Abstract
Introduction:
Well-care use can positively impact adolescents’ current and future health. Understanding adolescents’ longitudinal well-care use is critical to determine to whom and when to target engagement strategies to improve healthcare access. This study describes prospective well-care use patterns from childhood through adolescence stratified by sex.
Methods:
The sample (N=6,872) was drawn from the Child/Young Adult component of the household-based 1979 National Longitudinal Survey of Youth consisting of biological children born to female respondents (1980–1997). Well-care use (routine checkup with doctor within last year) data were assessed from age 5 years (1986–2003) until 17 years (1998–2015). Conducted in 2019, latent class analyses stratified by sex identified well-care use patterns reported over 7 biennial time points adjusted for cohort, race/ethnicity, urbanicity, maternal education, and insurance.
Results:
Four well-care use classes emerged for female adolescents: The majority belonged to Engaged (37%) and Moderately Engaged (39%) classes and remainder to Gradually Re-engaged (14%), and Disengaged-With-Rebound (10%) classes. Three classes emerged for male adolescents: The majority belonged to the Persistently Disengaged (48%) class and remainder in Engaged (34%) and Gradually Re-engaged (18%) classes. For both sexes, comparing each cohort to the first, Engaged class membership increased for subsequent cohorts. Less engaged well-care use classes had more non-Hispanic White adolescents living in rural areas with lower insurance coverage. Maternal education differentiated well-care use classes for male but not female adolescents, being higher for male adolescents in the Engaged than other classes.
Conclusions:
Findings highlight well-care use patterns for both sexes changed during the transition from childhood to adolescence and class membership differed by covariates. Results suggest sex-specific strategies may be needed to enhance adolescents’ well-care use engagement over time.
INTRODUCTION
Adolescence is an important time to improve health across the lifespan. National professional organizations promote adolescent well-care use (WCU) to address a range of health-promoting and risk-reducing behaviors.1–3 Although research demonstrates WCU can positively impact adolescents’ health,4,5 few studies have examined adolescents’ WCU patterns over time. More recently, adolescents’ transition into adult care has been examined,6,7 yet fewer studies have examined WCU transitions from childhood into adolescence—a vulnerable time when adolescents may experience health issues and healthcare disconnection, particularly male adolescents.8
Past studies examining adolescents’ WCU are mainly cross-sectional in nature and report overall WCU rates, WCU rates by age and sex, or WCU cohort trends.9–11 For example, younger (aged 11–14 years) rather than older (aged 15–19 years) adolescents attended more past-year well-care visits9 and past-year checkup rates increased from 2000 (63%) to 2012 (74%).10 However, cross-sectional data analysis describes only group-level differences. These studies have shown adolescents’ WCU to be associated with sex, race/ethnicity, health insurance, and prior WCU.8,9,12–19 Given limited longitudinal examination of adolescents’ WCU, it remains unclear how these factors are associated with patterns of adolescents’ WCU over time.
Studies examining adolescents’ individual WCU patterns over time let alone WCU patterns from middle childhood (age 6–11 years) through adolescence are rare.12–15 A couple of insurance claims panel analyses have examined only continuously insured adolescents and summarized cumulative annual visits rather than patterns of adolescents’ WCU over time or factors associated with these patterns.12,13 Other limitations to these and other past studies include use of narrow inclusion criteria for panel samples (e.g., continuously insured adolescents only) and evaluating average visits and short time frames.14,15 Taking full advantage of prospective data to examine changes in adolescents’ WCU from middle childhood through adolescence is also important as WCU in the immediate prior period (middle childhood) may influence adolescents’ subsequent WCU given household-level preventive care proclivities.20
Addressing these gaps, this study’s main goal is to explore prospective WCU patterns from ages 5 to 17 years stratified by sex using the National Longitudinal Survey of Youth (NLSY79) Child/Young Adult component. This study also explores factors associated with adolescents’ longitudinal WCU, including race/ethnicity, mother’s education, health insurance, and birth cohort. Facilitating pediatric to adult healthcare transitions, contingent on adolescents’ WCU engagement, will not be successful if WCU declines before adolescence. Evaluating longitudinal WCU patterns is necessary to identify earlier intervention points for children disconnecting from health care before adolescence.
METHODS
Study Sample
Data were analyzed in 2019 using the publicly available NLSY79 sponsored by the Bureau of Labor Statistics and funded by the National Institute of Child Health and Human Development. Through the biennial survey Child/Young Adult component, a household-based child sample born to women from the original nationally representative NLSY79 sample were followed. Children eligible for this analysis (N=6,872; n=3,379 female, n=3,493 male) were born in 1980–1997 to women from the original NLSY79 and completed at-home surveys via trained interviewers and self-administered survey for sensitive information. Study procedures are described elsewhere.21 The Johns Hopkins University IRB approved this secondary analysis as exempt. Participants were included in analyses if they had WCU data at least once between ages 5 years (1986–2003) and 17 (1998–2015) years to explore WCU trajectories starting at school entry and to maximize available NLSY79 sample size.
Measures
For measures used in this study, mothers responded for children of all ages (5–17 years) and children aged ≥14 years completed their own surveys.
