Abstract
A robust body of research has shown that traumatic experiences occurring during critical developmental periods of childhood when neuronal plasticity is high increase risks for a spectrum of physical and mental health problems in adulthood, including substance use disorders. However, until recently, relatively few studies had specifically examined the relationships between early life stress (ELS) and opioid use disorder (OUD). Associations with opioid use initiation, injection drug use, overdose, and poor treatment outcome have now been demonstrated. In rodents, ELS has also been shown to increase the euphoric and decrease antinociceptive effects of opioids, but little is known about these processes in humans or about the neurobiological mechanisms that may underlie these relationships. This review aims to establish a theoretical model that highlights the mechanisms by which ELS may alter opioid sensitivity, thereby contributing to future risks for OUD. Alterations induced by ELS in mesocorticolimbic brain circuits, and endogenous opioid and dopamine neurotransmitter systems are described. The limited but provocative evidence linking these alterations with opioid sensitivity and risks for OUD is presented. Overall, the findings suggest that better understanding of these mechanisms holds promise for reducing vulnerability, improving prevention strategies, and prescribing guidelines for high-risk individuals.
Keywords: early life stress, opioid use disorder, opioid sensitivity, mesocorticolimbic, endogenous opioid, dopamine, emotion processing, reward processing
1. Introduction
1.1. Prevalence of Early Life Stress (ELS)
In 2018, United States (US) Child Protective Service (CPS) agencies received an estimated 4.3 million referrals involving approximately 7.8 million children [1]. Approximately one-fifth of the children investigated were determined to be victims of maltreatment (abuse or neglect). The youngest and most vulnerable children (aged birth to one-year) have the highest rates of victimization at 26.7 per 1000. While these numbers are appalling, they probably represent only the tip of the iceberg as they do not include cases that go unreported or are unverified or cases that involve other forms of traumatic experiences. Findings from one of the largest and most diverse studies on adverse childhood experiences conducted to date revealed that 62% of the 248,934 non-institutionalized adults sampled across the US reported at least one traumatic experience during childhood and about a quarter reported at least three [2].
Adverse childhood experiences, also referred to as early life stress (ELS), may include events such as physical, sexual, or emotional abuse or neglect; exposure to domestic violence; family dysfunction; divorce; or death of a parent [3], which are outside the control of the child, have the potential to impair normal development, and may impair the child’s physical and/or psychological well-being [4]. The events often reflect either a threat involving harm to the physical integrity of the child or deprivation involving the absence of expected support, nurturance, or environmental enrichments [5]. Risk factors for maltreatment include caregivers with alcohol or drug problems, which are present in 12.3% and 30.7% of cases reported to the CPS, respectively. The rates of both of these risk factors have increased in the past several years, which is believed to be at least partially related to the increasing misuse of both prescription and non-prescription opioids [1].
1.2. Consequences of ELS
A robust body of research has now demonstrated that ELS exposure during early development when neuronal plasticity is high seems to have particularly damaging effects on an individual’s well-being. A history of severe or prolonged ELS is associated with increased likelihood of engaging in health risk behaviors, such as smoking, drug taking, and suicide attempts, as well as heightened risks for an array of emotional and physical health problems across their lifespan [6,7,8,9]. Indeed, findings of a growing number of studies, beginning with the landmark Adverse Childhood Experiences (ACE) study [10], suggest that there is a “dose–response” relationship between ELS and adult pathology, such that greater trauma is associated with a greater likelihood of such problems and with worse prognosis [11,12,13,14,15,16,17].
Epidemiological studies have identified positive associations between ELS and substance use disorders (SUDs) in both adolescents and adults [18,19,20]. While the majority of these findings have not been specific to opioid use disorder (OUD), the number of studies targeting opioids has grown in recent years. Consistent with the relationships observed between ELS and other types of SUDS, the findings show that ELS is associated with increased risks for opioid use initiation, injection drug use, overdose, use disorder, and poor treatment outcome [21,22,23,24,25,26,27]. Nevertheless, empirical studies elucidating the neurobiological mechanisms linking ELS with vulnerability for OUD are lacking.
1.3. Aim of this Review
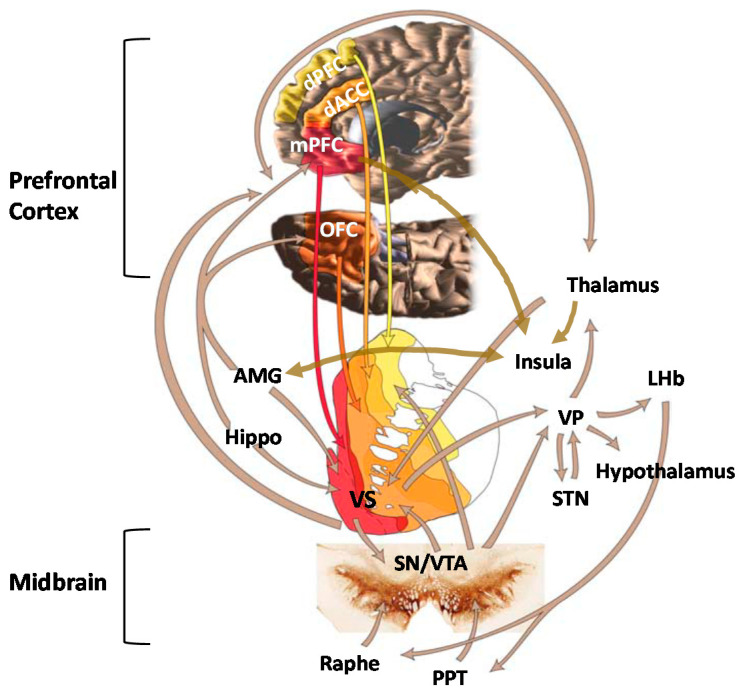
There is substantial and well-recognized variation in opioid sensitivity across individuals [28,29,30], which has been proposed to confer different levels of risk for opioid misuse and eventual OUD [31]. This review aims to establish a theoretical model (Figure 1) that summarizes the potential neurobiological mechanisms by which ELS alters opioid sensitivity, thereby contributing to future risks for OUD. This review first describes individual variation in risks for opioid misuse, the public health implications of opioid misuse/OUD, and the relationships between ELS and OUD. Next, the effects of ELS on mesocorticolimbic circuits that underlie emotion and reward processing and on the endogenous opioid and dopamine (DA) neurotransmitter circuits that play fundamental roles in these processes are discussed. Evidence linking these changes with individual differences in opioid sensitivity and risks for OUD is presented in each of the sections. The overarching hypothesis is that ELS-induced derangements in mesocorticolimbic brain regions lead to altered opioid sensitivity, which increases the abuse liability of these drugs and represents a preexisting vulnerability phenotype for OUD.
Figure 1.
Key structures of the mesocorticolimbic system include the ventral tegmental area (VTA); ventral striatum (VS); hippocampus (Hippo); amygdala (AMG); thalamus; insula; hypothalamus; and cortical regions, including the dorsal anterior cingulate cortex (dACC), medial prefrontal cortex (mPFC), orbitofrontal cortex (OFC), and dorsal prefrontal cortex (dPFC). Additional structures shown on the figure are the ventral pallidum (VP), lateral habenula (LHb), subthalamic nucleus (STN), substantia nigra (SN), and pedunculopontine nucleus (PPT). Adapted from Haber and Knutson, 2010.
2. Individual Differences Confer Differential Risk for OUD
2.1. Opioid Sensitivity
Animal studies examining characteristics of drug intake repeatedly find that a subset of animals display a strong preference for opioids over other reinforcers and that preference is opioid-specific and does not represent a general sensitivity to reinforcing substances. For instance, rats given the opportunity to self-administer heroin versus other drug (e.g., cocaine) or non-drug (e.g., saccharin) reinforcers frequently develop an immediate preference for one but not all substances; this preference predicts future heroin-administration and development of “heroin addiction” [32,33,34,35,36]. Such individual differences in preference are also evident in nonhuman primates; one study found that nonhuman primates exposed to five different psychoactive substances (cocaine, remifentanil, methohexital, ethanol, and ketamine) developed strong individual preferences for a single drug class in a manner similar to what was observed in rats [37]. Although there are limited data to inform of this effect in humans, empirical support is growing. One human laboratory study found that a given individual generally experienced the same level of effect (positive or negative) when administered the opioids heroin and hydromorphone but that the level of effect differed markedly across individuals, suggesting that humans also display pronounced individual differences in risk for opioid misuse [38]. Moreover, retrospective human cohort studies have repeatedly found that patient self-reported experiences of their first opioid exposure varied widely across individuals and that the subset of participants who experienced an initial euphoric effect were more likely to develop OUD [39,40], suggesting that experiencing euphoria during the first opioid exposure was not a universal response but did signal a risk for opioid misuse [41].
2.2. Mechanisms Underlying Opioid Sensitivity
The mechanisms underlying variations in opioid effects have not yet been clearly elucidated but are hypothesized to include an array of pharmacokinetic, pharmacodynamic, and pharmacogenetic contributions [42]. For instance, rats that were tested with four different mu agonists displayed strong within-subject consistency but substantial dose variability (30- to 300-fold) across animals with regard to analgesia [43], suggesting a strong biological mechanism underlying differences in opioid sensitivity. An examination of opioid effects across different animal strains revealed that the opioid dose needed to produce equivalent levels of conditioned place preference (CPP, a measure of drug reward) was substantially and consistently higher among Wistar versus Sprague Dawley rats and corresponded to differential levels of DA release in the nucleus accumbens (NAc) [44]. Such a variability is also evident within the same animal strain; one study observed a continuum of responses in Sprague Dawley rats ranging from the 10% of animals showing a preference for morphine over food after 4 days to another 10% of the sample not developing a morphine preference even after 38 days of access [45]. A final study observed pronounced differences in the rate of heroin and oxycodone intake and preference across the four different sub-strains of the 129 mouse [46]. These strain-based differences suggest a pharmacogenetic contribution to individual differences; the most frequently explored gene in the context of opioid use has been OPRM1, which codes for the mu opioid receptor. OPRM1 appears to produce clinically meaningful differences in human opioid sensitivity [47,48,49,50] and to modulate human cortisol stress response [51], thus providing a putative pathway by which ELS may confer a unique risk for opioid misuse and OUD.
Stress has been independently associated with opioid sensitivity, with several studies observing evidence of greater OUD risk (e.g., increased opioid self-administration and drug reinstatement) [52,53,54] among animals exposed to stress from restraint [55], foot-shock [52,56], and intermittent swim [57] assays. Stressful stimuli have also been shown to produce a hyporesponsive state of the endogenous opioid system in animals [58], and corticosterone release following a stressful stimulus has been causally and independently linked to increased opioid self-administration [57]. Early life stress appears to be particularly destructive because it produces enduring conformational changes in the endogenous opioid system that impact drug use behavior [59,60]. The deleterious impact of ELS can be observed as far back as gestational exposure, wherein pups whose mothers were exposed to stress during gestation were more likely to acquire morphine CPP during their adolescence [61]. Converging evidence indicates that ELS in animals reduces opioid (particularly mu) receptor availability [62,63,64] and decreases downstream dopamine signaling [63,65] in a way that may bolster the reinforcing effects of opioids. Such an effect is also evident in behavioral tests where young animals exposed to stress display more CPP for µ- versus κ-opioid agonists [66]. Altogether, these data suggest that ELS may produce conformational changes in the opioid system that enhance opioid sensitivity, which may serve as the basis for the pronounced behavioral effects observed among adults.
3. Societal Impact of Opioid Misuse/Use Disorder
3.1. Epidemiological Findings
Not all persons who are exposed to opioids develop OUD, but those who do can experience devastating consequences. Opioids are considered essential medicines for acute and cancer pain, palliative care, and treatment of opioid dependence by the World Health Organization [67] and are used for medicinal purposes worldwide. Although the availability and consumption of opioid analgesics are considered inadequate to provide sufficient pain relief in some regions [68], in high-income countries, such as the US and Canada, increased prescribing and availability, aggressive promotion, and under-regulation of these drugs from the 1990s to around 2011 has led to a serious national crisis and spiraling needs for healthcare services. In 2018, 57.8 million people globally were estimated to have used opioids in the past year, with almost half of them misusing pharmaceutical opioids [69]. In fact, prescription pain reliever misuse in the US is second only to marijuana as the first illicit substance that people try, with approximately 4400 new initiates each day [70].
Examination of trends in opioid analgesic abuse from 2002 to 2011 showed that approximately 75% of US heroin users reported being introduced to opioids through prescription drug use [71,72]. However, despite evidence that misuse of prescription pain relievers has declined (from 4.7% in 2015 to 3.5% in 2019), heroin use has remained relatively stable over the past decade. It is estimated that 1.6 million people in the US suffered from OUD in 2019 [70]. These problems are accompanied by school dropout, unemployment, poor quality of life, cooccurring psychiatric disorders, and problems with the criminal justice system [73], which represent not only tremendous burdens to individuals and families but also a US “economic burden” of roughly $78.5 billion a year [74]. Two out of three drug overdose deaths in the US in 2018 involved an opioid, which can be attributed to the wider availability of high potency opioid analgesics and synthetic opioids since about 2013 [73,75,76].
3.2. Risk Factors
Risk factors for opioid misuse and OUD include both genetic and environmental determinants. Findings of twin studies suggest that genetic variance explains approximately half of the liability for OUD, although some of this variance is likely a genetic disposition to drug use disorders in general [77,78,79]. However, environmental factors also play a prominent role, including drug availability, peer pressure, other substance use, adverse childhood experiences, family history of alcohol and drug use disorder, and other comorbid mental health problems [71,73,80,81,82,83,84]. Predictors of prolonged opioid use in patients with musculoskeletal problems include past or current substance use problems, higher initially prescribed doses, mood disorders, and depression [71,85,86]. Among chronic pain patients, predictors of misuse include anxiety, anger, pain intensity, and depression [87,88,89] as well as measures of distress intolerance [90], pain catastrophizing [91], and difficulties in emotion regulation [92].
4. Evidence of ELS and OUD Associations
4.1. ELS Is Highly Prevalent among Persons with OUD
An extensive body of research has shown that ELS exposure profoundly increases risks for the development of alcohol, cocaine, marijuana, and nicotine use disorders [18,93,94,95,96,97], but only recently has it become evident that childhood adversity is also common among individuals with OUD [22,98,99,100,101]. A recent meta-analysis found that 41% of women and 16% of men with OUD reported a history sexual abuse and that 38–42% reported other types of mistreatment before the age of 18 [100]. Early life stress has also been linked to higher rates of relapse, suicidal ideation, overdose, and a more rapid transition from misuse to OUD in these individuals [21,22,102,103].
Data from the National Longitudinal Study of Adolescent to Adult Health study (n = 12,288) revealed a dose–response relationship between ELS and adulthood prescription pain reliever misuse that increased in strength from young to middle adulthood [104]. There is also evidence that the odds of prescription opioid/pain reliever misuse increase as a function of the number of ELS events experienced [26,104,105,106] and that other behaviors, such as age of first opioid use and injection drug use, are also associated with the number of early life stressors endorsed [25,104,106]. Although the aggregate number of events seems to have a cumulative effect [22,107], the type of early life stressor may also impact the outcomes. For example, in one study, neglect, emotional abuse, and parental incarceration were associated with 25–55% increased odds of prescription pain reliever misuse in young adults while sexual abuse and witnessing violence were associated with nearly three and five times the odds of injection drug use [104]. Chronicity, severity, and developmental timing of these experiences are also differentially related to drug use outcomes [18].
4.2. Persons with ELS and/or OUD Exhibit Similar Pathologies
Early life stress is associated with deficits in emotion regulation and neuroendocrine responses to stress that persist into adulthood and are associated with the development of several forms of psychopathology [5,108,109,110,111,112,113,114,115,116,117,118]. Recently, it has been suggested that such deficits may be intermediaries in the pathway that links ELS with the development of OUD [90,103,119,120,121]. For instance, emotional responses to neutral and unpleasant stimuli were positively associated with childhood neglect and severity of addiction in heroin users, suggesting that ELS impairs the ability to modulate emotions and to cope with stress. These deficits then give rise to a range of maladaptive behaviors that can predispose to OUD [122]. Similar findings were reported by Ghorbani et al. [123], who showed that ELS was indirectly related to heroin craving via a limited ability to regulate emotions. Internalizing and externalizing symptoms have been shown to partially mediate the association between ELS and prescription opioid misuse [24,106]. These findings suggest that self-medication may play a role in generating and maintaining both recreational and prescription opioid misuse in ELS-exposed individuals [124,125]. In addition to their euphoric and analgesic effects, opioids relieve stress through their inhibitory actions on the hypothalamic-pituitary-adrenal (HPA) axis [120,126,127], which can be highly negatively reinforcing [128] to individuals with such affective vulnerabilities.
5. Role of Mesocorticolimbic Emotion Processing Circuits in ELS and OUD
5.1. Effects of ELS on Emotion Processing Circuits
Mesocorticolimbic brain circuits include several cortical and subcortical structures that are integrally involved in stress regulation and emotion and reward processing [129] (Figure 1). Two regions that seem to be particularly impacted by ELS are the amygdala (AMG) and medial prefrontal cortex (mPFC) [130,131,132,133]. These structures have extensive bidirectional connections and normally work together to integrate the expression of fundamental aspects of emotional learning, memory, and behavior as well as play prominent roles in stress responsivity [134,135,136]. As maturation of these regions occurs throughout juvenile and adolescent periods, perturbations that occur during childhood can alter their normal neurodevelopmental trajectories, which may negatively impact psychological function later in life [135]. Alterations in AMG volume [137,138] and task-related hyper-responsivity [133,139,140,141,142,143] have been observed in both adults and children with a history of ELS. Oshri et al. [144] showed that ELS-related changes in AMG volume were associated with increased anxiety, depressive symptoms, and alcohol use. Heightened threat-related AMG reactivity has been shown to predict internalizing symptoms [145] and risks for alcohol use disorder [146,147]. In contrast, ELS has been associated with reduced mPFC volume [148,149] and lower mPFC activation during both resting state and cognitive tasks [150,151,152].
