Abstract
Digital health technologies offer unique opportunities to improve health outcomes for mental health conditions such as peripartum depression (PPD), a disorder that affects approximately 10-15% of women in the U.S. every year. In this paper, we present the adaption of a digital technology development framework, Digilego, in the context of PPD. Methods include mapping of the Behavior Intervention Technology (BIT) model and the Patient Engagement Framework (PEF) to translate patient needs captured through focus groups. This informs formative development and implementation of digital health features for optimal patient engagement in PPD screening and management. Results show an array ofPPD-specific Digilego blocks (“My Diary”, “Mom Talk”, “My Care”, “Library”, “How am I doing today?”). Initial evaluation results from comparative market analysis indicate that our proposed platform offers advantageous technology aspects. Limitations and future work in areas of interdisciplinary care coordination and patient engagement optimization are discussed.
Introduction
Depression is the main cause of disease burden for women, on a worldwide scale [1]. Many women experience peripartum depression (PPD), a specific category of depression associated with the physical and psychological changes that occur during pregnancy and childbirth [2]. PPD can manifest at any time during pregnancy or shortly after childbirth [3]. Some common symptoms are general loss of interest and pleasure in life, anxiety attacks, insomnia, thoughts of harming oneself or the infant, and difficulty bonding with the infant. The symptoms are long-lasting (more than two weeks) and may interfere with daily normal functioning. This differentiates PPD from the less severe and transient “baby blues” [4]. If left untreated, PPD can have adverse health consequences for women and their infants. Women can start having longer and more intense episodes of depression, and infants can develop behavioral and cognitive problems later in life [5]. Fortunately, PPD can be managed with treatments such as therapy and medication [6]. It is widely reported that the annual prevalence rate of PPD for pregnant women and new mothers in the U.S. is somewhere around 10-15% [7, 8]. However, such figures only capture about half of all PPD cases [9]. This gap in PPD diagnosis is due to many social and logistical barriers [10, 11]. Social barriers include stigmas regarding the experience of pregnancy, inability to perceive joyous arrival of new baby, and expectations of being a new mother [10]. In addition to the gap in PPD diagnosis, there is a gap in care coordination and delivery. Even after a case is diagnosed, not all women undergo treatment. Cox and colleagues [12] reported that only 11-13% of cases receive the treatment they need. Access to care can be an issue for women with PPD, as they are likely to be experiencing adverse socioeconomic factors [10]. Because PPD is frequently managed by a team of interdisciplinary professionals, the coordination of care can be a complex process [13]. There are many clinical components that are managed by different specialties, such as depression management via therapy programs, prenatal/postnatal care, and pediatrics. Patient information must be timely updated and shared among all team members in order to provide the best care possible.
Digital technologies can streamline delivery of self-health management processes at patient-level and facilitate communication between providers and patients, effectively preventing information silos. These tools have been shown to improve health outcomes for mental health disorders, including PPD [14]. They also allow patients a discrete and practical medium that is suitable for the sensitive nature of mental health [15]. Many studies have indicated that mental health professionals will recommend and use mobile applications for treatment management [16]. PPD stakeholders, including patients and providers, have also shown optimism regarding digital management of PPD [17, 18]. This includes screening, information seeking, and support seeking [i.e. 19]. Thus, it is expected that digital technologies can be of great assistance in bridging existing gaps of PPD care coordination and management, such as the low rates of PPD screening and treatment [11,12].
The overarching objective of our paper is to describe and adapt a novel modular digital health development framework, Digilego [20], in the context of peripartum depression. As part of this process, we translate patient needs for PPD identification and management captured through traditional data collection methods into theory-driven digital health features, and optimize the digital features for sustained patient engagement and care coordination. In the next sections of the paper, we describe: (a) our efforts in Digilego adaptation, initial prototyping, and feature implementations, and (b) study limitations and future directions for seamless care coordination and patient engagement in digital health era.
