Abstract
Objective
This study aimed to explore the influence of coronary artery bypass grafting (CABG) on both postoperative cognitive dysfunction and quality of life (QoL) and the association between the two patient-related outcomes.
Methods
In a prospective, observational cohort study, patients with elective, isolated CABG were included. Cognitive function was assessed using the Cogstate computerised cognitive test battery preoperatively, 3 days and 6 months after surgery. QoL was measured preoperatively and at 6 months using the RAND-36 questionnaire including the Physical Component Score (PCS) and the Mental Component Score (MCS). Regression analysis, with adjustment for confounders, was used to evaluate the association between postoperative cognitive dysfunction and QoL.
Results
A total of 142 patients were included in the study. Evidence of persistent cognitive dysfunction was observed in 33% of patients after 6 months. At 6 months, the PCS had improved in 59% and decreased in 21% of patients, and the MCS increased in 49% and decreased in 29%. Postoperative cognitive changes were not associated with QoL scores.
Conclusions
Postoperative cognitive dysfunction and decreased QoL are common 6 months after surgery, although cognitive function and QoL were found to have improved in many patients at 6 months of follow-up. Impaired cognitive function is not associated with impaired QoL at 6 months.
Trial registration number
Keywords: coronary artery bypass, atherosclerosis, outcome assessment, healthcare
Key questions.
What is already known about this subject?
Postoperative cognitive dysfunction (POCD) is a common neurocognitive disorder with an incidence of 30%–60% after coronary artery bypass grafting. Despite the high incidence of POCD, the effect of POCD on patients’ daily lives after coronary bypass has not yet been investigated.
What does this study add?
This study showed that most patients benefit in terms of an increased quality of life (QoL) and recovery of cognitive functioning 6 months after surgery. However, long-term POCD was still present in one out of three patients and QoL was not yet at the preoperative level in a large proportion of patients 6 months after surgery. Impaired cognitive function was not associated with impaired QoL.
How might this impact on clinical practice?
These findings enable healthcare workers to tailor the care and guidance of patients during the process of shared decision making prior to surgery. Patients’ preferences and expectations on postoperative recovery need to be discussed thoroughly during the preoperative phase. Studies on patient-related outcomes can be valuable during this counselling process.
Introduction
In the past few decades, improvements in operative techniques and perioperative care have led to a steady decline in mortality after cardiac surgery. Although survival rates have improved, elderly patients are at increased risk of postoperative complications such as neurological and pulmonary problems.1 2 Neurological complications after cardiac surgery have been classified by the American College of Cardiology and the American Heart Association into two categories.3 Type I deficits result from well-defined local or regional insults resulting in transient ischaemic attack (TIA), stroke, coma and fatal brain injury. Type II deficits result from more diffuse and poorly understood insults, and include delirium and postoperative cognitive dysfunction (POCD). Delirium is clearly defined in the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition.4 In contrast, the definition and operationalisation of POCD is less clear; it is mostly described as a deficit of concentration, attention, memory and motor speed that lasts for several weeks or months.3 Recently, an expert working group produced a set of recommendations for diagnosis and nomenclature for postoperative neurocognitive disorders to align the terminology used with that of the DSM-V.5 They recommended that the term POCD be used for mild or major neurocognitive disorders found to be present between 1 and 12 months after surgery. Studies of patients who have undergone coronary artery bypass grafting (CABG) describe an incidence of POCD of 30%–60% depending on the timing, type and interpretation of cognitive tests used, and the patient population involved.6 7 Despite this high incidence and the fact that in vulnerable elderly patients even a small decline may have important consequences such as loss of independence,8 9 data on the impact of POCD on quality of life (QoL) are scarce. The primary aim of this study was to explore the influence of CABG on cognitive function and QoL, and the secondary aim was to investigate the association between POCD and QoL in adult patients after CABG.
Methods
We conducted a prospective single-centre cohort study. The study protocol is registered at ClinicalTrials.gov. This article describes the cognitive outcomes of our study population in relation to QoL; outcomes on physical performance, as described in the study protocol, will be reported in another article. The study results are reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines10 (online supplemental material S1).
openhrt-2020-001569supp001.pdf (102.5KB, pdf)
Eligibility criteria
We included adult patients admitted for elective, solitary on-pump CABG in the University Medical Centre Groningen, the Netherlands. Exclusion criteria were previous cardiac surgery and combined surgery (due to the increased risks of complications), pre-existing neurological deficits (ie, dementia, stroke and epilepsy) and psychiatric illness limiting reliability of screening tests. If patients were likely to experience difficulty completing cognitive testing due to impaired eyesight or hearing, or problems understanding the Dutch language, they were also excluded from the study.
