Abstract
The new coronavirus emergency spread to Italy when little was known about the infection’s impact on mothers and newborns. This study aims to describe the extent to which clinical practice has protected childbirth physiology and preserved the mother–child bond during the first wave of the pandemic in Italy. A national population-based prospective cohort study was performed enrolling women with confirmed SARS-CoV-2 infection admitted for childbirth to any Italian hospital from 25 February to 31 July 2020. All cases were prospectively notified, and information on peripartum care (mother–newborn separation, skin-to-skin contact, breastfeeding, and rooming-in) and maternal and perinatal outcomes were collected in a structured form and entered in a web-based secure system. The paper describes a cohort of 525 SARS-CoV-2 positive women who gave birth. At hospital admission, 44.8% of the cohort was asymptomatic. At delivery, 51.9% of the mothers had a birth support person in the delivery room; the average caesarean section rate of 33.7% remained stable compared to the national figure. On average, 39.0% of mothers were separated from their newborns at birth, 26.6% practised skin-to-skin, 72.1% roomed in with their babies, and 79.6% of the infants received their mother’s milk. The infants separated and not separated from their SARS-CoV-2 positive mothers both had good outcomes. At the beginning of the pandemic, childbirth raised awareness and concern due to limited available evidence and led to “better safe than sorry” care choices. An improvement of the peripartum care indicators was observed over time.
Keywords: birth, breastfeeding, COVID-19, perinatal care, pregnancy, SARS-CoV-2
1. Introduction
After its first recognition in China in December 2019, the new coronavirus emergency spread to Italy when little was known about the infection’s impact on mothers and newborns. Since April 2020, the leading international agencies, health authorities, and obstetrics and gynecology societies unanimously recommended the delivery mode must not be influenced by COVID-19 disease unless the woman’s respiratory conditions required urgent delivery [1,2,3,4]. Moreover, during labour and delivery, a support person’s presence had to be guaranteed and patients and healthcare workers had to use appropriate personal protective equipment during all interactions [3,4]. Skin-to-skin contact, rooming-in, and breastfeeding were all recommended practices unless the mother was acutely ill as the benefits outweigh the potential risks of SARS-CoV-2 transmission and subsequent development of COVID-19 [1,2,3,4]. Mother and baby separation was not advised, and the lack of presence of one’s partner during labour and delivery was found to predict postpartum women’s mental health in some studies conducted in Italy [5]. Currently, however, protecting childbirth physiology and preserving the mother–child bond during the COVID-19 pandemic is still a global challenge.
At the beginning of the pandemic, the Italian Obstetric Surveillance System (ItOSS) launched a national population-based prospective study [6,7], enrolling any woman with confirmed SARS-CoV-2 infection admitted to a hospital in the country. The present study aims to describe to what extent clinical practice was able to protect childbirth physiology and preserve the mother–child bond during the first wave of the COVID-19 pandemic in Italy.
2. Materials and Methods
This was a national population-based prospective cohort study enrolling all pregnant women with confirmed SARS-CoV-2 infection admitted to any Italian hospital for childbirth. Diagnosis required confirmation by reverse transcriptase polymerase chain reaction testing for the SARS-CoV-2 virus through a nasopharyngeal swab. Women aged <18 or unable to give informed consent or who refused to participate were excluded from the study.
The present analysis refers to the pandemic’s first wave, defined as the time frame between 25 February and 31 July 2020. From 25 February, the date of the first Italian obstetric case notification, until the end of March 2020, only symptomatic pregnant women and those defined as close contacts of a SARS-CoV-2 infected person were routinely tested. In April, the Italian regions progressively adopted universal screening policies, and as of May 2020, all pregnant women admitted to any Italian maternity were screened for SARS-CoV-2, regardless of symptoms and exposure.
Data on maternal characteristics, peripartum care (mother–newborn separation, skin-to-skin contact, breastfeeding, and rooming-in), and maternal and perinatal outcomes were collected through a structured online form and entered in a web-based secure system by trained reference clinicians from the participating maternity hospitals (Supplementary Materials).
