Abstract
Introduction
Observational studies constitute an important evidence base for hypoglycemia in diabetes management. This requires consistent and reliable ascertainment and reporting methodology, particularly in studies of type 2 diabetes where hypoglycemia risk is heterogeneous. Therefore, we aimed to examine the definitions of hypoglycemia used by observational studies of patients with type 2 diabetes.
Research design and methods
We conducted a meta-epidemiological review of observational studies reporting on hypoglycemia or evaluating glucose-lowering medications in adults with type 2 diabetes. MEDLINE and Google Scholar were searched from January 1970 to May 2018. The definitions of non-severe, severe and nocturnal hypoglycemia were examined.
Results
We reviewed 243 studies: 47.7% reported on non-severe hypoglycemia, 77.8% on severe hypoglycemia and 16.9% on nocturnal hypoglycemia; 5.8% did not specify. Among 116 studies reporting non-severe hypoglycemia, 18.1% provided no definition, 23.3% used glucose values, 38.8% relied on patient-reported symptoms, 17.2% accepted either glucose values or patient-reported symptoms and 2.6% relied on International Classification of Disease (ICD) codes. Among 189 studies reporting severe hypoglycemia, 11.1% provided no definition, 53.4% required symptoms needing assistance, 3.7% relied on glucose values, 14.8% relied on ICD codes, 2.6% relied on ICD codes or glucose values and 15.9% required both symptoms needing assistance and glucose values. Overall, 38.2% of non-severe and 67.7% of severe hypoglycemia definitions were consistent with the International Hypoglycemia Study Group.
Conclusions
The marked heterogeneity in how hypoglycemia is defined in observational studies may contribute to the inadequate understanding and correction of hypoglycemia risk factors among patients with type 2 diabetes.
Keywords: hypoglycemia, epidemiology, diabetes mellitus, type 2, observational study
Significance of this study.
What is already known about this subject?
Since 2016, the International Hypoglycemia Study Group (IHSG) defined hypoglycemia severity levels and recommended their use for assessment and report in research studies.
The definitions of hypoglycemia used by randomized clinical trials of diabetes therapies are still diverse and inconsistent.
What are the new findings?
In the 243 observational studies of type 2 diabetes therapies reviewed, the hypoglycemia definitions reported were heterogeneous.
More than half of the observational studies published after the IHSG hypoglycemia definition were compliant with their recommendations.
Almost a fifth of the observational studies reporting hypoglycemia outcomes did not provide a specific definition for the event.
How might these results change the focus of research or clinical practice?
Heterogeneity in hypoglycemia definitions hinders the comparison of observational studies.
Using standardized hypoglycemia definition, ascertainment and reporting in observational studies could lead to a better comprehension of these events in a real-world setting, as well as supporting the development of better risk stratification and prevention strategies.
Introduction
Hypoglycemia is a serious and potentially preventable adverse event in diabetes management, leading to morbidity, impaired quality of life, high costs for patients and society, and death.1–3 While hypoglycemia is more common among people with type 1 diabetes,4–6 it also affects people with type 2 diabetes, particularly those with multiple or advanced comorbidities and those treated with insulin (including concentrated insulin) and/or insulin secretagogues.7–11 Efforts to better understand hypoglycemia risk factors and develop interventions for those at highest risk are predicated on reliably, accurately and consistently identifying events as they occur. In epidemiologic assessments and in research, such efforts have been hindered by the lack of standardized and universally used reporting parameters for clinically significant hypoglycemia.
The International Hypoglycemia Study Group (IHSG), on behalf of the American Diabetes Association (ADA) and European Association for the Study of Diabetes (EASD), has defined level 1 hypoglycemia as any glucose value ≤70 mg/dL (3.9 mmol/L), level 2 hypoglycemia as glucose <54 mg/dL (3.0 mmol/L) and level 3 (‘severe’) hypoglycemia as any glucose value associated with severe cognitive impairment requiring external assistance for recovery.12 13 Recognizing the importance of consistent and standardized reporting of hypoglycemia as an adverse event in diabetes management and data demonstrating marked variability in how hypoglycemia is described in clinical (ie, interventional) trials,14 the IHSG recommended that level 2–3 hypoglycemia, but not level 1 hypoglycemia, be reported in such trials.12 13 However, real-world data and observational studies also constitute an importance evidence base for clinical decision making.15 16 This is particularly important for an outcome like hypoglycemia, the incidence of which is likely to be higher in real-world settings than in closely monitored trials that enroll narrowly defined, and often lower risk, populations. Standardization of hypoglycemia reporting is therefore equally, or even more, important in observational studies and those that rely on real-world data.
