Abstract
Currently, the novel coronavirus pneumonia has been widespread globally, and there is no specific medicine. In response to the emergency, we employed bioinformatics methods to investigate the virus's pathogenic mechanism, finding possible control methods. We speculated in previous studies that E protein was associated with viral infectivity. The present study adopted the domain search techniques to analyse the E protein. According to the results, the E protein could bind iron or haem. The iron and haem bound by the E protein came from the attacked haemoglobin and phagocytes. When E protein was attached to haem, it synthesised oxygen and water into superoxide anions, hydrogen peroxide and hydroxyl radicals. When the iron-bound E protein and the haem-bound E protein worked together, they converted superoxide anions and hydrogen peroxide into oxygen and water. These were the “ROS attack” and “ROS escape” of the virus. “ROS attack” damaged the tissues or cells exposed on the surface of the virus, and “ROS escape” decomposed the superoxide anion and hydrogen peroxide that attacked the virus. When NK cells were exposed to infected cells, viruses that had not shed from the infected cells’ surface damaged them through “ROS attack”. In addition, lymphocytes such as T cells and B cells, which could be close to the antigen of the virus surface, were also easily damaged or killed by the "ROS attack", generating a decrease in lymphocytes. When memory B cells were exposed to the virus’s surface antigen, they were also damaged by “ROS attack”, resulting in the patient's re-infection. The virus applied the “ROS escape” to decompose hydrogen peroxide released by phagocytes into oxygen and water. The surrounding cells were replenished with oxygen, and the patient was in a “happy hypoxia” state. When the phagocytes swallowed the virus, the E protein converted superoxide anions into oxygen and water. In this way, the virus parasitized in the vesicles of the phagocyte. While virus was in the lysosome, the E protein generated ROS to damage nearby hydrolases. In this way, the virus parasitized the lysosome. Excessive hydroxyl free radicals destroyed the membrane structure of the lysosome, causing the hydrolase release from lysosome, autophagy of phagocytic cells and subsequent cell death. As a result, the colonizing phagocytes of the virus was associated with asymptomatic infection or retest-positive. Briefly, the virus inhibited the immune system through “ROS escape”, and damaged the immune system by “ROS attack”. The destruction instigated a strong cytokine storm, leading to organ failure and complications.
Keywords: Novel coronavirus, envelope protein, asymptomatic infection, reinfection, lymphopenia, macrophage, cytokine storm
1. Background
Patients infected with COVID-19 will show different immune responses. Asymptomatic individuals have a weaker immune response to SARS-CoV-2 infection [1]. In symptomatic patients, the number of lymphocytes in the peripheral blood decreased rapidly [2] while the number of neutrophils and monocytes increased [3], presenting immune disorders and abnormal immune responses [4]. After being discharged from the hospital, some patients remained/recovered virus-positive, while others even relapsed, indicating that it may be challenging to induce virus-eliminating immune responses against SARS-CoV-2 in some patients [5]. Critically ill patients will have a high inflammatory immune response, generating acute respiratory distress syndrome (ARDS) and multiple organ failure [6]. The pathogenesis of severe COVID-19 pneumonia involves a cytokine storm of the dysregulated immune response rather than direct viral damage [7]. A fast and well-coordinated natural immune response remains a critical line in defense against viral infections. The innate immune system profoundly changes the adaptive immune response to foreign invaders and self-antigens [8]. However, when the immune response is unregulated, it can lead to excessive inflammation and even death [9]. Patients with COVID-19 pneumonia are highly autoimmune reaction, and their presence appears to be in association with a poor prognosis [10,11]. Innate immunity may exert an essential role in developing the cytokine storm and enhancing the severer forms [12]. Consequently, studying how viruses directly induce damage to the human immune system provides great significance for disease prevention and treatment during a pandemic.
The detailed immune response mechanism of asymptomatic infection is still unclear. The typical asymptomatic transmission of cohabiting family members is as long as 3 weeks [13]. During incubation period, patients also hold the virus [14]. About 15–45% of SARS-CoV-2 infections are asymptomatic [15,16], increasing at the population level [17,18]. Asymptomatic infections have no symptoms such as dyspnoea, lymphocyte counts, and chest CT images are familiar, but qRT-PCR specific for COVID-19 disease [19]. Only qRT-PCR specific for COVID-19 disease can be used for differential diagnosis [20]. The invasion of SARS-CoV-2 in asymptomatic patients only generates a specific mild immune response [21]. Neutralising antibodies in asymptomatic individuals decline rapidly, disappearing within a short period [22]. In asymptomatic and symptomatic SARS-CoV-2, specific T cells’ response is similar, but high level of IFN-γ and IL-2 in asymptomatic [23]. Weak antiviral immunity is the characteristic of asymptomatic SARS-CoV-2 infection. Moreover, it may trigger a highly functionalised virus-specific cellular immune response. They relate it to the proportional secretion of IL-10 and pro-inflammatory cytokines (IL-6, TNF-α and IL-1β). However, in symptomatic individuals, it disproportionately secretes them [23].
Reinfection is more mysterious than asymptomatic infection. Retest positive [24] and reinfection [25] have been sporadically reported. However, reinfection is not equal to retested positive. After the initial infection, T cell immunity is detectable in most recovered patients, including memory CD4+ T cells and memory CD8 + T cells [26,27]. Memory T cell responses include spike proteins and nucleocapsid proteins, and membrane proteins [28]. The interval between the reinfection and the last infection is generally 4–5 months, and the corresponding SARS-CoV-2 antibody is not detectable during the reinfection period. Although the virus strain is different from the previous one, it cannot be ascertained whether the amino acid mutation of spike protein causes reinfection [29]. However, high-affinity IgG and high-titer neutralising antibodies are found in the early stages of reinfection, causing more robust antibody responses. Yet, no IgM is found, and the lack of IgM response is compatible with reinfection [30].
SARS-CoV-2 infection can activate abnormal inflammation and immune response [4], which is manifested by increased levels of IL-6, IL-1β, IL-8, IL-17, G-CSF, GM-CSF, IP10, MCP1, MIP1α, TNF, C-reactive protein and D-dimer. Extremely high levels of pro-inflammatory cytokines can give rise to the cytokine storm, causing local or systemic tissue damage—excessive dimer and cellulose levels for extensive capillary coagulation reactions [31]. Inflammation and blood clotting occur in multiple types of organs, such as lungs, heart, kidneys, nervous system, bone marrow and vessels. According to relevant autopsy report, the novel coronavirus pneumonia is an extremely destructive disease and SARS-CoV-2 particles are detected in the patient’s respiratory system, kidneys and gastrointestinal tract [32]. Moreover, lungs are infiltrated by massive macrophages and monocytes, and the amount of polykaryocyte cells is still large. There are likewise a few lymphocytes, eosinophils and neutrophils. The lymphocytes are dominated by positive CD4 +T cells [33]. Moreover, the lesions are all manifested as diffuse alveolar damage, accompanied by fibrin membrane formation and fibrin clumps in the alveoli [34]. In addition, hyaline membrane formation, fibrin exudate, epithelial damage and diffuse-type II lung cell hyperplasia are also found in the lungs [35]. Inflammation and fibrin microthrombus appear in the tissues around the heart capillaries, liver sinuses and renal tubules [36]. Taken together, these features show that viruses also damage the human immune system, directly or indirectly causing these severe diseases.
Lymphopenia is considered as the common immune problem of COVID19 diseases. In death cases [37], the levels of IL-1α and IL-6 were increased, the percentages of Th2, Th17 cells and Treg were substantially lower, and patients are faced with exhausted CD4+ and CD8 + T cells and activated CD4 + T cells. The lymphopenia by SARS-CoV-2 contributes to the production of CD4 + T cells, CD8 + T cells, B cells and natural killer (NK) cells, with the damage of CD8 + T cells being more significant [2, 38]. In the recovery of COVID-19 patients [39], the level of lymphocytes is still significantly reduced; the levels of Treg, activated CD4 + T cells and depleted CD8 + T cells are significantly decreased; and the percentage of B cells is increased. At the last period of recovering from COVID-19 [39], the levels of IL-1α, IL-1β, IL-6, TNF-α and IL-10 are significantly decreased. After recovering, the level of IL-10 is significantly increased [37], the frequency of Th1, Th2 and Th17 cells is increased [39], the level of B cells is decreased. The recovery status of lymphocytes shows that despite the improved immune regulation in recovered patients, the disease can cause inevitable long-term damage to the immune system. There are many reasons for lymphopenia, such as IL-6, IL-10 or tumour necrosis factor (TNF). Dendritic cells and neutrophils also act indirectly to diminish lymphocytes [40]. Exaggerated activation of T cells or high-level expression of pro-apoptotic molecules is also likely to induce depletion of T cells [41,42]. However, the autopsy report reveals that the inflammatory cell infiltration comprised a mixture of CD4 + T and CD8 + T lymphocytes, mainly in the interstitial spaces and around the broader bronchioles and blood vessels. However, programmed cell death protein-1 (PD-1) and PD-L1 protein is undetectable on the surface of lymphocytes. No obvious virus infection is detected in lymphocytes and mesenchymal cells. S protein was not combined with T lymphocytes [43].
