Abstract
COVID-19 encephalitis is a rare condition usually presenting with altered mental status. Simultaneous presence of anti-NMDAR antibody and SARS-CoV-2 virus in CSF is a very rare condition described in a few case reports so far. On the other hand, brain edema is an unusual presentation of anti-NMDAR encephalitis. Herein, we reported a case with simultaneous detection of anti-NMDAR antibody and SARS-CoV-2 virus in her cerebrospinal fluid (CSF) presenting with brain edema, altered mental status, seizures, and respiratory symptoms.
Keywords: Autoimmune, COVID-19, Encephalitis, Seizures
Case report
An 18-year-old girl with no medical history was admitted on June 22, 2020, to the emergency room of Ghaem hospital, Karaj, Iran, with generalized tonic–clonic seizures. She had a 3-week history of mood change as depression and anhedonia accompanied by lack of concentration, low-grade fever, dry coughs, and shortness of breath. Her respiratory symptoms were aggravated after the initiation of seizures. Despite the initiation of sodium valproate, she had a second episode of tonic–clonic seizures. At initial evaluations, she had a 38.7 °C axillary fever, 100/60 mmHg blood pressure, pulse rate of 106, respiratory rate of 20, oxygen saturation of 90%, bilateral pulmonary crackles in lower lung zones, a confused state, minor meningismus, and neck stiffness. She did not have any other neurological symptoms such as papillary edema, cranial nerve palsy, and focal neurological deficit on the neurological exam. Initial brain and lung CT scans are showed below (Fig. 1).
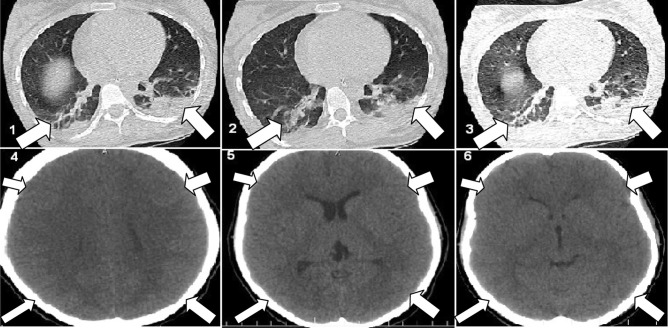
Fig. 1.
Pictures 1–3 show peripheral ground-glass opacities and consolidations in lower lung zones. Pictures 4–5 show generalized brain edema
Meanwhile, her level of consciousness was deteriorated so she was undergone lumbar puncture and transmitted to ICU and started on broad spectrum antibiotics and acyclovir. CBC showed a WBC of 13,900 with neutrophilia (87%) and lymphopenia(10%). C-reactive protein was 2+ . According to these findings, she was started on Remdesivir, Lopinavir/Ritonavir, and interferon b1a (Resigen). A day after, CSF analysis came back as appearance: semi turbid, color: light pink, WBC: 27, RBC: 1997, lymphocytes: 93%, PMN: 7%, glucose: 55 mg/dL, protein: 241 mg/dL. HSV1&2 DNA PCR also came back negative in CSF. No improvement in mental status and level of consciousness was seen in first 3 days but the seizures were controlled. At this time, an MRI was performed to have a closer look at the brain which came back normal and the brain edema was resolved (Fig. 2) so, she did not receive any specific treatments for the brain edema such as mannitol or hypertonic saline. Interestingly, her CSF PCR came back weakly positive for COVID-19. NMDAR antibody in CSF also came back positive in accordance with the result of indirect (transfected cells) immunofluorescence test (IIFT kit, EUROIMMUN Co., Lubeck, Germany). Therefore, she was started on IVIG (25 g/day). Her consciousness started to improve after 48 h of IVIG treatment. One week after admission, the blood and CSF cultures came back negative. Therefore, she was stopped on intravenous antibiotics and started on methylprednisolone (2.5 g/5 days) and then tapered using oral corticosteroids. In the same time, her IgM for COVID-19 came back positive. After 2 weeks of admission, she was discharged from ICU and neurology service with normal consciousness. During hospitalization, her respiratory symptoms were mild and she did not show severe problems with oxygenation; therefore, there was no need to mechanical ventilation for the patient. After 2 months of hospitalization for completing COVID-19 treatments, she was discharged with full recovery.
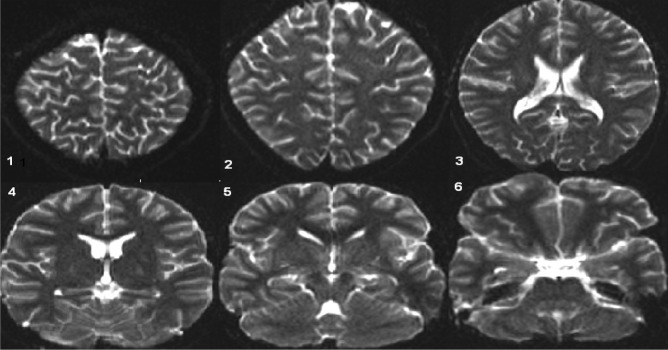
Fig. 2.
