Abstract
Prevention strategies for COVID-19 transmission are at the forefront of healthcare paradigms worldwide, the main emphasis of which is vaccination. We present an interesting case of a 37-year-old man who, 3 weeks following his first dose of the chimpanzee adenovirus-vectored COVID-19 vaccine, ChAdOx1, presented to hospital with a rapidly progressive ascending muscle weakness and back pain in the absence of any other triggers. He also had a negative COVID-19 swab during admission. A diagnosis of Guillain-Barre syndrome was confirmed by correlating the clinical features with cerebrospinal fluid analysis, nerve conduction studies and MRI of the brain and whole spine. The patient received treatment with 5 days of intravenous immunoglobulin and did not require any respiratory support. He was also regularly reviewed by a multidisciplinary team consisting of neurologists, speech and language therapists, and physiotherapists and is on the course to a recovery.
Keywords: healthcare improvement and patient safety, vaccination/immunisation, neurology, radiology, COVID-19
Background
The COVID-19 pandemic has proven to be a monumental challenge for healthcare services worldwide and is widely considered as a global public health threat. The causative organism, which is a highly transmissible novel respiratory pathogen called SARS-CoV-2, initially emerged in Wuhan, China, in late 2019.1 Since then, the disease has rapidly disseminated across several continents, claiming approximately 2.5 million deaths worldwide as of early March 2021 according to the WHO.2 Clinical presentations vary considerably depending on age, ethnicity and comorbidities from completely asymptomatic individuals to symptoms, such as dry cough, fever, anosmia, headache, myalgia and gastrointestinal disturbance. In critical cases, COVID-19 can cause a rapidly progressive pneumonitis or acute respiratory distress syndrome as well as multiorgan failure; which poses a considerable strain on intensive care and high dependency units globally.
Despite recent evidence to support mortality benefit with dexamethasone and tocilizumab, the main focus worldwide is to prevent disease transmission using strategies, such as social distancing, contact tracing, travel restrictions, personal protective equipment and more recently vaccination. There are currently three vaccinations against COVID-19, which have been approved by the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK.3 These are Oxford/AstraZeneca ChAdOx1, Pfizer/BioNTech BNT162b2 and Moderna mRNA-1273, with the UK supporting a global clinical trial for the recently Food and Drugs Administration (FDA) and European Medicines Agency (EMA) approved Janssen Ad26.COV2-S (recombinant) vaccine, with several more trials in the pipeline. The reported side effects following the ChAdOx1 vaccination include, but are not limited to, pain, injection site erythema, swelling, fatigue, headache, fever and lymphadenopathy.4
Guillain-Barre syndrome (GBS) is an acute, autoimmune demyelinating polyneuropathy characterised by progressive, proximal spreading muscle weakness. This is often self-resolving; however, in severe cases, it can be life-threatening secondary to respiratory muscle compromise, requiring mechanical ventilation.5 There have been a few reported cases documenting a possible link between COVID-19 and neurological manifestations, such as GBS, although an uncommon association.6–9 We describe a fascinating case of a 37-year-old man who was diagnosed with GBS 3 weeks post the first dose of the ChAdOx1 vaccine, in the absence of any other triggering factors.
Case presentation
A 37-year-old British Caucasian man, with no medical or travel history, received a first dose of the COVID-19 ChAdOx1 vaccine secondary to an opportunistic vaccine roll-out for younger people at a local centre. Approximately 2 weeks following the vaccination, the patient developed persistent back pain, new onset of distal paraesthesia within the hands and feet alongside a symmetrical, progressive ascending muscle weakness, presenting to accident and emergency a week later. The patient denied coryzal symptoms, urine or bowel incontinence, or preceding respiratory or gastrointestinal symptoms. He also denied previously contracting COVID-19 or having any of the typical symptoms associated with the infection since the beginning of the pandemic.
