Abstract
Addressing patients’ social determinants of health via community resource referrals has historically been the primary domain of social workers and information and referral specialists; however, community resource referral platforms have recently entered the market. We lack an account of the process of community resource referrals and the role of technologies within it. Using sociotechnical systems theory, we analyze data from 12 focus groups (n=102) with healthcare providers, and community organization staff and volunteers in Metropolitan Detroit to describe the process of community resource referral. Findings reveal a deeply sociotechnical process including the following steps: assessing patients’ social needs; choosing appropriate referral sources; and facilitating connections. We characterize the importance of knowledge and skills, personal relationships, interorganizational networks, and data sources such as service directories in the referral process. Findings suggest that digital platforms may augment referral functions, but should not be seen to replace interpersonal work, relationships, and interorganizational networks.
Introduction
Social determinants of health (SDOH) account for up to 80% of the individual variance in health outcomes. SDOH are those conditions in which individuals are born, live, and work.1 Factors associated with negative health outcomes, such as food insecurity or housing instability, are referred to as “social risk factors.”1 From a patient’s perspective, “social needs” are the most pressing social risk factors, taking into account specific preferences and priorities.1 To address patients’ social needs, working together with patients, healthcare providers may offer social care, including referrals to community social service agencies such as food pantries or temporary housing.2 By screening patients for social risks during routine healthcare, providers can systematically identify their social needs and provide subsequent social care via referrals to social services for necessary resources, potentially improving patient health outcomes.3
Information and referral (I&R) services, such as that provided by the national 211 helpline operated by the nonprofit United Way in North America, maintain information about community resources and coordinate referrals to connect patients to healthcare resources or social services agencies.4 Information and referral professionals, who may receive the Certification for I&R Specialists (CIRS) credential from the Alliance of Information and Referral Systems (AIRS), routinely maintain and update databases of services, assess patients’ needs, identify relevant resources to meet these needs, and provide referrals to chosen resources.4,5 In addition to I&R professionals primarily working in the nonprofit sector, larger healthcare organizations have also employed social workers, and increasingly patient navigators and community health workers, whose responsibilities may include community resource referrals.
Furthermore, aligned with the increase in social risk screening in healthcare organizations in the United States (US),6 there are now at least eleven technological platforms, including Aunt Bertha and Healthify, designed to identify community social service agencies and facilitate referrals to these organizations.7 Community resource referral platforms features include databases that serve as social service agency directories, sending referrals to community organizations, tracking post-referral outcomes, integrating with electronic health record (EHR) systems at healthcare organizations, suggesting resources based on social risk screening results, and generating analytic reports.7 While such platforms may increase awareness of social service agencies, these tools may have important limitations, namely, insufficiently frequent directory updates, limited interoperability with various EHR vendors or limited compatibility with agencies with minimal technological capacity, and prohibitive costs for smaller agencies.7 As a result, community resource referral platforms alone may be insufficient to ensure that patients get connected to necessary services. Moreover, little is known about the pre-existing processes of community referrals into which new systems are being introduced, which is necessary to achieve the ideal of “joint optimization” of social and technical systems.8 Using focus groups with social service agency staff, healthcare providers, and community leaders conducted before many of the tools on the market became available, we explore how healthcare and social service providers accomplished community referrals across the full cycle of steps, from identifying needs to completing the referral. Using sociotechnical systems as a theoretical framework, we cast analytical attention upon the social subsystem and its role alongside technologies and processes in accomplishing community referrals. Ultimately, we argue for a sociotechnical approach to designing systems intended to support community referral; that is, social and technological subsystems should be jointly optimized. Building on prior work in community I&R services and sociotechnical systems theory, this paper addresses the following research questions:
How do providers and staff assess patients’ needs? What is the role of social, technical, and external environmental subsystem elements in this work?4,8
How do providers and staff choose referral sources to meet patients’ needs? What is the role of social, technical, and external environmental subsystem elements in this work?4,8
How do providers and staff facilitate or restrict referrals to social service agencies and resources? What is the role of social, technical, and external environmental subsystem elements in this work?4,8
Theoretical Framework
Because community resource referrals rely on both the social relationships of I&R professionals and information resources, sociotechnical systems (STS) theory is an appropriate lens through which we consider community resource referrals, as it suggests that organizations are work systems made up of two independent but interacting systems: the social subsystem and technical subsystem (Figure 1).8,9 STS theory is a reminder that objects of design in informatics go beyond technology and into the social subsystem, including workflows and rules. The social subsystem is made up of people and their knowledge, skills, and values, relationships, and incentive and authority structures. The technical subsystem comprises technology, tasks, and processes.10 The two subsystems interact to produce the output of the work system; they also result in the level of work performance. In their ideal form, STS result in joint optimization of the human and the technological aspects of the overall system while accounting for the constraints and influences of the external environment subsystem, which may include factors such as interorganizational networks.10,11 Sociotechnical systems theory is used to describe and explain organizational performance, and in the tradition of the Tavistock Institute, to design new technologies and organizational processes. We use it to characterize community resource referrals as a work system in which elements of each subsystem contribute to the completion of referrals.
Figure 1.
