Abstract
Background:
Taking caring of patients with mental disorders is stressful and people who take care of these patients need to receive enough support and training to overcome this challenging situation. The present study was aimed at investigating the effects of a psychosocial support program on perceived stress of family caregivers of patients with mental disorders.
Materials and Methods:
This randomized controlled clinical trial was performed on 64 family caregivers of patients with mental disorders referred to Noor and Hazrat-e-Ali Asghar hospital in Isfahan, Iran, in 2018-19. The participants were randomly assigned to the intervention and control groups using a random number table. In the intervention group, the training program was held in 6 sessions of 90-minute training classes twice a week. Data were collected using a demographic characteristics form and the Perceived Stress Scale (PSS) before, immediately after, and 1 month after the intervention. Descriptive and inferential statistical tests such as Chi-square, Mann-Whitney, independent t-test, repeated measures ANOVA, and Kolmogorov-Smirnov test were used to analyze the data in SPSS software.
Results:
The result of the study showed that the total mean score of perceived stress in the intervention group was significantly less than the control group immediately after (F2=66.29, p<0.001) and 1 month after the intervention (F2=66.29, p<0.001).
Conclusions:
Delivering a training program on the different dimensions of support family caregivers need will reduce the perceived stress of family caregivers of patients with mental disorders. Therefore, the implementation of this intervention is recommended in this group of caregivers.
Keywords: Caregivers, Iran, mental disorders, psychosocial
Introduction
Among the various medical diseases, psychiatric disorders have a high prevalence and a significant burden on patients. According to the most recent meta-analysis, the average prevalence of mental disorders in the world is 13.4%.[1] About 27% of adults in European countries have had at least 1 psychiatric disorder during the last 12 months. These mental disorders account for 13% of all disorders.[2] The researches performed in Iran have revealed that the prevalence of mental disorders in 1999, 2002, and 2012 was 21%, 17.10%, and 23.6%, respectively. These findings show a rising trend in mental disorders in Iran in recent years.[3]
In the past, patients with mental disorders were isolated, but in the 1950s, after discovering psychiatric drugs and with increase in social-based services, hospitalizations in psychological departments decreased and patients were mostly referred to their families, and family caregivers became one of the greatest sources of care for these patients.[4] Family caregivers are recognized as uno?fficial health service providers, as they do not have any previous training regarding caring for patients.[5,6] A family member suffering from mental disorders can impose a great deal of stress and tension on the other family members.[7] Due to the stress caused by various roles and responsibilities related to caregiving and the lack of supportive resources, caregivers experience psychological and physical stress.[6] Lack of emotional, financial, and personal resources causes the caregivers to experience severe stress during the process of health care provision, and causes unpredictable stressors, which may lead to emotional loss, sense of guilt and loneliness, or family conflicts.[8] Based on the hypothetical model of adaptation and stress, the severity of the effect of stressful situations due to continuous caregiving is related to personal resources such as the style and amount of adaptation of the caregiver to stress, and having sufficient social support.[9]
In studies on the therapeutic, caregiving, and educational needs of families of mental patients, it was found that most of these families have announced their needs for social and psychological support and information.[10,11] Social support is always accompanied by psychological support in a twisted and inseparable way.[12] Social support is considered as a multi-dimensional structure categorized into the 4 major classes of emotional support (focusing on knowledge, understanding, defensive skills, rebuilding, and increasing self-confidence decreases the feeling of incompetence and increases the feeling of control), informational support (including consultation and education), appraisal support (including approval, acknowledgment, and providing feedback), and instrumental support (that is receiving direct, tangible, and real help such as financial support and care services).[13,14] Psychosocial support programs to improve or increase the skills of caregivers in order to manage their caregiving situation and help them provide the patients with suitable caregiving are of great importance. These interventional programs usually include releasing emotions, attending group work plans, cognitive treatments, education, and consultations. Training interventions are useful in providing information and teaching problem-solving skills, and they increase the Quality of Life (QOL) of both patients and caregivers.[15] The provision of interventional, psychological, and relief feelings programs for caregivers by authentic resources has positive outcomes such as relieving caregiving stress and increasing tranquility.[16]