Normally, the mPFC, particularly the ventral mPFC, modulates fear behavior by providing top-down control of AMG and HPA-axis responses to stress [153,154]. Dysfunction in AMG-mPFC connectivity has been implicated in several psychiatric disorders, including depression and schizophrenia [135], and there is evidence that top-down control may be altered in individuals with a history of ELS. While valence (positive or negative) and regional specificity vary somewhat across studies [136], atypical patterns of connectivity have been observed between the AMG and PFC in both youth and adults with a history of ELS. Findings in children and adolescents include evidence of weakened left AMG–anterior cingulate cortex (ACC) resting state functional connectivity (rs-FC), which was associated with higher levels of current anxiety in one study and mediated the relationship between ELS and internalizing symptoms in another [155,156,157]. Gee et al. [140] reported precocious maturation of the mPFC–AMG pathway in previously institutionalized youth, which reflected a developmental shift from positive to negative coupling and seemed to confer some degree of reduced anxiety. These somewhat counterintuitive findings suggested that accelerated maturation of these connections may serve to facilitate coping with environmental insults in the short term but lead to less efficient stress regulation and increased vulnerability for psychopathology in adulthood [135]. Associations between AMG–PFC connectivity and cortisol levels have also been reported in humans [158] and nonhuman primates [159], suggesting that ELS-related changes in neuroendocrine function contribute to the neural deficits and problems with emotion regulation that are observed in these individuals in later life.
Similar ELS-related findings have been reported in adults, including weakened AMG–pregenual ACC rs-FC, which predicted elevated state anxiety [160], and reduced AMG–ventral mPFC rs-FC, which predicted increased levels of pro-inflammatory cytokines [161]. However, inconsistent findings have also been reported, which may be related to variations in network configurations between resting state and task-related co-activations, task-specific engagement, or other methodological differences among studies. In contrast to the findings during resting state scans, Jedd et al. [162] reported increased AMG–PFC during an emotion processing task in ELS-exposed adults. Kaiser et al. [163] found that ELS was associated with greater negative AMG–dorsolateral PFC rs-FC, which mediated the relationship between ELS severity and blunted cortisol response to acute stress, and elevated dynamic AMG–rostral ACC rs-FC, which was associated with reduced negative mood following a social evaluation stress challenge. These findings suggested that ELS may be associated with both maladaptive and compensatory changes in mesocorticolimbic circuits. Though most studies in this area of research are cross-sectional and preclude determinations of causality, overall, these findings suggest that neuroplastic aberrations incurred as a result of ELS may persist decades later into adulthood, leading to alterations in physiological and emotional responses to stress.
There has been growing evidence that the effects of ELS on mesocorticolimbic brain structures may be partially related to repeated or chronically high levels of corticotropin-releasing factor (CRF) and glucocorticoids (GCs) [164,165,166,167,168,169] that occur during early stages of ELS [170,171,172]. Although other mechanisms may be involved, composite findings from several lines of research indicate that epigenetic processes involving HPA-axis regulation and GC signaling underlie many of these effects [173,174]. Glucocorticoid receptors (GR) are densely located throughout the brain, including stress-sensitive regions such as the mPFC, AMG, hippocampus, NAc, and hypothalamus [175,176]. Regional differences in methylation and both increases and decreases in brain GR expression have been observed in rodents and monkeys exposed to ELS [177,178,179,180]. Findings of one postmortem study showed decreased levels of GR mRNA in the hippocampus of suicide victims with a history of ELS compared to those without this history [181]. Greater GC receptor methylation has also been found in the peripheral cells of ELS-exposed humans [182], which was recently shown to moderate associations between ELS and cortisol stress reactivity [183].
5.2. Emotion Processing Circuit Interface between ELS and OUD
Although OUD is underrepresented in the neuroimaging literature on addiction compared to other SUDs [184], findings from a limited number of human fMRI studies have implicated brain circuits involved in stress and emotion regulation in the perpetuation of this disorder. For example, the AMG has been shown to be activated in response to heroin drug cues [185,186,187] and plays a central role in the generation of cue-elicited craving in persons with OUD [188]. Schmidt et al. [189] found that patients with OUD displayed higher left AMG response to fearful faces than healthy controls during acute withdrawal, which correlated with levels of state anxiety, ACTH, and cortisol levels in all subjects and with heroin craving in patients. However, AMG connectivity was reduced to levels that did not differ from those of healthy controls after acute heroin maintenance treatment, suggesting that the results were driven by the drug-related attenuation of stress hormone release [189]. Alterations have also been found in mPFC activation and connectivity in abstinent, currently using, and methadone-maintained persons with OUD during resting state and cue reactivity, inhibitory control, and emotion processing tasks [190,191,192,193]. Administration of the opioid antagonist naltrexone has been shown to decrease AMG and to increase PFC responses to drug cues in abstinent heroin users, which suggests that naltrexone’s clinical effects may result in part from its ability to increase the capacity for conscious self-regulation [186]. Wang et al. [194] further showed that greater pretreatment mPFC response to heroin-related cues predicted greater adherence to naltrexone in detoxified heroin-dependent individuals, demonstrating that lower mPFC activity may contribute to increased craving, negative affect, and reduced treatment compliance. In general, the imaging data suggest that OUD is associated with reduced PFC monitoring, weak inhibitory controls, dysfunctional stress responses, problems with emotion regulation, and heightened negative affective states.
Nevertheless, in spite of the commonalities in behavioral and neural deficits that have been observed between ELS-exposed individuals and persons with OUD, to our knowledge, relationships between ELS-induced changes in brain function and opioid misuse have never been examined. Findings from several lines of research support speculations that ELS-related changes in circuits that underlie stress and emotion processing may represent an underlying opioid vulnerability pathway. For instance, impairments in AMG connectivity have been shown to mediate associations between ELS and internalizing symptoms in adolescents [155] while internalizing and externalizing symptoms partially mediate associations between ELS and opioid misuse [24,106]. These findings suggest that ELS may lead to changes in brain function that impair the ability to modulate emotions and to cope with stress, which may then lead to a range of maladaptive behaviors that can predispose to opioid misuse. Poor coping and emotion regulation profiles have previously been shown to predict initiation of opioids at an earlier age, past 90-day heroin use, increased probability of injecting a drug, and less likelihood of heroin abstinence after treatment, which may all be related to a need for self-medication [195].
It is important to note that these findings do not specifically explain the preference for opioids in these individuals as poor coping and emotion regulation have also been associated with misuse of other substances [195,196]. However, findings of a growing body of research suggest that ELS-related changes in emotion processing regions may lead to altered opioid sensitivity. Prefrontal and NAc activation are partially mediated by the endogenous opioid system [31,197], which is altered in ELS-exposed individuals. In one study, opioid antagonist naltrexone modulated activation of the mPFC during negative emotional processing as a function of ELS in both healthy controls and individuals with alcohol, cocaine, and/or opioid use disorders [198]. Specifically, the greater the severity of abuse, the greater the sensitivity of the mPFC to the effects of naltrexone, suggesting that ELS-related changes in mPFC function may underlie individual differences in responsiveness to the drug. Persons with AUD/SUD also reported higher levels of depression, anxiety, and stress sensitivity than the control group, which was somewhat ameliorated by naltrexone. These data are consistent with preclinical evidence showing that naltrexone reduces ethanol consumption in rats that experienced prolonged separation but not short absences of the dam [199]. Collectively, the data support hypotheses that ELS-induced derangements in endogenous opioid function in stress and emotion processing circuits may underlie part of the variability detected in opioid sensitivity across individuals. However, significant gaps still remain in our understanding of how ELS-induced changes in these circuits influence the course of opioid addiction and why alterations in function are associated with maladaptive behaviors in some individuals but not others.
6. Role of Mesocorticolimbic Reward Processing Circuits in ELS and OUD
6.1. Effects of ELS on Reward Processing Circuits
Reward functions underlying addiction are generally thought to involve the ventral tegmental area (VTA) and mesolimbic DA neurons that project from the midbrain VTA to the ventral striatum (VS) or, more specifically, the NAc, which is considered the center of reward learning. It is well-established that ELS increases feelings of dysphoria and anhedonia in humans and leads to an attenuation of behavioral responses to primary and conditioned rewards in animals [200,201,202,203,204,205]. Several investigators have hypothesized that these outcomes may be the result of ELS-induced alterations in NAc function. Goff et al. [206] reported hypoactivation of the NAc during an emotional faces task in adolescents with a history of ELS, which was associated with higher levels of depression. Between-subject comparisons of children ages 5–10 yrs. and adolescents 11–15 yrs. old further indicated that the ELS group failed to show the developmentally typical rise in NAc reactivity shown by the comparison group. The findings suggested that ELS impacts the development of the VS, resulting in hypoactivity, which leads to dysfunctional reward and motivational processing. Other investigators have shown similar findings consistent with notions of reduced activation of striatal structures and dampened behavioral responses to reward in ELS-exposed individuals [203,207,208]. Given prior evidence that blunted reward responsivity may be a marker of motivational mechanisms underlying addiction vulnerability [209,210,211,212,213], these findings suggest that alterations in vs. function may be one mechanism that underlies increased susceptibility for addiction in ELS-exposed individuals.
Several cross-sectional fMRI studies have examined associations between ELS-induced changes in reward circuitry and subjective measures of reward [214,215,216]. For example, Dillon et al. [203] found that ELS-exposed young adults reported elevated depressive and anhedonic symptoms, rated reward cues less positively, and exhibited decreased anticipatory reward activity in left basal ganglia regions relative to controls during completion of a monetary reward task. Corral-Frias et al. [217] showed that blunted vs. reactivity to reward was associated with increased anhedonic symptoms, which indirectly predicted other depressive symptoms and problematic alcohol use in ELS-exposed young adults. Marusak et al. [218] examined blood-oxygen-level-dependent (BOLD) responses to an emotional conflict task, showing that greater conflict-related AMG reactivity was also associated with diminished trait reward sensitivity in adolescents with a history of ELS. Overall, these findings are consistent with behavioral evidence from preclinical studies showing that ELS impairs motivation to work for rewards in animals, suggesting a downregulation of reward functions [219,220,221,222].
Longitudinal studies are somewhat rare in this area of investigation. However, Birn and colleagues [223] found that young adults who experienced a high level of stress as children showed deficits in decision-making during a reward processing task and reported more real-life risk-taking behaviors than individuals without this history. They also displayed alterations in reward processing regions, including the middle temporal gyrus, precuneus, putamen, insula, and left inferior frontal gyrus, some of which mediated relationships between ELS and reward processing or self-reported risk-taking behavior. Casement et al. [224] showed that cumulative life stress from ages 15–18 years was associated with decreased mPFC response during both anticipation and receipt of monetary reward at age 20 in adult males. The blunted mPFC response to reward predicted greater symptoms of alcohol dependence and mediated the relationship between life stress and alcohol use. Boecker et al. [225] found that ELS assessed at 3 months after birth and between the ages of 2 and 15 years was associated with hyporesponsiveness in reward circuits during reward anticipation (i.e., VS, putamen, and thalamus) and hyperresponsiveness during reward delivery (i.e., insula, pallidum, substantia nigra, and right posterior hippocampus) in healthy young adults who had been followed prospectively over 25 years.
To date, only a small number of studies have examined the influence of ELS on functional connectivity in reward processing regions. Fareri et al. [226] found that resting state coupling between the VS and mPFC was stronger in previously institutionalized youth than in youth who were raised by their biological parents; the fMRI findings mediated differences in social problems between the two groups. Blunted maturation of VTA–mPFC resting state connections [227] and increased connectivity of the insula to salience network seed regions have also been observed in trauma-exposed youth, which was associated with diminished reward sensitivity [216]. Hanson et al. [228] found elevated VS–mPFC functional connectivity during a monetary reward task in college-age adults with a history of both ELS and higher levels of recent life stress, which suggested that the deficits observed in youth persist into young adulthood. Although further prospective research is needed, collectively, the findings suggest that blunted VS activity and elevated functional connectivity in reward processing regions may represent neurobiological markers that serve as indicators of diathesis for psychological dysfunction in adults with a history of ELS. Overall, the findings are consistent with those of preclinical research showing broad changes in connectivity of the limbic and reward networks of adult rats exposed to ELS [229] as well as deficits in reward responsiveness and approach motivation [220].
6.2. Reward Processing Circuit Interface between ELS and OUD
In recent years, fMRI has been used to evaluate abnormalities in activation and functional connectivity of reward regions in abstinent and currently using heroin-dependent individuals using a variety of paradigms [184,230]. In general, brain activation has been shown to be upregulated in the reward and salience network brain regions of persons with OUD in response to drug-related cues [231]. Dysfunctional connectivity has also been reported using a variety of methods, including at rest, in response to heroin-related cues, and while performing decision-making or response inhibition tasks in regions that include the mPFC, orbitofrontal cortex (OFC), dorsolateral PFC, ACC, posterior cingulate cortex (PCC), and NAc [191,192,232,233,234,235]. In one study, rs-FC between regions involved in reward and motivation (e.g., VS-ACC and VS-OFC) was increased and connectivity between regions involved in cognitive control (e.g., PFC-ACC) was decreased in chronic heroin users, most of whom were being treated with methadone [236]. Functional connections between the AMG and mPFC have also been shown to be critical for the processing of opioid rewards [237,238,239]. Engagement of the reward networks is associated with craving, addiction severity, duration of use, and/or relapse in persons with OUD [191,240,241].
Preclinical studies have demonstrated that chronic opioid use produces abnormalities in mesocorticolimbic reward circuits that contribute to opioid misuse and OUD [191,239,242,243,244,245,246]. However, genetic and environmental factors, such as stress, may also lead to functional deficits in these circuits that underlie increased susceptibility for drug misuse and dysregulated responses to opioids. As previously described, ELS-related derangements in reactivity and connectivity of reward circuits have been associated with problematic alcohol use and risks for alcohol use disorder as well as well-established intermediate phenotypes for SUDs (e.g., anhedonia, deficits in decision-making, and problems with reward-based learning). However, virtually nothing is known about how ELS-induced alterations in reward circuits influence opioid sensitivity or about the role that such alterations play in the transition from opioid use to misuse. Similarities between ELS-induced alterations in connectivity and those observed in persons with OUD suggest that ELS-related derangements may predate and increase vulnerability for this disorder. This relationship is also suggested by evidence that ELS-induces changes in DA and endogenous opioid neurotransmission, which mediate the reward functions of these regions [247,248]. However, further research is needed to test these hypotheses.
7. Role of Endogenous Opioid Neurotransmitter System in ELS and OUD
7.1. Effects of ELS on Endogenous Opioid Function
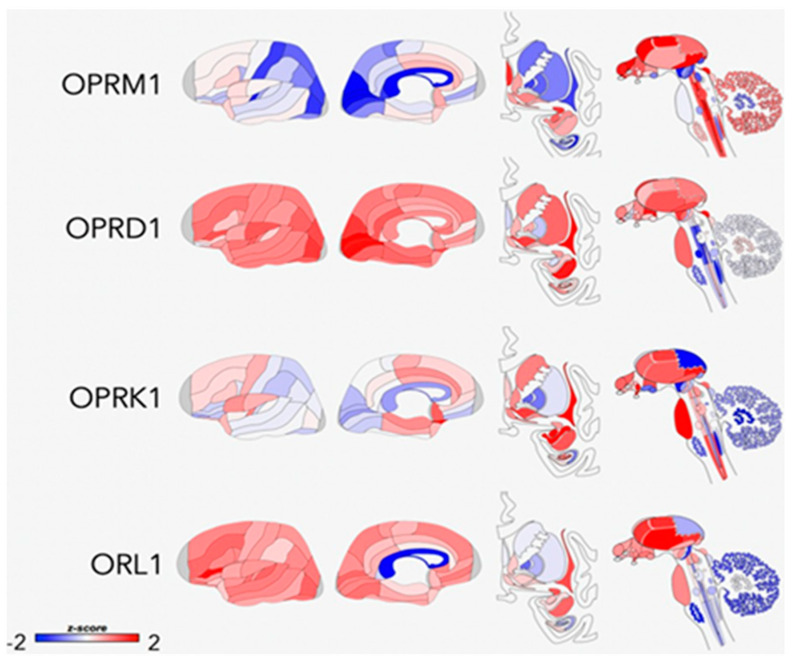
Opioid peptides and receptors are widely distributed throughout the central nervous system and are thought to modulate many aspects of human behavior, including reward, affective states, pain responses, and other physiological functions [249] (Figure 2). Considerable variability in responses to opioid drugs has been noted in the general population, which are associated with differences in therapeutic response to treatment as well as risks for drug misuse [41,47,250,251]. Such differences may be due to both heritable factors and environmental influences that interact with the genome through epigenetic or transcription mechanisms to produce long-term alterations in the endogenous opioid system [252]. Endogenous opioid peptides are found throughout the peripheral and central nervous systems, where they play a role in many different types of functions, including nociception and analgesia, stress responses, physiological functions, social behavior, mood, and reinforcement [127,253,254,255,256,257]. Normally, this system is activated by acute stress, leading to the release of endogenous opioids at multiple sites in the brain. The release of opioids generally serves to attenuate stress responses by actions that include modulating the release of CRF, which returns the systems to pre-perturbation levels. However, repetitive stress exposure (which is characteristic of ELS) leads to an imbalance between CRF and opioids such that opioid inhibitory tone is favored [258]. Although the relationships require further testing, there is some evidence that chronically high tonic levels of endogenous opioids may trigger downregulation or reduced affinity of µ-opioid receptors (MOR) and lower phasic release of opioid peptides, resulting in hypoactivity of this system [259,260].
Figure 2.
Areas of opioid receptor gene expression (μ = OPRM1, δ = OPRD1, κ = OPRK1, and NOP = ORL1) in the human brain (donor: H0351.1015, 55 yrs, male, and white or Caucasian). The cortical gene expression patterns are displayed on an inflated cortical surface (outer and inner surfaces of the left hemisphere). Subcortical structures of the brain are represented from the frontal view, and subcortical as well as brainstem structures are shown in the side view. The color bar displays expression values using z-score normalization. Reproduced from Peciña et al., 2019. Creative Commons license: http://creativecommons.org/licenses/by/4.0/, accessed on 14 April 2021.
