Abstract
(1) Background: Medial sigmoid depression (MSD) of the mandibular ramus is an anatomical variation that resembles non-odontogenic cystic lesion. (2) Aim: The aim of this systematic review was to survey the literature to identify the relevant journal publications, reveal their scientific impact in terms of citations and compare the reported prevalence of MSD. (3) Materials and methods: PubMed, Google Scholar, Scopus and Web of Science were queried to identify relevant publications. The search string was: “medial depression of mandibular ramus” OR “medial depression of the mandibular ramus” OR “medial depression of the mandibular rami” OR “medial depression of mandibular rami” OR “medial sigmoid depression”. (4) Results: Eight studies were identified. Dry mandibles and patient dental panoramic radiographs were evaluated in four and seven of the eight studies, respectively. The prevalence of MSD varied from 20.2% to 82.0%. In male and female patients, the prevalence was 18.3–76.0% and 22.0–64.0%, respectively. MSD tended to occur bilaterally and most prevalent in patients with Angle’s Class II occlusion. The semilunar and triangular shapes were more common than teardrop and circular shapes. The most cited study had 12 citations. (5) Conclusions: MSD was a seldom investigated and cited anatomical variation that was not uncommon. Its recognition should be further promoted.
Keywords: dental radiology, panoramic radiograph, anatomical variation, lesion, radiographic diagnosis, prevalence, diagnostic imaging
1. Introduction
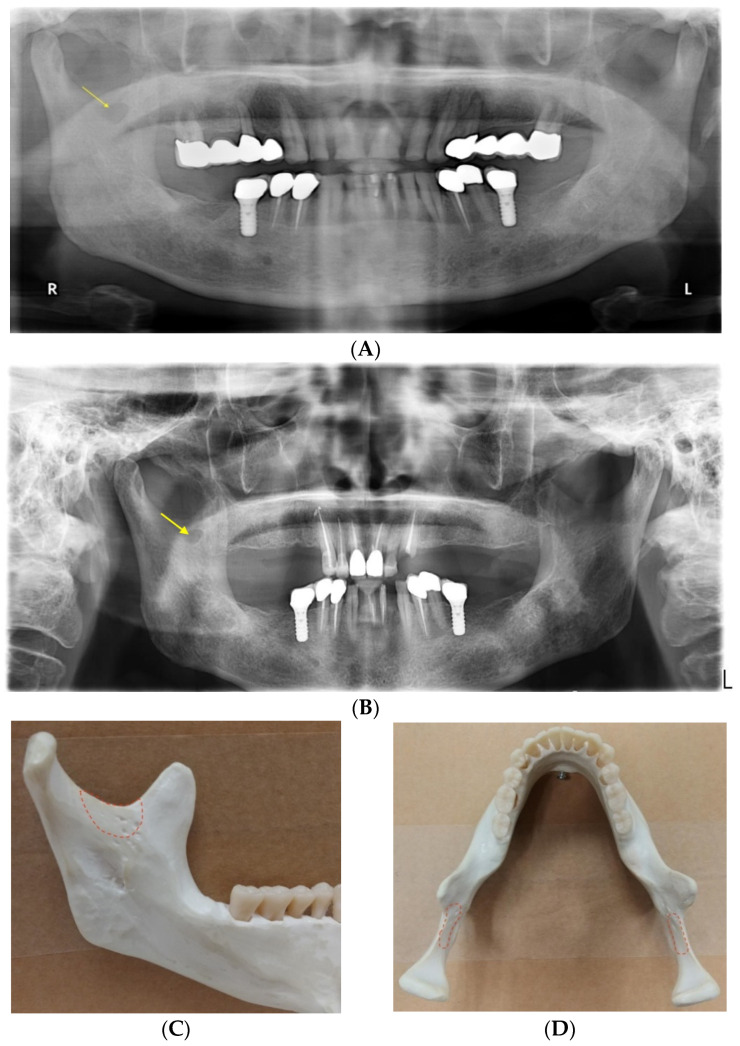
First described by Langlais et al. in 1983, the medial sigmoid depression (MSD) is a concavity located medial to the sigmoid notch of the mandible, present in over half of the evaluated samples [1]. Nearly four decades have lapsed since the publication of this pioneer work in the “Triple O” journal (known as Oral Surgery, Oral Medicine, Oral Pathology at that time). This anatomical entity was not indexed by Terminologia Anatomica and common dental radiology textbooks such as the ones by Whaites and Drage [2], White and Pharaoh [3] and Koenig et al. [4]. On a dental panoramic radiograph, the medial sigmoid depression may present as a radiolucent lesion inferior to the sigmoid notch that may or may not be connected to the latter (Figure 1A). The radiolucency is caused by reduced absorption of radiation due to the thinning of the bone on the lingual side of the sigmoid notch [5] (Figure 1B,C). The shape of MSD can be mainly classified into tear-drop, semilunar, circular and triangular [5]. The radiolucency may resemble a mandibular non-odontogenic cystic lesion that could lead to a dentist referring the patient to receiving additional advanced three-dimensional imaging with increased radiation dose. On the other hand, dentists are much more aware of the Stafne cavity (also known as Stafne cyst, defect or lacuna) that presents as a mandibular bone depression commonly located in the lingual posterior region of the mandible [6]. A common belief is that a hyperplastic or hypertrophic lobe of the major salivary glands may exert pressure upon the cortex of the mandible and result in the focal bone resorption [6]. Because of this mechanism, a Stafne cavity is usually slow-growing and apparent on radiographs of elderly patients. On the contrary, the MSD seemed to be much less recognized by the dental profession. The recognition of this anatomical entity, therefore, may save patients from receiving unnecessary radiation. The aim of this systematic review was to survey the literature to identify the relevant journal publications, reveal their scientific impact in terms of citations and compare the reported prevalence of MSD.