To contextualize the existing evidence base regarding hypoglycemia, we examined and summarized the definitions of hypoglycemia used in observational studies centered on patients with type 2 diabetes. We focused specifically on type 2 diabetes because the risk of hypoglycemia in this population is more heterogeneous and treatment-dependent and context-dependent than in type 1 diabetes.7
Research design and methods
Data sources and selection
We conducted a meta-epidemiological review of the literature in MEDLINE and Google Scholar for observational studies published between January 1970 and May 2018. Our search strategy for the bibliographic databases combined terms for hypoglycemia, glucose-lowering drugs and observational studies of type 2 diabetes in adults and was limited to English language studies and full-length articles. The applied search terms were: ‘Diabetes mellitus type 2’, ‘Hypoglycemia’, ‘Adverse event’, ‘Insulin’, ‘Sulfonylurea’, ‘Thiazolidinedione’, ‘Dipeptidyl peptidase 4 inhibitor’, ‘Glucagon-like peptide-1 receptor agonist’, ‘Sodium glucose cotransporter-2 inhibitor’, as well as different combinations and associated Medical Subject Headings. Two researchers working independently screened papers for eligibility, with a third one resolving discrepancies. We selected observational (ie, not interventional) studies that reported hypoglycemic events or evaluated glucose-lowering drugs (any type of insulin, sulfonylurea, thiazolidinedione, dipeptidyl peptidase 4 inhibitor, glucagon-like peptide-1 receptor agonist and sodium glucose cotransporter-2 inhibitor) in adults with type 2 diabetes. We excluded studies that did not report on hypoglycemic events.
Data extraction
From a total of 243 observational studies,17 two reviewers, working independently and in duplicate, reproducibly (kappa >0.6) extracted the exact definitions used to define non-severe (alternatively named mild/moderate), severe and nocturnal hypoglycemia. Severity of hypoglycemia was assigned on the basis of the definitions used in the reported studies. Unspecified hypoglycemia was defined as any reported hypoglycemic event without a clear definition of being non-severe, severe or nocturnal.
Statistical analysis
Data are presented as frequencies and percentages for categorical variables. Univariate between-group comparisons were performed using χ2 tests for categorical and binary variables. P values ≤0.05 were considered statistically significant. IBM SPSS V.22.0 (SPSS, Inc, Amonk, New York, USA) was used to perform all analyses.
Results
A total of 4862 research papers were retrieved from the databases search, with 1809 duplicates removed. After the title and abstract screening, 2182 studies did not meet the eligibility criteria and were eliminated. A total of 871 studies underwent full-text review, of which 628 were eliminated for not meeting eligibility criteria, mainly not reporting on hypoglycemia events (figure 1). A total of 243 studies were ultimately reviewed: 53 cross-sectional (21.8%), 99 prospective cohort (40.7%), two case–control (0.8%) and 89 retrospective cohort (36.6%). Overall, 47.7% (n=116) reported on non-severe hypoglycemia, 77.8% (n=189) reported on severe hypoglycemia and 16.9% (n=41) reported on nocturnal hypoglycemia. In 5.8% (n=14) of studies, hypoglycemia type was not specified (table 1). A total of 32 of the analyzed studies were published after November 2016 when IHGS recommendations on standardizing hypoglycemia definitions were published.12 13 Overall, 38.2% of non-severe and 67.7% of severe hypoglycemia definitions were consistent with the IHSG recommendations. Among studies published before November 2016, 33.3% of studies reporting on non-severe hypoglycemia and 69.6% of studies reporting on severe hypoglycemia were consistent with what would be the IHSG recommendations. After IHSG recommendations were published, 62.5% and 54.1% of non-severe and severe hypoglycemia definitions were consistent with them.
Figure 1.
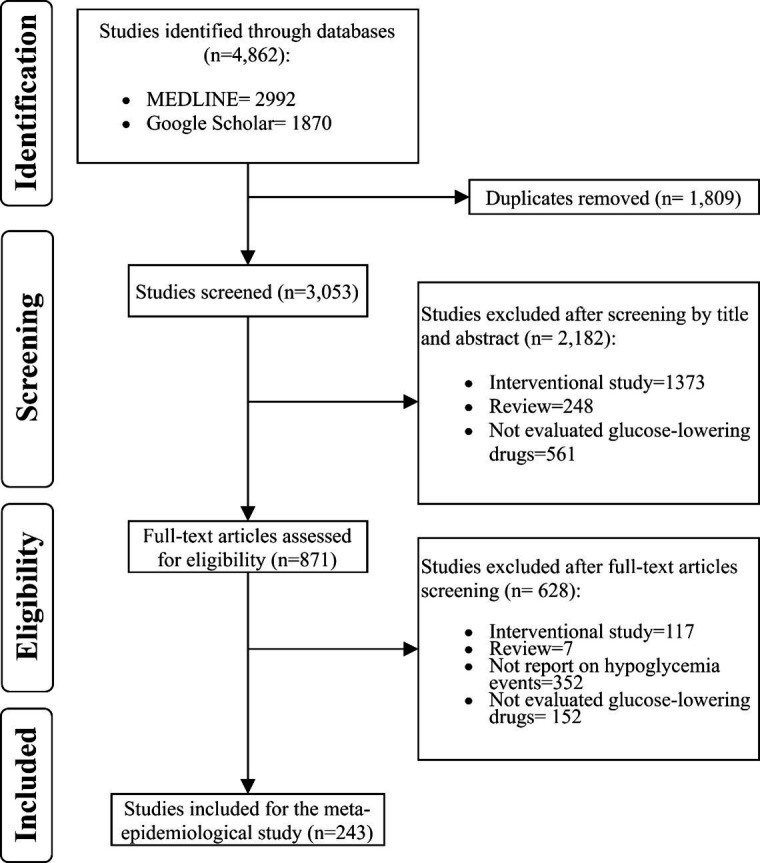
Flow chart of database research, screening and study selection.