Conformational changes that have been specifically associated with ELS in preclinical studies include changes in opioid peptide levels [63,261], kappa receptor signaling [262], and variations in mu- and kappa-receptor (KOR) gene expression [62,64,65,263,264] in brain regions that include the hypothalamus, PFC, periaqueductal gray (PAG), AMG, NAc, rostral ventromedial medulla, and lateral habenula. Nylander and Roman [251] concluded that the most pronounced effect of ELS on opioid peptides is on Met-inkephalinArg6Phe7 (MEAP) levels, which are reduced in ELS-exposed animals. Rats with lower MEAP levels exhibit altered risk-taking behavior and a propensity for high ethanol intake, consistent with theories that an inherent opioid deficiency leads to increased susceptibility for addiction. Given the large number of physiological functions that are regulated by the endogenous opioid system, it is reasonable to speculate that hypofunction of this system could also lead to dysregulation of stress responses, altered pain-processing, and an array of stress-related disorders.
The first direct evidence of ELS effects on opioid neurotransmission in humans was reported by Lutz et al. [92], who conducted a postmortem study showing that ELS was associated with the downregulation of kappa receptors in the anterior insula of both depressed individuals who died by suicide and controls who died suddenly from accidental causes. Cortisol response to naltrexone has also been found to be blunted in high vs. low ELS women, which similarly linked ELS with downregulation of endogenous opioid activity [265]. The authors posited that these effects may reflect an adaptation of the central opioid system that shapes how a person responds to motivationally significant stimuli. The findings of a recent study by Garland et al. [266] are consistent with these notions, showing that ELS was associated with blunted heart rate variability (HRV) and increased cue-elicited drug craving during a task involving negative emotions in female opioid-treated chronic pain patients. In theory, the reduced capacity to respond to negative emotional stimuli could be the result of reduced opioid function. However, opioid function was not specifically examined and the cross-sectional nature of the study makes it impossible to know whether the deficits predated or were a result of chronic opioid use. It is also unclear whether the findings would be replicated in an opioid-naïve sample without prior history of chronic pain. Nevertheless, in spite of the limitations, aggregate findings from this small body of human studies are consistent with the preponderance of preclinical evidence suggesting that ELS leads to a deficiency in opioid neurotransmission.
7.2. Interface between ELS and OUD via Endogenous Opioid Function
Much of the current research on the neurobiology of OUD is focused on gaining a better understanding of the molecular and cellular aspects of opioid receptor function that contribute to vulnerability for this disorder [267] or on characterizing how genetic influences on receptor function translate to abuse liability and treatment outcomes [268,269,270]. Although this research holds promise for explaining some of the variability in clinical responses to opioids, the evidence that heritability estimates for OUD are only about 23–54% [271] suggests that there is also a need for better understanding of the effects of environmental factors that help to shape the behavioral and molecular profiles of individuals with this disorder.
Recent preclinical findings have provided initial evidence that ELS-induced changes in endogenous opioid function may alter opioid agonist and antagonist sensitivity. In one study, ELS-exposed rats showed greater place preference for the µ-agonist morphine but lesser aversion to the k-receptor agonist spiradoline [66], suggesting that ELS may enhance opioid abuse vulnerability by both increasing reward sensitivity and by decreasing the aversive effects at k-receptors [272]. Vazquez et al. [273] showed that maternal deprivation in rat pups was associated with hypersensitivity to the reinforcing effects of morphine and development of morphine dependence in adulthood, which was likely a result of basal hypoactivity of the nucleus accumbens (NAc) enkephalinergic system. Nakamoto et al. [64] found that ELS-exposed mice displayed decreased µ- and k-opioid receptor messenger mRNA expression in the PAG and increased k-opioid receptor expression in the AMG. A lack of morphine antinociception was observed in stressed mice in adulthood but not immediately after ELS exposure. Bruehl et al. [41] recently extended these findings to humans, showing that endogenous opioid function assessed by naloxone administration was inversely associated with euphoric effects of a single dose of 0.09 mg/kg morphine sulfate in patients with low back pain. According to reinforcement theory [274], either hypersensitivity to the reinforcing effects or diminished sensitivity to the antinociceptive effects of opioids could lead to misuse of these drugs, through positive or negative reinforcement, respectively. There is also evidence that ELS-induced changes in endogenous opioid function may lead to dysfunctions in DA neurotransmission in rats [63,275]. In one study, ELS increased KOR-mediated inhibition of baseline and stimulated DA release, which contributed to a hypodopaminergic state and escalated ethanol intake. Taken together, these findings provide support for hypotheses that ELS-induced conformational changes in the endogenous opioid system [58,273] may alter the effects of opioid drugs in ways that increase risks for their misuse [59,276,277,278].
Although not specific to OUD, the findings from human positron-emission tomography (PET) imaging studies have found associations between endogenous opioid function, and subjective and behavioral responses to both drugs of abuse and pain. For example, k-opioid receptor availability is associated with stress-induced cocaine self-administration in subjects with cocaine-use disorder [279], altered vs. binding potential for the µ-receptor agonist [11C]carfentanil is associated with alcohol craving and relapse risk in abstinent alcoholics [280,281,282], the µ-receptor binding potential correlates with nicotine dependence and reward in smokers [283], and alterations in endogenous opioids and µ-receptors in patients with chronic nonspecific back pain are associated with both sensory and affective elements of the pain experience [284]. To date, we are not aware of any neuroimaging studies that have evaluated the effects of ELS on opioid neurotransmission in humans or any controlled human laboratory studies that have examined ELS contribution to human opioid sensitivity. Better understanding of the role that individual differences in sensitivity play as mediators in the transition from prescription or recreational opioid use to opioid misuse and risky-drug related behaviors may help to inform the development of more effective interventions for ELS-exposed individuals.
8. Role of Dopamine Neurotransmitter System in ELS and OUD
8.1. Effects of ELS on Dopamine Function
Another neurotransmitter system that plays a fundamental role in stress responses and emotional-motivational activation of reward seeking is the midbrain DA system [285,286,287,288]. The DA mesolimbic pathway projects from the VTA to the VS, AMG, and hippocampus, and the mesocortical pathway projects from the VTA to cortical regions such as the ACC, OFC, mPFC, and insula. Considerable preclinical evidence has emerged showing that ELS may lead to profound and long-term derangements in brain DA neurotransmission. Abnormalities that have been observed include but are not limited to altered D1, D2, and D3 receptor mRNA expression; decreased density of DA transporters; increased DA metabolites in the striatum and/or NAc [289,290,291,292,293,294]; and reduced rates of DA clearance in the mPFC [295]. Both enhanced [290,296,297] and blunted [290,296,297,298] striatal DA responses to stress have been observed in adult rodents exposed to ELS. It has been suggested that, in general, ELS induces a hypodopaminergic state with an associated enhancement of DA system responses to salient stimuli [63]. There is also a general consensus that the effects of ELS on DA neurotransmission has broad-based clinical implications for the development of psychopathological conditions, such as schizophrenia and addiction, which are known to be associated with malfunctions in DA neurotransmission [96,299,300,301]. It is hypothesized that these effects may be the result of excessive exposure to glucocorticoids during early life, which impacts the organization and epigenetic control of midbrain DA systems [302,303,304,305].
Functional changes that occur in the DA system as a result of ELS may also be associated with altered neurochemical and behavioral responses to drug abuse. Early life stress may lead to enhanced DA and behavioral responses to psychostimulants and changes in drug consumption patterns that reflect greater vulnerability for drug abuse in later life in animals [275,290,297,298,305,306,307,308,309]. The first evidence that some of these findings may translate to humans was provided by findings of an [11C]raclopride positron emission tomography (PET) study conducted by Pruessner and colleagues [310], who found that persons who reported low maternal care had greater VS DA release in response to stress than individuals who reported high maternal care. Oswald et al. [311] extended this line of research by showing that ELS is also associated with enhanced VS DA responses to amphetamine in healthy young adults. The relationship between ELS and DA response was partially mediated by current levels of perceived stress, which suggested that ELS may not directly influence DA function in some individuals unless accompanied by elevated levels of psychological stress in adulthood.
8.2. Interface between ELS and OUD via Dopamine Function
It has been proposed that the reinforcing effects of opioid agonists are, at least, partially dependent on their actions on mesolimbic DA circuits [312,313,314,315]. Interactions between the DA and endogenous opioid systems are well-established within mesocorticolimbic brain circuits [316,317,318,319,320] and play a role in behavioral responses to opioids and in relief of pain in animals [321,322,323]. It is reasonable to posit that extensive ELS-related dysfunctions in DA circuits could, therefore, influence sensitivity to opioids and vulnerability for OUD. Blum and colleagues [210] hypothesized that addiction results from an underlying reward deficiency state characterized by hypodopaminergia. This condition may be innate or acquired and is clinically manifested as anhedonia, numbing, apathy, or decreased motivation for natural reinforcers [324,325]. According to the hypothesis, opioid/endorphin deficiency increases a person’s vulnerability for OUD by disrupting interactions between midbrain opioid and DA neurotransmitter systems [326]. This has been supported by evidence that ELS alters µ- and k-receptor mRNA levels [62,63,64] and decreases downstream DA signaling [63,65] in a way that may alter the reinforcing and antinociceptive effects of opioids. Dopamine-deficient mice display decreased sensitivity to the analgesic effects of morphine [313] and mice lacking DA D2 receptors fail to self-administer morphine [327], which also provides evidence that individual differences in DA function may contribute to differential opioid sensitivity.
9. Conclusions
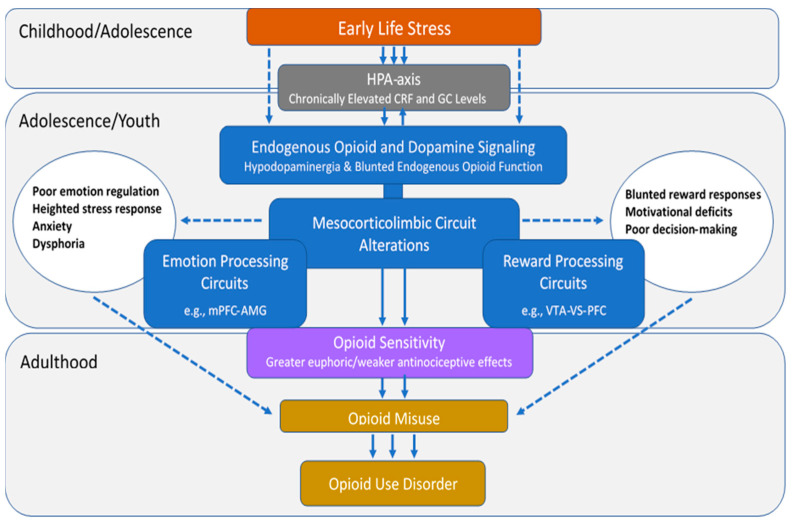
Epidemiological research has shown that ELS is highly prevalent in persons with OUD and is associated with opioid use initiation, injection drug use, overdose, and poor treatment outcome. However, despite evidence that ELS has a profound impact on mesocorticolimbic brain circuits implicated in OUD, the role that these alterations play in vulnerability for and severity of this disorder has yet to be elucidated. Figure 3 outlines a theoretical model based on the extant literature reviewed here, wherein ELS initiates a cascade of neurobiological changes that lead to altered opioid sensitivity and increased risks for OUD. This model is not meant to be exhaustive but to provide a foundation to support focused research in this area. The data suggest that ELS leads to chronically elevated CRF and GC levels in stress-sensitive mesocorticolimbic brain circuits during early exposure, which trigger changes in neurochemistry, activation patterns, and connectivity that persist into adulthood. The consequences include conformational changes in the endogenous opioid system that engender an endorphinergic deficiency and alterations in the DA neurotransmitter system that lead to hypodopaminergia. The presence of a vulnerability pathway involving opioid sensitivity is most strongly supported by preclinical evidence that ELS-induced changes in endogenous opioid function are associated with increased drug-seeking behavior and altered sensitivity to the reinforcing and antinociceptive effects of opioids and that DA-deficient mice exhibit decreased sensitivity to the analgesic effects of morphine, suggesting that DA function may also contribute to the ELS-exposed behavioral phenotype. Derangements in functional activation and connectivity in mesocorticolimbic circuits have been associated with emotion regulation and reward processing deficits in ELS-exposed humans and may reflect the underlying neurochemical imbalances in these regions. Such deficits may predispose an individual to a range of behaviors that independently increase opioid use and misuse. Once opioid use is initiated, ELS-induced neurochemical changes may be manifested as altered opioid sensitivity, which may facilitate the transition from use to misuse and ultimately OUD. Additional research that evaluates the effects of ELS exposure on opioid sensitivity and establishes the degree to which ELS-induced changes in endogenous opioid or DA neurotransmitter systems are present and/or contribute to these processes is warranted. This research could delineate key mechanisms underlying substantial individual variation in opioid risk and could lead to improved prevention strategies and prescribing guidelines for high-risk individuals.
Figure 3.
Putative pathway by which early life stress may alter opioid sensitivity and increase risks for opioid misuse/use disorder. The process begins with chronically elevated levels of corticotropin-releasing factor (CRF) and glucocorticoid (GC) levels that occur during the period of stress exposure, which have a long-term impact on endogenous opioid and dopamine neurotransmitter function, activation patterns, and connectivity in mesocorticolimbic emotion and reward processing regions. The neurobiological changes lead to increased euphoric and decreased antinociceptive responses to opioids and deficits in emotion regulation and reward processing in adulthood, which together may increase risks for recreational use or misuse of prescription opioids. The solid lines on the figure represent the direct pathway involving opioid sensitivity, and the dashed lines represent other mechanisms.
Author Contributions
Conceptualization: L.M.O. and K.E.D.; writing—original draft preparation: L.M.O., K.E.D., D.A.S. and C.L.S.; writing—review and editing: L.M.O., K.E.D. and D.A.S. All authors have read and agreed to the published version of the manuscript.
