Abstract
Background:
Controversy exists concerning whether tenotomy or tenodesis is the optimal surgical treatment option for proximal biceps tendon lesions.
Purpose:
To evaluate the clinical outcomes after arthroscopic tenodesis and tenotomy in the treatment of long head of the biceps tendon (LHBT) lesions.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed by searching PubMed, the Cochrane Library, Web of Science, and Embase to identify randomized controlled trials (RCTs) and cohort studies that compared the clinical efficacy of tenotomy with that of tenodesis for LHBT lesions. A standardized data extraction form was predesigned to obtain bibliographic information of the study as well as patient, intervention, comparison, and outcome data. A random-effects model was used to pool quantitative data from the primary outcomes.
Results:
A total of 21 eligible studies were separated into 3 methodological groups: (1) 4 RCTs with level 1 evidence, (2) 3 RCTs and 4 prospective cohort studies with level 2 evidence, and (3) 10 retrospective cohort studies with level 3 to 4 evidence. Analysis of the 3 groups demonstrated a significantly higher risk of the Popeye sign after tenotomy versus tenodesis (group 1: risk ratio [RR], 3.29 [95% CI, 1.92-5.49]; group 2: RR, 2.35 [95% CI, 1.43-3.85]; and group 3: RR, 2.57 [95% CI, 1.33-4.98]). Arm cramping pain remained significantly higher after tenotomy only in the retrospective cohort group (RR, 2.17 [95% CI, 1.20-3.95]). The Constant score for tenotomy was significantly worse than that for tenodesis in the prospective cohort group (standardized mean difference [SMD], –0.47 [95% CI, –0.73 to –0.21]), as were the forearm supination strength index (SMD, –0.75 [95% CI, –1.28 to –0.21]) and the Simple Shoulder Test (SST) score (SMD, –0.60 [95% CI, –0.94 to –0.27]).
Conclusion:
The results demonstrated that compared with tenodesis, tenotomy had a higher risk of a Popeye deformity in all 3 study groups; worse functional outcomes in terms of the Constant score, forearm supination strength index, and SST score according to prospective cohort studies; and a higher incidence of arm cramping pain according to retrospective cohort studies.
Keywords: Biceps, tenotomy, tenodesis, arthroscopic, meta-analysis
Lesions of the long head of the biceps tendon (LHBT) are a common cause of shoulder pain and disorders in patients with rotator cuff tears.11,32,37 Biceps tenotomy and tenodesis are well-established treatment options for addressing LHBT lesions when nonoperative management options have failed, but there is no consensus as to the superiority of either technique.24,25,29,33
Tenotomy might be a relatively easier technical procedure that prompts an earlier return to activity, faster rehabilitation, and fewer restrictions after the procedure.2,13 It also may adversely lead to functional deterioration of the biceps brachii such as strength of elbow flexion and forearm supination as well as the cosmetic deformity known as the Popeye sign.38 Conversely, tenodesis may maintain the LHBT with fewer cosmetic problems, preservation of elbow flexion and supination strength, alleviation of pain, and improvement of functional scores,34,39,40 but it may require a more difficult technique as well as longer operation and rehabilitation times7,23 with a higher complication rate (humeral fracture, incorrect muscle-tendon length, failure of tenodesis).
The methodology of a systematic review with meta-analysis allows the comparison of tenotomy and tenodesis across several outcome fields. Previous systematic reviews have analyzed small numbers of studies, using data only from prospective and retrospective studies, to investigate tenotomy or tenodesis. Although observational data provide some support for a comparison of 2 procedures, good-quality randomized controlled trials (RCTs) are limited. However, several RCTs3,6,19,27,28 and cohort studies20,29 not included in previous meta-analyses have recently been published. Including these studies may change the interpretation of existing data.
The purpose of this review and meta-analysis was to assess and compare the clinical effectiveness of arthroscopic tenodesis versus tenotomy in the treatment of LHBT lesions, as reported in RCTs and cohort studies. Our hypothesis was that arthroscopic tenodesis would have fewer complications and better functional outcomes than would arthroscopic tenotomy. To test this hypothesis, we established 3 groups of studies: group 1 included data from RCTs, group 2 included data from prospective cohort studies or low-quality RCTs, and group 3 included data from retrospective cohort studies. Then, given that the inclusion of low-evidence studies in the meta-analysis introduced higher levels of heterogeneity, we present 3 separate analyses for each outcome for a comparison where possible.
Methods
We performed a systematic review and meta-analysis in accordance with the MOOSE (Meta-analysis of Observational Studies in Epidemiology)36 and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.20 There were 2 authors (H.L. and X.S.) who independently searched PubMed, the Cochrane Library, Web of Science, and Embase for relevant articles without language restrictions between inception and April 30, 2020. The electronic search strategy used was as follows: tenotomy tenodesis biceps arthroscopic. In cases of a disagreement, a third reviewer (Q.Z.) made the final decision. Inclusion and exclusion criteria followed the PICOS (participants, interventions, comparators, outcomes, and study designs) strategy. Studies selected for inclusion met the following criteria:
Participants: patients undergoing arthroscopic shoulder surgery for LHBT lesions
Intervention: tenotomy
Comparator: tenodesis
Outcomes: clinical efficacy and adverse events
Study designs: RCTs, prospective cohort studies, and retrospective cohort studies
Exclusion criteria included all other study types (case reports and case series) and studies that did not meet the aforementioned inclusion criteria.
Data extraction for each study was performed by 2 authors (H.L. and X.S.) independently and then reviewed by a third author (Q.Z.). There was no need for funding or a third party to obtain any of the collected data. A standardized predesigned data extraction form was used to acquire the relevant data from each study including the author, publication year, baseline patient characteristics, numbers of participants enrolled and randomized, allocation concealment, blinding, interventions, outcomes of interest, and follow-up duration. The most up-to-date or comprehensive information was obtained if multiple publications involved the same study. Potential sources of bias in RCTs were assessed according to the Cochrane Collaboration risk of bias tool,17 stratifying the risk as high, unclear, or low risk in a traffic light configuration for random sequence generation, allocation concealment, blinding of participants, blinding of outcomes, and attrition bias. For study groups 2 and 3, the Newcastle-Ottawa scale39 was used to assess studies in 3 key areas including selection and comparability of cohorts as well as outcome.
Reporting Outcomes
We focused on important outcomes: (1) the composition of complications, including all incidences of a Popeye deformity, arm cramping pain, and retears of the rotator cuff; (2) functional outcomes, mainly consisting of the Constant score, visual analog scale (VAS) for pain score, American Shoulder and Elbow Surgeons (ASES) score, elbow flexion strength index, forearm supination strength index, Simple Shoulder Test (SST) score, and University of California, Los Angeles (UCLA) shoulder score; and (3) range of motion, mainly measuring forward flexion, external rotation with the arm at the side, and abduction.
Study Methodology Assessment
The modified Coleman Methodology Score (MCMS)9 was used by 2 reviewers (Q.Z. and W.G.) to assess the methodologic quality of the selected studies. The primary outcomes assessed via the MCMS are study size and type, follow-up time, attrition rate, number of interventions per group, and proper description of the study methodology. Scores range from 0 to 100 and are categorized as excellent (85-100), good (70-84), fair (55-69), and poor (<55).
Statistical Analysis
The overall summary estimates were calculated using inverse variance–weighted random-effects meta-analysis.18 Individual relative risk estimates and summary estimates were presented graphically in forest plots. The Q test and chi-square test were used to estimate statistical heterogeneity, with P values and I 2 statistics. Analysis could not be performed across the different types of studies owing to the significant differences in their design. Therefore, for each outcome, data from each type of study were displayed sequentially by group: RCTs, prospective cohort studies, and retrospective cohort studies. If no outcome data were presented in ≥1 of the groups, we commented on this. Meta-analysis statistics, generation of forest plots, and risk of bias assessments were performed using a combination of R (Version 3.5.1; R Foundation for Statistical Computing) and RevMan (Version 5.3; Cochrane Collaboration). The level of statistical significance was set as P < .05, with 95% CIs also used. All statistical tests performed were 2-sided.