Seven WCU time points were collected every 2 years from age 5 through 17 years. At each assessment, respondents were asked: When did [child/adolescent] last see a doctor for a routine health check-up? Responses were coded as having WCU in the past 12 months or not. This measure used mother reports for children aged ≤13 years and self-reports for adolescents aged ≥14 years. Most adolescents reported WCU (80.9%); mother’s WCU reports replaced 15% of missing adolescent responses.
Cohort was treated as a time-varying variable with 9 biennial entry points where a new cohort became eligible at age 5 years (1986–2003), participating until age 17 years (1998–2015). Other covariates included race (non-Hispanic White/non-Hispanic Black), Hispanic ethnicity (yes/no), urbanicity (non-urban/urban), mother’s education at child’s birth (Grade 11 or less/high school degree or general educational development [GED]/college or more), and health insurance at age 5 years (none/insured).
Statistical Analysis
This study used longitudinal latent class analysis (LCA), a person-centered approach, to estimate typical WCU patterns across 7 time points using Mplus, version 8.23 Longitudinal LCA identifies distinct subgroups of individuals with similar response patterns on a series of indicator variables, permitting examination of change over time and produces the probability of individuals belonging to each class where the highest probability identifies an individual’s class membership. It also tests differences in levels of covariates across identified classes. Longitudinal LCA was chosen because little is known about the longitudinal shape of WCU from childhood through adolescence that would be required for growth modeling and it allows for more flexible estimation of longitudinal patterns.24,25
Model fit was identified by comparing goodness-of-fit indices that describe the relative fit of the proposed model with the data (i.e., Bayesian Information Criterion [BIC], sample size–adjusted BIC [BIC-SSA], and Akaike Information Criterion [AIC]) (Appendix Table 1).29 Index values may continue decreasing as additional classes are extracted even when not meaningfully different; thus, models with index values showing significant decrease compared to a k+1 class model29 were chosen using Vuong–Lo–Mendell–Rubin log likelihood ratio test (LRT)30 and bootstrap LRT (BLRT).31 Secondary model characteristics that also informed model selection included entropy and class separation and homogeneity of class probabilities (Appendix Table 1 provides additional descriptions).
Models were stratified by sex (male/female) given prior work demonstrating sex differences in prospective WCU15 and given multiple group model analysis that demonstrated significant differences in model fit and class structure by sex. In each sex-specific model, all covariates (i.e., cohort, race/ethnicity, urbanicity, mother’s education, insurance) were added simultaneously as predictors of class structure, producing results that indicate differences in the level that each covariate has across identified classes. Cohort and mother’s education were entered as continuous variables; insurance and urbanicity were entered as discrete variables. The publicly available race/ethnicity was contrast coded so that each race/ethnicity identity was compared to all other participants. Fit statistics are presented for models with all covariates and did not differ substantially for models with and without covariates.
A model where insurance was included as time varying was considered and multiple-group LCA models where differences in class structure were considered between private and public insurance types. Insurance demonstrated very little change across childhood and adolescence (on average, participants demonstrated 5.6% change in insurance at each time point compared with age 5 years). Results did not substantially differ from models where insurance was time invariant (Appendix Table 2 and Appendix Figure 1) or when comparing private and public insurance types. For parsimony, results are presented for insurance as time invariant, measured at age 5 years, and classified as insured or not insured.
As well-care guidelines were introduced and pediatric insurance was expanded (e.g., Medicaid eligibility, Children’s Health Insurance Program in the mid-to-late 1990s,32,33 sensitivity analyses were conducted without the oldest birth cohort (born in 1980–1981 and turned age 17 years in 1998–1999, before these policies were released). Results did not substantially differ from when all cohorts were added. Multiple group comparison of longitudinal LCA for cohort 1 compared with Cohorts 2–9 showed that fit statistics were not significantly different (male adolescents: Δχ2=21.56, Δdf=22, p=0.49; female adolescents: Δχ2=37.32, Δdf=29, p=0.14). Thus, results are presented for the full sample.
Sensitivity analyses were conducted to explore the impact of shifting from mother to adolescent WCU report at age 14 years. Agreement between maternal and adolescent WCU report occurred 82% of the time, which was not significantly different overall (χ2=1.23, p=0.27) or for adolescent visits (age 14 years: χ2=0.24, p=0.62; age 16 years: χ2=0.06, p=0.87; age 18 years: χ2=0.59, p=0.46). Multiple group comparisons on longitudinal LCA models by sex that compared participants with and without agreement between adolescent and maternal WCU report showed fit statistics were not significantly different between models (male adolescents: Δχ2=47.24, Δdf=46, p=0.42; female adolescents: Δχ2=40.07, Δdf=29, p=0.08). Thus, models are presented with both mother and adolescent reports.
Given significant associations of birth cohort with class membership and the wide time period of this study, separate follow-up multinomial logistic regressions analyses were conducted to further explore the relationship between birth cohort and most likely class membership.34 The most engaged class and the first, oldest birth cohort served as reference groups.
Of the 6,872 participants meeting study inclusion criteria, 9% had missing data on urbanicity or insurance, reducing the analytic sample to 6,212 (n=3,074 female, n=3,138 male). Missingness occurred more frequently for Hispanics than other race/ethnicities, but was unrelated to other variables. Despite missingness, longitudinal LCA data coverage was sufficient with 85%–94% of data available for each variable in the model.35 Models used full information maximum likelihood estimation to reduce the impact of missing data.36
RESULTS
Half of respondents were female (49.5%) and non-Hispanic White (48.8%); 30.1% identified as non-Hispanic Black and 21.1% Hispanic. The majority (78.3%) lived in urban settings, had mothers with high school or more education (74.5%), and had health insurance (88.7%).