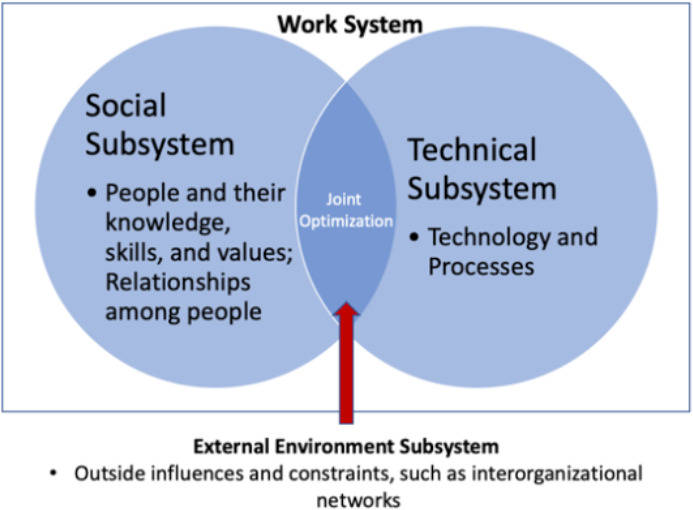
Sociotechnical Systems Theory (Adapted from Militello et al.8)
Methods
As part of a larger community-based participatory research (CBPR)12 project conducted in partnership with the National Kidney Foundation of Michigan (NKFM), we conducted 12 focus groups with 102 healthcare, service provider, and community leader participants. Focus groups were conducted in three high-poverty, predominately African-American cities in southeastern Michigan: Detroit, Inkster, and Flint. In each city, a community advisory committee (CAC) consisting of representatives of 4-6 organizations was established. These CACs reviewed and provided input on study instruments, including focus group discussion guides and demographic surveys. NKFM staff and CAC members identified and recruited participants from various organizations, primarily through community-wide, multidisciplinary health coalitions focused on preventing and managing diabetes, hypertension and kidney disease. NKFM had formed coalitions in each of these areas with project funding from the Centers for Disease Control and Prevention (i.e., Inkster Partnership for a Healthier Committee, Detroit Community Against Diabetes, Flint – Better Health Together; these have been described elsewhere).13,14 Participants were recruited through emails, phone calls, and announcements at meetings. Inclusion criteria included being a staff member, trainee, or volunteer at a local organization relevant to SDOH, including healthcare organizations, public health organizations, nonprofits such as food pantries or health promotion organizations, businesses such as healthcare suppliers or pharmacies, schools, churches, libraries, block clubs, law enforcement, community mental health services, and services for children or older adults. Focus groups were led by NKFM staff and University of Michigan researchers, conducted at public libraries and nonprofit community organizations, and lasted two hours on average. Participants received a $20 honorarium for their participation. Each focus group conversation was directed using a semi-structured discussion guide. Participants were asked to complete a brief demographic survey. Focus group discussions were audio recorded and professionally transcribed. Transcripts were initially analyzed using an iterative process coding approach incorporating deductive codes based on steps in the referral process identified in the extant literature5,7 and inductive codes using NVivo qualitative data analysis software.15 Following this, two researchers used the codebook to independently code the full transcripts; the Cohen’s kappa for the coding was 0.84, indicating excellent agreement. Following coding, memos were written to further synthesize the coded data and aggregated into a cross-case, time-ordered display.16
Results
Characteristics of Participants
Focus groups were held in Flint, Inkster, and Detroit, with Flint representing the largest proportion of participants. African-American participants were the largest group, followed by White participants. Participants had high levels of educational attainment, with 64.71% having at least an associate degree. Many were employed full time (42.16%), but nearly a quarter were retired or on disability benefits. Such individuals primarily served as volunteers at nonprofits such as churches and faith-based ministries.
Process of Community Resource Referral
As Figure 2 shows, findings revealed three major steps involved in community resource referral, producing the output of a completed referral. These steps are outlined below, alongside their attendant sub-tasks. For each sub-task, we describe the role of the social subsystems (people, personal relationships), technical subsystems (technologies), and external environmental subsystem (interorganizational networks).
Figure 2.
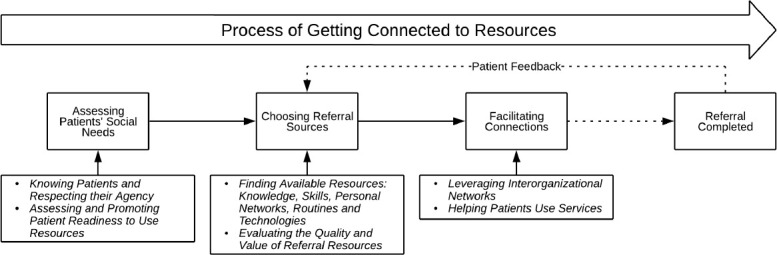
Process of Connecting Patients to Resources
Assessing Patients’ Social Needs
Knowing Patients and Respecting their Agency
Assessing patients’ social needs is an essential part of connecting them to resources (Figure 1). This process primarily involved interactions between people, and over time, resulted in knowing patients through interpersonal relationships (People, Social Subsystem). One nonprofit staff member described providers’ need to know enough about a patient to translate that knowledge into an understanding of their needs: “You need enough about them to help them navigate the system to get to what they need.” Knowing patients requires going beyond health needs to learn about social and financial circumstances: “You need to know about the person, you need to know about where they are and what their circumstances are because you can’t give them the best advice… if you don’t start with where they are.” Knowledge of the patient could be developed through designated tasks that were part of healthcare encounters: “When a physician does their family health history or their individual health history, that’s the time where you can get a lot of that information.” However, participants emphasized the difficulty of not having sufficient time and care continuity to build knowledge-sharing relationships with patients during healthcare encounters17: “Most of these doctors have not been with the patient for any length of time. They’ve just come into contact with them or they’re rotating in and out of residencies. So there is really no long-term knowledge base or relationship with the patient so what you’re getting is a lot of guessing most of the time.” Aside from records acquired during history taking, this knowledge appeared to be something which clinicians and social service providers primarily kept “in their heads.”
