Abstract
Objectives
The objective of this study was to investigate the influence of the COVID-19 pandemic on physical activity (PA) and the incidence of frailty among initially non-frail older adults in Japan.
Design
A follow-up online survey.
Setting and Subjects
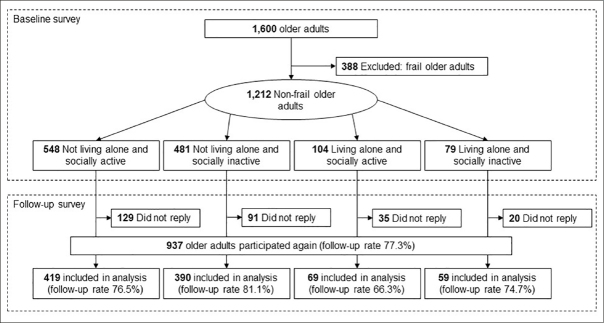
Among the 1,600 baseline online survey participants, 388 adults were already frail, and 275 older adults did not respond to the follow-up survey. Thus, the final number of participants in this study was 937 (follow-up rate: 77.3%).
Methods
We assessed the total PA time at four time points according to the COVID-19 waves in Japan: January 2020 (before the pandemic), April 2020 (during the first wave), August 2020 (during the second wave), and January 2021 (during the third wave). We then investigated the incidence of frailty during a one-year follow-up period (during the pandemic).
Results
The total PA time during the first, second, and third waves of the pandemic decreased from the pre-pandemic PA time by 33.3%, 28.3%, and 40.0%, respectively. In particular, the total PA time of older adults who were living alone and socially inactive decreased significantly: 42.9% (first wave), 50.0% (second wave), and 61.9% (third wave) less than before the pandemic, respectively. Additionally, they were at a significantly higher risk of incident frailty than those who were not living alone and were socially active (adjusted odds ratio: 2.04 [95% confidence interval: 1.01–4.10]).
Conclusion
Our findings suggest that older adults who live alone and are socially inactive are more likely to experience incident frailty/disability due to decreased PA during the pandemic. Understanding this mechanism may be crucial for maintaining the health status of older adults.
Key words: COVID-19, physical activity, frailty, living alone, social inactivity
Introduction
Coronavirus 2019 (COVID-19) has not only impacted high mortality rates but also physical activity (PA) worldwide. Many researchers, including ours, have reported PA statuses that were consistently and significantly less during the first wave of the COVID-19 pandemic than before it (1–5). This tendency may lead to increased incidences of frailty, disability, or mortality in the near future. Many academic societies have proposed recommendations or positions to maintain physical activity and decrease sedentary time during the pandemic (6–8).
Our previous surveys found that the total amount of time devoted to PA among older adults in April 2020 (during the first wave of the COVID-19 pandemic) had significantly decreased compared to that recorded in January 2020 (before the COVID-19 pandemic) (1), and the recovery in PA time was realized after the first wave of the pandemic in Japan (9). This potential, which runs counter to the stay-at-home message, is critical for maintaining health conditions and preventing adverse health outcomes. However, even after the first wave of the pandemic, the total PA time for some older adults did not recover sufficiently. Older adults who live alone and are socially inactive are not resilient (9), and they may be at high risk of incident frailty or disability in the near future. Living alone and being socially inactive are representative factors of social restriction in older adults (10–16).
After the first wave, COVID-19 continued to spread, leading to the second and third waves. The influence of the second and third waves on PA and the new rate of frailty are not well understood yet. Therefore, the objective of this study was to investigate the influence of the pandemic on PA and the new incidence of frailty among initially non-frail older adults in Japan. We hypothesized that the total PA time during the second and third waves of the pandemic is relatively shorter than that before the pandemic but higher than that in the first wave, with a higher incidence of frailty due to the decreased PA during the pandemic.