Figure 1.
Dental panoramic radiographs showing a medial sigmoid depression (MSD) on the right side of the mandible, taken in (A) 2012 and (B) 2021, respectively. Its appearance did not change much between two timepoints. A mandible model showing the location where an MSD may be present from the (C) lingual and (D) axial views.
2. Materials and Methods
On 15 March 2021, four literature databases, namely PubMed, Google Scholar, Scopus and Web of Science, were queried. The following phrases were typed into the search string: “medial depression of mandibular ramus” OR “medial depression of the mandibular ramus” OR “medial depression of the mandibular rami” OR “medial depression of mandibular rami” OR “medial sigmoid depression”. These terms were entered in English only. For PubMed, Scopus and Web of Science, the search covered “All fields” instead of limiting to article title, abstract and keywords. All publications returned by the searches were initially included. Exclusion criteria included duplicate publications, irrelevance, no access and no reporting of the prevalence of MSD.
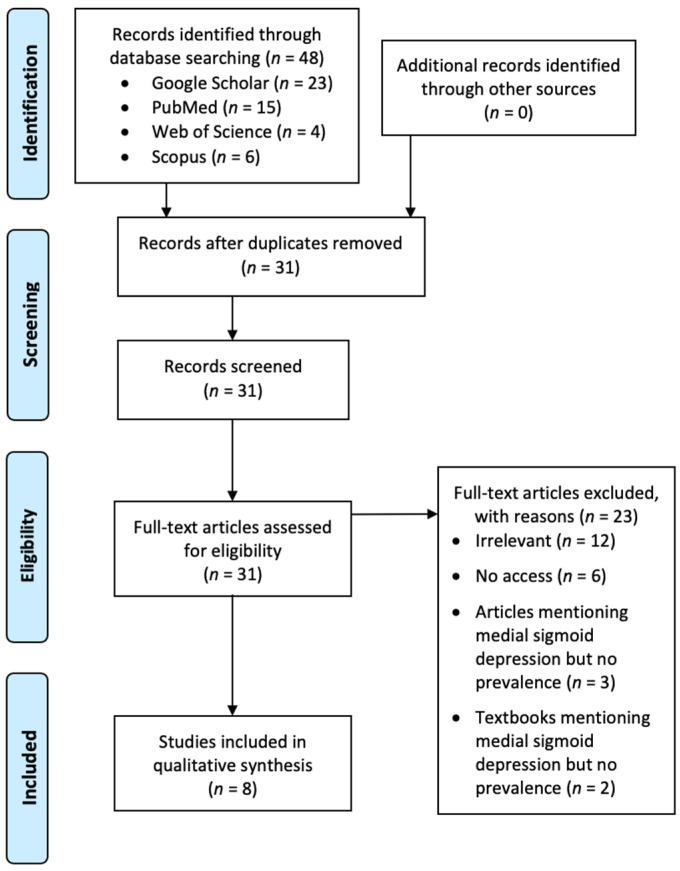
The searches initially returned with 48 publications. After removing duplicates, 31 publications remained. After screening and excluding unsuitable publications with specific reasons, eight studies remained for the review (Figure 2). Each author did the screening independently and a final consensus was reached.
Figure 2.
