On the 1st of April 2021, French President Emmanuel Macron decided a new nation-wide lockdown to slow down the contamination rate (> 30 000 cases per day) and prevent an overwhelming of ICU capacities. At this date, in addition to non-COVID-19 patients, 5,109 COVID-19 patients were treated in ICUs across the country, while only 5,080 adult ICU beds were officially registered in the country at the end of 2019 by the “Direction de la Recherche, des Études de l’Évaluation et des Statistiques” (Table 1 ) [1], [2].
Table 1.
Bed availability in paediatric and adult Intensive Care Units (ICU), Acute Care Units (ACU), Continuous Care Units (CCU) in France in 2019 [2].
| Adults | ICU | ACU | CCU | Total |
|---|---|---|---|---|
| Public | 4,245 | 3621 | 4,589 | 12,455 |
| Private | 835 | 3,740 | 1,365 | 5,940 |
| Total | 5,080 | 7,361 | 5,954 | 18,395 |
| Paediatric | ||||
| Public | 332 | 812 | 0 | 1,144 |
| Private | 21 | 44 | 0 | 65 |
| Total | 353 | 856 | 0 | 1,209 |
| Adults & Paediatric | ||||
| Public | 4,577 | 4,433 | 4,589 | 13,599 |
| Private | 856 | 3,784 | 1,365 | 6,005 |
| Total | 5,433 | 8,217 | 5,954 | 19,604 |
In this context of scarcity of ICU resources, the President also proposed to increase the number of ICU beds to 10,000. However, unlike the situation encountered in March and April 2020, the national plan for healthcare institutions (named “Plan Blanc”, used in response to a disaster and/or exceptional sanitary event) was not applied, and there was no nationwide decision to postpone all elective non-urgent surgical and medical procedures. This raises two questions:
-
i)
How France can rapidly increase the ICU capacity from 5,080 to 10,000 beds?
-
ii)
How France can staff these newly created ICU beds with sufficiently trained ICU personnel?
Since it is not realistic to create de novo 5000 ICU beds in less than 1 month, the only option is to transiently transform non-ICU beds into ICU beds. In this context, a standardised procedure to create so-called “ephemeral ICU beds” should be described and agreed upon. In addition, the operational organisation of these “ephemeral” units should be specified.
Staffing, equipment and patient typology
In France, critically ill patients are managed in 3 types of hospital units [3], [4]:
-
i)
Intensive Care Units (ICU) are dedicated to patients with (or at risk of) at least two organ failures. In such units, organ suppliance can be provided whenever necessary and physicians have to be trained in anaesthesiology (anaesthesiologist) and/or intensive care medicine (intensivist). There is no mandatory bed-to-physician ratio. In general, during daytime, about 4 full-time physicians are required to operate a 10-bed ICU. For nursing, a ratio of 2 ICU nurses for 5 patients and 1 nursing auxiliary for 4 patients is a legal requirement in French ICUs.
-
ii)
Continuous Care Units (CCU) are dedicated to patients with only one organ failure specific to a particular medical specialty, e.g., coronary care units or stroke units [3], [4]. For coronary care units, the 2002 guidelines recommend a ratio of 1 nurse and 1 nursing auxiliary for 4 patients during daytime and at least 1 nurse and 1 nursing auxiliary for 8 patients at night.
-
iii)
Acute Care Units (ACU) (also called high-dependency units) are dedicated to patients at risk of developing an organ failure [3], [4]. ACUs are considered intermediate level of care units, i.e., between ICU and classical ward. This type of unit is mainly managed by anaesthesiologists, intensivists and other physicians with a specific expertise and/or training in ACU. Importantly, patients needing a single organ suppliance can be transiently managed in these units, meaning that they require 24/7 physician staffing. There is no specific staff/patient ratio, but during daytime there is in general 2 physicians for a 10-bed ACU.
According to the “Direction de la Recherche, des Études de l’Évaluation et des Statistiques”, 18,395 beds were available (in public and private institutions) in December 2019 in France to care for critically ill patients, including: 5,080 ICU beds, 7,361 ACU beds and 5,954 CCU adult beds (Table 1) [2].
In 2009, a cross-sectional cohort study performed in 66 ICUs in Southern France (695 ICU beds) reported a 90% median bed occupancy rate [5]. At admission, patients were 63 (median value) years old (interquartile [52–76]), had a SAPSII score of 46 [34–58] and more than 75% of them suffered at least 2 organ failures during their ICU stay. This is in contrast with the ICU population described in other countries where the proportion of patients with two or more organ failures is usually lower [6]. This can be explained by the fact that the ICU population in other countries is often a mix of French ICU, ACU and CCU patients.
Rapid ICU bed capacity increase in response to a crisis?