We have always depended on families to provide support and to assist family members when they can no longer function independently. We expect them to provide care and support to each other during times of illness regardless of their needs.[17] The fact is that, without support, patients feel isolated and alone in the caregiving process and it is the responsibility of the health care and treatment staff to provide the necessary knowledge, skills, and support for family caregivers as “forgotten patients” and increase their hope and confidence.[18] Developing and providing supportive programs for this group by using the help of psychiatric mental health nurses can be a way to control the caregiving anxieties of the caregivers. One of the beliefs in family nursing is that illness is a family concern; therefore, it is important to involve all family members in the caregiving process.[19]
Many interventions for those with serious mental health problems provided by health and social care services are focused on the person using the service.[20,21,22] The present research was conducted on the primary caregivers of patients with severe mental illness (schizophrenia, bipolar disorder, depression, and anxiety disorders). The present study intervention mainly covered informational and emotional support; thus, it is suggested that other aspects of support family caregivers need be taken into consideration in interventions in future researches. While numerous studies have revealed the positive impacts of psychosocial interventions in different groups,[15,23,24,25] some interventions did not have any effect on the caregiver's burden and stress levels.[26,27] Very few studies have been performed on the impacts of these interventions on the family caregivers of patients with mental disorders, and very few authentic support and training services are available to Iranian caregivers.[28] Therefore, the researchers decided to evaluate the effects of a psychosocial support program on perceived stress in family caregivers of patients with mental disorders.
Materials and Methods
The present 2-group, 3-stage, clinical trial with the registered ID No. of IRCT20180416039321N2 was conducted from July 2018 to December 2019. It was performed on 64 main caregivers (father, mother, spouse, sister, brother, and children) of patients with mental disorders referred to the Noor and Hazrat-e-Ali Asghar hospital in Isfahan, Iran. The study inclusion criteria included being the main caregiver of a patient with severe mental disorders (schizophrenia, mood, and anxiety disorders) and accepting all his/her responsibilities, being able to speak, read, and write in Persian, being interested in and willing to take part in the study, no previous or concurrent enrollment in any other training schedules (any other researches similar to this research intervention), taking care of only 1 family patient with chronic problems, and lack of severe stress due to some situations such as losing (death) a family member or divorce in the last 6 months, lack of known mental problem in the caregiver. The participants were selected using convenience sampling method, and then, assigned randomly to control and intervention groups using a random number table. The sample size was calculated using statistical formulas and based on a similar study with about 32 participants.[5] Taking into account the possible loss of samples, 36 people were selected for each group, in which the Z1 was the confidence interval (CI) that was considered to be 95%, Z2 was test power that was 80%. The least difference between the mean of changes in perceived stress score between the groups was considered to be 0.70.
The researcher first visited the psychological departments of the hospital and checked the patients' documents and recorded their contact numbers. Then, they were contacted by phone, and after introducing and explaining the research goals, the main caregivers were invited to enter the research. The contents of the meetings [Table 1] were based on an educational pamphlet that was developed based on previous studies[29,30] and caregivers' problems. During the program, the researcher tried to establish an empathetic relationship with caregivers through active listening, empathy, and trust, and focused on increasing knowledge, awareness, and the sense of control in them. Moreover, as the program mainly provided information and recommendations for effectively dealing with problems and difficulties in the stressful and challenging circumstances of caregiving, it can be said that the focus of the program is mainly on emotional and informational support.
Table 1.
