Abstract
Relapsing polychondritis (RP) is a multisystemic rheumatic disease characterized by widespread and potentially destructive inflammatory lesions of the cartilage. The rarity of this disease and the lack of pathological diagnostic laboratory tests can occasionally lead to delayed diagnosis. We herein describe a 51-year-old woman with RP. She was sent to our hospital 4 days after the development of an upper respiratory tract infection with difficulty breathing. Her clinical condition significantly improved after the performance of extracorporeal membrane oxygenation support in an awake state, implantation of a tracheal stent, and administration of steroid therapy. Airway involvement of RP may be life-threatening. In this case, endotracheal intubation would have undoubtedly been very dangerous. Extracorporeal membrane oxygenation can be performed in an awake state to maintain oxygenation and improve the chance of survival.
Keywords: Relapsing polychondritis, extracorporeal membrane oxygenation, tracheal stent, tracheal stenosis, steroid therapy, case report
Background
Relapsing polychondritis (RP) is a rare multisystemic disease characterized by recurrent inflammation and destruction of cartilage tissue. The fatality rate of RP increases significantly once the airway becomes involved. Because its initial symptoms are atypical, RP is often misdiagnosed as asthma or chronic obstructive pulmonary disease in the early stages. We herein present a case in which a patient developed severe RP-induced airway stenosis that was further complicated by serious respiratory failure. The patient consented to tracheal stent implantation under extracorporeal membrane oxygenation (ECMO) support.
Case presentation
A 51-year-old woman with a history of asthma presented to the hospital after having experienced dyspnea and chest distress for 3 days after long-distance travel. The physician diagnosed her with an acute asthma attack. However, after treatment with inhaled corticosteroid and long-acting beta-agonist therapy, her symptoms did not improve and instead continued for a further 2 days.
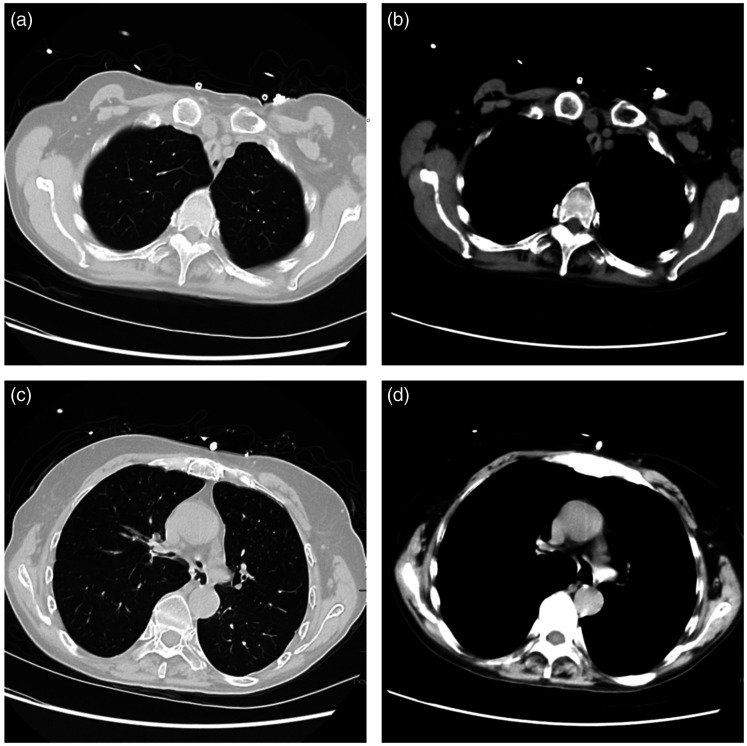
A chest computed tomography scan revealed tracheal stenosis from the glottis to above the carina, with a length of 8.5 cm and anteroposterior diameter of 1 to 2 mm (Figure 1(a)–(d)). There was no evidence of pneumonia. Physical examination revealed saddle-nose deformity and auricular chondritis (Figure 2), and the patient was diagnosed with RP based on McAdam’s criteria (respiratory tract chondritis, nasal chondritis, and auricular chondritis).1 The respiratory physician recommended methylprednisolone at 40 mg once a day, but the patient’s symptoms did not improve with this treatment.
Figure 1.
(a–d) Chest computed tomography showed narrowing of the whole main bronchus, blockage of the lobe bronchus, narrowing of the left and right main bronchus, and increased air volume of both lungs.