Table 1.
Study design, type of data source and treatment*
| Type of hypoglycemia | Not defined | Non-severe | Severe | Both | Nocturnal† | Total |
| (n=14) | (n=40) | (n=113) | (n=76) | (n=41) | (n=243) | |
| Study design | ||||||
| Cross-sectional | 0 (0) | 15 (37.5) | 18 (15.9) | 20 (26.3) | 8 (19.5) | 53 (21.8) |
| Prospective cohort | 5 (35.7) | 14 (35.0) | 38 (33.6) | 42 (55.3) | 31 (75.6) | 99 (40.7) |
| Retrospective case–control | 0 (0) | 0 (0) | 1 (0.9) | 1 (1.3) | 0 (0) | 2 (0.8) |
| Retrospective cohort | 9 (64.3) | 11 (27.5) | 56 (49.6) | 13 (17.1) | 2 (4.9) | 89 (36.6) |
| Type of data source | ||||||
| Administrative data | 5 (35.7) | 3 (7.5) | 33 (29.2) | 4 (5.3) | 0 (0) | 45 (18.5) |
| EHR | 3 (21.4) | 3 (7.5) | 12 (10.6) | 9 (11.8) | 0 (0) | 27 (11.1) |
| Interview | 0 (0) | 1 (2.5) | 2 (1.8) | 3 (3.9) | 1 (2.4) | 6 (2.5) |
| Registry | 2 (14.3) | 5 (12.5) | 19 (16.8) | 2 (2.6) | 0 (0) | 28 (11.5) |
| Study cohort | 4 (28.6) | 15 (37.5) | 34 (30.1) | 42 (55.3) | 33 (80.5) | 95 (39.1) |
| Survey | 0 (0) | 13 (32.5) | 13 (11.5) | 16 (21.1) | 7 (17.1) | 42 (17.3) |
| Type of treatment | ||||||
| Not specified | 7 (50) | 10 (25.0) | 42 (37.2) | 17 (22.4) | 3 (17.6) | 76 (31.3) |
| Insulin | 4 (28.6) | 17 (42.5) | 41 (36.3) | 33 (43.4) | 36 (87.8) | 95 (39.1) |
| Sulfonylurea | 0 (0) | 1 (2.5) | 7 (6.2) | 9 (11.8) | 0 (0) | 17 (7) |
| Insulin+SU | 1 (7.1) | 2 (5.0) | 10 (8.8) | 3 (3.9) | 0 (0) | 16 (6.6) |
| Other (TZD, DPP-4, GLP1 and SGLT-2) | 1 (7.1) | 6 (15.0) | 8 (7.1) | 7 (9.2) | 0 (0) | 22 (9.1) |
| Insulin+other (TZD, DPP-4, GLP1 and SGLT-2) | 1 (7.1) | 2 (5.0) | 3 (2.7) | 3 (3.9) | 2 (4.9) | 9 (3.7) |
| SU+others (TZD, DPP-4, GLP1 and SGLT-2) | 0 (0) | 2 (5.0) | 2 (1.8) | 4 (5.3) | 0 (0) | 8 (3.3) |
*Data are presented as number (percentage) unless specified otherwise.
†Studies that reported nocturnal hypoglycemia were the same studies that evaluated severe and/or non-severe episodes and therefore were not included in the statistical analysis.
DPP-4, dipeptidyl peptidase 4 inhibitor; EHR, electronic health record; GLP1, glucagon-like peptide 1 receptor agonist; SGLT-2, sodium glucose cotransporter-2 inhibitor; SU, sulfonylurea; TZD, thiazolidinedione.
