Abstract
The skeletal muscle is the largest organ in the body, by mass. It is also the regulator of glucose homeostasis, responsible for 80% of postprandial glucose uptake from the circulation. Skeletal muscle is essential for metabolism, both for its role in glucose uptake and its importance in exercise and metabolic disease. In this article, we give an overview of the importance of skeletal muscle in metabolism, describing its role in glucose uptake and the diseases that are associated with skeletal muscle metabolic dysregulation. We focus on the role of skeletal muscle in peripheral insulin resistance and the potential for skeletal muscle-targeted therapeutics to combat insulin resistance and diabetes, as well as other metabolic diseases like aging and obesity. In particular, we outline the possibilities and pitfalls of the quest for exercise mimetics, which are intended to target the molecular mechanisms underlying the beneficial effects of exercise on metabolic disease. We also provide a description of the molecular mechanisms that regulate skeletal muscle glucose uptake, including a focus on the SNARE proteins, which are essential regulators of glucose transport into the skeletal muscle.
Introduction: Diabetes and Insulin Resistance
Overview of diabetes and insulin resistance
Diabetes mellitus, hereafter referred to as diabetes, is a suite of metabolic disorders that impair glucose homeostasis and cause persistent elevation of blood glucose levels. This impaired glucose homeostasis increases the risk of heart disease, stroke, and neuropathy, among other complications. Most instances of diabetes are divided into types 1 and 2. Type 1 diabetes (T1D) is an autoimmune disorder that leads to pancreatic β-cell dysfunction and demise; impeding their ability to provide insulin to the body. The lack of insulin prevents glucose uptake in the peripheral tissues, including adipose tissue, and skeletal muscle, resulting in high blood glucose levels. In type 2 diabetes (T2D), the pancreatic β-cells initially produce insulin, but the malfunctioning peripheral tissues are resistant and unable to respond to the insulin, and blood glucose levels remain high. The persistent high levels of blood glucose provoke the continued demand for insulin in this dysregulated signaling state, which eventually leads to β-cell dysfunction and defective insulin secretion. Other types of diabetes include gestational diabetes, which can occur in pregnant women with no history of the disease, and diabetes that is secondary to another medical condition.
Insulin resistance—also called prediabetes—is characterized by elevated fasting blood glucose levels ranging from 101 to 125mg/dL (5.6–6.9mM) or impaired glucose tolerance (140–199mg/dL or 7.8–11.1mM, 2 h after a 75-g oral glucose challenge) (6, 7); however, diagnosis of prediabetes is somewhat controversial due to the lack of a consensus on diagnostic criteria (104). Prediabetic individuals have a 50% chance of developing T2D within 5years of diagnosis (41) and are also at a higher risk of developing other metabolic disorders such as cancer, cardio-metabolic complications, neuropathy, and sarcopenia that can ultimately lead to death (41, 197).
Public health impact
In 2015, around 415 million adults worldwide were estimated to have diabetes, and this is expected to increase by over 250 million people in the coming three decades (347). T2D accounts for over 90% of diabetes cases. As of 2017, there were 30.3 million people in the USA with diabetes and 84.1 million people (more than one in three adults) with prediabetes, a condition that places them at risk for T2D (41).
Therapies for prediabetes
Prediabetes is thought to be reversible. Current treatments for prediabetes include lifestyle interventions in the form of exercise or dietary modifications (323) and anti-hyperglycemic drugs that can increase insulin sensitivity, like metformin (194). However, metformin has not been approved by FDA for use in prediabetes and is less effective than lifestyle intervention (diet and exercise) in minimizing the incidence of T2D (41). What is more, metformin can cause unpleasant side effects, such as gastrointestinal effects, including nausea, diarrhea and abdominal pain, and compliance is a challenge for prescribed exercise regimens (130, 217). Exercise prescription often fails because of poor adherence to a sustained exercise program. In addition, many individuals cannot exercise due to medical conditions, including conditions exacerbated by a sedentary lifestyle (125, 305). There is currently great research interest in developing new T2D therapies that target prediabetes, including therapies that mimic the effects of exercise.
Role of Skeletal Muscle in T2D
Overview of skeletal muscle
The skeletal muscle organ system is the largest in the body, comprising about 40% of the body weight of a young man (141). It is important for movement, posture, temperature and glucose homeostasis, soft tissue support, and metabolism. The skeletal muscle is a striated muscle tissue that is attached to the bones via tendons. Unlike the other two human muscle tissue types, smooth and cardiac muscle, skeletal muscle is under voluntary control by the somatic nervous system. Skeletal muscle is made up of a number of muscle fiber bundles that can vary in fiber type. Skeletal muscle fibers can be divided into slow-twitch Type 1 and fast-twitch Type 2 fibers based on their metabolic characteristics, and then are further defined by their myosin heavy chain (MHC) isoform expression (88).
Importance of skeletal muscle in insulin resistance
Skeletal muscle is essential for glucose clearance and is responsible for over 80% of glucose uptake from an oral glucose load, postprandial (59, 72, 307). Insulin resistance is caused by the desensitization of muscle to the insulin released by the pancreas to elicit glucose uptake, leading to elevated blood glucose levels. Skeletal muscle insulin resistance can appear decades before the onset of β-cell failure and symptomatic T2D (59, 336). In addition, lean nondiabetic, normoglycemic individuals with a high risk of developing T2D (such as children with parents who are both diabetic) have been reported to show moderate skeletal muscle insulin resistance (125, 305), supporting a role for insulin resistance as an early step in the development of T2D.
As the principal site of insulin-stimulated glucose uptake, skeletal muscle is also considered the primary driver of whole-body insulin resistance. When the primary defect is in skeletal muscle, remediating insulin resistance in the muscle alone is sufficient to restore whole-body glucose homeostasis (59). Although skeletal muscle insulin resistance is reversible, β-cell demise to date is not.
Insulin resistance disrupts both the amount of glucose uptake into skeletal muscle and the timing of that uptake (58, 307). Under normal conditions, postprandial glucose uptake into muscle increases linearly with time. However, with insulin resistance and T2D, there is a delay in insulin action and glucose uptake, causing diminished overall glucose uptake by the skeletal muscle. This has been demonstrated by hyperinsulinemic-euglycemic clamping studies in nondiabetic and type 2 diabetic humans (58).
Insulin Resistance and Skeletal Muscle
Links between aging and skeletal muscle insulin resistance
Aging (after 40–50 years of age) of the human skeletal muscle manifests as a gradual decline in mitochondrial function and reduced muscle mass, also known as sarcopenia (359). The loss of muscle mass is concomitant with a decline in strength and muscle function (158), and with a loss in regenerative capacity. While aging is a major risk factor for T2D, in part due to the muscle dysfunction of sarcopenia, there are additional suggested reasons that underlie T2D etiology beyond sarcopenia (291).
This age-associated muscle dysfunction can also be exacerbated by T2D and other diseases—a phenomenon known as secondary aging (24). Although there is currently no way to slow aging, secondary aging can be circumvented or delayed with increased physical activity or exercise (25). However, because sarcopenia can limit movement, a feed-forward cycle of increasing sedentary behavior can occur.
Combined effects of aging and obesity on insulin resistance
The aforementioned metabolic defects overlap and converge upon one another, with insulin resistance at the juncture of aging, muscle atrophy/sarcopenia and obesity. Indeed, these metabolic disorders are so intertwined that the term “sarcopenic obesity” has been coined to describe the toxic feedback loop between increased fat mass (obesity) and decreased skeletal muscle mass (sarcopenia), where one exacerbates the other (93).
Links between obesity/inflammation and skeletal muscle insulin resistance
There is a causal relationship between weight and insulin resistance that has been demonstrated by classical studies of nondiabetic, lean individuals. When these individuals were given a regimen of over-nutrition, they become insulin resistant, suggesting that obesity increases the risk of insulin resistance (89, 202). Chronic inflammation caused by obesity is thought to be a major contributor to the pathogenesis of insulin resistance and T2D. T2D is typically associated with elevated free fatty acids (particularly saturated), increased circulating pro-inflammatory cytokines, and elevated blood glucose which can all lead to insulin resistance (165).
For example, the adipose tissue releases adipokines, which act as signaling molecules, and facilitate tissue cross-talk. Adipokines have been shown to become dysregulated in obese and diabetic patients (192), with one of the most notable adipokines being leptin (186). The discovery of adipokines established the adipose tissue as an official endocrine organ. Similarly, in the last two decades, it has been shown that the skeletal muscle can act as an endocrine organ, secreting factors termed “myokines.” Myokines are proteins released by skeletal muscle, capable of cross-talk with other organs such as the bone, brain, and adipose tissue. Similarly, skeletal muscle can also become a target of obesityinduced inflammation. Obesity-induced inflammation and insulin resistance can also cause the release of particular cytokine hormones from both tissues (adipo-myokines) (Table 1). Skeletal muscle can secrete interleukin-6 (IL-6), interleukin-8 (IL-8), and interleukin-15 (IL-15) as well as irisin, myonectin and myostatin, and unlike adipokines, muscle myokines are regulated by exercise and contraction (250). The release of these circulating factors can either increase or decrease obesity, inflammation, and insulin resistance.
Table 1.
Effects of Exercise and Obesity on Myokines, Adipokines, and Adipo-Myokines (Secreted by Both Muscle and Adipocytes)
| Secreted factors | Effect of obesity | Effect of exercise | |
|---|---|---|---|
| Myokines | BDNF | ↔ (270) | ↑ (73, 191, 255) |
| IL-7 | ? (182, 192) | ↑ (90) | |
| IL-15 | ? (155, 295) | ↑ (26, 213, 253, 353, 357) | |
| Irisin | ↑ (248) | ↑ (26) | |
| Myonectin | ↓ (278, 280) | ? (171, 279)a | |
| Adipo-myokines | ANGPTL4 | ↑ (17)b | ↑ (40, 139) |
| FGF21 | ↑ (364) | ? (82, 355)c | |
| Fstl1 | ↓ (105) | ↑ (86, 214) | |
| IL-6 | ↑ (20, 37, 329) | ↑ (137, 228) | |
| IL-8 | ↑ (259, 267) | ↑ (225, 326, 357) | |
| MCP-1 | ↑ (275) | ↑ (40, 54, 326) | |
| Myostatin | ↑ (101) | ↓ (159, 181, 190, 258, 260, 274) | |
| PAI-1 | ↑ (1) | ↑ (214) | |
| PEDF | ↑ (116, 261) | ↑ (214) | |
| VEGF | ↑ (178) | ↑ (102) | |
| Adipokines | Adiponectin | ↓ (107, 177) | ? (84, 123, 277) |
| Leptin | ↑ (56) | ↓ (131) | |
| Resistind | ↑ (294) | ↓ (129) |
↑, Enhanced in serum or muscle mRNA after exercise or in obesity; ↓, decreased in serum or muscle mRNA after exercise or in obesity; ?, contradicting evidence—some report enhancement and others report a decrease or no change; ↔, no change
Different results reported for mouse versus human.
E40K variant protective against dyslipidemia.
Sex differences reported.
Released by adipocytes in rodents but not humans.
Mechanisms of inflammation in skeletal muscle
Skeletal muscle can undergo infiltration by immune cells, such as macrophages and T cells, and in both humans and mouse models can become pro-inflammatory during obesity or T2D. The intramuscular adipose tissue depots, which expand with obesity and T2D and account for up to 10% of the total skeletal muscle mass (174), are thought to be the main contributors of pro-inflammatory immune cells (e.g. M1-like macrophages) to the skeletal muscle (68, 140). There are two adipose-type depots in skeletal muscle, which reside in an intramuscular or subcutaneous location. Separating the individual effects of these two depots is not yet technically feasible (81). Nevertheless, the cross-talk between adipose tissue and skeletal muscle drives the proinflammatory phenotype in skeletal muscle and is a major contributor to the development of insulin resistance due to the shift in myocyte metabolism imposed by inflammation (68).
There is growing research interest in the role of tissue cross talk in inflammation, including the influence of signaling factors from adipose tissue, circulating immune cells, and the gastrointestinal tract, on skeletal muscle metabolism. Progress is somewhat slow due to the technical challenge associated with isolating intramuscular adipose tissue away from skeletal muscles in the in vivo disease models (174). Recent work in mice has shown that in response to a high-fat diet, proinflammatory pathways are activated in endothelial cells, causing monocyte adhesion and transmigration (43). This promotes immune cell infiltration into muscle and other tissues. Skeletal muscle cells treated with saturated fatty acids attract monocytes and activate macrophage polarization to an M1-like pro-inflammatory state. These M1-like macrophages can cause insulin resistance (43). In muscle from mice fed high-fat diet, or in obese human skeletal muscle, there is also an increase in pro-inflammatory macrophages that is linked with increased adiposity and poor glucose tolerance (74).
Mechanisms of myokine action
Just as the discovery of adipokines established the adipose tissue as an endocrine organ, the identification of myokines hasestablishedthattheskeletalmusclecan actasanendocrine organ. Myokines mediate cross talk with organs including the bone, brain, and adipose tissue. Over 600 different peptides have been identified to be produced and secreted by the skeletal muscle (85, 96), and work is ongoing to characterize the complete secretome in muscle. Recent studies have shown that exercise or contraction of the skeletal muscle can induce the secretion of novel previously un-identified myokines (250), which have anti-inflammatory potential. Some of the most notable well-studied myokines are described below.
Interleukin-6 (IL-6)
IL-6, is a well-known pro-inflammatory cytokine released by skeletal muscle (226, 292), which, together with TNFα, contributes to the onset of insulin resistance. However, more recent evidence suggests that IL-6 can have anti-inflammatory effects, which are dependent on the signaling cascade and type of receptor binding. In macrophages, IL-6 release is caused by pro-inflammatory NFκB signaling and is accompanied by TNF activity. However, when IL-6 is released as a myokine in response to exercise, there is no NFκB signaling, but rather there is a calcium-dependent MAPK signaling pathway that leads to IL-6 release (340). This is thought to be regulated at the level of the IL-6 receptor, of which there are two types, IL-6R and sIL-6R. Classically, IL-6 binds to IL-6R, and this complex associates with gp130 (ubiquitously expressed) to stimulate the anti-inflammatory and anti-apoptotic MAPK signaling pathway (153). However, IL-6R expression is limited to hepatocytes and a limited number of lymphoid cells (124). In contrast, many cell types instead express a soluble IL-6R (sIL-6R), which has the same affinity for IL-6 and induces IL-6 trans-signaling. Thus, sIL-6R can induce IL-6 signaling through gp130 in cells without IL-6R (207). In human skeletal muscle, IL-6 release increases with exercise intensity and duration, this has been linked to lactate production. This IL-6 release depends on exercise-induced lactate production, and lactate alone without exercise, mimics the release of IL-6 from skeletal muscle (103).
Myostatin
Myostatin (growth differentiation factor 8) was the first identified myokine back in 1997, and its discovery has led to numerous secretome analyses, leading to the discovery of over 600 myokines (85). Myostatin, a highly conserved member of the transforming growth factor-beta (TGF-β) family of proteins (195) is highly expressed in skeletal muscle but can also be found in adipose and cardiac tissue. Myostatin is a negative regulator of muscle mass, and its ablation or mutation leads to muscle hypertrophy and a “hypermuscle” phenotype, like for example the Belgian blue cattle (195), or the whippet (205, 281). Myostatin protein abundance (135, 274) and expression (181, 190) decrease in humans after resistance exercise, with IL-6 plasma levels correlating with myostatin expression. Myostatin inhibits myogenesis and protein growth, and its inhibition leads to increased muscle growth (87, 204). Myostatin has also been associated with muscle sarcopenia, and females suffering from sarcopenia show increased serum levels (22). There is considerable research interest in exploring the therapeutic potential of myostatin inhibition to combat muscle atrophy. Indeed, since the early 2000s, there have been numerous agents tested as potential myostatin antagonists (99), including follistatin (22, 86, 105), and stamulumab [myostatin antibody, (330)], albeit with none found to be clinically successful in increasing muscle strength in muscle dystrophy patients (330), or, studies had to be discontinued for safety reasons (33). Some evidence does suggest that myostatin inhibition via the activin receptor extracellular domain fusion protein (ACVR2B-Fc) (21), or ActRIIB agonist (365), is able to inhibit cancer-induced cachexia in mice.
The effect of myostatin on skeletal muscle converges on the same pathway as does Activin A (both members of the TGF-β family of secreted factors). Myostatin binds to a multimeric receptor complex comprised of two type-I (ALK4 and ALK5) and two type-II (ActRIIA and ActRIIB) activin receptors. In skeletal muscle, ActRIIB is more abundant relative to ActRIIA, with a higher affinity for myostatin (167). Activation of the myostatin pathway and formation of the multimeric receptor complex leads to the phosphorylation of Smad2 and Smad3, and the recruitment of Smad4, to form a Smad 2/3/4 complex (276). The Smad complex then translocates into the nucleus where it inhibits genes that drive skeletal muscle proliferation and differentiation, leading to muscle cachexia and atrophy. In fact, myostatin levels are increased in cancer (13), and aging (diseases associated with muscle atrophy) (356). Furthermore, myostatin signaling can inhibit the AKT-mediated mTOR pathway involved in muscle protein synthesis (318). Inhibition of AKT leads to activation of autophagy via the FoxO pathway (166, 187, 188), and the ubiquitin-proteasome pathways, which are involved in protein degradation (179). Overall, elevated myostatin is associated with an increase in muscle atrophy and inhibition of muscle growth.
Irisin
Expression of irisin, also known as cleaved FNDC5, is stimulated by PGC1α and is thought to mediate the beneficial effects of exercise by promoting the beiging of white adipose tissue. This beiging process activates the uncoupling protein UCP1, causing white adipose tissue to partially take on a brown adipose tissue phenotype (26). Brown adipose tissue is associated with increased thermogenesis. Irisin transcript levels have been shown to increase in both human and rodent exercise models, and this is thought to involve an increase in mitochondrial number and oxygen consumption by increasing the expression of PGC1α (85, 324). However, there is controversy surrounding the exercise-induced increase in serum irisin, primarily due to the difficulty in detecting irisin in the blood (due to low serum levels). Quantification of irisin levels has been challenging, but a recent study has shown that circulating irisin levels increase (as detected by tandem mass spectroscopy) with exercise (115). Recently, a mutant Fndc5 mouse model was created to assess the ability of irisin to mediate exercise and adipocyte “beiging.” The mice showed no deficits in skeletal muscle development or function, but they showed reduced running capability, as well as reduced insulin sensitivity and glucose uptake in response to running, highlighting irisin’s importance in mediating the metabolic effects of exercise (349). In addition, irisin treatment of mouse myotubes increases expression of PGC-1α and mitochondrial transcription factor A, both involved in increased mitochondrial content and function (324). However, harmful nutrients such as palmitate can decrease irisin expression and hence decrease its insulin-sensitizing benefits. Specifically, palmitate drives the binding of Smad3 to a Smad3 binding motif in the FNDC5 gene promoter to negatively regulate FNDC5 expression (313). This highlights one potential mechanism whereby insulin resistance in muscle is caused by the downregulation of insulin-sensitizing factors like irisin.
Myonectin
Myonectin belongs to the CTRP (C1q/TNF related protein) family (279) and is a nutrient-responsive myokine that is structurally homologous to adiponectin and is released by muscle contraction. Myonectin mimics insulin’s ability to promote fatty acid uptake by upregulating the expression of fatty acid transport genes such as CD36 and Fabp1/4 in response to exercise (280). Myonectin can inhibit autophagy in the mouse liver (278). The ability of myonectin to inhibit autophagy is abolished when the phosphatidylinositol-3 kinase (PI3K)/AKT pathway is suppressed. Since the PI3K/AKT pathway is known to be important in skeletal muscle anabolism, it is through this pathway that myonectin may inhibit muscle atrophy to promote muscle growth (278). In addition, myonectin activates the nutrient-sensing AMP-activated protein kinase (AMPK) pathway in myocytes, leading to increased translocation of the GLUT4 glucose transporter and glucose uptake (229). Myonectin has also been associated with mitochondrial deoxyribonucleic acid (mtDNA) density, and decreased mtDNA levels in response to insulin resistance can upregulate myonectin (171, 229). Myonectin levels have been shown to be dependent on the skeletal muscle fiber type, with slow-twitch fibers expressing higher levels of the myokine compared to fast-twitch fibers (280).
Interleukin 15 (IL-15)
IL-15 is an exercise- and muscle contraction-regulated myokine that can decrease obesity and inflammation and is of interest as a candidate therapeutic target to combat the negative effects of obesity (155, 295). It is thought to mediate the benefits of exercise; however, the exact effect of exercise on expression, protein, and secretion of IL-15 varies from study to study (26, 213, 253, 353, 357). These studies differ in exercise intensity and type (acute vs. training), as well as IL-15 measurement protocols. The consensus is that moderate-intensity training has a positive impact on IL-15 serum levels in humans (251). IL-15 is upregulated during myoblast differentiation, and IL-15 enrichment in cultured skeletal muscle can induce differentiation and increase muscle mass (164, 242). In contrast, another group showed that IL-15 administration to young rats leads to reduced muscle mass and increased apoptosis (236), suggesting that the conditions of IL-15 administration can affect its role in skeletal muscle. IL-15 increases fatty acid oxidation and glycogen synthesis in skeletal muscle (5), and in adipose tissue, IL-15 has been shown to reduce lipid accumulation while increasing adiponectin secretion (similar to exercise) (243, 244). IL-15 has also been shown to increase glucose uptake into rat skeletal muscle and cultured skeletal muscle cells (31), via the STAT3 (152), and AMPK pathways (209) similar to the effect of exercise on these pathways (193, 319). The lack of consensus regarding IL-15 action indicates that more work needs to be done to understand the mechanism underlying its function as a myokine. Toward this, a recent publication (discussed below) has shed light on the potential mechanism of IL-15 regulation in vivo (282).
Other myokines
Other notable myokines include BDNF and Decorin, which play roles in fat metabolism, muscle regeneration, and differentiation (164, 251). In addition, new myokines have been identified that respond to exercise [termed exerkines (263)]. As for the effect of exerkines on insulin resistance, more work is needed to characterize the function of these exerkines, and understand their role in insulin resistance, before they can be leveraged for therapeutic purposes.
O-GlcNAc: Muscle Nutrient Sensor
O-GlcNAcylation (O-GlcNAc) has been proposed to increase IL-15 expression in skeletal muscle. β-Linked N-acetylglucosamine (O-GlcNAc) is a dynamic posttranslational modification of serine or threonine hydroxyl groups of proteins in the nucleus and cytoplasm. O-GlcNAc is regulated by two proteins: O-GlcNAcase (OGA), which removes O-GlcNAc from serine/threonine hydroxyl groups, and O-GlcNAc transferase (OGT), which adds O-GlcNAc. O-GlcNAc levels are real-time nutrient sensors in the skeletal muscle and other organs. This posttranslational modification was discovered over three decades ago, but its biological relevance, especially in skeletal muscle, was not known until very recently (282).