Results
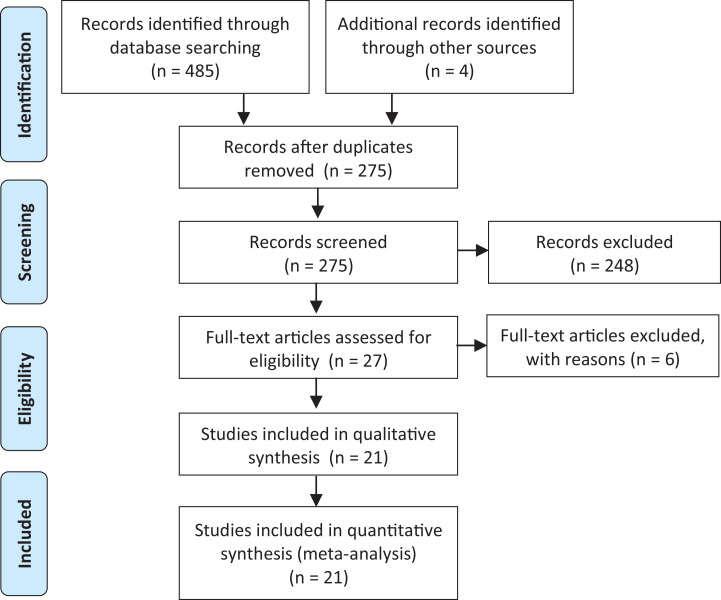
A total of 485 potentially relevant citations were initially identified using our search strategy; 4 additional reports were found during the manual search of references. There were 214 duplicate studies excluded using EndNote software (Version X9; Clarivate Analytics). An additional 248 studies were removed after screening the title and abstract. Then, 27 articles remained for a full-text assessment, and 6 were subsequently excluded. Thus, 21 studies** reporting on 1753 participants (n = 958 tenotomy; n = 795 tenodesis) were included in the final analysis. The flowchart of selecting relevant articles is shown in Figure 1. The main characteristics of the included studies are listed in Table 1. The characteristics of study patients are shown in Table 2. LHBT and rotator cuff injury types and tenodesis methods of the included studies are presented in Table 3.
Figure 1.
Flowchart of the number of studies identified and included in this meta-analysis based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Table 1.
Characteristics of Included Studiesa
| Lead Author (Year) | Study Design | LoE | Outcome Measuresb | Follow-up, mo | MCMS Score | |
|---|---|---|---|---|---|---|
| Tenotomy | Tenodesis | |||||
| MacDonald27 (2020) | RCT | 1 | 1, 5, 6 | 24 | 24 | 91 |
| Castricini6 (2018) | RCT | 1 | 1, 2, 3, 4, 5 | 12 | 12 | 94 |
| Lee26 (2016) | RCT | 1 | 1, 3 | 25.1 | 19.7 | 89 |
| Zhang44 (2015) | RCT | 1 | 1, 2, 4, 5, 7, 8 | 25 | 25 | 95 |
| Belay3 (2019) | RCT | 2 | 1, 2, 5 | 24 | 24 | 83 |
| Hufeland19 (2019) | RCT | 2 | 1, 2, 4, 6, 9 | 12 | 12 | 86 |
| Mardani-Kivi28 (2018) | RCT | 2 | 1, 2, 4, 9 | 24 | 24 | 87 |
| Oh31 (2016) | PCS | 2 | 1, 2, 3, 5, 6, 7, 8, 11, 12 | 21.98 | 21.46 | 84 |
| Kukkonen25 (2013) | PCS | 2 | 1, 2 | 24 | 24 | 86 |
| De Carli10 (2012) | PCS | 2 | 1, 4, 9 | 23 | 25 | 89 |
| Koh24 (2010) | PCS | 2 | 1, 2, 4, 6, 7 | 27.93 | 27.05 | 92 |
| Aflatooni1 (2020) | RCS | 3 | 1, 2 | 38.4 | 30.7 | 79 |
| Zhang43 (2019) | RCS | 3 | 1, 5, 10 | 14.3 | 14.3 | 70 |
| Kerschbaum22 (2017) | RCS | 3 | 1, 4 | 39 | 39 | 76 |
| Meraner29 (2016) | RCS | 4 | 1, 2, 4 | 34 | 34 | 76 |
| Cho8 (2014) | RCS | 3 | 1, 4, 10 | 24.2 | 26.1 | 79 |
| Biz4 (2012) | RCS | 3 | 1 | 30 | 30 | 71 |
| Ikemoto21 (2012) | RCS | 3 | 1 | 41.84 | 45.36 | 76 |
| Sentürk33 (2011) | RCS | 4 | 4, 10 | 37.2 | 37.2 | 70 |
| Wittstein41 (2011) | RCS | 3 | 1, 2, 6 | 57 | 58 | 63 |
| Boileau5 (2007) | RCS | 3 | 1, 2, 4, 11, 12 | 36 | 34 | 79 |
aLoE, level of evidence; MCMS, modified Coleman Methodology Score; PCS, prospective cohort study; RCS, retrospective cohort study; RCT, randomized clinical trial.
bOutcome measures: 1 = Popeye deformity; 2 = arm cramping pain; 3 = rotator cuff retear; 4 = Constant score; 5 = visual analog scale for pain; 6 = American Shoulder and Elbow Surgeons score; 7 = elbow flexion strength index; 8 = forearm supination strength index; 9 = Simple Shoulder Test; 10 = University of California, Los Angeles score; 11 = forward flexion; and 12 = external rotation at the side.
Table 2.
Characteristics of Study Patientsa
| Lead Author (Year) | Sample Size, n | Age,b y | Female Sex, n | |||
|---|---|---|---|---|---|---|
| Tenotomy | Tenodesis | Tenotomy | Tenodesis | Tenotomy | Tenodesis | |
| MacDonald27 (2020) | 57 | 57 | 56.3 ± 8.1 | 58.7 ± 10.9 | 12 | 10 |
| Castricini6 (2018) | 31 | 24 | 59.9 ± 8.0 | 57.1 ± 8.0 | 17 | 17 |
| Lee26 (2016) | 56 | 72 | 62.8 (55-77) | 62.9 (50-75) | 45 | 54 |
| Zhang44 (2015) | 77 | 74 | 61 (55-67) | 61 (55-71) | 41 | 39 |
| Belay3 (2019) | 20 | 14 | 57.7 ± 8.7 | 52.9 ± 10.8 | 1 | 2 |
| Hufeland19 (2019) | 11 | 9 | 52.8 ± 8.0 | 51.5 ± 9.5 | 7 | 2 |
| Mardani-Kivi28 (2018) | 29 | 33 | 54.5 ± 5.3 | 55.5 ± 5.2 | 9 | 11 |
| Oh31 (2016) | 27 | 31 | 61.04 (53-69) | 56.61 (42-76) | 18 | 10 |
| Kukkonen25 (2013) | 26 | 24 | 62.7 (F); 63.7 (M) | 54.1 (F); 54.9 (M) | 13 | 9 |
| De Carli10 (2012) | 30 | 35 | 59.6 ± 8.7 | 56.3 ± 3.9 | NG | NG |
| Koh24 (2010) | 41 | 43 | 66 (55-82) | 65 (55-77) | 32 | 27 |
| Aflatooni1 (2020) | 104 | 111 | 63.5 ± 8.6 | 58.9 ± 8.8 | 56 | 31 |
| Zhang43 (2019) | 18 | 22 | 62.2 ± 6.1 | 60.5 ± 6.3 | 12 | 14 |
| Kerschbaum22 (2017) | 36 | 49 | 69 ± 10 | 63 ± 11 | 23 | 17 |
| Meraner29 (2016) | 29 | 24 | 59.2 ± 9.2 | 57.6 ± 9.0 | 16 | 9 |
| Cho8 (2014) | 41 | 42 | 63.8 (44-68) | 58.6 (45-70) | 21 | 19 |
| Biz4 (2012) | 202 | 50 | 61.4 | 55.34 | 108 | 19 |
| Ikemoto21 (2012) | 55 | 22 | 58.05 | 58.18 | NG | NG |
| Sentürk33 (2011) | 10 | 10 | 63 | 57 | 5 | 4 |
| Wittstein41 (2011) | 19 | 16 | 62.5 ± 10.7 | 52.0 ± 14.3 | 9 | 12 |
| Boileau5 (2007) | 39 | 33 | 68 ± 6 | 68 ± 6 | NG | NG |
aF, female; M, male; NG, not given.
bData are presented as mean, mean ± SD, or mean (range).