Informed consent to participate in the study was acquired from any woman at study enrolment. The incidence rate of the SARS-CoV-2 infection with a 95% confidence interval was estimated at a national level and by geographical area. National denominator estimates were based on the 2018 National Birth Registry data, retrieved assuming an annual reduction in births of 3%. Data analysis, performed at the Italian National Health Institute (INHI) using the Statistical Package Stata/MP 14.2, focused on descriptive statistics.
3. Results
The infection estimated incidence rate among women who gave birth between 25 February and 31 July 2020 was 3.2/1000 deliveries at a national level, 5.9/1000 in the North, 1.6/1000 in the Centre, and 0.4/1000 in the South of the country.
The data analysis includes 525 women who gave birth with confirmed SARS-CoV-2 infection, of which 44.8% were asymptomatic. Table 1 shows the women’s socio-demographic and obstetric characteristics. Women’s mean age is 31.8 years (SD = 5.69); almost a quarter of the cohort has foreign citizenship, and over 60% is multipara.
Table 1.
Women’s socio-demographic and obstetric characteristics (n = 525).
| Characteristics | n | % |
|---|---|---|
| Maternal age (3 missing) | ||
| <30 | 169 | 32.4 |
| 30–34 | 180 | 34.5 |
| ≥35 | 173 | 33.1 |
| Citizenship | ||
| Not Italian | 125 | 23.8 |
| Italian | 400 | 76.2 |
| Country of birth | ||
| Italy and Western Europe | 368 | 70.1 |
| Eastern Europe | 34 | 6.5 |
| Africa | 49 | 9.3 |
| South/Central America | 37 | 7 |
| Asia | 37 | 7 |
| Parity (11 missing) | ||
| Nulliparae | 187 | 36.4 |
| Multiparae | 327 | 63.6 |
| Multiple pregnancies | ||
| No | 508 | 96.8 |
| Yes | 17 | 3.2 |
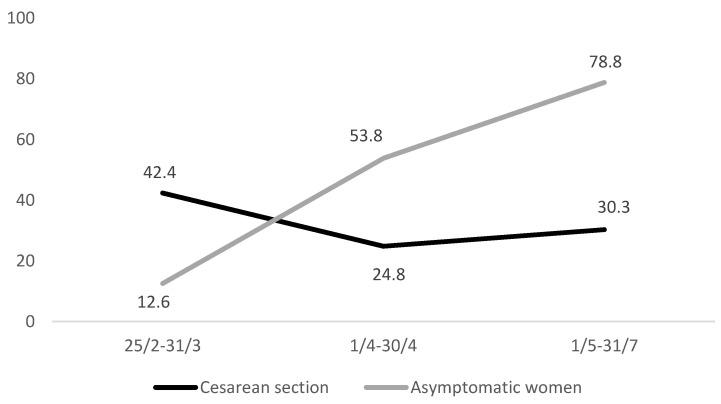
During labour, 95% of the women wore a surgical mask. At delivery, 51.9% of the mothers had a birth support partner in the delivery room. The average caesarean section (CS) rate was 33.7%; elective CS was performed in 15.4% of the cases; urgent/emergency CS due to maternal or foetal indications was performed in 15%; urgent/emergency CS due to COVID-19 was performed in 3.3% of the cases. Figure 1 shows how the sharp increase in asymptomatic women detected over the study period corresponds to a downward trend of CS, describing the reliable estimates over time.
Figure 1.
Temporal trend of caesarean section and percentage of asymptomatic women.
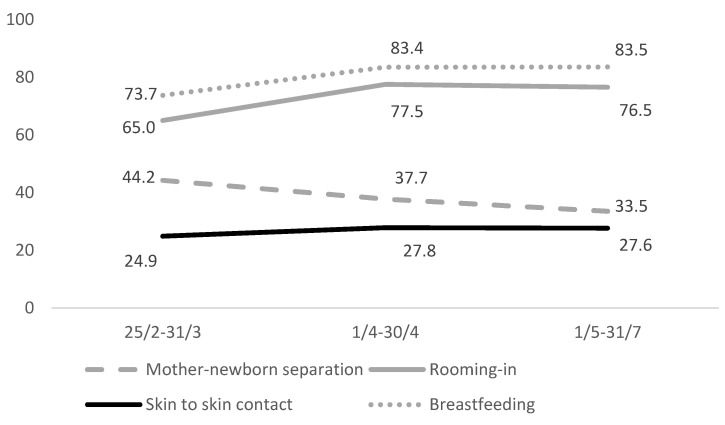
During the hospital stay, on average, 39% of the mothers were separated from their newborns at birth; 26.6% practised skin-to-skin contact; 72.1% were able to room in with their babies; and 79.6% of the infants received their mother’s milk, 69% by direct breastfeeding and 10.6% by pumping or expressing breastmilk. Figure 2 shows an overall improvement of the peripartum assistance indicators over time.