Oxidative stress damage to lymphocytes is considered to possibly cause lymphopenia. The autopsy report further proves that T-cell lymphocytes with a CD4:CD8 proportion of 1.7 infiltrated the interstitial myocardium. Hypertrophy in the myocardial fibre occurs–-iron-catalysed regulatory cell death induced by extreme peroxidation of fatty acids [44]. Myocardial interstitial macrophage infiltration spreads, and there is no clear concerning damage to myocardial cells containing the left and right ventricles [45]. Therefore, myocarditis is lymphocytic inflammation, which collects massive positive CD20-B cells, CD3+ T lymphocytes and various CD68+ macrophages without eosinophils, giant cells or granulomas. Moreover, fibroblasts/macrophages in the heart play a vital role in motivating myocardial destruction [46].
When T cell help is damaged, NK cells can help trigger autoimmune independent of T cells [47]. NK cells are a subset of monocytes, playing an immunomodulatory role in preventing autoimmune diseases [48]. For COVID-19 patients, the number of CD56low CD16+NK cells is increased in the late recovery period [39]. Autoimmune mechanisms are also critically involved in the pathogenesis of autoimmune fatigue syndrome [49], which may reflect myasthenia gravis as an immune disorder [50]. The severe fatigue sequelae of COVID19 patients may be associated with this mechanism. Type 1 interferon (IFN-I) promotes the expansion of NK cells [51], but SARS-CoV-2 infection of respiratory epithelial cells does not significantly induce antiviral IFN-1 and Type III interferon (IFN-III) [52]. It derived NK cells from the differentiation and development of bone marrow haematopoietic stem cells. Relatively low fluctuations in oxidative stress levels can control the self-renewal and proliferation capabilities of haematopoietic stem cells [53]. Haematopoietic stem cells with elevated oxidative stress levels undergo proliferation and differentiation after mobilising to a more oxygen-rich bloodstream [54]. High oxidative stress levels may trigger phenotype alteration in haematopoietic stem cells [55] and differentiation into more NK cells. Therefore, relevant report has shown that patients who die during treatment face a significantly increased frequency of CD56dim CD16 + NK cells and CD56bright CD16dim/- NK cells compared to recovered and healthy individuals, indicating that COVID19 patients who died are burdened with higher oxidative stress damage [37].
Macrophages play a role in eliminating pathogens and promoting organ repair. However, Macrophages promotes a series of pathogenic functions, including the release of cytokines and enzymes, the production of reactive oxygen species [56]. Macrophages are the prominent participants in the so-called cytokine storm and may damage tissues instead [57]. The number of megakaryocytes discovered in the lungs and heart is much more than usual. The deceased alveolar cavity with the pneumonia is filled with massive macrophages scattered with neutrophils and lymphocytes. CD61 + megakaryocytes represent lung megakaryocytes, with obvious nuclear proliferation and atypicality, which are located in the alveolar capillaries. Neutrophils partially denature and trapped—many neutrophils in small blood vessels [58]. Positive CD68 macrophages show the phenomena of intracytoplasmic phagocytosis, spherical eosinophilic hyaloplasm or hemophagocytic and multinucleated giant cells. Several chemokines and inflammatory cytokines are secreted by alveolar macrophages, including IL-6, IL-10 and TNFα. Pulmonary inflammatory macrophages show potent interferon characteristics. In spite of the protective effect of interferon in the previous stage of the disease, the continuous production of IFNγ may cause an extravagant macrophage activation problem.
The persistence of SARS-CoV-2 in monocytes may be temporary. After infection by virus replication, the monocytes are differentiate into tissue macrophages, where the virus can replicate and produce progeny virions that can further infect surrounding cells [57]. Electron microscope observation discloses the presence of SARS-CoV-2 particles in the cytoplasm of macrophages [59]. Coronavirus-specific antibodies enhance the virus uptake by macrophages by combining with FcR. SARS-CoV-2 may enter alveolar macrophages through the interaction between S protein and ACE2 receptor. ACE2 is also expressed on the surface of lung macrophages. It can detect CD68 and CD169 macrophages expressing ACE2 in the spleen’s marginal area and the marginal sinuses of lymph nodes. These macrophages have the SARS-CoV-2 nucleoprotein antigen and can upregulate IL-6 level. S protein cooperates with monocytes/macrophages—CD68. Programmed death-ligand (PD-L1) is widely expressed on the surface of alveolar macrophages [43].
These signs show that CD169 macrophages, like a Trojan horse, make virus transmission, excessive inflammation and activation-induced lymphocyte death [60]. Phagocytes infected with MERS-CoV can facilitate virus replication and spread by acting as virus reservoirs and transport proteins. MERS-CoV replicates inside phagocytes and attenuates the innate immunity in hosts [61]. Besides, phagocytes cannot kill Mycobacterium tuberculosis [62], Brucella [63], Leishmania [64] or HIV [65]. For example, Leishmania parasites in phagocytic vacuoles. Therefore, the SARS-CoV-2 virus may also colonise phagocytes. Moreover, pathogens such as silica sand [66,67] and Mycobacterium tuberculosis [68,69] rupture lysosomes. After the phagocytes swallowed pathogens, lysosomes also rupture to release hydrolase. Hydrolase promotes the inflammation and death of phagocytes. After the phagocytes swallow the debris and Mycobacterium tuberculosis, they are similarly inflamed and die. This vicious circle induces severe inflammation and fibrosis in neighbouring tissues. SARS-CoV-2 pneumonia has similar tissue inflammation and fibrosis.
Although COVID-19 patients are also accompanied by nervous system inflammation, there is no sufficient evidence supporting that the SARS-CoV-2 virus infects neurons [70]. Patients with severe neurological diseases (such as stroke) only have mixed lymphocytes or mononuclear inflammatory infiltration in the meningeal space and cortical tissues. The patients have a neurovascular brain injury or microvascular dysfunction [71]. RT-PCR result of cerebrospinal fluid (CSF) from patients with encephalitis and meningitis is negative for COVID-19 [72]. Polymerase chain reaction (PCR) of cerebrospinal fluid of patients for acute disseminated encephalomyelitis is also negative [72]. In patients with neuromuscular diseases, cerebrospinal fluid analysis discloses that albumin cytology is dissociated. However, the PCR test for COVID-19 is also negative [73]. Odour and taste disorders are characteristic symptoms of SARS-CoV-2 infection. Contrary to other infectious odour damage, the odour and taste loss of COVID-19 sounds to be characterised by a severe nose blocked; not any changes in the paranasal sinuses, such as ethmoid plate olfactory nerve and meninges. There are no signs of acute or chronic ischaemic events [74]. Only RT-PCR result of cerebrospinal fluid from patients with epilepsy is positive for COVID-19 [75].
The inflammation was also an oxidative stress injury because SARS-CoV-2 viruses might release reactive oxygen species (ROS). A strange coincidence was noticed that the most consumed T and B lymphocytes could contact the antigen of virus surface. According to immune theory, if the antigen (such as pathogen-specific protein) is present on the surface of the pathogen, the pathogen can directly stimulate T cells. It entailed that oxidative stress broke the cell membranes structure of T and B lymphocytes, such as lipids and proteins when exposing to the virus. Lymphocytes will rupture or apoptosis. The total number of lymphocytes in the body subsequently decreases. Sometimes, NK cells did not require antigen stimulation to kill infected cells. When NK cells were exposed to the surface of infected cells, the nearby unshed virus particles would release ROS, and NK cells were also destroyed by oxidative stress. Because of the difference in the shedding position, the destruction efficiency of the virus may not be high, resulting in more NK cells in patients who died [37]. Therefore, it believed that the virus could release ROS to damage the human immune system.