Procedures
On the day of admission, usually the day before surgery, patients were identified and contacted for informed consent by the attending doctor or nurse practitioner. After informed consent was obtained, patients were included and baseline preoperative measurements were obtained. Postoperative assessment of cognitive function was performed in the hospital 3 days after surgery (short term) and at the patients’ homes 6 months after surgery (long term). QoL was measured at baseline and 6 months after surgery.
Demographic and medical characteristics
Baseline demographic data were retrieved from the electronic patient medical records and included age, sex, Body Mass Index, education level (low: primary school; moderate: high school or secondary vocational education; high: college (applied sciences) or university), EuroSCORE I and II, and the presence of comorbidity such as diabetes,11 pulmonary disease,11 arterial vascular disease,11 renal disease12 and impaired ventricular function.13 Definitions of comorbidities are included in online supplemental material S2. Perioperative data included duration of surgery, time of cardiopulmonary bypass, cross-clamp time (in minutes) and the number of (arterial) grafts.
openhrt-2020-001569supp002.pdf (93.4KB, pdf)
Outcome measures
Cognitive function was assessed using the Cogstate brief computerised cognitive test battery (Cogstate, Melbourne, Australia). The test battery we used consisted of four tasks: the detection task, the identification task, the one card learning task and the one back task (ONB), assessing psychomotor speed, selective attention, visual learning and working memory, respectively.14 The Cogstate tests have been used in several other studies, indicating a good sensitivity for detecting subtle changes in cognitive performance and strong test–retest reliability.14 15 On the day before surgery, the tests were performed twice as recommended by the software vendor. The first was to minimise practice effects and the second was used as baseline test. Before starting, each task was introduced by the researcher using standardised written instruction. Each set of four tests required approximately 20 min to complete. All cognitive function scores were standardised according to normative data from age-matched controls.16 A standardised score higher than 100 indicated a better than average score compared with the age-matched population.17 As suggested by Evered et al,5 signs of cognitive dysfunction 3 days after surgery were interpreted as delayed neurocognitive recovery effected by drugs, anaesthesia and/or pain with the potential for recovery.
To perform a within-subject analysis a standardised reliable change Z-score for each postoperative cognitive test was calculated, based on the difference between the postoperative and baseline score, and normalised using test–retest variability data provided by the software vendor.18 The standardised change Z-scores of all four individual tasks were summed to generate a composite Z-score.7 POCD was operationally defined as a Z-score of <−2 in two or more individual tasks or a composite Z-score of <−2.18 This threshold of <−2 was chosen to provide consistency with the suggestion of the expert working party of defining POCD as equivalent to major neurocognitive disorder if the decline in test scores is >2 SDs.5
QoL was measured using the RAND-36 V.2 questionnaire. The questionnaire is a widely used and validated instrument containing eight health domains: physical functioning, social functioning, role limitations due to physical health problems, role limitations due to emotional problems, mental health, vitality, pain and general health perception.19 Each dimension is scored on a scale between 0 and 100; a higher score is equivalent to better health. Two summarised scores were calculated: a Physical Component Score (PCS) and a Mental Component Score (MCS). We considered a minimal clinically important difference to be 5 points and calculated the change in QoL for each patient between preoperative and postoperative measurements. QoL was judged as being improved (>5 points), worse (<5 points) or unchanged (≤5 points decrease or increase in score).11 Secondary outcomes were postoperative complications including delirium,20 atrial fibrillation,21 myocardial infarction,22 surgical re-exploration,11 deep sternal wound infection11 and renal failure,11 all within 30 days after surgery and stroke/TIA within 72 hours after surgery.23 Definitions of complications are included in online supplemental material S2. Additional outcomes were duration of stay at the intensive care unit (ICU) and discharge destination.
Data analysis
The sample size calculation was based on the hypothetical association between POCD and QoL. POCD was assumed to be the independent variable and QoL as the dependent variable. A previous study on patients with POCD after CABG reported an SD of 8.517 and a study on QoL after cardiac events reported an SD of 11.24 A sample size of 123 patients was required for a two-tailed test at a minimal detectable difference of 0.33, an α of 0.05 and power of 80% to detect an association between POCD and QoL. To account for missing data, we included 142 patients.
