Abstract
Background:
Proximal, distal, and combined proximal and distal procedures have been performed for patellofemoral instability in the presence of patella alta. No consensus exists regarding the accepted surgical management for this condition.
Purpose:
To pool the outcomes of surgical management for patellofemoral instability in the presence of patella alta and to determine whether the outcomes differ for different surgical techniques.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
This systematic review was conducted using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. All studies that reported surgical outcomes for patellofemoral instability in the presence of patella alta were included. The random-effects model was used to analyze pooled estimates of preoperative and postoperative differences for outcomes that were reported in ≥3 studies. If heterogeneity existed among the studies, further analysis was performed using random-effects meta-regression analysis, which allowed for the identification of moderators.
Results:
A total of 11 studies with 546 knees were included. The pooled relative risk (RR) of having no patellofemoral dislocation and no patellofemoral apprehension or subjective instability postoperatively was 51.80 (95% CI, 20.75-129.31) and 48.70 (95% CI, 17.22-137.71), respectively. The pooled weighted mean improvement (WMI) for the Kujala and Lysholm scores postoperatively was 31.98 (95% CI, 28.66-35.30) and 35.93 (95% CI, 30.12-41.74), respectively. The pooled WMI for patellar tilt angles postoperatively was 10.94 (95% CI, 7.87-14.01). These outcomes were homogeneous across all studies. The pooled WMI for Insall-Salvati ratio, Caton-Deschamps index, and tibial tubercle–trochlear groove distance postoperatively was 0.31 (95% CI, 0.17-0.45), 0.24 (95% CI, 0.12-0.36), and 6.77 (95% CI, 1.96-11.58), respectively. These outcomes were heterogeneous across the studies, with the presence of distal procedures being a significant moderator. The presence of distal procedures had a significantly higher unweighted RR of 38.07 (95% CI, 2.37-613.09) for major complications compared with proximal procedures alone, although the incidence of minor complications was comparable (unweighted RR, 1.25; 95% CI, 0.35-4.48).
Conclusion:
Surgical management for patellofemoral instability in the presence of patella alta consistently led to improvement in clinical and functional outcomes, regardless of the type of procedure performed. Distal procedures were better able to correct the patellar height and tibial tubercle–trochlear groove distance, although these procedures also posed a higher RR of subsequent surgery compared with proximal procedures alone.
Keywords: patellar instability, patellofemoral instability, patellar height, patella alta
Patellofemoral instability has been estimated to affect up to 49 people per 100,000.28 Patients with recurrent patellofemoral instability often have ≥1 predisposing risk factors, including limb alignment, osseous architecture of the patella and trochlea, integrity of the soft tissue constraints, and relationship of the surrounding musculature.28 Surgeries for patellofemoral instability have therefore been described as ala carte, specially designed to target the risk factors for each patient.31
Controversy exists regarding the ideal surgery for certain risk factors.‡ One of these risk factors is patella alta.6,7,14–18,21–23 Patella alta, defined as a Caton-Deschamps index >1.2, has been noted to be present in 24% of patients with patellofemoral instability but only 3% of normal controls.13 Patella alta has also been shown to be a strong predictor of recurrent patellofemoral instability.13 Multiple surgeries have been described for patella alta; however, there is a lack of consensus regarding the accepted techniques for the management of patellofemoral instability in the presence of patella alta.6,7,14–18,21–23,33 A previous systematic review concluded that tibial tubercle distalization is an effective technique to correct patellar height and prevent recurrent patellar dislocations.13 However, the systematic review included only studies in which tibial tubercle distalization was performed to manage patella alta and recurrent patellofemoral instability, despite there being many other studies that also published the outcomes for patella alta and patellofemoral instability after other proximal or distal procedures.6,7,14–18,21–23,33
The aims of the current systematic review and meta-analysis were 2-fold. First, the study aimed to pool the outcomes of patellofemoral instability in the presence of patella alta after the various surgical techniques described. Second, the study aimed to determine whether the outcomes differed when different surgical techniques were used, therefore allowing for a better understanding of the accepted techniques in the management of patellofemoral instability in the presence of patella alta.
Methods
Systematic Review
The systematic review was performed using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The search was conducted using PubMed from inception through March 31, 2020. The keywords used were “patell*” and “alta.”
All studies that reported the outcomes of surgeries performed for patellofemoral instability in the presence of patella alta were included. We excluded studies that did not include patients with patella alta or patellofemoral instability, studies in which the outcomes of patients with patella alta or patellofemoral instability could not be isolated, studies that did not report preoperative and postoperative outcomes, nonhuman studies, studies with sample size <10, review articles, commentaries, non--English language articles, and articles with no full text available.
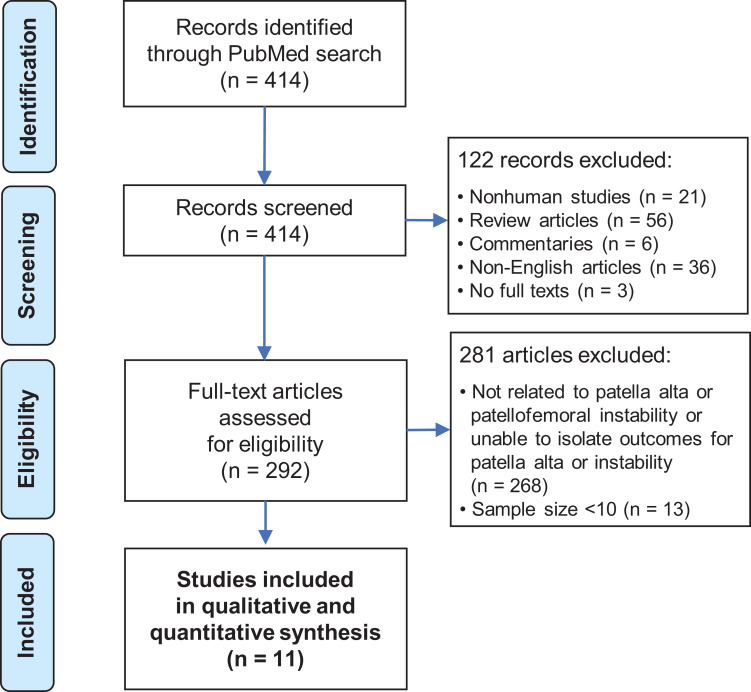
The articles were selected in 2 stages (Figure 1). First, the abstracts identified using the above searches were downloaded, and the list was screened using the inclusion and exclusion criteria. Second, the full texts of these shortlisted articles were downloaded and assessed for eligibility. The reference lists of the publications were then hand-searched for additional relevant studies. This process was repeated twice independently.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for the systematic review and meta-analysis.