We considered that SARS-CoV-2 virus also damaged tissues nearby neurological system through oxidative stress action. If the phagocytes ruptured neared the odour and taste cells, the free SARS-CoV-2 virus would attack the cells, generating oxidative stress damage to the cells, followed by the appearance of odour and taste disorders. If the infected phagocytes ruptured near the meningeal space, the released virus could damage the cerebral cortex through ROS attack and induced brain inflammation. The oxidative stress damage to the immune and nervous system of patients with epilepsy was more serious since the infected phagocytes would rupture after penetrating the spinal cord tissue. The virus could invade the spinal fluid and be further carried into the cerebrospinal fluid through the cerebrospinal fluid circulation.
It is still confusing that the E protein was not included in the report mentioned above on memory T cells' response. The haem theory believes that SARS-CoV-2, an acidophilic anaerobic virus, can suppresse haem metabolism by attacking haemoglobin and dissociating haem and hunting porphyrins [76]. This attack provides an enormous amount of iron or haem. The E protein of SARS-CoV-2 is associated with high infection. E owns a haem iron linked sites and carries iron catalytic properties similar to the cytochrome C oxidase. If these sites had the iron catalytic activity of superoxide dismutase, catalase, peroxidase, it could offer ROS such as O-, H2O2, or ·OH. Peroxidase can produce hydroxyl radical OH(78). OH could damage the structure of membranes, proteins and nucleic acids [77], which also provoked peroxidation and rupture of lysosomal membranes. In this study, bioinformatics methods were applied to investigate the catalytic function of viral E protein. The MEME tool was adopted to explore the conserved domains between E protein and bacterial superoxide dismutase, catalase, peroxidase on a large scale and determine the iron link site of E protein with iron-catalysed production of ROS. We subsequently determined the iron catalytic region of E protein outside the membrane-binding area, which revealed the E protein had sites that captured iron and generated ROS to damage the human immune system.
2. Method
2.1. Flow chart of analysis method
It indicates the flow chart of bioinformatics analysis in this study. First, we employed the localised MEME tool to search for several conserved domains of E protein enzymes. We subsequently analysed that the haem linked site of E protein was on the outer surface of the viral membrane. Finally, in this comprehensive study, we summarised the various enzymatic functions of E protein to catalyse the generation or decomposition of ROS.
2.2. Localised MEME tool to scan for conserved domains
The analysis steps are listed as follows:
Download MEME from the official website and subsequently install in the virtual machine ubuntu operating system. The virtual machine was VM 15.2.
Download the E protein sequence of SARS-CoV-2 from NCBI official website.
Download the fasta format sequence of superoxide dismutase, catalase, peroxidase from Uniprot official website, respectively. The search keyword was “bacteria” + enzyme name.
For each sequence in all enzyme (each species), paired with the E protein sequence to generate fasta format files for MEME analysis.
For the files generated in Step 4, a batch of 50000 was used to create several batches. It was considered as the limited space of the virtual ubuntu system.
In ubuntu, searched the conserved domains of E protein and enzymes (various species) with MEME tools in batches.
Collected the result files of conserved domains.
Searched and download the 3D space files or domain functions of related enzymes from the NCBI official website and analysed the functional roles of the conserved domains.
2.3. Transmembrane analysis
We directly compared the transmembrane sites of E Protein to the haem linked sites, which subsequently determined that the haem linked sites were outside the membrane structure.
3. Results
3.1. E Protein had activity of the superoxide dismutase
It describes the superoxide dismutase (SOD) catalysing the conversion from superoxide radicals to molecular oxygen in InterPro entry IPR019831. Functionally, SOD can destroy free radicals produced in cells. Fe/Mn SODs are ubiquitous enzymes responsible for most SOD activity in prokaryotes, fungi, cyanobacteria and mitochondria.s Fe/MnSOD, a homodimer or homotetramer, is divided into two domains, an αN-terminal domain connected by a loop and an alpha/beta C-terminal domain.
We downloaded 184306 SOD enzyme sequences of various bacteria from the UniProt website. We further adopted the local MEME tool to search for motif between each sequence and the E protein (E-value < 0.05). We subsequently explored the conserved domain name corresponding to the motif on the SOD sequence from the UniProt website through the web crawler method. Finally, we searched for the conserved domains containing “Fe”. The conserved domains related to the SOD enzyme properties of E protein were listed in Table 1. “CAYCC” was the haem-binding motif found in haem theory. As shown in Table 1, E protein has the N-terminal and C-terminal conserved domains of Fe/Mn-SOD. “CAYCC” and its left is Sod_Fe_N, “CAYCC” and its right is Sod_Fe_C. “CAYCC” also was the conserved motif of ferritin, ferric oxidoreductase and ferredoxin (2Fe-2S ferredoxin-type, 4Fe-4S ferredoxin-type). Therefore, E protein had the catalytic regions of SOD enzyme at 1-69, including the transmembrane area and the outer part of the membrane: “MYSFVSEETGTLIVNSVLLFLAFVVFLLVTLAILTALRLCAYCCNIVNVSLVKPSFYVYSRVKNLNSSR”.
Table 1.
Domains of superoxide dismutase active of E protein.
| Domain | Motif | Count |
|---|---|---|
| 1.Sod_Fe_N | ALRLCAYCC | 1 |
| CAYCCN | 3 | |
| CAYCCNI | 13 | |
| CAYCCNIV | 1 | |
| CAYCCNIVN | 18 | |
| CAYCCNIVNVSLVKPSF | 1 | |
| CCNIVN | 1 | |
| CCNIVNVSLVKP | 1 | |
| ILTALRLCAYCCN | 1 | |
| ILTALRLCAYCCNI | 1 | |
| ILTALRLCAYCCNIVNVSLVKPSFYVY | 1 | |
| KPSFYVYSRVKNLN | 2 | |
| LCAYCC | 1 | |
| LRLCAYCCNIVNV | 1 | |
| MYSFVSEETGTLIVNSVLLFLAFVVFLLV | 1 | |
| TALRLCAYCC | 1 | |
| TLAILTALRLCAYCC | 2 | |
| TLAILTALRLCAYCCN | 5 | |
| TLAILTALRLCAYCCNIVNVS | 1 | |
| VTLAILTALRLCAYCCNIVNVSLVKPSFYVYSRVKNLN | 1 | |
| YCCNIVNVSLVKPS | 1 | |
| YCCNIVNVSLVKPSFYVYSRVK | 1 | |
| 2.Sod_Fe_C | AILTALRLCAYCC | 1 |
| CAYCCN | 8 | |
| CAYCCNI | 14 | |
| CAYCCNIV | 2 | |
| CAYCCNIVN | 58 | |
| CAYCCNIVNV | 2 | |
| CAYCCNIVNVSLVKPSF | 1 | |
| CAYCCNIVNVSLVKPSFYVYS | 1 | |
| CCNIVN | 9 | |
| CCNIVNV | 1 | |
| CCNIVNVSLVKPSF | 2 | |
| CCNIVNVSLVKPSFYVYSRVK | 2 | |
| CCNIVNVSLVKPSFYVYSRVKNLNSSR | 1 | |
| CNIVNVSLVKPSFYVYSRVKN | 1 | |
| FLAFVVF | 1 | |
| MYSFVSEETGTLIVNSVLLFLAFVVF | 1 | |
| RLCAYCC | 4 | |
| RLCAYCCN | 1 | |
| RLCAYCCNI | 2 | |
| RLCAYCCNIVN | 2 | |
| RLCAYCCNIVNVSLVKPSFYVYSRVKNLNSSR | 1 | |
| YCCNIV | 4 | |
| YCCNIVN | 3 | |
| YCCNIVNVSLVKPSFYVYSRVKNLNSSR | 1 | |
| YSFVSEETGTLIVNSVLLFLAFVVFLLVTLAILTALRLCAY | 1 | |
| 3. 2Fe-2S ferredoxin-type | CAYCCN | 1 |
| CAYCCNI | 1 | |
| 4. 4Fe-4S ferredoxin-type | CAYCCNI | 1 |
| CAYCCNIVNVS | 1 | |
| CAYCCNIVNVSLVKPSFY | 1 | |
| CAYCCNIVNVSLVKPSFYVYS | 2 | |
| CAYCCNIVNVSLVKPSFYVYSRVKNLNSS | 1 | |
| 5. Ferric oxidoreductase | YCCNIVNVSLVKPSFYVYSRVKN | 1 |
| 6. Ferritin | CAYCCN | 5 |
| CAYCCNI | 1 |
The UniProt online ID mapping service was used to convert the PKB name into the ref-protein ID, which gave rise to five ref-proteins “F8FQ25 -> WP_013914333.1; H6NSN4 -> WP_013914333.1; A0A0K2HBM7 -> WP_012820698.1; A0A2A5K0Y4 -> WP_023485148.1; A0A2Z6BF72 -> WP_008879697.1”. For WP_013914333.1 and WP_023485148.1, we failed to open the linked webpage of “Related Structures (Summary)” on the NCBI, and “Master data error” was prompted. The “Related Structures (Summary)” link of WP_012820698.1 and WP_008879697.1 corresponded to the file“2NYBA.cn3”. The motifs of these two proteins were “IEHWWNVVN”, which were comparable to the “CAYCCNIVN” of E protein. But neither of them was in the iron linked site in “2NYBA.cn3”. Due to a lack of structure files, we could not accurately determine that the last C of "CAYCCN" was the iron linked site of SOD enzyme.