Methods
Participants
From April 23 to 27, 2020, an online baseline survey was completed by 1,600 community-dwelling older adults in Japan (1), and a follow-up online survey was conducted from January 15 to 25, 2021. The baseline survey included adults between the ages of 65 and 84 years and residents of Tokyo, Kanagawa, Chiba, Saitama, Aichi, Osaka, Hyogo, and Fukuoka prefectures, which are urban areas. Incidentally, the first state of emergency was declared on April 7, 2020 and lifted on May 25, 2020, whereas the second state of emergency was declared on January 7, 2021 in these prefectures. This analysis excluded adults who were frail at the baseline survey and did not respond to the follow-up survey. Among the 1,600 baseline survey participants, 388 adults were already frail, as defined by the Kihon checklist (17), and 275 older adults did not respond to the follow-up survey. Thus, the final number of participants in this study was 937 (follow-up rate: 77.3%) (Figure 1). This study was conducted in accordance with the guidelines proposed by the Declaration of Helsinki, and the study protocol was reviewed and approved by the Ethics Committee of the Faculty of Human Sciences, University of Tsukuba.
Figure 1.
Flow chart showing the distribution of participants throughout the survey
PA measurement
We assessed PA using a questionnaire based on a short version of the International Physical Activity Questionnaire [18]. We multiplied the activity frequency per week and activity time per day (minutes) at each activity level and determined the total PA time (minutes) as added values for each level. A detailed description of the PA at the baseline survey has been provided previously (1). We investigated PA at four time points according to the waves of the COVID-19 pandemic in Japan: January 2020, April 2020, August 2020, and January 2021. In the baseline survey (April 2020), the participants were required to provide two types of answers: recalled answers before the COVID-19 pandemic (January 2020) and non-recalled answers during the first wave of the COVID-19 pandemic (April 2020) (1). Similarly, in the follow-up survey (January 2021), the participants were required to provide two types of answers: recalled answers during the second wave of the COVID-19 pandemic (August 2020) and non-recalled answers during the third wave of the COVID-19 pandemic (January 2021).
Definition of frailty
We defined frailty using the Kihon checklist (19), which consists of 25 items divided into seven domains: lifestyle, motor abilities, nutrition, oral function, seclusion, forgetfulness, and mood. We defined scores of 8 or more as frailty, 4 to 7 as pre-frailty, and 0 to 3 as robust, according to a previous study (17). We assessed the participants’ frailty status using the Kihon checklist at two points: recalled answers before the COVID-19 pandemic (January 2020) and non-recalled answers during the third wave of the COVID-19 pandemic (January 2021) in the baseline and follow-up surveys, respectively.
Social factors
In the baseline survey, we investigated the participants’ family structure (living alone or not living alone) and social activity (socially active or socially inactive) (9), which are key elements of social frailty (10–16). The question about family structure was, “Do you live alone?” Participants were asked to choose between yes (a) or no (b), with (a) signifying “living alone.” The question about social activity was, “How do you get along with your neighbors?” The choices included (a) I have a neighbor who comes and goes to each house, (b) I have a neighbor to chat with on the street, (c) I have a neighbor to say hello to, and (d) I do not communicate with neighbors. “Socially inactive” was defined as answering with (c) or (d). The participants were categorized into four groups based on their combination of family structure and social activity: (1) not living alone and socially active, (2) not living alone and socially inactive, (3) living alone and socially active, and (4) living alone and socially inactive (14).
Demographic data
In the baseline survey, we assessed several types of demographic data: age, sex, height, weight, number of medications, morbidity, and health literacy. We calculated body mass index (BMI) from height and weight and defined underweight as less than 18.5 (20). We defined the use of five or more medications as polypharmacy according to a previous systematic review (21). We investigated the comorbidity condition based on the following diseases: hypertension, hyperlipidemia, diabetes, cancer, cardiovascular disease, kidney disease, and orthopedic disease. We assessed the level of health literacy using the Critical Health Literacy Scale and defined a score of less than 4 points as lower health literacy (22).