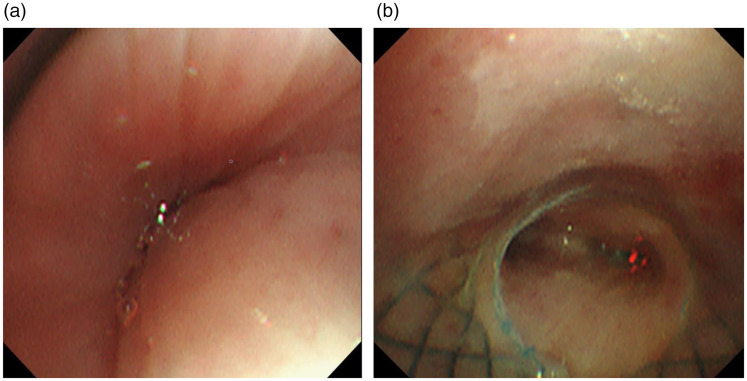
Figure 2.
(a) Endoscopic view of tracheal stricture. (b) Bronchoscopic imaging after esophageal stenting.
The patient was provided with a mask for oxygen inhalation, and arterial blood gas analysis revealed a pH of 7.21, pCO2 of 72.6 mmHg, pO2 of 56 mmHg, and pO2/PaO2 of <150. The patient was subsequently admitted to the intensive care unit.
The patient’s symptoms of dyspnea, especially coughing, worsened during her hospital stay; her lowest pO2/PaO2 was <100. After a consultation, the multidisciplinary team, including respiratory physicians and anesthesiologists, stated that the patient was at significantly high risk of requiring an artificial airway. Because airway stenosis can quickly become irreversible, the physicians decided to perform ECMO without artificial airway support because the patient was conscious. This was performed to prevent respiratory failure and prepare the patient for further treatment by placement of an airway stent.
Veno-venous (V-V) ECMO catheterization was conducted after shallow sedation with dexmedetomidine and local anesthesia with lidocaine. At initiation of ECMO, the mode was V-V, the intubation sites were the right femoral vein and right internal jugular vein, and the tube sizes were 16F and 22F, respectively. After the operation, the pCO2 was adjusted to 45 to 55 mmHg and the SpO2 was adjusted to >96%, upon which the patient’s symptoms drastically improved.
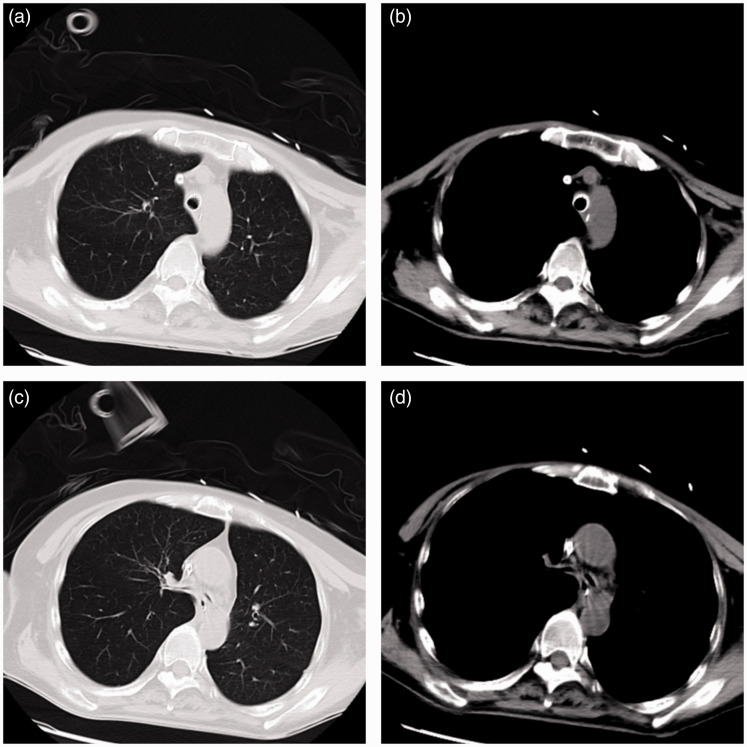
The stent for the main trachea was placed while the patient was under anesthesia on her 5th day in the intensive care unit. Implantation of a silicone airway stent was initially attempted, but this was unsuccessful because the patient had serious glottic edema and a rigid bronchoscope could not be used. A metal bare stent (diameter, 18 mm; length, 50 mm; MicroPort, Shanghai, China) was then placed in the airway (Figure 3(a)–(d)). After implantation of the stent, the patient began to use the ventilator. A combination of local and systemic hormone therapy was adopted, and a bronchoscopy test revealed that the left and right sides of the main bronchus were patent (Figure 4). Meanwhile, the ventilator revealed that the tidal volume was 331 to 384 mL.