In order to rapidly increase the ICU capacity, one has to transform beds initially dedicated to other purposes. During the first wave, a study on 315 out of the 325 institutions with a registered ICU activity reported a 95% increase in ICU bed availability [7]. New ICU beds were created from ACUs (48%), Post Anaesthetic Care Units (PACUs) and Operating Theatres (OT) (32%) and other units (20%). As a consequence, ACU and PACU bed capacities decreased by 41 and 37%, respectively. This increase in the ICU capacity was associated with 74%, 70% and 45% increases in the number of ICU physicians, nurses and nursing auxiliaries respectively, and a 54% increase in the number of ventilators [7].
The increases in the number of physicians and ventilators were rendered possible by a dramatic decrease in the surgical activity [8], [9], [10]. Similar redeployments of hospital resources have been reported elsewhere [11], [12] and locally implemented during terror attacks [13], [14], [15].
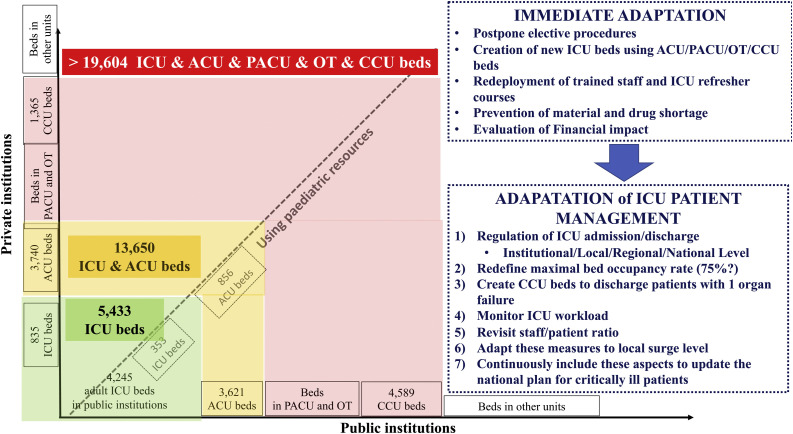
Hence, recent crises have demonstrated that increasing the number of ICU beds is possible if PACU and OT are transformed into ICUs (Fig. 1 ).
Fig. 1.
Availability of beds for critically ill patients and adaptations for increasing bed capacities.
ICU: Intensive Care Unit.
ACU: Acute Care Unit.
CCU: Continuous Care Unit.
PACU: Post Anaesthetic Care Unit.
OT: Operating Theatre.
Therefore, the real operational number of ICU, CCU and ACU beds can be transiently increased to over 20,000 during an acute crisis if all institutions are taken into account and if all elective procedural activities are cancelled or postponed. However, unpredictable emergencies (myocardial infarction, peritonitis, polytrauma etc.) still need to be taken care of and some elective procedures, such as cancer surgery or screening in high-risk situations do carry some degree of urgency. Therefore, maintaining a spare capacity to admit and treat any medical emergency and to perform some scheduled procedures is mandatory.
Increasing the ICU capacity requires to redeploy competent staff (physician, nurses) to the ICU from other areas of the hospital. The level of expertise and comfort of the staff deployed to work in the newly created units have not been formally evaluated, especially for the treatment of the most severe ICU patients requiring complex organ support techniques such as continuous renal replacement therapy (CRRT) or extra corporeal membrane oxygenation (ECMO). Redeployment capacities should be thought through in advanced by health care authorities with the idea that the permanent ICU staff has to be primarily engaged on treating the most severe patients in the highest acuity units, while redeployed personnel should be essentially asked to care for less acute patients, namely the one not requiring complex ICU techniques such as CRRT or ECMO. The true effective total ICU capacity in response to a crisis should be calculated following this concept. Finally, the longer-term financial and medical consequences of creating “ephemeral” units (and associated postponing or cancellation of other activities) on the healthcare system remains to be evaluated.
What can we do better?
-
-
How to optimise patient management during a sudden outbreak?
To contain the first outbreak in 2020, many solutions have been proposed and used:
In units rapidly overwhelmed (Eastern and Paris), many patients were transferred to other units in France or in foreign countries and a mobile military intensive care unit was deployed in Mulhouse [16], [17], [18], [19].
Some regions organised a daily assessment of regional bed capacity in order to balance ICU admissions over this area [20].
In institutions where “ephemeral” ICU beds were created, an initial triage was sometimes needed to admit the most critically ill patients in the ICU while less severe patients were treated in the newly created ephemerous units. This was done at the local (e.g., transfer of patients with only 1 organ failure from a regular ICU to an ephemeral ICU bed within the same institution) and at the regional level (triage of patients between ICU expert centres and other centres).
-
-
Which lessons can be learned from the COVID-19 pandemic? (Fig. 1).