Funding
K.E.D. received salary support from NIDA R01DA042751, R01DA040644, and UG3DA048734. DAS received funding from NIH/NINDS R01 NS112356-01, NIH/NINDS R61 NS113269-01, and NIH/NCCIH R61 AT010134-01.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
In the past 3 years, K.E.D. has consulted for Grünenthal, Inc. and MindMed; received honoraria for advisory board work for Canopy Corporation and Beckley-Canopy; and served as an unpaid advisor to Peabody Pharmaceuticals. No other authors have conflicts of interest to declare.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Child Welfare Information Gateway . Child Maltreatment 2018: Summary of Key Findings. Children’s Bureau/ACYF/ACF/HHS; Washington, DC, USA: 2020. [Google Scholar]
- 2.Merrick M.T., Ford D.C., Ports K.A., Guinn A.S. Prevalence of Adverse Childhood Experiences from the 2011–2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatr. 2018;172:1038–1044. doi: 10.1001/jamapediatrics.2018.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkelhor D. Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abus. Negl. 2018;85:174–179. doi: 10.1016/j.chiabu.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Burgermeister D. Childhood adversity: A review of measurement instruments. J. Nurs. Meas. 2007;15:163–176. doi: 10.1891/106137407783095766. [DOI] [PubMed] [Google Scholar]
- 5.McLaughlin K.A., DeCross S.N., Jovanovic T., Tottenham N. Mechanisms linking childhood adversity with psychopathology: Learning as an intervention target. Behav. Res. Ther. 2019;118:101–109. doi: 10.1016/j.brat.2019.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell J.A., Walker R.J., Egede L.E. Associations between Adverse Childhood Experiences, High-Risk Behaviors, and Morbidity in Adulthood. Am. J. Prev. Med. 2016;50:344–352. doi: 10.1016/j.amepre.2015.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murphy M.O., Cohn D.M., Loria A.S. Developmental origins of cardiovascular disease: Impact of early life stress in humans and rodents. Neurosci. Biobehav. Rev. 2017;74:453–465. doi: 10.1016/j.neubiorev.2016.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nurius P.S., Green S., Logan-Greene P., Longhi D., Song C. Stress pathways to health inequalities: Embedding ACEs within social and behavioral contexts. Int. Public Health J. 2016;8:241–256. [PMC free article] [PubMed] [Google Scholar]
- 9.Westfall N.C., Nemeroff C.B. The Preeminence of Early Life Trauma as a Risk Factor for Worsened Long-Term Health Outcomes in Women. Curr. Psychiatry Rep. 2015;17:1–18. doi: 10.1007/s11920-015-0625-6. [DOI] [PubMed] [Google Scholar]
- 10.Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am. J. Prev. Med. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 11.D’Andrea W., Ford J., Stolbach B., Spinazzola J., van der Kolk B.A. Understanding Interpersonal Trauma in Children: Why We Need a Developmentally Appropriate Trauma Diagnosis. Am. J. Orthopsychiatry. 2012;82:187–200. doi: 10.1111/j.1939-0025.2012.01154.x. [DOI] [PubMed] [Google Scholar]
- 12.Dubé C.M., Molet J., Singh-Taylor A., Ivy A., Maras P.M., Baram T.Z. Hyper-excitability and epilepsy generated by chronic early-life stress. Neurobiol. Stress. 2015;2:10–19. doi: 10.1016/j.ynstr.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edwards V.J., Holden G.W., Felitti V.J., Anda R.F. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. Am. J. Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- 14.Finkelhor D., Ormrod R.K., Turner H.A. Polyvictimization and trauma in a national longitudinal cohort. Dev. Psychopathol. 2007;19:149–166. doi: 10.1017/S0954579407070083. [DOI] [PubMed] [Google Scholar]
- 15.Huang M.C., Schwandt M.L., Ramchandani V.A., George D.T., Heilig M. Impact of Multiple Types of Childhood Trauma Exposure on Risk of Psychiatric Comorbidity Among Alcoholic Inpatients. Alcohol. Clin. Exp. Res. 2012;36:1099–1107. doi: 10.1111/j.1530-0277.2011.01695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Putnam K.T., Harris W.W., Putnam F.W. Synergistic childhood adversities and complex adult psychopathology. J. Trauma. Stress. 2013;26:435–442. doi: 10.1002/jts.21833. [DOI] [PubMed] [Google Scholar]
- 17.Weber K., Rockstroh B., Borgelt J., Awiszus B., Popov T., Hoffmann K., Schonauer K., Watzl H., Pröpster K. Stress load during childhood affects psychopathology in psychiatric patients. BMC Psychiatry. 2008;8:63. doi: 10.1186/1471-244X-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cicchetti D., Handley E.D. Child maltreatment and the development of substance use and disorder. Neurobiol. Stress. 2019;10 doi: 10.1016/j.ynstr.2018.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilowsky D.J., Keyes K.M., Hasin D.S. Adverse childhood events and lifetime alcohol dependence. Am. J. Public Health. 2009;99:258–263. doi: 10.2105/AJPH.2008.139006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rothman E.F., Edwards E.M., Heeren T., Hingson R.W. Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:e298–e304. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- 21.Derefinko K.J., Salgado García F.I., Talley K.M., Bursac Z., Johnson K.C., Murphy J.G. Adverse childhood experiences predict opioid relapse during treatment among rural adults. Addict. Behav. 2019;96:171–174. doi: 10.1016/j.addbeh.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 22.Garami J., Valikhani A., Parkes D., Haber P., Mahlberg J., Misiak B., Frydecka D., Moustafa A.A. Examining Perceived Stress, Childhood Trauma and Interpersonal Trauma in Individuals With Drug Addiction. Psychol. Rep. 2019;122:433–450. doi: 10.1177/0033294118764918. [DOI] [PubMed] [Google Scholar]
- 23.Groenewald C.B., Law E.F., Fisher E., Beals-Erickson S.E., Palermo T.M. Associations Between Adolescent Chronic Pain and Prescription Opioid Misuse in Adulthood. J. Pain. 2019;20:28–37. doi: 10.1016/j.jpain.2018.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quinn K., Frueh B.C., Scheidell J., Schatz D., Scanlon F., Khan M.R. Internalizing and externalizing factors on the pathway from adverse experiences in childhood to non-medical prescription opioid use in adulthood. Drug Alcohol Depend. 2019;197:212–219. doi: 10.1016/j.drugalcdep.2018.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stein M.D., Conti M.T., Kenney S., Anderson B.J., Flori J.N., Risi M.M., Bailey G.L. Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug Alcohol Depend. 2017;179:325–329. doi: 10.1016/j.drugalcdep.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swedo E.A., Sumner S.A., de Fijter S., Werhan L., Norris K., Beauregard J.L., Montgomery M.P., Rose E.B., Hillis S.D., Massetti G.M. Adolescent Opioid Misuse Attributable to Adverse Childhood Experiences. J. Pediatr. 2020;224:102–109.e3. doi: 10.1016/j.jpeds.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams J.R., Cole V., Girdler S., Cromeens M.G. Exploring stress, cognitive, and affective mechanisms of the relationship between interpersonal trauma and opioid misuse. PLoS ONE. 2020;15:1–19. doi: 10.1371/journal.pone.0233185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Comer S.D., Zacny J.P., Dworkin R.H., Turk D.C., Bigelow G.E., Foltin R.W. Core outcome measures for opioid abuse liability laboratory assessment studies in humans: IMMPACT recommendations. Pain. 2012;153:2315–2324. doi: 10.1016/j.pain.2012.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Food and Drug Administration . Guidance for Industry: Assessment of Abuse Potential of Drugs. FDA Center for Drug Evaluation and Research; Silver Spring, MD, USA: 2010. [Google Scholar]
- 30.Galer B.S., Coyle N., Pasternak G.W., Portenoy R.K. Individual variability in the response to different opioids: Report of five cases. Pain. 1992;49:87–91. doi: 10.1016/0304-3959(92)90192-E. [DOI] [PubMed] [Google Scholar]
- 31.George O., Koob G.F. Individual Differences in Prefrontal Cortex Function and the Transition from Drug Use to Drug Dependence. Neurosci. Biobehav. Rev. 2011;35:232–247. doi: 10.1016/j.neubiorev.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Imperio C.G., McFalls A.J., Colechio E.M., Masser D.R., Vrana K.E., Grigson P.S. Assessment of individual differences in the rat nucleus accumbens transcriptome following taste-heroin extended access. Brain Res. Bull. 2016;123:71–80. doi: 10.1016/j.brainresbull.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jenney C.B., Petko J., Ebersole B., Njatcha C.V.N., Uzamere T.O., Alexander D.N., Grigson P.S., Levenson R. Early avoidance of a heroin-paired taste-cue and subsequent addiction-like behavior in rats. Brain Res. Bull. 2016;123:61–70. doi: 10.1016/j.brainresbull.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lenoir M., Guillem K., Koob G.F., Ahmed S.H. Drug specificity in extended access cocaine and heroin self-administration. Addict. Biol. 2012;17:964–976. doi: 10.1111/j.1369-1600.2011.00385.x. [DOI] [PubMed] [Google Scholar]
- 35.Schwartz L.P., Kim J.S., Silberberg A., Kearns D.N. Heroin and saccharin demand and preference in rats. Drug Alcohol Depend. 2017;178:87–93. doi: 10.1016/j.drugalcdep.2017.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tunstall B.J., Riley A.L., Kearns D.N. Drug specificity in drug versus food choice in male rats. Exp. Clin. Psychopharmacol. 2014;22:364–372. doi: 10.1037/a0037019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koffarnus M.N., Hall A., Winger G. Individual differences in rhesus monkeys’ demand for drugs of abuse. Addict. Biol. 2012;17:887–896. doi: 10.1111/j.1369-1600.2011.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunn K.E., Barrett F.S., Brands B., Marsh D.C., Bigelow G.E. Individual differences in human opioid abuse potential as observed in a human laboratory study. Drug Alcohol Depend. 2019;205:1–11. doi: 10.1016/j.drugalcdep.2019.107688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agrawal A., Jeffries P.W., Srivastava A.B., McCutcheon V.V., Lynskey M.T., Heath A.C., Nelson E.C. Retrospectively assessed subjective effects of initial opioid use differ between opioid misusers with opioid use disorder (OUD) and those who never progressed to OUD: Data from a pilot and a replication sample. J. Neurosci. Res. 2020;2020 doi: 10.1002/jnr.24643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bieber C.M., Fernandez K., Borsook D., Brennan M.J., Butler S.F., Jamison R.N., Osgood E., Sharpe-Potter J., Thomson H.N., Weiss R.D., et al. Retrospective Accounts of Initial Subjective Effects of Opioids in Patients Treated for Pain Who Do or Do Not Develop Opioid Addiction: A Pilot Case-Control Study. Exp. Clin. Psychopharmacol. 2008;16:429–434. doi: 10.1037/1064-1297.16.5.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruehl S., Burns J.W., Passik S.D., Gupta R., Buvanendran A., Chont M., Schuster E., Orlowska D., France C.R. The Contribution of Differential Opioid Responsiveness to Identification of Opioid Risk in Chronic Pain Patients. J. Pain. 2015;16:666–675. doi: 10.1016/j.jpain.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith H.S. Variations in opioid responsiveness. Pain Physician. 2008;11:237–248. doi: 10.36076/ppj.2008/11/237. [DOI] [PubMed] [Google Scholar]
- 43.Morgan D., Picker M.J. Contribution of individual differences to discriminative stimulus, antinociceptive and rate-decreasing effects of opioids: Importance of the drug’s relative intrinsic efficacy at the mu receptor. Behav. Pharmacol. 1996;7:261–284. doi: 10.1097/00008877-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Shoaib M., Spanagel R., Stohr T., Shippenberg T.S. Strain differences in the rewarding and dopamine-releasing effects of morphine in rats. Psychopharmacology. 1995;117:240–247. doi: 10.1007/BF02245193. [DOI] [PubMed] [Google Scholar]
- 45.Rönnbäck L. Morphine preference in individual rats after morphine ingestion. Psychopharmacology. 1990;102:257–262. doi: 10.1007/BF02245930. [DOI] [PubMed] [Google Scholar]
- 46.Jimenez S.M., Healy A.F., Coelho M.A., Brown C.N., Kippin T.E., Szumlinski K.K. Variability in prescription opioid intake and reinforcement amongst 129 substrains. Genes Brain Behav. 2017;16:709–724. doi: 10.1111/gbb.12393. [DOI] [PubMed] [Google Scholar]
- 47.Ikeda K., Ide S., Han W., Hayashida M., Uhl G.R., Sora I. How individual sensitivity to opiates can be predicted by gene analyses. Trends Pharmacol. Sci. 2005;26:311–317. doi: 10.1016/j.tips.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 48.Haerian B.S., Haerian M.S. OPRM1 rs1799971 polymorphism and opioid dependence: Evidence from a meta-analysis. Pharmacogenomics. 2013;14:813–824. doi: 10.2217/pgs.13.57. [DOI] [PubMed] [Google Scholar]
- 49.Ren Z.-Y.Y., Xu X.-Q.Q., Bao Y.-P.P., He J.J., Shi L.L., Deng J.-H.H. The impact of genetic variation on sensitivity to opioid analgesics in patients with postoperative pain: A systematic review and meta-analysis. Pain Physician. 2015;18:131–152. [PubMed] [Google Scholar]
- 50.Zhang Y., Gandhi P.R., Standifer K.M. Increased nociceptive sensitivity and nociceptin/orphanin FQ levels in a rat model of PTSD. Mol. Pain. 2012;8:76. doi: 10.1186/1744-8069-8-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lovallo W.R., Enoch M.A., Acheson A., Cohoon A.J., Sorocco K.H., Hodgkinson C.A., Vincent A.S., Glahn D.C., Goldman D. Cortisol Stress Response in Men and Women Modulated Differentially by the Mu-Opioid Receptor Gene Polymorphism OPRM1 A118G. Neuropsychopharmacology. 2015;40:2546–2554. doi: 10.1038/npp.2015.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shaham Y., Stewart J. Exposure to mild stress enhances the reinforcing efficacy of intravenous heroin self-administration in rats. Psychopharmacology. 1994;114:523–527. doi: 10.1007/BF02249346. [DOI] [PubMed] [Google Scholar]
- 53.Shaham Y. Effect of stress on opioid-seeking behavior: Evidence from studies with rats. Ann. Behav. Med. 1996;18:255–263. doi: 10.1007/BF02895287. [DOI] [PubMed] [Google Scholar]
- 54.Banna K.M., Back S.E., Do P., See R.E. Yohimbine stress potentiates conditioned cue-induced reinstatement of heroin-seeking in rats. Behav. Brain Res. 2010;208:144–148. doi: 10.1016/j.bbr.2009.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaham Y. Immobilization stress-induced oral opioid self-administration and withdrawal in rats: Role of conditioning factors and the effect of stress on ‘relapse’ to opioid drugs. Psychopharmacology. 1993;111:477–485. doi: 10.1007/BF02253539. [DOI] [PubMed] [Google Scholar]
- 56.Shaham Y., Alvares K., Nespor S.M., Grunberg N.E. Effect of stress on oral morphine and fentanyl self-administration in rats. Pharmacol. Biochem. Behav. 1992;41:615–619. doi: 10.1016/0091-3057(92)90382-P. [DOI] [PubMed] [Google Scholar]
- 57.Stafford N.P., Kazan T.N., Donovan C.M., Hart E.E., Drugan R.C., Charntikov S. Individual vulnerability to stress is associated with increased demand for intravenous heroin self-administration in rats. Front. Behav. Neurosci. 2019;13:1–16. doi: 10.3389/fnbeh.2019.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Amini-Khoei H., Amiri S., Shirzadian A., Haj-Mirzaian A., Alijanpour S., Rahimi-Balaei M., Mohammadi-Asi A., Hassanipou M., Mehr S.E., Dehpour A.R. Experiencing neonatal maternal separation increased the seizure threshold in adult male mice: Involvement of the opioid system. Epilepsy Behav. 2015;52:37–41. doi: 10.1016/j.yebeh.2015.08.025. [DOI] [PubMed] [Google Scholar]
- 59.Granholm L., Roman E., Nylander I. Single housing during early adolescence causes time-, area- and peptide-specific alterations in endogenous opioids of rat brain. Br. J. Pharmacol. 2015;172:606–614. doi: 10.1111/bph.12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kalinichev M., White D.A., Holtzman S.G. Individual differences in locomotor reactivity to a novel environment and sensitivity to opioid drugs in the rat. I. Expression of morphine-induced locomotor sensitization. Psychopharmacology. 2004;177:61–67. doi: 10.1007/s00213-004-1990-8. [DOI] [PubMed] [Google Scholar]
- 61.Vey L.T., Rosa H.Z., Barcelos R.C.S., Segat H.J., Metz V.G., Dias V.T., Duarte T., Duarte M.M.M.F., Burger M.E. Stress during the gestational period modifies pups’ emotionality parameters and favors preference for morphine in adolescent rats. Behav. Brain Res. 2016;296:408–417. doi: 10.1016/j.bbr.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 62.Chang L., Kigar S.L., Ho J.H., Cuarenta A., Gunderson H.C., Baldo B.A., Bakshi V.P., Auger A.P. Early life stress alters opioid receptor mRNA levels within the nucleus accumbens in a sex-dependent manner. Brain Res. 2019;1710:102–108. doi: 10.1016/j.brainres.2018.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Karkhanis A.N., Rose J.H., Weiner J.L., Jones S.R. Early-life social isolation stress increases kappa opioid receptor responsiveness and downregulates the dopamine system. Neuropsychopharmacology. 2016;41:2263–2274. doi: 10.1038/npp.2016.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nakamoto K., Taniguchi A., Tokuyama S. Changes in opioid receptors, opioid peptides and morphine antinociception in mice subjected to early life stress. Eur. J. Pharmacol. 2020;881:1–8. doi: 10.1016/j.ejphar.2020.173173. [DOI] [PubMed] [Google Scholar]
- 65.Ploj K., Nylander I. Long-term effects on brain opioid and opioid receptor like-1 receptors after short periods of maternal separation in rats. Neurosci. Lett. 2003;345:195–197. doi: 10.1016/S0304-3940(03)00515-9. [DOI] [PubMed] [Google Scholar]
- 66.Michaels C.C., Holtzman S.G. Early postnatal stress alters place conditioning to both μ- and κ-opioid agonists. J. Pharmacol. Exp. Ther. 2008;325:313–318. doi: 10.1124/jpet.107.129908. [DOI] [PubMed] [Google Scholar]
- 67.Richards G.C., Aronson J.K., Heneghan C., Mahtani K.R., Koshiaris C., Persaud N. Relation between opioid consumption and inclusion of opioids in 137 national essential medicines lists. BMJ Glob. Health. 2020;5:1–8. doi: 10.1136/bmjgh-2020-003563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seya M.J., Gelders S.F.A.M., Achara O.U., Milani B., Scholten W.K. A first comparison between the consumption of and the need for opioid analgesics at country, regional, and global levels. J. Pain Palliat. Care Pharmacother. 2011;25:6–18. doi: 10.3109/15360288.2010.536307. [DOI] [PubMed] [Google Scholar]
- 69.United Nations . World Drug Report 2020 (United Nations Publication, Sales No. E.20.XI.6) United Nations Office on Drugs and Crime; Vienna, Austria: 2020. [Google Scholar]