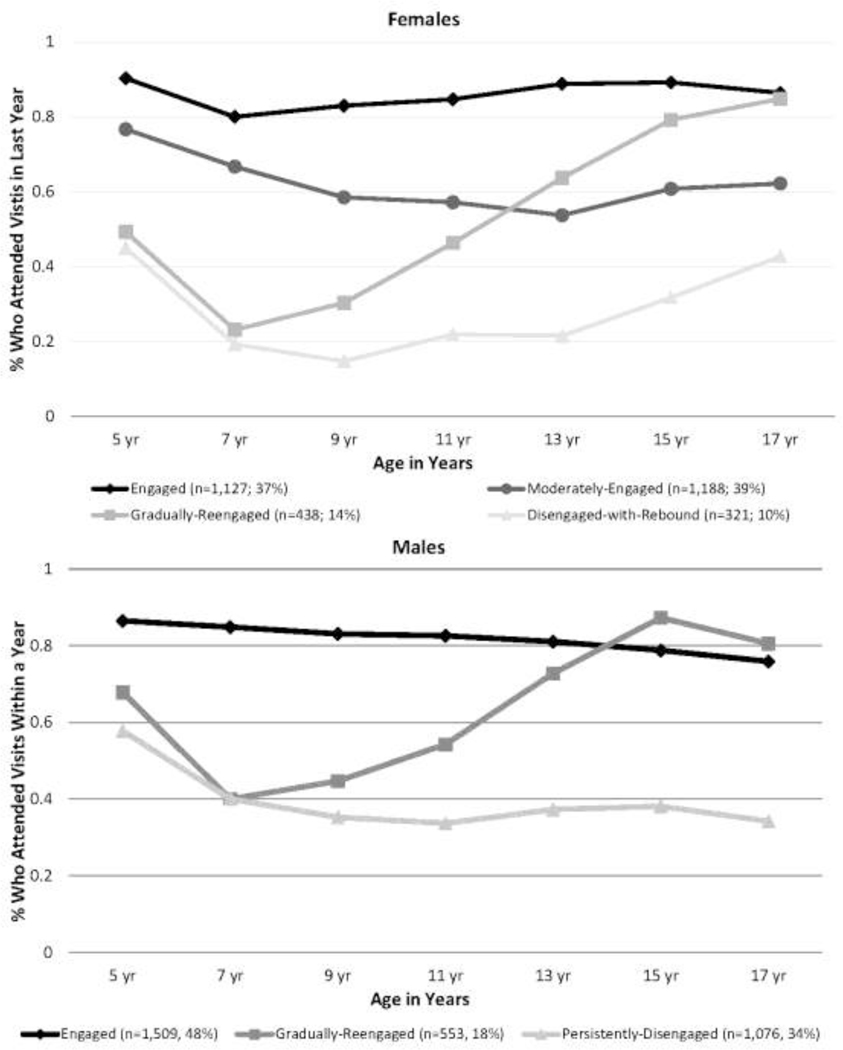
Goodness-of-fit indices aligned with 4 WCU classes for female adolescents and 3 for male adolescents (Appendix Table 1). For female adolescents, BLRT was not significant beyond 4 classes: The BIC, BIC-SSA, and AIC decreased substantially until 4 classes, where values demonstrated limited decreases thereafter. Although entropy was low across models, class membership posterior probabilities demonstrated adequate class separation (0.003–0.22) and class homogeneity (0.57–0.78). The female Engaged class (n=1,127, 37%) started at 90% WCU at age 5 years and was sustained over time (Figure 1). The female Moderately Engaged class (n=1,188, 39%) started at 77% WCU, declined to 54% by age 13 years, and increased to 62% by age 17 years. The female Gradually Re-engaged class (n=438, 14%) started at 49% WCU, steeply dropped to 23% at age 7 years, and increased to 85% by age 17 years. The female Disengaged-With-Rebound class (n=321, 10%) started at 45% WCU, declined to 15% at age 9 years, and rebounded to 43% by age 17 years.
Figure 1.
Proportion of adolescents’ well-care use over time by class and by sex.
For male adolescents, LRT was not significant beyond 3 classes. BIC, BIC-SSA, and AIC decreased substantially until 3 classes, where values demonstrated limited decreases thereafter. Although entropy was low in all models, posterior probabilities demonstrated adequate class separation (0.07–0.19) and class homogeneity (0.62–0.85). The male Engaged class (n=1,509, 48%) started at 87% WCU at age 5 years and declined to 76% over time (Figure 1). The male Gradually Re-engaged class (n=553, 18%) started at 68% WCU, dropped to 40% at age 7 years, but increased to 87% by age 15 years. The male Persistently Disengaged class (n=1,076, 34%) started at 58% WCU and declined to 34% over time.