Defining non-severe hypoglycemia
Among the 116 studies reporting non-severe hypoglycemia (table 2), 18.1% (n=21) did not provide a specific definition, stating only that hypoglycemia was ‘mild’, ‘moderate’ or ‘not severe’; 23.3% (n=27) relied on a range of glucose values; 38.8% (n=45) relied on patient-reported symptoms alone; 17.2% (n=20) accepted either glucose values or patient-reported symptoms; and 2.6% (n=3) relied on International Classification of Disease (ICD) diagnosis codes for hypoglycemia.
Table 2.
Hypoglycemia definitions*
| Not defined | Non-severe | Severe | Total | |
| (n=14) | (n=116) | (n=189) | (n=319)† | |
| Hypoglycemia definition | ||||
| Not specific definition | 14 (100) | 21 (18.1) | 21 (11.1) | 56 (17.6) |
| Glucose only | – | 27 (23.3) | 7 (3.7) | 34 (10.7) |
| Symptoms only | – | 45 (38.8) | 0 (0) | 45 (14.1) |
| Symptoms requiring ED or health provider assistance | – | 0 (0) | 101 (53.4) | 101 (31.7) |
| ICD codes only | – | 3 (2.6) | 28 (14.8) | 31 (9.7) |
| Glucose and/or symptoms | – | 20 (17.2) | 30 (15.9) | 41 (12.9) |
| Glucose and/or ICD codes | – | 0 (0) | 2 (1.1) | 5 (1.6) |
*Data are presented as number (percentage) unless specified otherwise.
†This denominator represents all the hypoglycemia definitions for non-severe or severe events across all the analyzed studies.
ED, emergency department; ICD, International Classification of Disease.
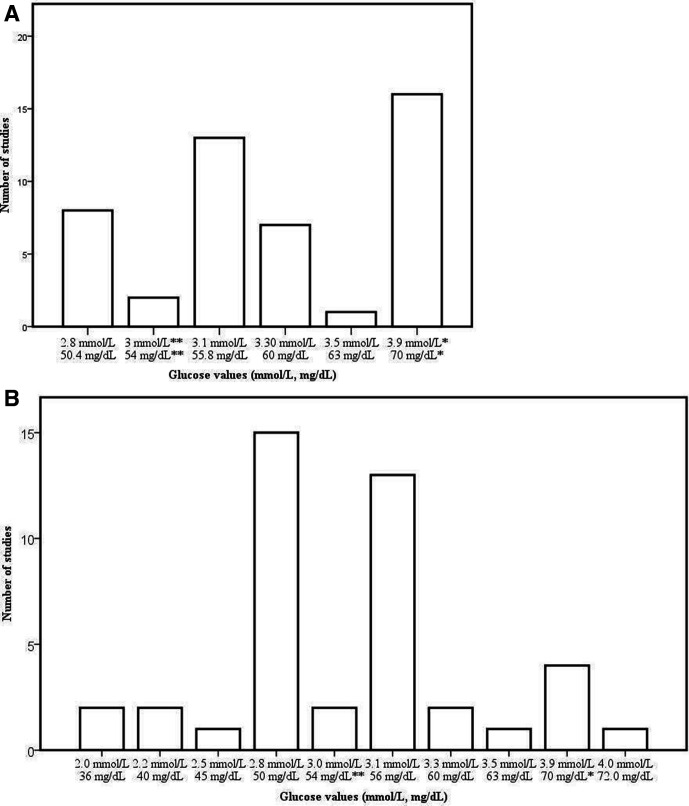
Although 47 studies (40.5% of all studies reporting on non-severe hypoglycemia) relied on specific glucose ranges to define non-severe hypoglycemia, only 13.8% (n=16) and 1.7% (n=2) used glucose values consistent with ADA/EASD guidelines and IHSG definitions of level 1 (<3.9 mmol/L) and level 2 hypoglycemia (<3.0 mmol/L), respectively. Remaining studies used thresholds ranging between <50 mg/dL (<2.8 mmol/L) and <70 mg/dL (<3.9 mmol/L) (figure 2A). None of the studies defined hypoglycemia at glucose levels ≥70 mg/dL (3.9 mmol/L).
Figure 2.
(A) Blood glucose cut-off values for non-severe hypoglycemia (mmol/L, mg/dL). (B) Blood glucose cut-off values for severe hypoglycemia (mmol/L, mg/dL). *The International Hypoglycemia Study Group (IHSG) level 1 of hypoglycemia definition. **IHSG level 2 of hypoglycemia definition. Figure part A shows the glucose values used by the analyzed studies to define non-severe hypoglycemia episodes. Figure part B shows the glucose values used by the analyzed studies to define severe hypoglycemia episodes.