Statistical analysis
We examined the influence of the COVID-19 pandemic on the total PA time in both the main and subgroup analyses. The Friedman test and the Wilcoxon test with Bonferroni adjustment were used to assess the differences in the time devoted to PA at four time points corresponding to the COVID-19 pandemic waves in Japan. Subgroup analysis according to the four groups was based on the combination of family structure and social activity. Logistic regression models were used to estimate the odds ratio (OR) and 95% confidence interval (CI) of the relationships between the four groups and the new incidence of frailty in univariate and multivariate analyses. Multivariate analyses were adjusted for age, sex, underweight, polypharmacy, hypertension, hyperlipidemia, diabetes, cancer, cardiovascular disease, kidney disease, orthopedic disease, lower health literacy, total PA time, and the total Kihon checklist score in January 2020. The data were analyzed using the Statistical Package for the Social Sciences (SPSS, Windows version 26.0; SPSS, Inc., Chicago, IL, USA). A p-value less than 0.05 was considered to indicate statistical significance for all analyses.
Results
The demographic variables are listed in Table 1. The mean age, proportion of women, mean BMI, and proportion of pre-frailty at baseline were 73.5±5.5 years, 48.9% (n=458), 22.4±2.8, and 51.7% (n=484), respectively. According to the combination of family structure and social activity, 419 participants did not live alone and were socially active, 390 participants did not live alone and were socially inactive, 69 participants lived alone and were socially active, and 59 participants lived alone and were socially inactive. Overall, 150 participants (16.0%) had a new incidence of frailty during the follow-up period (COVID-19 pandemic).
Table 1.
Demographic characteristics of four groups according to family structure and social activity
| Overall n=937 | Not living alone and socially active n=419 | Not living alone and socially inactive n=390 | Living alone and socially active n=69 | Living alone and socially inactive n=59 | |
|---|---|---|---|---|---|
| Demographic | |||||
| Age, mean (SD) | 73.5 (5.5) | 74.2 (5.3) | 72.7 (5.4) | 73.8 (5.6) | 72.7 (6.2) |
| Women, n (%) | 458 (48.9) | 231 (55.1) | 141 (36.2) | 52 (75.4) | 34 (57.6) |
| Height, mean (SD) | 160.4 (8.3) | 159.3 (7.8) | 162.5 (8.4) | 157.1 (8.7) | 158.5 (8.0) |
| Weight, mean (SD) | 57.9 (10.2) | 56.6 (9.7) | 60.3 (10.4) | 55.0 (9.7) | 54.9 (10.9) |
| BMI, mean (SD) | 22.4 (2.8) | 22.2 (2.6) | 22.7 (2.8) | 22.2 (2.9) | 21.7 (3.2) |
| Underweight (<18.5), n (%) | 75 (8.0) | 36 (8.6) | 25 (6.4) | 5 (7.2) | 9 (15.3) |
| Lower health literacy, n %) | 419 (44.7) | 178 (42.5) | 173 (44.4) | 33 (47.8) | 35 (59.3) |
| Polypharmacy, n (%) | 140 (14.9) | 63 (15.0) | 63 (16.2) | 6 (8.7) | 8 (13.6) |
| Morbidity | |||||
| Hypertension, n (%) | 305 (32.6) | 128 (30.5) | 140 (35.9) | 21 (30.4) | 16 (27.1) |
| Hyperlipidemia, n (%) | 127 (13.6) | 57 (13.6) | 50 (12.8) | 12 (17.4) | 8 (13.6) |
| Diabetes, n (%) | 91 (9.7) | 30 (7.2) | 48 (12.3) | 6 (8.7) | 7 (11.9) |
| Cancer, n (%) | 51 (5.4) | 28 (6.7) | 16 (4.1) | 5 (7.2) | 2 (3.4) |
| Cardiovascular disease, n (%) | 48 (5.1) | 22 (5.3) | 19 (4.9) | 4 (5.8) | 3 (5.1) |
| Kidney disease, n (%) | 46 (4.9) | 27 (6.4) | 15 (3.8) | 2 (2.9) | 2 (3.4) |
| Orthopedic disease, n (%) | 40 (4.3) | 24 (5.7) | 14 (3.6) | 1 (1.4) | 1 (1.7) |
