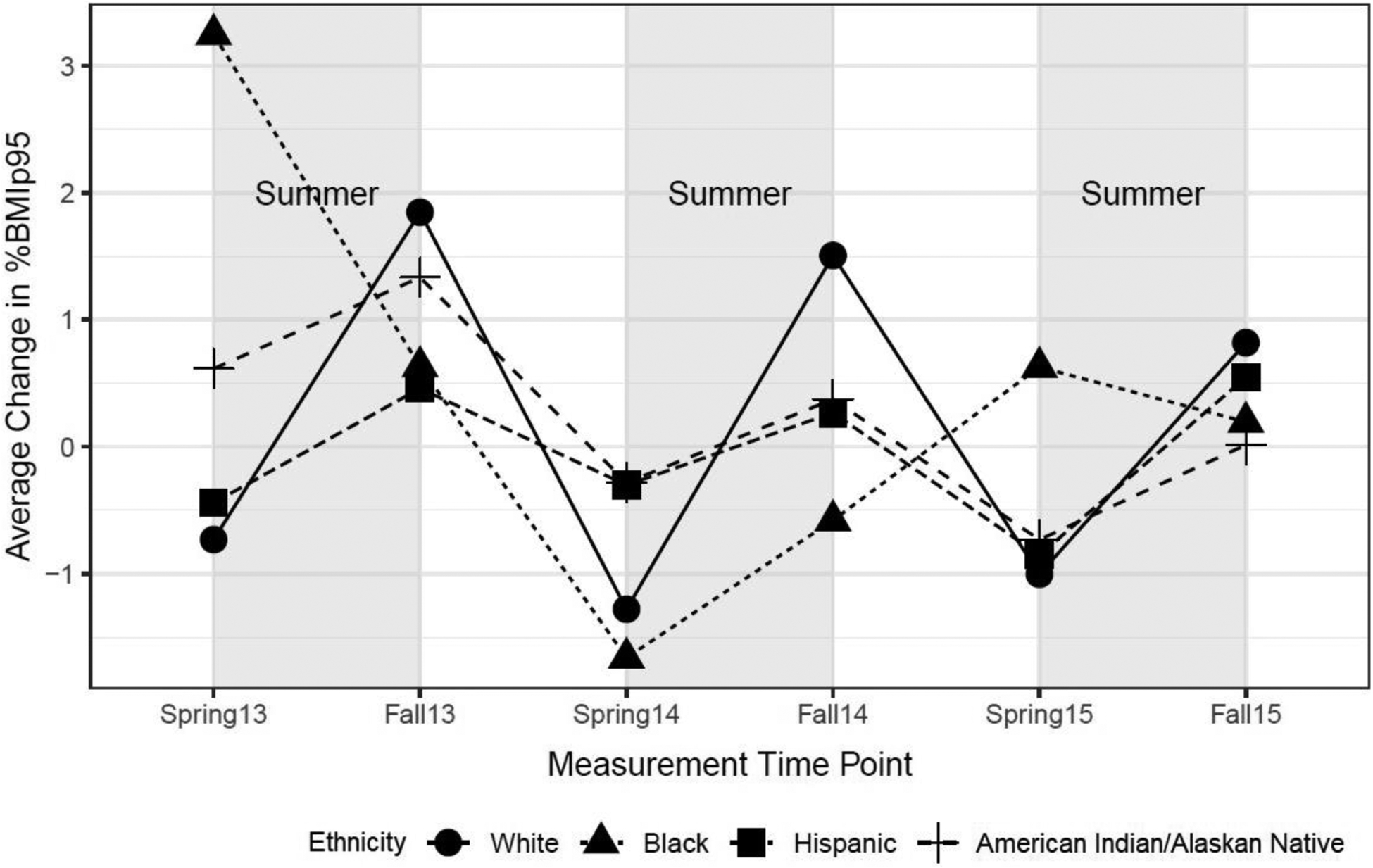
Average change in %BMIp95 in children classified as obese by ethnicity.
To assess whether seasonal changes varied by ethnicity, an interaction term of season by ethnicity was included in the linear mixed effect models (Table 2). Across all models, seasonal effects for AI/AN children were significantly less pronounced compared with White children (reference category), for underweight/healthy weight (b= −0.37, 95% CI= −0.60, −0.15, p=0.001), overweight (b= −1.20, 95% CI= −1.91, −0.52, p<0.001), and obese (b= −1.56, 95% CI= −2.48, −0.63, p=0.001) children. Expressed in raw BMI (Table 2), effects for AI/AN children who were overweight/obese were approximately 0.28–0.35 kg/m2 per summer season lower compared with White children. Thus, although far more AI/AN children fell within the highest risk categories for greater summer weight changes, effects were less strong compared with White children within those weight status categories. Finally, seasonal effects did not differ consistently between boys and girls and across school SES.