Regarding comparative associations of covariates with well-care use classes by sex, for female adolescents, classes varied by all covariates except mother’s education (Table 1 summarizes rates of covariates across classes; Table 2 summarizes comparative associations of covariates with classes). Non-Hispanic Black female adolescents were significantly more likely to be in the Engaged versus Gradually Re-engaged or Disengaged-With-Rebound classes. Hispanic female adolescents were more likely to be in the Moderately Engaged versus Engaged class. Female adolescents living in urban areas were more likely to be in the Moderately Engaged than Gradually Re-engaged class. Female adolescents with insurance were more likely to be in the Moderately Engaged than Disengaged-With-Rebound class.
Table 1.
Overall Class Frequencies and Class Proportions by Covariates for Adolescents’ Well-Care Use Stratified by Sex
| Females (n=3,074) | Males (n=3,138) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Well-care use class | 1 | 2 | 3 | 4 | 1 | 2 | 3 | ||
| Total | Engaged | Moderately-engaged | Gradually-reengaged | Disengaged-with-rebound | Total | Engaged | Gradually-reengaged | Persistently-disengaged | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Class proportion Covariates | - | 1,127 (37) | 1,188 (39) | 438 (14) | 321 (10) | - | 1,509 (48) | 553 (18) | 1,076 (34) |
| Birth cohort (Year turned 17) | |||||||||
| 1980–81 (1998–99) | 354 (12) | 59 (17) | 190 (54) | 32 (9) | 73 (21) | 386 (12) | 119 (31) | 46 (12) | 221 (57) |
| 1982–83 (2000–01) | 472 (15) | 112 (24) | 214 (45) | 66 (14) | 80 (17) | 406 (13) | 157 (39) | 48 (12) | 201 (50) |
| 1984–85 (2002–03) | 438 (14) | 114 (26) | 206 (47) | 74 (17) | 44 (10) | 445 (14) | 180 (40) | 85 (19) | 180 (40) |
| 1986–87 (2004–05) | 417 (14) | 143 (34) | 155 (37) | 64 (15) | 55 (13) | 434 (14) | 196 (45) | 79 (18) | 159 (37) |
| 1988–89 (2006–07) | 389 (13) | 154 (40) | 139 (36) | 68 (17) | 28 (7) | 465 (15) | 228 (49) | 111 (24) | 126 (27) |
| 1990–91 (2008–09) | 367 (12) | 171 (47) | 130 (35) | 46 (13) | 20 (5) | 350 (11) | 210 (60) | 71 (20) | 69 (20) |
| 1992–93 (2010–11) | 293 (10) | 155 (53) | 79 (27) | 46 (16) | 13 (4) | 309 (10) | 198 (64) | 51 (17) | 60 (19) |
| 1994–95 (2012–13) | 161 (5) | 97 (60) | 39 (24) | 22 (14) | 3 (2) | 189 (6) | 116 (61) | 39 (21) | 34 (18) |
| 1996–97 (2014–15) | 183 (6) | 122 (67) | 36 (20) | 20 (11) | 5 (3) | 154 (5) | 105 (68) | 23 (15) | 26 (17) |
| Race/Ethnicity | |||||||||
| Non-Hispanic White | 1,502 (49) | 533 (36) | 496 (33) | 283 (19) | 190 (13) | 1,531 (48) | 604 (40) | 417 (27) | 510 (33) |
| Non-Hispanic Black | 940 (31) | 457 (49) | 332 (35) | 88 (9) | 63 (7) | 931 (30) | 586 (63) | 82 (9) | 263 (28) |
| Hispanic | 632 (21) | 137 (22) | 360 (57) | 67 (11) | 68 (11) | 676 (22) | 319 (47) | 54 (8) | 303 (45) |
| Urbanicity | |||||||||
| Urban | 2,383 (78) | 875 (37) | 1,004 (42) | 286 (12) | 218 (9) | 2,480 (79) | 1,253 (51) | 428 (17) | 799 (32) |
| Non-urban | 691 (23) | 252 (37) | 184 (27) | 152 (22) | 103 (15) | 658 (21) | 256 (39) | 125 (19) | 277 (42) |
| Mother’s education level | |||||||||
| 11th grade or less | 784 (26) | 226 (29) | 389 (50) | 81 (10) | 88 (11) | 800 (26) | 355 (44) | 52 (7) | 393 (49) |
| High school degree/GED | 1,207 (39) | 413 (34) | 480 (40) | 183 (15) | 131 (11) | 1,178 (38) | 545 (46) | 184 (16) | 449 (38) |
| College or more | 1,083 (35) | 488 (45) | 319 (29) | 174 (16) | 102 (9) | 1,160 (37) | 609 (53) | 317 (27) | 234 (20) |
| Health insurance | 2,726 (89) | 1,013 (37) | 1,106 (41) | 366 (13) | 241 (9) | 2,781 (89) | 1,392 (50) | 535 (19) | 854 (31) |
Note: Covariates were added as predictors of the class structure. Birth cohort and mother’s education at child’s birth were entered as continuous variables. Health insurance refers to insurance coverage when participants were age 5 years. Race/ethnicity, as assessed in the publicly available data, was dummy coded into the variables of “Non-Hispanic White”, Non-Hispanic black, and “Hispanic”. Each variable compares the identified race/ethnicity to all other individuals in the dataset. For example, individuals identifying as “Hispanic” are compared to all other individuals in the sample who identify as “Non-Hispanic White” and “Non-Hispanic Black”.