Table 3.
LHBT Injury Types, Rotator Cuff Injury Types, and Tenodesis Methodsa
| Lead Author (Year) | LHBT Injury Type | Rotator Cuff Injury Type | Tenodesis Method |
|---|---|---|---|
| MacDonald27 (2020) | LHBT lesion | Repairable rotator cuff, irreparable rotator cuff, no rotator cuff tear | Arthroscopic suprapectoral approach with interference screw or open subpectoral approach with button |
| Castricini6 (2018) | Tenosynovitis, subluxation, dislocation, partial tear | Grade I or II full-thickness repairable supraspinatus tendon tear | Interference screw |
| Lee26 (2016) | Partial tear | Small to medium rotator cuff tear | Interference screw |
| Zhang44 (2015) | Severe inflammation, hypertrophy, instability, partial-thickness tear, SLAP lesion | Small to large full-thickness rotator cuff tear | Suture anchor |
| Belay3 (2019) | Partial tear, subluxation | Small to large full-thickness rotator cuff tear | Interference screw |
| Hufeland19 (2019) | Isolated SLAP or biceps pulley lesion | — | Interference screw |
| Mardani-Kivi28 (2018) | Inflammation, partial tear, subluxation or SLAP lesion | Small to large full-thickness rotator cuff tear | Interference screw |
| Oh31 (2016) | Partial tear | Full-thickness supraspinatus (and infraspinatus) tendon tear, high-grade partial-thickness supraspinatus tendon tear, full-thickness subscapularis tendon tear with supraspinatus (and infraspinatus) tendon tear | Suture anchor |
| Kukkonen25 (2013) | Irritated/frayed and/or unstable biceps tendon | Full-thickness supraspinatus tendon tear | Nonabsorbable titanium suture anchor |
| De Carli10 (2012) | Degenerative tear, tenosynovitis, subluxation, SLAP lesion | Small to large rotator cuff tear | Suturing biceps tendon to rotator cuff tendon |
| Koh24 (2010) | Tear >30%, subluxation or dislocation or degenerative type 2 SLAP lesion | Rotator cuff tear | Suture anchor |
| Aflatooni1 (2020) | Proximal biceps or superior labral complex injury | Rotator cuff tear | Interference screw |
| Zhang43 (2019) | Inflammation | — | Suture anchor |
| Kerschbaum22 (2017) | Tendinitis, tear, subluxation or SLAP lesion | Rotator cuff tear | Suture anchor |
| Meraner29 (2016) | Complete or partial rupture or severe degeneration | Small to large full-thickness rotator cuff tear | Common suture anchor |
| Cho8 (2014) | LHBT lesion | Small to massive full-thickness rotator cuff tear | Ethibond suture |
| Biz4 (2012) | Tendinopathy, partial injury or instability | Rotator cuff tear | — |
| Ikemoto21 (2012) | LHBT injury | Rotator cuff tear | 2 anchors |
| Sentürk33 (2011) | Chronic biceps tenosynovitis | Small to medium rotator cuff tear | Bioabsorbable interference screw |
| Wittstein41 (2011) | LHBT lesion | Small to large full-thickness rotator cuff tear | — |
| Boileau5 (2007) | LHBT lesion | Irreparable rotator cuff tear | Bioabsorbable interference screw |
aLHBT, long head of the biceps tendon; SLAP, superior labrum from anterior to posterior; —, none reported.
Study Groups
Overall, 4 RCTs,6,26,27,44 each with an evidence level of 1, were included in group 1. This allowed an analysis of 448 participants (n = 221 tenotomy; n = 227 tenodesis) from the data. Group 2 included 7 publications3,10,19,24,25,28,31 of level 2 evidence, with 184 patients undergoing biceps tenotomy and 189 patients undergoing biceps tenodesis; 3 studies were low-quality RCTs, and 4 were prospective cohort studies. Group 3 included a further 10 retrospective cohort studies†† with a total of 932 patients (n = 553 tenotomy; n = 379 tenodesis). Of these retrospective studies, all were rated as level 3 evidence, except 2 publications of level 4 evidence. One written in Chinese43 and another written in German22 were included in this group.
Methodological Quality Assessment
The risk of bias of the included studies is shown in Tables 4 and 5. In group 1, the study by Castricini et al,6 which did not assess supination strength, and the study by Lee et al,26 which did not report the SD of the VAS pain score and Constant score at the last follow-up, were judged as having a high risk of attrition bias. In groups 2 and 3, there were 7 studies3,8,10,19,24,25,29 that were awarded 8 stars, 4 studies1,21,28,43 that were given 7 stars, and 6 studies4,5,22,31,33,41 that were granted 6 stars.
Table 4.
Risk of Bias for Randomized Clinical Trials Using the Cochrane Collaboration Toola
| Lead author | bItem No. | ||||||
|---|---|---|---|---|---|---|---|
| Study group 1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| MacDonald (2020)27 | + | + | + | ? | + | + | ? |
| Castricini (2018)6 | + | + | + | ? | - | + | + |
| Lee (2016)26 | + | + | ? | + | - | + | ? |
| Zhang (2015)44 | + | + | ? | + | + | + | + |
a+ = clear documentation that the study meets this requirement, ? = unclear from publication, - = no evidence that requirements met.
bItem No.: 1 = random sequence generation; 2 = allocation concealment; 3 = blinding of participants and personnel; 4 = blinding of outcomes; 5 = incomplete outcome data; 6 = selective reporting; and 7 = other bias.
Table 5.
Risk of Bias for Cohort Studies Using the Newcastle-Ottawa Scalea
| Lead Author | Selectionb | Comparabilityc | Outcomed | Score | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 1 | 1 | 2 | 3 | ||
| Study group 2 | |||||||||
| Belay3 (2019) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 8 |
| Hufeland19 (2019) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 8 |
| Mardani-Kivi28 (2018) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | — | 7 |
| Oh31 (2016) | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | — | 6 |
| Kukkonen25 (2013) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 8 |
| De Carli10 (2012) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 8 |
| Koh24 (2010) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 8 |
| Study group 3 | |||||||||
| Aflatooni1 (2020) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | 7 |
| Zhang43 (2019) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | 7 |
| Kerschbaum22 (2017) | ⋆ | ⋆ | ⋆ | ⋆ | — | — | ⋆ | ⋆ | 6 |
| Meraner29 (2016) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | 7 |
| Cho8 (2014) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | 7 |
| Biz4 (2012) | ⋆ | ⋆ | ⋆ | ⋆ | — | — | ⋆ | ⋆ | 6 |
| Ikemoto21 (2012) | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | 7 |
| Sentürk33 (2011) | ⋆ | ⋆ | ⋆ | ⋆ | — | — | ⋆ | ⋆ | 6 |
| Wittstein41 (2011) | — | ⋆ | ⋆ | ⋆ | ⋆ | — | ⋆ | ⋆ | 6 |
| Boileau5 (2007) | ⋆ | ⋆ | ⋆ | ⋆ | — | — | ⋆ | ⋆ | 6 |
aA study can be awarded a maximum of 1 star for each numbered item within the Selection and Outcome categories. A maximum of 2 stars can be given for the Comparability category. The dashes denote ineligibility for a star.
bSelection: 1 = representativeness of the exposed cohort; 2 = selection of the nonexposed cohort; 3 = ascertainment of exposure; and 4 = demonstration that the outcome of interest was not present at the start of the study.
cComparability: 1 = comparability of cohorts on the basis of the design or analysis.
dOutcome: 1 = assessment of outcomes; 2 = follow-up was long enough for outcomes to occur; and 3 = adequacy of follow-up.