O-GlcNAc is increased in the skeletal muscle of obese and T2D individuals, and this is consistent with its function as a nutrient sensor: O-GlcNAc levels positively correlate with nutrient availability; for example, high-fat diet-fed mice have elevated O-GlcNAc, and this is associated with disrupted angiogenesis (184). O-GlcNAc inhibits activity of many components of the insulin-stimulated glucose uptake pathway including AKT, PI3K and the insulin receptor (IR), making it an important signaling molecule in the mechanisms underlying insulin resistance and diabetes (338). Specifically, O-GlcNAc synthesis via the hexosamine biosynthesis pathway (HBP) is increased under hyperglycemic conditions and can lead to insulin resistance via the modulation of AKT signaling (230, 328). In hepatocytes, ablation of OGlcNAc by viral overexpression of OGA leads to increased AKT activity (284), while enhanced O-GlcNAc synthesis driven by glutamine treatment of endothelial cells inhibited angiogenesis via inhibition of AKT activity (184).
The effect of increased O-GlcNAc can also be inconsistent and dichotomous. For example, while elevated O-GlcNAc in the pancreata of young mice also associates with negative actions on serum and islet insulin contents and β-cell dysfunction, elevated O-GlcNAc in the pancreata of the mice at older ages was associated with increased AKT activation and improved β-cell function (283). Hence, O-GlcNAc modification can exert both positive and negative effects, depending upon the tissue/cell type, the specific proteins that are modified, and when the proteins are modified longitudinally. Furthermore, O-GlcNAc of glycogen synthase in 3T3-L1 adipocytes under high glucose conditions has been shown to contribute to insulin resistance, similarly, in hyperglycemic mice, O-GlcNAc of glycogen synthase was increased (231).
In addition, it has been shown that there is cross talk between O-GlcNAc and AMPK, whereby activation of AMPK can alter the substrate selectivity of OGT and lead to its nuclear localization (30). O-GlcNAc has also been associated with a vesicle trafficking protein, Munc18c, to impair GLUT4 vesicle translocation and glucose uptake in adipocytes (45). Munc18c that is O-GlcNAcylated remains clamped to syntaxin 4 (STX4), maintaining it in its closed conformation and blocking the activation of STX4. When STX4 activation is blocked, so is the formation of functional SNARE complexes in the adipocytes. Increased O-GlcNAc of Munc18c via glucosamine treatment in 3T3-L1 adipocytes leads to an inhibition of SNARE trafficking to the plasma membrane and blunted GLUT4 translocation. Interestingly, only Munc18c was found to be modified, none of the vesicle SNAREs (v-SNAREs) or target SNAREs (t-SNAREs) were O-GlcNAcylated (45).
The levels of O-GlcNAc are tightly regulated by OGT and OGA and the dysregulation of either of these enzymes can be detrimental in skeletal muscle. Loss of OGA leads to skeletal muscle atrophy, while OGT overexpression leads to insulin resistance, suggesting that O-GlcNAc plays a role in a signaling network in the muscle that can modulate a number of metabolic mechanisms and pathways. The precise role of O-GlcNAc in skeletal muscle is largely unknown, but it was recently shown that OGT knockout in mouse skeletal muscle improves insulin sensitivity, increases leanness, increases energy expenditure, and enhances glucose uptake (282). These mice also showed increased circulating IL-15 expression, which was accompanied by increased levels of adiponectin. Furthermore, OGT was found to control IL-15 expression via O-GlcNAc. This provides a mechanism for promoting IL-15 expression in skeletal muscle, which may be useful as a therapeutic target to combat insulin resistance and T2D.
Mechanisms of Glucose Uptake
Glucose transporters (GLUTs)
Multiple glucose transporters facilitate glucose movement across the plasma membrane. This membrane-spanning SLC2A family of proteins is integral to the transportation of glucose and other hexoses either to the inside or outside of the cell. There are over 14 SLC2A-family glucose transporters present in human cells across three classes [class I, II, and III (310)] based on sequence similarity (206).
There is variable tissue expression of glucose transporters in humans. In skeletal muscle, there are three GLUTs responsible for mediating glucose uptake: GLUT4, GLUT1, and GLUT3 (expressed in fetal and neonatal muscle only), in order of abundance (147) (i.e. GLUT4>GLUT1). GLUT1 localizes to the plasma membrane, whereas GLUT4 primarily localizes to intracellular vesicles and is transported to the cell surface in response to stimuli. GLUT5 has also been found in the skeletal muscle (108), where it primarily localizes to the plasma membrane for facilitating fructose transport across the muscle.
GLUT4 is best known as the insulin-regulated glucose transporter (112). It is encoded by the SCL2A4 gene, and it is highly abundant in skeletal muscle and adipose tissue. GLUT4 is an intracellular protein that depends on stimulus (insulin or exercise) to translocate to the plasma membrane and facilitate glucose uptake. Under unstimulated conditions, glucose transport is restricted, due to the intracellular localization of GLUT4, and a limited expression of GLUT1 at the plasma membrane. There are reported to be two pools of intracellular GLUT4, one recruited by insulin stimulation (Figure 1), and the other by exercise (Figure 2) (55). Below we discuss the differences in GLUT4 translocation and uptake between the two stimuli.
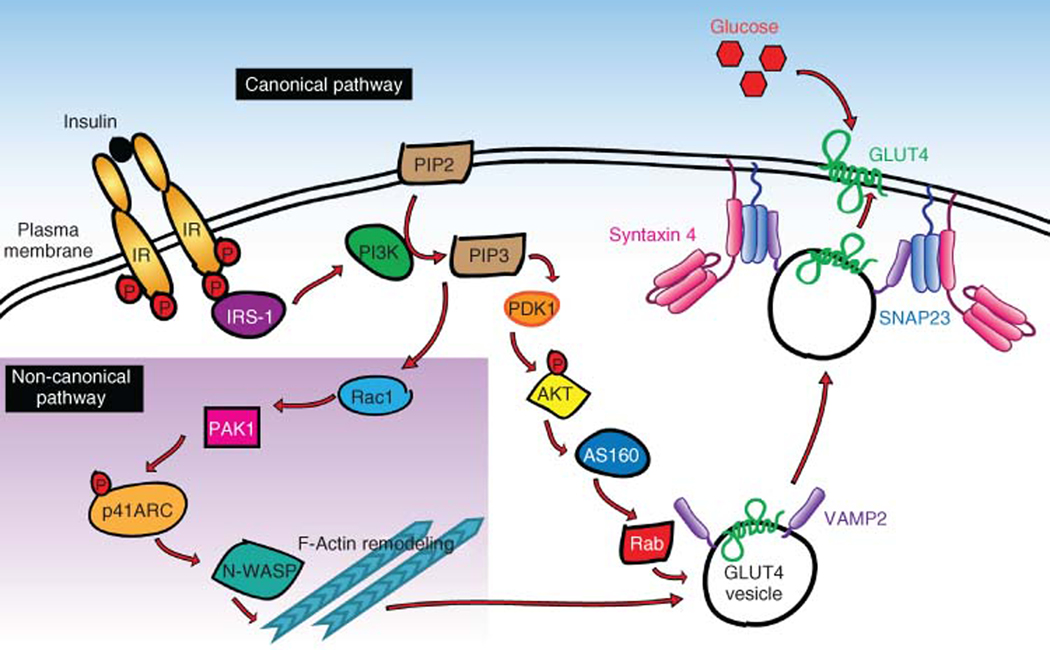
Figure 1.
A simplified model of insulin-stimulated translocation of the GLUT4 glucose transporter in skeletal muscle. Shown is the canonical insulin signaling pathway, and a noncanonical pathway (inset in purple). Both signaling pathways culminate with SNARE protein (Syntaxin 4, SNAP23, and VAMP2)-mediated vesicle trafficking and fusion with the plasma membrane. Vesicle fusion allows GLUT4 to integrate into the plasma membrane and transport glucose from the blood into the skeletal muscle.
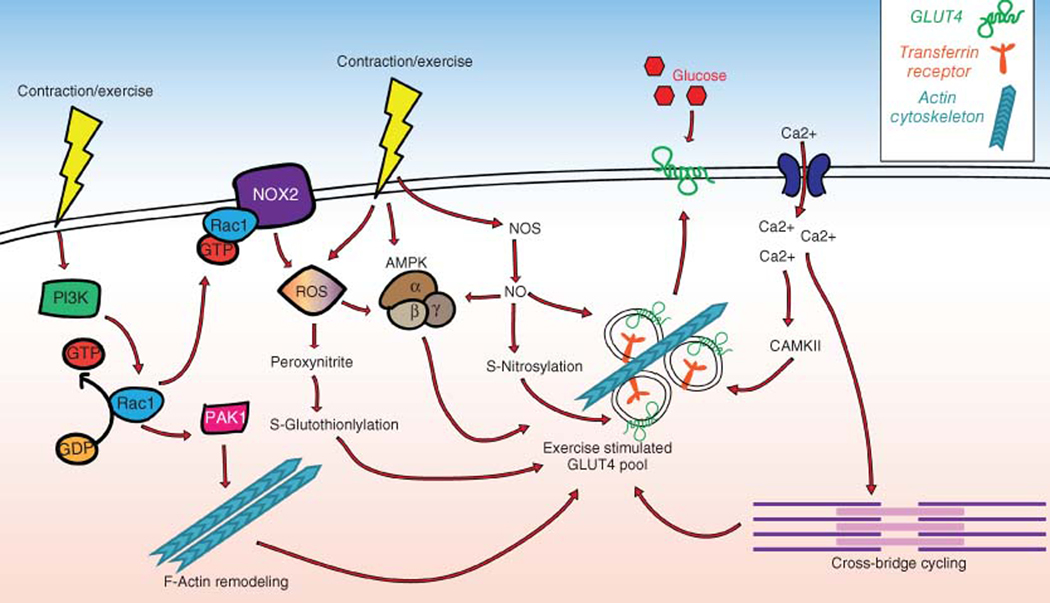
Figure 2.
Contraction-mediated GLUT4 translocation. When contraction occurs via exercise (depicted by yellow lightning bolts) multiple pathways are activated, which can all lead to GLUT4 translocation and glucose uptake. Left: contraction causes Rac1-GTP loading/activation, which induces PAK1 phosphorylation/activation, and F-actin remodeling to activate the exercise stimulated GLUT4 vesicle pool; it can also activate NOX2 which causes reactive oxygen species (ROS) formation. ROS can also be stimulated directly by contraction, leading to peroxynitrite and subsequent GLUT4 translocation, or can cause AMPK activation. Nitric oxide (NO) production can lead to S-nitrosylation of proteins that cause GLUT4 translocation. Muscle excitation can also cause calcium influx into the muscle cell (far right), which can activate CAMKII and lead to glucose uptake. Calcium influx can also stimulate cross-bridge cycling, the process of muscle fiber contraction, which leads to GLUT4 translocation and glucose uptake into the cell.
GLUT4 regulation of insulin-stimulated glucose uptake
Insulin-stimulated glucose uptake is rate-limited by the translocation of GLUT4-laden vesicles from the intracellular compartments to the PM. The translocation of the GLUT4 vesicles occurs in response to the canonical insulin signaling pathway (and in muscle, via a second noncanonical insulin signaling pathway). Once GLUT4 proteins are integrated into the PM, the influx of glucose into the muscle or adipocyte ensues. While this process has been delineated in both muscle and adipose tissue, the skeletal muscle is the focus of this review article. As shown in Figure 1, insulin stimulates GLUT4 vesicle translocation via two pathways in the skeletal muscle that bifurcate shortly after insulin binds the IR and activates the intracellular signaling cascade. These two pathways are normally distinguished by the activation of the serine/threonine kinase AKT in the canonical pathway, or the Rho-family GTPase Rac1 in the noncanonical pathway. These pathways are independent of one another: inhibition of one pathway does not affect the other pathway. Both can function autonomously to stimulate GLUT4 translocation (301). The two pathways are discussed in detail below.
Canonical insulin signaling pathway
Insulin binds to the α-subunit of the IR, which localizes to the plasma membrane of the skeletal muscle (341). This leads to both a conformation change and tyrosine phosphorylation of the IR ß-subunit (163, 361). Once the IR is phosphorylated, the insulin receptor substrate-1 (IRS-1) is recruited to the IR (296). In the canonical insulin signaling pathway, IRS-1 binds the SH2 domain of PI3K (160, 208), allowing PI3K to phosphorylate phosphatidylinositol 4,5-biphosphate (PIP2), and form phosphatidyl 3,4,5-triphosphate (PIP3) (4). PIP3 phosphorylation recruits AKT, which binds PIP3, and AKT is phosphorylated and activated by phosphatidylinositoldependent kinase (PDK1) (3, 4, 334). AKT phosphorylates AS160 (133, 309), a Rab GTPase activating protein (GAP) (273). AS160 prevents the inactivation of the small GTPase Rab proteins Rab8A and Rab13 in muscle, which occurs when AS160 is dephosphorylated (110, 297). Rab8A is required for GLUT4 translocation in muscle cells, and its loss inhibits glucose uptake (297), whereas Rab13 enables tethering of GLUT4 vesicles to filamentous actin (298). In contrast, Rab10 is the main substrate of AS160 in adipocytes (271). The adipose-specific Rab10 is required for glucose uptake into adipose tissue, and genetic ablation of adipocyte Rab10 in mice diminishes glucose uptake and GLUT4 translocation both in vivo and in vitro (325). These findings show that while the adipose tissue is responsible for only a minor portion of glucose uptake, its systemic signaling affects whole-body glucose homeostasis. GLUT4 translocation, facilitated by Rab proteins, guides the GLUT4 vesicles to the plasma membrane where members of the SNARE complex, including synaptosomal-associated protein 23 (SNAP23) (77, 134), and STX4, bind to the v-SNARE VAMP2 to fuse the vesicles with the PM and integrate GLUT4 onto the PM (220). This process permits glucose to enter the cell via facilitated diffusion.
Noncanonical insulin signaling pathway
Unlike the canonical insulin signaling cascade, this pathway involves small GTPases of the Rho family. In muscle, this is the Ras-related C3 botulinum toxin substrate 1 (Rac1) (113, 114), whereas in adipocytes, Rac1, as well as the small GTPase TC10, is used (50, 303). Signaling is initiated in a manner similar to that of the canonical pathway: insulin binds the IR, resulting in PI3K activation, which in turn generates PIP3. PIP3 recruits AKT and becomes phosphorylated and therefore activated by PDK1. After this point, the pathways diverge. In the noncanonical pathway, Rac1 is activated via GTP-loading by PI3K activation of guanine nucleotide exchange factors (GEFs) or inactivation of GAPs. Once activated, Rac1-GTP leads to activation of its effector protein, p21-activated kinase 1 (PAK1) (114, 300), which in turn causes phosphorylation of p41-ARC, an ARP2/3 subunit required for GLUT4 translocation, and leads to filamentous actin polymerization via interactions with N-WASP (320, 321). Actin remodeling allows for GLUT4 translocation to the plasma membrane, where the two signaling arms converge with SNARE complex formation and glucose uptake (51).
Mechanisms of GLUT Translocation in Muscle
SNARE-mediated vesicle exocytosis
SNARE proteins mediate vesicle fusion during GLUT4 translocation. Traditionally SNAREs are of two types, v-SNAREs or t-SNAREs, which are located on the membrane of vesicles or at terminal membranes, respectively. There are 6 v-SNAREs, and 11 t-SNAREs, present in the muscle and adipocytes. However, only the t-SNAREs STX4 and SNAP23 and the v-SNARE VAMP2 are required for insulin-stimulated GLUT4 vesicle fusion and exocytosis in muscle and adipocytes (134, 220, 352). Given the promiscuity of some SNARE proteins, which can localize to both vesicles and target membranes, an alternate classification scheme exists R-SNAREs and Q-SNAREs. R-SNAREs contribute an arginine residue (R) in SNARE complex formation and usually act as v-SNAREs, while Q-SNAREs contribute a glutamine (Q) to the SNARE complex zero ionic layer. Q-SNAREs can be further sub-categorized to Qa, Qb, and Qc (70). SNARE proteins are defined by a 60 to 70 amino acid SNARE motif, which has the propensity to form coiled-coil structures. Most SNARE proteins contain only one motif, but there are three identified SNAREs with two motifs: SNAP23, SNAP29, and SNAP47. In addition, v-SNARE proteins and syntaxin (STX) t-SNAREs have hydrophobic C-terminal transmembrane domains; however, some do not (SNAP23, SNAP29, SNAP47), and instead, they have posttranslational lipid modifications, such as palmitoylation, to anchor them into the plasma membrane. When t-SNAREs and v-SNAREs interact, they form a complex known as the SNARE core complex. A SNARE core complex is generally defined as having three Q-SNARE motifs and one R-SNARE motif and is notoriously SDS-resistant due to the induced high affinity binding of the four α-helices (e.g. two from SNAP23, one from STX4 and one from VAMP2). The helices create multiple hydrophobic layers and must be boiled to dissociate the protein complex (69).
SNARE proteins dock and fuse vesicles to the plasma membrane, but there is no consensus on the cargo of docked vesicles. For example, although STX4 is associated with GLUT4 vesicle docking, the potential for STX4 docked vesicles to mediate more than just glucose homeostasis has been proposed. STX4 was found to dock/fuse vesicles carrying the enzyme acid sphingomyelinase (A-SMase), which is central to sphingolipid metabolism, cancer drug cytotoxicity (e.g. cisplatin),and apoptosis (234). A-SMaseactivation and transport are dependent on STX4 abundance, and loss of STX4 can diminish A-SMase activity.
v-SNAREs
v-SNAREs are located on the GLUT4 vesicle membrane. In skeletal muscle, the following v-SNAREs have been found: VAMP2, VAMP3, VAMP5, and VAMP7. Although VAMP2 is the only v-SNARE implicated in insulin-stimulated GLUT4 translocation, during exercise, VAMP2, VAMP5, and VAMP7 have all been shown to co-immunoprecipitate, and translocate to the sarcolemma with GLUT4, and the transferrin receptor (256). This result suggests that all three VAMP proteins play a role in exercise-stimulated GLUT4 translocation and glucose uptake.
t-SNAREs
t-SNARE proteins, such as STX4 and SNAP23, reside on the sarcolemma in muscle. To anchor themselves into the sarcolemmal membrane, STX proteins contain a transmembrane C-terminal domain, whereas SNAP23 proteins associate with the membrane via palmitoylation of four cysteine residues in the central linker region of the protein allowing the formation of thioester linkages to the membrane (227). t-SNAREs are known to form binary sub-complexes (e.g. STX4-SNAP23), which aid v-SNARE binding by acting as templates. These sub-complexes are very stable, and usually contain three SNARE motifs residing within the same membrane (also called a t-SNARE complex) (64). The STX proteins have one SNARE motif and the SNAP23 proteins have two motifs separated by a linker region. The t-SNARE intermediate complex, a heterodimer, can be partially or completely zippered to form the receptor for v-SNARE binding (363).
SNARE zippering and complex formation
Once the v-SNARE and t-SNAREs are in close proximity, they form the SNARE complex. This process occurs via zippering, bringing the membranes (vesicle and plasma membranes) into position and facilitating fusion. The SNARE motifs, which are α-helical coiled -coils, assemble in a 4-strand parallel coiled-coil (237), with 15 layers of interacting hydrophobic side chains, in a 1:1:1 heterotrimeric ratio (285). At the center of the complex is one arginine residue from the v-SNARE and three glutamine residues from the t-SNARES, which represent the R and Q classifications mentioned above (70, 180). This is a conserved feature of SNARE complex formation. The term “zippering” is used to describe the interaction between the proteins, as it is believed that they assemble from the N-terminal region toward the C-terminal region, similar to a zipper closing a jacket. This brings the membranes close together to facilitate fusion (288).
SNARE accessory proteins
DOC2B
The double C2 domain-containing protein β (DOC2B) and two other DOC2 isoforms—DOC2α and DOC2γ—were originally discovered in the brain as synaptic proteins involved in calcium-dependent exocytosis (80, 223, 224). DOC2B functions as a priming protein that increases the number of fused vesicles in response to calcium. DOC2B lacks a transmembrane domain. In response to calcium, which binds both the C2A and C2B domains, a direct interaction between the DOC2B C2A domain and the plasma membrane can occur (150). DOC2 proteins also interact with Munc13 proteins (222).
DOC2B is also expressed in pancreatic β-cells, adipocytes and skeletal muscle. It has been shown to regulate glucosestimulated insulin secretion in β-cells (136), and insulin-stimulated glucose uptake in skeletal muscle (362). Enrichment of DOC2B promotes insulin secretion (12), and peripheral insulin sensitivity (246), by acting as a scaffold for Munc18 proteins to associate and promote SNARE complex assembly (245).
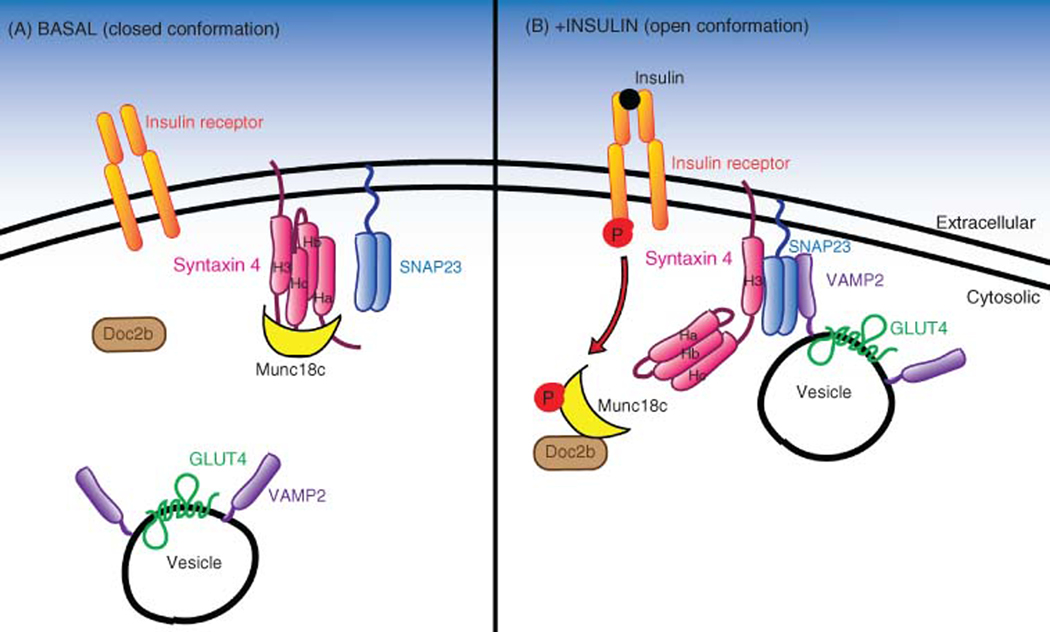
DOC2B deficiency in mice impairs GLUT4 translocation to the sarcolemmal surface and reduces SNARE complex formation (247). DOC2B is believed to recruit Munc18c away from STX4, allowing STX4 to adopt an open conformation (Figure 3), and allowing SNARE complex formation to continue (136). Without DOC2B, STX4 is maintained in a sequestered closed conformation by Munc18c (247). Indeed, DOC2B protein is reduced in human diabetic skeletal muscle, further implicating DOC2B as a key regulator of glucose homeostasis in muscle (362). DOC2B is a potential therapeutic candidate in T2D because of its ability to promote and protect functional beta-cell mass and to enhance and protect glucose homeostasis in vivo.