Characteristics of patients are presented as numbers (with percentages) for dichotomous variables and as means (with SD) or medians (with IQRs) for continuous variables depending on distributions. Differences between baseline and 6 months of follow-up of cognitive function and QoL were tested using paired t-tests. Differences in baseline, operative and postoperative characteristics between the patients with and without POCD were tested using the χ2 or Fisher’s exact test. Linear regression analysis was used to evaluate the impact of POCD on the difference in QoL (dependent variable). Possible risk factors for POCD based on literature, as well as age and baseline PCS/MCS, were included in the multivariable model. All analyses were tested two-sided, and tests with p values of <0.05 were considered statistically significant. All data were analysed using SPSS V.25.0.
Results
A total of 142 patients undergoing elective CABG were enrolled between October 2018 and July 2019 (online supplemental material S3). Table 1 presents all baseline, operative and postoperative characteristics. Based on the standardised composite Z-score at baseline, two patients already had mild cognitive impairment based on a composite Z-score of >1 SD preoperatively.
Table 1.
Baseline, operative and postoperative characteristics of patients with CABG
| n=142 | |
| Baseline characteristics | |
| Sex (female) | 18 (13) |
| Age (years), mean (SD) | 64.3 (9.4) |
| BMI (kg/m2) | |
| <25 | 34 (24) |
| 25–30 | 71 (50) |
| >30 | 37 (26) |
| Log EuroSCORE I, median (IQR) In groups |
2.7 (1.9–4.7) |
| <10% | 133 (94) |
| 10%–20% | 9 (6.3) |
| >20% | 0 (0.0) |
| EuroSCORE II, median (IQR) | 1.5 (1.1–2.2) |
| Diabetes mellitus | 31 (22) |
| Pulmonary disease | 15 (11) |
| Arterial vascular disease | 7 (4.9) |
| Renal disease | 14 (9.9) |
| LVEF | |
| >50% | 96 (68) |
| 30%–50% | 45 (32) |
| <30% | 1 (0.7) |
| Education level* | |
| Low | 40 (28) |
| Moderate | 55 (39) |
| High | 46 (33) |
| Operative characteristics | |
| Number of grafts | |
| One graft | 1 (0.7) |
| Two grafts | 139 (98) |
| Three grafts | 2 (1.4) |
| Number of arterial grafts | |
| Use of one arterial graft | 100 (70) |
| Use of two or more arterial grafts | 39 (27) |
| No arterial graft | 3 (2.1) |
| Surgical time,† mean (SD) | 254 (41) |
| CPB time,† mean (SD) | 106 (30) |
| Cross-clamp time,† mean (SD) | 64 (22) |
| Postoperative characteristics | |
| Delirium | 7 (4.9) |
| Atrial fibrillation | 14 (9.9) |
| Myocardial infarction | 2 (1.4) |
| Surgical re-exploration | 3 (2.1) |
| Deep sternal wound infection | 3 (2.1) |
| Stroke/TIA | 0 (0.0) |
| Renal failure | 0 (0.0) |
| ICU stay,‡ median (IQR) | 21 (18–25) |
| Discharge destination | |
| Home | 99 (71) |
| Other hospital | 21 (15) |
| Rehabilitation centre | 18 (13) |
| Nursing home | 1 (0.7) |
Values are presented as n (%) unless otherwise indicated.
*Education level for one patient unknown.
†Surgical time, CPB time and cross-clamp time in minutes.
‡ICU stay in hours.
BMI, Body Mass Index; CABG, coronary artery bypass grafting; CPB, cardiopulmonary bypass; ICU, intensive care unit; LVEF, left ventricular ejection fraction; TIA, transient ischaemic attack.