The contents of the psychosocial support program
| Session | Content |
|---|---|
| 1st | Familiarizing the caregivers with the program, completing the questionnaires, introducing the mental health criteria, group discussions about major problems the caregivers are faced with |
| 2nd | Familiarizing the caregivers with schizophrenia, mood, and anxiety disorders (definition, etiology, risk factors, types and signs, prognoses, and recurrence) |
| 3rd | Familiarizing the caregivers with their role in the process of the disease, communication skills, and how to deal with their patient’s behavioral problems due to the mental disorder (bizarre behaviors, suicide, aggression, and substance abuse) and how to control them |
| 4th | Familiarizing the caregivers with stress reduction methods such as progressive muscle relaxation, guided imagery, and deep breathing |
| 5th | Teaching stress management methods like problem-focused and emotion-focused coping strategies, problem-solving methods, and introducing available supportive resources |
| 6th | Reviewing the topics of the previous sessions, getting feedback from the participants about the sessions, completing the questionnaire, thanking the caregivers for their participation |
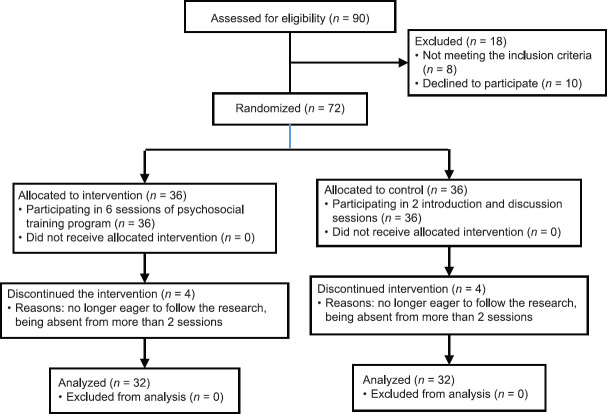
Before implementing the intervention, it was approved by 8 faculty members of the School of Nursing and Midwifery of Isfahan University of Medical Sciences, Iran. The caregivers were then provided with the pamphlets and the intervention was performed in 6 sessions of 90-minute training classes twice a week in the teaching classroom of Noor Hospital with group-working method in groups of 5-15 caregivers. In total, 3 courses of 6 sessions were held. Perceived stress was evaluated by the researcher in both groups (control and intervention) before, immediately after, and 1 month after the intervention using the Perceived Stress Scale (PSS). The control group did not receive any training programs and only took part in the 2 introduction and discussion sessions about the problems of families of patients with mental disorders. During the research, participants who were no longer willing to take part in the research or were absent from more than 2 sessions (Exclusion criteria) were excluded from the research [Figure 1].
Figure 1.
CONSORT flow diagram of the participants
Data were collected using the PSS and a demographic characteristics questionnaire including questions regarding age, sex, marital status, employment, family relationship, educational level, family income, the patient's mental disorder, and the duration of the patient's mental disorder. PSS was developed by Cohen, Kamark, and Mermelstein in 1983 to evaluate the stressful situations of the patient's life during the last month. In this research, the third edition of the PSS with 14 items was used. The items of this scale are scored on a 5-point scale ranging from 0 to 4 [never (0), hardly ever (1), sometimes (2), often (3), and always (4)]. It is worth noting that the 7 positive questions (4, 5, 6, 7, 9, 10, and 13) are reverse-scored. The total score of the scale ranges from 0 to 56, with higher scores indicating higher perceived stress.[31] The PSS is a standard questionnaire that is frequently applied and evaluated in various Iranian researches. Cohen . (1983) reported the test-retest reliability and internal consistency of the PSS to be 0.85 and 0.84-0.86, respectively. Mosavi et al. have approved the internal consistency coefficient of the questionnaire items in the Iranian population, and reported the Cronbach's alpha of the items to be 0.84.[32] The collected data were analyzed using descriptive and analytic statistical methods such as mean and standard deviation, Kolmogorov-Smirnov test (for checking normality of sample distribution), Chi-square, Mann-Whitney, and independent t-test (for analyzing demographic characteristics data), and repeated measures ANOVA (for analyzing perceived stress data) in SPSS software (Version 16; SPSS Inc., Chicago, IL, USA). A p value of less than 0.05 was considered significant.
Ethical considerations
The ethical approval for this study was obtained from Isfahan University of Medical Sciences (ethical approval code: IR.MUI.RESEARCH.REC.1398.231). Before the intervention, all the participants were informed of the study goal and method and the voluntary nature of the research and were assured of the confidentiality of their information. Written informed consent was obtained from all the participants.
Results
In total, 72 family caregivers met the study inclusion criteria and were randomly allocated to either the intervention (n = 36) or control group (n = 36). A total of 8 family caregivers (4 in the intervention group and 4 in the control group) did not complete the program due to their busy schedule or other unknown reasons [Figure 1]. No statistically significant differences were observed between the two groups in terms of mean scores of family caregivers' demographic variables (p > 0.05) and the groups were almost the same in terms of the demographic characteristics. The independent t-test revealed that before the intervention there were no significant differences between the groups.