Quality of Studies Assessment
The studies included were examined for the study design. The revised Methodological Index for Non-Randomized Studies (MINORS) tool was used to determine the methodological quality of the studies.24 The items were scored 0 if not reported, 1 if reported but inadequate, or 2 if reported and adequate. The global ideal score is 24 for comparative studies and 16 for case series.
Data Abstraction
Data from each study were retrieved individually. Details noted included the sample size, age distribution, sex distribution, and duration of follow-up. The surgical procedure for each study was classified as proximal, distal, or both.
All clinical outcomes reported in ≥3 studies were included. These included Kujala score, Lysholm score, recurrence of patellofemoral instability, patellar tilt angles, Caton-Deschamps index, Insall-Salvati ratio, and tibial tubercle–trochlear groove (TT-TG) distance.
The complications reported in each paper were recorded and classified as low grade or high grade according to the Clavien-Dindo system.5 Recurrence of patellofemoral dislocation, persistent patellofemoral apprehension and subjective instability, and inadequate correction of patella alta were not included in the computation of the number of low-grade or high-grade complications, because analyses were performed separately for these outcomes. The presence or absence of patellofemoral arthritis was also not included in the computation of the number of complications because these results were not reported consistently across the studies.
Attempts were made to contact authors of articles when certain details of the studies were not reported in the articles.
Data Analysis
The random-effects model was used to analyze pooled estimates of preoperative and postoperative differences for outcomes that were reported in ≥3 studies.4 Under this model, it was assumed that there was a mean population effect size about which the study-specific effect varied. Because the random-effects model properly considers interstudy heterogeneity, such as differences in study design, it provides a more conservative evaluation of the significance of the association than does one based on fixed effects.8 The pooled relative risk (RR) or weighted mean difference was then reported with the 95% CI. Forest plots were generated.
Tests of heterogeneity were conducted while pooling the differences. This was done using the Q statistic, which is distributed as a chi-square variate under the assumption of homogeneity of effect sizes. The extent of between-study heterogeneity was assessed using the I 2 statistic.10,11 If heterogeneity existed among the studies, further analysis was performed using random-effects meta-regression analysis, which allowed the effect of multiple continuous or categorical characteristics to be investigated simultaneously. This identified the moderators that might contribute to the heterogeneity of the effect sizes. Study identifiers were added to the model to control for the effect of any variations in study characteristics. The regression coefficient was calculated to indicate the percentage of variance explained by the moderators, and significant moderators were reported together with the 95% CI. The forest plots were stratified according to the significant moderators.
Funnel plots of the sample sizes were plotted against the SEs of each study. This was conducted together with the Egger statistical test to evaluate the possibility of publication bias for the outcomes analyzed.32
For the analysis of the postoperative complications, pooling of the incidence of complications was not performed using the random-effects model because many studies were excluded from the random-effects model, as no complications were reported in the studies. Instead, unweighted RRs were calculated using the raw data of the number of complications divided by the number of knees.
All statistical evaluations were made assuming a 2-sided test at the 5% level of significance using Stata Version 12 (Stata Corp).
Results
A total of 11 studies were included in the review.6,7,14–18,21–23,33 They included a total of 546 knees from 361 female patients and 156 male patients. The number of male and female patients in the study by Marteau et al14 was not included in the sample size calculation for the number of male and female patients because the sex distribution was not reported in the study. The mean age of the patients in the 11 studies was 22.7 years and the mean duration of follow-up was 27.6 months.
Proximal procedures were performed in 149 knees, distal procedures were performed in 331 knees, and combined proximal and distal procedures were performed in 66 knees.6,7,14–18,21–23,33 Proximal procedures performed included medial patellofemoral ligament reconstruction, Insall proximal realignment, and combined medial patellofemoral ligament and medial patellotibial ligament reconstructions.7,21,33 Distal procedures performed included tibial tubercle distalization with or without medialization and patellar tendon tenodesis.6,15,22,23 Combined proximal and distal procedures performed included tibial tubercle transfer combined with medial patellofemoral ligament reconstruction, medial plication, lateral release, and/or trochleoplasty.14,16–18 Table 1 illustrates the details of the patient and study characteristics of the studies included in the review.
Table 1.
Patient and Study Characteristics of Studies Included in the Reviewa
| Lead Author (Year) | LOE | Knees, n | Female/Male Patients, n | Age, y, mean (range) | Procedure | Follow-up, mo, mean (range) |
|---|---|---|---|---|---|---|
| Enea6 (2018) | 3 | 26 | 21/5b | 27.7 (NR) | Distal | 47.6 (NR) |
| Fabricant7 (2014) | 4 | 27 | 22/5 | 14.9 (NR) | Proximal | 3.0 (3.0-3.0) |
| Marteau14 (2011) | 4 | 14 | NR | 23.5 (16.0-48.0) | Combined | 90.0 (24.0-204.0) |
| Mayer15 (2012) | 4 | 27 | 16/9b | 20.4 (14.0-30.0) | Distal | 115.2 (72.0-168.0) |
| Otsuki17 (2013) | 4 | 12 | 8/2 | 20.2 (16.0-43.0) | Combined | 38.4 (13.2-66.0) |
| Otsuki16 (2017) | 4 | 28 | 21/7b | 26.3 (14.0-46.0) | Combined | 46.0 (16.0-97.0) |
| Otsuki18 (2018) | 4 | 12 | 10/2 | 44.0 (40.0-55.0) | Combined | 41.5 (24.0-72.0) |
| Roessler21 (2019) | 3 | 64 | 38/26 | 28.8 (NR) | Proximal | 50.5 (NR) |
| Rood22 (2020) | 4 | 263 | 194/69b | 20.5 (12.0-49.0)c | Distal | 4.0 (3.0-120.0)c |
| Simmons23 (1992) | 4 | 15 | 8/6 | 23.7 (17.0-31.0) | Distal | 54.0 (36.0-84.0) |
| Yang33 (2019) | 4 | 58 | 23/25 | 22.6 (NR) | Proximal | 35.6 (12.0-24.0) |
aLOE, level of evidence; NR, not reported.
bReported as number of knees instead of number of patients.
cReported as median instead of mean.