openhrt-2020-001569supp003.pdf (58.8KB, pdf)
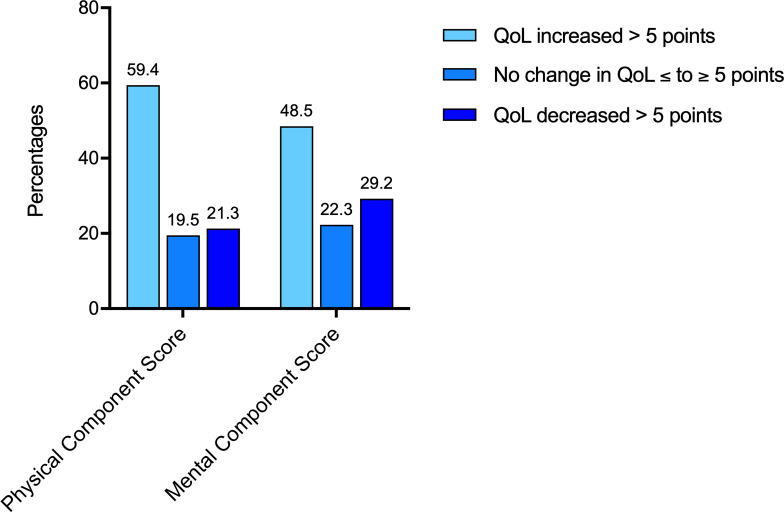
Short-term postoperative cognitive tests were performed after a median of 3 days (range 3–7) after surgery. Three patients refused further participation, and five patients were unable to complete the early postoperative test due to pain or dizziness during testing (three patients), a prolonged stay in the ICU (one patient) and transfer to another hospital on day 3 (one patient). Among the remaining 134 patients, 80 patients (60%) fulfilled the criteria for early cognitive dysfunction 3 days after surgery, based on delayed neurocognitive recovery in the terminology suggested by Evered et al.5 Two patients died during follow-up; one patient moved abroad; and five patients refused further participation. Long-term cognitive tests were performed in 131 patients after a median of 192 days (range 177–219) after surgery. Forty-three patients (33%) had cognitive dysfunction at long-term follow-up. Twenty-nine patients (22%) showed improved cognitive function with a >2 increase in their cognitive function scores compared with baseline scores. Figure 1 shows the composite standardised cognitive change scores measured at 3–7 days and 6 months after surgery. The mean cognitive test scores are presented in online supplemental material S4.
Figure 1.
Development of the composite standardised cognitive change scores per patient over time. Red solid lines indicate patients who had Z-scores below −2 at 6 months. Black dashed lines indicate patients who had a Z-score above −2 at 6 months of follow-up.
openhrt-2020-001569supp004.pdf (54.8KB, pdf)
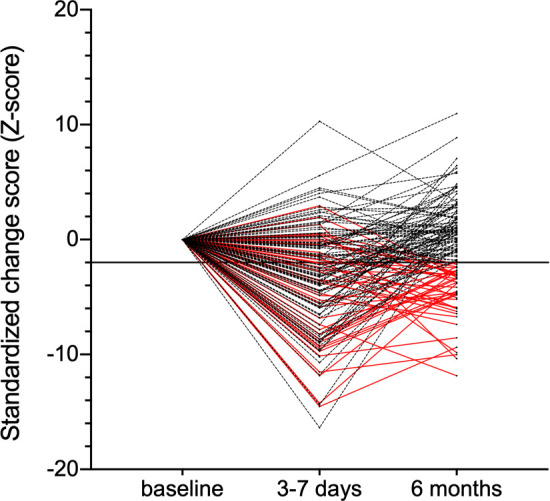
Quality of life
At 6 months of follow-up, PCS was increased (>5 points) in 59% of the patients and decreased (>5 points) in 21%. MCS was increased in 49% of the patients and decreased in 29% (figure 2). The mean MCS, PCS and subscale scores are presented in online supplemental material S5.
Figure 2.
Differences between baseline and 6 months follow-up in the QoL of patients with coronary artery bypass grafting: Physical Component Score and Mental Component Score; cut-off value: 5 points. QoL, quality of life.
openhrt-2020-001569supp005.pdf (64KB, pdf)
Association between postoperative cognitive dysfunction and QoL
Table 2 shows the results of the regression analysis. Associations between POCD and difference in QoL 6 months after surgery were non-significant (PCS p=0.66 and MCS p=0.91, respectively). The association between age and PCS did not reach statistical significance (p=0.06). In the multivariable analysis, baseline PCS and education level were statistically significantly correlated with difference in PCS at 6 months of follow-up. Baseline MCS was associated with the difference in MCS 6 months after CABG.
Table 2.