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart showing the screening process of the literature search.
Ethical approval was not applicable to this review.
3. Results
The eight identified studies are listed in Table 1 [1,5,7,8,9,10,11,12]. The main text of two of them were not written in English, one of which was translated into English successfully by Google Docs [11], whereas the other one had extractable data from the abstract written in English [9]. One study investigated dry mandibles only, four studies investigated panoramic radiographs only and three studies investigated both. The prevalence of MSD varied from 20.2% to 82.0%. In male and female patients, the prevalence was 18.3–76.0% and 22.0–64.0%, respectively. Most studies reported that MSD tended to occur bilaterally. Three studies reported that MSD was most prevalent in patients with Angle’s Class II occlusion (meaning that the maxillary first molar is positioned more anteriorly than normal relative to the mandibular first molar), whereas one study reported that it was most prevalent in Class I occlusion (normal occlusion). The semilunar and triangular shapes were more common than teardrop and circular shapes.
Table 1.
Details of the eight included studies of medial sigmoid depression (MSD).
| Prevalence | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Year | No. of Dry mandibles | No. of Patient Panoramic Radiographs | No. of MSD Reported | MSD | Male | Female | Unilateral MSD 1 | Bilateral MSD 1 | Angle Class I | Angle Class II | Angle Class III | Tear-drop 2 | Semilunar 2 | Circular 2 | Triangular 2 | No. of Citations |
| [11] | 2020 | / | 1000 | 298 | 0.234 | 0.220 | 0.242 | 0.170 | 0.064 | 0.289 | 0.326 | 0.077 | 0.309 | 0 | |||
| [8] | 2019 | 50 | 76 | 0.820 | 0.120 | 0.700 | 0.158 | 0.342 | 0.053 | 0.447 | 1 | ||||||
| 50 | 64 3 | 0.700 | 0.760 | 0.640 | 0.160 | 0.540 | 0.094 | 0.641 | 0.078 | 0.188 | |||||||
| [7] | 2018 | / | 110 | 83 | 0.500 | 0.525 | 0.484 | 0.487 | 0.120 | 0.361 | 0.289 | 0.229 | 2 | ||||
| [12] | 2014 | / | 300 | 106 3 | 0.233 | 0.117 | 0.117 | 0.190 | 0.280 | 0.230 | 0.210 | 0.343 | 0.171 | 0.286 | 3 | ||
| [9] | 2003 | / | 465 | 0.242 4 | 0.389 4 | 0.313 4 | 2 | ||||||||||
| [5] | 2001 | 251 | 118 | 0.339 | 0.131 | 0.208 | 8 | ||||||||||
| 2067 | 586 | 0.202 | 0.183 | 0.220 | 0.120 | 0.082 | 0.124 | 0.329 | 0.321 | 0.200 | 0.314 | 0.089 | 0.397 | ||||
| [10] | 1991 | 78 | / | 0.282 | 0.333 | 2 | |||||||||||
| [1] | 1983 | 88 | 76 | 0.557 | 0.250 | 0.307 | 12 | ||||||||||
| 1986 | 226 | 0.082 | 0.050 | 0.032 | |||||||||||||
1 Prevalence based on the total number of reported patients. 2 Prevalence based on the total number of reported MSD. 3 The study reported conflicting total numbers of MSD in patients. The largest number was listed here. 4 Values computed by simple averaging of data reported for right and left sides for each Class, respectively.
Data from Google Scholar indicated that the most cited paper was Langlais et al. [1] with 12 citations, followed by Carvalho et al. [5] with 8 citations. Other articles had 0–3 citations. No additional suitable paper was identified from these citing papers.
4. Discussion
This systematic review identified eight studies that reported the prevalence of MSD in dry mandibles and dental panoramic radiographs. They reported a wide range of overall prevalence as well as the prevalence in various subgroups according to sex, side of the mandible, Angle’s classification of occlusion and shape. There seemed to be no sex bias in having MSD. All reviewed studies received few citations. Langlais et al. [1] was acknowledged by four of the evaluated studies as the first report of MSD and it was otherwise cited in the introduction by the remaining three studies. Readers should be aware that the highest prevalence of MSD reported from dental panoramic radiographs was 70.0%, implying that MSD may be a commonly observed but seldom investigated anatomical entity. To support the “As Low As Reasonably Achievable” (ALARA) principle of using ionizing radiation [13], dentists and other healthcare workers should be able to recognize MSD on panoramic radiographs, so that unnecessary additional radiographic assessments would not be ordered for patients. Recently, the cone beam computed tomography (CBCT) has been more readily available and popular among dentists as it visualizes the region of interest in three-dimensional manner in high resolution. Its usage in various occasions for diagnosis and treatment planning in dental medicine has been advocated [14]. A thorough understanding of the radiographic anatomy and the radiographic device may avoid unnecessary CBCT examination with increased radiation dose [15,16].