The above analysis results revealed that the E protein had the catalytic role of SOD enzyme after binding iron. E protein catalysed superoxide anion and water to generate oxygen and hydrogen peroxide.
3.2. E Protein had an activity of the catalase
Hydrogen peroxide is a product of cell oxidative metabolism. It can be converted into hydroxyl free radicals through transition metals, which can damage various cellular molecules, leading to oxidative stress and cell death. Catalase (EC) is an antioxidant enzyme that catalyses hydrogen peroxide conversion into the water and molecular oxygen [78]. Most catalase enzymes are monofunctional haem-containing enzymes.
We downloaded 73,983 catalase sequences of various bacteria from the UniProt website, followed by searching for each sequence and the motif of E protein (E-VALUE < 0.05) by using the local MEME tool. We subsequently searched for the conserved domain corresponding to the motif on the hydrogen peroxide sequence from the UniProt website using a web crawler method. We also searched for the conserved domains containing “catalase”. The main conserved domains associated with the catalase properties of E protein were listed in Table 2. “CAYCC” is the haem-binding motif found in haem theory. As shown in Table 2, E protein has catalase conserved domains: Catalase, Catalase_C and Catalase-rel. Catalase is the core domain of haem catalase (InterPro entry IPR011614). Catalase-rel is a catalase-related immune response domain with an immunore active amphiphilic octapeptide recognised by T cells [79]. Moreover, catalase_C is an extra C-terminal domain present in large catalase enzymes. It is related to the class I glutamine transferase domain, however, the exact molecular function remains uncertain [80]. “CAYCC”, and its C-end fragments belong to the catalase functional region. The catalase catalytic characteristic region of E protein is at positions 30-69, including the transmembrane area and the outer part of the membrane: “TLAILTALRLCAYCCNIVNVSLVKPSFYVYSRVKNLNSSR”.
Table 2.
Domains of catalase active of E protein.
| Domain | Motif | Count |
|---|---|---|
| 1. Catalase | AILTALRLCAYCC | 1 |
| AILTALRLCAYCCNI | 1 | |
| ALRLCAYCC | 28 | |
| ALRLCAYCCNI | 13 | |
| CAYCCN | 2288 | |
| CAYCCNI | 762 | |
| CAYCCNIV | 506 | |
| CAYCCNIVN | 219 | |
| CAYCCNIVNV | 2 | |
| CAYCCNIVNVS | 47 | |
| CAYCCNIVNVSLVK | 3 | |
| CAYCCNIVNVSLVKPS | 1 | |
| CAYCCNIVNVSLVKPSF | 2 | |
| CAYCCNIVNVSLVKPSFY | 3 | |
| CAYCCNIVNVSLVKPSFYVY | 3 | |
| CAYCCNIVNVSLVKPSFYVYSR | 1 | |
| CAYCCNIVNVSLVKPSFYVYSRVK | 11 | |
| CAYCCNIVNVSLVKPSFYVYSRVKN | 19 | |
| CAYCCNIVNVSLVKPSFYVYSRVKNL | 209 | |
| CAYCCNIVNVSLVKPSFYVYSRVKNLN | 4 | |
| CAYCCNIVNVSLVKPSFYVYSRVKNLNS | 10 | |
| CAYCCNIVNVSLVKPSFYVYSRVKNLNSS | 20 | |
| CCNIVN | 5 | |
| CCNIVNVSLVK | 1 | |
| ILTALRLCAYCC | 7 | |
| ILTALRLCAYCCNI | 2 | |
| ILTALRLCAYCCNIVNVSLVKPSFYVYSRVK | 1 | |
| LCAYCC | 1889 | |
| LCAYCCN | 23 | |
| LCAYCCNI | 1 | |
| LCAYCCNIVN | 4 | |
| LCAYCCNIVNVS | 2 | |
| LCAYCCNIVNVSLVK | 1 | |
| LCAYCCNIVNVSLVKPSFYVYSRVKNLN | 1 | |
| LRLCAYCC | 36 | |
| LRLCAYCCNIVN | 249 | |
| LRLCAYCCNIVNVSLVKPSFYVYSRVKNLNS | 3 | |
| LRLCAYCCNIVNVSLVKPSFYVYSRVKNLNSSR | 8 | |
| RLCAYCC | 305 | |
| RLCAYCCN | 9 | |
| RLCAYCCNI | 25 | |
| RLCAYCCNIVN | 5 | |
| RLCAYCCNIVNVSLVKPSFYVYSR | 2 | |
| RLCAYCCNIVNVSLVKPSFYVYSRVKNLN | 9 | |
| RLCAYCCNIVNVSLVKPSFYVYSRVKNLNS | 44 | |
| RLCAYCCNIVNVSLVKPSFYVYSRVKNLNSS | 3 | |
| RLCAYCCNIVNVSLVKPSFYVYSRVKNLNSSR | 3 | |
| TALRLCAYCC | 52 | |
| TLAILTALRLCAYCCNI | 1 | |
| TLAILTALRLCAYCCNIVN | 1 | |
| YCCNIV | 2 | |
| YCCNIVN | 1 | |
| YCCNIVNVSLVK | 15 | |
| 2. Catalase_C | CAYCCNI | 3 |
| RLCAYCC | 1 | |
| RLCAYCCN | 2 | |
| 3. Catalase-rel | CAYCCNI | 4 |
The above results demonstrated that the E protein had the catalytic function of catalase after binding to haem. Protein E can catalyse the decomposition of hydrogen peroxide into oxygen and water.
3.3. E Protein had activity of the peroxidase
Haem peroxidase, a haem-containing enzyme, can use hydrogen peroxide as an electron acceptor to catalyse multiple oxidation reactions. Haem peroxidase includes two superfamilies: one is found in bacteria, fungi and plants, and the other is found in animals. Among them, Lignin fungi peroxidase has a strong capacity of ·OH generation [81]. In this study, we only selected conserved domains in fungal peroxidase.
We downloaded 554 peroxidase sequences of various fungi (keywords: Lignin fungi peroxidase) from the UniProt website. The local MEME tool was subsequently used to search for motifs between each sequence and the E protein (E-valuE < 0.05). We further searched the conserved domain corresponding to the motif through a web crawler method on the UniProt website, and also manually searched for the conserved domains containing “PEROXIDASE”. The conserved domains related to the peroxidase properties of E protein were listed in Table 3. “CAYCC” is the haem-binding motif found in haem theory. As shown in Table 3, E protein has a peroxidase conserved domain: PEROXIDASE_4. “CAYCC” and its C-end fragments belong to the peroxidase functional region. Moreover, the peroxidase catalytic characteristic region of E protein is the sequence of positions 38-64, including the outer membrane and a small part of the transmembrane region:“RLCAYCCNIVNVSLVKPSFYVYSRVKN”.
Table 3.