Severe hypoglycemia
Of the 189 studies reporting severe hypoglycemia (table 2), 11.1% (n=21) did not provide a specific definition for what was considered to be ‘severe’; 53.4% (n=101) required symptoms requiring external or medical assistance, including some specifying need for emergency department (ED) care or hospitalization; 3.7% (n=7) relied on a range of glucose values only, without mention of symptoms; 14.8% (n=28) relied on ICD diagnosis codes only; 2.6% (n=2) relied on ICD diagnosis codes and/or glucose values; and 15.9% (n=30) required both symptoms requiring medical assistance and a specific glucose value. In the 30 studies that relied on ICD diagnosis codes, hypoglycemic events were deemed to be ‘severe’ if the hypoglycemia diagnosis code was present in encounters in the ED only (n=1); hospital only (n=4); ED or hospital (n=3); outpatient clinic only (n=1); or either ED, hospital or outpatient clinic (n=9). Remaining studies did not specify the setting where hypoglycemia diagnoses were ascertained (n=12). Moreover, the diagnosis codes could be in any position of the claim (n=1), primary or secondary position (n=6) or primary position only (n=2); in the vast majority of cases (n=21), the position was not specified. Only 10 of the studies that relied on ICD diagnosis codes used the validated Ginde algorithm for hypoglycemia ascertainment,18 with the remainder using alternate code sets.
The 39 studies (20.6% of the 189 reporting on severe hypoglycemia) that included glucose values in their definition of severe hypoglycemia (figure 2B) did not have a consistent threshold for what glucose level constituted severe hypoglycemia. The most prevalent threshold was <50 mg/dL (2.8 mmol/L; n=15, 38.5%), followed by <55.8 mg/dL (3.1 mmol/L; 33.3%, n=13) but ranged between <72 mg/dL (4.0 mmol/L) and <36 mg/dL (2.0 mmol/L).
Nocturnal hypoglycemia
While 41 studies reported on nocturnal hypoglycemia, 41.5% (n=17) did not provide any definition for how these events were defined. In 53.7% (n=22) of the studies, nocturnal hypoglycemia was defined based on temporality without specification of symptom severity, for example: ‘A nocturnal hypoglycemic event was defined as an individualized symptomatic event consistent with hypoglycemia that occurred while the patient was asleep, between bedtime (±after the evening insulin injection) and before getting up in the morning (±before morning determination of fasting plasma glucose and morning injection)’.19 20 Blood glucose levels were required to confirm hypoglycemia in only 4.9% (n=2) of the studies.
Conclusions
Hypoglycemia is a common, serious, yet potentially preventable, adverse health outcome in the management of type 2 diabetes.7–9 Hypoglycemia prevention is predicted on the ability to capture, track and evaluate events as they occur in real-world practice. In this meta-epidemiological review of observational studies of patients with type 2 diabetes, we found substantial heterogeneity in the definition, ascertainment and report of hypoglycemia, particularly for non-severe events.
Recognizing the importance of a uniform definition for hypoglycemia, on 21 November 2016, the IHSG proposed a taxonomy for non-severe (further subdivided into level 1 and level 2) and severe (level 3) hypoglycemia.12 13 The IHSG further advised that all clinical trials of diabetes management report on level 2 and level 3 hypoglycemia, with an option to also report level 1 hypoglycemia.12 13 However, observational (ie, non-randomized) studies are an invaluable source of information on adverse events in real-world settings and as such it was critical to examine how hypoglycemia was defined in such studies. This is especially important for retrospective studies that rely on secondary analyses of existing data collected for other reasons, whether for clinical care or billing/administrative purposes. To our knowledge, this is the first study to systematically examine the definitions of non-severe and severe hypoglycemia used by observational studies that form the evidence base for hypoglycemia prevention among adults with type 2 diabetes. Although most of the recent studies tend to adhere to the IHSG recommendations, the hypoglycemia definitions remained inconsistent. Overall, almost a fifth of the studies provided no definition of hypoglycemia at all. An additional 17% were loosely adherent, as they relied on ICD diagnosis codes from clinical encounters and may be construed to indirectly imply need for medication attention. Such heterogeneity in hypoglycemia reporting hinders comparisons across studies and precludes generalizable inferences about the safety of diabetes management across populations and settings.
Our study builds on earlier work demonstrating heterogeneity in hypoglycemia definitions in randomized controlled trials (RCTs) of diabetes therapies.14 Despite the IHSG recommendation, Balijepalli et al14 found that 40% of RCTs included in the Canadian Agency for Drugs and Technologies in Health report for second-line and third-line therapies for type 2 diabetes either did not report on hypoglycemia or did not specify the definition of reported events. Of the 60% that reported and defined hypoglycemia, only 14% used the IHSG definition for level 1 hypoglycemia and 20.8% for level 2 hypoglycemia.14 In contrast, our analyses that were restricted to the post-IHSG recommendation period found that hypoglycemia reporting in observational studies of type 2 diabetes was better, with 62.5% of studies on non-severe hypoglycemia and 54.1% of studies on severe hypoglycemia consistent with IHSG definitions. Nevertheless, substantial opportunity for improvement remains.