Figure 3.
(a–d) After the tracheal stent was implanted, the main bronchus stenosis resolved; however, the left and right main bronchus remained stenotic.
Figure 4.
After the tracheal stent was implanted, the main bronchus stenosis resolved.
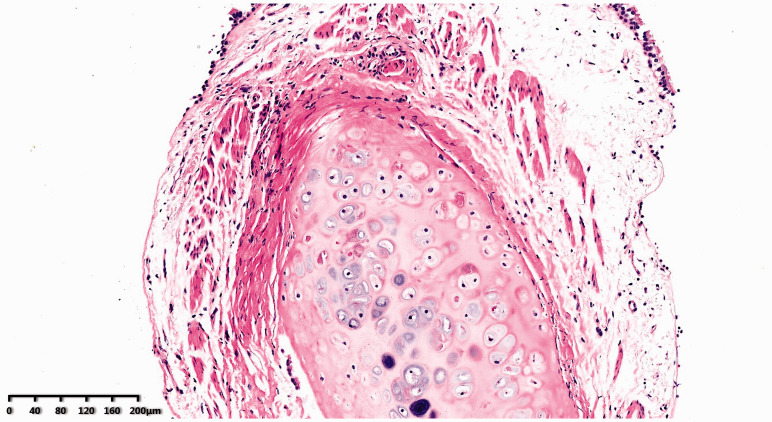
Pathological examination showed proliferation of fibrous tissue close to the periphery of the cartilage with a small amount of inflammatory cell infiltration and mild cartilage degeneration (Figure 5).
Figure 5.
Microscopic examination revealed proliferation of fibrous tissue close to the periphery of the cartilage with a small amount of inflammatory cell infiltration and mild cartilage degeneration.
On the 9th day in the intensive care unit, the patient was weaned from ECMO support. Because the patient’s tracheal lesion was severe, the methylprednisolone dosage was gradually reduced to 20 mg daily during her hospital stay. After discharge, prednisone was recommended at a dose of 10 mg with adjustment at the outpatient service.
Discussion
Because of better management of RP-related complications, the survival rate of patients with RP reportedly improved from 55% in 1986 to 94% in 1998.2 However, the mortality rate remains high in patients with airway involvement. About 50% of patients may experience airway involvement and 20% may experience upper airway collapse, which can involve the cartilage of both the upper and lower airways.3,4
Tracheal stent implantation is an effective surgical treatment for preserving airway patency in patients with tracheal stenosis due to RP.5,6 Silicone stents are preferred for patients with mild tracheal stenosis. The tracheal stenosis in the present case was severe, and a silicone stent could not be implanted because of the rigid bronchial tube. However, a metal stent was easily placed without dislodgement or shifting. Tracheal stent implantation can be considerably difficult and dangerous in patients with severe airway stenosis caused by RP. For tracheal stenosis as serious as that in the present case, artificial airway establishment is highly dangerous; in such cases, acute respiratory failure caused by asphyxia can be avoided by using ECMO.7 Previous research has indicated that ECMO can successfully assist patients with RP in terms of airway repair.8 Notably, the serious airway stenosis in the present case is considerably rare in clinical practice.
In general, patients with early-stage airway stenosis exhibit no obvious symptoms. In the present case, the computed tomography scan showed significant stenosis, which was visible from the epiglottis down to the left and right principal bronchi, in addition to significant respiratory failure. After consultations with relevant specialists, and considering the infeasibility of endotracheal intubation, an unconventional ECMO method was adopted for treatment.
When a patient is conscious, general anesthesia may result in respiratory depression or suffocation. For this reason, the ECMO catheterization was performed under local anesthesia in the present case. To prevent an emergency situation, Arrow catheters (Teleflex, Wayne, PA, USA) were indwelt beforehand in the femoral vein and femoral artery for rapid veno-arterial ECMO. Fortunately, the V-V ECMO catheterization process was smooth and no emergency occurred.