Assessment of Study Quality
The studies included were examined for the study design. The revised MINORS tool was used to determine the methodological quality of the studies.24 The average MINORS score for the case series was 11.3 out of 16, and the average score for the case-control studies was 20 out of 24. Table 2 reflects the assessment of the quality of the studies.
Table 2.
MINORS Scores of Included Studiesa
| MINORS Score Itemb | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Overall |
| Enea6 (2018) | 2 | 2 | 1 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 1 | 2 | 18 |
| Fabricant7 (2014) | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 0 | — | — | — | — | 12 |
| Marteau14 (2011) | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | — | — | — | — | 10 |
| Mayer15 (2012) | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | — | — | — | — | 10 |
| Otsuki17 (2013) | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | — | — | — | — | 11 |
| Otsuki16 (2017) | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 21 |
| Otsuki18 (2018) | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | — | — | — | — | 11 |
| Roessler21 (2019) | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 21 |
| Rood22 (2020) | 2 | 2 | 1 | 2 | 0 | 1 | 2 | 0 | — | — | — | — | 10 |
| Simmons23 (1992) | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 0 | — | — | — | — | 11 |
| Yang33 (2019) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | — | — | — | — | 15 |
aMINORS, Methodological Index for Non-Randomized Studies. The dashes indicate that the category of evaluation was not relevant to the article assessed.
bItem descriptions: 1, stated aim of the study; 2, inclusion of consecutive patients; 3, prospective collection of data; 4, endpoint appropriate to the study aim; 5, unbiased evaluation of endpoints; 6, follow-up period appropriate; 7, loss to follow-up not exceeding 5%; 8, a control group having the gold standard intervention; 9, contemporary groups; 10, baseline equivalence of groups; 11, prospective calculation of the sample size; and 12, statistical analyses adapted to the study design.
Patellofemoral Dislocation
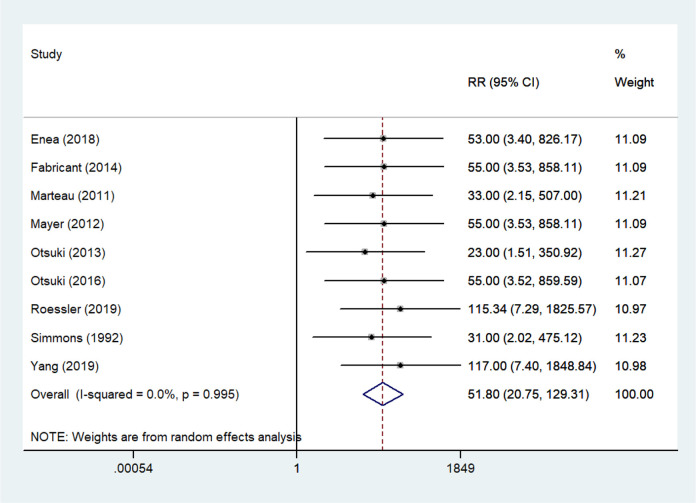
The presence or absence of recurrence of patellofemoral dislocation was reported in 9 of the 11 studies.6,7,14–17,21,23,33 All 9 studies reported a decrease in the rate of patellofemoral dislocation after surgical management for patellofemoral instability with patella alta. The pooled RR of having no patellofemoral dislocations postoperatively versus preoperatively was 51.80 (95% CI, 20.75-129.31) (Figure 2, Table 3).6,7,14–17,21,23,33 A total of 3 studies used proximal procedures,7,21,33 3 studies used distal procedures,6,15,23 and 3 studies used combined proximal and distal procedures.14,16, 17 The 9 studies were homogeneous regardless of the surgical techniques used (P = .995) (Figure 2, Table 3). No publication bias was identified across the 9 studies (P = .811) (Appendix and Table 3).
Figure 2.
Forest plot comparing the relative risk (RR) of having no patellofemoral dislocation postoperatively versus preoperatively.
Table 3.
Outcomes of Meta-analysisa
| Meta-analysis | Heterogeneity Test | Egger Test | |||
|---|---|---|---|---|---|
| Variable | Pooled Estimate | 95% CI | I 2, % | P Value | P Value |
| Patellofemoral dislocation | RR: 51.80 | 20.75 to 129.31 | 0.0 | .995 | .811 |
| Patellofemoral apprehension | RR: 48.70 | 17.22 to 137.71 | 0.0 | .963 | .051 |
| Kujala score | WMD: 31.98 | 28.66 to 35.30 | 18.5 | .297 | .956 |
| Lysholm score | WMD: 35.93 | 30.12 to 41.74 | 44.2 | .166 | .748 |
| Patellar tilt angle | WMD: –10.94 | –14.01 to –7.87 | 60.9 | .053 | .888 |
| Insall-Salvati | WMD: –0.31 | –0.45 to –0.17 | 90.8 | <.001 | .973 |
| Caton-Deschamps index | WMD: –0.24 | –0.36 to –0.12 | 92.3 | <.001 | .910 |
| TT-TG distance | WMD: –6.77 | –11.58 to –1.96 | 98.5 | <.001 | .083 |
aRR, relative risk; TT-TG, tibial tubercle–trochlear groove; WMD, weighted mean difference.
Patellofemoral Apprehension or Instability
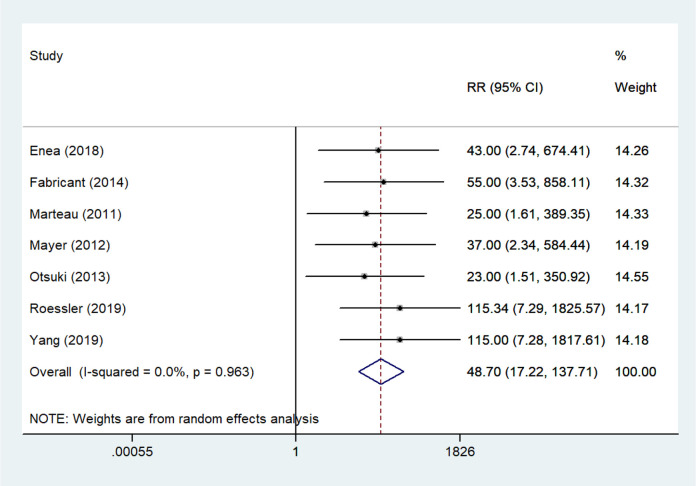
The presence or absence of patellofemoral apprehension and subjective instability in addition to patellofemoral dislocation was reported in 7 studies.6,7,14,15,17,21,33 All 7 studies consistently reported an improvement in the rates of patellofemoral apprehension and subjective instability after surgical management for patellofemoral instability with patella alta. For the 7 studies, the pooled RR of having no patellofemoral apprehension or instability postoperatively versus preoperatively was 48.70 (95% CI, 17.22-137.71) (Figure 3, Table 3). Of the 7 studies, 3 studies used proximal procedures,7,21,33 2 studies used distal procedures,6,15 and 2 studies used combined proximal and distal procedures.14,17 The 7 studies were homogeneous regardless of the surgical techniques used (P = .963) (Figure 3, Table 3). No publication bias was identified across the 7 studies (P = .051) (Appendix and Table 3).