Respect for patients expressed the values of some people involved in providing referrals and was enacted through dialogue with patients (People, Social Subsystem). For example, one participant described the need for healthcare providers to let patients identify the problems they were experiencing, recognizing the agency and motivation of the patient rather than pressing them to make changes: “I think that when we refer it’s because they brought a problem to us, so they’re generally appreciative of that… So it’s not us saying ‘you need to do this’ but rather ‘we perceive this as a problem, do you agree?’ and then ‘here’s some resources available that might help you.’ So it’s really generated from them, not us.” Trust between patients and staff/providers was seen as an important facilitator of patient information sharing: “Trust allows them to share these needs with us.” Patient trust was thought to be built over time and cumulative encounters, as one nurse ambulatory coordinator explained: “Their first visit, their guard’s up and they’re apprehensive and they’re scared and they’re overwhelmed and they’re kind of ‘I’m not gonna do this.’ But really it does have to do with time that you spend with those patients and then they earn your trust and boy! We’ve really seen some people come around. So it definitely needs to be more than one interaction….” Without trust, patients may resist disclosing sensitive information, such as information about finances, that may facilitate referrals: “There is a segment…who want nothing to do with free services or whatnot because they don’t want to have to tell you all their business, they don’t want anybody to know how much money they have.” As a result, providers often have to work without this information or make inferences (People, Social Subsystem), as one respondent explained: “We have to be the psychics most times because they’re not gonna be just forthcoming with that information.”
In some cases, participants believed, clinicians may do a poor job of assessing patient needs by resorting to negative judgments or biases: “or the physician does not open them up to the resources in this area because they don’t feel that they deserve it... it’s a judgment call that they’re actually judging the person based on what they see in that five minutes versus an hour walking in their shoes.”
Assessing and Promoting Patient Readiness to Use Resources
Focus group participants believed that patients’ readiness to seek and use a resource is an important precursor to the use of a community resource; accordingly, they described assessing patient readiness. Participants identified a variety of components of patient readiness. First, patients must be ready to share information about their social needs with providers (People, Social Subsystem) in order to receive information or referrals to resources: “I don’t think they bring a lot of the issues to us per se in my experience in my clinic. But if I hear of an issue then I offer [a resource] and put it in their hands. If they want it and when they’re ready, they’ll use it or not.”
Patients must be ready to accept the help that a resource may provide, which may lead to delays in use. A healthcare provider explained, “We let them know there’s a social worker available to speak to in our clinic. And if they’re ready to talk they’ll say okay. But if they’re feeling overwhelmed, they usually just don’t access that resource until they’re ready for it….” Patients may also face competing demands that prevent use of a resource, which may also result in delays. One healthcare provider advocated following up to promote resource use in such instances: “They do have a lot of other stuff going on… So I think the follow up and the community would be very beneficial.”
Participants indicated that patients may even actively resist using available community resources due to negative connotations—for instance, support groups may be seen as resources for people with problems—or due to negative experiences with organizations or parts of the healthcare system, as one participant explained (People, Social Subsystem): “I have a friend and she just doesn’t like doctors… she just refuses to go… She just says ’all doctors are like this’ because she’s had bad experiences with a person. [One bad experience] will definitely make them think twice about going to something similar or going to somebody similar.” Thus, participants indicated that persuasion was sometimes needed: “When we talk, we be referring, we be pushing, we be like ‘c’mon, go!’”
Choosing Referral Sources
Finding Available Resources: Knowledge, Skills, Personal Networks, Routines and Technologies
Once patients’ needs are identified, providers must find the most appropriate community resources to address those needs (Figure 2). This step was facilitated in part by the attributes of referral providers (People, Social Subsystem) in terms of their knowledge of resources and skills at finding them, as well as the technical subsystem in the form of processes of routine referrals for recurring needs and technologies in the form of resource directories and resources found on the Internet.
Providers may be more effective at referring patients to resources if they themselves have baseline knowledge of available resources that are needed on a regular basis (People’s Knowledge, Social Subsystem): “The competent healthcare provider would also know where to refer their patients for additional help and education, realizing that there are other competent healthcare providers in the area that can add to their education.” Knowing about resources includes knowing where medications are available for free or at discounted rates: “Our doctors do know to prescribe only the $4 medications.” In some organizations, there was also a staff role which was charged with maintaining knowledge of available community resources: “[the social worker] knows all the resources…” Another individual recalled that their organization “hired a social worker … she knows all the resources. She works in Flint. So with that she knows where everything is.” Patient navigators also played this specialist role in some organizations. Part of this involved knowing about specific eligibility requirements for some services and their availability depending on patients’ health insurance. For instance, one participant observed, “As far as getting transportation…some insurances…offer the transportation.” Another provider explained, “A lot of the clientele does not know their Medicaid/HMO has transportation resources for them so we frequently identify that resource for them. There’s the bus service, there’s YourRide. I think those things are pretty plentiful here in Flint….”