Univariable and multivariable linear regression models of the effect of preoperative and postoperative factors on the difference in quality of life 6 months after coronary artery bypass grafting
| Univariable analysis | Multivariable analysis | |||||
| PCS | PCS | R2=0.42 | ||||
| Beta | 95% CI | P value | Beta | 95% CI | P value | |
| POCD Z-score at 6 months | 0.20 | −0.68 to 1.07 | 0.66 | 0.18 | −0.53 to 0.88 | 0.62 |
| Age | −0.35 | −0.71 to 0.02 | 0.06 | −0.23 | −0.52 to 0.07 | 0.13 |
| Baseline PCS | −0.59 | −0.73 to −0.45 | <0.001 | −0.59 | −0.73 to −0.45 | <0.001 |
| Baseline cognitive functioning | 7.83 | −19.8 to 35.1 | 0.57 | 6.99 | −15.3 to 29.3 | 0.54 |
| Education level | 4.50 | 0.17 to 8.84 | 0.04 | 5.00 | 1.52 to 8.48 | 0.05 |
| Delirium | 3.72 | −12.3 to 19.8 | 0.65 | −4.06 | −17.5 to 9.45 | 0.55 |
| MCS | MCS | R2=0.28 | ||||
| Beta | 95% CI | P value | Beta | 95% CI | P value | |
| POCD Z-score at 6 months | 0.03 | −0.71 to 0.76 | 0.94 | −0.18 | −0.85 to 0.50 | 0.61 |
| Age | −0.10 | −0.41 to 0.21 | 0.52 | 0.06 | −0.23 to 0.34 | 0.69 |
| Baseline MCS | −0.41 | −0.53 to −0.29 | <0.001 | −0.43 | −0.56 to −0.30 | <0.001 |
| Baseline cognitive functioning | −0.99 | −32.1 to 14.1 | 0.44 | −1.99 | −23.4 to 19.4 | 0.86 |
| Education level | 0.16 | −3.52 to 3.84 | 0.93 | 0.60 | −2.69 to 3.89 | 0.72 |
| Delirium | 3.78 | −9.78 to 17.3 | 0.58 | −5.00 | −18.0 to 7.97 | 0.45 |
MCS, Mental Component Score; PCS, Physical Component Score; POCD, postoperative cognitive dysfunction.
Patients with and without POCD at 6 months of follow-up
Of 80 patients with POCD at short-term follow-up, 37 (46%) recovered their cognitive dysfunction 6 months after surgery. Forty-three patients (54%) were classified as having persistent POCD at long-term follow-up. Baseline characteristics, operative characteristics and postoperative complications of patients with and without POCD at 6 months after surgery are presented in table 3. Age (p=0.040), education level (p=0.046) and postoperative delirium (p=0.015) were different between the groups. Differences in PCS and MCS between the groups were not statistically significant (online supplemental material S6).
Table 3.
Characteristics of patients with or without POCD 6 months after CABG
| No POCD (n=88) |
POCD (n=43) |
P value | |
| Baseline characteristics | |||
| Sex (female) | 10 (11) | 5 (12) | >0.99 |
| Age (years), mean (SD) | 63 (9.2) | 67 (9.0) | 0.040 |
| BMI (kg/m2) | 0.29 | ||
| <25 | 18 (20) | 13 (30) | |
| 25–30 | 49 (56) | 18 (42) | |
| >30 | 21 (24) | 12 (28) | |
| Log EuroSCORE I, median (IQR) In groups |
2.6 (1.5–4.4) | 3.6 (2.1–5.3) | 0.72 |
| <10% | 83 (94) | 40 (93) | 0.15 |
| 10%–20% | 5 (6.0) | 3 (7.0) | |
| EuroSCORE II, median (IQR) | 1.5 (1.1–2.2) | 1.5 (1.1–2.5) | 0.71 |
| Diabetes mellitus | 20 (2.3) | 9 (20.9) | 0.79 |
| Pulmonary disease | 7 (8.0) | 7 (16.3) | 0.23 |
| Arterial vascular disease | 4 (4.5) | 3 (7.0) | 0.68 |
| Renal disease | 8 (9.1) | 5 (11.6) | 0.76 |
| LVEF | 0.54 | ||
| >50% | 58 (66) | 33 (36) | |
| 30%–50% | 29 (33) | 10 (23) | |
| <30% | 1 (1.1) | 0 (0.0) | |
| Education level | 0.046 | ||
| Low | 27 (31) | 9 (21) | |
| Moderate | 39 (44) | 14 (33) | |
| High | 22 (25) | 20 (46) | |
| Baseline PCS, mean (SD) | 65 (20) | 63 (19) | 0.46 |
| Baseline MCS, mean (SD) | 71 (20) | 73 (21) | 0.51 |
| Cognitive test results, mean (SD) | |||
| DET | 101 (6.7) | 103 (5.3) | 0.24 |
| IDN | 100 (4.9) | 101 (4.9) | 0.69 |
| OCL | 104 (8.7) | 104 (8.4) | 0.71 |
| ONB | 98 (5.6) | 98 (6.1) | 0.49 |
| Operative characteristics | |||
| Surgical time,* mean (SD) | 257 (46) | 249 (33) | 0.24 |
| CPB time,* mean (SD) | 108 (32) | 101 (24) | 0.21 |
| Cross-clamp time,* mean (SD) | 66 (23) | 61 (22) | 0.21 |
| Postoperative characteristics | |||
| Delirium | 1 (1.1) | 5 (12) | 0.015 |
| Atrial fibrillation | 9 (10) | 5 (12) | >0.99 |
| Myocardial infarction | 1 (1.1) | 0 (0.0) | >0.99 |
| Surgical re-exploration | 2 (2.3) | 0 (0.0) | >0.99 |
| Deep sternal wound infection | 2 (2.3) | 0 (0.0) | >0.99 |
| ICU stay†, median (IQR) | 21 (18–25) | 21 (17–23) | 0.25 |
| Discharge destination | 0.99 | ||
| Home | 63 (72) | 31 (72) | |
| Other hospital | 12 (14) | 6 (14) | |
| Rehabilitation centre | 12 (14) | 6 (14) | |
| Nursing home | 0 (0.0) | 0 (0.0) | |
Values are presented as n (%) unless otherwise indicated.