An important consideration for studies that leverage real-world data is how to optimally use administrative claims and electronic health records (EHRs) for large-scale hypoglycemia ascertainment and reporting. Doing so requires accurate and reliable identification of events, which in turn is predicated on patient’s reliably reporting events, healthcare providers consistently and uniformly documenting them and such documentation to be available in a format amenable to large scale ascertainment. Our analysis included both prospective and retrospective observational studies, and both study designs demonstrated heterogeneity in how hypoglycemia is defined. However, while prospective studies can homogenize their approach to hypoglycemia ascertainment by adopting IHSG definitions, retrospective studies that rely on secondary analysis of data collected for other reasons (eg, billing or routine care) require that hypoglycemia be uniformly defined and documented across all settings and not just research.
In our analysis, 3 of 116 (2.6%) studies that reported on non-severe hypoglycemia and 30 of 189 (15.9%) studies that reported on severe hypoglycemia used ICD codes to identify events. Because the IHSG definition of non-severe hypoglycemia is predicated solely on glucose levels, diagnosis codes and claims data cannot be used to establish a corresponding definition. Severe hypoglycemia is characterized by the need for third party or medical assistance. It can be inferred that ED or hospital encounters for hypoglycemia represent acute severe events. However, ambulatory documentation of hypoglycemia may reflect prior events being discussed in the office, both severe and non-severe, and not convey the frequency or timing of those events relative to the encounter. Diagnosis codes from ED-based or hospital-based encounters are less likely to be misclassified, particularly if the hypoglycemia code is listed as the primary or principle diagnosis for the acute event. This is the approach used by the Centers for Disease Control and Prevention to quantify severe hypoglycemic events.21 In contrast, many of the studies examined here did not specify the position of the hypoglycemia code in the encounter, what date range of claims was considered (ie, only from the date of hospital admission, only on the date of discharge or any day throughout the hospitalization) or even the setting(s) eligible for inclusion (ie, office evaluation and management visit, any ambulatory visit, ED visit, observation or inpatient hospital stay). Finally, there is heterogeneity in the specific ICD codes used to define hypoglycemia and whether studies relied on the Ginde algorithm,18 a modified version of the Ginde algorithm, or other codes entirely. Each of these parameters has the potential to alter event rates and study inferences. Nevertheless, it is important to note that up to 95% of severe hypoglycemic events do not culminate in an ED visit or hospitalization,7 22 23 and as such, studies that rely solely on claims data greatly underestimate their frequency.
Many observational studies rely on events documented as part of routine care (eg, registries, EHR and claims), yet collecting data about hypoglycemia in the real-world is challenging. Patients rarely volunteer information about hypoglycemia to their clinicians,24–28 and clinicians do not routinely screen their patients for hypoglycemia even when they are at risk for these events.7 29 As a result, patient-reported hypoglycemia is not easily captured in clinical practice, despite its association with increased all-cause mortality and impaired quality of life.30 31 Data from glucometers and continuous glucose monitors (CGMs), while valuable, is also not commonly available in the EHR, whether due to patients not using these devices (particularly in developing countries) or the inability of many practices, particularly in primary care, to consistently download device information into the EHR. Additionally, CGM use among patients with type 2 diabetes remains uncommon particularly when not treated with intensive insulin therapy.32 Reliance on events that do come to medical attention, whether in the ambulatory setting, ED or hospital, will miss most events and patients who experience them. Thus, it is critical to raise awareness among clinicians, patients and policy makers about the importance of routine and standardized hypoglycemia ascertainment and documentation, in accordance with ADA guidelines.33
This study should be considered in the context of its limitations. We focused on observational studies conducted among patients with type 2 diabetes. A large number of studies were excluded from analysis because they did not specify diabetes type and thus included patients with both type 1 and type 2 diabetes, as reliable classification of diabetes is often challenging in real-world data sources (references 214–243 of the online supplemental material).17 This contributed to the relatively small number of observational research studies analyzed. Our analyses included studies through May 2018, and hypoglycemia reporting may have improved over the past 2 years with greater attention and awareness paid to hypoglycemia by clinicians, professional societies and regulatory agencies. Nevertheless, our data point to the substantial gap in the quality of hypoglycemia ascertainment and reporting in research. This is confounded by persistent gaps in clinical hypoglycemia ascertainment7 and ultimately may contribute to inadequate understanding and correction of hypoglycemia risk factors among patients with diabetes.