However, participants complained about a lack of knowledge among some healthcare providers in their communities, which resulted in patients not receiving needed referrals (People’s Knowledge, Social Subsystem). Physicians may be unable to refer patients because they may be unaware of resources: “The physicians don’t know or either don’t refer in a timely manner…. If the physician community isn’t also engaged in some of these educational processes we still have a problem.” One explanation for providers’ lack of awareness of resources is that many do not have a professional focus on referrals to resources: “It is not their job to wonder about…low-cost pharmacies….” Social service staff members described the need to advertise resources to physicians to raise awareness, which was “a challenge…from a program perspective, other than advertising to the physicians, which I’m pretty sure we all do.”
Personal connections and experiences were critical to creating knowledge of resources (People & Relationships, Social Subsystem): “I think it’s individuals and relationships, who you personally know, who you’ve worked with, who you like. So, two ways. We have a resource guide but then we also have people we know that we have worked with that we know might help with this thing.” One respondent described how they learned about free medications available at a local grocery store through their brother: “My brother [works at the grocery store] and he got [free medication] and he let me know, that’s how I found out.”
In terms of the “organization” part of the social subsystem, some participants described routine selection of sets of referrals in response to common social needs among patients, including transportation and low-cost pharmaceuticals. For example, one provider described recurring referrals made to help patients acquire medication and supplies.
Technologies facilitate information sharing across interorganizational networks, a key part of the external environment subsystem. In particular, local email lists for people working in a given sector facilitated awareness. One respondent described their organization’s efforts to send information via email to caseworkers, who in turn relayed this information to clients: “We send information through various LISTSERVs, or can be people working in various health arenas or case workers, because our case workers are working directly with their clients, so any time there is anything useful... It gets pushed to at least the case workers... There's always a constant flow of information coming to them that they can then, if the opportunity arises, pass along to their clients.” Paper-based resources were also part of the technologies that supported interorganizational networks (Technology, Technical Subsystem). One participant described leaving flyers for their program on the reception desk of primary care providers’ offices: “Most of the PCPs in the area allow me to drop off my flyer to leave on their reception desk about our classes.” Sharing information with other providers and organizations may enable that information to be incorporated into other organizations’ referral work. Occasionally, interorganizational communication did not occur, resulting in a lack of information sharing. One respondent described the need for improved communication between organizations: “[Some] agencies and groups in the community… have their own mission, they are seeking to use their vision in the community. And they’re not collaborating at all with individuals or organizations in the community to share or to provide information.” Participants indicated a need for more interorganizational communication between organizations of all types: “Venues around Inkster need to start communicating with each other what’s going on.”
Some organizations attempt to provide education and informational tools (Technology, Technical Subsystem) to physicians to facilitate awareness of resources and subsequent referrals: “One of the things we’ve done… is create the Green Book and send it to all the physicians and provide education to physician groups about what’s available in this community. The Green Book is a listing of all the physical activity and nutrition education programs geared towards children and families… it was created was because we heard from our health insurance partners that the physicians didn’t know where to provide referrals for their patients that needed help.” In some cases, social service agency staff may use multiple directories to identify resources: “We have a community resource list that we generated and also the Greater Flint Health Coalition has put one together.” However, keeping printed directories up to date with sufficient information about accessing services was considered challenging: “There is a booklet of listings of all the free and low-cost health services in Wayne County, however I think it’s only printed like once every so many years and by the time it comes truly into print the clinic is closed.”
The technical subsystem may also provide knowledge of available resources in the form of resource directories, such as the United Way’s 211 service, as one participant explained: “We can send ‘em to get information as far as United Way, we also... give them resources for cheaper supplies and medications. Some options for them to discuss with their doctor.” One respondent described their process for determining how best to refer a patient, indicating the need for better informational resources (Technology, Technical Subsystem): “It depends on what the question is and what they’re looking for. If they need health care… we’ll usually refer them to 211 or if you have to, go to the ER, they have to treat you, even if you can’t pay, but it usually is not that urgent… if it’s not directly health-related… we can make some referrals for that too, so, but again there’s definitely a need for more information about the resources that are out there.” Informational tools, including physical information displays and hospital phone directories, were seen as valuable resources (Technology, Technical Subsystem): “We have racks in all of our education rooms with community resources where they can go like brochures… a lot of times that triggers for our patients to say something to us because we’re offering the information and what kind of resources they do need.”
Participants in the three cities articulated a need for “some type of database,” in the words of one participant (Technology, Technical Subsystem). Such a database may be populated with details about the availability of healthcare providers and community resources, including services offered and pricing. It could feature tagging for relevant diseases or circumstances, allowing for rapid identification of relevant resources, as one respondent described: “Put all the information free clinics, free meals, this physician will take X amount of people, these are open a certain amount of days, this is for almost low cost, this is gonna cost you $40, and this is a sliding income scale, as much information as we can.” However, participants complained that most directories featured missing information: “And besides they don’t print all the information about the various clinics like how much you have to have or is it based on income or things like that.”