The mean (SD) age of the caregivers in the intervention and control groups was 49.25 (10.88) and 47.37 (13.64) years, respectively. Most of the caregivers in both the intervention (62.50%) and control group (71.90%) were women, and a majority of the participants in the intervention (84.40%) and control groups (75%) were married. Most of the caregivers in the intervention (43.70%) and control (46.90%) groups were homemakers. The highest prevalence of family relation in both intervention (46.90%) and control groups (43.80%) were related to mothers. The education level of most caregivers in the intervention (46.90%) and control groups (46.90%) was pre-high school diploma. The income of the families in the intervention (62.50%) and control groups (62.50%) was lower than their expenditure. The highest prevalence of the type of mental disorder in the intervention (50%) and control groups (59.40%) was related to mood disorders. The mean (SD) duration of the disorder in the intervention and control group was 8.66 (7.78) and 8.52 (6.52) years, respectively.
Moreover, the results of the present study showed that the mean score of perceived stress in the control group was significantly higher than that in the intervention group immediately after the intervention (F2=66.29, p<0.001) and 1 month after the intervention (F2=66.29, p<0.001). Repeated measures ANOVA revealed that the mean score of perceived stress of the caregivers in the intervention group had significantly differed in the 3 stages of the study (P < 0.05), but no significant differences were observed among the 3 study stages in the control group (P > 0.05) [Table 2].
Table 2.
Caregivers’ stress mean score at different times in two groups
| Time | Mean (SD*) | Independent t-test | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | t | df | p | ||
| Before the intervention | 28.37 (8.86) | 28.62 (8.14) | 0.12 | 62 | 0.91 | |
| Immediately after the intervention | 21.83 (7.39) | 29.53 (7.71) | 4.08 | 62 | < 0.001 | |
| One month after the intervention | 21.68 (7.15) | 29.66 (8.24) | 4.10 | 62 | < 0.001 | |
| Repeated measures ANOVA** | F | 66.29 | 2.03 | - | ||
| df | 2 | 2 | - | |||
| p | < 0.001 | 0.13 | - | |||
*SD: Standard deviation, **ANOVA: Analysis of variance
Discussion
The results of the present study revealed that the psychosocial support program reduced perceived stress in family caregivers of patients with mental disorders. This decrease in stress in the caregivers compared to before the intervention can be due to the fact that some of the perceived stress of the caregivers was related to dealing with and meeting the various needs of the patients and their lack of information in this regard, and that the intervention of the present study focused on providing the caregivers with training on support and information about the aforementioned topics. To support this finding, the results of the same studies can be applied. This finding is in line with that of the study by Mojarad Kahani et al.[33] They showed that group psycho-educational interventions can decrease the experienced stress of families of patients with bipolar disorders and can be efficient in reducing the psychological problems of families with patients suffering from mood disorders.[33] Bastani et al. reported a significant decrease in the perceived stress of caregivers in the intervention group after a group-based intervention.[34] Moreover, Pahlavanzadeh et al. reported that family psycho-education can reduce stress in family caregivers of patients with mental disorders.[30] The results of the study by Mansouri et al. also revealed that communication skills training significantly decreased the perceived stress of caregivers of elderly with Alzheimer's disease.[35] The findings of George and Raju were also consistent with that of the present study. They revealed that the experimental group had positive coping strategies, such as planful problem solving and seeking social support, after hardiness training and suggested that hardiness training is an effective therapeutic modality in reducing perceived stress in caregivers of patients with schizophrenia.[36]
These studies showed that combining family psycho-educational interventions with routine mental health care has significant effect on decreasing mental problems such as the stress of family caregivers.[30] Psycho-interventional plans to improve or increase caregivers' skills in order to develop their caregiving roles and their ability to provide high-quality services to the mentally ill member of the family had decreased the stressful load of caregiving and increased the caregiving capacity of the caregivers.[16]
