Abstract
Eosinophilic cystitis is a rare inflammatory disease in the pediatric population with varied presentations. Diagnosis requires a high index of suspicion and cystoscopy with biopsy of the bladder mass. There are no standard treatment guidelines, however, these patients usually respond with medical management, but recurrence is a possibility. We present a case of eosinophilic cystitis in a 6-year-old boy who presented with lower urinary tract symptoms, gross hematuria, and bladder mass.
KEYWORDS: Bladder, bladder wall biopsy, cystitis, eosinophilia, rhabdomyosarcoma
INTRODUCTION
Eosinophilic cystitis is a rare condition in children, and to date, 73 cases have been reported in the literature.[1,2] The clinical manifestations range from suprapubic pain, increased frequency to urinary retention, and hematuria. It is usually seen as a bladder mass on ultrasound and computed tomography (CT) urography which have a differential diagnosis of bladder malignancy. Cystoscopy and biopsy remain the gold standard in coming to this unusual diagnosis. There are no standard treatment guidelines. The current treatment option ranges from supportive care, identification of an antigenic stimulus, medical management with antihistamines, steroids, immunosuppressants, and antibiotics to surgical management such as partial cystectomy and transurethral bladder resection.[3] We report a 6-year-old male child with complaints of lower urinary tract symptoms and gross hematuria with bladder mass and histopathological diagnosis of eosinophilic cystitis.
CASE REPORT
A 6-year-old developmentally normal male child presented with complaints of acute-onset suprapubic pain during micturition, increased frequency and dribbling, and gross hematuria for the past 20 days. There was no history of fever, upper respiratory tract infection, retention of urine, or swelling of the body. He was treated as urinary tract infection (UTI), but symptoms did not subside, and he was brought to our center. On examination, there was no pallor or edema with normal blood pressure. On evaluation, his hemogram showed the presence of eosinophilia (22%), with an absolute eosinophil count of 1.9 × 109/L (hemoglobin – 12.3 g/dL, total leukocyte – 8.6 × 109/L, neutrophils – 22.3%, lymphocytes – 46.9%, eosinophils – 22.0%, monocytes – 7.6%, basophils – 1.2%, and platelet – 297 × 103/L). Renal function test was normal, and blood sugar was 100 mg/dL. Urine examination revealed 150–200 red blood cells/high-power field (RBCs/HPF) with no dysmorphic RBCs, 5–6 white blood cells/HPF, no albumin, sugar, casts, or crystals. Urine culture was sterile. There was no palpable mass on per abdominal examination, however, per rectal examination revealed smooth mass palpable at the tip of the index finger on the left side of the midline, and the overlying mucosa was free, mobile, and nonindurated. On detailed radiological evaluation, ultrasonography (USG) of the lower abdomen showed an asymmetric thickening of the left lateral wall of the urinary bladder (maximum: 19 mm) with mobile internal echoes. A contrast-enhanced computerized tomography of the abdomen and computerized tomography urography [Figure 1] showed asymmetric urinary bladder wall thickening along the left lateral and posterior wall of the urinary bladder suggestive of infectious or neoplastic etiology. In view of CT findings and the presence of peripheral eosinophilia with urinary symptoms, the possibility of rhabdomyosarcoma of the urinary bladder versus eosinophilic cystitis was considered, and urinary bladder biopsy was planned. Cystoscopy was carried out under general anesthesia, and findings were suggestive of mild bladder wall thickening on the left lateral wall and adjacent to the left ureteric orifice. Multiple punch biopsies were taken from near the left ureteric orifice to the left anterolateral bladder wall. The biopsy specimen showed denuded mucosa with edema, mild fibrosis, and moderate chronic inflammatory infiltrate with excess of eosinophils infiltrating the smooth muscle bundles in the lamina propria with mild capillary proliferation suggestive of eosinophilic cystitis [Figure 2a and b. The child was started on oral prednisolone and tapered and stopped over a period of 8 weeks. His symptoms subsided over a period of 4 weeks following steroid therapy and repeat follow-up USG of the lower abdomen done at 8 weeks showed no abnormal urinary bladder wall thickening and his hemogram showed no peripheral eosinophilia. On follow-up at 8 weeks, he is doing well with no urinary symptoms.
Figure 1.