Table 2.
Comparative Associations of Covariates and Adolescents’ Well-Care Use Classes for Females
| Females | Engaged vs | Moderately-engaged vs | Gradually-reengaged vs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderately-engageda | Gradually-reengagedb | Disengaged-with-reboundc | Gradually-reengagedd | Disengaged-with-rebounde | Disengaged-with-reboundf | |||||||
| Covariates | b (SE) | OR | b (SE) | OR | b (SE) | OR | b (SE) | OR | b (SE) | OR | b (SE) | OR |
| Birth cohort | −0.22 (0.06)** | 0.80 | −0.17 (0.06)** | 0.84 | −0.42 (0.08)** | 0.66 | 0.05 (0.08) | 1.05 | −0.20 (0.08)* | 0.82 | −0.25 (0.10)* | 0.78 |
| NH Black vs all others (NH White and Hispanic) | −0.49 (0.35) | 0.62 | −0.88 (0.35)* | 0.42 | −1.18 (0.36)** | 0.31 | −0.39 (0.49) | 0.68 | −0.70 (0.46) | 0.50 | −0.31 (0.59) | 0.74 |
| Hispanic vs all others (NH Black and NH White) | 0.53 (0.26)* | 1.71 | −0.03 (0.37) | 0.97 | 0.13 (0.45) | 1.14 | −0.57 (0.36) | 0.57 | −0.40 (0.43) | 0.67 | 0.16 (0.55) | 1.17 |
| Urban vs non-urban residence | 0.23 (0.32) | 1.26 | −0.42 (0.25) | 0.66 | −0.40 (0.27) | 0.67 | −0.66 (0.32)* | 0.52 | −0.63 (0.34) | 0.53 | 0.02 (0.35) | 1.02 |
| Mother’s education level | −0.16 (0.15) | 0.85 | 0.07 (0.16) | 1.07 | 0.14 (0.17) | 1.15 | 0.23 (0.18) | 1.25 | 0.30 (0.21) | 1.35 | 0.07 (0.23) | 1.07 |
| Insured vs not insured | 0.59 (0.54) | 1.80 | −0.35 (0.39) | 0.70 | −0.60 (0.42) | 0.55 | −0.94 (0.51) | 0.39 | −1.19 (0.37)** | 0.30 | −0.25 (0.47) | 0.78 |
Note: Covariates were added as predictors of the class structure. Boldface indicates statistical significance (*p<0.05; **p<0.005). Birth cohort and mother’s education at child’s birth were entered as continuous variables. Health insurance refers to insurance coverage when participants were age 5. Race/ethnicity, as assessed in the publicly available data, was contrast coded into the variables of “Non-Hispanic White”/”Non-Hispanic Black”, and “Hispanic”. Each variable compares the identified race/ethnicity to all other individuals in the dataset. For example, individuals identifying as “Hispanic” are compared to all other individuals in the sample who identified as “Non-Hispanic White” or “Non-Hispanic Black”.
b=unstandardized logit; NH, non-Hispanic.
Male adolescents showed significant differences in class membership by all covariates (Tables 1 and 3). Non-Hispanic Black male adolescents were more likely to be in the Engaged versus other classes. Hispanic male adolescents were more likely to be in the Engaged versus Gradually Re-engaged class. Male adolescents living in urban areas were more likely to be in the Engaged than Persistently Disengaged class. Maternal education was significantly higher for male adolescents in the Engaged than other classes; those whose mothers had less education were more likely to be in the Persistently Disengaged than Gradually Re-engaged class. Male adolescents with insurance were more likely to be in the Engaged than Persistently Disengaged class.
Table 3.
Comparative Associations of Covariates and Adolescents’ Well-Care Use Classes for Males
| Males | Engaged vs | Gradually-reengaged vs | ||||
|---|---|---|---|---|---|---|
| Gradually-reengaged | Persistently-disengaged | Persistently-disengaged | ||||
| Covariates | b (SE) | OR | b (SE) | OR | b (SE) | OR |
| Birth cohort | −0.15 (0.06) * | 0.86 | −0.24 (0.03) ** | 0.79 | −0.08 (0.06) | 0.92 |
| NH Black vs all others (NH White and Hispanic) | −1.15 (0.27) ** | 0.32 | −0.81 (0.18) ** | 0.44 | 0.34 (0.28) | 1.40 |
| Hispanic vs all others (NH Black and NH White) | −0.89 (0.38) * | 0.41 | −0.12 (0.18) | 0.89 | 0.77 (0.41) | 2.16 |
| Urban vs non-urban residence | −0.13 (0.25) | 0.88 | −0.46 (0.15) ** | 0.63 | −0.36 (0.24) | 0.70 |
| Mother’s education level | 0.34 (0.17) * | 1.40 | −0.19 (0.09) * | 0.83 | −0.53 (0.17) ** | 0.59 |
| Insured vs not insured | 0.22 (0.59) | 1.24 | −0.73 (0.19) ** | 0.48 | −0.95 (0.54) | 0.39 |
Note: Covariates were added as predictors of the class structure. Boldface indicates statistical significance (*p<0.05; **p<0.005). Birth cohort and mother’s education at child’s birth were entered as continuous variables. Health insurance refers to insurance coverage when participants were age 5. Race/ethnicity, as assessed in the publicly available data, was contrast coded into the variables of “Non-Hispanic White”/”Non-Hispanic Black”, and “Hispanic”. Each variable compares the identified race/ethnicity to all other individuals in the dataset. For example, individuals identifying as “Hispanic” are compared to all other individuals in the sample who identified as “Non-Hispanic White” or “Non-Hispanic Black”.
b=unstandardized logit; NH, non-Hispanic.