Modified Coleman Methodology Score
Table 1 shows the MCMS scores from the 21 included studies (mean, 81.7 ± 8.8). There were 9 studies6,10,19,24–28,44 that received excellent scores, 11 studies‡‡ that received good scores, and 1 study41 that received a fair score.
Outcomes
A summary of all data analyses is presented in Table 6. For ease of comparisons, data from study groups 1 to 3 are presented separately for each outcome measure. For ease of interpretation, the effect of treatment type (tenotomy or tenodesis) on the incidence of each outcome measure was summarized as forest plots (Figures 2 -13).
Table 6.
Tenotomy Versus Tenodesis Outcomes by Study Groupa
| Outcome | Study Group 1 | Study Group 2 | Study Group 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| RR or SMD (95% CI) | I 2 | Q Value (P Value) | RR or SMD (95% CI) | I 2 | Q Value (P Value) | RR or SMD (95% CI) | I 2 | Q Value (P Value) | |
| Popeye deformity | 3.29 (1.92 to 5.49)b | 0% | 0.23 (.97) | 2.35 (1.43 to 3.85)b | 0% | 4.97 (.55) | 2.57 (1.33 to 4.98)b | 45% | 14.60 (.07) |
| Arm cramping pain | 1.73 (0.61 to 4.92) | — | — | 3.16 (0.99 to 10.15) | 1% | 3.02 (.39) | 2.17 (1.20 to 3.95)b | 0% | 1.15 (.56) |
| Rotator cuff retear | 1.03 (0.47 to 2.23) | 0% | 0.04 (.83) | 2.87 (0.61 to 13.61) | — | — | — | — | — |
| Constant score | –0.16 (–0.57 to 0.24) | 45% | 1.81 (.18) | –0.47 (–0.73 to –0.21)b | 0% | 1.94 (.58) | –0.26 (–0.60 to 0.08) | 53% | 8.42 (.08) |
| VAS pain score | 0.04 (–0.18 to 0.26) | 0% | 1.26 (.53) | –0.36 (–1.33 to 0.60) | 79% | 4.77 (.03) | 0.26 (–0.37 to 0.89) | — | — |
| ASES score | 0.15 (–0.22 to 0.51) | — | — | –0.39 (–0.78 to 0.00) | 28% | 2.78 (.25) | 0.26 (–0.41 to 0.92) | — | — |
| Elbow flexion strength index | 0.00 (–0.32 to 0.32) | — | — | –0.02 (–0.35 to 0.31) | 0% | 0.35 (.56) | — | — | — |
| Forearm supination strength index | 0.00 (–0.32 to 0.32) | — | — | –0.75 (–1.28 to –0.21)b | — | — | — | — | — |
| SST score | — | — | — | –0.60 (–0.94 to –0.27)b | 0% | 1.91 (.39) | — | — | — |
| UCLA score | — | — | — | — | — | — | –0.18 (–0.55 to 0.19) | 14% | 2.31 (.31) |
| Forward flexion | — | — | — | 0.06 (–0.45 to 0.58) | — | — | –0.39 (–0.85 to 0.08) | — | — |
| External rotation at the side | — | — | — | 0.08 (–0.43 to 0.60) | — | — | –0.57 (–1.04 to –0.10) | — | — |
aGroup 1 = randomized clinical trials; group 2 = prospective cohort studies; and group 3 = retrospective cohort studies. I 2 and Q values quantify study heterogeneity. Dashes indicate no data or inadequate data available. ASES, American Shoulder and Elbow Surgeons; RR, risk ratio; SMD, standard mean difference; SST, Simple Shoulder Test; UCLA, University of California, Los Angeles; VAS, visual analog scale.
bSignificant results.
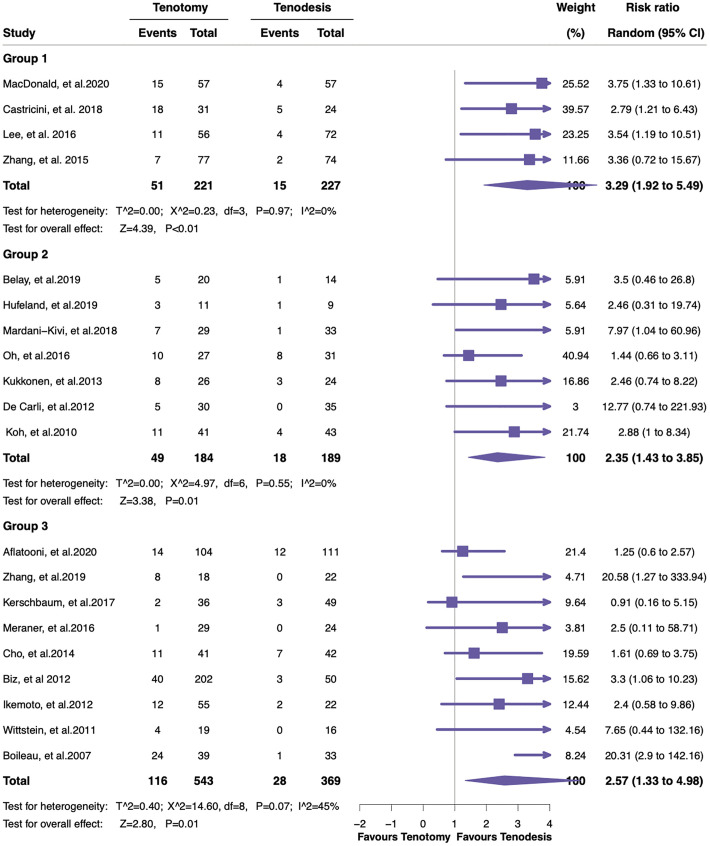
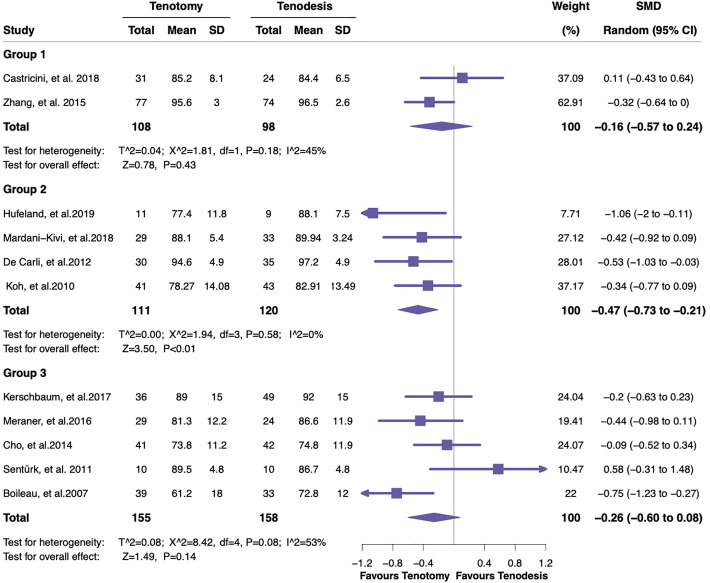
Figure 2.
Forest plot displaying the risk ratio and 95% CI for the effect of treatment using tenotomy or tenodesis on the incidence of a Popeye deformity.