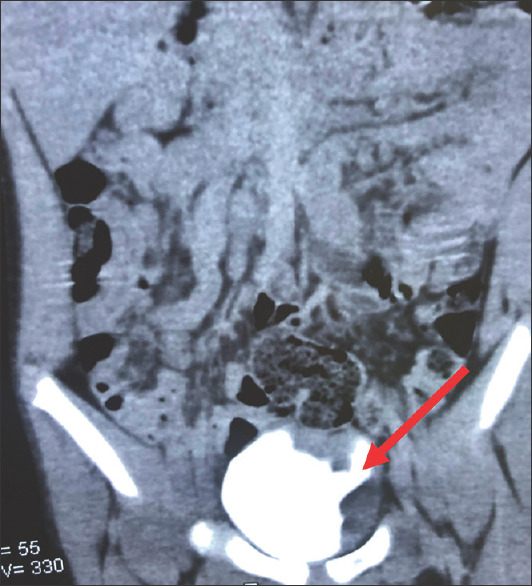
Computed tomography urography. CECT showing thickened bladder wall (Red arrow)
Figure 2.
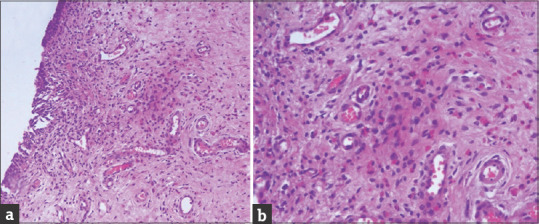
(a and b) Urinary bladder biopsy photomicrograph
DISCUSSION
While majority of the patients will present with lower urinary tract symptoms, they can also have a wide spectrum of clinical presentation such as bladder mass with hematuria mimicking malignancy, UTI, underlying allergic diseases such as asthma or allergic rhinitis, celiac disease, and viral infections such as infectious mononucleosis.[4] The imaging studies and cystoscopy findings of bladder lesions closely mimic bladder tumors and highlight the importance of performing a mandatory biopsy before an oncological diagnosis is made.[5]
Eosinophilic cystitis has been proposed to be due to immunoglobulin E-mediated activation of eosinophils secondary to an antigenic stimulus which results in mast cell degranulation, leading to the release of inflammatory mediators and damage to the bladder wall. The exact etiology is not known and many have postulated it to be due to an allergen inciting the anaphylaxis process. However, in our index case, there was no history of any allergy to food or environmental exposure. His clinical symptoms and blood investigations were suggestive of eosinophilic cystitis, however, as these symptoms are nonspecific, they can be often confused with nonspecific UTI.[5] Eosinophil count was significantly elevated in the index child, and it became normal after steroid therapy along with the resolution of his urinary symptoms.
The current treatment option ranges from supportive care, identification of an antigenic stimulus, medical management with antihistamines, steroids, immunosuppressants, and antibiotics to surgical management such as partial cystectomy and transurethral bladder resection.[3] The role of steroids as an anti-inflammatory agent has been emphasized in the literature though spontaneous resolution of symptoms has been reported. Immunosuppressants such as cyclosporine and azathioprine have been used if there is no response to steroids.
Dilatation of the upper urinary tract is a common complication encountered which can sometimes lead to temporary decline in kidney function. Our index case did not have any abnormality in the upper urinary tract. For localized lesions in the urinary bladder, surgeries such as transurethral resection and partial cystectomy have a good outcome. However, despite the improvement in the symptoms, recurrence still remains a risk. This emphasizes the importance of follow-up of these patients to detect the recurrence of the disease. A high index of clinical suspicion coupled with a mandatory histopathological diagnosis is important for the proper management and outcome.
CONCLUSION
Eosinophilic cystitis is a rare disease with a wide spectrum of clinical presentation. A mandatory biopsy of the urinary bladder is required to differentiate the disease from malignancy. It usually follows a benign course, although recurrence remains a possibility.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zhou AG, Amin A, Yates JK, Diamond DA, Tyminski MM, Badway JA, et al. Mass forming eosinophilic cystitis in pediatric patients. Urology. 2017;101:139–41. doi: 10.1016/j.urology.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Sparks S, Kaplan A, DeCambre M, Kaplan G, Holmes N. Eosinophilic cystitis in the pediatric population: A case series and review of the literature. J Pediatr Urol. 2013;9:738–44. doi: 10.1016/j.jpurol.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Ladocsi LT, Sullivan B, Hanna MK. Eosinophilic granulomatous cystitis in children. Urology. 1995;46:732–5. doi: 10.1016/S0090-4295(99)80313-6. [DOI] [PubMed] [Google Scholar]
- 4.Thompson RH, Dicks D, Kramer SA. Clinical manifestations and functional outcomes in children with eosinophilic cystitis. J Urol. 2005;174:2347–9. doi: 10.1097/01.ju.0000180423.06285.72. [DOI] [PubMed] [Google Scholar]
- 5.Thijssen A, Gerridzen RG. Eosinophilic cystitis presenting as invasive bladder cancer: Comments on pathogenesis and management. J Urol. 1990;144:977–9. doi: 10.1016/s0022-5347(17)39638-6. [DOI] [PubMed] [Google Scholar]