The neurological examination findings demonstrated reduced motor strength in all four limbs (table 1), with decreased light touch sensation and proprioception in the lower limbs from the groin distally. The patient also had an ataxic gait on heel-to-toe walking and was areflexic bilaterally in the lower limbs. His pupils were equal and reactive to light and the examination of cranial nerves I–XII was also unremarkable. The Glasgow Coma Score was 15/15. Cardiorespiratory and abdominal examinations were normal.
Table 1.
Neurological examination on admission documented with the Oxford Medical Research Council (MRC) criteria
| Motor function | Right | Left |
| Shoulder abduction | 3 | 3 |
| Shoulder adduction | 4 | 5 |
| Elbow flexion | 3 | 3 |
| Elbow extension | 4 | 4 |
| Wrist extension | 5 | 5 |
| Wrist flexion | 4 | 4 |
| Extensor digitorum | 4 | 4 |
| Flexor pollicis longus | 5 | 5 |
| Hip flexion | 3 | 3 |
| Hip extension | 5 | 5 |
| Knee flexion | 3 | 5 |
| Knee extension | 3 | 5 |
| Ankle dorsiflexion | 4 | 4 |
| Ankle plantar flexion | 5 | 5 |
| Extensor hallucis longus | 4+ | 4 |
His vital signs were as follows: temperature 36.9°C, pulse rate 118 beats/min, blood pressure 148/89 mm Hg, respiratory rate 21 breaths/min and an oxygen saturation of 96%. He had a normal forced vital capacity (FVC) on admission, which measured 3.13 L.
Investigations
On the day of admission, laboratory findings were within normal range as follows: haemoglobin 168 g/L (135–180 g/L), white cell count 8.42×109/L (3.5–11×109/L), platelet count 311×109/L (140–400×109/L), neutrophil count 6.17×109/L (1.7–7.5×109/L), lymphocyte count 1.52×109/L (1–4×109/L), monocyte count 0.69×109/L (0.2–1.5×109/L), sodium 143 mmol/L (135–145 mmol/L), potassium 4.2 mmol/L (3.5–5.1 mmol/L), urea serum 3.5 mmol/L (2.1–7.1 mmol/L), creatinine 69 μmol/L (66-112 μmol/L), estimated glomerular filtration rate >90 mL/min, bilirubin serum 11 μmol/L (0–21 μmol/L), alanine aminotransferase 15 U/L (10–50 U/L), aspartate aminotransferase 20 U/L (10-50 U/L), alkaline phosphatase 82 U/L (0–129 U/L), albumin serum 48 g/L (35–50 g/L) and C reactive protein of 1 mg/L (0–5 mg/L). The vitamin B12 serum was 673 ng/L (160–925 ng/L), folate 10.4 μg/L (2.9–50 μg/L), free T4 plasma 21.3 pmol (12–22 pmol) and thyroid stimulating hormone serum 1.82 mU/L (0.3–4.2 mU/L).
A blood-borne viral screen was negative, including the hepatitis screen, Epstein-Barr virus (EBV) and cytomegalovirus (CMV). Furthermore, antinuclear and antineutrophil cytoplasmic antibody serology tests were also negative. On admission to hospital, he was tested negative for COVID-19 on PCR swab. A chest radiograph during admission demonstrated clear lungs and pleural spaces, with no radiological features to indicate COVID-19 pneumonitis (figure 1).
Figure 1.
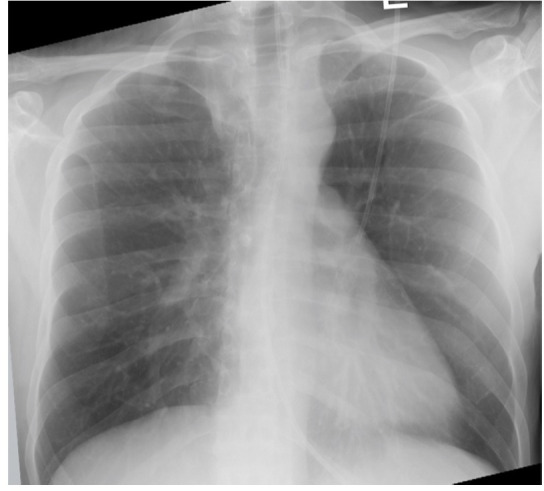
Chest radiograph on admission illustrating a normal cardiomediastinal outline as well as clear lungs and pleural recesses. No radiographic features of COVID-19 are demonstrated.