bmjdrc-2020-001906supp001.pdf (159.2KB, pdf)
Observational studies and real-world data are an invaluable evidence base for comparative effectiveness and safety research that complement knowledge gleaned from interventional trials. They are particularly useful when studying adverse drug events such as hypoglycemia. The marked heterogeneity in how hypoglycemia is defined, documented and reported is a major barrier to assessing its prevalence, identifying highest risk subpopulations, promoting screening for and disclosure of events and developing prevention strategies. As such, this work reinforces the urgent need to promote, facilitate and use standardized ascertainment, documentation and reporting of hypoglycemia in observational studies and in the data sources that feed them. Using tools such as the IHSG hypoglycemia definitions in research studies could homogenize hypoglycemia reporting and evaluation. Furthermore, patients’ education to recognize, report and manage hypoglycemia is a very important tool we can use right now to decrease mortality and morbidity. Ultimately, the ability to reliably study hypoglycemic events in real-world settings will support better risk stratification and prevention strategies aimed to stopping these common, harmful yet potentially preventable adverse events.
Footnotes
RR-G and AS-M contributed equally.
Contributors: All authors analyzed the data, designed the research and wrote the manuscript. R-RG and AS-M performed the statistical analysis. RGM designed the search strategy used for this and our previous paper. All authors had read and approved the final version of this manuscript.
Funding: This work was funded by National Institute of Diabetes and Digestive and Kidney Diseases of the National Institute of Health grant number K23DK114497.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
References
- 1.Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410–8. 10.1056/NEJMoa1003795 [DOI] [PubMed] [Google Scholar]
- 2.Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the Accord study. BMJ 2010;340:b4909. 10.1136/bmj.b4909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khunti K, Davies M, Majeed A, et al. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes Care 2015;38:316–22. 10.2337/dc14-0920 [DOI] [PubMed] [Google Scholar]
- 4.Zhong VW, Juhaeri J, Cole SR, et al. Incidence and trends in hypoglycemia hospitalization in adults with type 1 and type 2 diabetes in England, 1998-2013: a retrospective cohort study. Diabetes Care 2017;40:1651–60. 10.2337/dc16-2680 [DOI] [PubMed] [Google Scholar]
- 5.Donnelly LA, Morris AD, Frier BM, et al. Frequency and predictors of hypoglycaemia in type 1 and insulin-treated type 2 diabetes: a population-based study. Diabet Med 2005;22:749–55. 10.1111/j.1464-5491.2005.01501.x [DOI] [PubMed] [Google Scholar]
- 6.Ratzki-Leewing A, Harris SB, Mequanint S, et al. Real-world crude incidence of hypoglycemia in adults with diabetes: results of the InHypo-DM study, Canada. BMJ Open Diabetes Res Care 2018;6:e000503. 10.1136/bmjdrc-2017-000503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R, et al. Hypoglycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Curr Diab Rep 2018;18:53. 10.1007/s11892-018-1018-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karter AJ, Warton EM, Lipska KJ, et al. Development and validation of a tool to identify patients with type 2 diabetes at high risk of hypoglycemia-related emergency department or hospital use. JAMA Intern Med 2017;177:1461–70. 10.1001/jamainternmed.2017.3844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schroeder EB, Xu S, Goodrich GK, et al. Predicting the 6-month risk of severe hypoglycemia among adults with diabetes: development and external validation of a prediction model. J Diabetes Complications 2017;31:1158–63. 10.1016/j.jdiacomp.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCoy RG, Lipska KJ, Van Houten HK, et al. Association of cumulative multimorbidity, glycemic control, and medication use with Hypoglycemia-Related emergency department visits and hospitalizations among adults with diabetes. JAMA Netw Open 2020;3:e1919099. 10.1001/jamanetworkopen.2019.19099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chatterjee S, Khunti K, Davies MJ. Achieving glycaemic control with concentrated insulin in patients with type 2 diabetes. Drugs 2019;79:173–86. 10.1007/s40265-018-1048-6 [DOI] [PubMed] [Google Scholar]
- 12.International Hypoglycaemia Study Group . Glucose concentrations of less than 3.0 mmol/L (54 mg/dL) should be reported in clinical trials: a joint position statement of the American diabetes association and the European association for the study of diabetes. Diabetes Care 2017;40:155–7. 10.2337/dc16-2215 [DOI] [PubMed] [Google Scholar]
- 13.International Hypoglycaemia Study Group . Glucose concentrations of less than 3.0 mmol/l (54 mg/dl) should be reported in clinical trials: a joint position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 2017;60:3–6. 10.1007/s00125-016-4146-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balijepalli C, Druyts E, Siliman G, et al. Hypoglycemia: a review of definitions used in clinical trials evaluating antihyperglycemic drugs for diabetes. Clin Epidemiol 2017;9:291–6. 10.2147/CLEP.S129268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesselheim AS, Avorn J. New "21st Century Cures" Legislation: Speed and Ease vs Science. JAMA 2017;317:581–2. 10.1001/jama.2016.20640 [DOI] [PubMed] [Google Scholar]
- 16.21St century cures act. may 19, 2015. Available: https://docs.house.gov/meetings/IF/IF00/20150519/103516/BILLS-1146ih.pdf [Accessed 15 Dec 2019].