Moreover, promoting communication skills during group-based meetings for the caregivers can be a defensive strategy to regulate their stress.[35] Other studies on caregivers of patients with other medical disorders reported the same results. For example, the meaningful results of the study by Etemadifar et al. on the effects of family-centered empowerment intervention on perceived stress among family caregivers of patients with epilepsy revealed that family-centered caregiving can greatly decrease the perceived stress of family caregivers.[18]
However, the results of the present study were not in line with that of McDonell et al. (2003).[37] They reported that family psycho-education did not have a significant impact on the stress level of caregivers. The reason for this difference may be the long duration of the intervention; the condition of the patients may have decreased and the caregivers have not been able to adapt to the conditions, and thus, their tension has increased. The long duration between the intervention and the post-test in the study by McDonell et al. (immediately after and 2 years later) shadowed the effects of the training intervention, and accordingly, the stress level of the caregivers had increased.[37] Vaghee et al. found no significant differences between the control group and experimental group in terms of total scores at the post-intervention stage.[38] The results of this study suggested that the caregivers in the experimental group who received stress management training had higher levels of positive experience than those in the control group; nevertheless, this difference was not statistically significant and is inconsistent with the findings of the present investigation. This can be due to the tendency to report positive aspects in the Iranian culture and the educational level of the participants because this factor could affect their perception of training and the way they complete the questionnaire.[38] Generally, the present study was effective in the reduction of family caregiver's perceived stress in the intervention group. Thus, health care providers, especially nurses, can play an important role in supporting family caregivers by considering and implementing this program.
The limitations of the present study were individual differences of the learners, the motivation of individuals to attend sessions, the correct use of learned methods, the events and stresses of everyday life, and the way individuals adapt to these issues. Since this study was carried out on humans, and it was not possible to control all human aspects in the study, including physiological, psychological, social, and economic factors, these factors are considered as limitations of the study.
Conclusion
Family caregivers of patients with mental disorders welcomed the informational and emotional support presented in this psychosocial support program because such a program places more emphasis on providing information about the disease, support, training, coping, and communicational skills in order to decrease the pressure on the caregivers. It seems that the provision of a psychosocial support program by nurses and health organization personnel can reduce perceived stress in family caregivers of patients with mental disorders.
Financial support and sponsorship
Isfahan University of Medical Sciences, Iran
Conflicts of interest
Nothing to declare.
Acknowledgements
This manuscript has been extracted from a Master's thesis in psychiatric nursing. This study was financially supported by the Vice Chancellor for research of Isfahan University of Medical Sciences (Grant No: 398270). The authors would like to thank all the participants and authorities of the School of Nursing and Midwifery and Noor and Hazrat-e- Ali Asghar hospital, and all those who somehow supported and guided us in this project.
References
- 1.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–65. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 2.Kohrt BA, Blasingame E, Compton MT, Dakana SF, Dossen B, Lang F, et al. Adapting the Crisis Intervention Team (CIT) model of police-mental health collaboration in a low-income, post-conflict country: Curriculum development in Liberia, West Africa. Am J Public Health. 2015;105:73–80. doi: 10.2105/AJPH.2014.302394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noorbala AA, Damari B, Riazi-Isfahani S. Evaluation of mental disorders incidence trend in Iran. Sci Res J Shahed University. 2014;21:1–11. [Google Scholar]