A lumbar puncture was performed, the results of which revealed a 0.5 mL colourless sample of fluid with an isolated elevated protein level of 1.77 g/L (0.15–0.45). Cerebrospinal fluid (CSF) glucose was 3.9 mmol/L, white cell count <0.001 ×109/L and red blood cell <0.001 ×109/L. In addition, microbiology and culture of the CSF sample yielded no growth of organisms. Oligoclonal band studies illustrated a pattern consistent with a passive transfer of oligoclonal IgG from a systemic inflammatory response and was not indicative of intrathecal synthesis (typically seen in conditions such as multiple sclerosis).
A nerve conduction study showed patchy attenuation of the upper limb motor responses on direct stimulation. No definitive features to suggest demyelination were identified at the time of study; however, it was noted that the study was performed at a slightly early, and therefore, suboptimal time in the suspected clinical course of GBS.
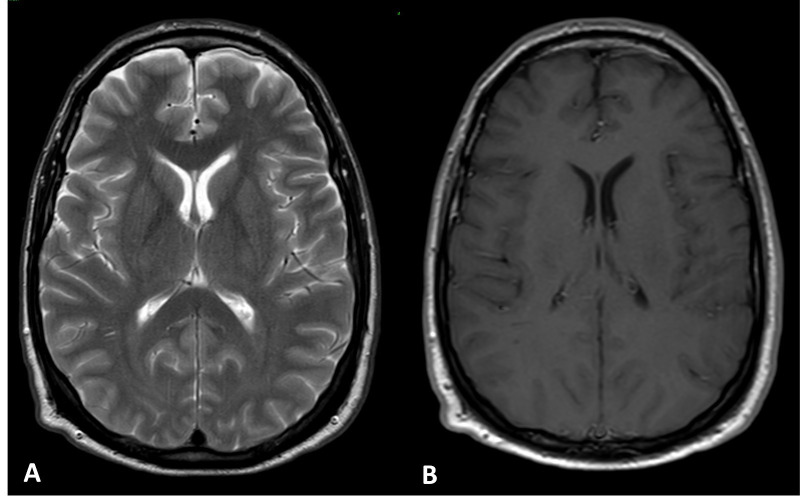
A MRI head demonstrated normal appearances of the brain parenchyma, ventricles and subarachnoid spaces. Gadolinium-enhanced T1-weighted images depicted no abnormal parenchymal, pachymeningeal or leptomeningeal enhancement (figure 2). Furthermore, a MRI whole spine with gadolinium contrast illustrated globally thickened cauda equina nerve rootlets bilaterally, particularly at the level of S1 (figure 3). On the sagittal postcontrast T1 sequence, there was prominent ventral cauda equina nerve root enhancement as well as pial enhancement of the conus medullaris (figure 4). The MRI features were in keeping with an underlying autoimmune aetiology. The clinical picture, CSF analyses, nerve conduction study and MRI features all supported a diagnosis of GBS.
Figure 2.
(A) T2-weighted and (B) postcontrast T1-weighted axial images of the brain. (A) Normal appearance of the brain parenchyma, ventricles and subarachnoid spaces on the T2-weighted image. (B) Postcontrast T1-weighted image demonstrates no abnormal parenchymal, pachymeningeal or leptomeningeal enhancement.
Figure 3.