Figure 2.
Temporal trend of peripartum care indicators.
During the first pandemic wave, 20.8% of women who gave birth had COVID-19 pneumonia, 3.8% received invasive ventilation, and 2.7% were admitted to the intensive care unit. Four stillbirths and no maternal or neonatal deaths were recorded. Out of 538 newborns, 12 (2.2%) developed severe morbidity, namely seven acute respiratory distress syndromes, one interstitial pneumonia, two perinatal infections, one acute drug reaction, and one hyaline membrane disease. Eighty-six percent of the newborns weighed ≥2500 g, and the median Apgar index was 9 at 1 min and 10 at 5 min. Eighteen newborns (3.4%) tested positive for SARS-CoV-2 after birth, 10 within 24 h of life. Six of the eighteen positive newborns were delivered by women with COVID-19 pneumonia. Only one positive infant requested intensive care admission due to acute respiratory distress syndrome, reporting a good outcome. Infants born to SARS-CoV-2 infected mothers registered favourable outcomes, regardless of whether early mother–child separation had occurred or not.
4. Discussion
The paper describes the first 525 pregnant women positive for SARS-CoV-2 who gave birth in Italy from the beginning of the epidemic to 31 July 2020. ItOSS was strategic in allowing timely population-based data collection, thanks to the availability of a consolidated network monitoring maternal mortality and severe morbidity in the country [8,9]. The detected disparities in incidence across Italian regions were due to the dynamics of the infection’s spread, which affected almost exclusively the northern regions during the first wave. The socio-demographic and obstetric characteristics of the women enrolled in the study (Table 1) did not present significant differences with the reference population of women who gave birth in the northern Italian regions in 2019 [10,11], except for an increased proportion of multiparous women probably related to the easier circulation of the virus in families with children. The maternal and neonatal outcomes detected by the study described a mild COVID-19 disease; 3% of women required intensive care, and 2% of newborns developed severe morbidity without any maternal and neonatal death.
Although the World Health Organization (WHO) recommended not exceeding the threshold of 9–16% of CS even in high-income countries [12], according to the most recent Euro-Peristat figures, CS rates in Europe ranged from 14.8 to 52.2% [13]. In 2018, Italy reported a national CS rate of 32.3%, with significant interregional variations, ranging between 20% in the North and 53% in the South of the country [14]. At the beginning of the pandemic, CS was frequently performed in COVID-19 positive women with compromised clinical and respiratory conditions. The downward CS trend shown in Figure 1 was likely due to better ascertainment of asymptomatic women over time; the slight rise during the last three months was attributable to the cases notified from the southern Italian regions, which had steadily higher CS rates compared to the northern regions [14]. Despite the long-standing elevated CS rates in Italy, the ItOSS study showed lower percentages than those recorded in other countries during the first wave of the COVID-19 pandemic [15,16,17]. In China, almost all women underwent CS; all newborns were separated from their mothers, and none were breastfed [15]. Between February and April 2020, the United Kingdom tested only symptomatic pregnant women, and 59% of those with confirmed SARS-CoV-2 infection delivered by CS [16] compared to a national CS rate of 30% in 2019 [18]. The living systematic review and meta-analysis by Allotey and colleagues [17] estimated a proportion of 65% CS (95% confidence interval 0.57–0.73), corresponding to previous findings.