- 4.Zauszniewski JA, Bekhet AK. Factors associated with the emotional distress of women family members of adults with serious mental illness. Arch Psychiatr Nurs. 2014;28:102–7. doi: 10.1016/j.apnu.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Shariati Far F, Moreini M, Kheirabadi GR. Analysis of the effects of a support program based on psychosocial needs of families on care burdens of family caregivers of patients with ischemic heart disease hospitalized in Chamran heart ward of Isfahan University of Medical Sciences. Int J Med Res Health Sci. 2016;5:152–7. [Google Scholar]
- 6.Narasipuram S, Kasimahanti S. Quality of life and perception of burden among caregivers of persons with mental illness. Arch Mental Health. 2012;13:99–103. [Google Scholar]
- 7.Akbari M, Alavi M, Irajpour A, Maghsoudi J. Challenges of family caregivers of patients with mental disorders in Iran: A narrative review. Iran J Nurs Midwifery Res. 2018;23:329–37. doi: 10.4103/ijnmr.IJNMR_122_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan SW. Global perspective of burden of family caregivers for persons with schizophrenia. Arch Psychiatr Nurs. 2011;25:339–49. doi: 10.1016/j.apnu.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Lopez J, Romero-Moreno R, Marquez-Gonzalez M, Losada A. Spirituality and self-efficacy in dementia family caregiving: Trust in God and in yourself. Int Psychogeriatr. 2012;24:1943–52. doi: 10.1017/S1041610212001287. [DOI] [PubMed] [Google Scholar]
- 10.Barekatain M, Attari A, Noori F, Aminoroaia Assessment of Psycho-educational needs of families of patients with bipolar I disorder. J Res Behav Sci. 2016;14:23–9. [Google Scholar]
- 11.Zeinalian P, Mottaghipour Y, Samimi Ardestani M. Validity and the cultural adaptation of the carers' needs assessment for schizophrenia and assessing the needs of family members of bipolar mood disorder and schizophrenia spectrum patients. J Fund Ment Health. 2011;12:684–91. [Google Scholar]
- 12.Barilla D, Marshak HH, Anderson SE, Hopp JW. Postpartum follow-up: Can psychosocial support reduce newborn readmissions? MCN Am J Matern. 2010;35:33–9. doi: 10.1097/01.NMC.0000366808.75079.cc. [DOI] [PubMed] [Google Scholar]
- 13.Drentea P, Clay OJ, Roth DL, Mittelman MS. Predictors of improvement in social support: Five-year effects of a structured intervention for caregivers of spouses with Alzheimer's disease. Soc Sci Med. 2006;63:957–67. doi: 10.1016/j.socscimed.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Nabi H, Hall M, Koskenvuo M, Singh-Manoux A, Oksanen T, Suominen S, et al. Psychological and somatic symptoms of anxiety and risk of coronary heart disease: The health and social support prospective cohort study. Biol Psychiatry. 2010;67:378–85. doi: 10.1016/j.biopsych.2009.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruvik FK, Allore HG, Ranhoff AH, Engedal K. The effect of psychosocial support intervention on depression in patients with dementia and their family caregivers: An assessor-blinded randomized controlled trial. Dement Geriatr Cogn Dis Extra. 2013;3:386–97. doi: 10.1159/000355912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carretero S, Garces J, Rodenas F, Sanjose V. The informal caregiver's burden of dependent people: Theory and empirical review. Arch Gerontol Geriatr. 2009;49:74–9. doi: 10.1016/j.archger.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Schulz R. Family caregiving roles and impacts. In: Schulz R, Eden J, editors. Families caring for an aging America. Washington, DC: National Academies of Sciences, Engineering, and Medicine; 2016. pp. 73–122. [Google Scholar]
- 18.Etemadifar S, Heidari M, Jivad N, Masoudi R. Effects of family-centered empowerment intervention on stress, anxiety, and depression among family caregivers of patients with epilepsy. Epilepsy Behav. 2018;88:106–12. doi: 10.1016/j.yebeh.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 19.Østergaard B, Clausen AM, Agerskov H, Brødsgaard A, Dieperink KB, Funderskov KF, et al. Nurses' attitudes regarding the importance of families in nursing care: A cross-sectional study. J Clin Nur. 2020;29:1290–301. doi: 10.1111/jocn.15196. [DOI] [PubMed] [Google Scholar]