One year into the pandemic, over 139 million COVID-19 cases were diagnosed causing nearly 3 million deaths worldwide and > 100,000 deaths in France [21]. A pandemic of this magnitude is very rare, the last one being the Spanish influenza in 1918−19 (300,000 deaths in France). Using 2018 International Health Regulations State Party Annual Reporting, Kantel et al. [22] reported that out of 182 countries analysed, only 104 (57%) were operationally ready to prevent, detect, and control an outbreak resulting from a novel infectious disease. The COVID-19 pandemic has demonstrated the need to improve our capacity to respond to any potential future health crisis. To do so, the following aspects need to be analysed and addressed.
First, the COVID-19 outbreak occurred in the context of ICUs that were already overwhelmed with a bed-occupancy rate chronically over 80–90%. In the past, French healthcare authorities have proposed 80% as a target for the ICU occupancy rate [23]. Targeting a lower bed-occupancy rate such as the one used in the US (75%) could increase ICU availability by 10–15% and result in more than 750 ICU beds available nationally.
Second, dedicating ICU beds only for patients with ≥ 2 organ failures is an open question. A single centre study has shown that a third of ICU hospitalisation days are used for managing patients with only one organ failure [24]. Opening more units capable of managing patients with single one organ failure would spare ICU beds by avoiding some patient admissions and facilitating ICU discharge when patients are improving. However, this would mechanically result in an increase in the ICU workload since these units would be reserved for patients with ≥ 2 organ failures. As a result, the ratio between staff and patients should be revisited. Indeed, managing only highly acute patients with ventilatory support, CRRT and ECMO is likely to require more than 2 nurses/5 patients as proposed by the French law back in 2002. Of course, revisiting the ICU bed capacities and staff ratios would lead to increase the cost of ICU care [25], [26]. The trend to revisit the management of critically ill patients with more high acuity beds is leading to increased costs, but is balanced by an increased proportion of come-and-go procedures and the development of enhanced recovery program after surgery, which should help contain costs. Altogether, this constitutes a profound transformation of the hospital, with higher proportion of critically ill patients [26].
Third, the COVID-19 outbreak has highlighted the need for more local and regional management of the ICU bed capacity [20] involving both public and private institutions and all physicians implied in the management of the critically ill patients (anaesthesiologists, intensivists, surgeons, and physician involved in Emergency Department and in patient transfer organisation).
Fourth, in case of sudden crisis such as a pandemic, “healthcare workers reserve” trained for ICU practice and ready to take-over and reinforce permanent ICU staff could be planned.
Planning for the next sanitary crisis is of paramount importance. Creating more ICU beds is probably not the only answer. If taken in isolation, such a measure will likely prove inefficient and put additional strain on the finance of our national health care system. A more global rethinking of the trajectory of critically-ill patients is warranted. This new vision for critical care has to be embraced by healthcare professionals as well as by politics.
Conflict of interest
The authors have no conflicts of interest to declare.
References
- 1.https://www.gouvernement.fr/info-coronavirus/carte-et-donnees.
- 2.Nombre de lits de réanimation, de soins intensifs et de soins continus en France, fin 2013 et 2019. https://drees.solidarites-sante.gouv.fr/article/nombre-de-lits-de-reanimation-de-soins-intensifs-et-de-soins-continus-en-france-fin-2013-et 2019.
- 3.Décret n° 2002-466 du 5 avril 2002 relatif aux conditions techniques de fonctionnement auxquelles doivent satisfaire les établissements de santé pour pratiquer les activités de réanimation, de soins intensifs et de surveillance continue et modifiant le code de la santé publique. https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000000585557.