Domains of peroxidase (lignin fungi) active of E protein.
| Domain | Motif | Count |
|---|---|---|
| PEROXIDASE_4 | CAYCCN | 1 |
| CAYCCNI | 8 | |
| CAYCCNIVN | 3 | |
| CAYCCNIVNVSLVK | 1 | |
| CAYCCNIVNVSLVKPSFY | 1 | |
| CAYCCNIVNVSLVKPSFYVYSRVK | 26 | |
| CAYCCNIVNVSLVKPSFYVYSRVKN | 2 | |
| RLCAYCCNIVNVSLVKPSFYVYSRVK | 4 | |
| YCCNIVNVSLVKPSFYVYSRVKN | 1 |
By using Uniprot to find the Ref protein name of the fungi peroxidase sequence, we got three groups of protein names: R7T0H4->XP_007365204.1; R7SP50->XP_007370520.1; R7SH99-> XP_007272084.1. The E protein corresponding to R7SH99 was “YCCNIVNVSLVKPSFYVYSRVKN”, which contained the haem linked site "YCC". In the NCBI webpage, there was no “Related Structures (Summary)” content for these three proteins. After clicking “Conserved Domains (Concise)” in the NCBI webpage of these three proteins, the introduction of “cd00692: Ligninase; Ligninase and other manganese-dependent fungal peroxidase” was displayed, suggesting that the fungal PEROXIDASE_4 type domain was lignin peroxidase. Taken together, the above analysis results showed that the E protein had the catalytic role of the peroxidase enzyme after binding to haem. E protein catalysed the formation of hydrogen peroxide, even ·OH.
3.4. The haem linked sites were located on the outer surface of the viral membrane structure
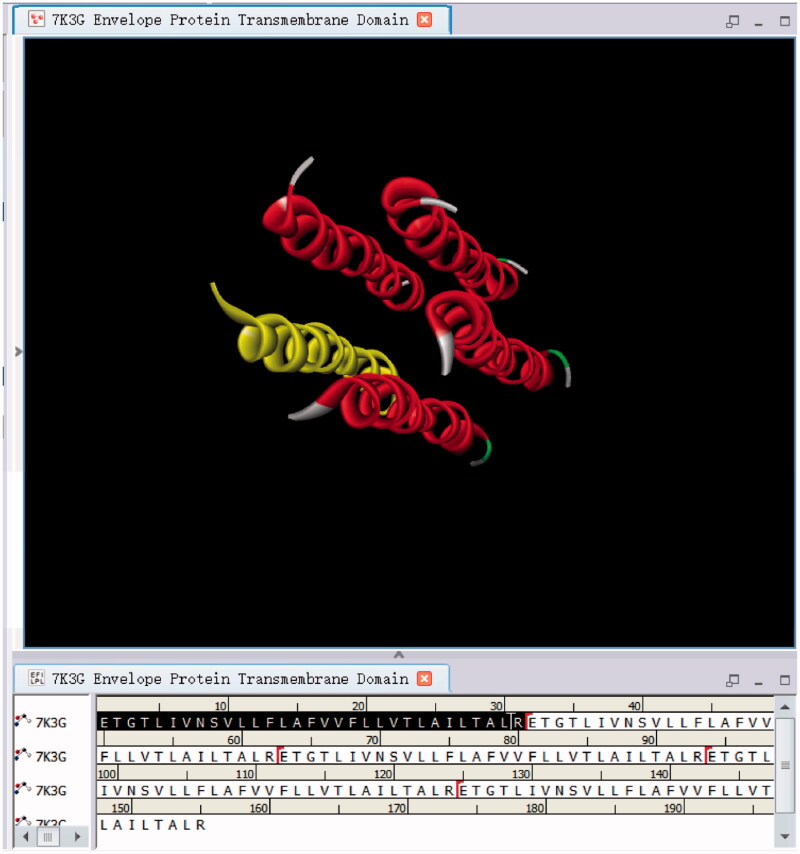
The haem theory revealed the haem linked site “CAYCC” of E protein. We further investigated whether the sites was outside the viral membrane. We downloaded the transmembrane domain (7K3G) of SARS-COV-2 E protein from the PDB database. As shown in Figure 1, the transmembrane structure sequence is at the N-terminus of E protein: “ETGTLIVNSVLLFLAFVVFLLVTLAILTALR”, at positions 8–38. The haem linked site “CAYCC” is near the outer side of the viral membrane structure, at 40–44. The transmembrane structure of E proteins makes up a 5-mer ion channel. The enzyme catalytic properties of E protein are probably associated with the ion channels.
Figure 1.
Transmembrane structure of E protein.
3.5. The spear (ROS attack) and shield (ROS escape) of virus
The viral membrane structural proteins include surface glycoproteins (Spike protein), E protein and M protein. The haem theory found that E protein had haem linked sites and Cytochrome c oxidase activity. And the surface glycoprotein could bind to haem with poor stability and M protein did not bind to haem. Surface glycoprotein may assist E protein in capturing haem. The present study still supported that E protein had the haem-iron linked site. When E protein was attached to iron, it had Fe-SOD enzyme activity. When E protein was linked to haem, it had cytochrome c oxidase, catalase and peroxidase activity. E protein catalysed superoxide anion and hydrogen peroxide into oxygen and water through Cytochrome c oxidase activity. E protein also catalysed hydroxyl radicals from hydrogen peroxide through peroxidase activity. Moreover, it catalysed the hydrogen peroxide and oxygen from superoxide anion through Fe-SOD enzyme activity. E Protein catalysed water and oxygen from hydrogen peroxide through catalase activity.
E protein-joined to iron and E protein-bound haem collaborated to catalyse the decomposition of superoxide anion and hydrogen peroxide into water and oxygen. The virus can escape the immune system from attacking the virus by decomposing superoxide anions and hydrogen peroxide through the E protein. It was called the virus’s shield–-”ROS escape”. After E protein was associated with haem, E protein could catalyse superoxide anions, hydrogen peroxide, and hydroxyl radicals to oxygen and water. The virus attacked neighbouring tissues by the superoxide anion, hydrogen peroxide and hydroxyl free radicals. It was named the spear of the virus –-”ROS attack”. Hydroxyl free radical was the primary tool for viruses to invade tissues for its more significant damage on lipids, proteins and nucleic acids. Then, the E protein binding to haem damaged the immune system.
4. Discussion
4.1. Iron and haem required for the E-catalysis came from haemoglobin or phagocytes
The iron required for catalysing the E protein probably came from two major pathways. One was the iron or haem dissociated by the viral proteins attacking haemoglobin. The second was iron or haem engulfed by the macrophages. With the haem theory, ORF3 and other viral proteins attacked haemoglobin, dissociating haem into iron and porphyrin. This attack produced substantial amounts of dissociated iron and haem. SARS-COV-2 virus in the blood was capable of capturing these released iron and haem to achieve “ROS escape” or “ROS attack”. There were also many iron or haem particles in phagocytes. Upon elevated systemic iron levels or inflammation, the elevated hepcidin acted on the channel for macrophage iron transport, resulting in iron retention in the macrophages. The autopsy reports also demonstrated the presence of numerous hemophagocytic behaviours for phagocytes. Thus, this phagocytosis would even swallow many iron or haem particles.
4.2. Iron on the balance between viral infection and “ROS attack”
The haem theory discovered the presence of haem iron-binding sites in N protein as well, and viral replication might commence with iron catalysis. When the virus replicated in large numbers, the demand for iron increased, and the attack on erythrocytes also intensified. Upon saturation of viral iron uptake, the attack on haemoglobin weakened. There was a probable trade-off relationship between viral infection and ROS attacks. When the iron intake was excessive, the virus impaired the cells with ACE and CD147 receptors through a ROS attack. Otherwise, the virus infected these cells to induce viral replication. Research evidence suggested that the erythrocyte membranes of patients were harmed by denaturation, injuring structural proteins [82]. When the virus got less iron, it might infect erythrocytes through the CD147 receptor. Otherwise, the virus might impair the erythrocyte membranes through ROS, inducing withering of erythrocytes. Phagocytes would strengthen the phagocytosis for erythrocytes with impaired functions. This might also explain why some patients did not show excessive iron levels in the erythrocytes.
4.3. The virus colonised phagocytes and caused asymptomatic infection
Asymptomatic infection was associated with mononuclear phagocytes, the viral haven. When phagocytes engulfed pathogens, they produced numerous superoxide anions via the respiratory outbreak mechanism, which killed the aerobic bacteria. The E proteins had activities through the iron catalytic process. They converted superoxide anions into H2O2, and then decomposed it into water and oxygen for preventing viral oxidation, so that the virus could live in the vesicles.