Methods
(a) Theoretical Rational: Digilego
In this paper, we adapt Digilego, a digital health development framework for patient-facing health applications that are (a) theory-driven in needs translation, (b) engaging for long-term sustained use, and (c) integrative of care coordination processes that are multilevel, inter- and intra-personal in nature [20]. These factors can range from personal demographics, clinical data points from electronic health records for patient review, and patient-generated health data from survey instruments, wearables, and home-based monitoring systems. The framework facilitates and supports the distributed nature of patient needs and care processes. The ability to support care coordination and health promotion across the technology spectrum (ranging from wellness surveys to deep learning for social media analysis and AI based predictions for content recommendations) makes Digilego an innovative, agile, and rapid-prototyping framework. Digilego is a two-arm framework: one is a theoretically-aligned tier digital health development framework, and the second is a digital ecosystem comprised of programmable implementations of clinical and public health modules (Digilego blocks) that can be reused and customized. It has been previously used to develop digital platforms for self-management of cancer survivorship and psychological stress [21,22]. Such a framework provides health researchers the ability to scale their platforms and interventions to groups of individuals and populations, and to optimize engagement of their end users, all while ensuring their final products are theory-driven and standards-compliant. The Digilego framework integrates four main components of digital health development: (a) needs assessment using traditional and data-intensive methods (data sources examples: published sources, focus groups, social media), (b) theory infusion to facilitate behavior change using Behavioral Intervention Technologies (BIT) model , (c) engagement optimization for sustained use, using the Healthcare Information and Management Systems Society (HIMSS) Patient Engagement Framework (PEF) , and (d) compliance with Fast Healthcare Interoperability Resources (FHIR) Specification, a standard for exchanging healthcare information electronically [23]. Research shows the use of multiple approaches for needs gathering and theory integration produces an effective design paradigm for patient-centered health applications, specifically for the purpose of self-monitoring and behavior change in self-health management [24–26].
(b) Digilego for PPD
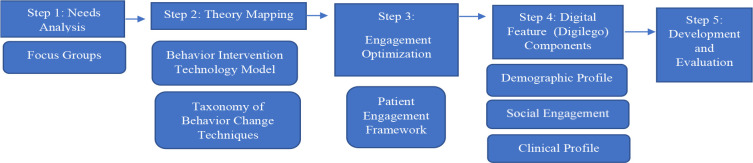
Our instantiation of the Digilego framework in the PPD case study is summarized in Figure 1. In our adaptation process, we have applied the following steps to develop a digital ecosystem for our target population of PPD patients.
Figure 1.
Framework for Digilego Development (Peripartum Depression)
Step 1: Needs Analysis
While Digilego allows a range of needs analysis methodologies as described earlier, we have chosen focus groups as our main study technique. Focus group interviews were done at an academic OB/GYN clinic in Houston for women of low socio-economic status, with approval from UT Health’s IRB Committee. Recruitment was done on site and informed consent was obtained from patients. The purpose of the focus groups was to assess patients opinions regarding digital technologies in the management of their healthcare. A survey was also administered to collect data on participant’s technology use. A total of nine patients participated in the focus groups, which were semi-structured. Participant comments were extracted from focus group recordings, and ground-theory thematic analysis was used to derive major themes.
Step 2: Theory Mapping
Our theoretical basis to make behavior change an easier process for PPD patients is Mohr’s Behavioral Intervention Technology (BIT) model [27]. This model prompts intervention developers to answer the questions of Why?, How? (conceptual and technical), What?, and When? at the time of technology development. The main idea of the model is to define a relationship between digital features and their aims and characteristics. We will use this model for initial mapping of our PPD outcome goals to digital features. The BIT component of How? (conceptual) calls for the identification of a behavior change theory to be integrated into the technology, therefore we will incorporate techniques from Michie’s Behavior Change Taxonomy (BCT) [28]. This is a standardized, comprehensive taxonomy of 93 theory-linked techniques for use in health behavior change interventions. It is based on principles from different disciplines such as psychology, social sciences, and engineering [29].
Step 3: Engagement Optimization
The HIMSS PEF framework [30] is designed to assist healthcare organizations, such as hospitals, in creating digital platforms for their patient population. However, it can also be applied to a more specific population of patients, such as PPD patients. It consists of five categories that are cumulative in their level of engagement and complexity: “inform me,” “engage me,” “empower me,” “partner with me,” and “support my e-community”. The framework shows how digital features can be used to reach different patient engagement levels. For instance, if e-tools allow a patient to keep track of her pregnancy, this would be considered under the “engage me” level because it keeps the patient informed but requires no other action. However, if the e-tools advance to provide a secure messaging function where the patient can actively pursue more specific queries related to pregnancy, this would be considered the “empower Me” level.