- 70.Substance Abuse and Mental Health Services Administration (SAMHSA) Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PET20-07-01-001, NSDUH Series H-55); Center for Behavioral Health Statistics and Quality, SAMHSA2020. [(accessed on 14 April 2021)]; Available online: https://www.samhsa.gov/data/
- 71.Knipper E., Banta-Green C.J., Jimenez N. Opioid use disorder and misuse: A review of the epidemiology and medical implications for pediatric anesthesiologists. Paediatr Anaesth. 2017;27:1070–1076. doi: 10.1111/pan.13225. [DOI] [PubMed] [Google Scholar]
- 72.Muhuri P.K., Gfroerer J.C., Davies M. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. CBHSQ Data Review; Center for Behavioral Health Statistics and Quality, SAMHSA 2013. [(accessed on 14 April 2021)]; Available online: http://www.samhsa.gov/data/
- 73.Degenhardt L., Grebely J., Stone J., Hickman M., Vickerman P., Marshall B.D.L., Bruneau J., Altice F.L., Henderson G., Movaghar A.R., et al. Global patterns of opioid use and dependence: Harms to populations, interventions, and future action. Lancet. 2019;394:1560–1579. doi: 10.1016/S0140-6736(19)32229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Florence C.S., Zhou C., Luo F., Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med. Care. 2016;54:901–906. doi: 10.1097/MLR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Roth G.A., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., Abdela J., Abdelalim A., et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wilson N., Kariisa M., Seth P., Smith H., Davis N.L. Drug and Opioid-Involved Overdose Deaths—United States, 2017–2018. Morbidity and Mortality Weekly Report. US Department of Health and Human Services/Centers for Disease Control and Prevention. [(accessed on 14 April 2021)];2020 Volume 69:290–297. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6911a4.htm. [Google Scholar]
- 77.Berrettini W. A brief review of the genetics and pharmacogenetics of opioid use disorders. Dialogues Clin. Neurosci. 2017;19:229–236. doi: 10.31887/DCNS.2017.19.3/wberrettini. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kendler K.S., Jacobson K.C., Prescott C.A., Neale M.C. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. Am. J. Psychiatry. 2003;160:687–695. doi: 10.1176/appi.ajp.160.4.687. [DOI] [PubMed] [Google Scholar]
- 79.Tsuang M.T., Lyons M.J., Meyer J.M., Doyle T., Eisen S.A., Goldberg J., True W., Lin N., Toomey R., Eaves L. Co-occurrence of abuse of different drugs in men: The role of drug- specific and shared vulnerabilities. Arch. Gen. Psychiatry. 1998;55:967–972. doi: 10.1001/archpsyc.55.11.967. [DOI] [PubMed] [Google Scholar]
- 80.Barnett T.E., Thompson E.L., Litt D.M., Lewis M.A. Correlates of Nonmedical Prescription Opioid Use Among U.S. Adolescents. Am. J. Prev. Med. 2019;57:e175–e179. doi: 10.1016/j.amepre.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 81.Cheatle M.D., Compton P.A., Dhingra L., Wasser T.E., O’Brien C.P. Development of the Revised Opioid Risk Tool to Predict Opioid Use Disorder in Patients with Chronic Nonmalignant Pain. J. Pain. 2019;20:842–851. doi: 10.1016/j.jpain.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chinneck A., Thompson K., Mahu I.T., Davis-MacNevin P., Dobson K., Stewart S.H. Personality and prescription drug use/misuse among first year undergraduates. Addict. Behav. 2018;87:122–130. doi: 10.1016/j.addbeh.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 83.Mahu I.T., Conrod P.J., Barrett S.P., Sako A., Swansburg J., Lawrence M., Laroque F., Morin J.F., Chinneck A., Nogueira-Arjona R., et al. Specificity of personality relationships to particular forms of concurrent substance use among methadone maintenance therapy clients. Addict. Behav. 2019;98:106056. doi: 10.1016/j.addbeh.2019.106056. [DOI] [PubMed] [Google Scholar]
- 84.Roos C.R., Kiluk B.D., McHugh R.K., Carroll K.M. Evaluating a longitudinal mediation model of perceived stress, depressive symptoms, and substance use treatment outcomes. Psychol. Addict. Behav. 2020;34:660–668. doi: 10.1037/adb0000581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lanzillotta-Rangeley J., Clark A., Christianson A., Kalarchian M.A. Association of prescription opioid exposure and patient factors with prolonged postoperative opioid use in opioid-naïve patients. AANA J. 2020;88:18–26. [PubMed] [Google Scholar]
- 86.Riva J.J., Noor S.T., Wang L., Ashoorion V., Foroutan F., Sadeghirad B., Couban R., Busse J.W. Predictors of Prolonged Opioid Use after Initial Prescription for Acute Musculoskeletal Injuries in Adults: A Systematic Review and Meta-analysis of Observational Studies. Ann. Intern. Med. 2020;173:721–729. doi: 10.7326/M19-3600. [DOI] [PubMed] [Google Scholar]
- 87.Gilam G., Sturgeon J.A., You D.S., Wasan A.D., Darnall B.D., Mackey S.C. Negative Affect-Related Factors Have the Strongest Association with Prescription Opioid Misuse in a Cross-Sectional Cohort of Patients with Chronic Pain. Pain Med. 2020;21:e127–e138. doi: 10.1093/pm/pnz249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ramírez-Maestre C., Reyes-Pérez Á., Esteve R., López-Martínez A.E., Bernardes S., Jensen M.P. Opioid pain medication prescription for chronic pain in primary care centers: The roles of pain acceptance, pain intensity, depressive symptoms, pain catastrophizing, sex, and age. Int. J. Environ. Res. Public Health. 2020;17:6428. doi: 10.3390/ijerph17176428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Smit T., Rogers A.H., Garey L., Allan N.P., Viana A.G., Zvolensky M.J. Anxiety sensitivity and pain intensity independently predict opioid misuse and dependence in chronic pain patients. Psychiatry Res. 2020;294:1–8. doi: 10.1016/j.psychres.2020.113523. [DOI] [PubMed] [Google Scholar]
- 90.McHugh R.K., Kneeland E.T. Affective vulnerability in substance use disorders. Curr. Opin. Psychol. 2019;30:54–58. doi: 10.1016/j.copsyc.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Finan P.H., Carroll C.P., Moscou-Jackson G., Martel M.O., Campbell C.M., Pressman A., Smyth J.M., Tremblay J.-M., Lanzkron S.M., Haythornthwaite J.A. Daily Opioid Use Fluctuates as a Function of Pain, Catastrophizing, and Affect in Patients With Sickle Cell Disease: An Electronic Daily Diary Analysis. J. Pain. 2018;19:46–56. doi: 10.1016/j.jpain.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lutz J., Gross R.T., Vargovich A.M. Difficulties in emotion regulation and chronic pain-related disability and opioid misuse. Addict. Behav. 2018;87:200–205. doi: 10.1016/j.addbeh.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 93.Anda R.F., Croft J.B., Felitti V.J., Nordenberg D., Giles W.H., Williamson D.F., Giovino G.A. Adverse childhood experiences and smoking during adolescence and adulthood. J. Am. Med. Assoc. 1999;282:1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 94.Dube S.R., Miller J.W., Brown D.W., Giles W.H., Felitti V.J., Dong M., Anda R.F. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J. Adolesc. Health. 2006;38:444.e1–444.e10. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 95.Duncan A.E., Sartor C.E., Scherrer J.F., Grant J.D., Heath A.C., Nelson E.C., Jacob T., Bucholz K.K. The association between cannabis abuse and dependence and childhood physical and sexual abuse: Evidence from an offspring of twins design. Addiction. 2008;103:990–997. doi: 10.1111/j.1360-0443.2008.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Enoch M.-A.A. The role of early life stress as a predictor for alcohol and drug depemdence. Psychopharmacology. 2011;214:17–31. doi: 10.1007/s00213-010-1916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Teixeira C.A.B., Lasiuk G., Barton S., de Fernandes M.N.F., da Gherardi-Donato E.C.S. An exploration of addiction in adults experiencing early-life stress: A metasynthesis. Rev. Lat. Am. Enfermagem. 2017;25 doi: 10.1590/1518-8345.2026.2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Conroy E., Degenhardt L., Mattick R.P., Nelson E.C. Child maltreatment as a risk factor for opioid dependence: Comparison of family characteristics and type and severity of child maltreatment with a matched control group. Child Abus. Negl. 2009;33:343–352. doi: 10.1016/j.chiabu.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Evans E.A., Goff S.L., Upchurch D.M., Grella C.E. Childhood adversity and mental health comorbidity in men and women with opioid use disorders. Addict. Behav. 2020;102:106149. doi: 10.1016/j.addbeh.2019.106149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Santo T., Campbell G., Gisev N., Tran L.T., Colledge S., Di Tanna G.L., Degenhardt L. Prevalence of childhood maltreatment among people with opioid use disorder: A systematic review and meta-analysis. Drug Alcohol Depend. 2021;219 doi: 10.1016/j.drugalcdep.2020.108459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Winstanley E.L., Mahoney J.J., Lander L.R., Berry J.H., Marshalek P., Zheng W., Haut M.W. Something to despair: Gender differences in adverse childhood experiences among rural patients. J. Subst. Abuse Treat. 2020;116:108056. doi: 10.1016/j.jsat.2020.108056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Larance B., Gisev N., Cama E., Nelson E.C., Darke S., Larney S., Degenhardt L. Predictors of transitions across stages of heroin use and dependence prior to treatment-seeking among people in treatment for opioid dependence. Drug Alcohol Depend. 2018;191:145–151. doi: 10.1016/j.drugalcdep.2018.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mohammadzadeh A., Ganji Z., Khosravani V., Mohammadpanah Ardakan A., Amirinezhad A. Direct and indirect associations between perception of childhood trauma and suicidal ideation through emotion dysregulation in males who use heroin. Addict. Behav. 2019;98:1–10. doi: 10.1016/j.addbeh.2019.05.035. [DOI] [PubMed] [Google Scholar]
- 104.Quinn K., Boone L., Scheidell J.D., Mateu-Gelabert P., McGorray S.P., Beharie N., Cottler L.B., Khan M.R. The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug Alcohol Depend. 2016;169:190–198. doi: 10.1016/j.drugalcdep.2016.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Merrick M.T., Ford D.C., Haegerich T.M., Simon T. Adverse Childhood Experiences Increase Risk for Prescription Opioid Misuse. J. Prim. Prev. 2020;41:139–152. doi: 10.1007/s10935-020-00578-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tang S., Ports K.A., Zhang K., Lin H.C. Adverse childhood experiences, internalizing/externalizing symptoms, and associated prescription opioid misuse: A mediation analysis. Prev. Med. 2020;134:106034. doi: 10.1016/j.ypmed.2020.106034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lloyd D.A., Turner R.J. Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug Alcohol Depend. 2008;93:217–226. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Agorastos A., Pervanidou P., Chrousos G.P., Baker D.G. Developmental trajectories of early life stress and trauma: A narrative review on neurobiological aspects beyond stress system dysregulation. Front. Psychiatry. 2019;10:1–25. doi: 10.3389/fpsyt.2019.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Daskalakis N.P., Bagot R.C., Parker K.J., Vinkers C.H., de Kloet E.R. The three-hit concept of vulnerability and resilience: Toward understanding adaptation to early-life adversity outcome. Psychoneuroendocrinology. 2013;38:1858–1873. doi: 10.1016/j.psyneuen.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Heim C., Shugart M., Craighead W.E., Nemeroff C.B. Neurobiological and psychiatric consequences of child abuse and neglect. Dev. Psychobiol. 2010;52:671–690. doi: 10.1002/dev.20494. [DOI] [PubMed] [Google Scholar]
- 111.Kern S., Laurent H.K. Childhood abuse predicts affective symptoms via HPA reactivity during mother-infant stress. Psychoneuroendocrinology. 2019;107:19–25. doi: 10.1016/j.psyneuen.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 112.Khosravani V., Samimi Ardestani S.M., Sharifi Bastan F., Mohammadzadeh A., Amirinezhad A. Childhood maltreatment, cognitive emotion regulation strategies, and alcohol craving and dependence in alcohol-dependent males: Direct and indirect pathways. Child Abus. Negl. 2019;98:104197. doi: 10.1016/j.chiabu.2019.104197. [DOI] [PubMed] [Google Scholar]
- 113.Kuhlman K.R., Chiang J.J., Horn S., Bower J.E. Developmental psychoneuroendocrine and psychoneuroimmune pathways from childhood adversity to disease. Neurosci. Biobehav. Rev. 2017;80:166–184. doi: 10.1016/j.neubiorev.2017.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lovallo W.R., Cohoon A.J., Sorocco K.H., Vincent A.S., Acheson A., Hodgkinson C.A., Goldman D. Early-Life Adversity and Blunted Stress Reactivity as Predictors of Alcohol and Drug use in Persons With COMT (rs4680) Val158Met Genotypes. Alcohol. Clin. Exp. Res. 2019;43:1519–1527. doi: 10.1111/acer.14079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.MacMillan H.L., Georgiades K., Duku E.K., Shea A., Steiner M., Niec A., Tanaka M., Gensey S., Spree S., Vella E., et al. Cortisol Response to Stress in Female Youths Exposed to Childhood Maltreatment: Results of the Youth Mood Project. Biol. Psychiatry. 2009;66:62–68. doi: 10.1016/j.biopsych.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Strüber N., Strüber D., Roth G. Impact of early adversity on glucocorticoid regulation and later mental disorders. Neurosci. Biobehav. Rev. 2014;38:17–37. doi: 10.1016/j.neubiorev.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 117.Tottenham N., Sheridan M.A. A review of adversity, the amygdala and the hippocampus: A consideration of developmental timing. Front. Hum. Neurosci. 2010;3:68. doi: 10.3389/neuro.09.068.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang H., Yao Z., Lin L., Sun X., Shi X., Zhang L. Early life stress predicts cortisol response to psychosocial stress in healthy young adults. PsyCh J. 2019;8:353–362. doi: 10.1002/pchj.278. [DOI] [PubMed] [Google Scholar]
- 119.Gorka S.M. Interpersonal trauma exposure and startle reactivity to uncertain threat in individuals with alcohol use disorder. Drug Alcohol Depend. 2020;206:1–18. doi: 10.1016/j.drugalcdep.2019.107727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kreek M.J., Koob G.F. Drug dependence: Stress and dysregulation of brain reward pathways. Drug Alcohol Depend. 1998;51:23–47. doi: 10.1016/S0376-8716(98)00064-7. [DOI] [PubMed] [Google Scholar]
- 121.Mackesy-Amiti M.E., Donenberg G. Negative affect and emotion dysregulation among people who inject drugs: An ecological momentary assessment study. Psychol. Addict. Behav. 2020;34:650–659. doi: 10.1037/adb0000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gerra G., Somaini L., Manfredini M., Raggi M.A., Saracino M.A., Amore M., Leonardi C., Cortese E., Donnini C. Dysregulated responses to emotions among abstinent heroin users: Correlation with childhood neglect and addiction severity. Prog. Neuro Psychopharmacol. Biol. Psychiatry. 2014;48:220–228. doi: 10.1016/j.pnpbp.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 123.Ghorbani F., Khosravani V., Mohammadzadeh A., Shadnia S. The role of emotion dysregulation in the relation of childhood trauma to heroin craving in individuals with heroin dependence. Drug Alcohol Depend. 2019;195:132–139. doi: 10.1016/j.drugalcdep.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 124.Darke S. Pathways to heroin dependence: Time to re-appraise self-medication. Addiction. 2013;108:659–667. doi: 10.1111/j.1360-0443.2012.04001.x. [DOI] [PubMed] [Google Scholar]
- 125.Schepis T.S., Klare D.L., Ford J.A., McCabe S.E. Prescription Drug Misuse: Taking a Lifespan Perspective. Subst. Abus. Res. Treat. 2020;14:1–28. doi: 10.1177/1178221820909352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Calogero A.E. Neurotransmitter Regulation of the Hypothalamic Corticotropin-Releasing Hormone Neuron. Ann. N. Y. Acad. Sci. 1995;771:31–40. doi: 10.1111/j.1749-6632.1995.tb44668.x. [DOI] [PubMed] [Google Scholar]
- 127.Oswald L.M., Wand G.S.S. Opioids and alcoholism. Physiol. Behav. 2004;81:339–358. doi: 10.1016/j.physbeh.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 128.McHugh R.K., Nguyen M.D., Fitzmaurice G.M., Dillon D.G. Behavioral strategies to reduce stress reactivity in opioid use disorder: Study design. Health Psychol. 2020;39:806–814. doi: 10.1037/hea0000862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Haber S.N., Knutson B. The reward circuit: Linking primate anatomy and human imaging. Neuropsychopharmacology. 2010;35:4–26. doi: 10.1038/npp.2009.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Arnett M.G., Pan M.S., Doak W., Cyr P.E.P., Muglia L.M., Muglia L.J. The role of glucocorticoid receptor-dependent activity in the amygdala central nucleus and reversibility of early-life stress programmed behavior. Transl. Psychiatry. 2015;5:e542. doi: 10.1038/tp.2015.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bremner J.D. Long-term effects of childhood abuse on brain and neurobiology. Child Adolesc. Psychiatr. Clin. N. Am. 2003;12:271–292. doi: 10.1016/S1056-4993(02)00098-6. [DOI] [PubMed] [Google Scholar]
- 132.McCrory E., De Brito S.A., Viding E. The link between child abuse and psychopathology: A review of neurobiological and genetic research. J. R. Soc. Med. 2012;105:151–156. doi: 10.1258/jrsm.2011.110222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tottenham N., Hare T.A., Millner A., Gilhooly T., Zevin J.D., Casey B.J. Elevated amygdala response to faces following early deprivation. Dev. Sci. 2011;14:190–204. doi: 10.1111/j.1467-7687.2010.00971.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Liu W.Z., Zhang W.H., Zheng Z.H., Zou J.X., Liu X.X., Huang S.H., You W.J., He Y., Zhang J.Y., Wand X.D., et al. Identification of a prefrontal cortex-to-amygdala pathway for chronic stress-induced anxiety. Nat. Commun. 2020;11:1–15. doi: 10.1038/s41467-020-15920-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Uliana D.L., Gomes F.V., Grace A.A. Stress impacts corticoamygdalar connectivity in an age-dependent manner. Neuropsychopharmacology. 2021;46:731–740. doi: 10.1038/s41386-020-00886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.VanTieghem M.R., Tottenham N. Neurobiological programming of early life stress: Functional development of amygdala-prefrontal circuitry and vulnerability for stress-related psychopathology. Curr. Top. Behav. Neurosci. 2018;38:117–136. doi: 10.1007/7854_2016_42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Aust S., Stasch J., Jentschke S., Alkan Härtwig E., Koelsch S., Heuser I., Bajbouj M. Differential effects of early life stress on hippocampus and amygdala volume as a function of emotional abilities. Hippocampus. 2014;24:1094–1101. doi: 10.1002/hipo.22293. [DOI] [PubMed] [Google Scholar]