According to the ItOSS data, skin-to-skin contact seemed to be the most neglected practice in early newborn care during the COVID-19 pandemic, showing a stably very low rate over time, although it is known to improve infant physiology and odds of successful breastfeeding while reducing neonatal morbidity [2,3]. The improved promotion of the mother–child bond observed over time was probably due to identifying all asymptomatic women. However, it may also result from a growing body of evidence suggesting the importance of supporting the protection of childbirth physiology in SARS-CoV-2 positive women. Advancements in organisational aspects of care might also have impacted, and shortage of health personnel and insufficient personal protective equipment should be considered when interpreting these data. Perinatal care has effectively been a challenge for health services already engaged in tackling the emergency, especially during the first months of the pandemic, when the ItOSS data collection started.
In line with the evidence stating that continuous support during labour may reduce medical interventions and improve outcomes for women and infants [19], before the pandemic Italian mothers used to share their delivery experience with a support person. During the pandemic’s first wave, women with confirmed SARS-CoV-2 infection, suspected cases, and sometimes even women not affected by the virus too often gave birth alone in the name of “safety” and were separated from their babies in the name of “precaution”. Instead, some Italian studies have successively suggested that the lack of presence of one’s partner during labour and delivery might predict its impact on postpartum women’s mental health well-being [5,20]. Even though definitive evidence showing that early separation improves neonatal outcomes is still lacking, the short- and long-term benefits of bonding and breastfeeding are universally recognised [2,3]. Available evidence shows that COVID-19 perinatal transmission is unlikely to occur if correct hygiene measures are undertaken and that rooming-in and direct breastfeeding are safe procedures [1,2,3,4,6]. Labour and delivery care policy modifications implemented in a US maternity unit successfully protected pregnant women and healthcare providers from COVID-19, without registering worse outcomes for mothers and newborns [21]. Moreover, separation during the maternity stay may delay but not prevent infection once the infant is discharged, as viral shedding from the mother or other household members may occur after returning home. How can we forget the terrible consequences of the recommendation to replace breastfeeding with formula feeding during the HIV epidemic [22]?
In a comment, Ryan M. Antiel wrote: “The isolation we have experienced during the current pandemic has refocused our attention on the tendency of modern medicine to isolate individual patients” [23]. Let us try to do our best to remember that birth requires a participatory environment where mothers are the conductors and health professionals the musicians.
5. Conclusions
At the beginning of the pandemic, childbirth raised awareness and concern. The limited available evidence surrounding pregnancy, labour, and delivery understandably led to “better safe than sorry” care choices and policies. Today, however, the evidence shows that respecting physiology in women with confirmed or suspected SARS-CoV-2 infection during labour and delivery secures good maternal and neonatal outcomes and avoids unnecessary CS, early mother–infant separation, and formula feeding unless the severity of the women’s clinical conditions requires such decisions [3]. The detailed information on early newborn care reported in the paper is an original and helpful contribution supporting childbirth physiology protection during the COVID-19 pandemic. It is hoped that these data, together with the available evidence on the protective effect of the mother–child relationship, will support health professionals in developing a more assertive positive attitude towards natural birth practices and drive decision-makers and professional organisations to manage appropriately both the subsequent waves of the COVID-19 pandemic and future similar emergencies.
Acknowledgments
We thank Silvia Andreozzi and Mauro Bucciarelli for their valuable technical support and assistance in the operation of the web-based data collection system. We thank Francesca Conway for language editing. Our heartfelt thanks go to all the clinicians working in the national network of maternity units (Supplementary Materials) for the assistance offered to women and for collecting the data. We thank all women who agreed to participate in the study.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18084244/s1.