Step 4: Digital Features (PPD-specific Digilego Blocks)
To create digital features specific to PPD, we will leverage existing Digilego core architecture [20]. The unique engagement aspects from these existing Digilego blocks that we can repurpose and leverage for PPD management include the patient’s demographic profile, clinical profile, and social engagement (Table 1).
Table 1.
Leveraging Digilego Core Architecture to Peripartum Depression
| Existing Digilego and Features | Related New PPD Digilego |
| DigiMe: A digital representation of the patient’s profile (i.e. name, age, location). Features: insurance information, transition assistance, related surveys according to target condition, and personal profile. | In addition to the main user page containing the patient’s personal profile, the “How am I doing today?” Digilego block is a repository of screening survey tools that can be accessed by the patient on a regular basis. |
| DigiSocial: Encompasses digital social engagement. May include components such as online discussion forums and education sources. Features: Social hub, education, question corner, and journaling. | “My Diary”: notebook-style tool for patients to record recent experiences and feelings. “Library”: information center where patients can search the latest evidence-based information about PPD, and related topics. “Mom Talk”: social media feature where patients can share their experiences and provide each other support and a sense of community. |
| DigiEHR: A digital record of the patient’s clinical profile. Features: treatment summary, labs, alerts, and follow-up. | “My Care”: repository of the patient’s clinical information, including caregiver profile, medications, and upcoming clinical appointments. |
Results
Needs Analysis
Majority of participants in our focus groups were young (25-34 years old) and African-American. Survey results indicated three of the nine participants were expecting their first child, while six had at least one child. Seven of nine participants had experienced depression symptoms during their current pregnancy, and six had these symptoms in past pregnancies. Of the seven participants who had experienced depression during pregnancy, five had mentioned it to their doctor. The internet was their main source of information for pregnancy-related questions. Six major information themes have been identified and extracted from our focus groups in regards to PPD care and management. Table 2 provides a list of these themes and sample participant comments illustrating participant needs.
Table 2.
Information Themes from Needs Analysis
| Theme | Participant Comment |
| Open and timely communication with providers. | “[If your doctor can see your journal entries from an app] they will see you as a human, not just as a patient. They will know ‘This patient is really concerned, so let’s not wait to answer this question, let’s call them right now’“ |
| Feeling part of a community environment. | “Having someone [a fellow app user] say Hey, let me bring you some food and let’s have a talk’ even though we don’t want to talk and want to shut down, in a sense that can help you get through it” |
| Tailored support, given on a daily basis and based on medical history and individual needs. | “The apps aren’t really personalized. They’re general, they’re like, average. Me, I have [medical condition], so it’s not designed for people like me” |
| Support for unique pregnancy experiences. | “For people who have had several miscarriages, they can talk to someone [who has gone through a similar experience through the app]” |
| Tools to overcome information silos in the care setting. | “I use it for appointments, but most of my doctors don’t even have it [the patient portal]” |
| Tools to overcome barriers and disparities when seeking mental health care. | I wish I had video chat if I can’t make it to an appointment.” |
Theory Mapping Using Behavioral Intervention Technology Model
While our digital features are more thoroughly described in the next section of our results, Table 3 shows the results of BIT model application to initially map their overall aims, technical characteristics, and workflow.
Table 3.
Mapping of Behavioral Intervention Technology Model to Identify Digital Features for Peripartum Depression Management
| BIT Component | Mapping to PPD (Examples) |
| Why | Reduction and remission of depression symptoms: (a) increasing healthy, positive thoughts and actions, (b) increasing awareness of and access to PPD screening and education |
| How (conceptual) | The taxonomy of Behavior Change Techniques (i.e. Self-Monitoring, Social Support) [27] |
| What | Digital features:
|
| How (Technical) | Mobile digital platform with modular, user-centered design. |
| When | Workflow will be tailored to participant and provider. Example: If participant transitions from pregnancy to motherhood, the catalogue of information will be focused on coping with this transition. |
Engagement Optimization Using HIMSS Patient Engagement Framework
Based on results from our needs analysis and theory mapping, we found that the following PEF features would be particularly useful for our target patients: Patient-Specific Education, Patient Access and Use, e-Visits and e-Tools, and Care-team generated data. These features will be used at different engagement levels ranging from engage me to support my e-community. Table 4 further illustrates these results.