- 138.Pechtel P., Lyons-Ruth K., Anderson C.M., Teicher M.H. Sensitive periods of amygdala development: The role of maltreatment in preadolescence. Neuroimage. 2014;97:236–244. doi: 10.1016/j.neuroimage.2014.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Dannlowski U., Kugel H., Huber F., Stuhrmann A., Redlich R., Grotegerd D., Dohm K., Sehlmeyer C., Konrad C., Baune B.T., et al. Childhood maltreatment is associated with an automatic negative emotion processing bias in the amygdala. Hum. Brain Mapp. 2013;34:2899–2909. doi: 10.1002/hbm.22112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gee D.G., Gabard-Durnam L.J., Flannery J., Goff B., Humphreys K.L., Telzer E.H., Hare T.A., Bockheimer S.Y., Tottenham N. Early developmental emergence of human amygdala-prefrontal connectivity after maternal deprivation. Proc. Natl. Acad. Sci. USA. 2013;110:15638–15643. doi: 10.1073/pnas.1307893110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Suzuki H., Luby J.L., Botteron K.N., Dietrich R., McAvoy M.P., Barch D.M. Early life stress and trauma and enhanced limbic activation to emotionally valenced faces in depressed and healthy children. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53:800–813.e10. doi: 10.1016/j.jaac.2014.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.van Harmelen A.L., van Tol M.J., Demenescu L.R., van der Wee N.J.A., Veltman D.J., Aleman A., van Buchem M.A., Spinhoven P., Penninx B.W.J.H., Elzinga B.M. Enhanced amygdala reactivity to emotional faces in adults reporting childhood emotional maltreatment. Soc. Cogn. Affect. Neurosci. 2013;8:362–369. doi: 10.1093/scan/nss007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yamamoto T., Toki S., Siegle G.J., Takamura M., Takaishi Y., Yoshimura S., Okada G., Matsumoto T., Nakao T., Muranaka H., et al. Increased amygdala reactivity following early life stress: A potential resilience enhancer role. BMC Psychiatry. 2017;17:1–11. doi: 10.1186/s12888-017-1201-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Oshri A., Gray J.C., Owens M.M., Liu S., Duprey E.B., Sweet L.H., MacKillopm J. Adverse Childhood Experiences and Amygdalar Reduction: High-Resolution Segmentation Reveals Associations With Subnuclei and Psychiatric Outcomes. Child Maltreat. 2019;24:400–410. doi: 10.1177/1077559519839491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gerin M.I., Viding E., Pingault J.B., Puetz V.B., Knodt A.R., Radtke S.R., Brigidi B., Swartz J.R., Hariri A.R., McCrory E.J. Heightened amygdala reactivity and increased stress generation predict internalizing symptoms in adults following childhood maltreatment. J. Child Psychol. Psychiatry Allied Discip. 2019;60:752–761. doi: 10.1111/jcpp.13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Elsayed N.M., Kim M.J., Fields K.M., Olvera R.L., Hariri A.R., Williamson D.E. Trajectories of Alcohol Initiation and Use During Adolescence: The Role of Stress and Amygdala Reactivity. J. Am. Acad. Child Adolesc. Psychiatry. 2018;57:550–560. doi: 10.1016/j.jaac.2018.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Nikolova Y.S., Knodt A.R., Radtke S.R., Hariri A.R. Divergent responses of the amygdala and ventral striatum predict stress-related problem drinking in young adults: Possible differential markers of affective and impulsive pathways of risk for alcohol use disorder. Mol. Psychiatry. 2016;21:348–356. doi: 10.1038/mp.2015.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hanson J.L., Chung M.K., Avants B.B., Rudolph K.D., Shirtcliff E.A., Gee J.C., Davidson R.J., Poliak S.D. Structural variations in prefrontal cortex mediate the relationship between early childhood stress and spatial working memory. J. Neurosci. 2012;32:7917–7925. doi: 10.1523/JNEUROSCI.0307-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Van Harmelen A.L., Van Tol M.J., Van Der Wee N.J.A., Veltman D.J., Aleman A., Spinhoven P., van Buchem M.A., Zitman F.G., Penninx B.W.J.H., Elzinga B.M. Reduced medial prefrontal cortex volume in adults reporting childhood emotional maltreatment. Biol. Psychiatry. 2010;68:832–838. doi: 10.1016/j.biopsych.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 150.Nakao T., Matsumoto T., Morita M., Shimizu D., Yoshimura S., Northoff G., Morinobu S., Okamoto Y., Yamawaki S. The Degree of Early Life Stress Predicts Decreased Medial Prefrontal Activations and the Shift from Internally to Externally Guided Decision Making: An Exploratory NIRS Study during Resting State and Self-Oriented Task. Front. Hum. Neurosci. 2013;7:339. doi: 10.3389/fnhum.2013.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Van Harmelen A.L., Van Tol M.J., Dalgleish T., Van der Wee N.J.A., Veltman D.J., Aleman A., Spinhoven P., Penninx B.W.J.H., Elzinga B.M. Hypoactive medial prefrontal cortex functioning in adults reporting childhood emotional maltreatment. Soc. Cogn. Affect. Neurosci. 2014;9:2026–2033. doi: 10.1093/scan/nsu008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wang L., Paul N., Stanton S.J., Greeson J.M., Smoski M.J. Loss of sustained activity in the ventromedial prefrontal cortex in response to repeated stress in individuals with early-life emotional abuse: Implications for depression vulnerability. Front. Psychol. 2013;4:1–9. doi: 10.3389/fpsyg.2013.00320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Giustino T.F., Maren S. The role of the medial prefrontal cortex in the conditioning and extinction of fear. Front. Behav. Neurosci. 2015;9:298. doi: 10.3389/fnbeh.2015.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Peters J., Kalivas P.W., Quirk G.J. Extinction circuits for fear and addiction overlap in prefrontal cortex. Learn Mem. 2009;16:279–288. doi: 10.1101/lm.1041309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Herringa R.J., Birn R.M., Ruttle P.L., Burghy C.A., Stodola D.E., Davidson R.J., Essex M.J. Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proc. Natl. Acad. Sci. USA. 2013;110:19119–19124. doi: 10.1073/pnas.1310766110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Pagliaccio D., Luby J.L., Bogdan R., Agrawal A., Gaffrey M.S., Belden A.C., Botteron K.N., Harms M.P., Barch D.M. Amygdala functional connectivity, HPA axis genetic variation, and life stress in children and relations to anxiety and emotion regulation. J. Abnorm. Psychol. 2015;124:817–833. doi: 10.1037/abn0000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Thomason M.E., Marusak H.A., Tocco M.A., Vila A.M., McGarragle O., Rosenberg D.R. Altered amygdala connectivity in urban youth exposed to trauma. Soc. Cogn. Affect. Neurosci. 2014;10:1460–1468. doi: 10.1093/scan/nsv030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Burghy C.A., Stodola D.E., Ruttle P.L., Molloy E.K., Armstrong J.M., Oler J.A., Fox M.E., Hayes A.S., Kalin N.H., Essex M.J., et al. Developmental pathways to amygdala-prefrontal function and internalizing symptoms in adolescence. Nat. Neurosci. 2012;15:1736–1741. doi: 10.1038/nn.3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Morin E.L., Howell B.R., Feczko E., Earl E., Pincus M., Reding K., Kovacs-Balint Z.A., Meyer J.S., Styner M., Fair D., et al. Developmental outcomes of early adverse care on amygdala functional connectivity in nonhuman primates. Dev. Psychopathol. 2020;32:1579–1596. doi: 10.1017/S0954579420001133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Fan Y., Herrera-Melendez A.L., Pestke K., Feeser M., Aust S., Otte C., Pruessner J.C., Böker H., Bajbouj M., Grimm S. Early life stress modulates amygdala-prefrontal functional connectivity: Implications for oxytocin effects. Hum. Brain Mapp. 2014;35:5328–5339. doi: 10.1002/hbm.22553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kraynak T.E., Marsland A.L., Hanson J.L., Gianaros P.J. Retrospectively reported childhood physical abuse, systemic inflammation, and resting corticolimbic connectivity in midlife adults. Brain Behav. Immun. 2019;82:203–213. doi: 10.1016/j.bbi.2019.08.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Jedd K., Hunt R.H., Cicchetti D., Hunt E., Cowell R.A., Rogosch F.A., Toth S.L., Thomas K.M. Long-term consequences of childhood maltreatment: Altered amygdala functional connectivity. Dev. Psychopathol. 2015;27:1577–1589. doi: 10.1017/S0954579415000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kaiser R.H., Clegg R., Goer F., Pechtel P., Beltzer M., Vitaliano G., Olson D.P., Teicher M.H., Pizzagalli D.A. Childhood stress, grown-up brain networks: Corticolimbic correlates of threat-related early life stress and adult stress response. Psychol. Med. 2018;48:1157–1166. doi: 10.1017/S0033291717002628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Babenko O., Kovalchuk I., Metz G.A.S. Stress-induced perinatal and transgenerational epigenetic programming of brain development and mental health. Neurosci. Biobehav. Rev. 2015;48:70–91. doi: 10.1016/j.neubiorev.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 165.Chocyk A., Majcher-Maoelanka I., Dudys D., Przyborowska A., Wêdzony K. Impact of early-life stress on the medial prefrontal cortex functions-a search for the pathomechanisms of anxiety and mood disorders. Pharmacol. Rep. 2013;65:1462–1470. doi: 10.1016/S1734-1140(13)71506-8. [DOI] [PubMed] [Google Scholar]
- 166.Raymond C., Marin M.F., Majeur D., Lupien S. Early child adversity and psychopathology in adulthood: HPA axis and cognitive dysregulations as potential mechanisms. Prog. Neuro Psychopharmacol. Biol. Psychiatry. 2018;85:152–160. doi: 10.1016/j.pnpbp.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 167.Lux V. Epigenetic Programming Effects of Early Life Stress: A Dual-Activation Hypothesis. Curr. Genom. 2018;19:638–652. doi: 10.2174/1389202919666180307151358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Silveira S., Shah R., Nooner K.B., Nagel B.J., Tapert S.F., de Bellis M.D., Mishra J. Impact of Childhood Trauma on Executive Function in Adolescence—Mediating Functional Brain Networks and Prediction of High-Risk Drinking. Biol. Psychiatry Cogn. Neurosci. Neuroimaging. 2020;5:499–509. doi: 10.1016/j.bpsc.2020.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Thomason M.E., Marusak H.A. Toward understanding the impact of trauma on the early developing human brain. Neuroscience. 2017;342:55–67. doi: 10.1016/j.neuroscience.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.De Bellis M.D., Zisk A. The Biological Effects of Childhood Trauma. Child Adolesc. Psychiatr. Clin. N. Am. 2014;23:185–222. doi: 10.1016/j.chc.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Pervanidou P., Chrousos G.P. Metabolic consequences of stress during childhood and adolescence. Metabolism. 2012;61:611–619. doi: 10.1016/j.metabol.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 172.Zouikr I., Karshikoff B. Lifetime modulation of the pain system via neuroimmune and neuroendocrine interactions. Front. Immunol. 2017;8:276. doi: 10.3389/fimmu.2017.00276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kundakovic M., Champagne F.A. Early-life experience, Epigenetics, and the developing brain. Neuropsychopharmacology. 2015;40:141–153. doi: 10.1038/npp.2014.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Suderman M., Borghol N., Pappas J.J., Pinto Pereira S.M., Pembrey M., Hertzman C., Power C., Szyf M. Childhood abuse is associated with methylation of multiple loci in adult DNA. BMC Med. Genom. 2014;7:1–12. doi: 10.1186/1755-8794-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Meaney M.J., Diorio J., Francis D., Widdowson J., LaPlante P., Caldji C., Sharma S., Secki J.R., Plotsky P.M. Early Environmental Regulation of Forebrain Glucocorticoid Receptor Gene Expression: Implications for Adrenocortical Responses to Stress. Dev. Neurosci. 1996;18:49–60. doi: 10.1159/000111395. [DOI] [PubMed] [Google Scholar]
- 176.Myers B., McKlveen J.M., Herman J.P. Glucocorticoid actions on synapses, circuits, and behavior: Implications for the energetics of stress. Front. Neuroendocrinol. 2014;35:180–196. doi: 10.1016/j.yfrne.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Arabadzisz D., Diaz-Heijtz R., Knuesel I., Weber E., Pilloud S., Dettling A.C., Feldon J., Law A.J., Harrison P.J., Pryce C.R. Primate Early Life Stress Leads to Long-Term Mild Hippocampal Decreases in Corticosteroid Receptor Expression. Biol. Psychiatry. 2010;67:1106–1109. doi: 10.1016/j.biopsych.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 178.Prusator D.K., Greenwood-Van Meerveld B. Amygdala-mediated mechanisms regulate visceral hypersensitivity in adult females following early life stress: Importance of the glucocorticoid receptor and corticotropin-releasing factor. Pain. 2017;158:296–305. doi: 10.1097/j.pain.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 179.Szyf M., Bick J. DNA Methylation: A Mechanism for Embedding Early Life Experiences in the Genome. Child. Dev. 2013;84:49–57. doi: 10.1111/j.1467-8624.2012.01793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.van der Doelen R.H.A., Calabrese F., Guidotti G., Geenen B., Riva M.A., Kozicz T., Homber J.R. Early life stress and serotonin transporter gene variation interact to affect the transcription of the glucocorticoid and mineralocorticoid receptors, and the co-chaperone FKBP5, in the adult rat brain. Front. Behav. Neurosci. 2014;8:1–11. doi: 10.3389/fnbeh.2014.00355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.McGowan P.O., Sasaki A., D’Alessio A.C., Dymov S., Labonté B., Szyf M., Turecki G., Meaney M.J. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat. Neurosci. 2009;12:342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Palma-Gudiel H., Córdova-Palomera A., Leza J.C., Fañanás L. Glucocorticoid receptor gene (NR3C1) methylation processes as mediators of early adversity in stress-related disorders causality: A critical review. Neurosci. Biobehav. Rev. 2015;55:520–535. doi: 10.1016/j.neubiorev.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 183.Alexander N., Kirschbaum C., Wankerl M., Stauch B.J., Stalder T., Steudte-Schmiedgen S., Muehlhan M., Miller R. Glucocorticoid receptor gene methylation moderates the association of childhood trauma and cortisol stress reactivity. Psychoneuroendocrinology. 2018;90:68–75. doi: 10.1016/j.psyneuen.2018.01.020. [DOI] [PubMed] [Google Scholar]
- 184.Zilverstand A., Huang A.S., Alia-Klein N., Goldstein R.Z. Neuroimaging Impaired Response Inhibition and Salience Attribution in Human Drug Addiction: A Systematic Review. Neuron. 2018;98:886–903. doi: 10.1016/j.neuron.2018.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Li Q., Wang Y., Zhang Y., Li W., Yang W., Zhu J., Wu N., Chang H., Zheng Y., Qin W., et al. Craving correlates with mesolimbic responses to heroin-related cues in short-term abstinence from heroin: An event-related fMRI study. Brain Res. 2012;1469:63–72. doi: 10.1016/j.brainres.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 186.Langleben D.D., Ruparel K., Elman I., Loughead J.W., Busch E.L., Cornish J., Lynch K.G., Nuwayser E.S., Childress A.R., O’Brien C.P. Extended-release naltrexone modulates brain response to drug cues in abstinent heroin-dependent patients. Addict. Biol. 2014;19:262–271. doi: 10.1111/j.1369-1600.2012.00462.x. [DOI] [PubMed] [Google Scholar]
- 187.Mei W., Zhang J.X., Xiao Z. Acute effects of sublingual buprenorphine on brain responses to heroin-related cues in early-abstinent heroin addicts: An uncontrolled trial. Neuroscience. 2010;170:808–815. doi: 10.1016/j.neuroscience.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 188.Murphy A., Lubman D.I., McKie S., Bijral P.S., Peters L.A., Faiz Q., Holmes S.E., Anderson I.M., Deakin B., Elliott R. Time-dependent neuronal changes associated with craving in opioid dependence: An fMRI study. Addict. Biol. 2018;23:1168–1178. doi: 10.1111/adb.12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Schmidt A., Borgwardt S., Gerber H., Wiesbeck G.A., Schmid O., Riecher-Rössler A., Smieskova R., Lang U.E., Walter M. Acute effects of heroin on negative emotional processing: Relation of amygdala activity and stress-related responses. Biol. Psychiatry. 2014;76:289–296. doi: 10.1016/j.biopsych.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 190.Fu L.P., Bi G.H., Zou Z.T., Wang Y., Ye E.M., Ma L., Fan M., Yang Z. Impaired response inhibition function in abstinent heroin dependents: An fMRI study. Neurosci. Lett. 2008;438:322–326. doi: 10.1016/j.neulet.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 191.Liu J., Qin W., Yuan K., Li J., Wang W., Li Q., Wang Y., Sun J., von Deneen K.M., Liu Y., et al. Interaction between dysfunctional connectivity at rest and heroin cues-induced brain responses in male abstinent heroin-dependent individuals. PLoS ONE. 2011;6:1–11. doi: 10.1371/journal.pone.0023098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ma X., Qiu Y., Tian J., Wang J., Li S., Zhan W., Wang T., Zeng S., Jiang G., Xu Y. Aberrant default-mode functional and structural connectivity in heroin-dependent individuals. PLoS ONE. 2015;10:1–17. doi: 10.1371/journal.pone.0120861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Wei X., Chen J., Zhu J., Li Q., Li W., Wang W. Functional connectivity of posterior cingulate gyrus in heroin dependents treated by methadone maintenance and protracted abstinence measures: An event-related fMRI study. Brain Imaging Behav. 2021;27:1–9. doi: 10.1007/s11682-020-00447-8. [DOI] [PubMed] [Google Scholar]