Author Contributions
Conceptualization, methodology, supervision, project administration, and writing—original draft preparation, S.D.; investigation, data curation, and writing—review and editing, E.C.; for-mal analysis, data curation, and writing—review and editing, M.A.S.; methodology, formal analysis, data curation, and writing—review and editing, A.M. (Alice Maraschini); supervision and writ-ing—review and editing, S.B., P.C., I.C. (Ilaria Cataneo), I.C. (Irene Cetin), P.D., G.D., E.D.A., E.F., S.F., M.P.F., G.G., E.I., L.L., M.L. (Marco Liberati), S.L., M.L. (Mariavittoria Locci), L.M., C.M., G.M., F.M., A.M. (Alessandra Meloni), A.D.M., L.P., E.P. (Edda Pellegrini), F.P. (Francesca Perotti), E.P. (Enrica Perrone), F.P. (Federico Prefumo), L.R., R.R., V.S., S.C.A.S., D.S., S.S., A.S., M.S., S.T., G.T., R.T., V.T., P.V. and S.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the INHI (Prot. 0010482 CE 01.00, Rome 24 March 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Clinical Management of COVID-19. Interim Guidance 27 May 2020 WHO/2019-nCoV/Clinical/2020.5. World Health Organization; Geneva, Switzerland: 2020. [(accessed on 11 April 2021)]. Available online: https://apps.who.int/iris/bitstream/handle/10665/332196/WHO-2019-nCoV-clinical-2020.5-eng.pdf?sequence=1&isAllowed=y. [Google Scholar]
- 2.UNICEF UK Baby-Friendly Hospital Initiative Infant Feeding during the COVID-19 Outbreak. [(accessed on 23 March 2021)]; UNICEF UK. Published 2020. Updated 10 July 2020. Available online: https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2020/04/Unicef-UK-Baby-Friendly-Initiative-statement-on-infant-feeding-during-the-Covid-19-outbreak.pdf.
- 3.Royal College of Obstetricians and Gynaecologists, Royal College of Midwives, Royal College of Paediatrics and Child Health, Public Health England and Health Protection Scotland Coronavirus (COVID-19) Infection in Pregnancy. [(accessed on 11 April 2021)];2020 Information for Healthcare Professionals. [Version 13: Published Friday 19 February 2021] Available online: https://www.rcog.org.uk/globalassets/documents/guidelines/2021-02-19-coronavirus-covid-19-infection-in-pregnancy-v13.pdf.
- 4.Narang K., Ibirogba E.R., Elrefaei A., Trad A.T.A., Theiler R., Nomura R., Picone O., Kilby M., Escuriet R., Suy A., et al. SARS-CoV-2 in Pregnancy: A Comprehensive Summary of Current Guidelines. J. Clin. Med. 2020;9:1521. doi: 10.3390/jcm9051521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molgora S., Accordini M. Motherhood in the Time of Coronavirus: The Impact of the Pandemic Emergency on Expectant and Postpartum Women’s Psychological Well-Being. Front. Psychol. 2020;11:567155. doi: 10.3389/fpsyg.2020.567155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maraschini A., Corsi E., Salvatore M.A., Donati S., ItOSS COVID-19 Working Group Coronavirus and birth in Italy: Results of a national population-based cohort study. Ann. Ist. Super. Sanita. 2020;56:378–389. doi: 10.4415/ANN_20_03_17. [DOI] [PubMed] [Google Scholar]
- 7.Corsi E., Maraschini A., Perrone E., Salvatore M.A., D’Aloja P., Donati S., Gruppo di lavoro ItOSS COVID-19 La preparedness dell’Italian obstetric surveillance system in occasione della pandemia da SARS-CoV-2: Aspetti metodologici di uno studio di popolazione [The preparedness of the Italian obstetric surveillance system in the response to the emergency of the SARS-CoV-2 pandemic: Methodological aspects of a population-based study] Epidemiol. Prev. 2020;44:81–87. doi: 10.19191/EP20.5-6.S2.089. [DOI] [PubMed] [Google Scholar]
- 8.Donati S., Maraschini A., Lega I., D’Aloja P., Buoncristiano M., Manno V., Regional Maternal Mortality Working Group Maternal mortality in Italy: Results and perspectives of record-linkage analysis. Acta. Obstet. Gynecol Scand. 2018;97:1317–1324. doi: 10.1111/aogs.13415. [DOI] [PubMed] [Google Scholar]
- 9.Maraschini A., Lega I., D’Aloja P., Buoncristiano M., Dell’Oro S., Donati S., Regional Obstetric Surveillance System Working Group Women undergoing peripartum hysterectomy due to obstetric hemorrhage: A prospective population-based study. Acta. Obstet. Gynecol. Scand. 2020;99:274–282. doi: 10.1111/aogs.13727. [DOI] [PubMed] [Google Scholar]
- 10.Campi R., Cartabia M., Miglio D., Bonati M. Certificato di Assistenza al Parto (CedAP)—Regione Lombardia—Analisi dell’evento nascita anno 2017 Laboratorio per la Salute Materno Infantile, Dipartimento di Salute Pubblica, IRCCS—Istituto di Ricerche Farmacologiche Mario Negri Milano: Lombardia Region 2019 [The certificate of delivery care (CeDAP)—Lombardy Region—Year 2017] [(accessed on 23 March 2021)]; Available online: www.dati.lombardia.it/dataset/Rapporto-Cedap/v74r-mqr5.