DISCUSSION
The current study aimed to gain insight into the seasonal variability in weight gain among a diverse sample of almost 8,000 children, including 2,184 AI/AN children, from longitudinal data collected over 3.5 years. Obesity prevalence was higher at baseline among AI/AN, Hispanic, and Black children, in comparison with white children.7–11,29 An acceleration in BMI and %BMIp95 was found during summer months (May to September) compared with non-summer months (October to April), with stronger effects for obese children. Although a higher proportion of AI/AN children were obese at baseline, seasonal effects were less pronounced for AI/AN children compared with White children.
Children classified as obese, on average, significantly accelerated their %BMIp95 and BMI over the summer season in the current study by +2.69% and 0.50 kg/m2 more than the rest of the year, with about half the effect for children who were overweight (+1.47% and 0.27 kg/m2). Although the magnitude of the difference in %BMIp95 is modest for each summer independently, accumulated over several years, the effects demonstrate the potential for substantial changes over time and the importance of intervention during the summer. In addition, the magnitude of BMI change among obese and overweight children of 0.27–0.50 kg/m2 over a 5-month summer period, or 0.05–0.12 kg/m2 per month, was similar to prior research, showing 0.05–0.10 kg/m2 monthly weight gain during the summertime and almost none during the rest of the year.13,30 Findings support prior literature documenting accelerated seasonal weight gain during summer months for children who are overweight or obese.11,14,23,29 Prior research has suggested that during summer months, almost all children are removed from the consistent structured schedule that school provides, thus allowing for an increase in obesogenic behaviors such as increased sedentary/screen time behaviors,19 increased food consumption,38 and reductions in sleep.39 Further, the lack of consistent structure during summer months could be interrupting children’s circadian clock and interfering with biological processes that influence fat storage and fat breakdown.20 Further research is needed to understand and disentangle the biological, environmental, and behavioral factors associated with accelerated summer weight gain. In this study, AI/AN children had much higher obesity prevalence at baseline than White children, and thus a greater proportion of AI/AN children were in the group at highest risk for accelerated summer BMI gain. However, although effects of summer weight gain were present for children of all ethnicities who were obese, they were less pronounced for AI/AN children than White children. These findings are somewhat similar to several prior studies.11,29,30 One study including 141 AI/AN children from Wyoming found that AI/AN children who were overweight or obese significantly increased their BMI over the summer, but not children of healthy weight.11 Another study, the Bright Start Trial of 440 AI/AN children residing in a Northern Plains Tribal nation, found that children had significantly lower velocity of weight gain during the summer season compared with the academic year after.29 However, both studies included only 1 summer of data, were implemented on tribal lands, and could not compare AI/AN children to other groups. The only study that directly compared AI/AN children’s summer weight changes with other ethnic/racial groups included 181 AI/AN children as part of a nationally representative sample based on the Early Childhood Longitudinal Study-Kindergarten: 2011 cohort.30 This study found significantly higher per-month weight change among AI/AN children during the second school year, but no significant differences between AI/AN children and White children during 2 summer seasons. In fact, although not statistically significant, the largest difference in magnitude between any ethnic group during any season was found during the second summer, when AI/AN children had a per-month −0.066 kg/m2 lower weight change compared with White children.30
These data underscore that the seasonal patterns of weight gain among high-risk AI/AN children may potentially be different than White children. As mentioned by Zhang and colleagues,29 the reasons for lower weight changes compared with national averages among AI/AN populations during summer season are likely multifactorial, and AI/AN children residing on reservation areas are likely to be exposed to obesogenic environments the entire year. Though the current study did not include schools on reservation areas, it is located near several sovereign Tribal nations and it is possible that a proportion of AI/AN children travel long distances during the school year. In addition, it is possible that regional or seasonal aspects impact AI/AN students’ activity and dietary intake, with weather patterns being more conducive to physical activity during the summer, and overnight low temperatures in the area resulting in traditional agricultural activities occurring primarily between April and September.