Providers might do individual research to identify relevant resources for patients, which reflected both the skills of people (people, social subsystem) and available data on the Internet (Technology, Technical Subsystem). Some providers kept lists of resources based on their own research: “We also have a resource list. But I think sometimes we get stuck in a rut in our profession… So I like to have a list of mental health resources available and also support groups.” Identifying affordable sources of medication was also a major research task in healthcare organizations.
Evaluating the Quality and Value of Referral Resources
Participants felt a responsibility to facilitate access to community resources that offered high-quality services. In part, this was because patient experiences with organizations to which they were referred reflected on their own organizations, and them as individual providers. One said, “If you can’t give a good referral or you don’t know how to refer, people gonna lose confidence real quick. It’s a challenging proposition, but I would just say you need to really really learn the community more than anything.”
Locating reputable community resources required additional groundwork to verify quality: “Any information you get, once you get it, you check it out. You could call the number and if they said, ‘yes we can help you, no we can’t.’” Verification included asking patients about “success stories” and experiences using a given resource (People, Social Subsystem): “We always try and listen to people when they go and find out if it was a good place.” Quality assessment involved both social and external environmental subsystems, often incorporating a patient feedback loop (Figure 2).
Trusted referrals may also be made based on personal relationships (Relationships, Social Subsystem) such that staff and volunteers relied on personal connections to identify high quality resources: “If somebody has kidney disease and they were like ‘what do I do?’ I would be like ‘Oh! You should probably talk to [name of nonprofit employee] she can help you.’ I’d look for a person that I knew and trusted, that had expertise in that area.” Staff and volunteers may even leverage connections with patients for information about resources: “I’ve had patients tell me about resources in the community too, so then I add those to the list, or she says I’m telling them something wrong, so the education goes both ways.”
Staff and volunteers may also look to the Internet for information (Technology, Technical Subsystem), though this was described as less desirable due to a lack of personal experience with the quality of the resource: “I would probably be a little bit cautious of just looking something up on the Internet because I don’t know the programs… what if it’s a terrible program? And then they quit it and then they are like ‘Oh I went to one of those programs it was horrible so I’ve never doing it again,’ so I’d rather call somebody that I know….”
Some healthcare staff members suggested that information needed to make referrals was available to providers, but that the determinant of the use of this information was whether the provider valued the resource (Peoples’ Values, Social Subsystem): “[Information is] out there! But it all goes back to valuing. If they are looking for it, I think they can find it because for all the collaboratives and relationships with all the hospitals with all the community organizations partnerships that’s why they were established was to share all that information.”
Facilitating Connections
Leveraging Interorganizational Networks
Leveraging interorganizational networks may help to facilitate referrals to resources (External Environment Subsystem, Figure 2). In particular, community coalitions and networks that met regularly created mutual awareness of services. As one nonprofit worker explained, “Through all our collaboratives we learned about [a local university] extension… I think we do a pretty good job of communicating internally, communicating externally.” Participants showed how organizations build interorganizational communication, referral, and information sharing networks: “If [patients] are looking for it, I think they can find it because for all the collaboratives and relationships with all the hospitals and with all the community organizations partnerships that’s why they were established was to share all that information.”
Interorganizational networks may facilitate patient first contacts and their intake by organizations. Staff may help by making phone calls to ensure that people are accepted by a service: “I would make the call for ‘em as far as getting transportation because some insurances they offer the transportation.” For instance, staff members and providers may help patients by filling out forms: “We have one nurse who does nothing but find free medication from the pharmaceutical companies. All pharmaceutical companies have a free option in there but they’ll give you a stack of papers like this to fill out in order to get that patient into their system for free medication. But she does it anyway” (People’s skills, Social Subsystem; Technology, Technical Subsystem; External Environment Subsystem).
Additionally, interorganizational networks may help patients use services. This included helping people understand when and where to get services, as well as making sure people could timely access to a specific resource: “If I think they are personally in a state where they really need health evaluation right away, I’ll figure out a way with the secretaries to get them in without having to wait 3 or 4 weeks.” Where necessary, staff may facilitate referrals by accompanying patients to visits to resource providers: “We don’t just send them along, we take them with us.”
Helping Patients Use Services
Participants described a need for both patients and providers to know how to navigate the healthcare and social service system in order to get connected to necessary resources (People’s Knowledge, Social Subsystem). To begin, it was seen as important that patients know of available resources: “The actual call to the clinic and... making the connection... that goes back to navigating the system, the whole idea of navigating the system how do you find what you need if you don’t have access to all of the information?” Having enough information to get started was seen as a potential obstacle: “Not knowing where to get started is a big part… but also not knowing what’s out there and what’s available.” Knowing how to navigate the system may be challenging for patients, as one respondent explained: “People have a very difficult job just trying to navigate the whole system and trying to get what you need.” Navigating the system was seen as challenging in part due to the lack of a coherent inter-organization service system that could help patients understand how to access resources: “There isn’t a real good structure there that’s a foundation that even talks about when you can even give them resources [or] how they use them [or] who helps them integrate them.”