Figure 3.
Forest plot comparing the relative risk (RR) of having no patellofemoral apprehension or subjective instability postoperatively versus preoperatively.
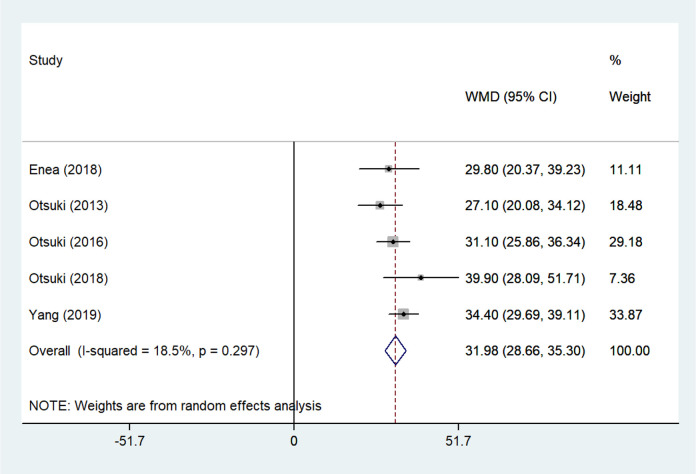
Kujala Score
A total of 5 studies reported preoperative and postoperative Kujala scores.6,16–18,33 All of these studies consistently reported improvement in Kujala scores after surgical management for patellofemoral instability with patella alta. The pooled weighted mean improvement was 31.98 (95% CI, 28.66-35.30) across the 5 studies (Figure 4, Table 3). One study used proximal procedures,33 another study used distal procedures,6 and the remaining 3 studies used combined proximal and distal procedures.16–18 The improvement across the 5 studies was homogeneous regardless of the surgical techniques used (P = .297) (Figure 4, Table 3). No publication bias was identified across the 5 studies (P = .956) (Appendix and Table 3).
Figure 4.
Forest plot comparing the weighted mean difference (WMD) of Kujala scores postoperatively versus preoperatively.
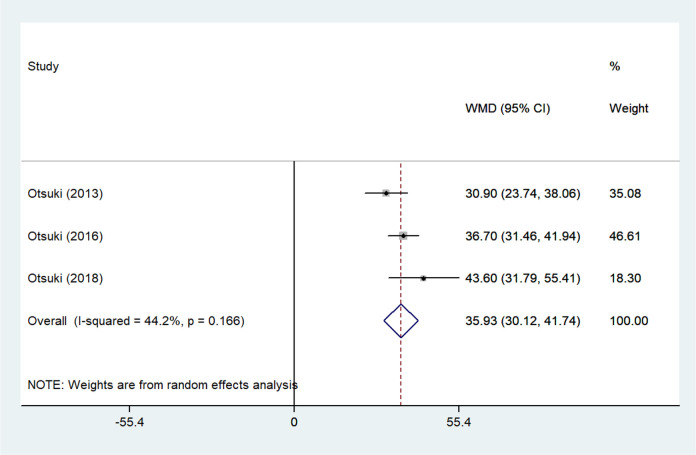
Lysholm Score
A total of 3 studies reported preoperative and postoperative Lysholm scores.16–18 All 3 of these studies consistently reported improvement in Lysholm scores after surgical management for patella alta and patellofemoral instability. The pooled weighted mean improvement was 35.93 (95% CI, 30.12-41.74) across the 3 studies (Figure 5, Table 3). All 3 studies performed combined proximal and distal procedures. The 3 studies were homogeneous (P = .166) (Figure 5, Table 3), and no publication bias was identified across the studies (P = .748) (Appendix and Table 3).
Figure 5.
Forest plot comparing the weighted mean difference (WMD) of Lysholm scores postoperatively versus preoperatively.
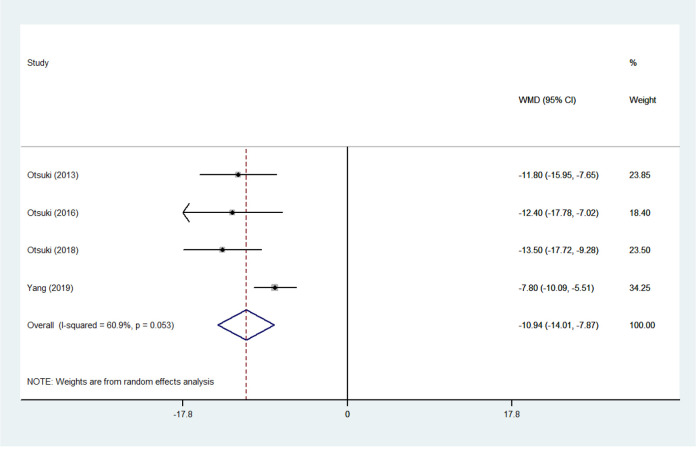
Patellar Tilt Angles
Patellar tilt angles were reported in 4 studies.16–18,33 All 4 studies consistently reported improvement in patellar tilt angles after surgical management for patellofemoral instability and patella alta. The pooled weighted mean improvement was 10.94 (95% CI, 7.87-14.01) (Figure 6, Table 3). One study performed proximal procedures,33 whereas 3 studies performed combined proximal and distal procedures.16–18 The improvement across the 4 studies was homogeneous regardless of the surgical techniques used (P = .053) (Figure 6, Table 3). No publication bias was identified across the 4 studies (P = .888) (Appendix and Table 3).
Figure 6.
Forest plot comparing the weighted mean difference (WMD) of patellar tilt angles postoperatively versus preoperatively.