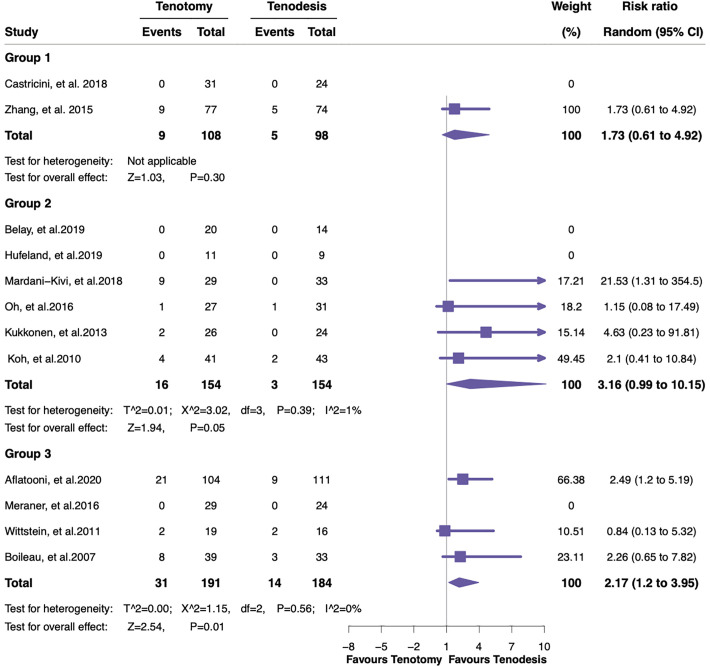
Figure 3.
Forest plot displaying the risk ratio and 95% CI for the effect of treatment using tenotomy or tenodesis on the incidence of arm cramping pain.
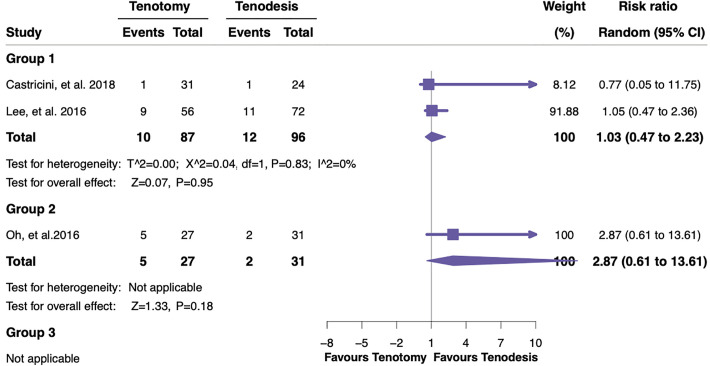
Figure 4.
Forest plot displaying the risk ratio and 95% CI for the effect of treatment using tenotomy or tenodesis on the incidence of rotator cuff retears.
Figure 5.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on the Constant score.
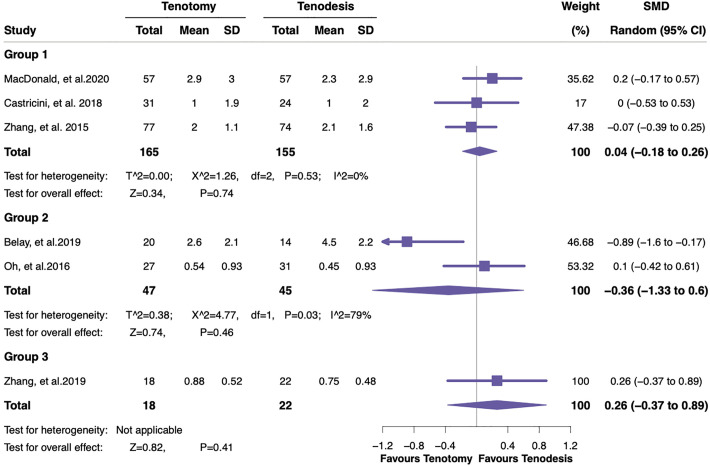
Figure 6.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on the visual analog scale pain score.
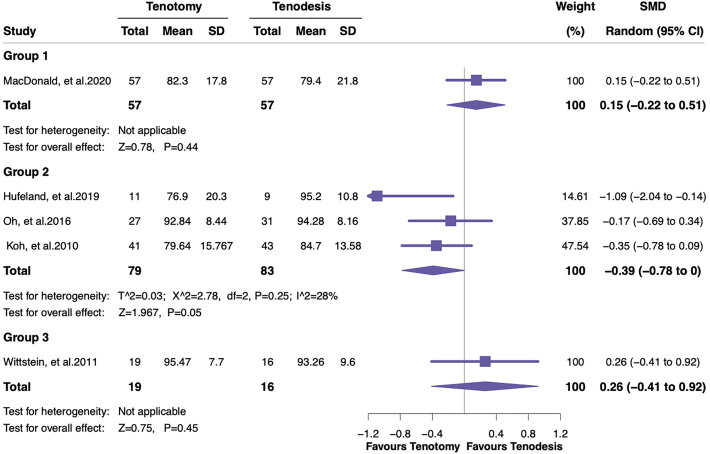
Figure 7.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on the American Shoulder and Elbow Surgeons score.
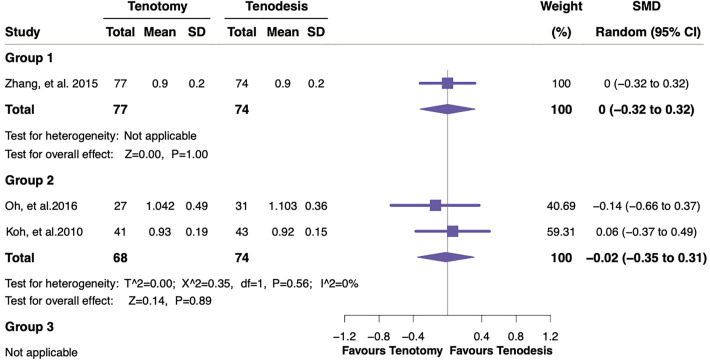
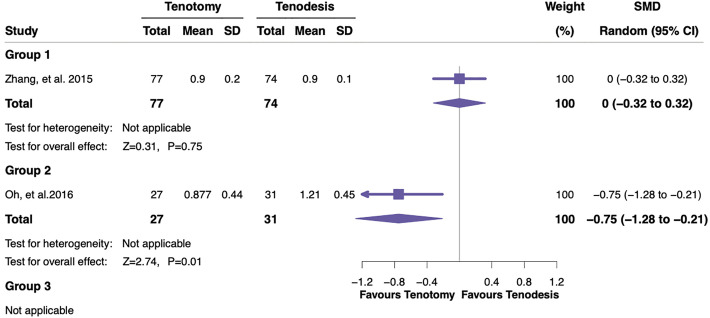
Figure 8.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on elbow flexion strength index.
Figure 9.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on forearm supination strength index.
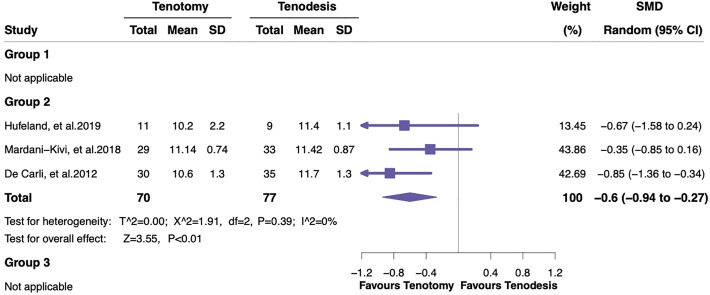
Figure 10.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on the Simple Shoulder Test score.