Limitations
The length of data collection, number of AI/AN children, and direct comparison of children from different ethnic groups represent strengths of the study compared with the existing literature. Utilizing an outcome measure (%BMIp95) most sensitive to tracking weight over time among young obese and overweight students provides additional insight, even if %BMIp95 is a proxy for adiposity. However, there are several limitations to the current data set. The established protocol for measuring height to the nearest quarter inch was less precise than the gold standard of nearest eighth of an inch. This could have increased the chance for error in estimation of child BMI and %BMIp95. Also, date of measurement could not be controlled, which resulted in comparison of an average measurement time period from October through April, contrasted with May through September. However, it is similar to other studies including AI/AN children. In this study, the average number of days during the summer season was 155 days, and 211 days during the academic year. In the Bright Start trial, the number of days between measurements was 168 days including the initial summer season and 144 and 226 during the preceding and following academic years.29 In the Early Childhood Longitudinal Study-Kindergarten: 2011 study, children were measured, on average, 5–7 weeks after the first day of school in the fall semester with spring measurements 8 weeks before the last day of school.30 It possible that the effects found in these studies are conservative estimates, given that several weeks of summer were actually in the school year. Further, variables such as individual-level SES or distance traveled to school were not able to be captured, which may be important confounding variables to summer weight gain among AI/AN populations. Finally, despite a large sample size and direct comparisons to other ethnic groups, findings may not be directly comparable to AI/AN populations living in very different settings and climates.
CONCLUSIONS
The current study assessed seasonal changes in %BMIp95 and BMI among a large sample of ethnically diverse students and found that overweight and obese students gained significantly more weight during summer compared with the rest of the year. These findings underscore the urgent need to intervene during these time periods among the highest-risk children. All ethnic minorities were at much higher risk for obesity at baseline, but seasonal effects were significantly less pronounced for AI/AN students. Future research should examine activity, dietary intake, and sleep patterns among AI/AN children during different seasons to gain greater insight into factors underlying health behaviors across seasons.
Supplementary Material
ACKNOWLEDGMENTS
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities to the Southwest Health Equity Research Collaborative under award number U54MD012388. The authors also gratefully acknowledge members of the Pediatric Obesity Weight Evaluation Registry Research Committee who contributed to the refinement of the research concept, study design, and statistical analysis approach for this study. The content is solely the responsibility of the authors and does not represent the views of the funders. The funding agency had no role in data collection, analysis, interpretation, or the decision to write this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Fast Stats: Obesity and Overweight. Centers for Disease Control and Prevention. https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Accessed November 21, 2017. [Google Scholar]
- 2.Tsiros MD, Coates AM, Howe PR, Grimshaw PN, Buckley JD. Obesity: the new childhood disability? Obes Rev. 2011;12(1):26‒36. 10.1111/j.1467-789x.2009.00706.x [DOI] [PubMed] [Google Scholar]
- 3.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(suppl 2):518‒525. [PubMed] [Google Scholar]
- 4.Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Smith GD. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr. 1998;67(6):1111‒1118. 10.1093/ajcn/67.6.1111. [DOI] [PubMed] [Google Scholar]
- 5.Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013;13(1):6‒13. 10.1016/j.acap.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Franks PW, Hanson RL, Knowler WC, et al. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485‒493. 10.1056/nejmoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan L, McGuire LC, Blanck HM, May-Murriel AL, Grummer-Strawn LM. Racial/ethnic differences in obesity trends among young low-income children. Am J Prev Med. 2015;48(5):570‒574. 10.1016/j.amepre.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29(1):6‒28. 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 9.Rossen LM, Schoendorf KC. Measuring health disparities: trends in racial− ethnic and socioeconomic disparities in obesity among 2-to 18-year old youth in the United States, 2001–2010. Ann Epidemiol. 2012; 22(10):698‒704. 10.1016/j.annepidem.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caballero B, Clay T, Davis SM et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030‒1038. 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith DT, Bartee RT, Dorozynski CM, Carr LJ. Prevalence of overweight and influence of out-of-school seasonal periods on body mass index among American Indian schoolchildren. Prev Chronic Dis. 2009;6(1):A20. [PMC free article] [PubMed] [Google Scholar]
- 12.Diabetes in American Indians and Alaskan Natives Facts at a Glance, 2012. HHS. https://www.ihs.gov/MedicalPrograms/Diabetes/HomeDocs/Resources/FactSheets/Fact_sheet_AIAN_508c.pdf. Published June 2012. Accessed October 10, 2019. [Google Scholar]