Figure 3.
SNARE complex formation under basal versus insulin-stimulated conditions. (A) Under basal conditions, Syntaxin 4 (STX4, pink) is in a closed conformation, which is maintained by the accessory protein Munc18c (yellow). (B) Upon insulin stimulation, the insulin receptor (IR) is phosphorylated, after which phospho-IR binds to and phosphorylates Munc18c. Phospho-Munc18c then lets go of STX4 and binds to DOC2B (brown), allowing STX4 to adopt its open conformation. In its open conformation. In its open conformation, the STX4 H3 domain is exposed, enabling STX4 to associate with SNAP23 and VAMP2 (purple) on the GLUT4 vesicle, leading to the formation of the SNARE complex, mediating vesicle docking and fusion to the plasma membrane.
Munc18c
Mammalian uncoordinated-18 protein C (Munc18c or MUNC18–3) is the mammalian homolog of Unc-18c, an important component in exocytosis. The Munc18 family of proteins is 66 to 68kDa soluble proteins that localize to the plasma membrane and cytosolic compartments; two of the three Munc18 family, Munc18c and Munc18b, are expressed in muscle and fat cells (306). Munc18 proteins have both positive and negative roles. Munc18 proteins play a positive required role in SNARE-mediated fusion, wherein Munc18 protein reduction impairs SNARE-mediated fusion. Munc18 proteins can also play a negative role when over-expressed, by clamping their cognate STX partners in a closed conformation that impedes SNARE complex formation. For example, Munc18c binds to STX4 and is required for insulin-stimulated GLUT4 vesicle docking and fusion in 3T3L1 adipocytes (290, 304, 311), and mediating peripheral insulin action in skeletal muscle in vivo (216, 290). The high affinity of Munc18c for STX4, on the order of 12nM [entire cytoplasmic region, (120, 203)] is thought to localize Munc18c to the plasma membrane (360). It has been reported that Munc18c binds to the N-terminal region of STX4 (360), or to the C-terminal region (120, 252). Recognizing this, another report suggests that Munc18c binds to both domains of STX4, keeping STX4 in its closed conformation, similar to the interaction demonstrated for the neuronal Munc18–1 and STX1A proteins (203).
It was later discovered that Munc18c is rapidly tyrosine phosphorylated at Tyr219 and Tyr521 in response to insulin stimulation, serving as an IR substrate (121). Interestingly, Munc18c Tyr219 phosphorylation occurs independently of PI3K suggesting that Munc18c activation occurs in a parallel pathway to IRS-1 activation (121). Upon Munc18c’s tyrosine phosphorylation, STX4 binding to Munc18c is decreased by 60%, releasing the clamp on STX4 and promoting SNARE complex formation and GLUT4 vesicle fusion (121). This decrease is accompanied by a twofold increase in the association between Munc18c and another SNARE accessory protein, DOC2B (120, 121), and STX4 activation and assembly into SNARE complexes. In essence, Munc18c switches binding partners depending upon its phosphorylation status. Munc18c levels in healthy muscle and fat cells are tightly controlled, as is common for key regulatory factors, with 2 to 3nM of Munc18c found to be required to maintain glucose homeostasis. Munc18c levels that are reduced or increased are associated with insulin resistance (290).
Syntaxin 4 interacting protein (synip)
Syntaxin 4 interacting protein (synip) is a STX4 binding protein which regulates glucose transport and GLUT4 vesicle translocation and was first identified in adipocytes (199). Synip binds to STX4 under resting/basal conditions, and insulin stimulation reduces the binding affinity of synip for STX4. Both the v-SNARE VAMP2 and synip compete for the same binding site on STX4. Therefore, when synip is bound to STX4, GLUT4 vesicles cannot dock and SNARE complexes cannot form (199). Insulin modulates synip binding to STX4 by activating AKT2, which phosphorylates synip at Ser99, leading to its dissociation from STX4 (350). Expression of a Ser99Phe synip mutant blocked GLUT4 translocation in response to insulin (350). While a follow-up study using a Ser99Ala mutation of synip resulted in congruent findings regarding ablation of insulin-stimulated GLUT4 translocation (219), this outcome was contested by a different group that also used the Ser99Ala mutant (272). The underlying cause of this discrepancy remains unresolved.
Although synip is an important modulator of insulin-stimulated GLUT4 translocation in adipocytes (199) and podocytes (350), and of glucose-stimulated insulin secretion in the pancreas (264, 265), no studies have evaluated synip function in the skeletal muscle, despite report of abundant synip mRNA expression in skeletal muscle and heart (199). Hence, whether synip plays a parallel role in insulin-stimulated skeletal muscle glucose uptake as has been demonstrated in adipocytes, remains to be tested.
STX4 in SNARE-mediated exocytosis: trafficking versus docking versus fusion—the rate-limiting step
Insulin-stimulated GLUT4 translocation requires the interaction of VAMP2 with STX4 and SNAP23 to form the SNARE complex (327). However, it was unknown whether trafficking (movement of the GLUT4 vesicle to the plasma membrane), docking (arriving at the plasma membrane) or fusion (fusing with the plasma membrane) constituted the rate-limiting step in this process. Using a temperaturesensitive Munc18c mutant as a novel tool to address this question, it was demonstrated that the rate-limiting step for insulin-stimulated GLUT4 translocation is principally vesicle trafficking (312). In brief, overexpression of wildtype Munc18c inhibited insulin-stimulated GLUT4 translocation, as had been previously reported (304, 311), the overexpression of a Munc18c mutant (Arg240Lys) also inhibited GLUT4 translocation at the permissive temperature, and was rapidly reversible upon shifting to the nonpermissive temperature. Evaluation of the rate of GLUT4 translocation following temperature shifts demonstrated that the ratelimiting step in insulin-stimulated GLUT4 translocation is the trafficking of the vesicles to the PM (312). The concept of the rate-limiting step preceding docking and fusion steps was later supported using TIRF microscopy in adipocytes (16). However, another group also using TIRFM suggested that the rate limiting step was vesicle fusion to the PM (176). Further studies will likely be required to reconcile the differences in TIRFM methodological differences to yield a consensus.
Exercise-stimulated GLUT4 translocation and glucose uptake
When muscle contracts, it stimulates the translocation of GLUT4 vesicles to the plasma membrane, to facilitate the uptake of glucose into the muscle. Exercise duration and intensity determine the amount of glucose uptake by the skeletal muscle. Increased intensity and time lead to increased glucose uptake (331). Exercise increases blood flow (8), which further increases glucose uptake from the blood into the skeletal muscle.
Exercise is an important regulator of glucose metabolism and uptake (332) and is considered a therapeutic for insulin resistance and T2D (337). This is because exercise-stimulated glucose uptake is maintained during insulin resistance, as it does not rely on the AKT signaling arm of the GLUT4 translocation pathway (52, 344). Instead, the pathways are additive: glucose uptake can be further enhanced by combining muscle contraction and insulin stimulation (183). However, some studies suggest that the pathways for insulinand exercise-stimulated GLUT4 translocation may converge downstream (146, 339).
During exercise, an exercise-sensitive pool of GLUT4 vesicles is induced to translocate to the sarcolemma, and GLUT4 endocytosis from the sarcolemma is coordinately reduced in both skeletal muscle and cardiomyocytes, as demonstrated by the use of exercise mimetics (71, 132, 354). The exercise-stimulated GLUT4 pool is distinguished from the insulin-stimulated GLUT4 pool by the presence of the transferrin receptor selectively on the exercise-stimulated GLUT4 vesicles (169). The precise signaling mechanism used to elicit exercise-stimulated GLUT4 translocation is not well known. Implicated signaling pathways in exercise-induced GLUT4 vesicle translocation are described below.
AMP-activated protein kinase (AMPK)
AMPK is involved in mediating glucose uptake via exerciseinduced GLUT4 vesicle translocation (144, 221). AMPK is a cellular energy sensor, serving as a nexus for impacting multiple metabolic pathways such as fatty acid synthesis, glucose uptake, and fatty acid oxidation (19, 66, 221). AMPK is a heterotrimer made up of AMPK-α, -β, and -γ subunits, with α being a catalytic subunit, and the β and γ being regulatory subunits (65). There are multiple subtypes of each type of subunit, and the skeletal muscle has been shown to primarily express the α2β2 subtypes, and the α1β1 subtypes to a lesser extent (48). Exercise triggers activation of both α1 and α2 subtypes; α1 is activated during high-intensity acute exercise bouts, while α2 is activated during lower-intensity exercise (79). AMPK-β subunits are also important for glucose uptake and exercise capacity, as evidenced by muscle-specific β1β2 double knockout mice that exhibit noted physical inactivity (221), and have reduced exercise capacity and exercise-induced glucose uptake into skeletal muscle (302). An increase in the ADP:ATP ratio (i.e. low energy status as is induced by exercise) in the cell leads to activation of AMPK. AMPK is activated by phosphorylation of the α-subunit at Thr172 (91, 215, 268). This phosphorylation is mediated by upstream kinases, including calmodulin-dependent protein kinase (CAMK) (92, 109, 346); liver kinase B1 (LKB1) is the principle upstream kinase to phosphorylate AMPK in skeletal muscle (149, 266, 308). The pharmacological activator of AMPK is AICAR (5-aminoimidazoel-4-carboxamide1-D-riborfuronosil-5′monophosphate), which can mimic exercise-stimulated GLUT4 translocation and glucose uptake (AICAR details are discussed in greater detail in the section titled “Therapeutic Development of Exercise Mimetics”).
AMPK regulates exercise-stimulated glucose uptake via its phosphorylation of two downstream targets, AS160 and TBC1D1 (tre-2/USP6, BUB2, cdc16 domain family member 1, a member of the TBC1 Rab-GAP family of proteins) (47). AS160 was implicated in exercise-stimulated glucose uptake by evidence showing that ex vivo contraction of rat skeletal muscle leads to AS160 phosphorylation (29), and that mutation of AS160 phosphorylation sites reduces exercise-stimulated glucose uptake in rodent and human skeletal muscle (151, 317). While AS160 is central to both exercise- and insulin-stimulated glucose uptake, AMPK is the upstream regulator of AS160 in the exercise-stimulated pathway, while AKT regulates AS160 in response to insulin stimulation (151). In brief, AICAR treatment was shown to increase phosphorylation of AS160 at four sites, and that expression of an AS160 mutant (with all four phosphorylation sites mutated) reduced AICAR-induced glucose uptake (29). AMPK phosphorylates TBC1D1 at several sites, with the predominant phosphorylation site being Ser237, a site also phosphorylated in response to exercise (78). Inhibiting the phosphorylation of TBC1D1 decreases exercise-stimulated glucose uptake (145, 232).
Most recently, a novel myokine-ATP synthase inhibitory factor 1 (IF1) has been identified as a downstream target of AMPK activation, via reactive oxygen species (ROS), which leads to Rac1 activation (162). This further highlights the breadth of AMPK’s regulation of exercise-stimulated glucose uptake, and that additional facets and factors may be yet to be discovered.
Beyond exercise-stimulated glucose uptake, AMPK also contributes to insulin sensitivity in skeletal muscle, via its linkage to IRS1 phosphorylation (111), mTOR inhibition (67, 127, 142), adiponectin activation (351), and through its interaction with the myokine IL-6 (38). AMPK modulates insulin-stimulated glucose uptake via the phosphorylation and inhibition of glycogen synthase (39), a key enzyme for the conversion of glucose into glycogen (238).
Calcium-activated signaling
Calcium influx into the muscle leads to muscle contraction via a process known as excitation-contraction coupling (269). When an action potential is created upon depolarization of the skeletal muscle, this spreads throughout the cell, eventually depolarizing the T-tubules. This opens the voltage-gated calcium channel Cav1.1 at the sarcolemma, also known as the dihydropyridine receptor. Cav1.1 is a voltage-dependent, L-type α1S subunit calcium channel, and interacts with calcium release channels in the sarcoplasmic reticulum known as ryanodine receptors (RyRs) (10). There are three RyR isoforms, with RyR1 (skeletal muscle calcium release channel) being the isoform primarily expressed in skeletal muscle. Specifically, Cav1.1 undergoes a conformational change that activates RyR1 in the skeletal muscle (241), and causes calcium release into the muscle, leading to a “calcium spark.” Several thousand calcium sparks increase the calcium concentration within the muscle (49). The calcium can bind proteins like troponin C to lead to cross bridge cycling, a mechanism of muscle contraction. A regulator of this process that controls the duration of contraction is the sarco/endoplasmic reticulum calcium ATPase (SERCA), which removes the calcium from the cytosol and returns it to the sarcoplasmic reticulum, allowing the muscle to relax (32).
Calcium has been shown to enhance muscle GLUT4 translocation, and subsequently glucose uptake (9). For example, calcium induced by caffeine addition to rat L6 myotubes leads to an increase in GLUT4 translocation; this effect can be blocked by a CAMK inhibitor (calmodulin-dependent kinase protein, a protein activated by calcium), or induced by the AMPK activator AICAR (218). Interestingly, the effect of AICAR and caffeine, that is activation of calcium and AMPK, were additive and their combined effects were similar to the effects achieved by exercise (348). Contrary to these data, use of RyR inhibitors failed to support a direct role for calcium release in the process of exercise-stimulated glucose uptake into skeletal muscle (117, 119). Given the importance of calcium in muscle contraction and the number of calcium-sensing proteins that are known to be modulated with exercise, it is plausible that calcium is an important modulator of exercise-stimulated glucose uptake, perhaps through an indirect mechanism (348). For example, inhibition of CAMKII reduces contraction-stimulated glucose uptake in mouse muscle (343).
Nitric oxide (NO) signaling
Exercise increases the activity of nitric oxide synthase (NOS) (18), which produces the gaseous signaling molecule nitric oxide (NO) from L-arginine, oxygen, and NADPH (76). Inhibition of NOS using L-NMMA blunts glucose uptake in skeletal muscle during exercise in both healthy and T2D individuals (27, 143). nNOSμ is the main isoform expressed in skeletal muscle (210), is constitutively active, and muscle contraction causes a twofold increase in NO production (233). However, there is some disagreement in the field as to whether NOS inhibition decreases exercise-stimulated glucose uptake (27, 143), as this is not universally observed (94, 138).
The mechanism linking NO to increased GLUT4 translocation is not known. NO has been suggested to modulate the GLUT4 translocation pathway, since it was found to be independent of an increase in blood flow in either rodents (257), or humans (95). Some reports also suggest that NO could be acting via the soluble guanylate cyclase/cyclic guanosine monophosphate/protein kinase G pathway, or by posttranslational modifications such as s-nitrosylation, which leads to nitrosylation of proteins in adipocytes (128) and tyrosine nitration, which activates PI3K, PKC, and AMPK (173). All of these pathways increase glucose uptake. The SNARE protein STX4 is s-nitrosylated in human islets and MIN6 (mouse insulinoma cell line) β-cells. In pancreatic islets, STX4 is nitrosylated at Cys141, impacting SNARE complex assembly; nitrosylation can be induced by exposure to damaging proinflammatory cytokines (342). However, it remains unknown whether STX4 can be nitrosylated in other tissue types, such as the skeletal muscle.
In addition to NO, the generation of peroxynitrite through the s-nitrosylation of proteins induces ROS, which stimulates GLUT4 translocation and glucose uptake in cardiomyocytes (106). Exercise-stimulated ROS in skeletal muscle is discussed in greater detail in the subsequent section.
Reactive oxygen species (ROS)
Exercise increases ROS in the skeletal muscle, yet until recently, this has only been demonstrated via ex vivo contraction-mimicking stimuli (i.e. hydrogen peroxide, a potent ROS producing reagent), which increases AMPK activation (366), as well as AKT phosphorylation, and glucose uptake (118). While these stimuli implicated ROS in the mechanism of exercise-stimulated glucose uptake, whether the source of ROS in skeletal muscle during exercise was mitochondrial or cytosolic, limited elucidation of the mechanism. In a very recent study (97), cytosolic ROS was identified as the predominant source. Using vivo fluorescent dyes and biosensors, ROS was shown to be generated during moderate-intensity exercise in both humans and mouse models (97). Moreover, cytosolic ROS production was shown to be dependent upon NADPH oxidase 2 (NOX2), with NOX2 loss-of-function models showing defective exercise-stimulated GLUT4 translocation and glucose uptake (97). Indeed, NOX2 activity was also recently shown to be essential for exercise-induced glucose uptake (98), and this newest evidence shows that this is linked to NOX2-dependent ROS production. Upstream of this, NOX2 is activated by the Rac1 GTPase, which can lead to the assembly of a NOX2 complex in other cell types (2, 148, 170). It has been suggested that Rac1 can regulate muscle glucose uptake through NOX2, based on shared phenotypes between Rac1 and Nox2 knockout mice (289). However, this data is correlative and we can only extrapolate that Rac1 is a vital upstream mediator of NOX2, impinging upon the downstream GLUT4 translocation pathway.
NO is also increased with passive stretching, and it was previously postulated that passive stretching increases glucose uptake via NOS activation (18). However, more recent work has demonstrated that glucose uptake stimulated by passive stretching is independent of NOS (138). Mechanical stress has also been shown to activate AMPK and ROS production, which stimulates glucose uptake into the skeletal muscle (42).
Therapeutic Development of Exercise Mimetics
Given the ability of exercise-stimulated glucose uptake to bypass insulin resistance, there is great interest in developing exercise mimetic therapies. However, progress has been limited by technical and conceptual challenges. From a technical perspective, there is a lack of in vitro models of contraction, and it is difficult to conduct live analysis in the contracting muscle of animal models.
From a conceptual perspective, it is unclear how GLUT4 is mobilized to the sarcolemma in response to exercise, and current models are probably overly simplistic. In addition, recent proteomic analyses have identified thousands of proteins that are changed with exercise (154, 157), with many of those likely to contribute to exercise-stimulated glucose uptake, suggesting that many key components of the mechanism remain to be discovered. With no defined mechanism for exercise-stimulated glucose uptake, it is challenging to leverage any one aspect of the contributing pathways and recapitulate the benefits of exercise for therapeutic purposes.
There have been multiple attempts to develop exercise mimetics, as outlined in Table 2. In 2007, it was reported that GW501516, a PPARδ receptor agonist, improves training performance in mice (211). This result was widely publicized by media outlets as “exercise-in-a-pill.” However, this drug had previously been in clinical trials as a therapeutic for T2D (NCT00388180, NCT00841217) and cardiovascular disease (CVD, NCT00318617) and was abandoned by the manufacturer when two abstracts reported that this agonist causes cancer in rodents (rats and mice), even though these studies were never published in peer-reviewed journals at the time. Later, studies emerged demonstrating the tumor-promoting effects of GW501516 (239, 240, 333, 358).
Table 2.
Candidate Exercise Mimetic Targets and Drugs
| Target | Function | Drug | Drug function | Drug effect | Natural/synthetic | References |
|---|---|---|---|---|---|---|
| AMPK | Master metabolic sensor-induces mitochondrial biogenesis and fatty acid oxidation | AICAR | Directly activates AMPK | Increased glucose uptake and fatty acid oxidation, enhanced endurance, protection against obesity | Synthetic | (211) |
| Compound 14 (Cpd14)a | Increases ZMP via ATIC inhibition, a metabolite that activates AMPK | Reduced weight gain, improved glucose tolerance | Synthetic | (11) | ||
| Metformina | Mildly inhibits mitochondrial complex 1 and activates AMPK | Increased glucose tolerance via reduced hepatic production, increased glucose uptake | Synthetic | (28) | ||
| R419 | Activates AMPK by inhibiting mitochondrial complex 1; decreases MAPK signaling in neurons | Improved insulin sensitivity, insulin-stimulated glucose uptake, mitochondrial function, and exercise capacity; in neurons can inhibit pain | Synthetic | (189, 196) | ||
| O304 | Suppresses dephosphorylation of pAMPK | Increased glucose uptake in skeletal muscle; reduced β-cell stress, plasma glucose, and blood pressure; exercise mimetic effects in rodent hearts | Synthetic | (293) | ||
| SIRT1 | Mediates gene activity in response to nutrient availability, enhances fat oxidation | Resveratrol | Indirectly activates SIRT1 via AMPK activation | Increased PGC1α in skeletal muscle, mitochondrial biogenesis, fatty acid transport, and oxidative metabolism; protection against obesity | Natural—found in red grapes | (34, 36, 156) |
| SIRT1 | Mediates gene activity in response to nutrient availability, enhances fat oxidation | Resveratrol | Indirectly activates SIRT1 via AMPK activation | Increased PGC1α in skeletal muscle, mitochondrial biogenesis, fatty acid transport, and oxidative metabolism; protection against obesity | Natural—found in red grapes | (34, 36, 156) |
| NR (nicotinamide riboside) | NAD+ precursor that activates SIRT1 | Increased oxidative metabolism; improved insulin sensitivity, exercise performance, and glucose tolerance; reduced weight gain | Natural—found in milk, form of vitamin B3 | (35, 61, 62, 316) | ||
| MRL-45696 | Inhibits PARP1 (NAD+ consuming enzyme) | Blunted weight gain, reduced fat accumulation, higher energy expenditure, enhanced mitochondrial function, longer running, and higher VO2 max |
Derived from niraparib (ovarian cancer treatment) | (235) | ||
| REV-ERBα | Nuclear receptor important in metabolism, exercise, and circadian rhythm | SR9009/SR9011 | REV-ERBα ligands that inhibit REV-ERB target gene expression | Improved endurance and stamina, increased mitochondrial abundance and function in skeletal muscle | Synthetic | (286, 345) |
| PPARδ | Regulates fatty acid metabolism | GW501516 | PPARδ ligand | Increased fatty acid oxidation and energy expenditure; works synergistically with AICAR to improve oxidative metabolism; poor pharmacokinetics, causes tumors | Synthetic | (211) |
| ERRγ | Regulates mitochondria | GSK4716a | ERRγ ligand | Improved mitochondrial biogenesis and fatty acid oxidation | Synthetic | (63, 212, 249) |
Elicits the same effects as exercise training but not yet tested in exercise models.
Numerous different types of AMPK activators have been explored as potential exercise mimetics, given that AMPK elicits insulin-sensitizing effects and increases glucose uptake. Drugs that have been found to agonize AMPK include Compound 14 (11), Metformin (28), R419 (189, 196), and O304 (293), and AICAR. AICAR increases glucose uptake and fatty acid oxidation (198), enhances endurance via regulation of PPARδ-dependent genes and protects against obesity (211). AICAR is a direct activator of AMPK, as it is converted into an analog of adenosine monophosphate (AMP) that is required for stimulation of AMPK (262). AICAR primarily activates the AMPKα2 isoform (209), although it can also activate AMPKα1 but to a much lesser extent (126). AICAR has the capacity to elicit a multi-faceted array of signals that culminate in an “exercise phenotype,” given that AMPK can impinge upon an array of signaling pathways, and that AMPK-defective mouse models have reduced exercise capacity, supporting this concept (221, 302). Indeed, AICAR is such a potent exercise mimetic that it, and all activators of AMPK, have been officially declared banned substances by the World Anti-doping Agency, due to its supposed performance-enhancing capabilities (http://www.wada-ama.org).