The E protein got peroxidase activity through the iron catalytic system contributing to ·OH. When the ·OH concentration approached a certain threshold, the lysosomal membranes ruptured. Then, hydrolase was released into the cytoplasm, which led to autophagic death of phagocytes, releasing virus, iron or haem particles. When the ·OH accumulation was low, SARS-CoV-2 could inhibit the activity of hydrolytic enzymes near itself. The lysosome neither digested the virus nor ruptured, achieving parasitism of the virus.
Therefore, mononuclear phagocytes scattered in the body might be the central sheltering place for viruses. There was an interesting coincidence of time here. The life cycle of macrophages was longer than several weeks, which might be longer in some people due to physical disparities. The macrophage life cycle was consistent with the quarantine duration. The time for quarantine measures was based on the statistical data. A 14-day quarantine measure was performed on people who have been in contact with COVID-19 patients, which could confirm infected people positively by nucleic acid test before the end of quarantine. If travellers returned from an epidemic area abroad, they would be quarantined for 14 days in the city of arrival. Then, they would also be sequestered for 14 days after returning to their town of residence. Some people with recessive infections had a negative nucleic acid test in the first phase of quarantine measure. The nucleic acid test would be positive during the second phase of quarantine measure. There was also a minimal number of negative cases in both quarantine phases, which only transformed into positive after the two quarantine phases.
4.4. Oxidative stress damage of memory B cells caused reinfection
B lymphocytes differentiates into long-lived antibody-forming cells and memory B cells that produce antibodies [83]. Differentiation process of B cells is divided into five stages: pre-B cells, immature B cells, mature B cells, activated B cells and plasma cells. The differentiation of pre-B cells and immature B cells is an antigen-independent process that takes place in the bone marrow. Meanwhile, during the antigen-dependent stage, mature B cells are stimulated by antigens and continuously differentiate into plasma cells that synthesise and secrete antibodies. The differentiation at this stage is mainly carried out in the peripheral immune organs. The differentiation of most memory B cells depends on the germinal centres of lymph nodes. Abnormal regulation of spontaneous centres (Spt-GCs) is thought to promote mutations of antibody secreting cells and autoimmune diseases [84]. Although it has been reported that the SARS-COV-2 virus has been found in lymph nodes, the existing evidence still does not strongly support the virus infecting lymphocytes, especially B cells.
In the early stages of onset, the frequencies of CD27+ and CD38+ plasma cells in COVID-19 patients were lower than that in surviving patients [85]. Among memory B cells including CD27+, CD27- and Ag-specific cells [86], the CD27+ memory B cells played a significant role in secondary immunity [87]. CD27 is a vital surface antigen marker for memory B cells, a kind of leucocytes expressing various membrane immunoglobulins (mIg), which are antigen receptors (BCR). CD27+ expresses mIgG and mIgM, while CD27 expresses mIgG. The mIg can recognise antigens, receive the first signal of antigen stimulation, stimulate B cells to differentiate into plasma cells through a cascade reaction, and secrete antibodies again. Therefore, losing IgM antibodies in reinfections was linked to the abnormal loss of CD27+ memory B cells. When these cells were exposed to the viral surface in the direction of mIgM, they were easily damaged and died due to the "ROS attack".
4.5. "Happy hypoxia" was a symptom that attacked haemoglobin and impaired immune cell
Former patients experienced a weird stage called “happy hypoxia”. At this stage, the patients’ blood oxygen saturation was only 70%. Although, in theory, such patients should have difficulty in breathing and movement, they could move, talk and laugh. Nevertheless, their condition deteriorated.
During erythrocyte oxygen transport to the capillaries, the oxygen molecules fell off from the haemoglobin, which then passed through the erythrocyte membranes via osmosis and entered the capillaries. Eventually, they joined the nearby tissue cells from the capillaries via osmosis. Blood oxygen saturation referred to the ratio of oxygenated haemoglobin to all haemoglobin. According to the haem theory, proteins such as ORF3 attacked haemoglobin, which reduced the amount of oxygenated haemoglobin and decreased the patients’ blood oxygen saturation.
If the level of oxygenated haemoglobin decreased, the tissue cells should appear hypoxic. Therefore, the patients should not be “happy”. Since the hypoxia of cells caused shock, it should not be a type of neural paralysis. The haem theory speculated that the attacked haemoglobin released oxygen molecules into the blood. This was an important factor for the "happiness" phenomenon, and another reason might be associated with the immune response.
After activation, phagocytes released substantial H2O2 outside of the cells for pathogen killing. The SARS-COV-2 virus catalysed the decomposition of these H2O2 to yield oxygen. When this catalysis occurred in the blood, the blood level of dissolved oxygen was quite high. And when it occurred nearby the cells, the oxygen entered the tissue cells through osmosis. This concealed the problem of cellular hypoxia induced by the decreased amount of oxygenated haemoglobin. The virus also expanded infection in a patients’ “happy” state.
Specific T, B and NK cells were impaired by the virus’s “ROS attack”, an oxygen-consuming process, when exposed to the viral surface. The virus could steal the oxygen molecules inside or outside the erythrocytes to produce ·OH. However, after haemoglobin attack by viral proteins, the level of oxygenated haemoglobin was lowered, and few exogenous oxygen molecules were present. Accordingly, the virus could decompose H2O2 released by phagocytes to produce ·OH, which impaired the membrane structures of T, B and NK cells, leading to damage or death of these cells. This exacerbated inflammation and made immune cells secrete more cytokines.
5. Conclusion
The novel coronavirus pneumonia is a deadly disease, and the current global pandemic is inseparable from its high contagion. Understanding its critical damage mechanism to the immune system is of great significance to containing the epidemic, curing the disease and saving lives. In our previous study on haem theory, we speculated that the E protein of the SARS-COV-2 virus had an essential association with the disease’s infectiousness. This study used domain search techniques to analyse the E protein of the SARS-CoV-2 virus.
The results showed that the E protein of the SARS-COV-2 virus had the conserved domains of cytochrome c oxidase, Fe-SOD enzyme, catalase and peroxidase. The haem-binding sites were on the outer surface of the viral membrane structure. When E protein bound to iron, it had a Fe-SOD enzyme activity. When bound to haem, it exhibited cytochrome c oxidase (found in haem theory), catalase and peroxidase activities. After haem binding of E protein, oxygen and water were set as a starting point to synthesise superoxide anion, hydrogen peroxide and hydroxyl radicals. This phenomenon was called “ROS attack” of the virus. When an iron-bound E protein cooperated with a haem-bound E protein, they converted superoxide anion and hydrogen peroxide into oxygen and water. This phenomenon was called “ROS escape” of the virus. “ROS attacks” damaged the tissues or cells exposed on the viral surface, while “ROS escape” dissolved the superoxide anion and hydrogen peroxide that attacked the virus.
The iron and haem bound by E protein came from attacked haemoglobin and phagocytes. Viral proteins attacked haemoglobin and dissociated them to release substantial amounts of iron and haem. E protein of the virus could bind these iron and haem. The attack on haemoglobin also enhanced the hemophagocytic behaviour of phagocytes. The phagocytes also swallowed iron, haem and erythrocytes. After entering phagocytes, the virus directly got iron and haem from vesicles or lysosomes, which, following rupture of phagocytes, captured the overflowing iron and haem as well.
Lymphopenia was associated with “ROS attack”. After exposure to infected cells, the NK cells were attacked by the virus that had not shed from the infected cells’ surfaces through ROS, consequently being damaged or died due to the attack on their membrane structure. Because of the difference in the shedding position, the destruction efficiency of the virus may not be high. When lymphocytes like T and B cells neared the viral surface antigens, they were also injured or died by the virus’s ROS attack. Noteworthy is that the E protein also has a Catalase-rel domain related to T cell immunity, which overlaps with the haem binding site, although its specific function is unknown. Memory B cells were also damaged or decomposed by the virus’s ROS attack upon exposure to the viral surface antigens. Thus, the abnormal deficiency of memory B cells was an essential factor for reinfection of patients.