A patient may face additional barriers once in the system when seeking resources (External Environment Subsystem). First, accessing resources may take much time, as one respondent explained: “The length of time it takes to get through the system is difficult. I’ve signed up for the county health plan and it was a lot of ‘fill this out and come back (laughs) and fill this out and turn this in.’” Filling out paperwork and other administrative time demands may be additionally burdensome to patients who work multiple jobs. One individual described being unable to complete a process: “I gotta leave my place in the line at the health department and go get on the bus so I can go to work on time.” Literacy, perseverance, access to transportation, and having a valid driver’s license were indicated to be other prerequisites (and potential barriers) to accessing social services.
Patient navigators may help patients by facilitating connections between patients and relevant resources; this work requires longer-term personal relationships with patients and navigator knowledge and skills (Social Subsystem), technologies such as telephones, email and record-keeping systems (Technical Subsystem), and interacting with outside organizations (External Environment Subsystem). For patients who require developing a long-term care routine, providers may assign a patient navigator to support the patient and ensure they stay on track, as one respondent explained: “The primary physician then says to the nurse ‘this person needs to be followed; [they] need to have some support.’” Patient navigators may help patients overcome barriers, as one individual explained in a story about a diabetes patient who received help from a navigator: “She figured out what all these barriers were, she got all of his ‘scripts lined up, she got them all in mail order, she got him discounts … in exchange she says now ‘you… give me a sugar reading once a day…’ for someone who’s just diagnosed…, it gives you a basis and a foundation.”
While participants worked hard to overcome referral barriers, participants also suggested that patient initiative was needed: “[Patients have] got to do their part too. I mean we’re here, we’re helping, but people have to value it and take responsibility and accept the help that’s out there. I think that’s a stumbling block for us now.” Participants described a distinction between knowing about resources and actively seeking them out, suggesting that making the effort did not always happen: “Most of the time we can’t make folks. It’s the action part. Just because we know all this knowledge and we done gave it to them, they still don’t make a move to do anything with it.”
Discussion
This study used STS theory to describe the key steps involved in the process of connecting patients to resources in the community, as well as the roles of components of the social, technical, and external environment subsystems which make up the sociotechnical community resource referral work system. Assessing patients involves patient-provider communication to elicit patients’ social needs and determine patients’ readiness to use the resources to which they are referred. Primarily, this involves elements of the social subsystem. Choosing a referral source requires finding resources and evaluating their quality in order to make the best choice for patients. Finding resources involved all subsystems, although quality assessment occurred primarily in the domain of the social subsystem. Finally, personal relationships (social subsystem) and interorganizational networks (external environment subsystem) were most prominently engaged in facilitating connections between patients and resources. Communication technologies such as email lists, telephones, and flyers played a role but were less prominent than in choosing referral sources.
This research emphasizes the importance of the social and external subsystems in the work completed by community service, church volunteers, and healthcare providers to refer patients to community resources. As potentially part of the technical subsystem, community resource referral platforms offer useful functionalities, including maintaining resource directories, managing and tracking referrals, offering case management services, providing analytics and reports, screening for SDOH, and automatically suggesting resources, which emulate and potentially automate existing capacities of I&R specialists, and healthcare and community organization staff and volunteers.5,7 While automating these capacities may create efficiencies of volume and speed, it cannot replace the role the personal and external subsystems in the process, such as gaining interpersonal trust that may be required to elicit disclosure of social needs, and helping people with acute needs get appointments at another organization more quickly than “rules” permit. Given the importance of non-technical subsystems in community referrals, attempts to offload work onto technologies such as referral platforms may introduce new challenges that necessitate the continued participation of people in referrals.
Findings showed that the assessment of patients is a complex interpersonal task involving assessing patients’ social needs and readiness to act on those needs. Current standardized SDOH screening tools may be used to automatically assess patients’ social needs and prompt digital worflows;18 furthermore, they may help to address possible healthcare provider bias against some patients. However, previous research has shown that the sole use of standardized tools to screen patients for social needs may result in failure to capture narrative information about a patient, which is important to understanding a patient’s social needs and how to address them, including the patient’s readiness to use a resource.19 Community organization staff or volunteers, healthcare providers, and I&R specialists may be uniquely qualified to capture and evaluate contextual narrative information while respecting patients’ agency, resulting in more accurate assessment of patients’ social needs and readiness. Moreover, as participants outlined, the trust and care continuity that develops in the context of longer-term relationships, and the resultant phenomenon of “knowing the patient,” may result in more disclosure and more support for patients in developing readiness to use resources. However, there may be components of readiness assessment for which digital tools are well suited. For example, some screening tools ask patients if they want help with their social needs.20 More extensive assessment tools could also be developed, building up the technical subsystem and allowing for joint optimization to occur.8 Furthermore, persuasive technologies have been shown to promote health and wellness behaviors, including physical activity, smoking cessation, and healthy eating,21 suggesting the potential for use of these technologies to help patients follow through with resource use. Persuasive technologies may thus aid in enhancing patient readiness and improve resource use outcomes. While these technologies may offer value, the technical subsystem alone cannot fully substitute for the work of the social subsystem; joint optimization is necessary to leverage their combined strengths.