Although it has already been suggested that metformin works by activating AMPK to elicit its insulin-sensitizing capabilities in adipose, liver and skeletal muscle (75, 168, 299), a recent report suggests that metformin’s mechanism of action is dependent on the dosage: pharmacological concentrations improve mitochondrial respiration, whereas supra-pharmacological concentrations of metformin inhibit mitochondrial activity (335).
Although multiple exercise mimetic targets and drugs/agonists have been studied, there are no confirmed candidates that can function as “exercise-in-a-pill.” This is in part because many candidate exercise mimetic therapies are in the early stages of development, with promising studies in rodents or in vitro models, but they have not been tested in in vivo exercise studies per se. In addition, early clinical trial results have not always supported the conclusions from animal studies. For example, the SIRT1 agonist nicotinamide riboside (NR) improved insulin sensitivity and exercise capacity in rodents (35, 316). However, when tested as a supplement in obese human males, the drug did not improve exercise endurance, insulin sensitivity, or any of the other parameters tested (61). In addition, as mentioned for GW501516, many exercise mimetics have severe side effects that prevent progress in clinical trials. That being said, exercise in excess can also be harmful to the body, leading to conditions like rhabdomyolysis, which can cause severe muscle damage and kidney failure (315). As the technical and conceptual challenges are overcome, it is anticipated that more candidate exercise mimetics will enter the development pipeline for further evaluation.
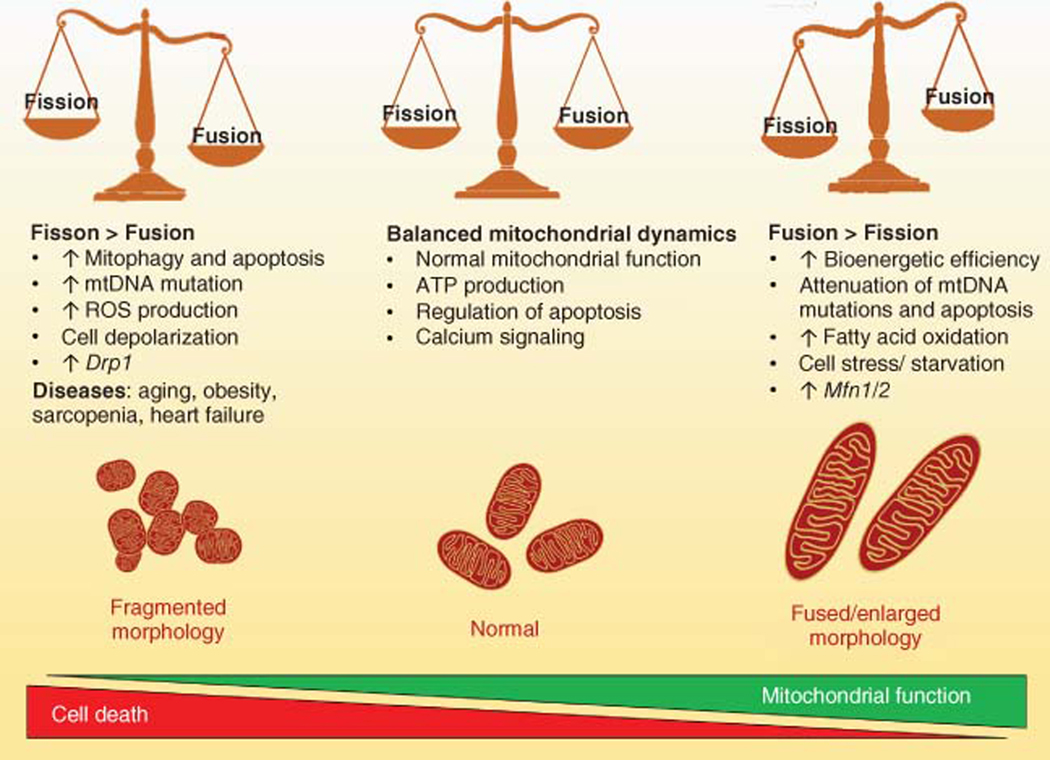
Role for Mitochondria in Insulin Resistance
Mitochondria, the powerhouses of the cell, are dynamic organelles that cycle between fusion and fission states. Mitochondrial dynamics are central to mitochondrial function and integrity and are carefully regulated. When mitochondrial fission is too high there is an increase in mitophagy, and subsequently, apoptosis. Increased fission is associated with aging and aging-related diseases like sarcopenia (100), heart failure (46), and neurodegeneration (287). In contrast, when fusion outweighs fission, there is an increase in mtDNA and mitochondrial bioenergetics. Fusion is usually associated with improved mitochondrial function, and exercise increases mitochondrial elongation (14). However, excessive mitochondrial enlargement and elongation can be associated with starvation and cell stress, which can damage mitochondria and increase ROS production (83). These changes have been linked with muscle aging (161), though many counter-studies have found fission to be associated with sarcopenia and aging (Figure 4).
Figure 4.
The role of mitochondrial dynamics in maintaining skeletal muscle function and preventing disease. Center: mitochondrial fission and fusion are balanced and under these conditions, there is normal mitochondrial function, ATP production, and cell death. Left: fission outweighs fusion, so mitochondria become fragmented, there is an increase in mitophagy and cell death, a reduction in mitochondrial function, and increased ROS production. This contributes to diseases including aging, obesity, and insulin resistance. Right: mitochondrial fusion outweighs fission, leading to increased mitochondrial function, reduced cell death, elongated mitochondria, and increased fatty acid oxidation. However, this can also cause cell stress and starvation due to the high demands of the large mitochondria.
The skeletal muscle has a high mitochondrial density that is second only to the heart, as measured by mtDNA copy number in humans; mtDNA copy number positively correlates with mitochondrial mass and respiratory activity (60). The mitochondria play a vital role in skeletal muscle metabolism, energy supply, and apoptosis. As such, mitochondrial dysfunction in skeletal muscle is associated with a variety of diseases, like muscular dystrophies (322), aging (57, 172), sarcopenia (100), and insulin resistance (23, 200).
High-fat diet causes mitochondrial dysfunction, decreases mitochondrial number in human skeletal muscle (23, 200, 254), changes the mitochondrial structure, and reduces oxidative phosphorylation and mitochondrial respiration (15, 44). Another hallmark of high-fat diet-fed mice is increased mitochondrial fission and mitophagy (314). In addition, mitochondrial dynamics and structure play a large role in mitochondrial function and integrity. Changes in mitochondrial size and structure, mediated by changes in fission or fusion, are central to complications in obesity and diabetes (Figure 4). Indeed, a 40% high-fat diet-fed to mice for only 4weeks was reported to increase mitochondrial fission and vacuolization in oocytes (185). Similarly, increases in mitochondrial fission and dysfunction in palmitate-treated skeletal muscle cells (122), and muscle of obese mice (175) is observed.
Exercise appears to improve mitochondrial function. For example, exercise can induce mitochondrial elongation (14). Exercise-trained mice show improved mitochondrial function and have increased spontaneous physical activity levels compared to untrained controls (53). Also, mitochondrial dynamics are tailored to muscle fiber type, with oxidative fibers (Type I, IIA) having elongated and highly fused mitochondria relative to glycolytic (Type IIX, IIB) fiber types (201).
Mitochondria are of special interest when considering exercise mimetics and insulin resistance therapeutics. Mitochondrial dysfunction can cause disease, and some view mitochondrial bioenergetics and remodeling as crucial elements of a successful exercise mimetic, due to the importance of mitochondria in the metabolic benefits of exercise. It has been proposed that an ideal exercise mimetic would mimic the benefits of fitness by inducing mitochondrial remodeling, increased oxidative phosphorylation, and fatty acid metabolism (68).
Concluding Remarks
Insulin action on skeletal muscle is pivotal in metabolic homeostasis, and insulin action in skeletal muscle is an important target in generating therapeutics that can combat metabolic disease. In this article, we have discussed the interplay among obesity, aging, exercise, and the skeletal muscle. We have described the importance of exercise as a therapeutic, not only for insulin resistance but also for a variety of skeletal muscle metabolic disorders, as well as general health. We have highlighted the therapeutic potential of exercise mimetics and the current limitations in producing these therapeutic agents.
Didactic Synopsis.
Major teaching points
Type 2 diabetes is a worldwide epidemic characterized by peripheral insulin resistance and insulin insufficiency.
Skeletal muscle plays a major role in metabolic disease, including insulin resistance, diabetes, obesity, aging, and sarcopenia.
Skeletal muscle can function as an endocrine organ that releases myokines to facilitate tissue cross talk. Myokine release is increased with exercise, with some myokines having anti-inflammatory potential.
Glucose uptake into the skeletal muscle can occur via multiple signaling pathways that lead to the translocation of the glucose transporter GLUT4; there are separate pathways for exercise-stimulated and insulin-stimulated glucose uptake.
Exercise can reverse insulin resistance, and researchers are seeking exercise mimetic therapies that target the mechanisms underlying the benefits of exercise.
The SNARE proteins regulate GLUT4 translocation and there is a growing understanding that the SNAREs, especially STX4, regulate metabolism and disease through glucose uptake.
Acknowledgments
This work was supported by grants from the National Institutes of Health (DK067912, DK1129712, and DK102233 to D.C.T.), as well as the Helen and Payson Chu fellowship to K.E.M. We would like to extend our thanks to Nancy Linford, PhD, for provided editing assistance.
Footnotes
Related Articles
Insulin Resistance
Molecular Aspects of Insulin Signaling
Obesity
Regulation of Glucose Metabolism in Skeletal Muscle Regulation of Glucose Transporters by Insulin and Exercise: Cellular Effects and Implications for Diabetes
Regulation of Muscle Glucose Uptake in Vivo
Skeletal Muscle Adaptability: Significance for Metabolism and Performance
Diseases of Skeletal Muscle
Exocytosis and Synaptic Vesicle Function
Cellular Processes Integrating the Metabolic Response to Exercise
Lack of Exercise is A Major Cause of Chronic Disease
Metabolic Syndrome and Insulin Resistance: Underlying Causes and Modification by Exercise Training
Muscle as a Secretory Organ
References
- 1.Ahirwar AK, Jain A, Goswami B, Bhatnagar MK, Bhatacharjee J. Imbalance between protective (adiponectin) and prothrombotic (Plasminogen Activator Inhibitor-1) adipokines in metabolic syndrome. Diabetes Metab Syndr 8: 152–155, 2014. [DOI] [PubMed] [Google Scholar]
- 2.Akbar H, Duan X, Piatt R, Saleem S, Davis AK, Tandon NN, Bergmeier W, Zheng Y. Small molecule targeting the Rac1-NOX2 interaction prevents collagen-related peptide and thrombin-induced reactive oxygen species generation and platelet activation. J Thromb Haemost 16: 2083–2096, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alessi DR, Andjelkovic M, Caudwell B, Cron P, Morrice N, Cohen P, Hemmings BA. Mechanism of activation of protein kinase B by insulin and IGF-1. EMBO J 15: 6541–6551, 1996. [PMC free article] [PubMed] [Google Scholar]
- 4.Alessi DR, James SR, Downes CP, Holmes AB, Gaffney PR, Reese CB, Cohen P. Characterization of a 3-phosphoinositide-dependent protein kinase which phosphorylates and activates protein kinase Balpha. Curr Biol 7: 261–269, 1997. [DOI] [PubMed] [Google Scholar]
- 5.Almendro V, Busquets S, Ametller E, Carbo N, Figueras M, Fuster G, Argiles JM, Lopez-Soriano FJ. Effects of interleukin-15 on lipid oxidation: Disposal of an oral [(14)C]-triolein load. Biochim Biophys Acta 1761: 37–42, 2006. [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Standards of Medical Care in Diabetes—2011. Diabetes Care 34: S11–S61, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care 40: S11–S24, 2017. [DOI] [PubMed] [Google Scholar]
- 8.Andersen P, Saltin B. Maximal perfusion of skeletal muscle in man. J Physiol 366: 233–249, 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angin Y, Schwenk RW, Nergiz-Unal R, Hoebers N, Heemskerk JWM, Kuijpers MJ, Coumans WA, van Zandvoort MA, Bonen A, Neumann D, Glatz JFC, Luiken JJFP. Calcium signaling recruits substrate transporters GLUT4 and CD36 to the sarcolemma without increasing cardiac substrate uptake. Am J Physiol Endocrinol Metab 307: E225–E236, 2014. [DOI] [PubMed] [Google Scholar]
- 10.Araya R, Liberona JL, Cardenas JC, Riveros N, Estrada M, Powell JA, Carrasco MA, Jaimovich E. Dihydropyridine receptors as voltage sensors for a depolarization-evoked, IP3R-mediated, slow calcium signal in skeletal muscle cells. J Gen Physiol 121: 3–16, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asby DJ, Cuda F, Beyaert M, Houghton FD, Cagampang FR, Tavassoli A. AMPK activation via modulation of de novo purine biosynthesis with an inhibitor of ATIC homodimerization. Chem Biol 22: 838–848, 2015. [DOI] [PubMed] [Google Scholar]
- 12.Aslamy A, Oh E, Olson EM, Zhang J, Ahn M, Moin ASM, Tunduguru R, Salunkhe VA, Veluthakal R, Thurmond DC. Doc2b protects beta-cells against inflammatory damage and enhances function. Diabetes 67: 1332–1344, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aversa Z, Bonetto A, Penna F, Costelli P, Di Rienzo G, Lacitignola A, Baccino FM, Ziparo V, Mercantini P, Fanelli FR. Changes in myostatin signaling in non-weight-losing cancer patients. Ann Surg Oncol 19: 1350–1356, 2012. [DOI] [PubMed] [Google Scholar]
- 14.Axelrod CL, Fealy CE, Mulya A, Kirwan JP. Exercise training remodels human skeletal muscle mitochondrial fission and fusion machinery towards a pro-elongation phenotype. Acta Physiol (Oxf) 225: e13216, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bach D, Pich S, Soriano FX, Vega N, Baumgartner B, Oriola J, Daugaard JR, Lloberas J, Camps M, Zierath JR, Rabasa-Lhoret R, Wallberg-Henriksson H, Laville M, Palacin M, Vidal H, Rivera F, Brand M, Zorzano A. Mitofusin-2 determines mitochondrial network architecture and mitochondrial metabolism. A novel regulatory mechanism altered in obesity. J Biol Chem 278: 17190–17197, 2003. [DOI] [PubMed] [Google Scholar]
- 16.Bai L, Wang Y, Fan J, Chen Y, Ji W, Qu A, Xu P, James DE, Xu T. Dissecting multiple steps of GLUT4 trafficking and identifying the sites of insulin action. Cell Metab 5: 47–57, 2007. [DOI] [PubMed] [Google Scholar]
- 17.Bailetti D, Bertoccini L, Mancina RM, Barchetta I, Capoccia D, Cossu E, Pujia A, Lenzi A, Leonetti F, Cavallo MG, Romeo S, Baroni MG. ANGPTL4 gene E40K variation protects against obesity-associated dyslipidemia in participants with obesity. Obes Sci Pract 5: 83–90, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balon TW, Nadler JL. Evidence that nitric oxide increases glucose transport in skeletal muscle. J Appl Physiol 82: 359–363, 1997. [DOI] [PubMed] [Google Scholar]
- 19.Barnes BR, Marklund S, Steiler TL, Walter M, Hjalm G, Amarger V, Mahlapuu M, Leng Y, Johansson C, Galuska D, Lindgren K, Abrink M, Stapleton D, Zierath JR, Andersson L. The 5′-AMP-activated protein kinase gamma3 isoform has a key role in carbohydrate and lipid metabolism in glycolytic skeletal muscle. J Biol Chem 279: 38441–38447, 2004. [DOI] [PubMed] [Google Scholar]
- 20.Bastard JP, Maachi M, Van Nhieu JT, Jardel C, Bruckert E, Grimaldi A, Robert JJ, Capeau J, Hainque B. Adipose tissue IL-6 content correlates with resistance to insulin activation of glucose uptake both in vivo and in vitro. J Clin Endocrinol Metab 87: 2084–2089, 2002. [DOI] [PubMed] [Google Scholar]
- 21.Benny Klimek ME, Aydogdu T, Link MJ, Pons M, Koniaris LG, Zimmers TA. Acute inhibition of myostatin-family proteins preserves skeletal muscle in mouse models of cancer cachexia. Biochem Biophys Res Commun 391: 1548–1554, 2010. [DOI] [PubMed] [Google Scholar]
- 22.Bergen HR 3rd, Farr JN, Vanderboom PM, Atkinson EJ, White TA, Singh RJ, Khosla S, LeBrasseur NK. Myostatin as a mediator of sarcopenia versus homeostatic regulator of muscle mass: Insights using a new mass spectrometry-based assay. Skelet Muscle 5: 21, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonnard C, Durand A, Peyrol S, Chanseaume E, Chauvin M-A, Morio B, Vidal H, Rieusset J. Mitochondrial dysfunction results from oxidative stress in the skeletal muscle of diet-induced insulin-resistant mice. J Clin Invest 118: 789–800, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Booth FW, Laye MJ, Roberts MD. Lifetime sedentary living accelerates some aspects of secondary aging. J Appl Physiol (1985) 111: 1497–1504, 2011. [DOI] [PubMed] [Google Scholar]
- 25.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol 2: 1143–1211, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bostrom P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, Rasbach KA, Bostrom EA, Choi JH, Long JZ, Kajimura S, Zingaretti MC, Vind BF, Tu H, Cinti S, Hojlund K, Gygi SP, Spiegelman BM. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 481: 463–468, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradley SJ, Kingwell BA, McConell GK. Nitric oxide synthase inhibition reduces leg glucose uptake but not blood flow during dynamic exercise in humans. Diabetes 48: 1815–1821, 1999. [DOI] [PubMed] [Google Scholar]
- 28.Brunmair B, Staniek K, Gras F, Scharf N, Althaym A, Clara R, Roden M, Gnaiger E, Nohl H, Waldhausl W, Furnsinn C. Thiazolidinediones, like metformin, inhibit respiratory complex I: A common mechanism contributing to their antidiabetic actions? Diabetes 53: 1052–1059, 2004. [DOI] [PubMed] [Google Scholar]
- 29.Bruss MD, Arias EB, Lienhard GE, Cartee GD. Increased phosphorylation of Akt substrate of 160 kDa (AS160) in rat skeletal muscle in response to insulin or contractile activity. Diabetes 54: 41–50, 2005. [DOI] [PubMed] [Google Scholar]
- 30.Bullen JW, Balsbaugh JL, Chanda D, Shabanowitz J, Hunt DF, Neumann D, Hart GW. Cross-talk between two essential nutrient-sensitive enzymes: O-GlcNAc TRANSFERASE (OGT) and AMP-ACTIVATED PROTEIN KINASE (AMPK). J Biol Chem 289: 10592–10606, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Busquets S, Figueras M, Almendro V, Lopez-Soriano FJ, Argiles JM. Interleukin-15 increases glucose uptake in skeletal muscle. An antidiabetogenic effect of the cytokine. Biochim Biophys Acta 1760: 1613–1617, 2006. [DOI] [PubMed] [Google Scholar]
- 32.Calderón JC, Bolaños P, Caputo C. The excitation-contraction coupling mechanism in skeletal muscle. Biophys Rev 6: 133–160, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campbell C, McMillan HJ, Mah JK, Tarnopolsky M, Selby K, McClure T, Wilson DM, Sherman ML, Escolar D, Attie KM. Myostatin inhibitor ACE-031 treatment of ambulatory boys with Duchenne muscular dystrophy: Results of a randomized, placebo-controlled clinical trial. Muscle Nerve 55: 458–464, 2017. [DOI] [PubMed] [Google Scholar]
- 34.Canto C, Gerhart-Hines Z, Feige JN, Lagouge M, Noriega L, Milne JC, Elliott PJ, Puigserver P, Auwerx J. AMPK regulates energy expenditure by modulating NAD+ metabolism and SIRT1 activity. Nature 458: 1056–1060, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Canto C, Houtkooper RH, Pirinen E, Youn DY, Oosterveer MH, Cen Y, Fernandez-Marcos PJ, Yamamoto H, Andreux PA, Cettour-Rose P, Gademann K, Rinsch C, Schoonjans K, Sauve AA, Auwerx J. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab 15: 838–847, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Canto C, Jiang LQ, Deshmukh AS, Mataki C, Coste A, Lagouge M, Zierath JR, Auwerx J. Interdependence of AMPK and SIRT1 for metabolic adaptation to fasting and exercise in skeletal muscle. Cell Metab 11: 213–219, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carey AL, Bruce CR, Sacchetti M, Anderson MJ, Olsen DB, Saltin B, Hawley JA, Febbraio MA. Interleukin-6 and tumor necrosis factor-alpha are not increased in patients with Type 2 diabetes: Evidence that plasma interleukin-6 is related to fat mass and not insulin responsiveness. Diabetologia 47: 1029–1037, 2004. [DOI] [PubMed] [Google Scholar]
- 38.Carey AL, Steinberg GR, Macaulay SL, Thomas WG, Holmes AG, Ramm G, Prelovsek O, Hohnen-Behrens C, Watt MJ, James DE, Kemp BE, Pedersen BK, Febbraio MA. Interleukin-6 increases insulin-stimulated glucose disposal in humans and glucose uptake and fatty acid oxidation in vitro via AMP-activated protein kinase. Diabetes 55: 2688–2697, 2006. [DOI] [PubMed] [Google Scholar]
- 39.Carling D, Hardie DG. The substrate and sequence specificity of the AMP-activated protein kinase. Phosphorylation of glycogen synthase and phosphorylase kinase. Biochim Biophys Acta 1012: 81–86, 1989. [DOI] [PubMed] [Google Scholar]
- 40.Catoire M, Mensink M, Boekschoten MV, Hangelbroek R, Muller M, Schrauwen P, Kersten S. Pronounced effects of acute endurance exercise on gene expression in resting and exercising human skeletal muscle. PLoS One 7: e51066, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. National Diabetes Statistics Report. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services, 2017. [Google Scholar]
- 42.Chambers MA, Moylan JS, Smith JD, Goodyear LJ, Reid MB. Stretch-stimulated glucose uptake in skeletal muscle is mediated by reactive oxygen species and p38 MAP-kinase. J Physiol 587: 3363–3373, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan KL, Boroumand P, Milanski M, Pillon NJ, Bilan PJ, Klip A. Deconstructing metabolic inflammation using cellular systems. Am J Physiol Endocrinol Metab 312: E339–E347, 2017. [DOI] [PubMed] [Google Scholar]
- 44.Chen D, Li X, Zhang L, Zhu M, Gao L. A high-fat diet impairs mitochondrial biogenesis, mitochondrial dynamics, and the respiratory chain complex in rat myocardial tissues. J Cell Biochem 119: 9602, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen G, Liu P, Thurmond DC, Elmendorf JS. Glucosamine-induced insulin resistance is coupled to O-linked glycosylation of Munc18c. FEBS Lett 534: 54–60, 2003. [DOI] [PubMed] [Google Scholar]