Normal brain MRI. Pictures 1–6 show the brain edema has been resolved
Discussion
Neurological symptoms of COVID-19 are caused by nervous system directly affected by the virus or immune-mediated para-infectious conditions (Romero-Sánchez et al. 2020; Helms et al. 2020; Moriguchi et al. 2020). Anti-NMDAR encephalitis has been reported in few cases of COVID-19 before (Panariello et al. 2020; Monti et al. 2020; Burr et al. 2020). On the other hand, brain edema which is an unusual finding in anti-NMDAR encephalitis has also been rarely reported in COVID-19 patients (Coolen et al. 2020; Kadono et al. 2020). In this case, we had simultaneous presence of SARS-CoV-2 RNA and NMDAR antibody in CSF accompanied by generalized brain edema which is rare, and to our knowledge, it has never been addressed so far. Although many new insights have been provided in regard to the pathogenesis of COVID-19, precise interactions between virus-host cells remain unclear. Indeed, the integration of new emerging sciences will help us to fight COVID-19 disease and related complications more efficiently in the future. (Mohammadpour et al. 2021; Mirzaei et al. 2020a; Heiat et al. 2021; Mirzaie et al. 2020b).
Acknowledgements
We would like to thank the Clinical Research Development Unit of Baqiyatallah University of Medical Science for their kindly cooperation.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fakhri Allahyari and Ramin Hosseinzadeh contributed equally as first authors.
References
- Burr T, Barton C, Doll E, Lakhotia A, Sweeney M (2020) NMDA-receptor encephalitis associated with COVID-19 infection in a toddler. Pediatric Neurol [DOI] [PMC free article] [PubMed]
- Coolen T, Lolli V, Sadeghi N, Rovai A, Trotta N, Taccone FS, et al. Early postmortem brain MRI findings in COVID-19 non-survivors. Neurology. 2020;95(14):e2016–e2027. doi: 10.1212/WNL.0000000000010116. [DOI] [PubMed] [Google Scholar]
- Heiat M, Hashemi-Aghdam MR, Heiat F, Rastegar Shariat Panahi M, Aghamollaei H, Moosazadeh Moghaddam M, Thozhukat Sathyapalan, Reza Ranjbar, Sahebkar A (2021) Integrative role of traditional and modern technologies to combat COVID-19. Expert Review of Anti-infective Therapy 19 (1):23–33 [DOI] [PubMed]
- Helms J, Kremer SŠ, Merdji H, Clere-Jehl Rl, Schenck M, Kummerlen C et al (2020) Neurologic features in severe SARS-CoV-2 infection. New England J Med [DOI] [PMC free article] [PubMed]
- Kadono Y, Nakamura Y, Ogawa Y, Yamamoto S, Kajikawa R, Nakajima Y, et al. A case of COVID-19 infection presenting with a seizure following severe brain edema. Seizure. 2020;80:53. doi: 10.1016/j.seizure.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirzaie A, Halaji M, Dehkordi FS, Ranjbar R, Noorbazargan H (2020a) A narrative literature review on traditional medicine options for treatment of corona virus disease 2019 (COVID-19). Complementary Therapies in Clinical Practice 40:101214 [DOI] [PMC free article] [PubMed]
- Mirzaei R, Karampoor S, Sholeh M, Moradi P, Ranjbar R, Ghasemi F (2020b) A contemporary review on pathogenesis and immunity of COVID-19 infection. Mol Biol Rep 47 (7):5365–5376 [DOI] [PMC free article] [PubMed]
- Mohammadpour S, Torshizi Esfahani A, Halaji M, Lak M, Ranjbar R (2021) An updated review of the association of host genetic factors with susceptibility and resistance to COVID-19 J Cell Physiol 236:49–54 [DOI] [PMC free article] [PubMed]
- Monti G, Giovannini G, Marudi A, Bedin R, Melegari A, Simone AM, et al. Anti-NMDA receptor encephalitis presenting as new onset refractory status epilepticus in COVID-19. Seizure. 2020;81:18. doi: 10.1016/j.seizure.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Nakao A (2020) A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. International Journal of Infectious Diseases [DOI] [PMC free article] [PubMed]
- Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M et al (2020) Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: a case report. Brain, behavior, and immunity [DOI] [PMC free article] [PubMed]
- Romero-Sánchez CM, Díaz-Maroto I, Fernández-Díaz E, Sánchez-Larsen Á, Layos-Romero A, García-García J, et al. Neurological manifestations in hospitalized patients with COVID-19: a retrospective. The ALBACOVID Registry: observational study from a Spanish population; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]