Exploiting the “ROS escape” method, the virus decomposed the phagocyte-released H2O2 into oxygen and water, thereby avoiding external killing. In this process, the surrounding cells were unexpectedly supplemented by oxygen molecules, which put the patients into a "happy hypoxic" state. During phagocytosis of the virus, the E protein converted superoxide anions into oxygen. Then, it transferred hydrogen peroxide, the intermediate product, into oxygen and water. In this way, the virus was parasitised in the vesicles of phagocytes. After vesicle fusion with lysosomes, the E protein produced ROS, and the hydrolase near the virus was damaged by oxidative stress, losing its activity. The virus was parasitised in the lysosomes of phagocytes in this way. The hydroxyl radicals damaged the lysosomal membranes when exceeding a specific number. Lysosome ruptured to release hydrolase, and phagocytes died by autophagy. After phagocytosis of cell fragments and viral particles by the surrounding phagocytes, death similar to autophagy occurred again. This vicious circle caused inflammation and fibrosis of surrounding tissues or cells. Thus, the virus parasitising vesicles or lysosomes of phagocytes was linked to the asymptomatic infection or retest positivity.
In brief, the studied virus exploited "ROS attack" to damage multiple organs and tissues in the body, such as immune (e.g. bone marrow, spleen) and neural (e.g. spinal cord, brain) organs. The attack provoked a strong cytokine storm and caused organ failure and complications.
Acknowledgements
Thanks readers for free review and suggestions.
Funding Statement
This work was funded by a grant from the National Natural Science Foundation for the Talent Introduction Project of Sichuan University of Science and Engineering [award number: 2018RCL20, grant recipient: WZL].
Disclosure statement
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Author contributions
Funding was obtained by WZL. Besides, design, analysis and writing are finished by WZL, while data curation and manuscript check are undertaken by HLL. Both authors have read and agreed to the published version of the manuscript.
Data availability statement
The datasets and results supporting the conclusions of this article are available at https://pan.baidu.com/s/1YBe6TXLTCcN9AH9ZMbznkQ, code: ordn.
References
- 1.Long Q-X, Tang X-J, Shi Q-L, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26(8):1200–1204. [DOI] [PubMed] [Google Scholar]
- 2.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun S, Cai X, Wang H, et al. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou, China. Clin Chim Acta. 2020;507:174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020;71(15):762–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi Y, Wang Y, Shao C, et al. 2020. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yazdanpanah F, Hamblin MR, Rezaei N.. The immune system and COVID-19: friend or foe? Life Sci. 2020;256:117900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casadevall A, Pirofski L-A.. In fatal COVID-19, the immune response can control the virus but kill the patient. Proc Natl Acad Sci 2020;117:30009–30011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi F-D, Zhou Q.. Natural killer cells as indispensable players and therapeutic targets in autoimmunity. Autoimmunity. 2011;44(1):3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw AC, Goldstein DR, Montgomery RR.. Age-dependent dysregulation of innate immunity. Nat Rev Immunol. 2013;13(12):875–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pascolini S, Vannini A, Deleonardi G, et al. COVID‐19 and immunological dysregulation: can autoantibodies be useful? Clin Transl Sci. 2021;14(2):502–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou Y, Han T, Chen J, et al. Clinical and autoimmune characteristics of severe and critical cases of COVID-19. Clin Transl Sci. 2020;13(6):1077–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birra D, Benucci M, Landolfi L, et al. COVID 19: a clue from innate immunity. Immunol Res. 2020;68(3):161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu Z, Song C, Xu C, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63(5):706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao W, Li L.. Advances on presymptomatic or asymptomatic carrier transmission of COVID-19. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(4):485–488. [DOI] [PubMed] [Google Scholar]
- 15.Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020;94:154–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance. 2020;25(10):2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vermund SH, Pitzer VE.. Asymptomatic transmission and the infection fatality risk for COVID-19: implications for school reopening. Clinical Infectious Diseases. 2020;, ciaa855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Tawfiq JA. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19). Travel Med Infect Dis. 2020;35:101608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu X, Yang R.. COVID‐19 transmission through asymptomatic carriers is a challenge to containment. Influenza Other Respi Viruses. 2020;14(4):474–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Treibel TA, Manisty C, Burton M, et al. COVID-19: PCR screening of asymptomatic health-care workers at London hospital. The Lancet. 2020;395(10237):1608–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu Z, Ci C.. Screening and management of asymptomatic infection of corona virus disease 2019 (COVID-19). Zhonghua yu Fang yi Xue za Zhi [Chinese Journal of Preventive Medicine. 2020;54:E025–E025. [DOI] [PubMed] [Google Scholar]
- 22.Lei Q, Li Y, Hou H. y, et al. Antibody dynamics to SARS-CoV-2 in asymptomatic COVID-19 infections . Allergy. 2021;76(2):551–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Le Bert N, Clapham HE, Tan AT, et al. Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection. J Exp Med. 2021;218(5):e20202617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yuan B, Liu H-Q, Yang Z-R, et al. Recurrence of positive SARS-CoV-2 viral RNA in recovered COVID-19 patients during medical isolation observation. Scientific reports. 2020;10:11887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duggan NM, Ludy SM, Shannon BC, et al. A case report of possible novel coronavirus 2019 reinfection. Am J Emerg Med. 2021;39:256.e1–256.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snyder, T. M., Gittelman R. M., Klinger M., May D. H., Osborne E. J., Taniguchi R., Zahid H. J., Kaplan I. M., Dines J. N., and Noakes M. T.. 2020. Magnitude and dynamics of the T-cell response to SARS-CoV-2 infection at both individual and population levels. medRxiv. [Google Scholar]
- 27.Grifoni A, Weiskopf D, Ramirez SI, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181(7):1489–1501.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dong, T., Peng Y., Mentzer A. J., Liu G., Yao X., Yin Z., Dong D., Dejnirattisai W., Turtle L., and Rostron T.. 2020. Broad and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK convalescent COVID-19 patients. bioRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.To KK-W, Hung IF-N, Ip JD, et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clin Infect Dis. 2020;ciaa1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.To KK-W, Hung IF-N, Chan K-H, et al. Serum antibody profile of a patient with COVID-19 reinfection. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iba T, Levy JH, Levi M, et al. Coagulopathy in COVID-19. J Thromb Haemost. 2020;18(9):2103–2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bradley BT, Maioli H, Johnston R, et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. The Lancet. 2020;396(10247):320–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yao X, Li T, He Z, et al. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing li Xue za Zhi. 2020;49:E009–E009. [DOI] [PubMed] [Google Scholar]
- 34.Youd E, and, Moore L.. COVID-19 autopsy in people who died in community settings: the first series. J Clin Pathol. 2020;73(12):840–844. [DOI] [PubMed] [Google Scholar]
- 35.Tian S, Xiong Y, Liu H, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rapkiewicz AV, Mai X, Carsons SE, et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. EClin Med. 2020;24:100434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sami R, Fathi F, Eskandari N, et al. Characterizing the immune responses of those who survived or succumbed to COVID-19: can immunological signatures predict outcome? Cytokine. 2021;140:155439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fathi F, Sami R, Mozafarpoor S, et al. Immune system changes during COVID-19 recovery play key role in determining disease severity. Int J Immunopathol Pharmacol. 2020;34:205873842096649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shi N, Ma Y, Fan Y, et al. Predictive value of the neutrophil-to-lymphocyte ratio (NLR) for diagnosis and worse clinical course of the COVID-19: findings from ten provinces in China. 2020. [Google Scholar]