- 46.Chen L, Gong Q, Stice JP, Knowlton AA. Mitochondrial OPA1, apoptosis, and heart failure. Cardiovasc Res 84: 91–99, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen S, Murphy J, Toth R, Campbell DG, Morrice NA, Mackintosh C. Complementary regulation of TBC1D1 and AS160 by growth factors, insulin and AMPK activators. Biochem J 409: 449–459, 2008. [DOI] [PubMed] [Google Scholar]
- 48.Chen Z, Heierhorst J, Mann RJ, Mitchelhill KI, Michell BJ, Witters LA, Lynch GS, Kemp BE, Stapleton D. Expression of the AMP-activated protein kinase beta1 and beta2 subunits in skeletal muscle. FEBS Lett 460: 343–348, 1999. [DOI] [PubMed] [Google Scholar]
- 49.Cheng H, Lederer W, Cannell M. Calcium sparks: Elementary events underlying excitation-contraction coupling in heart muscle. Science 262: 740–744, 1993. [DOI] [PubMed] [Google Scholar]
- 50.Chiang SH, Baumann CA, Kanzaki M, Thurmond DC, Watson RT, Neudauer CL, Macara IG, Pessin JE, Saltiel AR. Insulin-stimulated GLUT4 translocation requires the CAP-dependent activation of TC10. Nature 410: 944–948, 2001. [DOI] [PubMed] [Google Scholar]
- 51.Chiu TT, Jensen TE, Sylow L, Richter EA, Klip A. Rac1 signalling towards GLUT4/glucose uptake in skeletal muscle. Cell Signal 23: 1546–1554, 2011. [DOI] [PubMed] [Google Scholar]
- 52.Cho H, Mu J, Kim JK, Thorvaldsen JL, Chu Q, Crenshaw EB 3rd, Kaestner KH, Bartolomei MS, Shulman GI, Birnbaum MJ. Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKB beta). Science 292: 1728–1731, 2001. [DOI] [PubMed] [Google Scholar]
- 53.Chow LS, Greenlund LJ, Asmann YW, Short KR,McCrady SK, Levine JA, Nair KS. Impact of endurance training on murine spontaneous activity, muscle mitochondrial DNA abundance, gene transcripts, and function. J Appl Physiol (1985) 102: 1078–1089, 2007. [DOI] [PubMed] [Google Scholar]
- 54.Cleto LS, Oleto AF, Sousa LP, Barreto TO, Cruz JS, Penaforte CL, Magalhaes JC, Sousa-Franco J, Pinto KM, Campi-Azevedo AC, Rocha-Vieira E. Plasma cytokine response, lipid peroxidation and NF-kB activation in skeletal muscle following maximum progressive swimming. Braz J Med Biol Res 44: 546–552, 2011. [DOI] [PubMed] [Google Scholar]
- 55.Coderre L, Kandror KV, Vallega G, Pilch PF. Identification and characterization of an exercise-sensitive pool of glucose transporters in skeletal muscle. J Biol Chem 270: 27584–27588, 1995. [DOI] [PubMed] [Google Scholar]
- 56.Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR, Ohannesian JP, Marco CC, McKee LJ, Bauer TL, Caro JF. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med 334: 292–295, 1996. [DOI] [PubMed] [Google Scholar]
- 57.Corral-Debrinski M, Shoffner JM, Lott MT, Wallace DC. Association of mitochondrial DNA damage with aging and coronary atherosclerotic heart disease. Mutat Res 275: 169–180, 1992. [DOI] [PubMed] [Google Scholar]
- 58.DeFronzo RA, Jacot E, Jequier E, Maeder E, Wahren J, Felber JP. The effect of insulin on the disposal of intravenous glucose. Results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes 30: 1000–1007, 1981. [DOI] [PubMed] [Google Scholar]
- 59.DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 32 (Suppl 2): S157–S163, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.D’Erchia AM, Atlante A, Gadaleta G, Pavesi G, Chiara M, De Virgilio C, Manzari C, Mastropasqua F, Prazzoli GM, Picardi E, Gissi C, Horner D, Reyes A, Sbisà E, Tullo A, Pesole G. Tissue-specific mtDNA abundance from exome data and its correlation with mitochondrial transcription, mass and respiratory activity. Mitochondrion 20: 13–21, 2015. [DOI] [PubMed] [Google Scholar]
- 61.Dollerup OL, Christensen B, Svart M, Schmidt MS, Sulek K, Ringgaard S, Stodkilde-Jorgensen H, Moller N, Brenner C, Treebak JT, Jessen N. A randomized placebo-controlled clinical trial of nicotinamide riboside in obese men: Safety, insulin-sensitivity, and lipid-mobilizing effects. Am J Clin Nutr 108: 343–353, 2018. [DOI] [PubMed] [Google Scholar]
- 62.Dolopikou CF, Kourtzidis IA, Margaritelis NV, Vrabas IS, Koidou I, Kyparos A, Theodorou AA, Paschalis V, Nikolaidis MG. Acute nicotinamide riboside supplementation improves redox homeostasis and exercise performance in old individuals: A double-blind cross-over study. Eur J Nutr, 2019. DOI: 10.1007/s00394-019-01919-4. [DOI] [PubMed] [Google Scholar]
- 63.Dufour CR, Wilson BJ, Huss JM, Kelly DP, Alaynick WA, Downes M, Evans RM, Blanchette M, Giguere V. Genome-wide orchestration of cardiac functions by the orphan nuclear receptors ERRalpha and gamma. Cell Metab 5: 345–356, 2007. [DOI] [PubMed] [Google Scholar]
- 64.Dun AR, Rickman C, Duncan RR. The t-SNARE complex: A close up. Cell Mol Neurobiol 30: 1321–1326, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dyck JR, Gao G, Widmer J, Stapleton D, Fernandez CS, Kemp BE, Witters LA. Regulation of 5′-AMP-activated protein kinase activity by the noncatalytic beta and gamma subunits. J Biol Chem 271: 17798–17803, 1996. [DOI] [PubMed] [Google Scholar]
- 66.Dzamko N, Schertzer JD, Ryall JG, Steel R, Macaulay SL, Wee S, Chen ZP, Michell BJ, Oakhill JS, Watt MJ, Jorgensen SB, Lynch GS, Kemp BE, Steinberg GR. AMPK-independent pathways regulate skeletal muscle fatty acid oxidation. J Physiol 586: 5819–5831, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Egan D, Kim J, Shaw RJ, Guan KL. The autophagy initiating kinase ULK1 is regulated via opposing phosphorylation by AMPK and mTOR. Autophagy 7: 643–644, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fan W, Evans RM. Exercise mimetics: Impact on health and performance. Cell Metab 25: 242–247, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fasshauer D, Otto H, Eliason WK, Jahn R, Brunger AT. Structural changes are associated with soluble N-ethylmaleimide-sensitive fusion protein attachment protein receptor complex formation. J Biol Chem 272: 28036–28041, 1997. [DOI] [PubMed] [Google Scholar]
- 70.Fasshauer D, Sutton RB, Brunger AT, Jahn R. Conserved structural features of the synaptic fusion complex: SNARE proteins reclassified as Q- and R-SNAREs. Proc Natl Acad Sci U S A 95: 15781–15786, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fazakerley DJ, Holman GD, Marley A, James DE, Stockli J, Coster AC. Kinetic evidence for unique regulation of GLUT4 trafficking by insulin and AMP-activated protein kinase activators in L6 myotubes. J Biol Chem 285: 1653–1660, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ferrannini E, Simonson DC, Katz LD, Reichard G Jr, Bevilacqua S, Barrett EJ, Olsson M, DeFronzo RA. The disposal of an oral glucose load in patients with non-insulin-dependent diabetes. Metabolism 37: 79–85, 1988. [DOI] [PubMed] [Google Scholar]
- 73.Ferris LT, Williams JS, Shen CL. The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognitive function. Med Sci Sports Exerc 39: 728–734, 2007. [DOI] [PubMed] [Google Scholar]
- 74.Fink LN, Costford SR, Lee YS, Jensen TE, Bilan PJ, Oberbach A, Bluher M, Olefsky JM, Sams A, Klip A. Pro-inflammatory macrophages increase in skeletal muscle of high fat-fed mice and correlate with metabolic risk markers in humans. Obesity (Silver Spring) 22: 747–757, 2014. [DOI] [PubMed] [Google Scholar]
- 75.Ford RJ, Fullerton MD, Pinkosky SL, Day EA, Scott JW, Oakhill JS, Bujak AL, Smith BK, Crane JD, Blümer RM. Metformin and salicylate synergistically activate liver AMPK, inhibit lipogenesis and improve insulin sensitivity. Biochem J 468: 125–132, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Förstermann U, Sessa WC. Nitric oxide synthases: Regulation and function. Eur Heart J 33: 829–837d, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Foster LJ, Yaworsky K, Trimble WS, Klip A. SNAP23 promotes insulin-dependent glucose uptake in 3T3-L1 adipocytes: Possible interaction with cytoskeleton. Am J Phys 276: C1108–C1114, 1999. [DOI] [PubMed] [Google Scholar]
- 78.Frosig C, Pehmoller C, Birk JB, Richter EA, Wojtaszewski JF. Exercise-induced TBC1D1 Ser237 phosphorylation and 14–3-3 protein binding capacity in human skeletal muscle. J Physiol 588: 4539–4548, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fujii N, Hayashi T, Hirshman MF, Smith JT, Habinowski SA, Kaijser L, Mu J, Ljungqvist O, Birnbaum MJ, Witters LA, Thorell A, Goodyear LJ. Exercise induces isoform-specific increase in 5′AMP-activated protein kinase activity in human skeletal muscle. Biochem Biophys Res Commun 273: 1150–1155, 2000. [DOI] [PubMed] [Google Scholar]
- 80.Fukuda M, Mikoshiba K. Doc2gamma, a third isoform of double C2 protein, lacking calcium-dependent phospholipid binding activity. Biochem Biophys Res Commun 276: 626–632, 2000. [DOI] [PubMed] [Google Scholar]
- 81.Gallagher D, Kuznia P, Heshka S, Albu J, Heymsfield SB, Goodpaster B, Visser M, Harris TB. Adipose tissue in muscle: a novel depot similar in size to visceral adipose tissue. Am J Clin Nutr 81: 903–910, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Geng L, Liao B, Jin L, Huang Z, Triggle CR, Ding H, Zhang J, Huang Y, Lin Z, Xu A. Exercise alleviates obesity-induced metabolic dysfunction via enhancing FGF21 sensitivity in adipose tissues. Cell Rep 26: 2738–2752.e2734, 2019. [DOI] [PubMed] [Google Scholar]
- 83.Gomes LC, Di Benedetto G, Scorrano L. During autophagy mitochondria elongate, are spared from degradation and sustain cell viability. Nat Cell Biol 13: 589–598, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gomez-Merino D, Drogou C, Guezennec CY, Chennaoui M. Effects of chronic exercise on cytokine production in white adipose tissue and skeletal muscle of rats. Cytokine 40: 23–29, 2007. [DOI] [PubMed] [Google Scholar]
- 85.Gorgens SW, Eckardt K, Jensen J, Drevon CA, Eckel J. Exercise and regulation of adipokine and myokine production. Prog Mol Biol Transl Sci 135: 313–336, 2015. [DOI] [PubMed] [Google Scholar]
- 86.Gorgens SW, Raschke S, Holven KB, Jensen J, Eckardt K, Eckel J. Regulation of follistatin-like protein 1 expression and secretion in primary human skeletal muscle cells. Arch Physiol Biochem 119: 75–80, 2013. [DOI] [PubMed] [Google Scholar]
- 87.Haidet AM, Rizo L, Handy C, Umapathi P, Eagle A, Shilling C, Boue D, Martin PT, Sahenk Z, Mendell JR, Kaspar BK. Long-term enhancement of skeletal muscle mass and strength by single gene administration of myostatin inhibitors. Proc Natl Acad Sci 105: 4318–4322, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Handschin C, Chin S, Li P, Liu F, Maratos-Flier E, Lebrasseur NK, Yan Z, Spiegelman BM. Skeletal muscle fiber-type switching, exercise intolerance, and myopathy in PGC-1alpha muscle-specific knock-out animals. J Biol Chem 282: 30014–30021, 2007. [DOI] [PubMed] [Google Scholar]
- 89.Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes 19: 81–87, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Haugen F, Norheim F, Lian H, Wensaas AJ, Dueland S, Berg O, Funderud A, Skalhegg BS, Raastad T, Drevon CA. IL-7 is expressed and secreted by human skeletal muscle cells. Am J Physiol Cell Physiol 298: C807–C816, 2010. [DOI] [PubMed] [Google Scholar]
- 91.Hawley SA, Davison M, Woods A, Davies SP, Beri RK, Carling D, Hardie DG. Characterization of the AMP-activated protein kinase kinase from rat liver and identification of threonine 172 as the major site at which it phosphorylates AMP-activated protein kinase. J Biol Chem 271: 27879–27887, 1996. [DOI] [PubMed] [Google Scholar]
- 92.Hawley SA, Pan DA, Mustard KJ, Ross L, Bain J, Edelman AM, Frenguelli BG, Hardie DG. Calmodulin-dependent protein kinase kinase-beta is an alternative upstream kinase for AMP-activated protein kinase. Cell Metab 2: 9–19, 2005. [DOI] [PubMed] [Google Scholar]
- 93.Heber D, Ingles S, Ashley JM, Maxwell MH, Lyons RF, Elashoff RM. Clinical detection of sarcopenic obesity by bioelectrical impedance analysis. Am J Clin Nutr 64: 472S–477S, 1996. [DOI] [PubMed] [Google Scholar]
- 94.Heinonen I, Saltin B, Kemppainen J, Nuutila P, Knuuti J, Kalliokoski K, Hellsten Y. Effect of nitric oxidesynthase inhibition on the exchange of glucose and fatty acids in human skeletal muscle. Nutr Metab (Lond) 10: 43, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Heinonen I, Saltin B, Kemppainen J, Sipila HT, Oikonen V, Nuutila P, Knuuti J, Kalliokoski K, Hellsten Y. Skeletal muscle blood flow and oxygen uptake at rest and during exercise in humans: A pet study with nitric oxide and cyclooxygenase inhibition. Am J Physiol Heart Circ Physiol 300: H1510–H1517, 2011. [DOI] [PubMed] [Google Scholar]
- 96.Henningsen J, Rigbolt KT, Blagoev B, Pedersen BK, Kratchmarova I. Dynamics of the skeletal muscle secretome during myoblast differentiation. Mol Cell Proteomics 9: 2482–2496, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Henriquez-Olguin C, Knudsen JR, Raun SH, Li Z, Dalbram E, Treebak JT, Sylow L, Holmdahl R, Richter EA, Jaimovich E, Jensen TE. Cytosolic ROS production by NADPH oxidase 2 regulates muscle glucose uptake during exercise. Nat Commun 10: 4623, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Henríquez-Olguin C, Knudsen JR, Raun SH, Li Z, Sylow L, Richter EA, Jaimovich E, Jensen TE. OP-4 - NOX2 is a major ROS source in exercising muscle regulating glucose uptake. Free Radic Biol Med 120: S30, 2018. [Google Scholar]
- 99.Hill JJ, Davies MV, Pearson AA, Wang JH, Hewick RM, Wolfman NM, Qiu Y. The myostatin propeptide and the follistatin-related gene are inhibitory binding proteins of myostatin in normal serum. J Biol Chem 277: 40735–40741, 2002. [DOI] [PubMed] [Google Scholar]
- 100.Hiona A, Sanz A, Kujoth GC, Pamplona R, Seo AY, Hofer T, Someya S, Miyakawa T, Nakayama C, Samhan-Arias AK, Servais S, Barger JL, Portero-Otín M, Tanokura M, Prolla TA, Leeuwenburgh C. Mitochondrial DNA mutations induce mitochondrial dysfunction, apoptosis and sarcopenia in skeletal muscle of mitochondrial DNA mutator mice. PLoS One 5: e11468, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hittel DS, Berggren JR, Shearer J, Boyle K, Houmard JA. Increased secretion and expression of myostatin in skeletal muscle from extremely obese women. Diabetes 58: 30–38, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hoier B, Nordsborg N, Andersen S, Jensen L, Nybo L, Bangsbo J, Hellsten Y. Pro- and anti-angiogenic factors in human skeletal muscle in response to acute exercise and training. J Physiol 590: 595–606, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hojman P, Brolin C, Norgaard-Christensen N, Dethlefsen C, Lauenborg B, Olsen CK, Abom MM, Krag T, Gehl J, Pedersen BK. IL-6 release from muscles during exercise is stimulated by lactate-dependent protease activity. Am J Physiol Endocrinol Metab 316: E940–E947, 2019. [DOI] [PubMed] [Google Scholar]
- 104.Hollander P, Spellman C. Controversies in prediabetes: Do we have a diagnosis? Postgrad Med 124: 109–118, 2012. [DOI] [PubMed] [Google Scholar]
- 105.Horak M, Kuruczova D, Zlamal F, Tomandl J, Bienertova-Vasku J. Follistatin-like 1 is downregulated in morbidly and super obese centralEuropean population. Dis Markers 2018: 4140815, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Horie T, Ono K, Nagao K, Nishi H, Kinoshita M, Kawamura T, Wada H, Shimatsu A, Kita T, Hasegawa K. Oxidative stress induces GLUT4 translocation by activation of PI3-K/Akt and dual AMPK kinase in cardiac myocytes. J Cell Physiol 215: 733–742, 2008. [DOI] [PubMed] [Google Scholar]
- 107.Hu E, Liang P, Spiegelman BM. AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem 271: 10697–10703, 1996. [DOI] [PubMed] [Google Scholar]
- 108.Hundal HS, Ahmed A, Guma A, Mitsumoto Y, Marette A, Rennie MJ, Klip A. Biochemical and immunocytochemical localization of the ‘GLUT5 glucose transporter’ in human skeletal muscle. Biochem J 286 (Pt 2): 339–343, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hurley RL, Anderson KA, Franzone JM, Kemp BE, Means AR, Witters LA. The Ca2+/calmodulin-dependent protein kinase kinases are AMP-activated protein kinase kinases. J Biol Chem 280: 29060–29066, 2005. [DOI] [PubMed] [Google Scholar]
- 110.Ishikura S, Bilan PJ, Klip A. Rabs 8A and 14 are targets of the insulin-regulated Rab-GAP AS160 regulating GLUT4 traffic in muscle cells. Biochem Biophys Res Commun 353: 1074–1079, 2007. [DOI] [PubMed] [Google Scholar]
- 111.Jakobsen SN, Hardie DG, Morrice N, Tornqvist HE. 5′-AMP-activated protein kinase phosphorylates IRS-1 on Ser-789 in mouse C2C12 myotubes in response to 5-aminoimidazole-4-carboxamide riboside. J Biol Chem 276: 46912–46916, 2001. [DOI] [PubMed] [Google Scholar]
- 112.James DE, Brown R, Navarro J, Pilch PF. Insulin-regulatable tissues express a unique insulin-sensitive glucose transport protein. Nature 333: 183–185, 1988. [DOI] [PubMed] [Google Scholar]
- 113.JeBailey L, Rudich A, Huang X, Di Ciano-Oliveira C, Kapus A, Klip A. Skeletal muscle cells and adipocytes differ in their reliance on TC10 and Rac for insulin-induced actin remodeling. Mol Endocrinol 18: 359–372, 2004. [DOI] [PubMed] [Google Scholar]
- 114.JeBailey L, Wanono O, Niu W, Roessler J, Rudich A, Klip A. Ceramide- and oxidant-induced insulin resistance involve loss of insulin-dependent Rac-activation and actin remodeling in muscle cells. Diabetes 56: 394–403, 2007. [DOI] [PubMed] [Google Scholar]
- 115.Jedrychowski MP, Wrann CD, Paulo JA, Gerber KK, Szpyt J, Robinson MM, Nair KS, Gygi SP, Spiegelman BM. Detection and quantitation of circulating human irisin by tandem mass spectrometry. Cell Metab 22: 734–740, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jenkins A, Zhang SX, Gosmanova A, Aston C, Dashti A, Baker MZ, Lyons T, Ma JX. Increased serum pigment epithelium derived factor levels in Type 2 diabetes patients. Diabetes Res Clin Pract 82: e5–e7, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jensen TE, Angin Y, Sylow L, Richter EA. Is contraction-stimulated glucose transport feedforward regulated by Ca2+? Exp Physiol 99: 1562–1568, 2014. [DOI] [PubMed] [Google Scholar]
- 118.Jensen TE, Schjerling P, Viollet B, Wojtaszewski JF, Richter EA. AMPK alpha1 activation is required for stimulation of glucose uptake by twitch contraction, but not by H2O2, in mouse skeletal muscle. PLoS One 3: e2102, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jensen TE, Sylow L, Rose AJ, Madsen AB, Angin Y, Maarbjerg SJ, Richter EA. Contraction-stimulated glucose transport in muscle is controlled by AMPK and mechanical stress but not sarcoplasmatic reticulum Ca2+ release. Mol Metab 3: 742–753, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jewell JL, Oh E, Bennett SM, Meroueh SO, Thurmond DC. The tyrosine phosphorylation of Munc18c induces a switch in binding specificity from syntaxin 4 to Doc2beta. J Biol Chem 283: 21734–21746, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jewell JL, Oh E, Ramalingam L, Kalwat MA, Tagliabracci VS, Tackett L, Elmendorf JS, Thurmond DC. Munc18c phosphorylation by the insulin receptor links cell signaling directly to SNARE exocytosis. J Cell Biol 193: 185–199, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jheng HF, Tsai PJ, Guo SM, Kuo LH, Chang CS, Su IJ, Chang CR, Tsai YS. Mitochondrial fission contributes to mitochondrial dysfunction and insulin resistance in skeletal muscle. Mol Cell Biol 32: 309319, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jimenez-Maldonado A, Virgen-Ortiz A, Lemus M, Castro-Rodriguez E, Cerna-Cortes J, Muniz J, Montero S, Roces E. Effects of moderateand high-intensity chronic exercise on the adiponectin levels in slow-twitch and fast-twitch muscles in rats. Medicina (Kaunas) 55: 291, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Joan Flynn CM, Aparicio-Siegmund S, Rose-John S, Garbers C. ID: 207: Cell-surface expression of the IL-6R is controlled by proteolysis, internalization and recycling. Cytokine 76: 102, 2015. [Google Scholar]
- 125.Jones F, Harris P, McGee L. Adherence to prescribed exercise. In: Myers L, Midence K, editors. Adherence to Treatment in Medical Conditions. Amsterdam: Harwood, 1998, p. 343–363. [Google Scholar]
- 126.Jorgensen SB, Viollet B, Andreelli F, Frosig C, Birk JB, Schjerling P, Vaulont S, Richter EA, Wojtaszewski JF. Knockout of the alpha2 but not alpha1 5′-AMP-activated protein kinase isoform abolishes 5-aminoimidazole-4-carboxamide-1-beta-4-ribofuranosidebut not contraction-induced glucose uptake in skeletal muscle. J Biol Chem 279: 1070–1079, 2004. [DOI] [PubMed] [Google Scholar]