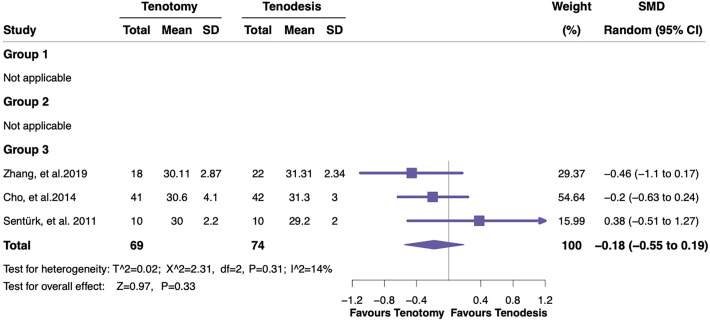
Figure 11.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on the University of California, Los Angeles score.
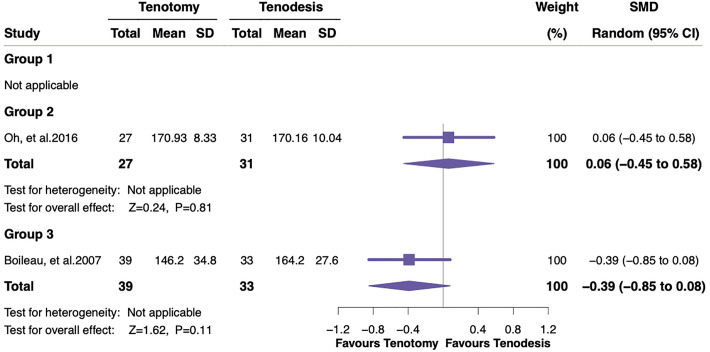
Figure 12.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on forward flexion.
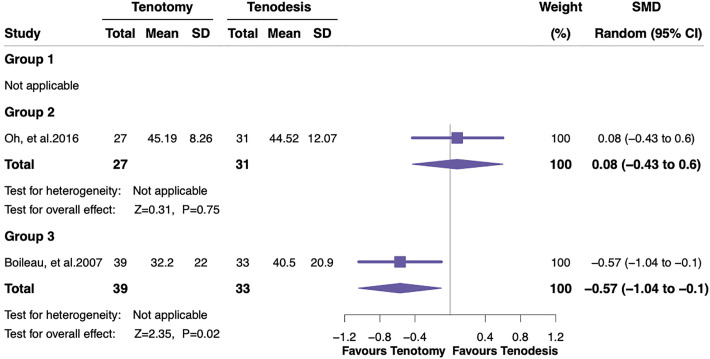
Figure 13.
Forest plot displaying the standardized mean difference (SMD) and 95% CI for the effect of treatment using tenotomy or tenodesis on external rotation at the side.
Popeye Deformity
A total of 20 studies§§ involving 948 tenotomy and 785 tenodesis procedures reported results for the incidence of a Popeye deformity. There was a significantly higher rate of a Popeye deformity after tenotomy versus tenodesis in groups 1, 2, and 3 (Figure 2). In group 1, data from the 4 RCTs showed a significantly higher incidence of a Popeye deformity after tenotomy (risk ratio [RR], 3.29 [95% CI, 1.92-5.49]).6,26,27,44 Data from group 2 included 7 studies, with a significant RR of 2.35 (95% CI, 1.43-3.85). 3,10,19,24,25,28,31 Data from 9 retrospective cohort studies were included in group 3, which showed a significant RR of 2.57 (95% CI, 1.33-4.98).1,4,8,21,22,29,41,43
Arm Cramping Pain
A total of 12 studies∥∥ specifically reported arm cramping pain as an outcome measure. Data were included from 453 tenotomy and 436 tenodesis procedures in this analysis. There was no significant difference in groups 1 and 2 but a significantly higher rate of arm cramping pain after tenotomy than tenodesis in group 3 (Figure 3). In group 1, of 2 RCTs available, 1 reporting no incidence of arm cramping pain was excluded, so data from only 1 RCT showed an RR of 1.73 (95% CI, 0.61-4.92).6,44 In group 2, data from 4 of 6 studies showed an RR of 3.16 (95% CI, 0.99-10.15); the other 2 studies showing no result were excluded.3,19,24,25,28,31 In group 3, with the exclusion of 1 study with no result, data from 4 cohort studies showed an RR of 2.17 (95% CI, 1.20-3.95).1,5,29,41
Rotator Cuff Retear
A total of 3 studies6,26,31 were included with 114 tenotomy and 127 tenodesis procedures. We found no significant difference in the risk of rotator cuff retears between tenotomy and tenodesis (Figure 4). In group 1, there were 2 RCTs that reported an RR of 1.03 (95% CI, 0.47-2.23).6,26 Data from 1 study were included in group 2, showing a corresponding RR of 2.87 (95% CI, 0.61-13.61).31 In group 3, no study reported the rotator cuff retear rate, so it could not be included in the analysis.
Constant Score
A total of 11 studies¶¶ including 374 tenotomy and 376 tenodesis procedures specifically reported Constant scores. A higher score was related to a better clinical outcome. In this analysis, significantly higher functional Constant scores were achieved after tenodesis than after tenotomy in group 2, but the difference was not significant in groups 1 and 3 (Figure 5). In group 1, data were presented from 2 RCTs,6,44 which showed a standardized mean difference (SMD) of –0.16 (95% CI, –0.57 to 0.24). In group 2, data from 4 studies10,19,24,28 showed an SMD of –0.47 (95% CI, –0.73 to –0.21). In group 3, data from 5 retrospective studies5,8,22,29,33 showed an overall SMD of –0.26 (95% CI, –0.60 to 0.08).
VAS Pain Score
A total of 6 studies3,6,27,31,43,44 reported VAS pain scores in 230 tenotomy and 222 tenodesis procedures. VAS scores were found to be equivocal after tenodesis compared with tenotomy in all study groups (Figure 6). In group 1, data were presented from 3 RCTs (SMD, 0.04 [95% CI, –0.18 to 0.26]).6,27,44 In group 2, data from 2 prospective cohort studies showed an SMD of –0.36 (95% CI, –1.33 to 0.60).3,31 Data from 1 retrospective cohort study in group 3 showed an SMD of 0.26 (95% CI, –0.37 to 0.89).43
ASES Score
The ASES score was reported in 5 studies,19,24,27,31,41 allowing an analysis of 155 tenotomy and 156 tenodesis procedures. In all levels of analysis, no significantly better ASES score was recorded for tenodesis or tenotomy (Figure 7). In group 1, data presented from 1 RCT demonstrated an SMD of 0.15 (95% CI, –0.22 to 0.51).27 In group 2, data from 3 prospective studies showed an SMD of –0.39 (95% CI, –0.78 to 0.00).19,25,31 In group 3, data from 1 retrospective study showed a corresponding SMD of 0.26 (95% CI, –0.41 to 0.92).41
Elbow Flexion Strength Index
Data were presented in 3 studies24,31,44 regarding elbow flexion strength index and included 145 tenotomy and 148 tenodesis procedures. The analysis showed no significantly different result of elbow flexion strength index in any level (Figure 8). In group 1, there was 1 RCT that presented an SMD of 0.00 (95% CI, –0.32 to 0.32).44 In group 2, there were 2 studies presenting an SMD of –0.02 (95% CI, –0.35 to 0.31).24,31 No data were available for inclusion from retrospective cohort studies in group 3.
Forearm Supination Strength Index
Data from only 2 studies31,44 were included regarding forearm supination strength index, including 104 tenotomy and 105 tenodesis procedures. In the analysis of all groups, only 1 prospective study from group 2 showed a significant trend that forearm supination strength index was higher after tenodesis than tenotomy (Figure 9).44 The other study, from group 1, presented an SMD of 0.00 (95% CI, –0.32 to 0.32).31 Group 3 studies presented no relevant data.
SST Score
A total of 3 studies10,19,28 reported the SST score after tenotomy or tenodesis, including data from 70 tenotomy and 77 tenodesis procedures (Figure 10). In group 2, data were presented from 3 prospective cohort studies, which showed a significant increase in the SST score after tenodesis, with an SMD of –0.60 (95% CI, –0.94 to –0.27). No data were available in groups 1 and 3.