- 13.von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007;97:696–702. 10.2105/ajph.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baranowski T, O’Connor T, Johnston CA, et al. School year versus summer differences in child weight gain: a narrative review. Child Obes. 2014;10(1):18‒24. 10.1089/chi.2013.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11(12):130355. 10.5888/pcd11.130355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weaver RG, Beets MW, Brazendale K, Brusseau TA. Summer weight gain and fitness loss: causes and potential solutions. Am J Lifestyle Med. 2019;13(2):116‒128. 10.1177/1559827617750576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tanaka C, Reilly JJ, Tanaka M, Tanaka S. Changes in weight, sedentary behaviour and physical activity during the school year and summer vacation. Int J Environ Res Public Health. 2018;15(5):915. 10.3390/ijerph15050915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillis L, McDowell M, Bar-Or O, et al. Relationship between summer vacation weight gain and lack of success in a pediatric weight control program. Eat Behav. 2005;6(2):137‒143. 10.1016/j.eatbeh.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act. 2017;14:100. 10.1186/s12966-017-0555-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreno JP, Crowley SJ, Alfano CA. Physiological mechanisms underlying children’s circannual growth patterns and their contributions to the obesity epidemic in elementary school age children. Obes Rev. 2020;21(3):e12973. 10.1111/obr.12973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Downey DB, Boughton HR. Childhood body mass index gain during the summer versus during the school year. New Dir Youth Dev. 2007;(114):33‒44. 10.1002/yd.211. [DOI] [PubMed] [Google Scholar]
- 22.Wang YC, Vine S, Hsiao A, Rundle A, Goldsmith J. Weight-related behaviors when children are in school versus on summer breaks: does income matter? J Sch Health. 2015;85(7):458‒466. 10.1111/josh.12274. [DOI] [PubMed] [Google Scholar]
- 23.Mahoney JL. Adolescent summer care arrangements and risk for obesity the following school year. J Adolesc. 2011;34(4):737‒749. 10.1016/j.adolescence.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moreno JP, Johnston CA, Woehler D. Changes in weight over the school year and summer vacation: results of a 5-year longitudinal study. J Sch Health. 2013;83(7):473‒ 477. 10.1111/josh.12054. [DOI] [PubMed] [Google Scholar]
- 25.Hart CN, Jelalian E, Raynor HA. Behavioral and social routines and biological rhythms in prevention and treatment of pediatric obesity. Am Psychol. 2020;75(2):152‒162. 10.1037/amp0000599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moreno JP, Crowley SJ, Alfano CA et al. Potential circadian and circannual rhythm contributions to the obesity epidemic in elementary school age children. Int J Behav Nutr Phys Act. 2019;16:25. 10.1186/s12966-019-0784-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Entwisle DR, Alexander KL. Summer setback: race, poverty, school composition, and mathematics achievement in the first two years of school. Am Sociol Rev. 1992;57(1):72‒ 84. 10.2307/2096145. [DOI] [Google Scholar]
- 28.Weaver RG, Beets MW, Brazendale K, Brusseau TA. Summer weight gain and fitness loss: causes and potential solutions. Am J Lifestyle Med. 2019;13(2):116‒128. 10.1177/1559827617750576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang J, Himes JH, Hannan PJ, et al. Summer effects on body mass index (BMI) gain and growth patterns of American Indian children from kindergarten to first grade: a prospective study. BMC Public Health. 2011;11:951. 10.1186/1471-2458-11-951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.von Hippel PT, Workman J. From kindergarten through second grade, US children’s obesity prevalence grows only during summer vacations. Obesity (Silver Spring). 2016;24(11):2296‒2300. 10.1002/oby.21613. [DOI] [PubMed] [Google Scholar]
- 31.Healthy Weight: About Child & Teen BMI. Division of Nutrition, Physical Activity, and Obesity. Centers for Disease Control and Prevention. https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Published 2018. Accessed October 15, 2019. [Google Scholar]
- 32.Freedman DS, Butte NF, Taveras EM et al. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999‒2000 to 2013‒ 2014. Obesity (Silver Spring). 2017;25(4):739‒746. 10.1002/oby.21782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freedman DS, Berenson GS. Tracking of BMI z scores for severe obesity. Pediatrics. 2017;140(3):e20171072. 10.1542/peds.2017-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vogel M Childsds: Data and Methods Around Reference Values in Pediatrics. https://cran.r-project.org/web/packages/childsds/childsds.pdf. Published 2019. Accessed March 12, 2020.
- 35.Kumar S, King EC, Christison AL, et al. Health outcomes of youth in clinical pediatric weight management programs in POWER. J Pediatr. 2019;208:57‒65.e4. 10.1016/j.jpeds.2018.12.049. [DOI] [PubMed] [Google Scholar]
- 36.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 37.Lenth R emmeans: Estimated Marginal Means. R package version 1.4.7. Published 2020.
- 38.Nixon GM, Thompson JM, Han DY et al. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31(1):71‒78. 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brazendale K, Beets MW, Turner‐McGrievy GM, et al. Children’s obesogenic behaviors during summer versus school: a within‐person comparison. J Sch Health. 2018;88(12):886‒892. 10.1111/josh.12699. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