| Total PA time (minutes) | |||||
| January-2020, median (IQR) | 300 (120–540) | 330 (120–580) | 280 (105–540) | 360 (190–580) | 210 (120–360) |
| April-2020, median (IQR) | 200 (45–420) | 210 (60–450) | 200 (20–420) | 240 (90–540) | 120 (0–220) |
| August-2020, median (IQR) | 215 (60–450) | 230 (60–450) | 223 (60–450) | 300 (110–540) | 105 (0–240) |
| January-2021, median (IQR) | 180 (30–420) | 180 (30–420) | 200 (30–420) | 300 (60–540) | 80 (0–240) |
| KCL, mean (SD) | |||||
| January-2020, mean (SD) | 3.60 (1.98) | 3.28 (2.03) | 3.91 (1.87) | 3.13 (2.06) | 4.31 (1.67) |
| April-2020, mean (SD) | 4.84 (2.87) | 4.70 (2.89) | 4.86 (2.74) | 4.61 (3.03) | 5.93 (3.15) |
| Frail category, n (%) | |||||
| January-2020 | |||||
| Robust, n (%) | 453 (48.3) | 228 (54.4) | 165 (42.3) | 37 (53.6) | 23 (39.0) |
| Pre-frailty, n (%) | 484 (51.7) | 191 (45.6) | 225 (57.7) | 32 (46.4) | 36 (61.0) |
| Frailty, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| January-2021 | |||||
| Robust, n (%) | 342 (36.5) | 166 (39.6) | 137 (35.1) | 26 (37.7) | 13 (22.0) |
| Pre-frailty, n (%) | 445 (47.5) | 188 (44.9) | 193 (49.5) | 35 (50.7) | 29 (49.2) |
| Frailty, n (%) | 150 (16.0) | 65 (15.5) | 60 (15.4) | 8 (11.6) | 17 (28.8) |
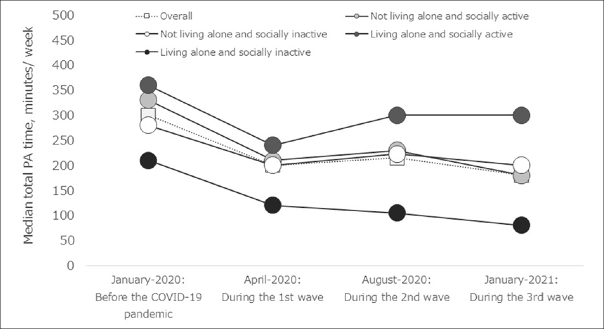
Figure 2 shows the changes in the median total time devoted to PA based on the COVID-19 pandemic waves in Japan: January 2020 (before the pandemic), April 2020 (during the first wave of the pandemic), August 2020 (during the second wave of the pandemic), and January 2021 (during the third wave of the pandemic). Overall, we found a significant decrease in total PA time in April 2020 (median [interquartile range (IQR)], 200 [45–420]), August 2020 (215 [60–450]), and January 2021 (180 [30–420]) than in January 2020 (median [IQR], 300 [120–540]) (P<0.001). We also performed a subgroup analysis based on a combination of family structure and social activity and found that the total PA time in each group had the same tendency as the overall time. Among them, in the living alone and socially inactive groups, total PA time gradually decreased during the first to third waves of the pandemic (P<0.001) (Table 1, Figure 2).
Figure 2.
Changes in median total PA time according to the COVID-19 pandemic. In all (white square), total PA time during the first, second, and third waves of the pandemic decreased by 33.3%, 28.3%, and 40.0%, respectively, from the pre-pandemic PA time. The total PA time of older adults who live alone and are socially inactive decreased significantly; −42.9% (first wave), −50.0% (second wave), and −61.9% (third wave) compared to the pre-pandemic PA time
During the follow-up year (COVID-19 pandemic), 65 participants (15.5%) in the non-living alone and socially active group, 60 (15.4%) in the non-living alone and socially inactive group, 8 (11.6%) in the living alone and socially active group, and 17 (28.8%) in the living alone and socially inactive group had new incident frailty (Table 2). The OR and CI for incident frailty were stratified into four groups according to their combination of family structure and social activity. The living alone and socially inactive group (OR: 2.20 [95% CI 1.18–4.11] and adjusted OR: 2.04 [95% CI 1.01–4.10]) had a significantly elevated risk of incident frailty according to univariate and multivariate analyses using the non-living alone and socially active group as the reference.