Class membership significantly varied by birth cohort for both sexes with a visual trend of increased membership in Engaged classes across birth cohorts (Appendix Figure 2). Follow-up multinomial logistic regression analyses stratified by sex indicated that birth cohort year significantly predicted class membership (female adolescents: χ2(24)=371.35, p<0.001, Nagelkerke pseudo R2=0.13; male adolescents: χ2(16)=278.12, p<0.001, Nagelkerke pseudo R2=0.10). Female adolescents from the second through fifth cohorts were more likely to belong to the Engaged than other classes (p<0.05), except for the Gradually Re-engaged class. Male adolescents from all cohorts were more likely to belong to the Engaged than Persistently Disengaged class (p<0.001), except for the second cohort. No differences were observed across cohorts in male adolescents’ belonging to the Moderately Engaged than Engaged class.
DISCUSSION
This study, exploring WCU patterns from middle childhood through adolescence using longitudinal LCA stratified by sex, identified 4 WCU classes for female adolescents and 3 for male adolescents. WCU disengagement began during middle childhood for both sexes, rather than in adolescence, and for some, particularly male adolescents, WCU disengagement persisted throughout adolescence. Class membership by sex also varied by demographic covariates. In more recent birth cohorts, adolescents from both sexes were more likely to have Engaged class membership. Findings highlight the importance of examining longitudinal WCU patterns from childhood to adolescence and how the childhood/adolescence transition can be leveraged to increase WCU for both sexes.
This is one of the first studies to explore person-centered longitudinal WCU patterns from childhood through adolescence using a household-based sample. Whereas prior studies have described cumulative visits,12,13 the current study describes individual patterns of adolescents’ WCU engagement and disengagement over time. Findings highlight common vulnerability points for WCU engagement across development, especially after the visit at age 5 years, and subgroups who displayed consistent WCU disengagement, especially male adolescents. Innovative strategies may be needed to address WCU disengagement, especially during the childhood/adolescence transition, including considerations for how best to deliver well-care during this time. For example, developing communication strategies with providers, families, and youth about the importance of WCU from middle childhood through adolescence may sustain young adult WCU attendance. Emphasizing WCU, especially after the age 5 years visit tied to required school-entry vaccinations, may also be critical to prevent later WCU drop off. Leveraging pubertal issues and other school requirements (e.g., vaccinations, sports physicals) that may have triggered observed WCU increases for some adolescents, are also needed. It is important to collect and evaluate such longitudinal WCU data during childhood and adolescence to inform practice improvements.
Findings that demonstrated longitudinal differences in WCU classes for male and female adolescents suggesting increased WCU engagement over time for female adolescents extends findings from past cross-sectional work.13 Although disengagement appeared initially for both sexes, male adolescents were particularly prone to decreased WCU across adolescence. Further, more than one sixth of male adolescents (17%–20%) born in 1991–1997 still belonged to the Persistently Disengaged class whereas fewer female adolescents belonged to the similar Disengaged-With-Rebound class (3%–5%). Current study findings demonstrated that a large minority of male adolescents experienced WCU declines much earlier during middle childhood than previously described.8,17 Although past research does not elucidate well reasons for sex differences in adolescents’ care engagement, it is possible that male adolescents do not receive the same messages as female adolescents about healthcare engagement, especially related to sexual and reproductive health.37 Further research is needed to better understand lower WCU for male versus female adolescents. Study findings highlight the need for sex-specific approaches that keep male adolescents engaged in WCU during childhood and childhood/adolescence transition periods and beyond.
Findings indicated that mother’s educational status differentiated WCU class membership for male adolescents but not female adolescents. Mothers with lower education may place less value on connecting their sons to preventive care. Other work demonstrates that mothers may show greater involvement in daughter’s care given its alignment with their own health and gynecologic-related experiences (e.g., menstrual issues, contraception).38 Primary caregiver-focused educational approaches are needed to teach parents about the importance of well-care for their sons from childhood through adolescence.
Other covariate findings suggested that membership in classes with decreased WCU, regardless of participants’ sex, may reflect barriers in adolescents’ healthcare access especially among European-American adolescents living in rural areas with lower insurance coverage. Nearly 80% of federally designated medically underserved areas are located in rural areas, emphasizing the challenge some rural families face in accessing any healthcare let alone WCU.39 The longitudinal association between WCU engagement and insurance is not surprising, given its important role in past cross-sectional work. This study extends past insurance claims panel study findings that have not included uninsured adolescents. Greater class membership by non-Hispanic Blacks to the more engaged classes is also consistent with past study findings.16
Findings highlight that birth cohort was significantly associated with increased class membership for female adolescents over time, which was more gradual for male adolescents. This trend may indicate responsiveness to well-care guidelines and insurance coverage expansion in the mid-to-late 1990s,32,33 and potentially increased provider training on these guidelines. Future work should evaluate the role such guidelines and policies have had on increasing adolescents’ WCU over this period.