Indeed, MSD was not mentioned in the most common dental radiology textbooks as mentioned in the Introduction. Five of the eight reviewed studies were published in journals without an impact factor. However, other textbooks did mention it, such as Wood and Goaz [17] and William Jr and Merritt [18]. MSD was also briefly mentioned by several other papers in the literature as a potential radiographic finding or a differential diagnosis for other pathologies [19,20,21,22,23]. One common differential diagnosis would be Stafne cavity, which usually occurs at the angle of the mandible below the mandibular canal but can also occur at other locations in the mandible [6]. It should be noted that Stafne cavity had a strong male preponderance [6] but MSD did not. In addition, it could be potentially referred to or discussed with other names, such as pseudocyst in the coronoid process [24] and coronoid foramina or foramen [25,26].
There were some limitations of this review. First, only eight studies were eligible to be reviewed. This small sample of papers might not be enough to obtain a very precise conclusion regarding the prevalence of MSD. Second, there was a wide range of the number of panoramic radiographs examined by the reviewed studies, rendering them not very homogeneous.
5. Conclusions
To conclude, MSD was a seldom investigated and cited anatomical variation. It has a high relevance to oral and maxillofacial radiology and head and neck imaging, as its radiographic appearance resembles a non-odontogenic cystic lesion in the mandible. Its recognition should be further promoted. Based on very limited data available from dry mandible and patient radiographic studies, its prevalence was reported to be from 20.2% to 82.0%.
Acknowledgments
The author thanked Charles Hau, Institute for Advanced Dentistry, Faculty of Dentistry, University of Hong Kong, for an initial discussion on the topic and image provision.
Author Contributions
A.W.K.Y. is responsible for all parts of the work. N.S.M.W. is responsible for study selection and data extraction. Both authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The author declares no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Langlais R.P., Glass B.J., Bricker S.L., Miles D.A. Medial sigmoid depression: A panoramic pseudoforamen in the upper ramus. Oral Surg. Oral Med. Oral Pathol. 1983;55:635–638. doi: 10.1016/0030-4220(83)90385-7. [DOI] [PubMed] [Google Scholar]
- 2.Whaites E., Drage N. Essentials of Dental Radiography and Radiology. Elsevier Health Sciences; Amsterdam, The Netherlands: 2013. [Google Scholar]
- 3.White S., Pharaoh M. Oral Radiology Principles and Interpretation. 5th ed. Mosby; Maryland Heights, MO, USA: 2004. [Google Scholar]
- 4.Koenig L.J., Tamimi D., Petrikowski C.G., Perschbacher S.E. Diagnostic Imaging: Oral and Maxillofacial. Elsevier Health Sciences; Amsterdam, The Netherlands: 2017. [Google Scholar]
- 5.Carvalho I., Damante J., Tallents R., Ribeiro-Rotta R. An anatomical and radiographic study of medial depression of the human mandibular ramus. Dentomaxillofacial Radiol. 2001;30:209–213. doi: 10.1038/sj.dmfr.4600609. [DOI] [PubMed] [Google Scholar]
- 6.Philipsen H., Takata T., Reichart P., Sato S., Suei Y. Lingual and buccal mandibular bone depressions: A review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofacial Radiol. 2002;31:281–290. doi: 10.1038/sj.dmfr.4600718. [DOI] [PubMed] [Google Scholar]
- 7.Adisen M.Z., Okkesim A., Misirlioglu M. A possible association between medial depression of mandibular ramus and maximum bite force. Folia Morphol. 2018;77:711–716. doi: 10.5603/FM.a2018.0026. [DOI] [PubMed] [Google Scholar]
- 8.Asdullah M., Aggarwal A., Khawja K.J., Khan M.H., Gupta J., Ratnakar K. An anatomic and radiographic study of medial sigmoid depression in human mandible. J. Indian Acad. Oral Med. Radiol. 2019;31:123–127. doi: 10.4103/jiaomr.jiaomr_218_18. [DOI] [Google Scholar]