Similarly, the process of choosing referral sources may benefit from human-computer collaboration. A strength of community resource referral platforms is their potential for maintaining comprehensive and frequent agency directory updates. However, depending on the frequency of updates and the accuracy of data sources from which databases are maintained,7 they may not reflect the current availability in an area. As participants said, services may come and go, and smaller agencies may have limited online presence from which a platform could scrape data, suggesting the need for local expertise in dedicated roles, and facilitated by interorganizational communications and committees. Additionally, databases may have limited ability to evaluate resource quality and navigate trust relationships between patients and community resources, although crowdsourced ratings and recommender systems offer some promise. Participants described a trust-building feedback loop, in which staff and volunteers ask patients about personal experiences using community resources in order to inform future referrals. By learning about the quality of resources from personal experiences, they may develop a better understanding of where best to refer patients. Community resource referral platforms may offer interorganizational communication and follow up services, though these capacities should be implemented to allow for the joint optimization of both the technical and the social subsystems, considering existing referral networks to complement rather than replace the social subsystem.
Facilitating connections to community resources is a complex process that may go beyond giving patients contact information; instead, participants leveraged interorganizational networks to connect with resources, and helped patients navigate complicated care systems. Warm handoffs, in which providers personally connect patients to a representative of a resource, have been shown to be more effective in enrolling patients in tobacco quitlines than simply providing contact information.22 Referrals are a sociotechnical process that results from the interplay of interpersonal relationships, interorganizational networks, and technology. While databases and communication technologies are important parts of facilitating connections, it is important to recognize the role of relationships in the referral process. Relationships broker trust between patients and the resources to which they are referred. By leveraging both local community expertise and referral databases, patients can be matched to trusted up-to-date resources. Local expertise and personal relationships play important roles in negotiating patient referrals, which aligns with findings from previous work demonstrating the role of interpersonal negotiations when transferring patients between hospitals.23 Using an STS perspective, the dual advantages of both comprehensive and rapidly queried databases and patient navigators’ social and relational work may be leveraged to jointly optimize the community resource referral system, facilitating connections between patients and necessary resources.
This study has limitations to consider. First, we collected data in three cities in Michigan, and while the sites offer diversity in both population and services, experiences at these sites may not generalize nationwide, particularly to higher-income areas. Similarly, focus groups were conducted in 2013, before the implementation of many community resource referral platforms. However, we believe that this underscores the importance of the social subsystem in the community referral system, as robust referral systems existed before new database-driven platforms.
This study supports the ongoing importance of the social and external environmental subsystems even as new community referral platforms become available. Thus, informaticists should appreciate that implementation of community resource referral platforms may be made more successful by new or continued investment in people, personal relationships, and interorganizational networks. Consequently, we advocate sociotechnical design approaches when developing novel interventions to enhance community referrals.9,10
Conclusion
Community resource referral is a sociotechnical work system in which social, technical, and external environmental subsystems play roles. The process involved, from assessing patients, to choosing resources to facilitating connections, may benefit from new technologies—but also relies upon people’s knowledge and skills, personal relationships, and interorganizational networks. Organizations should consider how community resource referral platforms can enhance, rather than replace, the interpersonal work of community organization staff or volunteers, patient navigators, healthcare providers, and I&R specialists to improve community resource referrals.
Acknowledgements
We gratefully acknowledge funding from the Institute of Museum and Library Services (IMLS, Grant LG-52-11-0212-11). Any views, findings, or conclusions expressed here do not necessarily represent those of IMLS.
Figures & Table
Table 1.
Characteristics of Focus Group Participants (n=102)
| Characteristic | Mean | SD |
| Age | 49.5 | 13.64 |
| Focus Group Location | N | % |
| Flint | 43 | 42.16% |
| Inkster | 32 | 31.37% |
| Detroit | 27 | 26.47% |
| Race/Ethnicity | ||
| Black or African American | 70 | 68.63% |
| White | 28 | 27.45% |
| American Indian or Alaskan Native | 2 | 1.96% |
| Hispanic/Latino | 2 | 1.96% |
| Arab Descent | 3 | 2.94% |
| Other | 6 | 5.88% |
| Education | ||
| Grades 9 to 12, no diploma | 2 | 1.96% |
| High school graduate or equivalent | 13 | 12.75% |
| Some college or associate degree | 33 | 32.36% |
| Bachelor’s degree (e.g., BA, BS) | 15 | 14.71% |
| Graduate or professional degree (e.g., MA, MD, JD) | 37 | 36.27% |
| Employment | ||
| Full-time | 43 | 42.16% |
| Part-time | 12 | 11.76% |
| Student | 6 | 5.88% |
| Unemployed, retired, disability benefits, or other | 41 | 40.19% |
References
- 1.Alderwick H, Gottlieb LM. Meanings and Misunderstandings: A Social Determinants of Health Lexicon for Health Care Systems. Milbank Q [Internet] 2019 May 9;97(2) doi: 10.1111/1468-0009.12390. [cited 2020 Jan 20]; Available from: https://www.milbank.org/quarterly/articles/meanings-and-misunderstandings-a-social-determinants-of-health-lexicon-for-health-care-systems/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adler NE, Stead WW. Patients in Context — EHR Capture of Social and Behavioral Determinants of Health. N Engl J Med. 2015 Feb 19;372(8):698–701. doi: 10.1056/NEJMp1413945. [DOI] [PubMed] [Google Scholar]
- 3.Cantor MN, Thorpe L. Integrating Data On Social Determinants Of Health Into Electronic Health Records. Health Aff (Millwood). 2018 Apr 1;37(4):585–90. doi: 10.1377/hlthaff.2017.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MI-AIRS: Michigan Alliance of Information & Referral Systems [Internet] [cited 2020 Mar 9]. Available from: http://www.mi-airs.com/aboutus/aboutirsystems.html .