Table 2.
Effect of combination of family structure and social activity on incident frailty during the pandemic
| Total | Incident Frailty | Crude model | Adjusted model | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n | % | OR | 95%CI | P-value | OR | 95%CI | P-value | |||
| Items | Min | Max | Min | Max | |||||||
| Not living alone and socially active | 419 | 65 | 15.5 | 1.00 | Ref | 1.00 | Ref | ||||
| Not living alone and socially inactive | 390 | 60 | 15.4 | 0.99 | 0.68 | 1.45 | 0.960 | 0.94 | 0.61 | 1.45 | 0.774 |
| Living alone and socially active | 69 | 8 | 11.6 | 0.71 | 0.33 | 1.56 | 0.400 | 0.64 | 0.27 | 1.51 | 0.310 |
| Living alone and socially inactive | 59 | 17 | 28.8 | 2.20 | 1.18 | 4.11 | 0.013 | 2.04 | 1.01 | 4.10 | 0.047 |
OR, odds ratio; CI, confidence interval; Min, minimum; Max, maximum; Adjusted model: adjusted for age, sex, underweight, polypharmacy, hypertension, hyperlipidemia, diabetes, cancer, cardiovascular disease, kidney disease, orthopedic disease, lower health literacy, total PA time, and total Kihon checklist score in January 2020.
Discussion
The total PA time for initially non-frail older adults during the first, second, and third waves of the pandemic decreased by 33.3%, 28.3%, and 40.0%, respectively, compared to the pre-pandemic period. In particular, the total PA time of older adults who live alone and are socially inactive decreased significantly: −42.9% (first wave), −50.0% (second wave), and −61.9% (third wave) compared to that before the pandemic. Additionally, those who lived alone and were socially inactive had a significantly higher risk of incident frailty than those who did not live alone or were socially active. These findings suggest that older adults who live alone and are socially inactive are more likely to experience incident frailty or disability due to decreased PA during the pandemic.
During the pandemic, especially during a lockdown or a state of emergency, the effect of stay-at-home messages from each government led to decreased PA time and increased sitting time in older adults. These inactive or sedentary behaviors are a serious problem for older people worldwide. PA surveys on older adults have been widely conducted worldwide, and they have consistently reported less PA time during the first wave of the pandemic than before the pandemic (1–5). The current findings are consistent with those of previous reports and show that this sedentary lifestyle continued during the second and third waves of the pandemic. We also reported that the total recovery time devoted to PA by older adults has been realized since the first wave of the pandemic (9). Moreover, the expected total PA time was maintained during the second and third waves of the pandemic. Thus, this level of inactive lifestyle during the second and third waves of the pandemic was expected.
In particular, the total PA time of the living alone and socially inactive groups was more gravely affected by the pandemic than that of the other groups. Our previous survey found that the recovery in PA time for most older adults was established after the first wave of the pandemic, but not in older adults who were living alone and were socially inactive (9). Many older individuals have the potential for resilience against the pandemic because they can communicate with family and neighbors and may be able to obtain valuable information for maintaining their health status, such as the importance of exercise and nutrition. Contrarily, such activities are laborious for older adults who live alone, and they may be at high risk of lower PA time through negative behavior changes due to the pandemic. This tendency was increasingly serious during the second and third waves of the pandemic.
The one-year follow-up period (COVID-19 pandemic) showed that older adults who were living alone and were socially inactive were more likely to have new incidences of frailty compared to those who did not live alone and were socially active. The proportion of new incidences of frail cases in the living alone and socially inactive group (28.8%) was approximately twice that of the other groups (11.6–15.5%). A recent systematic review reported that the incidence rate of frailty was estimated at 60.6/1000 person-years for initially non-frail older adults before the pandemic (23), and this incidence rate was notably lower than our overall results (16.0%) during the pandemic. This striking difference may have resulted from not only the pandemic but also the frailty criteria. Most previous studies used Fried’s Cardiovascular Health Study criteria for defining frailty (24). In this study, frailty was defined using the Kihon checklist (17). According to previous surveys, the prevalence of frailty has a higher tendency in surveys using the Kihon checklist (25) than in surveys using Fried’s criteria (26). However, even if the effect of each criterion is relatively large, the combination of living alone and being socially inactive may have a modifying effect on the incidence of frailty through a significant decrease in PA.