Limitations
This study has a number of limitations. This data set comprised participants’ mothers from a nationally representative sample of women aged 14–21 years in 1979 and children born from 1980 to 1997, representing a wide birth cohort. As national demographics have shifted since 1979, this sample of women and children may be less representative of current national demographics and does not include immigrant children or children born to immigrants after 1979. Future work should determine whether findings hold among a more contemporary longitudinal adolescent cohort that assesses WCU annually and across other measures not assessed herein (e.g., SES). This study’s WCU measure relies on adolescents’ and parents’ report, which may raise concerns about the validity of response. Sensitivity analyses with only mother report versus mother and adolescent report did not demonstrate any differences in WCU classes. Further, research shows that adolescents’ self-reported care receipt is valid40 and may capture appointments attended without a parent. Although models demonstrated low entropy values and classes may not represent fully homogeneous groups, entropy alone is not a reliable contributor to model selection; rather, using all model characteristics, including LRT and BLRT, is preferred for model selection. Despite these limitations, the NLSY79 is one of few longitudinal data sets that assesses WCU data from middle childhood through adolescence that allows for the description of longitudinal patterns of adolescents’ WCU and associated factors.
CONCLUSIONS
Findings highlight the utility of examining longitudinal patterns of adolescents’ WCU from childhood through adolescence and the timing and individuals who may benefit from WCU engagement. Results suggest that sex-specific strategies may be needed to enhance male adolescents’ WCU engagement during childhood and adolescence.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by Hopkins Population Center pilot funds (Principal Investigator [PI]: Dr. Marcell, from R24HD042854, PI: Dr. Hao) and by National Institute on Drug Abuse funds (PI: Pamela Matson, K01DA03538). The other authors (Drs. Van Eck and Madhuli Thakkar) have no disclosures. The study sponsor did not have any role in the study design, collection, analysis, and interpretation of data; writing the report; or the decision to submit the manuscript for publication. The findings and conclusions in this paper are those of the authors and do not necessarily present official positions of the NIH or the affiliated institutions.
Dr. Van Eck wrote the first draft of the manuscript and no honorarium, grant, or other form of payment was given to anyone else to produce the manuscript. None of the authors have any other disclosures. No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Elster A, Kuzsets N. American Medical Association Guidelines for Adolescent Preventive Services (GAPS). Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- 2.Green M, ed. Bright futures: Guidelines for health supervision of infants, children, and adolescents. Arlington, VA: National Center for Education in Maternal and Child Health; 1994. [Google Scholar]
- 3.National Committee for Quality Assurance. Health Plan Employer Data and Information Set (HEDIS) 3.0. Washington, DC; 1996. [Google Scholar]
- 4.Ozer EM, Adams SH, Orrell-Valente JK, et al. Does delivering preventive services in primary care reduce adolescent risky behavior? J Adolesc Health. 2011;49(5):476–482. 10.1016/j.jadohealth.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Harris SK, Aalsma MC, Weitzman ER, et al. Research on clinical preventive services for adolescents and young adults: where are we and where do we need to go? J Adolesc Health. 2017;60(3):249–260. 10.1016/j.jadohealth.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fortuna RJ, Halterman JS, Pulcino T, Robbins BW. Delayed transition of care: a national study of visits to pediatricians by young adults. Acad Pediatr. 2012;12(5):405–411. 10.1016/j.acap.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 7.Wisk LE, Finkelstein JA, Sawicki GS, et al. Predictors of timing of transfer from pediatric- to adult-focused primary care. JAMA Pediatr. 2015;169(6):e150951. 10.1001/jamapediatrics.2015.0951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marcell AV, Klein JD, Fischer I, Allan MJ, Kokotailo PK. Male adolescent use of health care services: where are the boys? J Adolesc Health. 2002;30(1):35–43. 10.1016/s1054-139x(01)00319-6. [DOI] [PubMed] [Google Scholar]
- 9.Rand CM, Goldstein NPN. Patterns of primary care physician visits for US adolescents in 2014: implications for vaccination. Acad Pediatr. 2018;18(2 suppl):S72–S78. 10.1016/j.acap.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Park MJ, Scott JT, Adams SH, Brindis CD, Irwin CE Jr. Adolescent and young adult health in the United States in the past decade: little improvement and young adults remain worse off than adolescents. J Adolesc Health. 2014;55(1):3–16. 10.1016/j.jadohealth.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 11.Adams SH, Park MJ, Twietmeyer L, Brindis CD, Irwin CE Jr. Increasing delivery of preventive services to adolescents and young adults: does the preventive visit help? J Adolesc Health. 2018;63(2):166–171. 10.1016/j.jadohealth.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Tsai Y, Zhou F, Wortley P, Shefer A, Stokley S. Trends and characteristics of preventive care visits among commercially insured adolescents, 2003–2010. J Pediatr. 2014;164(3):625–630. 10.1016/j.jpeds.2013.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med. 2010;8(6):511–516. 10.1370/afm.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dempsey AF, Freed GL. Health care utilization by adolescents on Medicaid: implications for delivering vaccines. Pediatrics. 2010;125(1):43–49. 10.1542/peds.2009-1044. [DOI] [PubMed] [Google Scholar]