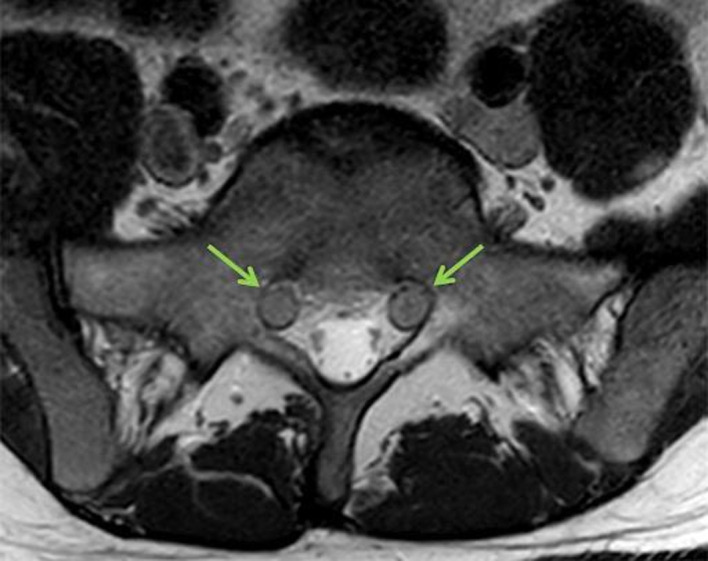
Axial T2-weighted image of the lumbosacral spine demonstrating bilateral, symmetrically thickened S1 nerves (green arrows).
Figure 4.
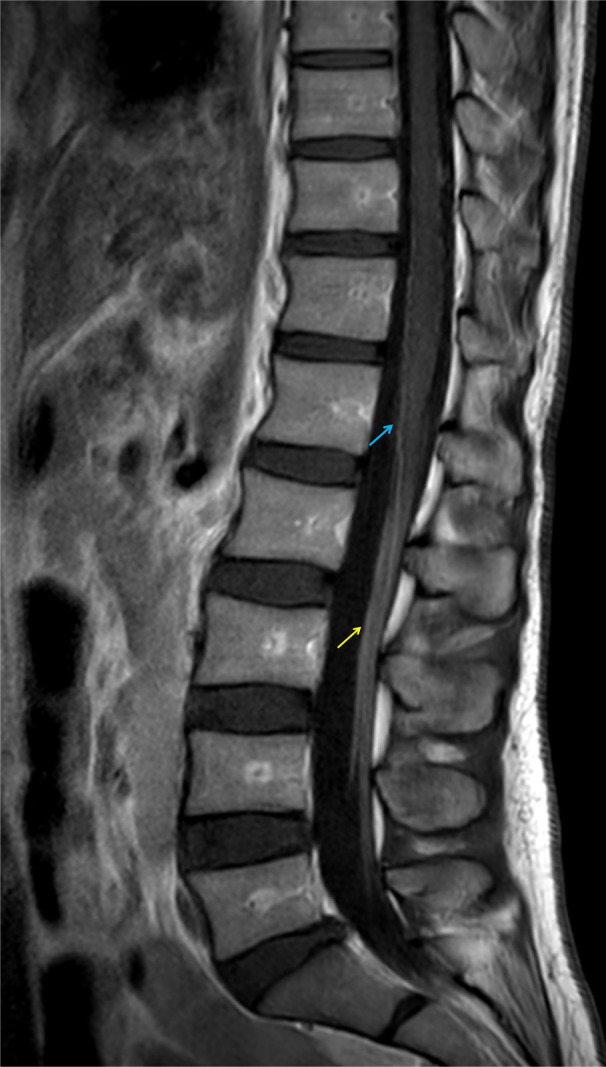
Postcontrast sagittal T1-weighted image showing enhancement of the cauda equina nerves, most pronounced at the ventral aspect (yellow arrow). In addition, there is evidence of pial enhancement at the conus medullaris (blue arrow). These imaging features are consistent with an underlying autoimmune aetiology.