- 11.Perrone E., Formisano D., Gargano G., Battaglia S., Di Mario S., Basevi V. La nascita in Emilia-Romagna—17° Rapporto sui dati del Certificato di Assistenza al Parto (CeDAP)—Anno 2019 [Birth in Emilia-Romagna—Report on the Data of the Certificate of Delivery Care (CeDAP)—Year 2019] [(accessed on 11 April 2021)]; Available online: https://salute.regione.emilia-romagna.it/siseps/sanita/cedap/documentazione/pubblicazioni.
- 12.Betran A.P., Torloni M.R., Zhang J., Ye J., Mikolajczyk R., Deneux-Tharaux C., Oladapo O.T., Souza J.P., Tunçalp Ö., Vogel J.P., et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod. Health. 2015;12:57. doi: 10.1186/s12978-015-0043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacFarlane A.J., Blondel B., Mohangoo A.D., Cuttini M., Nijhuis J., Novak Z., Ólafsdóttir H.S., Zeitlin J., Euro-Peristat Scientific Committee Wide differences in mode of delivery within Europe: Risk-stratified analyses of aggregated routine data from the Euro-Peristat study. BJOG. 2016;123:559–568. doi: 10.1111/1471-0528.13284. [DOI] [PubMed] [Google Scholar]
- 14.Ministero della Salute-Direzione Generale della digitalizzazione, del sistema informativo sanitario e della Statistica—Ufficio di Statistica Certificato di assistenza al parto (CeDAP) [(accessed on 11 April 2021)]; Analisi dell’evento nascita—2018 [Certificates of delivery care (CeDAP)—Year 2017] Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_3034_allegato.pdf.
- 15.Yan J., Guo J., Fan C., Juan J., Yu X., Li J., Feng L., Li C., Chen H., Qiao Y., et al. Coronavirus disease 2019 in pregnant women: A report based on 116 cases. Am. J. Obstet. Gynecol. 2020;223:111.e1–111.e14. doi: 10.1016/j.ajog.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knight M., Bunch K., Vousden N., Morris E., Simpson N., Gale C., O’Brien P., Quigley M., Brocklehurst P., Kurinczuk J.J. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in the UK: National population based cohort study. BMJ. 2020;369:m2107. doi: 10.1136/bmj.m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allotey J., Stallings E., Bonet M., Yap M., Chatterjee S., Kew T., Debenham L., Llavall A.C., Dixit A., Zhou D., et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.NHS—UK Maternity Services Monthly Statistics January 2019, Experimental Statistics. [(accessed on 11 April 2021)]; Available online: https://digital.nhs.uk/data-and-information/publications/statistical/maternity-services-monthly-statistics/january-2019.
- 19.Bohren M.A., Hofmeyr G.J., Sakala C., Fukuzawa R.K., Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst. Rev. 2017;7:CD003766. doi: 10.1002/14651858.CD003766.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fumagalli S., Ornaghi S., Borrelli S., Vergani P., Nespoli A. The experiences of childbearing women who tested positive to COVID-19 during the pandemic in northern Italy. Women Birth. 2021 doi: 10.1016/j.wombi.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greene N.H., Kilpatrick S.J., Wong M.S., Ozimek J.A., Naqvi M. Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM. 2020;2:100234. doi: 10.1016/j.ajogmf.2020.100234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young S.L., Mbuya M.N., Chantry C.J., Geubbels E.P., Israel-Ballard K., Cohan D., Vosti S.A., Latham M.C., Latham M.C. Current knowledge and future research on infant feeding in the context of HIV: Basic, clinical, behavioral, and programmatic perspectives. Adv. Nutr. 2011;2:225–243. doi: 10.3945/an.110.000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antiel R.M. Oedipus and the Coronavirus Pandemic. JAMA. 2020;323:2231–2232. doi: 10.1001/jama.2020.8594. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.