- 194.Wang A.L., Elman I., Lowen S.B., Blady S.J., Lynch K.G., Hyatt J.M., O’Brien C.P., Langleben D.D. Neural correlates of adherence to extended-release naltrexone pharmacotherapy in heroin dependence. Transl. Psychiatry. 2015;5:e531. doi: 10.1038/tp.2015.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Wong C.F., Silva K., Kecojevic A., Schrager S.M., Bloom J.J., Iverson E., Lankenau S.E. Coping and emotion regulation profiles as predictors of nonmedical prescription drug and illicit drug use among high-risk young adults. Drug Alcohol Depend. 2013;132:165–171. doi: 10.1016/j.drugalcdep.2013.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Estévez A., Jáuregui P., Sánchez-Marcos I., López-González H., Griffiths M.D. Attachment and emotion regulation in substance addictions and behavioral addictions. J. Behav. Addict. 2017;6:534–544. doi: 10.1556/2006.6.2017.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Zubieta J.K., Yau W.Y., Scott D.J., Stohler C.S. Belief or Need? Accounting for individual variations in the neurochemistry of the placebo effect. Brain Behav. Immun. 2006;20:15–26. doi: 10.1016/j.bbi.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 198.Savulich G., Riccelli R., Passamonti L., Correia M., Deakin J.F.W., Elliott R., Flechais R.S.A., Lingford-Hughes A.R., McGonigle J., Murphy A., et al. Effects of naltrexone are influenced by childhood adversity during negative emotional processing in addiction recovery. Transl. Psychiatry. 2017;7:e1054. doi: 10.1038/tp.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Daoura L., Nylander I. The response to naltrexone in ethanol-drinking rats depends on early environmental experiences. Pharmacol. Biochem. Behav. 2011;99:626–633. doi: 10.1016/j.pbb.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 200.Andersen S.L., Teicher M.H. Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neurosci. Biobehav. Rev. 2009;33:516–524. doi: 10.1016/j.neubiorev.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Burkholder A.R., Koss K.J., Hostinar C.E., Johnson A.E., Gunnar M.R. Early Life Stress: Effects on the Regulation of Anxiety Expression in Children and Adolescents. Soc. Dev. 2016;25:777–793. doi: 10.1111/sode.12170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Dillon D.G., Holmes A.J., Birk J.L., Brooks N., Lyons-Ruth K., Pizzagalli D.A. Childhood Adversity Is Associated with Left Basal Ganglia Dysfunction During Reward Anticipation in Adulthood. Biol. Psychiatry. 2009;66:206–213. doi: 10.1016/j.biopsych.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Fuentes S., Carrasco J., Hatto A., Navarro J., Armario A., Monsonet M., Ortiz J., Nadal R. Sex-dependent impact of early-life stress and adult immobilization in the attribution of incentive salience in rats. PLoS ONE. 2018;13:e0190044. doi: 10.1371/journal.pone.0190044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Grigsby T.J., Rogers C.J., Albers L.D., Benjamin S.M., Lust K., Eisenberg M.E., Forster M. Adverse Childhood Experiences and Health Indicators in a Young Adult, College Student Sample: Differences by Gender. Int. J. Behav. Med. 2020;27:660–667. doi: 10.1007/s12529-020-09913-5. [DOI] [PubMed] [Google Scholar]
- 205.Matthews K., Robbins T.W. Early experience as a determinant of adult behavioural responses to reward: The effects of repeated maternal separation in the rat. Neurosci. Biobehav. Rev. 2003;27:45–55. doi: 10.1016/S0149-7634(03)00008-3. [DOI] [PubMed] [Google Scholar]
- 206.Goff B., Gee D.G., Telzer E.H., Humphreys K.L., Gabard-Durnam L., Flannery J., Tottenham N. Reduced nucleus accumbens reactivity and adolescent depression following early-life stress. Neuroscience. 2013;249:129–138. doi: 10.1016/j.neuroscience.2012.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Hanson J.L., Albert D., Iselin A.M.R., Carré J.M., Dodge K.A., Hariri A.R. Cumulative stress in childhood is associated with blunted reward-related brain activity in adulthood. Soc. Cogn. Affect. Neurosci. 2016;11:405–412. doi: 10.1093/scan/nsv124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Mehta M.A., Gore-Langton E., Golembo N., Colvert E., Williams S.C.R., Sonuga-Barke E. Hyporesponsive reward anticipation in the basal ganglia following severe institutional deprivation early in life. J. Cogn. Neurosci. 2010;22:2316–2325. doi: 10.1162/jocn.2009.21394. [DOI] [PubMed] [Google Scholar]
- 209.Balodis I.M., Potenza M.N. Anticipatory reward processing in addicted populations: A focus on the monetary incentive delay task. Biol. Psychiatry. 2015;77:434–444. doi: 10.1016/j.biopsych.2014.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Blum K., Braverman E.R., Holder J.M., Lubar J.F., Monastra V.I., Miller D., Lubar J.O., Chen T.J., Comings D.E. The reward deficiency syndrome: A biogenetic model for the diagnosis and treatment of impulsive, addictive and compulsive behaviors. J. Psychoact. Drugs. 2000;32:1–112. doi: 10.1080/02791072.2000.10736099. [DOI] [PubMed] [Google Scholar]
- 211.Büchel C., Peters J., Banaschewski T., Bokde A.L.W., Bromberg U., Conrod P.J., Flor H., Papadopoulos D., Garavan H., Gowland P., et al. Blunted ventral striatal responses to anticipated rewards foreshadow problematic drug use in novelty-seeking adolescents. Nat. Commun. 2017;8:14140. doi: 10.1038/ncomms14140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Duffy K.A., Mclaughlin K.A., Green P.A. Early life adversity and health-risk behaviors: Proposed psychological and neural mechanisms. Ann. N. Y. Acad. Sci. 2018;1428:151. doi: 10.1111/nyas.13928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Weiland B.J., Zucker R.A., Zubieta J.K., Heitzeg M.M. Striatal dopaminergic reward response relates to age of first drunkenness and feedback response in at-risk youth. Addict. Biol. 2017;22:502–512. doi: 10.1111/adb.12341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Herzberg M.P., Gunnar M.R. Early life stress and brain function: Activity and connectivity associated with processing emotion and reward. Neuroimage. 2020;209:116493. doi: 10.1016/j.neuroimage.2019.116493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.McCrory E.J., Gerin M.I., Viding E. Annual Research Review: Childhood maltreatment, latent vulnerability and the shift to preventative psychiatry—The contribution of functional brain imaging. J. Child. Psychol. Psychiatry Allied Discip. 2017;58:338–357. doi: 10.1111/jcpp.12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Marusak H.A., Etkin A., Thomason M.E. Disrupted insula-based neural circuit organization and conflict interference in trauma-exposed youth. NeuroImage Clin. 2015;8:516–525. doi: 10.1016/j.nicl.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Corral-Frías N.S., Nikolova Y.S., Michalski L.J., Baranger D.A.A., Hariri A.R., Bogdan R. Stress-related anhedonia is associated with ventral striatum reactivity to reward and transdiagnostic psychiatric symptomatology. Psychol. Med. 2015;45:2605–2617. doi: 10.1017/S0033291715000525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Marusak H.A., Martin K.R., Etkin A., Thomason M.E. Childhood Trauma Exposure Disrupts the Automatic Regulation of Emotional Processing. Neuropsychopharmacology. 2015;40:1250–1258. doi: 10.1038/npp.2014.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Campbell E.J., Mitchell C.S., Adams C.D., Yeoh J.W., Hodgson D.M., Graham B.A., Dayas C.V. Chemogenetic activation of the lateral hypothalamus reverses early life stress-induced deficits in motivational drive. Eur. J. Neurosci. 2017;46:2285–2296. doi: 10.1111/ejn.13674. [DOI] [PubMed] [Google Scholar]
- 220.Novick A.M., Levandowski M.L., Laumann L.E., Philip N.S., Price L.H., Tyrka A.R. The effects of early life stress on reward processing. J. Psychiatr. Res. 2018;101:80–103. doi: 10.1016/j.jpsychires.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Pryce C.R., Dettling A., Spengler M., Spaete C., Feldon J. Evidence for altered monoamine activity and emotional and cognitive disturbance in marmoset monkeys exposed to early life stress. Ann. N. Y. Acad. Sci. 2004;1032:245–249. doi: 10.1196/annals.1314.030. [DOI] [PubMed] [Google Scholar]
- 222.Rüedi-Bettschen D., Pedersen E.M., Feldon J., Pryce C.R. Early deprivation under specific conditions leads to reduced interest in reward in adulthood in Wistar rats. Behav. Brain Res. 2005;156:297–310. doi: 10.1016/j.bbr.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 223.Birn R.M., Roeber B.J., Pollak S.D., Reyna V.F. Early childhood stress exposure, reward pathways, and adult decision making. Proc. Natl. Acad. Sci. USA. 2017;114:13549–13554. doi: 10.1073/pnas.1708791114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Casement M.D., Shaw D.S., Sitnick S.L., Musselman S.C., Forbes E.E. Life stress in adolescence predicts early adult reward-related brain function and alcohol dependence. Soc. Cogn. Affect. Neurosci. 2013;10:416–423. doi: 10.1093/scan/nsu061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Boecker R., Holz N.E., Buchmann A.F., Blomeyer D., Plichta M.M., Wolf I., Baumeister S., Meyer-Lindenberg A., Banaschewski T., Randeis D., et al. Impact of early life adversity on reward processing in young adults: EEG-fMRI results from a prospective study over 25 years. PLoS ONE. 2014;9:1–13. doi: 10.1371/journal.pone.0104185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Fareri D.S., Gabard-Durnam L., Goff B., Flannery J., Gee D.G., Lumian D.S., Caldera C., Tottenham N. Altered ventral striatal-medial prefrontal cortex resting-state connectivity mediates adolescent social problems after early institutional care. Dev. Psychopathol. 2017;29:1865–1876. doi: 10.1017/S0954579417001456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Park A.T., Tooley U.A., Leonard J.A., Boroshok A.L., McDermott C.L., Tisdall M.D., Mackey A.P. Early childhood stress is associated with blunted development of ventral tegmental area functional connectivity. Dev. Cogn. Neurosci. 2021;47:100909. doi: 10.1016/j.dcn.2020.100909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hanson J.L., Knodt A.R., Brigidi B.D., Hariri A.R. Heightened connectivity between the ventral striatum and medial prefrontal cortex as a biomarker for stress-related psychopathology: Understanding interactive effects of early and more recent stress. Psychol. Med. 2018;48:1835–1843. doi: 10.1017/S0033291717003348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Nephew B.C., Huang W., Poirier G.L., Payne L., King J.A. Altered neural connectivity in adult female rats exposed to early life social stress. Behav. Brain Res. 2017;316:225–233. doi: 10.1016/j.bbr.2016.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Ieong H.F., Yuan Z. Resting-State Neuroimaging and Neuropsychological Findings in Opioid Use Disorder during Abstinence: A Review. Front. Hum. Neurosci. 2017;11:169. doi: 10.3389/fnhum.2017.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Tabatabaei-Jafari H., Ekhtiari H., Ganjgahi H., Hassani-Abharian P., Oghabian M.A., Moradi A., Sadighi N., Zarei M. Patterns of brain activation during craving in heroin dependents successfully treated by methadone maintenance and abstinence-based treatments. J. Addict. Med. 2014;8:123–129. doi: 10.1097/ADM.0000000000000022. [DOI] [PubMed] [Google Scholar]
- 232.Lin H.C., Wang P.W., Wu H.C., Ko C.H., Yang Y.H., Yen C.F. Altered gray matter volume and disrupted functional connectivity of dorsolateral prefrontal cortex in men with heroin dependence. Psychiatry Clin. Neurosci. 2018;72:435–444. doi: 10.1111/pcn.12655. [DOI] [PubMed] [Google Scholar]
- 233.Pandria N., Kovatsi L., Vivas A.B., Bamidis P.D. Resting-state Abnormalities in Heroin-dependent Individuals. Neuroscience. 2018;378:113–145. doi: 10.1016/j.neuroscience.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 234.Zhang Y., Tian J., Yuan K., Liu P., Zhuo L., Qin W., Zhao L., Liu J., von Deneen K.M., Klahr N.J., et al. Distinct resting-state brain activities in heroin-dependent individuals. Brain Res. 2011;1402:46–53. doi: 10.1016/j.brainres.2011.05.054. [DOI] [PubMed] [Google Scholar]
- 235.Zou F., Wu X., Zhai T., Lei Y., Shao Y., Jin X., Tan S., Wu B., Wang L., Yang Z. Abnormal resting-state functional connectivity of the nucleus accumbens in multi-year abstinent heroin addicts. J. Neurosci. Res. 2015;93:1693–1702. doi: 10.1002/jnr.23608. [DOI] [PubMed] [Google Scholar]
- 236.Ma N., Liu Y., Li N., Wang C.X., Zhang H., Jiang X.F., Xu H.S., Fu X.M., Hu X., Zhang D.R. Addiction related alteration in resting-state brain connectivity. Neuroimage. 2010;49:738–744. doi: 10.1016/j.neuroimage.2009.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Gholizadeh S., Sun N., De Jaeger X., Bechard M., Coolen L., Laviolette S.R. Early versus Late-Phase Consolidation of Opiate Reward Memories Requires Distinct Molecular and Temporal Mechanisms in the Amygdala-Prefrontal Cortical Pathway. PLoS ONE. 2013;8:e63612. doi: 10.1371/journal.pone.0063612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Lintas A., Chi N., Lauzon N.M., Bishop S.F., Sun N., Tan H., Laviolette S.R. Inputs from the basolateral amygdala to the nucleus accumbens shell control opiate reward magnitude via differential dopamine D1 or D2 receptor transmission. Eur. J. Neurosci. 2012;35:279–290. doi: 10.1111/j.1460-9568.2011.07943.x. [DOI] [PubMed] [Google Scholar]
- 239.Rosen L.G., Zunder J., Renard J., Fu J., Rushlow W., Laviolette S.R. Opiate Exposure State Controls a D2-CaMKIIα-Dependent Memory Switch in the Amygdala-Prefrontal Cortical Circuit. Neuropsychopharmacology. 2016;41:847–857. doi: 10.1038/npp.2015.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Li Q., Li W., Wang H., Wang Y., Zhang Y., Zhu J., Zheng Y., Zhang D., Wang L., Li Y., et al. Predicting subsequent relapse by drug-related cue-induced brain activation in heroin addiction: An event-related functional magnetic resonance imaging study. Addict. Biol. 2015;20:968–978. doi: 10.1111/adb.12182. [DOI] [PubMed] [Google Scholar]
- 241.Upadhyay J., Maleki N., Potter J., Elman I., Rudrauf D., Knudsen J., Wallin D., Pendse G., McDonald L., Griffin M., et al. Alterations in brain structure and functional connectivity in prescription opioid-dependent patients. Brain. 2010;133:2098–2114. doi: 10.1093/brain/awq138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Bajic D., Commons K.G., Soriano S.G. Morphine-enhanced apoptosis in selective brain regions of neonatal rats. Int. J. Dev. Neurosci. 2013;31:258–266. doi: 10.1016/j.ijdevneu.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Bajo M., Roberto M., Madamba S.G., Siggins G.R. Neuroadaptation of GABAergic transmission in the central amygdala during chronic morphine treatment. Addict. Biol. 2011;16:551–564. doi: 10.1111/j.1369-1600.2010.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Robinson T.E., Kolb B. Structural plasticity associated with exposure to drugs of abuse. Neuropharmacology. 2004;47:33–46. doi: 10.1016/j.neuropharm.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 245.Yuan K., Sheng H., Song J., Yang L., Cui D., Ma Q., Zhang W., Lai B., Chen M., Zhenmg P. Morphine treatment enhances glutamatergic input onto neurons of the nucleus accumbens via both disinhibitory and stimulating effect. Addict. Biol. 2017;22:1756–1767. doi: 10.1111/adb.12438. [DOI] [PubMed] [Google Scholar]
- 246.Kosten T.R., George T.P. The neurobiology of opioid dependence: Implications for treatment. Sci. Pract. Perspect. 2002;1:13–20. doi: 10.1151/spp021113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Gardner E.L. Addiction and brain reward and antireward pathways. Adv. Psychosom. Med. 2011;30:22–60. doi: 10.1159/000324065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Koob G.F. Addiction is a reward deficit and stress surfeit disorder. Front. Psychiatry. 2013;4:72. doi: 10.3389/fpsyt.2013.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Peciña M., Karp J.F., Mathew S., Todtenkopf M.S., Ehrich E.W., Zubieta J.K. Endogenous opioid system dysregulation in depression: Implications for new therapeutic approaches. Mol. Psychiatry. 2019;24:576–587. doi: 10.1038/s41380-018-0117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.de Wit H., Phillips T.J. Do initial responses to drugs predict future use or abuse? Neurosci. Biobehav. Rev. 2012;36:1565–1576. doi: 10.1016/j.neubiorev.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Peltz G., Südhof T.C. The neurobiology of opioid addiction and the potential for prevention strategies. JAMA J. Am. Med. Assoc. 2018;319:2071–2072. doi: 10.1001/jama.2018.3394. [DOI] [PubMed] [Google Scholar]
- 252.Nylander I., Roman E. Neuropeptides as mediators of the early-life impact on the brain; implications for alcohol use disorders. Front. Mol. Neurosci. 2012;5:77. doi: 10.3389/fnmol.2012.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Bagley E.E., Ingram S.L. Endogenous opioid peptides in the descending pain modulatory circuit. Neuropharmacology. 2020;173:108131. doi: 10.1016/j.neuropharm.2020.108131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Gavériaux-Ruff C., Kieffer B.L. Opioid receptor genes inactivated in mice: The highlights. Neuropeptides. 2002;36:62–71. doi: 10.1054/npep.2002.0900. [DOI] [PubMed] [Google Scholar]
- 255.Kimmey B.A., McCall N.M., Wooldridge L.M., Satterthwaite T.D., Corder G. Engaging endogenous opioid circuits in pain affective processes. J. Neurosci. Res. 2020 doi: 10.1002/jnr.24762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Le Merrer J., Becker J.A.J., Befort K., Kieffer B.L. Reward processing by the opioid system in the brain. Physiol. Rev. 2009;89:1379–1412. doi: 10.1152/physrev.00005.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Trigo J.M., Martin-García E., Berrendero F., Robledo P., Maldonado R. The endogenous opioid system: A common substrate in drug addiction. Drug Alcohol Depend. 2010;108:183–194. doi: 10.1016/j.drugalcdep.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 258.Valentino R.J., Van Bockstaele E. Endogenous opioids: The downside of opposing stress. Neurobiol. Stress. 2015;1:23–32. doi: 10.1016/j.ynstr.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Schrepf A., Harper D.E., Harte S.E., Wang H., Ichesco E., Hampson J.P., Zubieta J.K., Clauw D.J., Harris R.E. Endogenous opioidergic dysregulation of pain in fibromyalgia: A PET and fMRI study. Pain. 2016;157:2217–2225. doi: 10.1097/j.pain.0000000000000633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Toubia T., Khalife T. The Endogenous Opioid System: Role and Dysfunction Caused by Opioid Therapy. Clin. Obstet. Gynecol. 2019;62:3–10. doi: 10.1097/GRF.0000000000000409. [DOI] [PubMed] [Google Scholar]
- 261.Palm S., Daoura L., Roman E., Nylander I. Effects of Rearing Conditions on Behaviour and Endogenous Opioids in Rats with Alcohol Access during Adolescence. PLoS ONE. 2013;8:e76591. doi: 10.1371/journal.pone.0076591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Simmons S.C., Shepard R.D., Gouty S., Langlois L.D., Flerlage W.J., Cox B.M., Nugent F. Early life stress dysregulates kappa opioid receptor signaling within the lateral habenula. Neurobiol. Stress. 2020;13:100267. doi: 10.1016/j.ynstr.2020.100267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Granholm L., Todkar A., Bergman S., Nilsson K., Comasco E., Nylander I. The expression of opioid genes in non-classical reward areas depends on early life conditions and ethanol intake. Brain Res. 2017;1668:36–45. doi: 10.1016/j.brainres.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 264.Kiosterakis G., Stamatakis A., Diamantopoulou A., Fameli M., Stylianopoulou F. Long-term effects of neonatal handling on Mu-opioid receptor levels in the brain of the offspring. Dev. Psychobiol. 2009;51:439–449. doi: 10.1002/dev.20383. [DOI] [PubMed] [Google Scholar]