Treatment
The patient was admitted for FVC monitoring every 4 hours and commenced on intravenous immunoglobulin (IVIg) with a dose of 2 g/kg daily for a total duration of 5 days. Amitriptyline 25 mg once daily was prescribed for neuropathic pain. On day 3 of treatment with IVIg, the patient’s FVC deteriorated to 2.6 L and a decision was made for a pre-emptive admission to intensive care for monitoring in the event he required mechanical ventilation. The patient was closely monitored in intensive care and received regular input from the neurology, speech and language, and physiotherapy teams. He was also started on temporary supplemental nutritional support via a nasogastric tube due to concerns regarding his swallowing.
Outcome and follow-up
We are pleased to report that the patient successfully completed a 5-day course of IVIg and did not require any mechanical ventilation in intensive care. His neurological symptoms, however, have been slow to recover and he is currently under observation in a quaternary neurology centre, receiving ongoing specialist neurology and physiotherapy input regarding the management of GBS.
Discussion
GBS is an autoimmune condition characterised by an acute, ascending peripheral polyradiculoneuropathy. Approximately 30% of patients exhibit respiratory muscle involvement and require admission to the intensive care unit for ventilatory support.5 The typical presenting features include an ascending flaccid paralysis, with some patients experiencing autonomic dysfunction. The classically reported stimulus for the development of GBS is a recent preceding bout of respiratory or gastrointestinal illness. Culprit pathogens, such as Campylobacter jejuni, CMV, EBV and Zika virus are well recognised in the literature as having a role in GBS development through a targeted secondary immune-mediated response against myelin sheaths triggered via a process of molecular mimicry.9
COVID-19 predominantly affects the respiratory system, sharing a common human coronavirus classification with SARS-CoV and the Middle East respiratory syndrome and having the potential to affect the nervous system.10 There are a few cases, which have been published correlating COVID-19 infection with the development of GBS,6–9 nonetheless there is limited data pertaining to the neurological outcome or the severity of symptoms for these patients. There are also several proposed mechanisms relating to the viral pathogenesis that may lead to the development of neurology symptoms. One theory is that ACE2 receptor expressed on the cell surface of the blood–brain barrier, glial cells and neurons is harnessed for viral entry and attack.11 Second, COVID-19 likely propagates a systemic inflammatory response on binding to pulmonary epithelium, releasing tumour necrosis factor alpha and interleukin (IL)-6, IL-12, IL-15, all of which can result in cytokine-induced neuronal injury. Furthermore, hypoxaemia secondary to a COVID-19 respiratory insult can result in cerebrovascular vasodilation, which can, therefore, result in cerebral oedema.11
With the ongoing pandemic, the COVID-19 vaccine roll-out has been of the utmost priority. Although there are clearly several proposed benefits to vaccination in terms of public health, the identification and declaration of potential risks is also imperative. The two approved vaccines currently undergoing mass rollout campaigns within the UK are Pfizer/BioNTech BNT162b2,3 12 and Oxford/AstraZeneca ChAdOx1.3 13 The Janssen Ad26.COV2-S (recombinant) vaccine has been recently approved by the EMA and US FDA; however, it is awaiting roll-out in the UK.14 15 Numerous previously established and tested vaccines caution patients about the extremely rare risk of GBS, likewise the ChAdOx1 vaccine forewarns patients that longer term side effects, such as GBS are extremely rare.16 During the 1976 influenza vaccination roll-out for swine influenza, an increased association with GBS was reported. In contrast, subsequent studies have reported no causal relationship between GBS and seasonal influenza vaccines with a probability of one case/million.17 Furthermore, a meta-analysis following the 2009 H1N1 monovalent influenza vaccination reported GBS incidence rates of 1.6 cases/million.17 Nonetheless, the uptake of the seasonal influenza vaccine is encouraged as the serious risk of mortality or morbidity from influenza significantly outweighs the risk of developing GBS. The Public Health England have reported that a single dose of either approved COVID-19 vaccine is 80% successful at reducing hospital admissions for patients above the age of 80 years in the 3 weeks following the first dose.18 The preliminary results from the phase III clinical trials for the ChAdOx1 vaccine reported it as being safe with no hospital admissions more than 22 days following the first dose.19 These statistics clearly demonstrate overall efficacy and improved outcomes following vaccination against COVID-19.