- 20.Puolakka K, Pitkänen A. Effectiveness of psychosocial interventions on quality of life of patients with schizophrenia and related disorders: A systematic review. Arch Psychiatr Nurs. 2019;33:73–82. doi: 10.1016/j.apnu.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 21.Sirati-Nir M, Khaghanizade M, Rahimi A, Khazaei M, Ghadirian F. The effect of social support skill-training group intervention on perceived social support in veterans with posttraumatic stress disorder. Iran J Nurs Midwifery Res. 2018;23:272–6. doi: 10.4103/ijnmr.IJNMR_165_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Silva MJ, Cooper S, Li HL, Lund C, Patel V. Effect of psychosocial interventions on social functioning in depression and schizophrenia: Meta-analysis. Br J Psychiatry. 2013;202:253–60. doi: 10.1192/bjp.bp.112.118018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fu F, Zhao H, Tong F, Chi I. A systematic review of psychosocial interventions to cancer caregivers. Front Psychol. 2017;8:1–12. doi: 10.3389/fpsyg.2017.00834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng HY, Chair SY, Chau JP. The effectiveness of caregiver psychosocial interventions on the psychosocial wellbeing, physical health and quality of life of stroke family caregivers and their stroke survivors: A systematic review. JBI Libr Syst Rev. 2012;10:679–797. doi: 10.11124/jbisrir-2012-66. [DOI] [PubMed] [Google Scholar]
- 25.Hudson PL, Remedios C, Thomas K. A systematic review of psychosocial interventions for family carers of palliative care patients. BMC Palliat Care. 2010;9:1–6. doi: 10.1186/1472-684X-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin-Carrasco M, Dominguez-Panchon AI, Gonzalez-Fraile E, Munoz-Hermoso P, Ballesteros J. Effectiveness of a psychoeducational intervention group program in the reduction of the burden experienced by caregivers of patients with dementia: The EDUCA-II randomized trial. Alzheimer Dis Assoc Disord. 2014;28:79–87. doi: 10.1097/WAD.0000000000000003. [DOI] [PubMed] [Google Scholar]
- 27.Jansen APD, van Hout HPJ, Nijpels G, Rijmen F, Dröes RM, Pot AM, et al. Effectiveness of case management among older adults with early symptoms of dementia and their primary informal caregivers: A randomized clinical trial. Int J Nurs Stud. 2011;48:933–43. doi: 10.1016/j.ijnurstu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Etemadifar S, Bahrami M, Shahriari M, Farsani AK. The effectiveness of a supportive educative group intervention on family caregiver burden of patients with heart failure. Iran J Nurs Midwifery Res. 2014;19:217–23. [PMC free article] [PubMed] [Google Scholar]
- 29.Mami S, Kaikhavani S, Amirian K, Neyazi E. The effectiveness of family psychoeducation (Atkinson and Coia Model) on mental health family members of patients with psychosis. JIUMS. 2016;24:8–17. [Google Scholar]
- 30.Pahlavanzadeh S, Navidian A, Yazdani M. The effect of psycho-education on depression, anxiety and stress in family caregivers of patients with mental disorders. Behbood J. 2010;14:228–36. [Google Scholar]
- 31.Cohen S, Kamark T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 32.Mosavi E, Ali Pour A, Agah Heris M, Zare H. The effectiveness of LEARN new program on reduction of perceived stress and worry among students. Health psychol. 2014;3:47–63. [Google Scholar]
- 33.Mojarad Kahani AH, Ghanbari Hashem Abadi BA, Soltanian G. The efficacy of group psycho educational interventions on level of depression, anxiety and burden experienced (stress) in families of patients with bipolar disorders. J Res Behav Sci. 2015;13:420–30. [Google Scholar]
- 34.Bastani F, Hosseini RS, Javanbakhtian Ghahfarokhi R. The effect of group discussion and telephone counselling on perceived stress of women as caregivers of patients with Alzheimer disease. J Clin Nurs Midwifery. 2012;1:61–72. [Google Scholar]
- 35.Mansouri T, Dehdari T, Seyedfatemi N, Gohari M, Barkhordari M. The effect of communication skills training on perceived stress of caregivers of elderly with Alzheimer's disease referral to Iranian Alzheimer Association in 2012. Razi J Med Sci. 2014;21:52–62. [Google Scholar]
- 36.George R, Raju S. Effect of hardiness training on perceived stress and ways of coping among family caregivers of patients with schizophrenia. Int J Indian Psychol. 2018;6:137–44. [Google Scholar]
- 37.McDonell MG, Short RA, Berry CM, Dyck DG. Burden in schizophrenia caregivers: Impact of family psychoeducation and awareness of patient suicidality. Fam Process. 2003;42:91–103. doi: 10.1111/j.1545-5300.2003.00091.x. [DOI] [PubMed] [Google Scholar]
- 38.Vaghee S, Rezaei M, Asgharipour N, Chamanzari H. The effect of stress management training on positive experiences of families caring for patients with schizophrenia. Evidence Based Care. 2017;6:57–65. [Google Scholar]