- 9.Dalili Z., Mohtavipour S. Frequency of medial sigmoid depression in panoramic view of orthodontic patients based on facial skeletal classification. J. Guilan Univ. Med Sci. 2003;12:16–23. [Google Scholar]
- 10.Kang B.-C. The Medial Sigmoid Depression: Its Anatomic and Radiographic Considerations. J. Korean Acad. Maxillofac. Radiol. 1991;21:7–13. [Google Scholar]
- 11.Özkan G., Sessiz AK R. Evaluation of the frequency of medial sigmoid depression using panoramic radiographs: A retrospective study. J. Dent. Fac. Atatürk Univ. 2020;20:552–556. [Google Scholar]
- 12.Sudhakar S., Kumar N., Prabhat M., Nalini J. Characteristics of medial depression of the mandibular ramus in patients with orthodontic treatment needs: A panoramic radiography study. J. Clin. Diagn. Res. 2014;8:ZC100–ZC104. doi: 10.7860/JCDR/2014/9869.5192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeung A.W.K. The “As Low As Reasonably Achievable” (ALARA) principle: A brief historical overview and a bibliometric analysis of the most cited publications. Radioprotection. 2019;54:103–109. doi: 10.1051/radiopro/2019016. [DOI] [Google Scholar]
- 14.Yeung A.W.K., Jacobs R., Bornstein M.M. Novel low-dose protocols using cone beam computed tomography in dental medicine: A review focusing on indications, limitations, and future possibilities. Clin. Oral Investig. 2019;23:2573–2581. doi: 10.1007/s00784-019-02907-y. [DOI] [PubMed] [Google Scholar]
- 15.Dave M., Horner K. Challenges in X-ray diagnosis: A review of referrals for specialist opinion. Br. Dent. J. 2017;222:431–437. doi: 10.1038/sj.bdj.2017.264. [DOI] [PubMed] [Google Scholar]
- 16.Harvey S., Ball F., Brown J., Thomas B. ‘Non-standard’ panoramic programmes and the unusual artefacts they produce. Br. Dent. J. 2017;223:248–252. doi: 10.1038/sj.bdj.2017.707. [DOI] [PubMed] [Google Scholar]
- 17.Wood N.K., Goaz P.W. Differential Diagnosis of Oral and Maxillofacial Lesions. Mosby; Maryland Heights, MO, USA: 1997. [Google Scholar]
- 18.William Jr G., Merritt C.R. Reeder and Felson’s Gamuts in Radiology: Comprehensive Lists of Roentgen Differential Diagnosis. Springer Science & Business Media; Amsterdam, The Netherlands: 2006. [Google Scholar]
- 19.Abramovitch K., Langlais R.P., Dolwick M.F. Panoramic radiography for temporomandibular joint arthrography: A description of arthropanoramograms. Oral Surg. Oral Med. Oral Pathol. 1989;67:775–780. doi: 10.1016/0030-4220(89)90023-6. [DOI] [PubMed] [Google Scholar]
- 20.Chudhry A., Sankireddy S. Variants of major salivary gland related bone defects—a case series. Int. J. Maxillofac. Imaging. 2016;2:69–72. [Google Scholar]
- 21.Hisatomi M., Munhoz L., Asaumi J., Arita E.S. Parotid mandibular bone defect: A case report emphasizing imaging features in plain radiographs and magnetic resonance imaging. Imaging Sci. Dent. 2017;47:269–273. doi: 10.5624/isd.2017.47.4.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miles D.A. Clinical Experience with Cone-beam Volumetric Imaging—Report of Findings in 381 Cases. Comput. Tomogr. 2005;20:416–424. [Google Scholar]
- 23.Miles D.A. Interpreting the cone beam data volume for occult pathology. Semin. Orthod. 2009;15:70–76. doi: 10.1053/j.sodo.2008.09.009. [DOI] [Google Scholar]
- 24.Clark M.J., McAnear J.T. Pseudocyst in the coronoid process of the mandible. Oral Surg. Oral Med. Oral Pathol. 1984;57:231. doi: 10.1016/0030-4220(84)90219-6. [DOI] [PubMed] [Google Scholar]
- 25.Subhan N.F.C. Bilateral ‘coronoid foramina’with accessory foramina on the ‘lateral aspect of ramus’ of mandible: An unseen variance discovery in humans. Surg. Radiol. Anat. 2018;40:641–646. doi: 10.1007/s00276-018-1984-6. [DOI] [PubMed] [Google Scholar]
- 26.Firdoose N. Concurrent ‘coronoid foramen’with trifid mandibular canal in a live human: CBCT exploration of a unilateral variant. Eur. J. Anat. 2020;24:229–234. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.