- 265.Lovallo W.R., Acheson A., Vincent A.S., Sorocco K.H., Cohoon A.J. Early life adversity diminishes the cortisol response to opioid blockade in women: Studies from the Family Health Patterns project. PLoS ONE. 2018;13:e0205723. doi: 10.1371/journal.pone.0205723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Garland E.L., Reese S.E., Bedford C.E., Baker A.K. Adverse childhood experiences predict autonomic indices of emotion dysregulation and negative emotional cue-elicited craving among female opioid-treated chronic pain patients. Dev. Psychopathol. 2019;31:1101–1110. doi: 10.1017/S0954579419000622. [DOI] [PubMed] [Google Scholar]
- 267.Valentino R.J., Volkow N.D. Untangling the complexity of opioid receptor function. Neuropsychopharmacology. 2018;43:2514–2520. doi: 10.1038/s41386-018-0225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Levran O., Peles E., Randesi M., Da Rosa J.C., Adelson M., Kreek M.J. The μ-opioid receptor nonsynonymous variant 118A>G is associated with prolonged abstinence from heroin without agonist treatment. Pharmacogenomics. 2017;18:1393–1400. doi: 10.2217/pgs-2017-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nikoshkov A., Drakenberg K., Wang X., Horvath M.C., Keller E., Hurd Y.L. Opioid neuropeptide genotypes in relation to heroin abuse: Dopamine tone contributes to reversed mesolimbic proenkephalin expression. Proc. Natl. Acad. Sci. USA. 2008;105:786–791. doi: 10.1073/pnas.0710902105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Ravindranathan A., Joslyn G., Robertson M., Schuckit M.A., Whistler J.L., White R.L. Functional characterization of human variants of the mu-opioid receptor gene. Proc. Natl. Acad. Sci. USA. 2009;106:10811–10816. doi: 10.1073/pnas.0904509106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Crist R.C., Reiner B.C., Berrettini W.H. A review of opioid addiction genetics. Curr. Opin. Psychol. 2019;27:31–35. doi: 10.1016/j.copsyc.2018.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Bardo M.T., Neisewander J.L., Kelly T.H. Individual Differences and Social Influences on the Neurobehavioral Pharmacology of Abused Drugs. Pharmacol. Rev. 2013;65:255–290. doi: 10.1124/pr.111.005124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Vazquez V., Penit-Soria J., Durand C., Besson M.J., Giros B., Daugé V. Maternal deprivation increases vulnerability to morphine dependence and disturbs the enkephalinergic system in adulthood. J. Neurosci. 2005;25:4453–4462. doi: 10.1523/JNEUROSCI.4807-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Skinner B.F. Science and Human Behavior. Macmillan; New York, NY, USA: 1953. [Google Scholar]
- 275.Rodrigues A.J., Leão P., Carvalho M., Almeida O.F.X., Sousa N. Potential programming of dopaminergic circuits by early life stress. Psychopharmacology. 2011;214:107–120. doi: 10.1007/s00213-010-2085-3. [DOI] [PubMed] [Google Scholar]
- 276.Kalinichev M., Easterling K.W., Holtzman S.G. Repeated neonatal maternal separation alters morphine-induced antinociception in male rats. Brain Res. Bull. 2001;54:649–654. doi: 10.1016/S0361-9230(01)00485-3. [DOI] [PubMed] [Google Scholar]
- 277.Kreek M.J., Reed B., Butelman E.R. Current status of opioid addiction treatment and related preclinical research. Sci. Adv. 2019;5:eaax9140. doi: 10.1126/sciadv.aax9140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Valentino R.J., Van Bockstaele E. Opposing regulation of the locus coeruleus by corticotropin-releasing factor and opioids: Potential for reciprocal interactions between stress and opioid sensitivity. Psychopharmacology. 2001;158:331–342. doi: 10.1007/s002130000673. [DOI] [PubMed] [Google Scholar]
- 279.Martinez D., Slifstein M., Matuskey D., Nabulsi N., Zheng M.Q., Lin S.F., Ropchan J., Urban N., Grassetti A., Chang D., et al. Kappa-opioid receptors, dynorphin, and cocaine addiction: A positron emission tomography study. Neuropsychopharmacology. 2019;44:1720–1727. doi: 10.1038/s41386-019-0398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Heinz A., Reimold M., Wrase J., Hermann D., Croissant B., Mundle G., Dohmen B.M., Braus D.R., Schumann G., Machulla H.J., et al. Correlation of stable elevations in striatal μ-opioid receptor availability in detoxified alcoholic patients with alcohol craving: A positron emission tomography study using carbon 11-labeled carfentanil. Arch. Gen. Psychiatry. 2005;62:57–64. doi: 10.1001/archpsyc.62.1.57. [DOI] [PubMed] [Google Scholar]
- 281.Hermann D., Hirth N., Reimold M., Batra A., Smolka M.N., Hoffmann S., Kiefer F., Noori H.R., Sommer W.H., Reischi G., et al. Low μ-Opioid Receptor Status in Alcohol Dependence Identified by Combined Positron Emission Tomography and Post-Mortem Brain Analysis. Neuropsychopharmacology. 2017;42:606–614. doi: 10.1038/npp.2016.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Weerts E.M., Wand G.S., Kuwabara H., Munro C.A., Dannals R.F., Hilton J., Frost J.J., McCaul M.E. Positron Emission Tomography Imaging of Mu- and Delta-Opioid Receptor Binding in Alcohol-Dependent and Healthy Control Subjects. Alcohol. Clin. Exp. Res. 2011;35:2162–2173. doi: 10.1111/j.1530-0277.2011.01565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Kuwabara H., Heishman S.J., Brasic J.R., Contoreggi C., Cascella N., Mackowick K.M., Taylor R., Rousset O., Willis W., Huestis M.A., et al. Mu opioid receptor binding correlates with nicotine dependence and reward in smokers. PLoS ONE. 2014;9:e113694. doi: 10.1371/journal.pone.0113694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Martikainen I.K., Peciña M., Love T.M., Nuechterlein E.B., Cummiford C.M., Green C.R., Harris R.E., Stohler C.S., Zubieta J.K. Alterations in endogenous opioid functional measures in chronic back pain. J. Neurosci. 2013;33:14729–14737. doi: 10.1523/JNEUROSCI.1400-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Douma E.H., de Kloet E.R. Stress-induced plasticity and functioning of ventral tegmental dopamine neurons. Neurosci. Biobehav. Rev. 2020;108:48–77. doi: 10.1016/j.neubiorev.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 286.Gregoriou G.C., Kissiwaa S.A., Patel S.D., Bagley E.E. Dopamine and opioids inhibit synaptic outputs of the main island of the intercalated neurons of the amygdala. Eur. J. Neurosci. 2019;50:2065–2074. doi: 10.1111/ejn.14107. [DOI] [PubMed] [Google Scholar]
- 287.Koob G.F. Neurobiology of Opioid Addiction: Opponent Process, Hyperkatifeia, and Negative Reinforcement. Biol. Psychiatry. 2020;87:44–53. doi: 10.1016/j.biopsych.2019.05.023. [DOI] [PubMed] [Google Scholar]
- 288.Wise R.A., Robble M.A. Dopamine and addiction. Annu. Rev. Psychol. 2020;71:79–106. doi: 10.1146/annurev-psych-010418-103337. [DOI] [PubMed] [Google Scholar]
- 289.Bonapersona V., Joëls M., Sarabdjitsingh R.A. Effects of early life stress on biochemical indicators of the dopaminergic system: A 3 level meta-analysis of rodent studies. Neurosci. Biobehav. Rev. 2018;95:1–16. doi: 10.1016/j.neubiorev.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 290.Brake W.G., Zhang T.Y., Diorio J., Meaney M.J., Gratton A. Influence of early postnatal rearing conditions on mesocorticolimbic dopamine and behavioural responses to psychostimulants and stressors in adult rats. Eur. J. Neurosci. 2004;19:1863–1874. doi: 10.1111/j.1460-9568.2004.03286.x. [DOI] [PubMed] [Google Scholar]
- 291.Lampert C., Arcego D.M., de Sá Couto-Pereira N., dos Santos Vieira A., Toniazzo A.P., Krolow R., Garcia E., Vendite D.A., Calcagnotto M.E., Dalmaz C. Short post-weaning social isolation induces long-term changes in the dopaminergic system and increases susceptibility to psychostimulants in female rats. Int. J. Dev. Neurosci. 2017;61:21–30. doi: 10.1016/j.ijdevneu.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 292.Lovic V., Belay H., Walker C.D., Burton C.L., Meaney M.J., Sokolowski M., Fleming A.S. Early postnatal experience and DRD2 genotype affect dopamine receptor expression in the rat ventral striatum. Behav. Brain Res. 2013;237:278–282. doi: 10.1016/j.bbr.2012.09.046. [DOI] [PubMed] [Google Scholar]
- 293.Sasagawa T., Horii-Hayashi N., Okuda A., Hashimoto T., Azuma C., Nishi M. Long-term effects of maternal separation coupled with social isolation on reward seeking and changes in dopamine D1 receptor expression in the nucleus accumbens via DNA methylation in mice. Neurosci. Lett. 2017;641:33–39. doi: 10.1016/j.neulet.2017.01.025. [DOI] [PubMed] [Google Scholar]
- 294.Yuan R., Nechvatal J.M., Buckmaster C.L., Ayash S., Parker K.J., Schatzberg A.F., Lyons D.M., Menon V. Long-term effects of intermittent early life stress on primate prefrontal–subcortical functional connectivity. Neuropsychopharmacology. 2021;25:1–9. doi: 10.1038/s41386-021-00956-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Matthews K., Dalley J.W., Matthews C., Tsai T.H., Robbins T.W. Periodic maternal separation of neonatal rats produces region- and gender-specific effects on biogenic amine content in postmortem adult brain. Synapse. 2001;40:1–10. doi: 10.1002/1098-2396(200104)40:1<1::AID-SYN1020>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 296.Fulford A.J., Marsden C.A. Effect of isolation-rearing on conditioned dopamine release in vivo in the nucleus accumbens of the rat. J. Neurochem. 1998;70:384–390. doi: 10.1046/j.1471-4159.1998.70010384.x. [DOI] [PubMed] [Google Scholar]
- 297.Meaney M.J., Brake W., Gratton A. Environmental regulation of the development of mesolimbic dopamine systems: A neurobiological mechanism for vulnerability to drug abuse? Psychoneuroendocrinology. 2002;27:127–138. doi: 10.1016/S0306-4530(01)00040-3. [DOI] [PubMed] [Google Scholar]
- 298.Jahng J.W., Ryu V., Yoo S.B., Noh S.J., Kim J.Y., Lee J.H. Mesolimbic dopaminergic activity responding to acute stress is blunted in adolescent rats that experienced neonatal maternal separation. Neuroscience. 2010;171:144–152. doi: 10.1016/j.neuroscience.2010.08.063. [DOI] [PubMed] [Google Scholar]
- 299.Barch D.M., Pagliaccio D., Luking K. Mechanisms underlying motivational deficits in psychopathology: Similarities and differences in depression and schizophrenia. Curr. Top Behav. Neurosci. 2016;27:411–449. doi: 10.1007/7854_2015_376. [DOI] [PubMed] [Google Scholar]
- 300.Köhler J.C., Gröger N., Lesse A., Guara Ciurana S., Rether K., Fegert J., Bock J., Braun K. Early-Life Adversity Induces Epigenetically Regulated Changes in Hippocampal Dopaminergic Molecular Pathways. Mol. Neurobiol. 2019;56:3616–3625. doi: 10.1007/s12035-018-1199-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Salamone J.D., Yohn S.E., López-Cruz L., San Miguel N., Correa M. Activational and effort-related aspects of motivation: Neural mechanisms and implications for psychopathology. Brain. 2016;139:1325–1347. doi: 10.1093/brain/aww050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Kapor S., Aksić M., Puškaš L., Jukić M., Poleksić J., Milosavljević F., Bjelica S., Filipović B. Long-Term Effects of Maternal Deprivation on the Volume of Dopaminergic Nuclei and Number of Dopaminergic Neurons in Substantia Nigra and Ventral Tegmental Area in Rats. Front. Neuroanat. 2020;14:72. doi: 10.3389/fnana.2020.578900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.McArthur S., McHale E., Dalley J.W., Buckingham J.C., Gillies G.E. Altered mesencephalic dopaminergic populations in adulthood as a consequence of brief perinatal glucocorticoid exposure. J. Neuroendocrinol. 2005;17:475–482. doi: 10.1111/j.1365-2826.2005.01331.x. [DOI] [PubMed] [Google Scholar]
- 304.McArthur S., McHale E., Gillies G.E. The size and distribution of midbrain dopaminergic populations are permanently altered by perinatal glucocorticoid exposure in a sex- region- and time-specific manner. Neuropsychopharmacology. 2007;32:1462–1476. doi: 10.1038/sj.npp.1301277. [DOI] [PubMed] [Google Scholar]
- 305.Niwa M., Jaaro-Peled H., Tankou S., Seshadri S., Hikida T., Matsumoto Y., Cascella N.G., Kano S., Ozaki N., Nabeshima T., et al. Adolescent stress-induced epigenetic control of dopaminergic neurons via glucocorticoids. Science. 2013;339:335–339. doi: 10.1126/science.1226931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Lo Iacono L., Catale C., Martini A., Valzania A., Viscomi M.T., Chiurchiù V., Guatteo E., Bussone S., Perrone F., Di Sabato P., et al. From Traumatic Childhood to Cocaine Abuse: The Critical Function of the Immune System. Biol. Psychiatry. 2018;84:905–916. doi: 10.1016/j.biopsych.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 307.Kosten T.A., Xiang Y.Z., Kehoe P. Heightened cocaine and food self-administration in female rats with neonatal isolation experience. Neuropsychopharmacology. 2006;31:70–76. doi: 10.1038/sj.npp.1300779. [DOI] [PubMed] [Google Scholar]
- 308.Moffett M.C., Vicentic A., Kozel M., Plotsky P., Francis D.D., Kuhar M.J. Maternal separation alters drug intake patterns in adulthood in rats. Biochem. Pharmacol. 2007;73:321–330. doi: 10.1016/j.bcp.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Wakeford A.G.P., Morin E.L., Bramlett S.N., Howell B.R., McCormack K.M., Meyer J.S., Nader M.A., Sanchez M.M., Howell L.L. Effects of early life stress on cocaine self-administration in post-pubertal male and female rhesus macaques. Psychopharmacology. 2019;236:2785–2796. doi: 10.1007/s00213-019-05254-8. [DOI] [PubMed] [Google Scholar]
- 310.Pruessner J.C., Champagne F., Meaney M.J., Dagher A. Dopamine Release in Response to A Psychological Stress in Humans and Its Relationship to Early Life Maternal Care: A Positron Emission Tomography Study Using [11C]raclopride. J. Neurosci. 2004;24:2825–2831. doi: 10.1523/JNEUROSCI.3422-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Oswald L.M., Wand G.S., Kuwabara H., Wong D.F., Zhu S., Brasic J.R. History of childhood adversity is positively associated with ventral striatal dopamine responses to amphetamine. Psychopharmacology. 2014;231:2417–2433. doi: 10.1007/s00213-013-3407-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Bozarth M.A. Neuroanatomical boundaries of the reward-relevant opiate-receptor field in the ventral tegmental area as mapped by the conditioned place preference method in rats. Brain Res. 1987;414:77–84. doi: 10.1016/0006-8993(87)91327-8. [DOI] [PubMed] [Google Scholar]
- 313.Hnasko T.S., Sotak B.N., Palmiter R.D. Morphine reward in dopamine-deficient mice. Nature. 2005;438:854–857. doi: 10.1038/nature04172. [DOI] [PubMed] [Google Scholar]
- 314.Johnson S.W., North R.A. Opioids excite dopamine neurons by hyperpolarization of local interneurons. J. Neurosci. 1992;12:483–488. doi: 10.1523/JNEUROSCI.12-02-00483.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Maldonado R., Saiardi A., Valverde O., Samad T.A., Roques B.P., Borrelli E. Absence of opiate, rewarding effects in mice lacking dopamine D2 receptors. Nature. 1997;388:586–589. doi: 10.1038/41567. [DOI] [PubMed] [Google Scholar]
- 316.al’Absi M., Nakajima M., Lemieux A. Impact of early life adversity on the stress biobehavioral response during nicotine withdrawal. Psychoneuroendocrinology. 2018;98:108–118. doi: 10.1016/j.psyneuen.2018.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Latagliata EC laudi Valzania A., Pascucci T., Campus P., Cabib S., Puglisi-Allegra S. Stress-induced activation of ventral tegmental mu-opioid receptors reduces accumbens dopamine tone by enhancing dopamine transmission in the medial pre-frontal cortex. Psychopharmacology. 2014;231:4099–4108. doi: 10.1007/s00213-014-3549-7. [DOI] [PubMed] [Google Scholar]
- 318.Olianas M.C., Dedoni S., Onali P. Potentiation of dopamine D1-like receptor signaling by concomitant activation of δ- And μ-opioid receptors in mouse medial prefrontal cortex. Neurochem. Int. 2012;61:1404–1416. doi: 10.1016/j.neuint.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 319.Svingos A.L., Garzón M., Colago E.E., Pickel V.M. Mu-opioid receptors in the ventral tegmental area are targeted to presynaptically and directly modulate mesocortical projection neurons. Synapse. 2001;41:221–229. doi: 10.1002/syn.1079. [DOI] [PubMed] [Google Scholar]
- 320.Wenzel J.M., Cheer J.F. Endocannabinoid Regulation of Reward and Reinforcement through Interaction with Dopamine and Endogenous Opioid Signaling. Neuropsychopharmacology. 2018;43:103–115. doi: 10.1038/npp.2017.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Corre J., van Zessen R., Loureiro M., Patriarchi T., Tian L., Pascoli V., Lüscher C. Dopamine neurons projecting to medial shell of the nucleus accumbens drive heroin reinforcement. eLife. 2018;7:e39945. doi: 10.7554/eLife.39945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Navratilova E., Xie J.Y., Okun A., Qu C., Eyde N., Ci S., Ossipov M.H., King T., Fields H.L., Porreca F. Pain relief produces negative reinforcement through activation of mesolimbic reward–valuation circuitry. Proc. Natl. Acad. Sci. USA. 2012;109:20709–20713. doi: 10.1073/pnas.1214605109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Negrete-Díaz J.V., Shumilov K., Real M.Á., Medina-Luque J., Valderrama-Carvajal A., Flores G., Rodriguez-Moreno A., Rivera A. Pharmacological activation of dopamine D4 receptor modulates morphine-induced changes in the expression of GAD65/67 and GABAB receptors in the basal ganglia. Neuropharmacology. 2019 doi: 10.1016/j.neuropharm.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 324.Borsook D., Linnman C., Faria V., Strassman A.M., Becerra L., Elman I. Reward deficiency and anti-reward in pain chronification. Neurosci. Biobehav. Rev. 2016;68:282–297. doi: 10.1016/j.neubiorev.2016.05.033. [DOI] [PubMed] [Google Scholar]
- 325.Comings D.E., Blum K. Reward deficiency syndrome: Genetic aspects of behavioral disorders. Prog. Brain Res. 2000;126:325–341. doi: 10.1016/S0079-6123(00)26022-6. [DOI] [PubMed] [Google Scholar]
- 326.Gold M.S., Baron D., Bowirrat A., Blum K. Neurological correlates of brain reward circuitry linked to opioid use disorder (OUD): Do homo sapiens acquire or have a reward deficiency syndrome? J. Neurol. Sci. 2020;418:1–14. doi: 10.1016/j.jns.2020.117137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Elmer G.I., Pieper J.O., Rubinstein M., Low M.J., Grandy D.K., Wise R.A. Failure of intravenous morphine to serve as an effective instrumental reinforcer in dopamine D2 receptor knock-out mice. J. Neurosci. 2002;22:RC224. doi: 10.1523/JNEUROSCI.22-10-j0004.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.