This panel survey has both strengths and weaknesses. The strength of this survey was the prompt release of the up-to-date status of PA and the incidence rate of frailty during the pandemic. In particular, it is valuable in identifying individuals at high risk of frailty. We believe that these findings can be useful in maintaining and improving the health status and preventing frailty and disability in older adults worldwide. However, there may be a lack of external validity in this survey, because the follow-up rate was relatively low (77.3%), and the study comprised participants who were registered with a survey company and could use Internet-connected devices. Moreover, no state of emergency was issued during the second wave of the pandemic in Japan, and the request for self-restraint was minor compared to the first and third waves. However, it is conceivable that physical activity was restricted during the second wave not only because of the pandemic but also because of the high temperature and humidity during summer (27).
In conclusion, owing to the COVID-19 pandemic, the total PA time for initially non-frail older adults during the first, second, and third waves of the pandemic was much lower than that prior to the pandemic. In particular, the total PA time for older adults who live alone and are socially inactive was more seriously affected by the pandemic, and their rate of new incidence of frailty was significantly higher than that of other older adults during the pandemic. These findings suggest that older adults who live alone and are socially inactive are more likely to have an incidence of frailty or disability due to decreased PA during the pandemic. Therefore, understanding this mechanism may be crucial for maintaining the health status of older adults during the pandemic.
Acknowledgments
This work was supported by the Research Fund for Longevity Science from the Grants-in-Aid for Comprehensive Research on Aging and Health from the Ministry of Health, Labor, and Welfare, Japan.
Conflict of interest: The authors have no potential conflicts of interest to disclose.
Ethical standards: The ethics committee approved this study.
References
- 1.Yamada M, Kimura Y, Ishiyama D, et al. Effect of the COVID-19 Epidemic on Physical Activity in Community-Dwelling Older Adults in Japan: A Cross-Sectional Online Survey. J Nutr Health Aging. 2020;24:948–950. doi: 10.1007/s12603-020-1501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tison GH, Avram R, Kuhar P, et al. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann Intern Med. 2020;173(9):767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Browne RAV, Macêdo GAD, Cabral LLP, et al. Initial impact of the COVID-19 pandemic on physical activity and sedentary behavior in hypertensive older adults: An accelerometer-based analysis. Exp Gerontol 2020 Epub. [DOI] [PMC free article] [PubMed]
- 5.Schlichtiger J, Steffen J, Huber BC, et al. Physical activity during COVID-19 lockdown in older adults. J Sports Med Phys Fitness. 2021;61(1):164–166. doi: 10.23736/S0022-4707.20.11726-2. [DOI] [PubMed] [Google Scholar]
- 6.Wedig IJ, Duelge TA, Elmer SJ. et al. Stay physically active during COVID-19 with exercise as medicine. Br J Sports Med 2020 Epub ahead of print. [DOI] [PubMed]
- 7.Faghy MA, Arena R, Stoner L, et al. The need for exercise sciences and an integrated response to COVID-19: A position statement from the international HL-PIVOT network. Prog Cardiovasc Dis 2021 Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 8.Lim WS, Liang CK, Assantachai P, et al. COVID-19 and older people in Asia: Asian Working Group for Sarcopenia calls to actions. Geriatr Gerontol Int. 2020;20(6):547–558. doi: 10.1111/ggi.13939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamada M, Kimura Y, Ishiyama D, et al. Letter to the Editor: Recovery of Physical Activity among Older Japanese Adults since the First Wave of the COVID-19 Pandemic. J Nutr Health Aging. 