*Surgical time, CPB time and cross-clamp time in minutes.
†ICU stay in hours.
BMI, Body Mass Index; CABG, coronary artery bypass grafting; CPB, cardiopulmonary bypass; DET, detection task; ICU, intensive care unit; IDN, identification task; LVEF, left ventricular ejection fraction; MCS, Mental Component Score; OCL, one card learning task; ONB, one back task; PCS, Physical Component Score; POCD, postoperative cognitive dysfunction.
openhrt-2020-001569supp006.pdf (909.6KB, pdf)
Discussion
In this prospective cohort study, we observed that many patients showed a postoperative improvement in cognitive function, and in the physical and mental component of QoL. However, POCD was persistent in 33% of patients 6 months after surgery, and there was either no change or a decline in QoL in approximately half of all patients. Contrary to our expectations, we did not find an association between POCD and difference in QoL at 6 months after CABG. A possible explanation could be that people with impaired cognitive function can still experience a high QoL. Alternatively, patients may adjust their perceived level of QoL (glad to be alive), so that the difference between the new and the intended level is normalised after surgery.
Many studies have been performed on POCD after CABG, mostly addressing the incidence and aetiology of POCD.6 17 25 The difficulty with studies on POCD are the lack of universally accepted definitions and gold standards for measuring POCD, sometimes leading to conflicting results.6 9 As in other POCD studies, we used the reliable change index that relates the change of scores to the normal test–retest variation in an age-matched control group.7 17 18 25 Other commonly used statistical methods are an absolute decline (usually >1 SD calculated from preoperative scores) or a percentage change from baseline (usually a decline of >20%). However, these methods do not relate to data from age-matched controls and therefore do not account for normal variability among a population.26 Recommendations about thresholds are published by the expert working group, but they do not recommend specific tests.5 The Cogstate test battery may be suitable as standard instrument because the major strength of this instrument is the comparability of retrieved data to data from age-matched controls. Also, several studies suggest this instrument to be both sensitive and reliable.14–16
The high number of patients in our study not improving after CABG indicates that CABG may have a high impact on patients’ QoL, as suggested by other studies.27 28 The long-term incidence of POCD in our study is also rather high, which is in line with other studies.6 7 Possible explanations for POCD include perioperative factors (ie, low blood pressure leading to altered cerebral perfusion, cerebral microemboli caused by disruption of aortic atherosclerotic plaques, anaesthesia and systemic inflammatory response) and patient-related factors (ie, systemic atherosclerosis and decline in cognitive performance caused by altered age). Current evidence suggests that on-pump and off-pump CABG procedures have similar long-term cognitive outcomes.6 25 29 One possible explanation is that some patients already have microinfarcts before surgery and another is that both CABG techniques cause new microinfarcts during surgery that are silent (ie, do not cause overall neurological deficits) but are sufficient to cause POCD. Studies to investigate this hypothesis could use diffusion-weighted MRI imaging before and after surgery to evaluate the correlation between microinfarct load and cognitive outcome.
Other explanations for the long-term decline in QoL and the high incidence of long-term POCD could be side effects of surgery (ie, new comorbidities or reduced independence) or other confounding factors unrelated to the intervention. Perhaps future studies should also assess functional status and work resumption alongside QoL to learn more about the impact of subtle changes in cognitive functioning on patients’ daily lives.