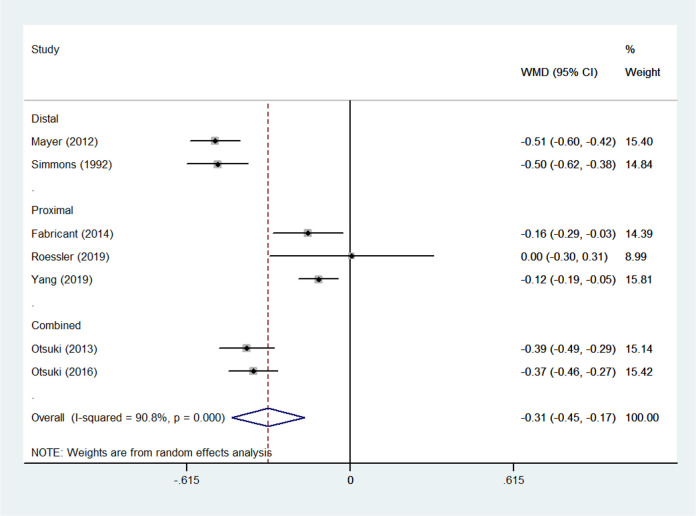
Insall-Salvati Ratio
The Insall-Salvati ratio was reported in 7 studies.7,15–17,21,23,33 The pooled weighted mean improvement was 0.31 (95% CI, 0.17-0.45) (Figure 7, Table 3). However, the 7 studies were heterogeneous (P < .001) (Figure 7, Table 3). The surgical technique was noted to be a significant moderator for the heterogeneity among the 7 studies. The use of a distal procedure further improved the Insall-Salvati ratio by 0.31 (95% CI, 0.23- 0.40) versus the use of a proximal procedure alone (P < .001). The addition of a proximal procedure to the distal procedure did not further improve the Insall-Salvati ratio compared with use of the distal procedure alone. The sample size, age, sex distribution, follow-up duration, and preoperative Insall-Salvati ratio were not significant moderators for the heterogeneity of the 7 studies. No publication bias was noted among the 7 studies (P = .973) (Appendix and Table 3).
Figure 7.
Forest plot comparing the weighted mean difference (WMD) of Insall-Salvati ratios postoperatively versus preoperatively.
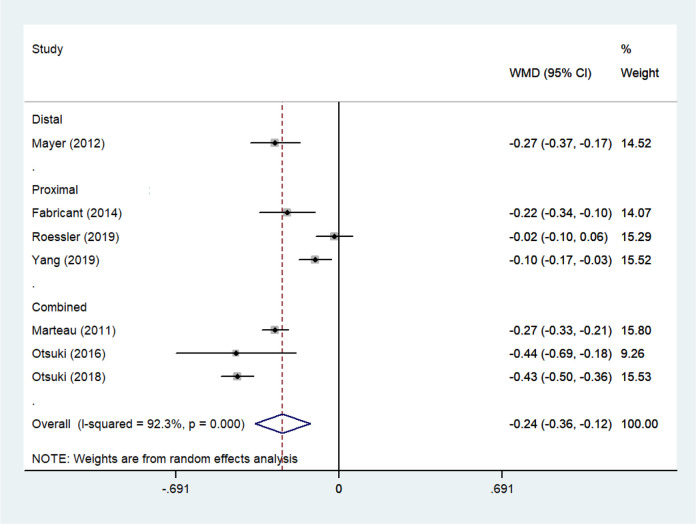
Caton-Deschamps Index
Caton-Deschamps indices were reported in 7 studies.7,14–16,18,21,33 The pooled weighted mean improvement was 0.24 (95% CI, 0.12-0.36) (Figure 8, Table 3). The 7 studies were, however, heterogeneous (P < .001) (Figure 8, Table 3). The surgical technique was a significant moderator for the heterogeneity among these studies, with the use of distal procedures decreasing the Caton-Deschamps index by 0.23 (95% CI, 0.11-0.35) compared with the use of proximal procedures (P < .001). The addition of proximal procedures to distal procedures did not moderate the Caton-Deschamps index compared with use of distal procedures alone. The sample size, age, sex distribution, follow-up duration, and preoperative Caton-Deschamps index were not significant moderators for the heterogeneity of the 7 studies. No publication bias was noted across these studies (P = .910) (Appendix and Table 3).
Figure 8.
Forest plot comparing the weighted mean difference (WMD) of Caton-Deschamps indices postoperatively versus preoperatively.
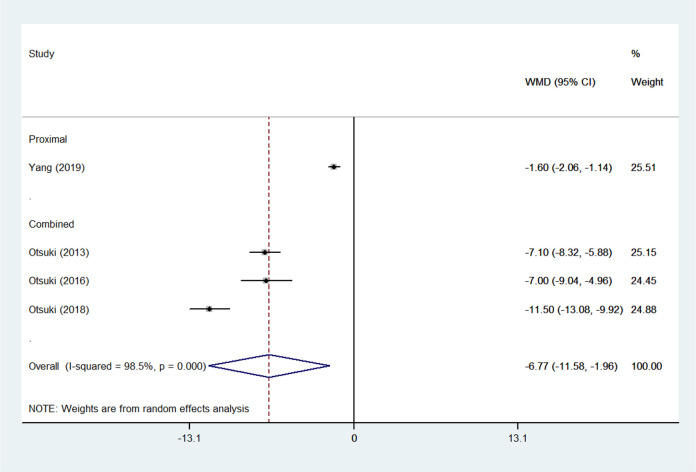
TT-TG Distance
The TT-TG distance was reported in 4 studies.16–18,33 The pooled weighted mean improvement was 6.77 (95% CI, 1.96-11.58) (Figure 9, Table 3). The 4 studies were, however, heterogeneous (P < .001) (Figure 9, Table 3). The use of distal procedures was a significant moderator for the heterogeneity among the 4 studies, significantly decreasing the TT-TG distances by 6.95 (95% CI, 3.26-10.65) compared with the use of proximal procedures alone (P < .001). No comparison could be made among studies using distal procedures alone and studies using combined proximal and distal procedures because no studies using distal procedures alone reported the preoperative and postoperative TT-TG distances. The sample size, age, sex distribution, follow-up duration, and preoperative TT-TG distance were not significant moderators for the heterogeneity of the 4 studies. No publication bias was noted across these studies (P = .083) (Appendix and Table 3).