UCLA Score
Overall, 3 studies8,33,43 reported the UCLA score for 69 tenotomy and 74 tenodesis procedures (Figure 11). Studies in groups 1 and 2 presented no relevant data. Data from 3 studies in group 3 showed no significantly different result, with an SMD of –0.18 (95% CI, –0.55 to 0.19).
Forward Flexion and External Rotation at the Side
A total of 2 studies5,31 reported postoperative range of motion for 66 tenotomy and 64 tenodesis procedures (Figures 12 and 13). The studies showed no significant change in forward flexion or external rotation at the side. Studies in group 1 presented no relevant data. In group 2, there was 1 prospective cohort study that showed forward flexion or external rotation at the side, with an SMD of 0.06 (95% CI, –0.45 to 0.58) or 0.08 (95% CI, –0.43 to 0.60), respectively.31 In group 3, data from 1 retrospective study were presented with an SMD of –0.39 (95% CI, –0.85 to 0.08) or –0.57 (95% CI, –1.04 to –0.10), respectively.5
Discussion
The most important findings of this study were that patients undergoing tenodesis had a significantly lower risk of a cosmetic Popeye deformity than did those undergoing tenotomy in group 1 consisting of level 1 studies; that a lower incidence of a Popeye deformity as well as a better Constant score, forearm supination strength index, and SST score were seen in patients undergoing tenodesis than in those undergoing tenotomy from group 2 comprising level 2 studies; and that group 3 composed of level 3 or 4 studies showed a lower risk of a Popeye deformity and arm cramping pain after tenodesis. Otherwise, no significant difference was found in rotator cuff retears, VAS pain score, ASES score, elbow flexion strength index, UCLA score, and range of motion.
A residual aesthetic deformity after 2 potential procedures for the repair of LHBT injuries is a concern for surgeons and patients. A Popeye deformity often occurs in patients undergoing tenotomy, and some studies have shown a significant difference compared with tenodesis. The occurrence of the Popeye sign after tenotomy in our present study was also significantly higher in all study groups. In 2005, Wolf et al42 performed a biomechanical analysis of the biceps and found that the occurrence of the Popeye sign was associated with a significant risk of distal biceps tendon migration and a lower load to failure after tenotomy. MacDonald et al27 revealed that the contributing factors to the occurrence of a Popeye deformity in those undergoing tenodesis may have been undertensioning of the biceps tendon or anchoring of the biceps tendon in a place where there was too much slack in the tendon. The recent prospective RCT by MacDonald et al27 also showed a 3.5-times higher risk of a cosmetic Popeye deformity after tenotomy compared with tenodesis. Several meta-analyses30,34 have shown a similar result. In a review of the literature, Frost et al13 found that the incidence of a Popeye deformity after tenotomy ranged from 3% to 70%. Otherwise, the literature available regarding the incidence of a Popeye deformity after tenodesis has been divided: some studies have shown no deformity after tenodesis,10,29,41 while others have revealed that rates varied from 5.5% to as high as 24%.6,12,24,26,44 Interestingly, a recent retrospective study by Godenèche et al15 reported that no deformity at all was found after biceps tenodesis or tenotomy at 10-year follow-up.
Biceps pain as a result of cramping is a potential drawback of biceps tenotomy. Even if a cosmetic deformity is present, it rarely causes problems and is often even ignored by patients themselves,5 but related arm cramping pain is noticed and might compromise patient satisfaction. Cramping and cramp-like arm pain have been revealed in anywhere between 8% and 40% of patients undergoing tenotomy.41 Cramping pain in the bicipital groove was more frequently observed in patients undergoing tenotomy. In our retrospective cohort study group, a significantly higher risk of cramping pain in patients after tenotomy was also found, consistent with the findings of Ge et al14 and Gurnani et al.16
The Constant score is most frequently utilized as a tool for the assessment of the shoulder joint. Recently, a series of systematic reviews and meta-analyses14,30,44 found a significantly higher Constant score after tenodesis than tenotomy, although an earlier meta-analysis derived from RCTs and cohort studies showed no significant difference in the Constant score between the 2 groups.16 In the present study, the pooled Constant scores in the prospective cohort study group were significant after tenodesis, consistent with the results reported by Na et al,30 Shang et al,34 and Ge et al.14
The researchers have reported decreases of 20% in forearm supination strength and 8% to 20% in elbow flexion strength after spontaneous LHBT ruptures.29,35 We found no significant difference in terms of elbow flexion strength index. Because of different kinds of assessment tools and scales regarding forearm supination strength, we had to analyze 2 studies using forearm supination strength index as an outcome measure. Also, only a prospective cohort study by Oh et al31 demonstrated a significantly higher forearm supination strength index after tenodesis. In addition, an RCT by Lee et al26 found greater forearm supination power in the tenodesis group, and a level 3 study by Wittstein et al41 reported that the tenodesis group had significantly higher peak supination torque than did the tenotomy group.
The SST is also a widely used measure that assesses functional limitations of the affected shoulder. To our knowledge, the present study is the first to report a higher SST score in patients undergoing tenodesis compared with tenotomy; it was a meaningful finding statistically.
Strengths and Limitations
We performed a detailed and robust search spanning multiple databases without language restrictions, which allowed us to include studies from all over the world, thus improving the generalizability of our findings. The application of trial data and cohort studies allowed the inclusion of as many data as possible, such as good-quality research data especially from retrospective studies that can often be omitted in systematic reviews, therefore providing the most comprehensive update on clinical outcomes after tenotomy and tenodesis.
There were several limitations. The analysis was limited by the few relevant RCTs6,26,27,44 that have been published and small sample sizes, given the outcomes of interest. The inclusion of multiple study types inevitably results in significant heterogeneity, which therefore compromised the robustness of this study’s conclusions. In the retrospective cohort study group, with the inclusion of 2 level 4 studies,29,33 the pooled results of a Popeye deformity, arm cramping pain, the Constant score, and the UCLA score as relevant outcome measures had high heterogeneity. Furthermore, there was variability in the populations assessed (age, sex, LHBT injury type, rotator cuff injury type, sedentary patient vs manual laborer, dominant vs nondominant extremity), the comparator (biceps tenodesis methods or materials), the reporting of outcomes (including different kinds of assessment tools and scales), and the follow-up duration.
Conclusion
This meta-analysis demonstrated that compared with tenodesis, tenotomy had a higher risk of a Popeye deformity in all study groups; worse functional outcomes in terms of the Constant score, forearm supination strength index, and SST score in the prospective cohort study group; and a higher incidence of arm cramping pain in the retrospective cohort study group.