- 5.Certification - Alliance of Information and Referral Systems [Internet] [cited 2020 Mar 9]. Available from: https://www.airs.org/i4a/pages/index.cfm?pageid=3449 .
- 6.Gottlieb L, Sandel M, Adler NE. Collecting and Applying Data on Social Determinants of Health in Health Care Settings. JAMA Intern Med. 2013 Jun 10;173(11):1017–20. doi: 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- 7.Research on Integrating Social & Medical Care | SIREN | Community Resource Referral Platforms: A Guide for Health Care Organizations [Internet] [cited 2020 Mar 5]. Available from: https://sirenetwork.ucsf.edu/tools-resources/resources/community-resource-referral-platforms-guide-health-care-organizations .
- 8.Militello L, Arbuckle N, Saleem J, Patterson E, Flanagan M, Haggstrom D, et al. Sources of variation in primary care clinical workflow: Implications for the design of cognitive support. Health Informatics J. 2013. Oct 8, [DOI] [PubMed]
- 9.Bostrom RP, Heinen JS. MIS problems and failures: A socio-technical perspective. Part I: The causes. MIS Q. 1977. pp. 17–32.
- 10.Bostrom RP, Heinen JS. MIS problems and failures: a socio-technical perspective, part II: the application of socio-technical theory. MIS Q. 1977. pp. 11–28.
- 11.Holden RJ, Karsh B-T. A theoretical model of health information technology usage behaviour with implications for patient safety. Behav Inf Technol. 2009;28(1):21–38. [Google Scholar]
- 12.Unertl KM, Schaefbauer CL, Campbell TR, Senteio C, Siek KA, Bakken S, et al. Integrating community-based participatory research and informatics approaches to improve the engagement and health of underserved populations. J Am Med Inform Assoc. 2015;23(1):60–73. doi: 10.1093/jamia/ocv094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lachance L, Kelly RP, Wilkin M, Burke J, Waddell S. Community-based efforts to prevent and manage diabetes in women living in vulnerable communities. J Community Health. 2018;43(3):508–517. doi: 10.1007/s10900-017-0444-2. [DOI] [PubMed] [Google Scholar]
- 14.Communities Against Diabetes: Flint, NW Detroit, Inkster . Program to Eliminate Diabetes-Related Health Disparities in African Americans Living in Flint. NW Detroit, and Inkster, Michigan Strategic Plan; 2011-2015 [Internet]. Available from: https://www.nkfm.org/sites/default/files/documents/pages/cad_strategic_plan.pdf . [Google Scholar]
- 15.Saldana J. The Coding Manual for Qualitative Researchers. SAGE; 2015. p. 369. [Google Scholar]
- 16.Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. Third edition. Thousand Oaks, Califorinia: SAGE Publications, Inc; 2013. p. 408. [Google Scholar]
- 17.Senteio C, Veinot T. Trying to make things right: adherence work in high-poverty, African American neighborhoods. Qual Health Res. 2014;24(12):1745–1756. doi: 10.1177/1049732314549027. [DOI] [PubMed] [Google Scholar]
- 18.Buitron de la Vega P, Losi S, Sprague Martinez L, Bovell-Ammon A, Garg A, James T, et al. Implementing an EHR-based Screening and Referral System to Address Social Determinants of Health in Primary Care. Med Care. 2019 Jun;57:S133. doi: 10.1097/MLR.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 19.Senteio C, Veinot T, Adler-Milstein J, Richardson C. Physicians’ perceptions of the impact of the EHR on the collection and retrieval of psychosocial information in outpatient diabetes care. Int J Med Inf. 2018;113:9–16. doi: 10.1016/j.ijmedinf.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Gold R, Bunce A, Cowburn S, Dambrun K, Dearing M, Middendorf M, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med. 2018;16(5):399–407. doi: 10.1370/afm.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orji R, Moffatt K. Persuasive technology for health and wellness: State-of-the-art and emerging trends. Health Informatics J. 2018 Mar 1;24(1):66–91. doi: 10.1177/1460458216650979. [DOI] [PubMed] [Google Scholar]
- 22.Richter KP, Faseru B, Shireman TI, Mussulman LM, Nazir N, Bush T, et al. Warm Handoff Versus Fax Referral for Linking Hospitalized Smokers to Quitlines. Am J Prev Med. 2016 Oct 1;51(4):587–96. doi: 10.1016/j.amepre.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bosk EA, Veinot T, Iwashyna TJ. Which Patients, and Where: A Qualitative Study of Patient Transfers from Community Hospitals. Med Care. 2011 Jun;49(6):592–8. doi: 10.1097/MLR.0b013e31820fb71b. [DOI] [PMC free article] [PubMed] [Google Scholar]