- 41.Mathew D, Giles JR, Baxter AE, et al. ; The UPenn COVID Processing Unit† . Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science. 2020;369(6508):eabc8511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Laing, A. G., Lorenc A., Del Barrio I. D. M., Das A., Fish M., Monin L., Munoz-Ruiz M., Mckenzie D., Hayday T., and Quijorna I. F.. A consensus Covid-19 immune signature combines immuno-protection with discrete sepsis-like traits associated with poor prognosis. medRxiv. 2020.06.08.20125112. [Google Scholar]
- 43.Wang C, Xie J, Zhao L, et al. Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients. EBioMedicine. 2020;57:102833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jacobs W, Lammens M, Kerckhofs A, et al. Fatal lymphocytic cardiac damage in coronavirus disease 2019 (COVID‐19): autopsy reveals a ferroptosis signature. ESC Heart Failure. 2020;7(6):3772–3781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Basso C, Leone O, Rizzo S, et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J. 2020;41(39):3827–3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pagliaro P. Is macrophages heterogeneity important in determining COVID-19 lethality? Med Hypotheses. 2020;143:110073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yuan D, Thet S, Zhou XJ, et al. The role of NK cells in the development of autoantibodies. Autoimmunity. 2011;44(8):641–651. [DOI] [PubMed] [Google Scholar]
- 48.Baxter AG, Smyth MJ.. The role of NK cells in autoimmune disease. Autoimmunity. 2002;35(1):1–14. [DOI] [PubMed] [Google Scholar]
- 49.Itoh Y, Igarashi T, Tatsuma N, et al. Immunogenetic background of patients with autoimmune fatigue syndrome. Autoimmunity. 2000;32(3):193–197. [DOI] [PubMed] [Google Scholar]
- 50.Sanmarco M, Bernard D.. Studies of IgG-class anticardiolipin antibodies in myasthenia gravis. Autoimmunity. 1994;18(1):57–63. [DOI] [PubMed] [Google Scholar]
- 51.Madera S, Rapp M, Firth MA, et al. Type I IFN promotes NK cell expansion during viral infection by protecting NK cells against fratricide. J Exp Med. 2016;213(2):225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blanco-Melo D, Nilsson-Payant BE, Liu W-C, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181(5):1036–1045. e1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yahata T, Takanashi T, Muguruma Y, et al. Accumulation of oxidative DNA damage restricts the self-renewal capacity of human hematopoietic stem cells. Blood. 2011;118:2941–2950. [DOI] [PubMed] [Google Scholar]
- 54.Yahata T, Muguruma Y, Yumino S, et al. Quiescent human hematopoietic stem cells in the bone marrow niches organize the hierarchical structure of hematopoiesis. Stem Cells. 2008;26(12):3228–3236. [DOI] [PubMed] [Google Scholar]
- 55.Naka K, Muraguchi T, Hoshii T, et al. Regulation of reactive oxygen species and genomic stability in hematopoietic stem cells. Antioxid Redox Signal. 2008;10(11):1883–1894. [DOI] [PubMed] [Google Scholar]
- 56.Shirai T, Hilhorst M, Harrison DG, et al. Macrophages in vascular inflammation-from atherosclerosis to vasculitis. Autoimmunity. 2015;48(3):139–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jafarzadeh A, Chauhan P, Saha B, et al. Contribution of monocytes and macrophages to the local tissue inflammation and cytokine storm in COVID-19: lessons from SARS and MERS, and potential therapeutic interventions. Life Sci. 2020;257:118102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fox SE, Akmatbekov A, Harbert JL, et al. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xu X, Chang X, Pan H, et al. Pathological changes of the spleen in ten patients with coronavirus disease 2019(COVID-19) by postmortem needle autopsy. Zhonghua Bing Li Xue Za Zhi. 2020;49(6):576–582. [DOI] [PubMed] [Google Scholar]
- 60.Park MD. 2020. Macrophages: a Trojan horse in COVID-19? Nat. Rev. Immunol. 2020;20:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhou J, Chu H, Li C, et al. Active replication of Middle East respiratory syndrome coronavirus and aberrant induction of inflammatory cytokines and chemokines in human macrophages: implications for pathogenesis. J Infect Dis. 2014;209(9):1331–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pieters J. Mycobacterium tuberculosis and the macrophage: maintaining a balance. Cell Host Microbe. 2008;3(6):399–407. [DOI] [PubMed] [Google Scholar]
- 63.Celli J. Surviving inside a macrophage: the many ways of Brucella. Res Microbiol. 2006;157(2):93–98. [DOI] [PubMed] [Google Scholar]
- 64.Handman E, Bullen DV.. Interaction of Leishmania with the host macrophage. Trends Parasitol. 2002;18(8):332–334. [DOI] [PubMed] [Google Scholar]
- 65.Gendelrnan HE, Orenstein JM, Baca LM, et al. The macrophage in the persistence and pathogenesis of HIV infection. Aids. 1989;3:475–496. [DOI] [PubMed] [Google Scholar]
- 66.Pollard KM. Silica, silicosis, and autoimmunity. Front Immunol. 2016;7:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Maejima I, Takahashi A, Omori H, et al. Autophagy sequesters damaged lysosomes to control lysosomal biogenesis and kidney injury. Embo J. 2013;32(17):2336–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wong KW, Jacobs WR. Jr.. Critical role for NLRP3 in necrotic death triggered by Mycobacterium tuberculosis. Cell Microbiol. 2011;13(9):1371–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goren M. Phagocyte lysosomes: interactions with infectious agents, phagosomes, and experimental perturbations in function. Annu Rev Microbiol. 1977;31:507–533. [DOI] [PubMed] [Google Scholar]
- 70.Alshebri MS, Alshouimi RA, Alhumidi HA, et al. Neurological complications of SARS-CoV, MERS-CoV, and COVID-19. SN Compr Clin Med. 2020;2:2037–2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Amezcua JMG, Jain R, Kleinman G, et al. COVID-19-induced neurovascular injury: a case series with emphasis on pathophysiological mechanisms. SN Compr Clin Med. 2020;2:2109–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ye M, Ren Y, and, Lv T.. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun. 2020;88:945–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang, T., Rodricks M. B., and Hirsh E.. 2020. COVID-19-associated acute disseminated encephalomyelitis: a case report. MedRxiv. [Google Scholar]
- 74.Schönegger CM, Gietl S, Heinzle B, et al. Smell and taste disorders in COVID-19 patients: objective testing and magnetic resonance imaging in five cases. SN Compr Clin Med. 2020;2:2535–2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS-coronavirus-2. Int J Infect Dis. 2020;94:55–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu W, Li H.. 2020. COVID-19: attacks the 1-beta chain of hemoglobin and captures the porphyrin to inhibit human heme metabolism. ChemRxiv. chemrxiv.11938173.v9. [Google Scholar]
- 77.Fong K-L, McCay PB, Poyer JL, et al. Evidence that peroxidation of lysosomal membranes is initiated by hydroxyl free radicals produced during flavin enzyme activity. J Biol Chem. 1973;248(22):7792–7797. [PubMed] [Google Scholar]
- 78.Bai J, Cederbaum AI.. Mitochondrial catalase and oxidative injury. Biol Signals Recept. 2001;10(3-4):189–199. [DOI] [PubMed] [Google Scholar]
- 79.Guy B, Krell T, Sanchez V, et al. Do Th1 or Th2 sequence motifs exist in proteins? Identification of amphipatic immunomodulatory domains in Helicobacter pylori catalase. Immunol Lett. 2005;96(2):261–275. [DOI] [PubMed] [Google Scholar]
- 80.Horvath MM, Grishin NV.. The C‐terminal domain of HPII catalase is a member of the type I glutamine amidotransferase superfamily. Proteins. 2001;42(2):230–236. [PubMed] [Google Scholar]
- 81.Chen SX, Schopfer P.. Hydroxyl-radical production in physiological reactions. A novel function of peroxidase. Eur J Biochem. 1999;260(3):726–735. [DOI] [PubMed] [Google Scholar]
- 82.Thomas T, Stefanoni D, Dzieciatkowska M, et al. 2020. Evidence for structural protein damage and membrane lipid remodeling in red blood cells from COVID-19 patients. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zouali M. "B cells and autoimmunity 2016". Autoimmunity. 2017;50(1):1–3. [DOI] [PubMed] [Google Scholar]
- 84.Domeier PP, Schell SL, Rahman ZSM.. Spontaneous germinal centers and autoimmunity. Autoimmunity. 2017;50(1):4–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang F, Hou H, Yao Y, et al. Systemically comparing host immunity between survived and deceased COVID-19 patients. Cell Mol Immunol. 2020;17(8):875–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Agematsu K, Nagumo H, Yang FC, et al. B cell subpopulations separated by CD27 and crucial collaboration of CD27+ B cells and helper T cells in immunoglobulin production. Eur J Immunol. 1997;27(8):2073–2079. [DOI] [PubMed] [Google Scholar]
- 87.Seifert M, and, Küppers R.. Molecular footprints of a germinal center derivation of human IgM+(IgD+)CD27+ B cells and the dynamics of memory B cell generation . J Exp Med. 2009;206(12):2659–2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets and results supporting the conclusions of this article are available at https://pan.baidu.com/s/1YBe6TXLTCcN9AH9ZMbznkQ, code: ordn.