- 127.Ju JS, Gitcho MA, Casmaer CA, Patil PB, Han DG, Spencer SA, Fisher JS. Potentiation of insulin-stimulated glucose transport by the AMP-activated protein kinase. Am J Physiol Cell Physiol 292: C564–C572, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kaddai V, Gonzalez T, Bolla M, Le Marchand-Brustel Y, Cormont M. The nitric oxide-donating derivative of acetylsalicylic acid, NCX 4016, stimulates glucose transport and glucose transporters translocation in 3T3-L1 adipocytes. Am J Physiol Endocrinol Metab 295: E162–E169, 2008. [DOI] [PubMed] [Google Scholar]
- 129.Kadoglou NP, Perrea D, Iliadis F, Angelopoulou N, Liapis C, Alevizos M. Exercise reduces resistin and inflammatory cytokines in patients with type 2 diabetes. Diabetes Care 30: 719–721, 2007. [DOI] [PubMed] [Google Scholar]
- 130.Kamiya A, Ohsawa I, Fujii T, Nagai M, Yamanouchi K, Oshida Y, Sato Y. A clinical survey on the compliance of exercise therapy for diabetic outpatients. Diabetes Res Clin Pract 27: 141–145, 1995. [DOI] [PubMed] [Google Scholar]
- 131.Karacabey K. The effect of exercise on leptin, insulin, cortisol and lipid profiles in obese children. J Int Med Res 37: 1472–1478, 2009. [DOI] [PubMed] [Google Scholar]
- 132.Karlsson HK, Chibalin AV, Koistinen HA, Yang J, Koumanov F, Wallberg-Henriksson H, Zierath JR, Holman GD. Kinetics of GLUT4 trafficking in rat and human skeletal muscle. Diabetes 58: 847–854, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Karlsson HK, Zierath JR, Kane S, Krook A, Lienhard GE, Wallberg-Henriksson H. Insulin-stimulated phosphorylation of the Akt substrate AS160 is impaired in skeletal muscle of type 2 diabetic subjects. Diabetes 54: 1692–1697, 2005. [DOI] [PubMed] [Google Scholar]
- 134.Kawanishi M, Tamori Y, Okazawa H, Araki S, Shinoda H, Kasuga M. Role of SNAP23 in insulin-induced translocation of GLUT4 in 3T3-L1 adipocytes. Mediation of complex formation between syntaxin4 and VAMP2. J Biol Chem 275: 8240–8247, 2000. [DOI] [PubMed] [Google Scholar]
- 135.Kazemi F. The correlation of resistance exercise-induced myostatin with insulin resistance and plasma cytokines in healthy young men. J Endocrinol Investig 39: 383–388, 2016. [DOI] [PubMed] [Google Scholar]
- 136.Ke B, Oh E, Thurmond DC. Doc2beta is a novel Munc18c-interacting partner and positive effector of syntaxin 4-mediated exocytosis. J Biol Chem 282: 21786–21797, 2007. [DOI] [PubMed] [Google Scholar]
- 137.Keller C, Steensberg A, Pilegaard H, Osada T, Saltin B, Pedersen BK, Neufer PD. Transcriptional activation of the IL-6 gene in human contracting skeletal muscle: Influence of muscle glycogen content. FASEB J 15: 2748–2750, 2001. [DOI] [PubMed] [Google Scholar]
- 138.Kerris JP, Betik AC, Li J, McConell GK. Passive stretch regulates skeletal muscle glucose uptake independent of nitric oxide synthase. J Appl Physiol (1985) 126: 239–245, 2019. [DOI] [PubMed] [Google Scholar]
- 139.Kersten S, Lichtenstein L, Steenbergen E, Mudde K, Hendriks HF, Hesselink MK, Schrauwen P, Muller M. Caloric restriction and exercise increase plasma ANGPTL4 levels in humans via elevated free fatty acids. Arterioscler Thromb Vasc Biol 29: 969–974, 2009. [DOI] [PubMed] [Google Scholar]
- 140.Khan IM, Perrard X-Y, Brunner G, Lui H, Sparks LM, Smith SR, Wang X, Shi Z-Z, Lewis DE, Wu H. Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int J Obes (Lond) 39: 1607, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med 31: 643–650, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kimura N, Tokunaga C, Dalal S, Richardson C, Yoshino K, Hara K, Kemp BE, Witters LA, Mimura O, Yonezawa K. A possible linkage between AMP-activated protein kinase (AMPK) and mammalian target of rapamycin (mTOR) signalling pathway. Genes Cells 8: 65–79, 2003. [DOI] [PubMed] [Google Scholar]
- 143.Kingwell BA, Formosa M, Muhlmann M, Bradley SJ, McConell GK. Nitric oxide synthase inhibition reduces glucose uptake during exercise in individuals with type 2 diabetes more than in control subjects. Diabetes 51: 2572–2580, 2002. [DOI] [PubMed] [Google Scholar]
- 144.Kjobsted R, Munk-Hansen N, Birk JB, Foretz M, Viollet B, Bjornholm M, Zierath JR, Treebak JT, Wojtaszewski JF. Enhanced muscle insulin sensitivity after contraction/exercise is mediated by AMPK. Diabetes 66: 598–612, 2017. [DOI] [PubMed] [Google Scholar]
- 145.Kjobsted R, Roll JLW, Jorgensen NO, Birk JB, Foretz M, Viollet B, Chadt A, Al-Hasani H, Wojtaszewski JFP. AMPK and TBC1D1 regulate muscle glucose uptake after, but not during, exercise and contraction. Diabetes 68: 1427–1440, 2019. [DOI] [PubMed] [Google Scholar]
- 146.Klip A, McGraw TE, James DE. Thirty sweet years of GLUT4. J Biol Chem 294: 11369–11381, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Klip A, Volchuk A, He L, Tsakiridis T. The glucose transporters of skeletal muscle. Semin Cell Dev Biol 7: 229–237, 1996. [Google Scholar]
- 148.Koga H, Terasawa H, Nunoi H, Takeshige K, Inagaki F, Sumimoto H. Tetratricopeptide repeat (TPR) motifs of p67(phox) participate in interaction with the small GTPase Rac and activation of the phagocyte NADPH oxidase. J Biol Chem 274: 25051–25060, 1999. [DOI] [PubMed] [Google Scholar]
- 149.Koh HJ, Arnolds DE, Fujii N, Tran TT, Rogers MJ, Jessen N, Li Y, Liew CW, Ho RC, Hirshman MF, Kulkarni RN, Kahn CR, Goodyear LJ. Skeletal muscle-selective knockout of LKB1 increases insulin sensitivity, improves glucose homeostasis, and decreases TRB3. Mol Cell Biol 26: 8217–8227, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kojima T, Fukuda M, Aruga J, Mikoshiba K. Calcium-dependent phospholipid binding to the C2A domain of a ubiquitous form of double C2 protein (Doc2 beta). J Biochem 120: 671–676, 1996. [DOI] [PubMed] [Google Scholar]
- 151.Kramer HF, Witczak CA, Fujii N, Jessen N, Taylor EB, Arnolds DE, Sakamoto K, Hirshman MF, Goodyear LJ. Distinct signals regulate AS160 phosphorylation in response to insulin, AICAR, and contraction in mouse skeletal muscle. Diabetes 55: 2067–2076, 2006. [DOI] [PubMed] [Google Scholar]
- 152.Krolopp JE, Thornton SM, Abbott MJ. IL-15 activates the Jak3/STAT3 Signaling pathway to mediate glucose uptake in skeletal muscle cells. Front Physiol 7: 626–626, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kunisada K, Hirota H, Fujio Y, Matsui H, Tani Y, Yamauchi-Takihara K, Kishimoto T. Activation of JAK-STAT and MAP kinases by leukemia inhibitory factor through gp130 in cardiac myocytes. Circulation 94: 2626–2632, 1996. [DOI] [PubMed] [Google Scholar]
- 154.Kurgan N, Noaman N, Pergande MR, Cologna SM, Coorssen JR, Klentrou P. Changes to the human serum proteome in response to high intensity interval exercise: A sequential top-down proteomic analysis. Front Physiol 10: 362, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lacraz G, Rakotoarivelo V, Labbé SM, Vernier M, Noll C, Mayhue M, Stankova J, Schwertani A, Grenier G, Carpentier A, Richard D, Ferbeyre G, Fradette J, Rola-Pleszczynski M, Menendez A, Langlois M-F, Ilangumaran S, Ramanathan S. Deficiency of Interleukin-15 confers resistance to obesity by diminishing inflammation and enhancing the thermogenic function of adipose tissues. PLoS One 11: e0162995, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lagouge M, Argmann C, Gerhart-Hines Z, Meziane H, Lerin C, Daussin F, Messadeq N, Milne J, Lambert P, Elliott P, Geny B, Laakso M, Puigserver P, Auwerx J. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell 127: 1109–1122, 2006. [DOI] [PubMed] [Google Scholar]
- 157.Laker RC, Garde C, Camera DM, Smiles WJ, Zierath JR, Hawley JA, Barrès R. Transcriptomic and epigenetic responses to short-term nutrient-exercise stress in humans. Sci Rep 7: 15134, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Larsson L, Grimby G, Karlsson J. Muscle strength and speed of movement in relation to age and muscle morphology. J Appl Physiol 46: 451–456, 1979. [DOI] [PubMed] [Google Scholar]
- 159.Laurentino GC, Ugrinowitsch C, Roschel H, Aoki MS, Soares AG, Neves M Jr, Aihara AY, Fernandes Ada R, Tricoli V. Strength training with blood flow restriction diminishes myostatin gene expression. Med Sci Sports Exerc 44: 406–412, 2012. [DOI] [PubMed] [Google Scholar]
- 160.Lavan BE, Kuhne MR, Garner CW, Anderson D, Reedijk M, Pawson T, Lienhard GE. The association of insulin-elicited phosphotyrosine proteins with src homology 2 domains. J Biol Chem 267: 11631–11636, 1992. [PubMed] [Google Scholar]
- 161.Leduc-Gaudet JP, Picard M, St-Jean Pelletier F, Sgarioto N, Auger MJ, Vallee J, Robitaille R, St-Pierre DH, Gouspillou G. Mitochondrial morphology is altered in atrophied skeletal muscle of aged mice. Oncotarget 6: 17923–17937, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lee HJ, Moon J, Chung I, Chung JH, Park C, Lee JO, Han JA, Kang MJ, Yoo EH, Kwak S-Y. ATP synthase inhibitory factor 1 (IF1), a novel myokine, regulates glucose metabolism by AMPK and Akt dual pathways. FASEB J 33: 14825–14840, 2019. DOI: 10.1096/fj.201901440RR. [DOI] [PubMed] [Google Scholar]
- 163.Lee J, Pilch PF, Shoelson SE, Scarlata SF. Conformational changes of the insulin receptor upon insulin binding and activation as monitored by fluorescence spectroscopy. Biochemistry 36: 2701–2708, 1997. [DOI] [PubMed] [Google Scholar]
- 164.Lee JH, Jun HS. Role of myokines in regulating skeletal muscle mass and function. Front Physiol 10: 42, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lee JS, Pinnamaneni SK, Eo SJ, Cho IH, Pyo JH, Kim CK, Sinclair AJ, Febbraio MA, Watt MJ. Saturated, but not n-6 polyunsaturated, fatty acids induce insulin resistance: Role of intramuscular accumulation of lipid metabolites. J Appl Physiol (1985) 100: 1467–1474, 2006. [DOI] [PubMed] [Google Scholar]
- 166.Lee JY, Hopkinson NS, Kemp PR. Myostatin induces autophagy in skeletal muscle in vitro. Biochem Biophys Res Commun 415: 632–636, 2011. [DOI] [PubMed] [Google Scholar]
- 167.Lee S-J, McPherron AC. Regulation of myostatin activity and muscle growth. Proc Natl Acad Sci 98: 9306–9311, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lee SK, Lee JO, Kim JH, Kim SJ, You GY, Moon JW, Jung JH, Park SH, Uhm KO, Park JM. Metformin sensitizes insulin signaling through AMPK-mediated pten down-regulation in preadipocyte 3T3-L1 cells. J Cell Biochem 112: 1259–1267, 2011. [DOI] [PubMed] [Google Scholar]
- 169.Lemieux K, Han XX, Dombrowski L, Bonen A, Marette A. The transferrin receptor defines two distinct contraction-responsive GLUT4 vesicle populations in skeletal muscle. Diabetes 49: 183–189, 2000. [DOI] [PubMed] [Google Scholar]
- 170.Li Q, Harraz MM, Zhou W, Zhang LN, Ding W, Zhang Y, Eggleston T, Yeaman C, Banfi B, Engelhardt JF. Nox2 and Rac1 regulate H2O2-dependent recruitment of TRAF6 to endosomal interleukin-1 receptor complexes. Mol Cell Biol 26: 140, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lim S, Choi SH, Koo BK, Kang SM, Yoon JW, Jang HC, Choi SM, Lee MG, Lee W, Shin H, Kim YB, Lee HK, Park KS. Effects of aerobic exercise training on C1q tumor necrosis factor alpha-related protein isoform 5 (myonectin): Association with insulin resistance and mitochondrial DNA density in women. J Clin Endocrinol Metab 97: E88–E93, 2012. [DOI] [PubMed] [Google Scholar]
- 172.Linnane AW, Marzuki S, Ozawa T, Tanaka M. Mitochondrial DNA mutations as an important contributor to ageing and degenerative diseases. Lancet 1: 642–645, 1989. [DOI] [PubMed] [Google Scholar]
- 173.Lira VA, Soltow QA, Long JH, Betters JL, Sellman JE, Criswell DS. Nitric oxide increases GLUT4 expression and regulates AMPK signaling in skeletal muscle. Am J Physiol Endocrinol Metab 293: E1062–E1068, 2007. [DOI] [PubMed] [Google Scholar]
- 174.Listrat A, Lebret B, Louveau I, Astruc T, Bonnet M, Lefaucheur L, Picard B, Bugeon J. How muscle structure and composition influence meat and flesh quality. Sci World J 2016: 3182746, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liu R, Jin P, Yu L, Wang Y, Han L, Shi T, Li X. Impaired mitochondrial dynamics and bioenergetics in diabetic skeletal muscle. PLoS One 9: e92810, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lizunov VA, Matsumoto H, Zimmerberg J, Cushman SW, Frolov VA. Insulin stimulates the halting, tethering, and fusion of mobile GLUT4 vesicles in rat adipose cells. J Cell Biol 169: 481–489, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lobo SM, Quinto BM, Oyama L, Nakamichi R, Ribeiro AB, Zanella MT, Dalboni MA, Batista MC. TNF-alpha modulates statin effects on secretion and expression of MCP-1, PAI-1 and adiponectin in 3T3-L1 differentiated adipocytes. Cytokine 60: 150–156, 2012. [DOI] [PubMed] [Google Scholar]
- 178.Loebig M, Klement J, Schmoller A, Betz S, Heuck N, Schweiger U, Peters A, Schultes B, Oltmanns KM. Evidence for a relationship between VEGF and BMI independent of insulin sensitivity by glucose clamp procedure in a homogenous group healthy young men. PLoS One 5: e12610, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lokireddy S, Mouly V, Butler-Browne G, Gluckman PD, Sharma M, Kambadur R, McFarlane C. Myostatin promotes the wasting of human myoblast cultures through promoting ubiquitin-proteasome pathwaymediated loss of sarcomeric proteins. Am J Physiol Cell Physiol 301: C1316–C1324, 2011. [DOI] [PubMed] [Google Scholar]
- 180.Lou X, Shin Y-K. SNARE zippering. Biosci Rep 36: e00327, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Louis E, Raue U, Yang Y, Jemiolo B, Trappe S. Time course of proteolytic, cytokine, and myostatin gene expression after acute exercise in human skeletal muscle. J Appl Physiol (1985) 103: 1744–1751, 2007. [DOI] [PubMed] [Google Scholar]
- 182.Lucas S, Taront S, Magnan C, Fauconnier L, Delacre M, Macia L, Delanoye A, Verwaerde C, Spriet C, Saule P, Goormachtigh G, Heliot L, Ktorza A, Movassat J, Polakowska R, Auriault C, Poulain-Godefroy O, Di Santo J, Froguel P, Wolowczuk I. Interleukin-7 regulates adipose tissue mass and insulin sensitivity in high-fat diet-fed mice through lymphocyte-dependent and independent mechanisms. PLoS One 7: e40351, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lund S, Holman GD, Schmitz O, Pedersen O. Contraction stimulates translocation of glucose transporter GLUT4 in skeletal muscle through a mechanism distinct from that of insulin. Proc Natl Acad Sci U S A 92: 5817–5821, 1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Luo B, Soesanto Y, McClain DA. Protein modification by O-linked GlcNAc reduces angiogenesis by inhibiting Akt activity in endothelial cells. Arterioscler Thromb Vasc Biol 28: 651–657, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Luzzo KM, Wang Q, Purcell SH, Chi M, Jimenez PT, Grindler N, Schedl T,Moley KH. High fat diet induced developmental defects in the mouse: Oocyte meiotic aneuploidy and fetal growth retardation/brain defects. PLoS One 7: e49217, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Maffei á, Halaas J, Ravussin E, Pratley R, Lee G, Zhang Y, Fei H, Kim S, Lallone R, Ranganathan S. Leptin levels in human and rodent: Measurement of plasma leptin and Ob RNA in obese and weight-reduced subjects. Nat Med 1: 1155, 1995. [DOI] [PubMed] [Google Scholar]
- 187.Mammucari C, Milan G, Romanello V, Masiero E, Rudolf R, Del Piccolo P, Burden SJ, Di Lisi R, Sandri C, Zhao J. FoxO3 controls autophagy in skeletal muscle in vivo. Cell Metab 6: 458–471, 2007. [DOI] [PubMed] [Google Scholar]
- 188.Mammucari C, Schiaffino S, Sandri M . Downstream of Akt: FoxO3 and mTOR in the regulation of autophagy in skeletal muscle. Autophagy 4: 524–526, 2008. [DOI] [PubMed] [Google Scholar]
- 189.Marcinko K, Bujak AL, Lally JSV, Ford RJ, Wong TH, Smith BK, Kemp BE,Jenkins Y, Li W,Kinsella TM, Hitoshi Y, Steinberg GR. The AMPK activator R419 improves exercise capacity and skeletal muscle insulin sensitivity in obese mice. Mol Metab 4: 643–651, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Mascher H, Tannerstedt J, Brink-Elfegoun T, Ekblom B, Gustafsson T, Blomstrand E. Repeated resistance exercise training induces different changes in mRNA expression of MAFbx and MuRF-1 in human skeletal muscle. Am J Physiol Endocrinol Metab 294: E43–E51, 2008. [DOI] [PubMed] [Google Scholar]
- 191.Matthews VB, Astrom MB, Chan MH, Bruce CR, Krabbe KS, Prelovsek O, Akerstrom T, Yfanti C, Broholm C, Mortensen OH, Penkowa M, Hojman P, Zankari A, Watt MJ, Bruunsgaard H, Pedersen BK, Febbraio MA. Brain-derived neurotrophic factor is produced by skeletal muscle cells in response to contraction and enhances fat oxidation via activation of AMP-activated protein kinase. Diabetologia 52: 1409–1418, 2009. [DOI] [PubMed] [Google Scholar]
- 192.Maury E, Ehala-Aleksejev K, Guiot Y, Detry R, Vandenhooft A, Brichard SM. Adipokines oversecreted by omental adipose tissue in human obesity. Am J Physiol Endocrinol Metab 293: E656–E665, 2007. [DOI] [PubMed] [Google Scholar]
- 193.McGee SL, Howlett KF, Starkie RL, Cameron-Smith D, Kemp BE, Hargreaves M. Exercise increases nuclear AMPK α2 in human skeletal muscle. Diabetes 52: 926–928, 2003. [DOI] [PubMed] [Google Scholar]
- 194.Mclntyre HD, Paterson CA, Ma A, Ravenscroft PJ, Bird DM, Cameron DP. Metformin increases insulin sensitivity and basal glucose clearance in type 2 (non-insulin dependent) diabetes mellitus. AustNZJMed 21: 714–719, 1991. [DOI] [PubMed] [Google Scholar]
- 195.McPherron AC, Lee SJ. Double muscling in cattle due to mutations in the myostatin gene. Proc Natl Acad Sci U S A 94: 12457–12461, 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Mejia GL, Asiedu MN, Hitoshi Y, Dussor G, Price TJ. The potent, indirect adenosine monophosphate-activated protein kinase activator R419 attenuates mitogen-activated protein kinase signaling, inhibits nociceptor excitability, and reduces pain hypersensitivity in mice. Pain Rep 1. pii: e562, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Mellbin LG, Anselmino M, Ryden L. Diabetes, prediabetes and cardiovascular risk. Eur J Cardiovasc Prev Rehabil 17 (Suppl 1): S9–S14, 2010. [DOI] [PubMed] [Google Scholar]
- 198.Merrill GF, Kurth EJ, Hardie DG, Winder WW. AICA riboside increases AMP-activated protein kinase, fatty acid oxidation, and glucose uptake in rat muscle. Am J Phys 273: E1107–E1112, 1997. [DOI] [PubMed] [Google Scholar]
- 199.Min J, Okada S, Kanzaki M, Elmendorf JS, Coker KJ, Ceresa BP, Syu LJ, Noda Y, Saltiel AR, Pessin JE. Synip: A novel insulin-regulated syntaxin 4-binding protein mediating GLUT4 translocation in adipocytes. Mol Cell 3: 751–760, 1999. [DOI] [PubMed] [Google Scholar]
- 200.Miotto PM, LeBlanc PJ, Holloway GP. High-fat diet causes mitochondrial dysfunction as a result of impaired ADP sensitivity. Diabetes 67: 2199–2205, 2018. [DOI] [PubMed] [Google Scholar]
- 201.Mishra P, Varuzhanyan G, Pham AH, Chan DC. Mitochondrial dynamics is a distinguishing feature of skeletal muscle fiber types and regulates organellar compartmentalization. Cell Metab 22: 1033–1044, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Modan M, Halkin H, Almog S, Lusky A, Eshkol A, Shefi M, Shitrit A, Fuchs Z. Hyperinsulinemia. A link between hypertension obesity and glucose intolerance. J Clin Invest 75: 809–817, 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Morey C, Kienle CN, Klopper TH, Burkhardt P, Fasshauer D. Evidence for a conserved inhibitory binding mode between the membrane fusion assembly factors Munc18 and syntaxin in animals. J Biol Chem 292: 20449–20460, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Morvan F, Rondeau JM, Zou C, Minetti G, Scheufler C, Scharenberg M, Jacobi C, Brebbia P, Ritter V, Toussaint G, Koelbing C, Leber X, Schilb A, Witte F, Lehmann S, Koch E, Geisse S, Glass DJ, Lach-Trifilieff E. Blockade of activin type II receptors with a dual anti-ActRIIA/IIB antibody is critical to promote maximal skeletal muscle hypertrophy. Proc Natl Acad Sci U S A 114: 12448–12453, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Mosher DS, Quignon P, Bustamante CD, Sutter NB, Mellersh CS, Parker HG, Ostrander EA. A mutation in the myostatin gene increases muscle mass and enhances racing performance in heterozygote dogs. PLoS Genet 3: e79, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Mueckler M, Thorens B. The SLC2 (GLUT) family of membrane transporters. Mol Asp Med 34: 121–138, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Muller-Newen G, Kuster A, Hemmann U, Keul R, Horsten U, Martens A, Graeve L, Wijdenes J, Heinrich PC. Soluble IL-6 receptor potentiates the antagonistic activity of soluble gp130 on IL-6 responses. J Immunol 161: 6347–6355, 1998. [PubMed] [Google Scholar]