The COVID-19 virus has spike (S) proteins on its outer surface used for cell entry and trigger for disease. The ChAdOx1 vaccine is a ‘monovalent vaccine composed of a single recombinant, replication-deficient chimpanzee adenovirus (ChAdOx1) vector that codes for the S glycoprotein of SARS-CoV-2 (ChAdOx1-S (recombinant))’.13 On vaccination, the vector enters cells stimulating the S glycoprotein of COVID-19, which is then exported to the cell surface, provoking the production of antibodies and T cells. This process theoretically provides immunity for a further exposure to COVID-19 in the future, the duration of which is yet to be established. However, in selected patients, we postulate that this mechanism may be associated with a molecular mimicry response, therefore leading to the assembly of antibodies against neuronal myelin sheaths and resulting in GBS.
A meta-analysis and systematic review identified the reported yearly incidence of GBS within the general population of Europe and North America to be 0.81–1.89 (median 1.11)/100 000 people.20 Furthermore, the MHRA stated that 6 patients from 42 917 developed GBS following the ChAdOx1 vaccine, with no further information available.21 Additionally, one case of GBS was reported 2 weeks following the patient’s first dose of the BNT162b2 COVID-19 vaccine being administered.22 Similar to our case, the patient presented 2 weeks after their first dose of the vaccine, with a neurological sequelae consisting of areflexia, decreased pinprick sensation in the lower limbs and abnormal gait. The patient was diagnosed with GBS following elevated protein in the lumbar puncture and an MRI spine demonstrating enhanced cauda equina nerve roots. The team also treated the patient with 5 days of IVIgs, with neurological improvement following the third dose and subsequent discharge to an acute rehabilitation unit. In contrast, our patient did not show drastic improvement with IVIgs and the neurological deficit remained static. Research suggests that 40% of patients who have the standardised treatment of IVIg or plasma exchange do not show immediate recovery within the first 4 weeks.23
The authors acknowledge and cannot completely exclude the possibility of GBS occurring by chance or secondary to an asymptomatic infection. However, we are reassured that the patient did not have any prior respiratory or gastrointestinal symptoms, clinical features, laboratory evidence or radiological features of active localised infection as a cause for GBS. Since the only new potential trigger in his clinical history was a recent first jab of the ChAdOx1 vaccine and since it is well reported that GBS can occur a few weeks post vaccination in general, we believe there is a reasonable possibility that the ChAdOx1 vaccine was the potential stimulus for the development of GBS in this particular case. Further research and continual monitoring of the side effects and complications of COVID-19 vaccinations may provide some clarity into these possible associations in the near future.
Learning points.
Guillain-Barre syndrome (GBS) is an extremely rarely reported side effect and risk following any vaccination.
We describe a case of GBS following vaccination against COVID-19, in the absence of any further triggers.
Further research is required to adequately determine the possible link between COVID-19 vaccination, GBS and long-term neurological sequelae.
Footnotes
Contributors: SUP and RK played a lead role in conception, formulating and writing the manuscript. AL is a clinical fellow in intensive care who provided a detailed clinical history and reviewed the manuscript. BQ is a consultant neuroradiologist who provided expert opinion pertaining to the imaging features and reviewed the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer-reviewed.