2020;24(9):1036–1037. doi: 10.1007/s12603-020-1516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bunt S, Steverink N, Olthof J, et al. Social frailty in older adults: a scoping review. Eur J Ageing. 2017;14(3):323–334. doi: 10.1007/s10433-017-0414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gobbens RJ, van Assen MA, Luijkx KG, et al. Determinants of frailty. J Am Med Dir Assoc. 2010;11(5):356–364. doi: 10.1016/j.jamda.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Teo N, Gao Q, Nyunt MSZ, et al. Social Frailty and Functional Disability: Findings From the Singapore Longitudinal Ageing Studies. J Am Med Dir Assoc. 2017;18(7):637.e13–637.e19. doi: 10.1016/j.jamda.2017.04.015. [DOI] [PubMed] [Google Scholar]
- 13.Makizako H, Shimada H, Tsutsumimoto K, et al. Social Frailty in Community-Dwelling Older Adults as a Risk Factor for Disability. J Am Med Dir Assoc. 2015;16(11):1003.e7–11. doi: 10.1016/j.jamda.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 14.Yamada M, Arai H. Social Frailty Predicts Incident Disability and Mortality Among Community-Dwelling Japanese Older Adults. J Am Med Dir Assoc. 2018;19(12):1099–1103. doi: 10.1016/j.jamda.2018.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Garre-Olmo J, Calvó-Perxas L, López-Pousa S, et al. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age Ageing. 2013;42(1):46–51. doi: 10.1093/ageing/afs047. [DOI] [PubMed] [Google Scholar]
- 16.Andrew MK, Rockwood K. Social vulnerability predicts cognitive decline in a prospective cohort of older Canadians. Alzheimers Dement. 2010;6(4):319–325. doi: 10.1016/j.jalz.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Satake S, Senda K, Hong YJ, et al. Validity of the Kihon Checklist for assessing frailty status. Geriatr Gerontol Int. 2016;16(6):709–715. doi: 10.1111/ggi.12543. [DOI] [PubMed] [Google Scholar]
- 18.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 19.Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015;15:518–9. doi: 10.1111/ggi.12397. [DOI] [PubMed] [Google Scholar]
- 20.Tamakoshi A, Yatsuya H, Lin Y, et al. BMI and all-cause mortality among Japanese older adults: findings from the Japan collaborative cohort study. Obesity (Silver Spring) 2010;18(2):362–369. doi: 10.1038/oby.2009.190. [DOI] [PubMed] [Google Scholar]
- 21.Hsu HF, Chen KM, Belcastro F, et al. Polypharmacy and pattern of medication use in community-dwelling older adults: A systematic review. J Clin Nurs. 2020 Epub ahead of print. [DOI] [PubMed]
- 22.Ishikawa H, Nomura K, Sato M, et al. Developing a measure of communicative and critical health literacy: a pilot study of Japanese office workers. Health Promot Int. 2008;23(3):269–274. doi: 10.1093/heapro/dan017. [DOI] [PubMed] [Google Scholar]
- 23.Ofori-Asenso R, Chin KL, Mazidi M, et al. Global Incidence of Frailty and Prefrailty Among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(8):e198398. doi: 10.1001/jamanetworkopen.2019.8398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.M146. [DOI] [PubMed] [Google Scholar]
- 25.Satake S, Shimokata H, Senda K, et al. Validity of Total Kihon Checklist Score for Predicting the Incidence of 3-Year Dependency and Mortality in a Community-Dwelling Older Population. J Am Med Dir Assoc. 2017;18(6):552.e1–552.e6. doi: 10.1016/j.jamda.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Satake S, Shimada H, Yamada M, et al. Prevalence of frailty among community-dwellers and outpatients in Japan as defined by the Japanese version of the Cardiovascular Health Study criteria. Geriatr Gerontol Int. 2017;17(12):2629–2634. doi: 10.1111/ggi.13129. [DOI] [PubMed] [Google Scholar]
- 27.Yasunaga A, Togo F, Watanabe E, et al. Sex, age, season, and habitual physical activity of older Japanese: the Nakanojo study. J Aging Phys Act. 2008;16(1):3–13. doi: 10.1123/japa.16.1.3. [DOI] [PubMed] [Google Scholar]