- 208.Myers MG, Backer JM, Sun XJ, Shoelson S, Hu P, Schlessinger J, Yoakim M, Schaffhausen B, White MF. IRS-1 activates phosphatidylinositol 3′-kinase by associating with src homology 2 domains of p85. Proc Natl Acad Sci U S A 89: 10350–10354, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Nadeau L, Patten DA, Caron A, Garneau L, Pinault-Masson E, Foretz M, Haddad P, Anderson BG, Quinn LS, Jardine K, McBurney MW, Pistilli EE, Harper ME, Aguer C. IL-15 improves skeletal muscle oxidative metabolism and glucose uptake in association with increased respiratory chain supercomplex formation and AMPK pathway activation. Biochim Biophys Acta Gen Subj 1863: 395–407, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Nakane M, Schmidt HH, Pollock JS, Forstermann U, Murad F. Cloned human brain nitric oxide synthase is highly expressed in skeletal muscle. FEBS Lett 316: 175–180, 1993. [DOI] [PubMed] [Google Scholar]
- 211.Narkar VA, Downes M, Yu RT, Embler E, Wang YX, Banayo E, Mihaylova MM, Nelson MC, Zou Y, Juguilon H, Kang H, Shaw RJ, Evans RM. AMPK and PPARdelta agonists are exercise mimetics. Cell 134: 405–415, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Narkar VA, Fan W, Downes M, Yu RT, Jonker JW, Alaynick WA, Banayo E, Karunasiri MS, Lorca S, Evans RM. Exercise and PGC-1alpha-independent synchronization of type I muscle metabolism and vasculature by ERRgamma. Cell Metab 13: 283–293, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Nielsen AR, Mounier R, Plomgaard P, Mortensen OH, Penkowa M, Speerschneider T, Pilegaard H, Pedersen BK. Expression of interleukin-15 in human skeletal muscle effect of exercise and muscle fibre type composition. J Physiol 584: 305–312, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Norheim F, Raastad T, Thiede B, Rustan AC, Drevon CA, Haugen F. Proteomic identification of secreted proteins from human skeletal muscle cells and expression in response to strength training. AmJPhysiol Endocrinol Metab 301: E1013–E1021, 2011. [DOI] [PubMed] [Google Scholar]
- 215.Oakhill JS, Steel R, Chen ZP, Scott JW, Ling N, Tam S, Kemp BE. AMPK is a direct adenylate charge-regulated protein kinase. Science 332: 1433–1435, 2011. [DOI] [PubMed] [Google Scholar]
- 216.Oh E, Spurlin BA, Pessin JE, Thurmond DC. Munc18c heterozygous knockout mice display increased susceptibility for severe glucose intolerance. Diabetes 54: 638–647, 2005. [DOI] [PubMed] [Google Scholar]
- 217.O’Hagan C, De Vito G, Boreham CA. Exercise prescription in the treatment of type 2 diabetes mellitus: Current practices, existing guidelines and future directions. Sports Med 43: 39–49, 2013. [DOI] [PubMed] [Google Scholar]
- 218.Ojuka EO, Jones TE, Nolte LA, Chen M, Wamhoff BR, Sturek M, Holloszy JO. Regulation of GLUT4 biogenesis in muscle: Evidence for involvement of AMPK and Ca2+. Am J Physiol Endocrinol Metab 282: E1008–E1013, 2002. [DOI] [PubMed] [Google Scholar]
- 219.Okada S, Ohshima K, Uehara Y, Shimizu H, Hashimoto K, Yamada M, Mori M. Synip phosphorylation is required for insulin-stimulated Glut4 translocation. Biochem Biophys Res Commun 356: 102–106, 2007. [DOI] [PubMed] [Google Scholar]
- 220.Olson AL, Knight JB, Pessin JE. Syntaxin 4, VAMP2, and/or VAMP3/cellubrevin are functional target membrane and vesicle SNAP receptors for insulin-stimulated GLUT4 translocation in adipocytes. Mol Cell Biol 17: 2425–2435, 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.O’Neill HM, Maarbjerg SJ, Crane JD, Jeppesen J, Jorgensen SB, Schertzer JD, Shyroka O, Kiens B, van Denderen BJ, Tarnopolsky MA, Kemp BE, Richter EA, Steinberg GR. AMP-activated protein kinase (AMPK) beta1beta2 muscle null mice reveal an essential role for AMPK in maintaining mitochondrial content and glucose uptake during exercise. Proc Natl Acad Sci U S A 108: 16092–16097, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Orita S, Naito A, Sakaguchi G, Maeda M, Igarashi H, Sasaki T, Takai Y. Physical and functional interactions of Doc2 and Munc13 in Ca2+-dependent exocytotic machinery. J Biol Chem 272: 16081–16084, 1997. [DOI] [PubMed] [Google Scholar]
- 223.Orita S, Sasaki T, Komuro R, Sakaguchi G, Maeda M, Igarashi H, Takai Y. Doc2 enhances Ca2+-dependent exocytosis from PC12 cells. J Biol Chem 271: 7257–7260, 1996. [DOI] [PubMed] [Google Scholar]
- 224.Orita S, Sasaki T, Naito A, Komuro R, Ohtsuka T, Maeda M, Suzuki H, Igarashi H, Takai Y. Doc2: A novel brain protein having two repeated C2-like domains. Biochem Biophys Res Commun 206: 439–448, 1995. [DOI] [PubMed] [Google Scholar]
- 225.Ostrowski K, Rohde T, Asp S, Schjerling P, Pedersen BK. Pro- and anti-inflammatory cytokine balance in strenuous exercise in humans. J Physiol 515 (Pt 1): 287–291, 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Ostrowski K, Rohde T, Zacho M, Asp S, Pedersen B. Evidence that interleukin-6 is produced in human skeletal muscle during prolonged running. J Physiol 508: 949–953, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Pallavi B, Nagaraj R. Palmitoylated peptides from the cysteine-rich domain of SNAP-23 cause membrane fusion depending on peptide length, position of cysteines, and extent of palmitoylation. J Biol Chem 278: 12737–12744, 2003. [DOI] [PubMed] [Google Scholar]
- 228.Papanicolaou DA, Petrides JS, Tsigos C, Bina S, Kalogeras KT, Wilder R, Gold PW, Deuster PA, Chrousos GP. Exercise stimulates interleukin-6 secretion: Inhibition by glucocorticoids and correlation with catecholamines. Am J Phys 271: E601–E605, 1996. [DOI] [PubMed] [Google Scholar]
- 229.Park SY, Choi JH, Ryu HS, Pak YK, Park KS, Lee HK, Lee W. C1q tumor necrosis factor alpha-related protein isoform 5 is increased in mitochondrial DNA-depleted myocytes and activates AMP-activated protein kinase. J Biol Chem 284: 27780–27789, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Park SY, Ryu J, Lee W. O-GlcNAc modification on IRS-1 and Akt2 by PUGNAc inhibits their phosphorylation and induces insulin resistance in rat primary adipocytes. Exp Mol Med 37: 220–229, 2005. [DOI] [PubMed] [Google Scholar]
- 231.Parker G, Taylor R, Jones D, McClain D. Hyperglycemia and inhibition of glycogen synthase in streptozotocin-treated mice: Role of O-linked N-acetylglucosamine. J Biol Chem 279: 20636–20642, 2004. [DOI] [PubMed] [Google Scholar]
- 232.Pehmoller C, Treebak JT, Birk JB, Chen S, Mackintosh C, Hardie DG, Richter EA, Wojtaszewski JF. Genetic disruption of AMPK signaling abolishes both contraction- and insulin-stimulated TBC1D1 phosphorylation and 14–3-3 binding in mouse skeletal muscle. Am J Physiol Endocrinol Metab 297: E665–E675, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Percival JM, Anderson KN, Huang P, Adams ME, Froehner SC. Golgi and sarcolemmal neuronal NOS differentially regulate contractioninduced fatigue and vasoconstriction in exercising mouse skeletal muscle. J Clin Invest 120: 816–826, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Perrotta C, Bizzozero L, Cazzato D, Morlacchi S, Assi E, Simbari F, Zhang Y, Gulbins E, Bassi MT, Rosa P, Clementi E. Syntaxin 4 is required for acid sphingomyelinase activity and apoptotic function. J Biol Chem 285: 40240–40251, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Pirinen E, Canto C, Jo YS, Morato L, Zhang H, Menzies KJ, Williams EG, Mouchiroud L, Moullan N, Hagberg C, Li W, Timmers S, Imhof R, Verbeek J, Pujol A, van Loon B, Viscomi C, Zeviani M, Schrauwen P, Sauve AA, Schoonjans K, Auwerx J. Pharmacological inhibition of poly(ADP-ribose) polymerases improves fitness and mitochondrial function in skeletal muscle. Cell Metab 19: 1034–1041, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Pistilli EE, Alway SE. Systemic elevation of interleukin-15 in vivo promotes apoptosis in skeletal muscles of young adult and aged rats. Biochem Biophys Res Commun 373: 20–24, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Poirier MA, Xiao W, Macosko JC, Chan C, Shin YK, Bennett MK. The synaptic SNARE complex is a parallel four-stranded helical bundle. Nat Struct Biol 5: 765–769, 1998. [DOI] [PubMed] [Google Scholar]
- 238.Polekhina G, Gupta A, Michell BJ, van Denderen B, Murthy S, Feil SC, Jennings IG, Campbell DJ, Witters LA, Parker MW, Kemp BE, Stapleton D. AMPK beta subunit targets metabolic stress sensing to glycogen. Curr Biol 13: 867–871, 2003. [DOI] [PubMed] [Google Scholar]
- 239.Pollock CB, Rodriguez O, Martin PL, Albanese C, Li X, Kopelovich L, Glazer RI. Induction of metastatic gastric cancer by peroxisome proliferator-activated receptordelta activation. PPAR Res 2010: 571783, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Pollock CB, Yin Y, Yuan H, Zeng X, King S, Li X, Kopelovich L, Albanese C, Glazer RI. PPARdelta activation acts cooperatively with 3-phosphoinositide-dependent protein kinase-1 to enhance mammary tumorigenesis. PLoS One 6: e16215, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Proenza C, O’Brien J, Nakai J, Mukherjee S, Allen PD, Beam KG. Identification of a region of RyR1 that participates inallosteric coupling with the alpha(1S) (Ca(V)1.1) II-III loop. J Biol Chem 277: 6530–6535, 2002. [DOI] [PubMed] [Google Scholar]
- 242.Quinn LS, Anderson BG, Drivdahl RH, Alvarez B, Argiles JM. Overexpression of interleukin-15 induces skeletal muscle hypertrophy in vitro: Implications for treatment of muscle wasting disorders. Exp Cell Res 280: 55–63, 2002. [DOI] [PubMed] [Google Scholar]
- 243.Quinn LS, Anderson BG, Strait-Bodey L, Stroud AM, Argiles JM. Oversecretion of interleukin-15 from skeletal muscle reduces adiposity. Am J Physiol Endocrinol Metab 296: E191–E202, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Quinn LS, Strait-Bodey L, Anderson BG, Argiles JM, Havel PJ. Interleukin-15 stimulates adiponectin secretion by 3T3-L1 adipocytes: Evidence for a skeletal muscle-to-fat signaling pathway. Cell Biol Int 29: 449–457, 2005. [DOI] [PubMed] [Google Scholar]
- 245.Ramalingam L, Lu J, Hudmon A, Thurmond DC. Doc2b serves as a scaffolding platform for concurrent binding of multiple Munc18 isoforms in pancreatic islet beta-cells. Biochem J 464: 251–258, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Ramalingam L, Oh E, Thurmond DC. Doc2b enrichment enhances glucose homeostasis in mice via potentiation of insulin secretion and peripheral insulin sensitivity. Diabetologia 57: 1476–1484, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Ramalingam L, Oh E, Yoder SM, Brozinick JT, Kalwat MA, Groffen AJ, Verhage M, Thurmond DC. Doc2b is a key effector of insulin secretion and skeletal muscle insulin sensitivity. Diabetes 61: 2424–2432, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Rana KS, Pararasa C, Afzal I, Nagel DA, Hill EJ, Bailey CJ, Griffiths HR, Kyrou I, Randeva HS, Bellary S, Brown JE. Plasma irisin is elevated in type 2 diabetes and is associated with increased E-selectin levels. Cardiovasc Diabetol 16: 147, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Rangwala SM, Wang X, Calvo JA, Lindsley L, Zhang Y, Deyneko G, Beaulieu V, Gao J, Turner G, Markovits J. Estrogen-related receptor gammaisakeyregulatorofmusclemitochondrialactivityandoxidative capacity. J Biol Chem 285: 22619–22629, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Raschke S, Eckardt K, Bjorklund Holven K, Jensen J, Eckel J. Identification and validation of novel contraction-regulated myokines released from primary human skeletal muscle cells. PLoS One 8: e62008, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Raschke S, Eckel J. Adipo-myokines: Two sides of the same coin–mediators of inflammation and mediators of exercise. Mediat Inflamm 2013: 320724, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Rehman A, Hu SH, Tnimov Z, Whitten AE, King GJ, Jarrott RJ, Norwood SJ, Alexandrov K, Collins BM, Christie MP, Martin JL. The nature of the Syntaxin4 C-terminus affects Munc18c-supported SNARE assembly. PLoS One 12: e0183366, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Riechman SE, Balasekaran G, Roth SM, Ferrell RE. Association of interleukin-15 protein and interleukin-15 receptor genetic variation with resistance exercise training responses. J Appl Physiol (1985) 97: 2214–2219, 2004. [DOI] [PubMed] [Google Scholar]
- 254.Ritov VB, Menshikova EV, He J, Ferrell RE, Goodpaster BH, Kelley DE. Deficiency of subsarcolemmal mitochondria in obesity and type 2 diabetes. Diabetes 54: 8–14, 2005. [DOI] [PubMed] [Google Scholar]
- 255.Rojas Vega S, Struder HK, Vera Wahrmann B, Schmidt A, Bloch W, Hollmann W. Acute BDNF and cortisol response to low intensity exercise and following ramp incremental exercise to exhaustion in humans. Brain Res 1121: 59–65, 2006. [DOI] [PubMed] [Google Scholar]
- 256.Rose AJ, Jeppesen J, Kiens B, Richter EA. Effects of contraction on localization of GLUT4 and v-SNARE isoforms in rat skeletal muscle. Am J Physiol Regul Integr Comp Physiol 297: R1228–R1237, 2009. [DOI] [PubMed] [Google Scholar]
- 257.Ross RM, Wadley GD, Clark MG, Rattigan S, McConell GK. Local nitric oxide synthase inhibition reduces skeletal muscle glucose uptake but not capillary blood flow during in situ muscle contraction in rats. Diabetes 56: 2885–2892, 2007. [DOI] [PubMed] [Google Scholar]
- 258.Roth SM, Martel GF, Ferrell RE, Metter EJ, Hurley BF, Rogers MA. Myostatin gene expression is reduced in humans with heavy-resistance strength training: A brief communication. Exp Biol Med (Maywood) 228: 706–709, 2003. [DOI] [PubMed] [Google Scholar]
- 259.Rotter V, Nagaev I, Smith U. Interleukin-6 (IL-6) induces insulin resistance in 3T3-L1 adipocytes and is, like IL-8 and tumor necrosis factor-alpha, overexpressed in human fat cells from insulin-resistant subjects. J Biol Chem 278: 45777–45784, 2003. [DOI] [PubMed] [Google Scholar]
- 260.Ruas JL, White JP, Rao RR, Kleiner S, Brannan KT, Harrison BC, Greene NP, Wu J, Estall JL, Irving BA, Lanza IR, Rasbach KA, Okutsu M, Nair KS, Yan Z, Leinwand LA, Spiegelman BM. A PGC-1alpha isoform induced by resistance training regulates skeletal muscle hypertrophy. Cell 151: 1319–1331, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Sabater M, Moreno-Navarrete JM, Ortega FJ, Pardo G, Salvador J, Ricart W, Fruhbeck G, Fernandez-Real JM. Circulating pigment epithelium-derived factor levels are associated with insulin resistance and decrease after weight loss. J Clin Endocrinol Metab 95: 4720–4728, 2010. [DOI] [PubMed] [Google Scholar]
- 262.Sabina RL, Patterson D, Holmes E. 5-Amino-4-imidazolecarboxamide riboside (Z-riboside) metabolism in eukaryotic cells. J Biol Chem 260: 6107–6114, 1985. [PubMed] [Google Scholar]
- 263.Safdar A, Saleem A, Tarnopolsky MA. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat Rev Endocrinol 12: 504–517, 2016. [DOI] [PubMed] [Google Scholar]
- 264.Saito T, Okada S, Yamada E, Ohshima K, Shimizu H, Shimomura K, Sato M, Pessin JE, Mori M. Syntaxin 4 and Synip (syntaxin 4 interacting protein) regulate insulin secretion in the pancreatic beta HC-9 cell. J Biol Chem 278: 36718–36725. [DOI] [PubMed] [Google Scholar]
- 265.Saitoh T, Okada S, Pessin JE, Ohshima K, Sato M, Mori M. The role of Syntaxin4 binding protein; synip and Munc18c on insulin secretion. Diabetes 49: A63, 2000. [Google Scholar]
- 266.Sakamoto K, McCarthy A, Smith D, Green KA, Grahame Hardie D, Ashworth A, Alessi DR. Deficiency of LKB1 in skeletal muscle prevents AMPK activation and glucose uptake during contraction. EMBO J 24: 1810–1820, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Samaras K, Botelho NK, Chisholm DJ, Lord RV. Subcutaneous and visceral adipose tissue gene expression of serum adipokines that predict type 2 diabetes. Obesity (Silver Spring) 18: 884–889, 2010. [DOI] [PubMed] [Google Scholar]
- 268.Sanders MJ, Grondin PO, Hegarty BD, Snowden MA, Carling D. Investigating the mechanism for AMP activation of the AMP-activated protein kinase cascade. Biochem J 403: 139–148, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Sandow A. Excitation-contraction coupling in muscular response. Yale J Biol Med 25: 176–201, 1952. [PMC free article] [PubMed] [Google Scholar]
- 270.Sandrini L, Di Minno A, Amadio P, Ieraci A, Tremoli E, Barbieri SS. Association between obesity and circulating brain-derived neurotrophic factor (BDNF) levels: Systematic review of literature and meta-analysis. Int J Mol Sci 19. pii: E2281, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Sano H, Eguez L, Teruel MN, Fukuda M, Chuang TD, Chavez JA, Lienhard GE, McGraw TE. Rab10, a target of the AS160 Rab GAP, is required for insulin-stimulated translocation of GLUT4 to the adipocyte plasma membrane. Cell Metab 5: 293–303, 2007. [DOI] [PubMed] [Google Scholar]
- 272.Sano H, Kane S, Sano E, Lienhard GE. Synip phosphorylation does not regulate insulin-stimulated GLUT4 translocation. Biochem Biophys Res Commun 332: 880–884, 2005. [DOI] [PubMed] [Google Scholar]
- 273.Sano H, Kane S, Sano E, Miinea CP, Asara JM, Lane WS, Garner CW, Lienhard GE. Insulin-stimulated phosphorylation of a Rab GTPase-activating protein regulates GLUT4 translocation. J Biol Chem 278: 14599–14602, 2003. [DOI] [PubMed] [Google Scholar]
- 274.Saremi A, Gharakhanloo R, Sharghi S, Gharaati MR, Larijani B, Omidfar K. Effects of oral creatine and resistance training on serum myostatin and GASP-1. Mol Cell Endocrinol 317: 25–30, 2010. [DOI] [PubMed] [Google Scholar]
- 275.Sartipy P, Loskutoff DJ. Monocyte chemoattractant protein 1 in obesity and insulin resistance. Proc Natl Acad Sci U S A 100: 7265–7270, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Sartori R, Milan G, Patron M, Mammucari C, Blaauw B, Abraham R, Sandri M. Smad2 and 3 transcription factors control muscle mass in adulthood. Am J Physiol Cell Physiol 296: C1248–C1257, 2009. [DOI] [PubMed] [Google Scholar]
- 277.Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF. A novel serum proteinsimilar to C1q,producedexclusively in adipocytes. J Biol Chem 270: 26746–26749, 1995. [DOI] [PubMed] [Google Scholar]
- 278.Seldin MM, Lei X, Tan SY, Stanson KP, Wei Z, Wong GW. Skeletal muscle-derived myonectin activates the mammalian target of rapamycin (mTOR) pathway to suppress autophagy in liver. J Biol Chem 288: 36073–36082, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Seldin MM, Peterson JM, Byerly MS, Wei Z, Wong GW. Myonectin (CTRP15), a novel myokine that links skeletal muscle to systemic lipid homeostasis. J Biol Chem 287: 11968–11980, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Seldin MM, Wong GW. Regulation of tissue crosstalk by skeletal muscle-derived myonectin and other myokines. Adipocyte 1: 200–202, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Shelton GD, Engvall E. Gross muscle hypertrophy in whippet dogs is caused by a mutation in the myostatin gene. Neuromuscul Disord 17: 721–722, 2007. [DOI] [PubMed] [Google Scholar]
- 282.Shi H, Munk A, Nielsen TS, Daughtry MR, Larsson L, Li S, Hoyer KF, Geisler HW, Sulek K, Kjobsted R, Fisher T, Andersen MM, Shen Z, Hansen UK, England EM, Cheng Z, Hojlund K, Wojtaszewski JFP, Yang X, Hulver MW, Helm RF, Treebak JT, Gerrard DE. Skeletal muscle O-GlcNAc transferase is important for muscle energy homeostasis and whole-body insulin sensitivity. Mol Metab 11: 160–177, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Soesanto Y, Luo B, Parker G, Jones D, Cooksey RC, McClain DA. Pleiotropic and age-dependent effects of decreased protein modification by O-linked N-acetylglucosamine on pancreatic beta-cell function and vascularization. J Biol Chem 286: 26118–26126, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Soesanto YA, Luo B, Jones D, Taylor R, Gabrielsen JS, Parker G, McClain DA. Regulation of Akt signaling by O-GlcNAc in euglycemia. Am J Physiol Endocrinol Metab 295: E974–E980, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Sollner T, Bennett MK, Whiteheart SW, Scheller RH, Rothman JE. A protein assembly-disassembly pathway in vitro that may correspond to sequential steps of synaptic vesicle docking, activation, and fusion. Cell 75: 409–418, 1993. [DOI] [PubMed] [Google Scholar]