Risk factors for a decreased QoL after CABG identified in this study are high baseline PCS and MCS, suggesting that patients with a good QoL before surgery are more likely to experience a decreased QoL after surgery, also known as regression to the mean.28 30 Although not the primary outcome of our study, we found several significant differences between the groups with and without POCD. Age, education level and postoperative delirium have been identified as risk factors for POCD in other studies as well as in our study.6 17 Although our results indicate these variables as risk factors, our study groups are too small to reach for strong conclusions and should therefore be interpreted as hypothesis generating, or supportive of previous findings.
Our study has some important limitations. First, our patient selection might differ from other hospitals, which may limit generalisability, although we included only elective patients in our cohort and mortality risk was low, with a mean log EuroSCORE I of 3.8 (SD ±3). Second, it is likely that the early postoperative cognitive tests performed at 3 days after surgery were influenced by factors like sleep disturbance and opioids. We specifically chose day 3 for assessment of short-term POCD due to logistic reasons: many of our patients are transferred back to other hospitals on day 4 after surgery.
The main reasons to offer bypass surgery are to increase survival and symptom relief. Patient-reported outcomes like QoL and POCD are also important outcomes considered from the patients’ perspective. Our study shows high incidences of long-term POCD and a decreased QoL 6 months after CABG, which may negatively influence patients’ daily lives. Studies addressing these topics can provide valuable information for patients, relatives and doctors regarding shared decision making.
Acknowledgments
The authors thank all participating patients and involved students and research nurses. We specially thank Karin Havinga, who ensured data processing and management.
Footnotes
Contributors: FB, FK, ICCvdH, MFR, WD and MAM provided substantial contributions to the conception and design of the work. FB, SH and ARA analysed and interpreted the data. FB drafted the work and all other authors revised the manuscript critically and approved the final version. All authors consented to the submission of this article. FB and MAM agreed to be accountable for all aspects of the work and ensured that questions related to the accuracy or integrity of any part of the will be appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MAM received grants from AtriCure, Edwards, Abbott, Getinge and Stichting Beatrixoord, and has provided training for Livanova and Medtronic. ARA received grants from The Medicines Company, Rigel Inc, Orion and Carefusion/BD, and has received personal fees from Johnson & Johnson, Ever Pharma, PAION and Philips.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. The data that support the findings in this study are available from the corresponding author (FB) on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the local ethics committee (METC University Medical Center Groningen, 2018/226) and was conducted in agreement with the principles of the Declaration of Helsinki. Informed consent was obtained from all participants.
References
- 1.Cloin ECW, Noyez L. Changing profile of elderly patients undergoing coronary bypass surgery. Neth Heart J 2005;13:132–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Markou ALP, van der Windt A, van Swieten HA, et al. Changes in quality of life, physical activity, and symptomatic status one year after myocardial revascularization for stable angina. Eur J Cardiothorac Surg 2008;34:1009–15. 10.1016/j.ejcts.2008.08.003 [DOI] [PubMed] [Google Scholar]
- 3.Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations. Circulation 1999;100:1464–80. 10.1161/01.CIR.100.13.1464 [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th edn, 2013. [Google Scholar]
- 5.Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth 2018;121:1005–12. 10.1016/j.bja.2017.11.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Selnes OA, Gottesman RF, Grega MA, et al. Cognitive and neurologic outcomes after coronary-artery bypass surgery. N Engl J Med 2012;366:250–7. 10.1056/NEJMra1100109 [DOI] [PubMed] [Google Scholar]
- 7.Kok WF, van Harten AE, Koene BMJA, et al. A pilot study of cerebral tissue oxygenation and postoperative cognitive dysfunction among patients undergoing coronary artery bypass grafting randomised to surgery with or without cardiopulmonary bypass*. Anaesthesia 2014;69:613–22. 10.1111/anae.12634 [DOI] [PubMed] [Google Scholar]
- 8.Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med 2001;344:395–402. 10.1056/NEJM200102083440601 [DOI] [PubMed] [Google Scholar]
- 9.Greaves D, Psaltis PJ, Ross TJ, et al. Cognitive outcomes following coronary artery bypass grafting: a systematic review and meta-analysis of 91,829 patients. Int J Cardiol 2019;289:43–9. 10.1016/j.ijcard.2019.04.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495–9. 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 11.Nederlandse Hart Registratie . Handboek Nederlandse Hartregistratie 2020, 2019. Available: www.nederlandsehartregistratie.nl [Accessed 17 Dec 2020].