- 17.Rodriguez-Gutierrez R, Salcido-Montenegro A, González-González JG, et al. Data from variation in hypoglycemia ascertainment and report in type 2 diabetes observational studies: a meta-epidemiological study. Available: https://figshare.com/articles/online_resource/Hypoglycemia_definition_Supplementary_1_docx/12971921 [DOI] [PMC free article] [PubMed]
- 18.Ginde AA, Blanc PG, Lieberman RM, et al. Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord 2008;8:86–92. 10.1186/1472-6823-8-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El Shiekh AR, Farrag HA, Ashour T, et al. Clinical safety of insulin detemir in patients with type 2 diabetes in the Gulf countries: the multicenter, noninterventional, open-label LevSafe study. Indian J Endocrinol Metab 2016;20:443–50. 10.4103/2230-8210.183461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lüddeke H-J, Sreenan S, Aczel S, et al. PREDICTIVE- a global, prospective observational study to evaluate insulin detemir treatment in types 1 and 2 diabetes: baseline characteristics and predictors of hypoglycaemia from the European cohort. Diabetes Obes Metab 2007;9:428–34. 10.1111/j.1463-1326.2006.00677.x [DOI] [PubMed] [Google Scholar]
- 21.Centers of Disease Control and Prevention . United States diabetes surveillance system, division of diabetes translation, CDC. Available: https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html [Accessed 15 Dec 2019].
- 22.Lipska KJ, Warton EM, Huang ES, et al. HbA1c and risk of severe hypoglycemia in type 2 diabetes: the diabetes and aging study. Diabetes Care 2013;36:3535–42. 10.2337/dc13-0610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karter AJ, Moffet HH, Liu JY, et al. Surveillance of hypoglycemia-limitations of emergency department and hospital utilization data. JAMA Intern Med 2018;178:987–8. 10.1001/jamainternmed.2018.1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brož J, Brabec M, Janíčková Žďárská D, et al. Fear of driving license withdrawal in patients with insulin-treated diabetes mellitus negatively influences their decision to report severe hypoglycemic events to physicians. Patient Prefer Adherence 2015;9:1367–70. 10.2147/PPA.S87393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohashi Y, Wolden ML, Hyllested-Winge J, et al. Diabetes management and daily functioning burden of non-severe hypoglycemia in Japanese people treated with insulin. J Diabetes Investig 2017;8:776–82. 10.1111/jdi.12642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brod M, Rana A, Barnett AH. Impact of self-treated hypoglycaemia in type 2 diabetes: a multinational survey in patients and physicians. Curr Med Res Opin 2012;28:1947–58. 10.1185/03007995.2012.743457 [DOI] [PubMed] [Google Scholar]
- 27.Emral R, Pathan F, Cortés CAY, et al. Self-reported hypoglycemia in insulin-treated patients with diabetes: results from an international survey on 7289 patients from nine countries. Diabetes Res Clin Pract 2017;134:17–28. 10.1016/j.diabres.2017.07.031 [DOI] [PubMed] [Google Scholar]
- 28.Levy JC, Davies MJ, Holman RR, et al. Continuous glucose monitoring detected hypoglycaemia in the treating to target in type 2 diabetes trial (4-T). Diabetes Res Clin Pract 2017;131:161–8. 10.1016/j.diabres.2017.01.022 [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez-Gutierrez R, Salcido-Montenegro A, Singh-Ospina NM, et al. Documentation of hypoglycemia assessment among adults with diabetes during clinical encounters in primary care and endocrinology practices. Endocrine 2020;67:552–60. 10.1007/s12020-019-02147-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCoy RG, Van Houten HK, Ziegenfuss JY, et al. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 2012;35:1897–901. 10.2337/dc11-2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCoy RG, Van Houten HK, Ziegenfuss JY, et al. Self-report of hypoglycemia and health-related quality of life in patients with type 1 and type 2 diabetes. Endocr Pract 2013;19:792–9. 10.4158/EP12382.OR [DOI] [PubMed] [Google Scholar]
- 32.Petrie JR, Peters AL, Bergenstal RM, et al. Improving the clinical value and utility of CGM systems: issues and recommendations: a joint statement of the European association for the study of diabetes and the American diabetes association diabetes technology Working group. Diabetes Care 2017;40:1614–21. 10.2337/dci17-0043 [DOI] [PubMed] [Google Scholar]
- 33.American Diabetes Association . 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S61–70. 10.2337/dc20-S002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2020-001906supp001.pdf (159.2KB, pdf)
Data Availability Statement
Data are available on reasonable request.