- 286.Solt LA, Wang Y, Banerjee S, Hughes T, Kojetin DJ, Lundasen T, Shin Y, Liu J, Cameron MD, Noel R, Yoo SH, Takahashi JS, Butler AA, Kamenecka TM, Burris TP. Regulation of circadian behaviour and metabolism by synthetic REV-ERB agonists. Nature 485: 62–68, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Song W, Chen J, Petrilli A, Liot G, Klinglmayr E, Zhou Y, Poquiz P, Tjong J, Pouladi MA, Hayden MR. Mutant huntingtin binds the mitochondrial fission GTPase dynamin-related protein-1 and increases its enzymatic activity. Nat Med 17: 377, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Sorensen JB, Wiederhold K, Muller EM, Milosevic I, Nagy G, de Groot BL, Grubmuller H, Fasshauer D. Sequential N- to C-terminal SNARE complex assembly drives priming and fusion of secretory vesicles. EMBO J 25: 955–966, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Souto Padron de Figueiredo A, Salmon AB, Bruno F, Jimenez F, Martinez HG, Halade GV, Ahuja SS, Clark RA, DeFronzo RA, Abboud HE, El Jamali A. Nox2 mediates skeletal muscle insulin resistance induced by a high fat diet. J Biol Chem 290: 13427–13439, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Spurlin BA, Thomas RM, Nevins AK, Kim HJ, Kim YJ, Noh HL, Shulman GI, Kim JK, Thurmond DC. Insulin resistance in tetracyclinerepressible Munc18c transgenic mice. Diabetes 52: 1910–1917, 2003. [DOI] [PubMed] [Google Scholar]
- 291.Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: Findings from the National Health and Nutrition Examination Survey III. PLoS One 5: e10805, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Steensberg A, Van Hall G, Osada T, Sacchetti M, Saltin B, Pedersen BK. Production of interleukin-6 in contracting human skeletal muscles can account for the exercise-induced increase in plasma interleukin-6. J Physiol 529: 237–242, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Steneberg P, Lindahl E, Dahl U, Lidh E, Straseviciene J, Backlund F, Kjellkvist E, Berggren E, Lundberg I, Bergqvist I, Ericsson M, Eriksson B, Linde K, Westman J, Edlund T, Edlund H. PAN-AMPK activator O304 improves glucose homeostasis and microvascular perfusion in mice and type 2 diabetes patients. JCI Insight 3. pii: 99114, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, Patel HR, Ahima RS, Lazar MA. The hormone resistin links obesity to diabetes. Nature 409: 307–312, 2001. [DOI] [PubMed] [Google Scholar]
- 295.Sun H, Ma Y, Gao M, Liu D. IL-15/sIL-15Rα gene transfer induces weight loss and improves glucose homeostasis in obese mice. Gene Ther 23: 349–356, 2016. [DOI] [PubMed] [Google Scholar]
- 296.Sun XJ, Rothenberg P, Kahn CR, Backer JM, Araki E, Wilden PA, Cahill DA, Goldstein BJ, White MF. Structure of the insulin receptor substrate IRS-1 defines a unique signal transduction protein. Nature 352: 73–77, 1991. [DOI] [PubMed] [Google Scholar]
- 297.Sun Y, Bilan PJ, Liu Z, Klip A. Rab8A and Rab13 are activated by insulin and regulate GLUT4 translocation in muscle cells. Proc Natl Acad Sci U S A 107: 19909–19914, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Sun Y, Jaldin-Fincati J, Liu Z, Bilan PJ, Klip A. A complex of Rab13 with MICAL-L2 and α-actinin-4 is essential for insulin-dependent GLUT4 exocytosis. Mol Biol Cell 27: 75–89, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Suwa M, Egashira T, Nakano H, Sasaki H, Kumagai S. Metformin increases the PGC-1α protein and oxidative enzyme activities possibly via AMPK phosphorylation in skeletal muscle in vivo. J Appl Physiol 101: 1685–1692, 2006. [DOI] [PubMed] [Google Scholar]
- 300.Sylow L, Jensen TE, Kleinert M, Mouatt JR, Maarbjerg SJ, Jeppesen J, Prats C, Chiu TT, Boguslavsky S, Klip A, Schjerling P, Richter EA. Rac1 is a novel regulator of contraction-stimulated glucose uptake in skeletal muscle. Diabetes 62: 1139–1151, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Sylow L, Moller LL, Kleinert M, Richter EA, Jensen TE. Rac1 – A novel regulator of contraction-stimulated glucose uptake in skeletal muscle. Exp Physiol 99: 1574–1580, 2014. [DOI] [PubMed] [Google Scholar]
- 302.Sylow L, Moller LLV, Kleinert M, D’Hulst G, De Groote E, Schjerling P, Steinberg GR, Jensen TE, Richter EA. Rac1 and AMPK account for the majority of muscle glucose uptake stimulated by ex vivo contraction but not in vivo exercise. Diabetes 66: 1548–1559, 2017. [DOI] [PubMed] [Google Scholar]
- 303.Takenaka N, Nakao M, Matsui S, Satoh T. A crucial role for the small GTPase Rac1 downstream of the protein kinase Akt2 in insulin signaling that regulates glucose uptake in mouse adipocytes. Int J Mol Sci 20. pii: 5443, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Tamori Y, Kawanishi M, Niki T, Shinoda H, Araki S, Okazawa H, Kasuga M. Inhibition of insulin-induced GLUT4 translocation by Munc18c through interaction with syntaxin4 in 3T3-L1 adipocytes. J Biol Chem 273: 19740–19746, 1998. [DOI] [PubMed] [Google Scholar]
- 305.Taylor AH, Doust J, Webborn N. Randomised controlled trial to examine the effects of a GP exercise referral programme in Hailsham, East Sussex, on modifiable coronary heart disease risk factors. J Epidemiol Community Health 52: 595–601, 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Tellam JT, McIntosh S, James DE. Molecular identification of two novel Munc-18 isoforms expressed in non-neuronal tissues. J Biol Chem 270: 5857–5863, 1995. [DOI] [PubMed] [Google Scholar]
- 307.Thiebaud D, Jacot E, Defronzo RA, Maeder E, Jequier E, Felber J-P. The effect of graded doses of insulin on total glucose uptake, glucose oxidation, and glucose storage in man. Diabetes 31: 957–963, 1982. [DOI] [PubMed] [Google Scholar]
- 308.Thomson DM, Porter BB, Tall JH, Kim HJ, Barrow JR, Winder WW. Skeletal muscle and heart LKB1 deficiency causes decreased voluntary running and reduced muscle mitochondrial marker enzyme expression in mice. Am J Physiol Endocrinol Metab 292: E196–E202, 2007. [DOI] [PubMed] [Google Scholar]
- 309.Thong FS, Bilan PJ, Klip A. The Rab GTPase-activating protein AS160 integrates Akt, protein kinase C, and AMP-activated protein kinase signals regulating GLUT4 traffic. Diabetes 56: 414–423, 2007. [DOI] [PubMed] [Google Scholar]
- 310.Thorens B, Mueckler M. Glucose transporters in the 21st century. Am J Physiol Endocrinol Metab 298: E141–E145, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Thurmond DC, Ceresa BP, Okada S, Elmendorf JS, Coker K, Pessin JE. Regulation of insulin-stimulated GLUT4 translocation by munc18c in 3T3L1 adipocytes. J Biol Chem 273: 33876–33883, 1998. [DOI] [PubMed] [Google Scholar]
- 312.Thurmond DC, Pessin JE. Discrimination of GLUT4 vesicle trafficking from fusion using a temperature-sensitive Munc18c mutant. EMBO J 19: 3565–3575, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Tiano JP, Springer DA, Rane SG. SMAD3 negatively regulates serum irisin and skeletal muscle FNDC5 and PGC-1α during exercise. J Biol Chem 290: 7671–7684, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Tong M, Saito T, Zhai P, Oka SI, Mizushima W, Nakamura M, Ikeda S, Shirakabe A, Sadoshima J. Mitophagy is essential for maintaining cardiac function during high fat diet-induced diabetic cardiomyopathy. Circ Res 124: 1360–1371, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: Pathogenesis, diagnosis, and treatment. Ochsner J 15: 58–69, 2015. [PMC free article] [PubMed] [Google Scholar]
- 316.Trammell SA, Weidemann BJ, Chadda A, Yorek MS, Holmes A, Coppey LJ, Obrosov A, Kardon RH, Yorek MA, Brenner C. Nicotinamide riboside opposes type 2 diabetes and neuropathy in mice. Sci Rep 6: 26933, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Treebak JT, Frosig C, Pehmoller C, Chen S, Maarbjerg SJ, Brandt N, MacKintosh C, Zierath JR, Hardie DG, Kiens B, Richter EA, Pilegaard H, Wojtaszewski JF. Potential role of TBC1D4 in enhanced post-exercise insulin action in human skeletal muscle. Diabetologia 52: 891–900, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Trendelenburg AU, Meyer A, Rohner D, Boyle J, Hatakeyama S, Glass DJ. Myostatin reduces Akt/TORC1/p70S6K signaling, inhibiting myoblast differentiation and myotube size. Am J Phys Cell Phys 296: C1258–C1270, 2009. [DOI] [PubMed] [Google Scholar]
- 319.Trenerry MK, Carey KA, Ward AC, Cameron-Smith D. STAT3 signaling is activated in human skeletal muscle following acute resistance exercise. J Appl Physiol 102: 1483–1489, 2007. [DOI] [PubMed] [Google Scholar]
- 320.Tunduguru R, Chiu TT, Ramalingam L, Elmendorf JS, Klip A, Thurmond DC. Signaling of the p21-activated kinase (PAK1) coordinates insulin-stimulated actin remodeling and glucose uptake in skeletal muscle cells. Biochem Pharmacol 92: 380–388, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Tunduguru R, Zhang J, Aslamy A, Salunkhe VA, Brozinick JT, Elmendorf JS, Thurmond DC. The actin-related p41ARC subunit contributes top21-activated kinase-1 (PAK1)-mediated glucose uptake into skeletal muscle cells. J Biol Chem 292: 19034–19043, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Turki A, Hayot M, Carnac G, Pillard F, Passerieux E, Bommart S, de Mauverger ER, Hugon G, Pincemail J, Pietri S, Lambert K, Belayew A, Vassetzky Y, Juntas Morales R, Mercier J, Laoudj-Chenivesse D. Functional muscle impairment in facioscapulohumeral muscular dystrophy is correlated with oxidative stress and mitochondrial dysfunction. Free Radic Biol Med 53: 1068–1079, 2012. [DOI] [PubMed] [Google Scholar]
- 323.Tuso P. Prediabetes and lifestyle modification: Time to prevent a preventable disease. Perm J 18: 88–93, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Vaughan RA, Gannon NP, Mermier CM, Conn CA. Irisin, a unique non-inflammatory myokine in stimulating skeletal muscle metabolism. J Physiol Biochem 71: 679–689, 2015. [DOI] [PubMed] [Google Scholar]
- 325.Vazirani RP, Verma A, Sadacca LA, Buckman MS, Picatoste B, Beg M, Torsitano C, Bruno JH, Patel RT, Simonyte K, Camporez JP, Moreira G, Falcone DJ, Accili D, Elemento O, Shulman GI, Kahn BB, McGraw TE. Disruption of adipose Rab10-dependent insulin Signaling causes hepatic insulin resistance. Diabetes 65: 1577–1589, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Vella L, Caldow MK, Larsen AE, Tassoni D, Della Gatta PA, Gran P, Russell AP, Cameron-Smith D. Resistance exercise increases NF-kappaB activity in human skeletal muscle. Am J Physiol Regul Integr Comp Physiol 302: R667–R673, 2012. [DOI] [PubMed] [Google Scholar]
- 327.Volchuk A, Wang Q, Ewart HS, Liu Z, He L, Bennett MK, Klip A. Syntaxin 4 in 3T3-L1 adipocytes: Regulation by insulin and participation in insulin-dependent glucose transport. Mol Biol Cell 7: 1075–1082, 1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Vosseller K, Wells L, Lane MD, Hart GW. Elevated nucleocytoplasmic glycosylation by O-GlcNAc results in insulin resistance associated with defects in Akt activation in 3T3-L1 adipocytes. Proc Natl Acad Sci U S A 99: 5313–5318, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Vozarova B, Weyer C, Hanson K, Tataranni PA, Bogardus C, Pratley RE. Circulating interleukin-6 in relation to adiposity, insulin action, and insulin secretion. Obes Res 9: 414–417, 2001. [DOI] [PubMed] [Google Scholar]
- 330.Wagner KR, Fleckenstein JL, Amato AA, Barohn RJ, Bushby K, Escolar DM, Flanigan KM, Pestronk A, Tawil R, Wolfe GI, Eagle M, Florence JM, King WM, Pandya S, Straub V, Juneau P, Meyers K, Csimma C, Araujo T, Allen R, Parsons SA, Wozney JM, Lavallie ER, Mendell JR. A phase I/IItrial of MYO-029 in adult subjects with muscular dystrophy. Ann Neurol 63: 561–571, 2008. [DOI] [PubMed] [Google Scholar]
- 331.Wahren J, Felig P, Ahlborg G, Jorfeldt L. Glucose metabolism during leg exercise in man. J Clin Invest 50: 2715–2725, 1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Wallberg-Henriksson H. Repeated exercise regulates glucose transport capacity in skeletal muscle. Acta Physiol Scand 127: 39–44, 1986. [DOI] [PubMed] [Google Scholar]
- 333.Wang D, Ning W, Xie D, Guo L, DuBois RN. Peroxisome proliferator-activated receptor delta confers resistance to peroxisome proliferator-activated receptor gamma-induced apoptosis in colorectal cancer cells. Oncogene 31: 1013–1023, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Wang Q, Somwar R, Bilan PJ, Liu Z, Jin J, Woodgett JR, Klip A. Protein kinase B/Akt participates in GLUT4 translocation by insulin in L6 myoblasts. Mol Cell Biol 19: 4008–4018, 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Wang Y, An H, Liu T, Qin C, Sesaki H, Guo S, Radovick S, Hussain M, Maheshwari A, Wondisford FE, O’Rourke B, He L. Metformin improves mitochondrial respiratory activity through activation of AMPK. Cell Rep 29: 1511–1523.e1515, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR. Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann Intern Med 113: 909–915, 1990. [DOI] [PubMed] [Google Scholar]
- 337.Way KL, Hackett DA, Baker MK, Johnson NA. The effect of regular exercise on insulin sensitivity in type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Metab J 40: 253–271, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Whelan SA, Dias WB, Thiruneelakantapillai L, Lane MD, Hart GW. Regulation of insulin receptor substrate 1 (IRS-1)/AKT kinase-mediated insulin signaling by O-linked beta-N-acetylglucosamine in 3T3-L1 adipocytes. J Biol Chem 285: 5204–5211, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Whitfield J, Paglialunga S, Smith BK, Miotto PM, Simnett G, Robson HL, Jain SS, Herbst EAF, Desjardins EM, Dyck DJ, Spriet LL, Steinberg GR, Holloway GP. Ablating the protein TBC1D1 impairs contraction-induced sarcolemmal glucose transporter 4 redistribution but not insulin-mediated responses in rats. J Biol Chem 292: 16653–16664, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Whitham M, Chan MHS, Pal M, Matthews VB, Prelovsek O, Lunke S, El-Osta A, Broenneke H, Alber J, Brüning JC, Wunderlich FT, Lancaster GI, Febbraio MA. Contraction-induced interleukin-6 gene transcription in skeletal muscle is regulated by c-Jun terminal kinase/activator protein-1. J Biol Chem 287: 10771–10779, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Wilden PA, Siddle K, Haring E, Backer JM, White MF, Kahn CR. The role of insulin receptor kinase domain autophosphorylation in receptormediated activities. Analysis with insulin and anti-receptor antibodies. J Biol Chem 267: 13719–13727, 1992. [PubMed] [Google Scholar]
- 342.Wiseman DA, Kalwat MA, Thurmond DC. Stimulus-induced S-nitrosylation of syntaxin 4 impacts insulin granule exocytosis. J Biol Chem 286: 16344–16354, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Witczak CA, Jessen N, Warro DM, Toyoda T, Fujii N, Anderson ME, Hirshman MF, Goodyear LJ. CaMKII regulates contraction- but not insulin-induced glucose uptake in mouse skeletal muscle. Am J Physiol Endocrinol Metab 298: E1150–E1160, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Wojtaszewski JF, Higaki Y, Hirshman MF, Michael MD, Dufresne SD, Kahn CR, Goodyear LJ. Exercise modulates postreceptor insulin signaling and glucose transport in muscle-specific insulin receptor knockout mice. J Clin Invest 104: 1257–1264, 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Woldt E, Sebti Y, Solt LA, Duhem C, Lancel S, Eeckhoute J, Hesselink MK, Paquet C, Delhaye S, Shin Y, Kamenecka TM, Schaart G, Lefebvre P, Neviere R, Burris TP, Schrauwen P, Staels B, Duez H. Rev-erb-alpha modulates skeletal muscle oxidative capacity by regulating mitochondrial biogenesis and autophagy. Nat Med 19: 1039–1046, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Woods A, Dickerson K, Heath R, Hong SP, Momcilovic M, Johnstone SR, Carlson M, Carling D. Ca2+/calmodulin-dependent protein kinase kinase-beta acts upstream of AMP-activated protein kinase in mammalian cells. Cell Metab 2: 21–33, 2005. [DOI] [PubMed] [Google Scholar]
- 347.World Health Organization. Global report on diabetes. Geneva, Switzerland, 2016. [Google Scholar]
- 348.Wright DC, Hucker KA, Holloszy JO, Han DH. Ca2+ and AMPK both mediate stimulation of glucose transport by muscle contractions. Diabetes 53: 330–335, 2004. [DOI] [PubMed] [Google Scholar]
- 349.Xiong Y, Wu Z, Zhang B, Wang C, Mao F, Liu X, Hu K, Sun X, Jin W, Kuang S. Fndc5 loss-of-function attenuates exercise-induced browning of white adipose tissue in mice. FASEB J 33: 5876–5886, 2019. [DOI] [PubMed] [Google Scholar]
- 350.Yamada E, Okada S, Saito T, Ohshima K, Sato M, Tsuchiya T, Uehara Y, Shimizu H, Mori M. Akt2 phosphorylates Synip to regulate docking and fusion of GLUT4-containing vesicles. J Cell Biol 168: 921–928, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, Yamashita S, Noda M, Kita S, Ueki K. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med 8: 1288, 2002. [DOI] [PubMed] [Google Scholar]
- 352.Yang C, Coker KJ, Kim JK, Mora S, Thurmond DC, Davis AC, Yang B, Williamson RA, Shulman GI, Pessin JE. Syntaxin 4 heterozygous knockout mice develop muscle insulin resistance. J Clin Invest 107: 1311–1318, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Yang H, Chang J, Chen W, Zhao L, Qu B, Tang C, Qi Y, Zhang J. Treadmill exercise promotes interleukin 15 expression in skeletal muscle and interleukin 15 receptor alpha expression in adipose tissue of high-fat diet rats. Endocrine 43: 579–585, 2013. [DOI] [PubMed] [Google Scholar]
- 354.Yang J, Holman GD. Insulin and contraction stimulate exocytosis, but increased AMP-activated protein kinase activity resulting from oxidative metabolism stress slows endocytosis of GLUT4 in cardiomyocytes. J Biol Chem 280: 4070–4078, 2005. [DOI] [PubMed] [Google Scholar]
- 355.Yang SJ, Hong HC, Choi HY, Yoo HJ, Cho GJ, Hwang TG, Baik SH, Choi DS, Kim SM, Choi KM. Effects of a three-month combined exercise programme on fibroblast growth factor 21 and fetuin-A levels and arterial stiffness in obese women. Clin Endocrinol 75: 464–469, 2011. [DOI] [PubMed] [Google Scholar]
- 356.Yarasheski K, Bhasin S, Sinha-Hikim I, Pak-Loduca J, Gonzalez-Cadavid N. Serum myostatin-immunoreactive protein is increased in 60–92 year old women and men with muscle wasting. J Nutr Health Aging 6: 343–348, 2002. [PubMed] [Google Scholar]
- 357.Yeo NH, Woo J, Shin KO, Park JY, Kang S. The effects of different exercise intensity on myokine and angiogenesis factors. J Sports Med Phys Fitness 52: 448–454, 2012. [PubMed] [Google Scholar]
- 358.Yin Y, Russell RG, Dettin LE, Bai R, Wei ZL, Kozikowski AP, Kopelovich L, Glazer RI. Peroxisome proliferator-activated receptor delta and gamma agonists differentially alter tumor differentiation and progression during mammary carcinogenesis. Cancer Res 65: 3950–3957, 2005. [DOI] [PubMed] [Google Scholar]
- 359.Young A, Stokes M, Crowe M. The size and strength of the quadriceps muscles of old and young men. Clin Physiol 5: 145–154, 1985. [DOI] [PubMed] [Google Scholar]
- 360.Yu H, Rathore SS, Lopez JA, Davis EM, James DE, Martin JL, Shen J. Comparative studies of Munc18c and Munc18–1 reveal conserved and divergent mechanisms of Sec1/Munc18 proteins. Proc Natl Acad Sci U S A 110: E3271–E3280, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Yu KT, Czech MP. Tyrosine phosphorylation of the insulin receptor beta subunit activates the receptor-associated tyrosine kinase activity. J Biol Chem 259: 5277–5286, 1984. [PubMed] [Google Scholar]
- 362.Zhang J, Oh E, Merz KE, Aslamy A, Veluthakal R, Salunkhe VA, Ahn M, Tunduguru R, Thurmond DC. DOC2B promotes insulin sensitivity in mice via a novel KLC1-dependent mechanism in skeletal muscle. Diabetologia 62: 845–859, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Zhang X, Rebane AA, Ma L, Li F, Jiao J, Qu H, Pincet F, Rothman JE, Zhang Y. Stability, folding dynamics, and long-range conformational transition of the synaptic t-SNARE complex. Proc Natl Acad Sci 113: E8031–E8040, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Zhang X, Yeung DC, Karpisek M, Stejskal D, Zhou ZG, Liu F, Wong RL, Chow WS, Tso AW, Lam KS, Xu A. Serum FGF21 levels are increased in obesity and are independently associated with the metabolic syndrome in humans. Diabetes 57: 1246–1253, 2008. [DOI] [PubMed] [Google Scholar]
- 365.Zhou X, Wang JL, Lu J, Song Y, Kwak KS, Jiao Q, Rosenfeld R, Chen Q, Boone T, Simonet WS, Lacey DL, Goldberg AL, Han HQ. Reversal of cancer cachexia and muscle wasting by ActRIIB antagonism leads to prolonged survival. Cell 142: 531–543, 2010. [DOI] [PubMed] [Google Scholar]
- 366.Zmijewski JW, Banerjee S, Bae H, Friggeri A, Lazarowski ER, Abraham E. Exposure to hydrogen peroxide induces oxidation and activation of AMP-activated protein kinase. J Biol Chem 285: 33154–33164, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]