Footnotes
Final revision submitted September 16, 2020; accepted November 11, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Beijing Municipal Science and Technology Commission (grant Z171100001017209), National Natural Science Foundation of China (grants 81972130, 81703896, 81972107, 81902203, and 82072494), National Key Research and Development Program of China (grant 2017YFC0108102), and Capital Health Research and Development of Special Fund (grant 2020-2-4067). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Aflatooni JO, Meeks BD, Froehle AW, Bonner KF. Biceps tenotomy versus tenodesis: patient-reported outcomes and satisfaction. J Orthop Surg Res. 2020;15:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmad CS, ElAttrache NS. Arthroscopic biceps tenodesis. Orthop Clin North Am. 2003;34(4):499–506. [DOI] [PubMed] [Google Scholar]
- 3. Belay ES, Wittstein JR, Garrigues GE, et al. Biceps tenotomy has earlier pain relief compared to biceps tenodesis: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):4032–4037. [DOI] [PubMed] [Google Scholar]
- 4. Biz C, Vinanti GB, Rossato A, Arnaldi E, Aldegheri R. Prospective study of three surgical procedures for long head biceps tendinopathy associated with rotator cuff tears. Muscles Ligaments Tendons J. 2012;2(2):133–136. [PMC free article] [PubMed] [Google Scholar]
- 5. Boileau P, Baque F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. [DOI] [PubMed] [Google Scholar]
- 6. Castricini R, Familiari F, De Gori M, et al. Tenodesis is not superior to tenotomy in the treatment of the long head of biceps tendon lesions. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):169–175. [DOI] [PubMed] [Google Scholar]
- 7. Checchia SL, Doneux PS, Miyazaki AN, et al. Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg. 2005;14(2):138–144. [DOI] [PubMed] [Google Scholar]
- 8. Cho NS, Cha SW, Rhee YG. Funnel tenotomy versus intracuff tenodesis for lesions of the long head of the biceps tendon associated with rotator cuff tears. Am J Sports Med. 2014;42(5):1161–1168. [DOI] [PubMed] [Google Scholar]
- 9. Coleman BD, Khan HM, Maffulli N, Cook JL, Wark JD; Victorian Institute of Sport Tendon Study Group. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10(1):2–11. [DOI] [PubMed] [Google Scholar]
- 10. De Carli A, Vadala A, Zanzotto E, et al. Reparable rotator cuff tears with concomitant long-head biceps lesions: tenotomy or tenotomy/tenodesis? Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2553–2558. [DOI] [PubMed] [Google Scholar]
- 11. Friedman DJ, Dunn JC, Higgins LD, Warner JJP. Proximal biceps tendon: injuries and management. Sports Med Arthrosc Rev. 2008;16(3):162–169. [DOI] [PubMed] [Google Scholar]
- 12. Friedman JL, FitzPatrick JL, Rylander LS, Bennett C, Vidal AF, McCarty EC. Biceps tenotomy versus tenodesis in active patients younger than 55 years: is there a difference in strength and outcomes? Orthop J Sports Med. 2015;3(2):2325967115570848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 2009;37(4):828–833. [DOI] [PubMed] [Google Scholar]
- 14. Ge H, Zhang Q, Sun Y, Li J, Sun L, Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta-analysis. PLoS One. 2015;10(3):e01212 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Godenèche A, Kempf JF, Nove-Josserand L, et al. Tenodesis renders better results than tenotomy in repairs of isolated supraspinatus tears with pathologic biceps. J Shoulder Elbow Surg. 2018;27(11):1939–1945. [DOI] [PubMed] [Google Scholar]
- 16. Gurnani N, van Deurzen DF, Janmaat VT, van den Bekerom MP. Tenotomy or tenodesis for pathology of the long head of the biceps brachii: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3765–3771. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JP, Altman DG, Gøtzsche PC, et al. Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 19. Hufeland M, Wicke S, Verde PE, Krauspe R, Patzer T. Biceps tenodesis versus tenotomy in isolated LHB lesions: a prospective randomized clinical trial. Arch Orthop Trauma Surg. 2019;139(7):961–970. [DOI] [PubMed] [Google Scholar]
- 20. Hutton B, Wolfe D, Moher D, Shamseer L. Reporting guidance considerations from a statistical perspective: overview of tools to enhance the rigour of reporting of randomized trials and systematic reviews. Evid Based Ment Health. 2017;20:46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ikemoto RY, Pileggi PE, Murachovsky J, et al. Tenotomy with or without tenodesis of the long head of the biceps using repair of the rotator cuff. Rev Bras Ortop. 2012;47(6):736–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kerschbaum M, Maziak N, Scheuermann M, Scheibel M. Arthroscopic tenodesis or tenotomy of the long head of the biceps tendon in preselected patients: does it make a difference? Orthopade. 2017;46(3):215–221. [DOI] [PubMed] [Google Scholar]
- 23. Klepps S, Hazrati Y, Flatow E. Arthroscopic biceps tenodesis. Arthroscopy. 2002;18(9):1040–1045. [DOI] [PubMed] [Google Scholar]
- 24. Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38(8):1584–1590. [DOI] [PubMed] [Google Scholar]
- 25. Kukkonen J, Rantakokko J, Virolainen P, Aarimaa V. The effect of biceps procedure on the outcome of rotator cuff reconstruction. ISRN Orthop. 2013;2013:840965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee HJ, Jeong JY, Kim CK, Kim YS. Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: a prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg. 2016;25(7):1107–1114. [DOI] [PubMed] [Google Scholar]
- 27. MacDonald P, Verhulst F, McRae S, et al. Biceps tenodesis versus tenotomy in the treatment of lesions of the long head of the biceps tendon in patients undergoing arthroscopic shoulder surgery: a prospective double-blinded randomized controlled trial. Am J Sports Med. 2020;48(6):1439–1449. [DOI] [PubMed] [Google Scholar]
- 28. Mardani-Kivi M, Karimi Mobarakeh M, Keyhani S, et al. Treatment of long head of biceps tendon lesions together with rotator cuff tears: which method is preferred? Tenotomy or tenodesis. Tech Shoulder Elbow Surg. 2018;19(3):101–105. [Google Scholar]
- 29. Meraner D, Sternberg C, Vega J, Hahne J, Kleine M, Leuzinger J. Arthroscopic tenodesis versus tenotomy of the long head of biceps tendon in simultaneous rotator cuff repair. Arch Orthop Trauma Surg. 2016;136(1):101–106. [DOI] [PubMed] [Google Scholar]
- 30. Na YY, Zhu Y, Shi YT, et al. A meta-analysis comparing tenotomy or tenodesis for lesions of the long head of the biceps tendon with concomitant reparable rotator cuff tears. J Orthop Surg Res. 2019;14:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Oh JH, Lee YH, Kim SH, et al. Comparison of treatments for superior labrum-biceps complex lesions with concomitant rotator cuff repair: a prospective, randomized, comparative analysis of debridement, biceps tenotomy, and biceps tenodesis. Arthroscopy. 2016;32(6):958–967. [DOI] [PubMed] [Google Scholar]
- 32. Patel KV, Bravman J, Vidal A, Chrisman A, McCarty E. Biceps tenotomy versus tenodesis. Clin Sports Med. 2016;35(1):93–111. [DOI] [PubMed] [Google Scholar]
- 33. Sentürk I, Ozalay M, Akpinar S, Leblebici B, Cinar BM, Tuncay C. Clinical and isokinetic comparison between tenotomy and tenodesis in biceps pathologies. Acta Orthop Traumatol Turc. 2011;45(1):41–46. [DOI] [PubMed] [Google Scholar]
- 34. Shang X, Chen J, Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PLoS One. 2017;12(10):e0185788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Soto-Hall R, Stroor JH. Treatment of ruptures of the long head of biceps brachii. Am J Orthop 1960;2:192–193. [Google Scholar]
- 36. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Group. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 37. Szabo I, Boileau P, Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc Rev. 2008;16(3):180–186. [DOI] [PubMed] [Google Scholar]
- 38. Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(3):238–246. [DOI] [PubMed] [Google Scholar]
- 39. Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Accessed May 2020. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 40. Werner BC, Brockmeier SF, Gwathmey FW. Trends in long head biceps tenodesis. Am J Sports Med. 2015;43(3):570–578. [DOI] [PubMed] [Google Scholar]
- 41. Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med. 2011;39(4):857–865. [DOI] [PubMed] [Google Scholar]
- 42. Wolf RS, Zheng N, Weichel D. Long head biceps tenotomy versus tenodesis: a cadaveric biomechanical analysis. Arthroscopy. 2005;21(2):182–185. [DOI] [PubMed] [Google Scholar]
- 43. Zhang B, Yuan Y, Zhang HJ, Luo H, Yang C. Comparison of two different arthroscopic techniques for long head of biceps tendinitis. China J Orthop Trauma. 2019;32(8):701–706. [DOI] [PubMed] [Google Scholar]
- 44. Zhang Q, Zhou J, Ge H, Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):464–469. [DOI] [PubMed] [Google Scholar]