Figure 9.
Forest plot comparing the weighted mean difference (WMD) of tibial tubercle–trochlear groove distance postoperatively versus preoperatively.
Complications
Complications of the various surgical procedures are listed in Table 4 for the 11 studies included in this review.6,7,14–18,21–23,33 These complications were classified as low-grade or high-grade complications according to the Clavien-Dindo system.5 The breakdown of the number of minor and major complications for proximal procedures, combined proximal and distal procedures, and distal procedures for all 11 studies is provided in Table 5. Comparisons were performed between studies with or without distal procedures. Distal procedures and combined proximal and distal procedures were grouped together for the comparison because the main complications in the combined group were secondary to those of the distal group (Table 4). No statistically significant difference was identified in the incidence of minor complications when comparing across the different surgical techniques across all 11 studies (unweighted RR, 1.25; 95% CI, 0.35-4.48) (Table 5). However, the use of distal procedures had a statistically significant, higher unweighted RR of 38.07 (95% CI, 2.37-613.09) for major complications than did the use of proximal procedures alone (Table 5). Statistical significance was not present, however, after we excluded surgeries for screw removals as a major complication, with the unweighted RR being 13.19 (95% CI, 0.80-217.99) (Table 5).
Table 4.
Details of Outcomes and Complications of Studies Included in Reviewa
| Lead Author (Year) | Outcomes, n | Other Complications (n) | |
|---|---|---|---|
| No Dislocation | Dislocation | ||
| Enea6 (2018) | 26 | 0 |
|
| Fabricant7 (2014) | 27 | 0 | None reported |
| Marteau14 (2011) | 16 | 0 |
|
| Mayer15 (2012) | 27 | 0 |
|
| Otsuki17 (2013) | 11 | 1 |
|
| Otsuki16 (2017) | 27 | 1 |
|
| Otsuki18 (2018) | NR | NR |
|
| Roessler21 (2019) | 59 | 5 |
|
| Rood22 (2020) | NRb | NRb |
|
| Simmons23 (1992) | 15 | 0 |
|
| Yang33 (2019) | 58 | 0 |
|
aNR, not reported.
bPostoperative redislocations were reported, but number of cases was not specified.
Table 5.
Incidence of Complications Across the Different Surgical Techniquesa
| Proximal Procedure (n = 149) | Combined Procedure (n = 66) | Distal Procedure (n = 331) | |
|---|---|---|---|
| Minor complications | |||
| Present | 3 (2.0) | 2 (3.0) | 8 (2.4) |
| Absent | 146 (98.0) | 64 (97.0) | 323 (97.6) |
| Major complications | |||
| Present | 0 (0.0) | 8 (12.1) | 42 (12.7) |
| Absent | 149 (100.0) | 58 (87.9) | 289 (87.3) |
| Major complications excluding screw removal | |||
| Present | 0 (0.0) | 1 (1.5) | 16 (4.8) |
| Absent | 149 (100.0) | 65 (98.5) | 315 (95.2) |
aData are reported as n (%).
Discussion
The principal finding of the current systematic review and meta-analysis was that surgical management for patellofemoral instability in the presence of patella alta consistently led to improvement in patellofemoral stability, alignment of the patellofemoral joint, and functional outcomes regardless of whether proximal, distal, or combined proximal and distal procedures were performed. However, using distal procedures could better correct the patellar height and TT-TG distances compared with using proximal procedures alone. Despite this, using distal procedures posed a higher RR of subsequent surgeries compared with using proximal procedures alone, whereas the risk of minor complications was comparable regardless of the type of procedure used.
These findings were novel to the current systematic review and meta-analysis. Only 1 other systematic review has been published regarding the surgical management of patellofemoral instability in the presence of patella alta. Magnussen et al13 published a systematic review in 2014 and concluded that tibial tubercle distalization was an effective technique for the correction of patellar height and prevention of recurrent patellar dislocation. However, that systematic review included only studies in which tibial tubercle distalization was performed for the management of patella alta and recurrent patellofemoral instability. Magnussen et al were therefore unable to compare the outcomes between proximal and distal procedures. Additionally, Magnussen et al stated that there was insufficient information across the studies to comment on the postoperative patient-reported outcomes.
All studies included in this systematic review and meta-analysis reported consistent and statistically significant improvement in patellofemoral stability, alignment of the patellofemoral joint, and functional outcomes after surgical management for patellofemoral instability with patella alta. The improvement in patellofemoral stability was evidenced by the decrease in the rates of patellofemoral dislocation, subjective instability, and apprehension postoperatively.6,7,14–18,21,23,33 The improvement in the alignment of the patellofemoral joint was evidenced by the improvement of patellar tilt angles postoperatively.16–18,33 The improvement in functional outcomes was evidenced by the increase in Kujala scores6,16–18,33 and Lysholm scores postoperatively.16–18 These outcomes were homogeneous and were consistently reported across all studies, regardless of the type of procedure used.
Because the improvements in patellofemoral stability, alignment of the patellofemoral joint, and functional outcomes were consistent irrespective of the type of procedure used, the current systematic review and meta-analysis also identified the advantages and disadvantages of proximal procedures versus distal alignment procedures. Advantages of using distal procedures in the surgical management of patellofemoral instability in the presence of patella alta included better correction of patellar height and TT-TG distances compared with using proximal procedures alone. A disadvantage of using distal procedures, however, was the higher RR of needing a subsequent operation, although these operations mainly entailed screw removal after distal procedures.