- 15.Marcell AV, Matson P, Ellen JM, Ford CA. Annual physical examination reports vary by gender once teenagers become sexually active. J Adolesc Health. 2011;49(1):47–52. 10.1016/j.jadohealth.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams SH, Park MJ, Irwin CE Jr. Adolescent and young adult preventive care: comparing national survey rates. Am J Prev Med. 2015;49(2):238–247. 10.1016/j.amepre.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 17.Ziv A, Boulet JR, Slap GB. Utilization of physician offices by adolescents in the United States. Pediatrics. 1999;104(1):35–42. 10.1542/peds.104.1.35. [DOI] [PubMed] [Google Scholar]
- 18.Marcell AV, Ford CA, Pleck JH, Sonenstein F. Masculine beliefs, parental communication, and adolescent males’ health care use. Pediatrics. 2007;119(4):e965–e974. 10.1542/peds.2006-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selden TM. Compliance with well-child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000–2002. Pediatrics. 2006;118(6):e1766–e1778. 10.1542/peds.2006-0286. [DOI] [PubMed] [Google Scholar]
- 20.Thakkar MY, Hao L, Marcell AV. Adolescents’ and young adults’ routine care use: the role of their mothers’ care use behaviors. J Adolesc Health. 2019;64(1):107–115. 10.1016/j.jadohealth.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Longitudinal Survey of Youth, 1979. (NLSY79). Sample Design, National Longitudinal Surveys. Washington, DC: Bureau of Labor Statistics. https://www.nlsinfo.org/content/cohorts/nlsy79-children/intro-to-the-sample/sample-design. Accessed January 1, 2016. [Google Scholar]
- 22.National Opinion Research Center (NORC). NLSY-National Longitudinal Survey of Labor Force Behavior Interviewer’s Manual-Household Screening. Chicago, IL: National Opinion Research Center (NORC) - University of Chicago; 1978. [Google Scholar]
- 23.Muthén LK, Muthén BO. Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén; 2017. [Google Scholar]
- 24.Feldman BJ, Masyn KE, Conger RD. New approaches to studying problem behaviors: a comparison of methods for modeling longitudinal, categorical adolescent drinking data. Dev Psychol. 2009;45(3):652–676. 10.1037/a0014851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masyn KE. Latent class analysis and finite mixture modeling. In: Little TD, ed. The Oxford Handbook of Quantitative Methods in Psychology. Vol 2. New York, NY: Oxford University Press; 2013:551–611. 10.1093/oxfordhb/9780199934898.013.0025. [DOI] [Google Scholar]
- 26.Vermunt JK, Tran B, Magidson J. Latent class models in longitudinal research. In: Menard S, ed. Handbook of longitudinal research: Design, measurement and analysis. Burlington: Elsevier; 2008:373–385. [Google Scholar]
- 27.Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral and health sciences. New York, NY: Wiley; 2010. [Google Scholar]
- 28.Lanza ST, Collins LM. A mixture model of discontinuous development in heavy drinking from ages 18 to 30: the role of college enrollment. J Stud Alcohol. 2006;67:552–561. 10.15288/jsa.2006.67.552. [DOI] [PubMed] [Google Scholar]
- 29.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. 10.1080/10705510701575396. [DOI] [Google Scholar]
- 30.Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. 10.1093/biomet/88.3.767. [DOI] [Google Scholar]
- 31.McLachlan GJ, Peel D. Finite mixture models. New York, NY: Wiley; 2000. [Google Scholar]
- 32.Mann C, Rowland D, Garfield R. Historical overview of children’s health care coverage. Future Child. 2003;13(1):31–53. 10.2307/1602638. [DOI] [PubMed] [Google Scholar]
- 33.Rosenbaum S, Johnson K, Sonosky C, Markus A, DeGraw C. The children’s hour: the State Children’s Health Insurance Program. Health Aff (Millwood). 1998;17(1):75–89. 10.1377/hlthaff.17.1.75. [DOI] [PubMed] [Google Scholar]
- 34.Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 2nd Edition. Mahwah, NJ: Lawrence Erlbaum Associates; 1983. [Google Scholar]
- 35.Dumville JC, Torgerson DJ, Hewitt CE. Reporting attrition in randomised controlled trials. BMJ. 2006;332(7547):969–971. 10.1136/bmj.332.7547.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–576. 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 37.Marcell AV, Morgan AR, Sanders R, et al. The socioecology of sexual and reproductive health care use among young urban minority males. J Adolesc Health. 2017;60(4):402–410. 10.1016/j.jadohealth.2016.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Monnat SM, Wallington SF. Is there an association between maternal Pap test use and adolescent human papillomavirus vaccination? J Adolesc Health. 2013;52(2):212–218. 10.1016/j.jadohealth.2012.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bureau of Health Workforce Health Resources and Services Administration. Fourth Quarter of Fiscal Year 2019, Designated Health Professional Shortage Areas (HPSA) Statistics, Quarterly Summary. HHS. https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport. Published 2019. Accessed December 5, 2019. [Google Scholar]
- 40.Klein JD, Graff C, Santelli J, Hedberg V, Allan MJ, Elster A. Developing quality measures for adolescent care: validity of adolescents’ self-reported receipt of preventive services. Health Serv Res. 1999;34(1 Pt 2):391–404. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.