References
- 1.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199–207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation [Internet] . WHO coronavirus disease (COVID-19) Dashboard, 2020. Available: https://covid19.who.int/
- 3.NHS England and NHS Improvement coronavirus [Internet] . Vaccination information from other organisations. Available: https://www.england.nhs.uk/coronavirus/covid-19-vaccination-programme/key-vaccination-information/
- 4.GOV.UK [Internet] . Information for UK recipients on COVID-19 vaccine Moderna, 2021. Available: https://www.gov.uk/government/publications/regulatory-approval-of-covid-19-vaccine-moderna/information-for-uk-recipients-on-covid-19-vaccine-moderna#possible-side-effects
- 5.Donofrio PD. Guillain-Barré syndrome. Continuum 2017;23:1295–309. 10.1212/CON.0000000000000513 [DOI] [PubMed] [Google Scholar]
- 6.Zhao H, Shen D, Zhou H, et al. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 2020;19:383–4. 10.1016/S1474-4422(20)30109-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sedaghat Z, Karimi N. Guillain Barre syndrome associated with COVID-19 infection: a case report. J Clin Neurosci 2020;76:233–5. 10.1016/j.jocn.2020.04.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virani A, Rabold E, Hanson T, et al. Guillain-Barré syndrome associated with SARS-CoV-2 infection. IDCases 2020;20:e00771. 10.1016/j.idcr.2020.e00771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med 2020;382:2574–6. 10.1056/NEJMc2009191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montalvan V, Lee J, Bueso T, et al. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin Neurol Neurosurg 2020;194:105921–7. 10.1016/j.clineuro.2020.105921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 2020;87:18–22. 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pfizer [Internet]. . Pfizer and BioNTech conclude phase 3 study of COVID-19 vaccine candidate, meeting all primary efficacy endpoints, 2020. Available: https://www.pfizer.com/news/press-release/press-releae-detail/pfizer-and-biontech-conclude-phase-3-study-covid-19-vaccine
- 13.Medicines and Healthcare products Regulatory Agency . Public Assessment Report Authorisation for Temporary Supply. COVID-19 Vaccine AstraZeneca, solution for injection in multidose container COVID-19 Vaccine (ChAdOx1-S [recombinant]). GOV.UK. Report number: Regulation 174, 2021.
- 14.European Medicines Agency [Internet] . COVID-19 vaccine Janssen, 2021. Available: https://www.ema.europa.eu/en/medicines/human/EPAR/covid-19-vaccine-janssen#authorisation-details-section
- 15.U.S. Food and Drug Administration [Internet] . Janssen COVID-19 vaccine, 2021. Available: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/janssen-covid-19-vaccine
- 16.North Central London COVID-19 Vaccine Pharmacy Group ed . Clinical information for vaccine consenters: AstraZeneca vaccine. National health service. Report number: version 1.4 2021.
- 17.Babazadeh A, Mohseni Afshar Z, Javanian M, et al. Influenza vaccination and Guillain-Barré syndrome: reality or fear. J Transl Int Med 2019;7:137–42. 10.2478/jtim-2019-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iacobucci G. Covid-19: Single dose of Pfizer and Oxford vaccines cuts risk of hospital admission by 80% in over 80s, data suggest. BMJ 2021;372:n612. 10.1136/bmj.n612 [DOI] [PubMed] [Google Scholar]
- 19.AstraZeneca [Internet] . COVID-19 Vaccine AstraZeneca confirms 100% protection against severe disease, hospitalisation and death in the primary analysis of Phase III trials, 2021. Available: https://www.astrazeneca.com/media-centre/press-releases/2021/covid-19-vaccine-astrazeneca-confirms-protection-against-severe-disease-hospitalisation-and-death-in-the-primary-analysis-of-phase-iii-trials.html#!
- 20.Sejvar JJ, Baughman AL, Wise M, et al. Population incidence of Guillain-Barré syndrome: a systematic review and meta-analysis. Neuroepidemiology 2011;36:123–33. 10.1159/000324710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Medicines and Healthcare products Regulatory Agency . COVID-19 vaccine AstraZeneca analysis print. GOV.UK.
- 22.Waheed S, Bayas A, Hindi F, et al. Neurological complications of COVID-19: Guillain-Barre syndrome following Pfizer COVID-19 vaccine. Cureus 2021;13:e13426. 10.7759/cureus.13426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leonhard SE, Mandarakas MR, Gondim FAA, et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat Rev Neurol 2019;15:671–83. 10.1038/s41582-019-0250-9 [DOI] [PMC free article] [PubMed] [Google Scholar]