Use of distal procedures in the surgical management of patellofemoral instability and patella alta would be recommended for patients with symptomatic patella alta and increased TT-TG distances that would have necessitated a tibial tubercle transfer regardless of the patellar height. This is because proximal procedures alone were unable to correct the patellar height and increased TT-TG distances adequately in the studies included.7,21,33 All of the studies included that used proximal procedures alone7,21,33 had mean Insall-Salvati ratios of >1.2 postoperatively, whereas 2 out of these 3 studies21,33 included had mean Caton-Deschamps indices of >1.2 postoperatively with the last study7 having a mean Caton-Deschamps index of 1.17 postoperatively. Patients with symptomatic patella alta would then benefit from distal procedures to correct the patellar height.1 This was because patella alta alone, without patellofemoral instability, was associated with patellofemoral knee pain, chondromalacia, increased patellofemoral peak pressure, and patellofemoral arthritis, which could be effectively managed using distal procedures.1,2,12,19 Similarly, the only study included that used a proximal procedure and reported preoperative and postoperative TT-TG distances showed a decrease of only 1.6 mm in TT-TG distance postoperatively, with the postoperative TT-TG distance being 19.9 mm.33 Patients with increased TT-TG distances who would need distal procedures regardless of patellar height would be advised to have distal procedures as well for their patella alta with patellofemoral instability.9,20,25
Despite the better correction of patellar height and TT-TG distances, however, patients planning to have distal procedures for patellofemoral instability in the presence of patella alta should be counseled preoperatively about the increased RR of subsequent surgeries compared with proximal procedures alone. Although a majority of these subsequent surgeries were for screw removals after tibial tubercle transfers, subsequent surgeries were also required for other major complications as listed in Table 4. An informed discussion should therefore be held with patients, weighing the risks and benefits of both procedures in the management of patellofemoral instability in the presence of patella alta. This is in line with the modern approach of patient-centered shared decision making after the Montgomery ruling, which redefined the standard for informed consent and disclosure.3
The current systematic review and meta-analysis exhibited several strengths. First, the current review is the first systematic review and meta-analysis to investigate the outcomes of surgical management of patellofemoral instability in the presence of patella alta after proximal, distal, and combined proximal and distal procedures. Second, the current review is the first study to compare the outcomes among the various surgical procedures for patellofemoral instability in the presence of patella alta. No other study, in the form of clinical studies or reviews, has directly compared the different surgical techniques in order to identify the ideal surgical technique for these patients. Third, we identified several novel findings that were unique to the current review, as discussed. Fourth, the homogeneity across most of the outcomes, the lack of publication bias across the outcomes, and the lack of other statistically and clinically significant moderators for the heterogeneity among the studies allows greater confidence to be placed on the conclusions drawn from the current systematic review and meta-analysis.
The current systematic review and meta-analysis also had several limitations. First, the level of evidence of the review was limited by the presence of adequately powered trials in the current literature. All the studies included were of evidence levels 3 and 4, and none of them directly compared the various surgical techniques for the management of patellofemoral instability in the presence of patella alta. Future high-powered, randomized controlled trials comparing these surgical techniques would help to confirm or refute the conclusions drawn from the current review. Second, the inclusion of level 3 and 4 studies in the current systematic review and meta-analysis could have introduced potential confounders that were not controlled in the original studies. Despite this, most of the outcomes analyzed were homogeneous, and there were no other moderators that could explain the heterogeneity between the studies. No publication bias was identified across the studies. Third, the inclusion of 3 papers from the same study group could have introduced overlapping samples in the review; however, we decided to include all 3 papers in the review because the overall study group was different across the 3 studies.16–18
Conclusion
Surgical management for patellofemoral instability in the presence of patella alta consistently led to improvement in patellofemoral stability, patellofemoral joint alignment, and functional outcomes, regardless of the type of procedure performed. Distal procedures could better correct patellar height and TT-TG distances, although these procedures posed a higher RR of subsequent surgeries compared with proximal procedures alone.
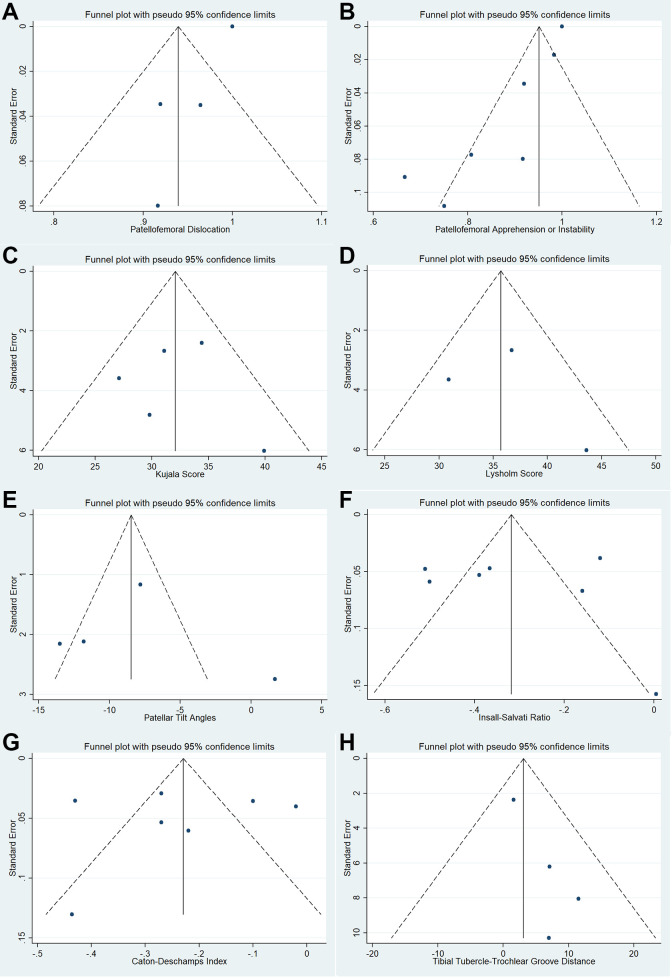
Appendix
Funnel plots with pseudo 95% CIs (diagonal lines) comparing the improvement by the SE of the reviewed studies for (A) rate of patellofemoral dislocation, (B) rate of patellofemoral apprehension or subjective instability, (C) Kujala score, (D) Lysholm score, (E) patellar tilt angle, (F) Insall-Salvati ratio, (G) Caton-Deschamps index, and (H) tibial tubercle–trochlear groove distance. The vertical line represents the meta-analysis summary estimate, and the scatter represents single study.