- 12.Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members . Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 2013;158:825. 10.7326/0003-4819-158-11-201306040-00007 [DOI] [PubMed] [Google Scholar]
- 13.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015;16:233–71. 10.1093/ehjci/jev014 [DOI] [PubMed] [Google Scholar]
- 14.Fredrickson J, Maruff P, Woodward M, et al. Evaluation of the usability of a brief computerized cognitive screening test in older people for epidemiological studies. Neuroepidemiology 2010;34:65–75. 10.1159/000264823 [DOI] [PubMed] [Google Scholar]
- 15.Falleti MG, Maruff P, Collie A, et al. Practice effects associated with the repeated assessment of cognitive function using the CogState battery at 10-minute, one week and one month test-retest intervals. J Clin Exp Neuropsychol 2006;28:1095–112. 10.1080/13803390500205718 [DOI] [PubMed] [Google Scholar]
- 16.Cogstate . Cogstate pediatric and adult normative data. Melbourne, Australia, 2018. [Google Scholar]
- 17.Kok WF, Koerts J, Tucha O, et al. Neuronal damage biomarkers in the identification of patients at risk of long-term postoperative cognitive dysfunction after cardiac surgery. Anaesthesia 2017;72:359–69. 10.1111/anae.13712 [DOI] [PubMed] [Google Scholar]
- 18.Rasmussen LS, Larsen K, Houx P, et al. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand 2001;45:275–89. 10.1034/j.1399-6576.2001.045003275.x [DOI] [PubMed] [Google Scholar]
- 19.Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med 2001;33:350–7. 10.3109/07853890109002089 [DOI] [PubMed] [Google Scholar]
- 20.Koster S, Hensens AG, Oosterveld FGJ, et al. The delirium observation screening scale recognizes delirium early after cardiac surgery. Eur J Cardiovasc Nurs 2009;8:309–14. 10.1016/j.ejcnurse.2009.02.006 [DOI] [PubMed] [Google Scholar]
- 21.Hartog J, Blokzijl F, Dijkstra S, et al. Heart Rehabilitation in patients awaiting Open heart surgery targeting to prevent Complications and to improve Quality of life (Heart-ROCQ): study protocol for a prospective, randomised, open, blinded endpoint (PROBE) trial. BMJ Open 2019;9:e031738. 10.1136/bmjopen-2019-031738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551–67. 10.1093/eurheartj/ehs184 [DOI] [PubMed] [Google Scholar]
- 23.Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:2064–89. 10.1161/STR.0b013e318296aeca [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oldridge N, Höfer S, McGee H, et al. The HeartQoL: Part I. development of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol 2014;21:90–7. 10.1177/2047487312450544 [DOI] [PubMed] [Google Scholar]
- 25.van Harten AE, Scheeren TWL, Absalom AR. A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anaesthesia. Anaesthesia 2012;67:280–93. 10.1111/j.1365-2044.2011.07008.x [DOI] [PubMed] [Google Scholar]
- 26.Rudolph JL, Schreiber KA, Culley DJ, et al. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand 2010;54:663–77. 10.1111/j.1399-6576.2010.02236.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abah U, Dunne M, Cook A, et al. Does quality of life improve in octogenarians following cardiac surgery? A systematic review. BMJ Open 2015;5:e006904. 10.1136/bmjopen-2014-006904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blokzijl F, Houterman S, van Straten BHM, et al. Quality of life after coronary bypass: a multicentre study of routinely collected health data in the Netherlands†. Eur J Cardiothoracic Surg 2019;56:526–33. 10.1093/ejcts/ezz051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marasco SF, Sharwood LN, Abramson MJ. No improvement in neurocognitive outcomes after off-pump versus on-pump coronary revascularisation: a meta-analysis. Eur J Cardiothorac Surg 2008;33:961–70. 10.1016/j.ejcts.2008.03.022 [DOI] [PubMed] [Google Scholar]
- 30.Shan L, Saxena A, McMahon R, et al. Coronary artery bypass graft surgery in the elderly: a review of postoperative quality of life. Circulation 2013;128:2333–43. 10.1161/CIRCULATIONAHA.112.000729 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2020-001569supp001.pdf (102.5KB, pdf)
openhrt-2020-001569supp002.pdf (93.4KB, pdf)
openhrt-2020-001569supp003.pdf (58.8KB, pdf)
openhrt-2020-001569supp004.pdf (54.8KB, pdf)
openhrt-2020-001569supp005.pdf (64KB, pdf)
openhrt-2020-001569supp006.pdf (909.6KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. The data that support the findings in this study are available from the corresponding author (FB) on reasonable request.