- 4.Leone M., Constantin J.M., Dahyot-Fizelier C., Durachet-Gout C., Joannes-Boyau O. French intensive care unit organisation. Anaesth Crit Care Pain Med. 2018;37:625–627. doi: 10.1016/j.accpm.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Constantin J.M., Jaber S., Allaouchiche B., Orban J.C., Cannesson M. Activity and the available human resources working in 66 French Southern intensive care units. Ann Fr Anesth Reanim. 2010;29:512–517. doi: 10.1016/j.annfar.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Lilly C.M., Zuckerman I.H., Badawi O., Riker R.R. Benchmark data from more than 240,000 adults that reflect the current practice of. Critical care in the United States. Chest. 2011;140:1232–1242. doi: 10.1378/chest.11-0718. [DOI] [PubMed] [Google Scholar]
- 7.Lefrant J.Y., Fischer M.O., Potier H., Degryse C., Jaber S., Muller L. A national healthcare response to intensive care bed requirements during the COVID-19 outbreak in France. Anaesth Crit Care Pain Med. 2020;39:709–715. doi: 10.1016/j.accpm.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Assistance Publique–Hôpitaux de Paris’response to the COVID-19 pandemic, Hirsch M., the COVID19 APHP group Lancet. 2020;395(10239) doi: 10.1016/S0140-6736(20)31210-1. 1760–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harkouk H., Jacob C., Fletcher D. Urgent development of an anaesthesiology-based intensive care unit for critical COVID-19 infected patients. Anaesth Crit Care Pain Med. 2020;39:359–360. doi: 10.1016/j.accpm.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gouel-Cheron A., Couffignal C., Elmaleh Y., Kantore E., Montravers P. Preliminary observations of anaesthesia ventilators use for prolonged mechanical ventilation in intensive care unit patients during the COVID-19 pandemic. Anaesth Crit Care Pain Med. 2020;39:371–372. doi: 10.1016/j.accpm.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fagiuoli S., Lorini F.L., Remuzzi G., Covid-19 Bergamo Hospital Crisis Unit Adaptations and lessons in the province of Bergamo. N Engl J Med. 2020;382:e71. doi: 10.1056/NEJMc2011599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peters A.W., Chawla K.S., Turnbull Z.A. Transforming ORs inti ICUs. N Engl J Med. 2020;382:e52. doi: 10.1056/NEJMc2010853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cushman J.G., Pachter H.L., Beaton H.L. Two New York city hospitals’ surgical response to the September 11, 2001, terrorist attack in New York City. J Trauma. 2003;54:147–154. doi: 10.1097/00005373-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Hirsh M., Carli P., Nizard R., Riou B., Baroudjian B., Baubet T. The medical response to multisite terrorist attacks in Paris. Lancet. 2015;386:2535–2538. doi: 10.1016/S0140-6736(15)01063-6. [DOI] [PubMed] [Google Scholar]
- 15.Orban J.C., Quintard Ichai C. ICU specialists facing terrorist attack: the nice experience. Intensive Care Med. 2017;43:683–685. doi: 10.1007/s00134-016-4570-6. [DOI] [PubMed] [Google Scholar]
- 16.Collange O., Sammour Y., Soulié R., Castelain V., Mertes P.M. ICU re-organisation to face the first COVID-19 epidemic wave in a tertiary hospital. Anaesth Crit Care Pain Med. 2020;39(December (6)):731–732. doi: 10.1016/j.accpm.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boutonnet M., Turc J., Dupre H.L., Paris R., Muller V. “MoRPHEE” fighting COVID-19. Anaesth Crit Care Pain Med. 2020;39(3):363–364. doi: 10.1016/j.accpm.2020.05.002. S2352-5568: 30085-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Painvin B., Messet H., Rodriguez M., Lebouvier T., Chatellier D., Soulat L. Inter-hospital transport of critically ill patients to manage the intensive care unit surge during the COVID-19 pandemic in France. Ann Intensive Care. 2021;11:54. doi: 10.1186/s13613-021-00841-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Danguy des Déserts M, Mathais Q., Luft A., Escarment J., Pasquier P. Conception and deployment of a 30-bed field military intensive care hospital in Eastern France during the 2020 COVID-19 pandemic. Anaesth Crit Care Pain Med. 2020;39(3):361–362. doi: 10.1016/j.accpm.2020.04.008. S2352-5568: 30075-30078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terrasi B., Arnaud E., Guilbart M., Besserve P., Mahjoub Y. French ICUs fight back: an example of regional ICU organisation to tackle the SARS-CoV-2 outbreak. Anaesth Crit Care Pain Med. 2020;39(3):355–357. doi: 10.1016/j.accpm.2020.03.018. S2352-5568: 30058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.https://covid19.who.int.
- 22.Kandel N., Chungong S., Omaar A., Xing J. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. Lancet. 2020;395:1047–1053. doi: 10.1016/S0140-6736(20)30553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Circulaire DHOS/SDO n° 2003-413 du 27 août 2003 relative aux établissements de santé publics et privés pratiquant la réanimation, les soins intensifs et la surveillance continue. https://solidarites-sante.gouv.fr/fichiers/bo/2003/03-45/a0453485.htm.
- 24.Roger C., Julie-Bibi S., Fages M., Castelli C., Jeannes P., Saissi G. Patients de réanimation, journées de réanimation? Modélisation d’un fonctionnement optimisé des unités de réanimation, de soins intensifs et de surveillance continue et conséquences sur les suppléments tarifaires induits. [ICU patients and days of intensive care: A mathematical model optimizing the consequences of ICU unit function, intensive care and continual monitoring on incurred supplementary costs] Annales Françaises d’Anesthésie Réanimation. 2013;32:742–748. doi: 10.1016/j.annfar.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 25.Halpern N.A., Pastores S.M. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;17:65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 26.Vincent J.L. Critical care - where have we been and where are we going? Crit Care. 2013;17(Suppl. 1):S2. doi: 10.1186/cc11500. [DOI] [PMC free article] [PubMed] [Google Scholar]