Footnotes
Final revision submitted November 1, 2020; accepted December 11, 2020
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. AL-Sayyad MJ, Cameron JC. Functional outcome after tibial tubercle transfer for the painful patella alta. Clin Orthop Relat Res. 2002;396:152-162. [DOI] [PubMed] [Google Scholar]
- 2. Caton J, Mironneau A, Walch G, Levigne C, Michel CR. Idiopathic high patella in adolescents: apropos of 61 surgical cases. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 1990;76(4):253-260. [PubMed] [Google Scholar]
- 3. Chan SW, Tulloch E, Cooper ES, Smith A, Wojcik W, Norman JE. Montgomery and informed consent: where are we now? BMJ. 2017;357:J2224. [DOI] [PubMed] [Google Scholar]
- 4. Deeks JJ, Altman DJ, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman DG, eds. Systematic Reviews in Health Care: Meta-analysis in Context. John Wiley & Sons; 2001:285–321. [Google Scholar]
- 5. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Enea D, Canè PP, Fravisini M, Gigante A, Dei Giudici L. Distalization and medialization of tibial tuberosity for the treatment of potential patellar instability with patella alta. Joints. 2018;6(2):80–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fabricant PD, Ladenhauf HN, Salvati EA, Green DW. Medial patellofemoral ligament (MPFL) reconstruction improves radiographic measures of patella alta in children. Knee. 2014;21(6):1180-1184. [DOI] [PubMed] [Google Scholar]
- 8. Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2(2):121–145. [DOI] [PubMed] [Google Scholar]
- 9. Franciozi CE, Ambra LF, Albertoni LJB, et al. Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity-trochlear groove distance of 17 to 20 mm. Arthroscopy. 2019;35(2):566-574. [DOI] [PubMed] [Google Scholar]
- 10. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 11. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jordan JM, Luta G, Renner JB, et al. Self-reported functional status in osteoarthritis of the knee in a rural southern community: the role of sociodemographic factors, obesity, and knee pain. Arthritis Care Res. 1996;9(4):273-278. [DOI] [PubMed] [Google Scholar]
- 13. Magnussen RA, De Simone V, Lustig S, Neyret P, Flanigan DC. Treatment of patella alta in patients with episodic patellar dislocation: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2545-2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Marteau E, Burdin P, Brilhault JM. Gracilis tendon transfer associated with distal alignment for patella alta with recurrent dislocations: an original surgical technique. Orthop Traumatol Surg Res. 2011;97(4)(suppl):S5-S11. [DOI] [PubMed] [Google Scholar]
- 15. Mayer C, Magnussen RA, Servien E, et al. Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta. Am J Sports Med. 2012;40(2):346-351. [DOI] [PubMed] [Google Scholar]
- 16. Otsuki S, Nakajima M, Fujiwara K, et al. Influence of age on clinical outcomes of three-dimensional transfer of the tibial tuberosity for patellar instability with patella alta. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2392-2396. [DOI] [PubMed] [Google Scholar]
- 17. Otsuki S, Nakajima M, Oda S, et al. Three-dimensional transfer of the tibial tuberosity for patellar instability with patella alta. J Orthop Sci. 2013;18(3):437-442. [DOI] [PubMed] [Google Scholar]
- 18. Otsuki S, Okamoto Y, Murakami T, et al. Patellofemoral reconstruction for patellar instability with patella alta in middle-aged patients: clinical outcomes. Orthop Traumatol Surg Res. 2018;104(2):217-221. [DOI] [PubMed] [Google Scholar]
- 19. Paar O, Riederer A. Comparative measurement of retropatellar pressure and contact surface before and after distal repositioning of the tibial tuberosity in patella alta: an experimental study. Article in German. Unfallchirurg. 1988;91(5):229-233. [PubMed] [Google Scholar]
- 20. Redler LH, Meyers KN, Brady JM, Dennis ER, Nguyen JT, Shubin Stein BE. Anisometry of medial patellofemoral ligament reconstruction in the setting of increased tibial tubercle-trochlear groove distance and patella alta. Arthroscopy. 2018;34(2):502-510. [DOI] [PubMed] [Google Scholar]
- 21. Roessler PP, Wimmer MD, Jacobs C, Bornemann R, Stein T, Lahner M. Medial patellofemoral ligament reconstruction fails to correct mild patella alta in cases of patellofemoral instability—a case-control study. Int Orthop. 2019;43(9):2071-2075. [DOI] [PubMed] [Google Scholar]
- 22. Rood A, van Sambeeck J, Koëter S, van Kampen A, van de Groes SAW. A detaching, V-shaped tibial tubercle osteotomy is a safe procedure with a low complication rate. Arch Orthop Trauma Surg. 2020;140(12):1867–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Simmons E, Jr, Cameron JC. Patella alta and recurrent dislocation of the patella. Clin Orthop Relat Res. 1992;274:265-269. [PubMed] [Google Scholar]
- 24. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 25. Stephen JM, Dodds AL, Lumpaopong P, Kader D, Williams A, Amis AA. The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med. 2015;43(9):2198-2207. [DOI] [PubMed] [Google Scholar]
- 26. Tan SHS, Chng KSJ, Lim BY, et al. The difference between cartilaginous and bony sulcus angles for patients with or without patellofemoral instability: a systematic review and meta-analysis. J Knee Surg. 2020;33(3):235–241. [DOI] [PubMed] [Google Scholar]
- 27. Tan SHS, Hui SJ, Doshi C, Wong KL, Lim AKS, Hui JH. The outcomes of distal femoral varus osteotomy in patellofemoral instability: a systematic review and meta-analysis. J Knee Surg. 2020;33(5):504–512. [DOI] [PubMed] [Google Scholar]
- 28. Tan SHS, Ibrahim MM, Lee ZJ, Chee YKM, Hui JH. Patellar tracking should be taken into account when measuring radiographic parameters for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3593-3600. [DOI] [PubMed] [Google Scholar]
- 29. Tan SHS, Lim BY, Chng KSJ, et al. The difference between computed tomography and magnetic resonance imaging measurements of tibial tubercle-trochlear groove distance for patients with or without patellofemoral instability: a systematic review and meta-analysis. J Knee Surg. 2020;33(8):768–776. [DOI] [PubMed] [Google Scholar]
- 30. Tan SHS, Lim SY, Wong KL, Doshi C, Lim AKS, Hui JH. The outcomes of isolated distal realignment procedures in patellofemoral instability: a systematic review and meta-analysis. J Knee Surg. 2020;33(6):547–552. [DOI] [PubMed] [Google Scholar]
- 31. Tan SHS, Tan LYH, Lim AKS, Hui JH. Hemiepiphysiodesis is a potentially effective surgical management for skeletally immature patients with patellofemoral instability associated with isolated genu valgum. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):845-849. [DOI] [PubMed] [Google Scholar]
- 32. Whitehead A. Meta-analysis of Controlled Clinical Trials. John Wiley; 2002. [Google Scholar]
- 33. Yang Y, Zhang Q. Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2599-2607. [DOI] [PubMed] [Google Scholar]