In our institution, the emergency plan for patients with airway stenosis considers preventive retention of vascular access to prevent sudden cardiac and respiratory arrest during catheterization. Currently, there is no reference regarding whether ECMO should be used as a preventive measure in airway treatments for patients with airway stenosis. Numerous articles have reported that early prophylactic ECMO catheterization can successfully prevent sequelae9,10; however, there is a scarcity of high-quality studies at the present time.
At the time of this writing, glucocorticoids were the only drugs that had been approved for RP treatment.11 High doses of intravenous methylprednisolone may be necessary for treatment of acute respiratory distress. Glucocorticoids are used to control acute airway flare-ups and reduce their severity, duration, and frequency. In the present case, the patient had received long-term inhalation and intravenous injection of glucocorticoids before the disease was confirmed, but this treatment was ineffective. We consider that this might be attributed to the excessively low dose of glucocorticoids administered. Immunosuppressants (e.g., methotrexate, cyclophosphamide, and cyclosporine A) are mainly applicable for patients with hormone resistance or intolerance and in those who develop relapse after hormone discontinuation.12 If the aforementioned drugs are combined during tracheal stent placement in a patient with RP, there is a high risk of secondary infection during the procedure.
Tracheal stent implantation with ECMO support has been shown to be a feasible method for patients in the terminal stage of RP. We hope that further clinical understanding of RP can be attained to allow for earlier diagnosis and treatment.
Footnotes
Ethics: This study was approved by the Human Ethics Committee of the First Affiliated Hospital of Zhejiang University (IIT20210194A). The patient consented to tracheal stent implantation under ECMO support. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Jingchen Zhang https://orcid.org/0000-0003-2011-1894
References
- 1.McAdam LP, O'Hanlan MA, Bluestone R, et al. Relapsing polychondritis: prospective study of 23 patients and a review of the literature. Medicine (Baltimore) 1976; 55: 193–215. [PubMed] [Google Scholar]
- 2.Vitale A, Sota J, Rigante D, et al. Relapsing polychondritis: an update on pathogenesis, clinical features, diagnostic tools, and therapeutic perspectives. Curr Rheumatol Rep 2016; 18: 3. [DOI] [PubMed] [Google Scholar]
- 3.Pearson CM, Kline HM, Newcomer VD. . Relapsing polychondritis. N Engl J Med 1960; 22: 51–58. [DOI] [PubMed] [Google Scholar]
- 4.Arnaud L, Mathian A, Haroche J, et al. Pathogenesis of relapsing polychondritis: a 2013 update. Autoimmun Rev 2014; 13: 90–95. [DOI] [PubMed] [Google Scholar]
- 5.Maciążek-Chyra B, Szmyrka M, Skoczyńska M, et al. Relapsing polychondritis-analysis of symptoms and criteria. Reumatologia 2019; 57: 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohammad A, Ambrose N, Tuohy M, et al. Relapsing polychondritis: reversible airway obstruction or asthma. Clin Exp Rheumatol 2008; 26: 938–940. [PubMed] [Google Scholar]
- 7.Mitilian D, Gonin F, Sage E, et al. From relapsing polychondritis to extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg 2013; 146: 49–51. [DOI] [PubMed] [Google Scholar]
- 8.Laliberte AS, McDonald C, Waddell T, et al . Use of veno-arterial extracorporeal membrane oxygenation in a case of tracheal injury repair in a patient with severe relapsing polychondritis. J Thorac Dis 2017; 9: 1002–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Napp LC, Kühn C, Hoeper MM, et al. Cannulation strategies for percutaneous extracorporeal membrane oxygenation in adults. Clin Res Cardiol 2016; 105: 283–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Honore PM, Barreto Gutierrez L, Kugener L, et al. Risk of harlequin syndrome during bi-femoral peripheral VA-ECMO: should we pay more attention to the watershed or try to change the venous cannulation site? Crit Care 2020; 24: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lekpa FK, Chevalier X. Refractory relapsing polychondritis: challenges and solutions. Open Access Rheumatol 2018; 10: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kingdon J, Roscamp J, Sangle S, et al. Relapsing polychondritis: a clinical review for rheumatologists. Rheumatology (Oxford) 2018; 57: 1525–1532. [DOI] [PubMed] [Google Scholar]