Table 4.
Engagement Optimization
| PEF Engagement Category | Digital Features | Related PPD Digilego |
|
Empower Me - Self-management diaries |
Patient Generated Data | “My Diary” |
|
Engage Me - Option to share progress and health milestones on social media. |
E-tools | “Mom Talk” |
| Support my e-Community | ||
| - Community Support | ||
|
Inform Me - Health Encyclopedia |
E-tools | “Library” |
| Support my e-Community - Shared care plans | Care team generated data | “My Care” |
|
Empower Me - Symptoms Assessment |
Patient Generated Data | “How am I doing today?” |
Digital Features (Digilego blocks)
Finally, the results of our application of the Digilego framework to develop a PPD-specific digital health solution, tentatively titled “Mom Mind” are as follows:
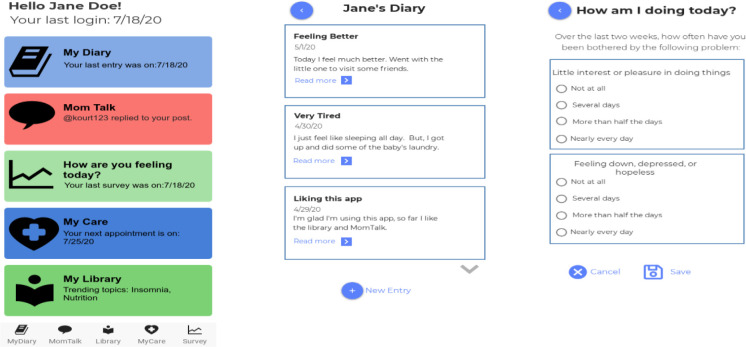
(a) “My Diary”- this is a journaling feature where patients will be able to create and submit entries at any time. Existing journal entries will be visible and accessible, and patients will have the option to share with others. This feature will allow participants to informally monitor their own mood and depression symptoms, and may help to identify stress inducers and techniques to prevent depression.
(b) “Mom Talk”- This feature will contain social forum characteristics, where patients can post a discussion thread and receive replies from other participants. Message notifications will be enabled in this Digilego.
(c) “Library”- This feature will function as a “newsstand” meant to expose the patient to the latest health education and research on the topics of PPD, pregnancy, and motherhood. Alerts for new topics will be provided. Content will be available in various formats such as text and video. Based on input from PPD experts (including OB/GYNs, Psychiatry, and Health Disparities researchers), content will be selected and curated from reliable research sources such as PubMed, PsychInfo, National Institutes of Health, and Centers for Disease Control. It will then be presented to patients in a summarized format. This library file will be maintained relevant by updating periodically (i.e. monthly) or as deemed necessary.
(d) “My Care”- In this feature, patients will be able to access personal clinical care components. For example, they will be able to know whether their medications are safe for breastfeeding, and when their next psychiatric appointment is scheduled. Alerts for events such as receiving a new message from provider will be incorporated into this feature. It borrows various components (i.e. Treatment Summary, Physician Communication) from the existing DigiEHR and DigiMe blocks.
(e) “How am I doing today?”- this feature contains self-report surveys, for patients to monitor their mental health status. Survey instruments planned for inclusion are the Patient Health Questionnaire- 2 (PHQ2) for daily screening, and the Edinburg Postnatal Depression Scale for weekly or bi-weekly screening. Both of these instruments have been shown to have acceptable performance [31, 32]. Screening results can be monitored by the clinical provider if necessary.
Table 5 provides a snapshot of the results derived from Digilego framework and their mapping to BCT and accommodation of user needs in Digilego components.
Table 5.
Digilego Results Mapping to Peripartum Depression Management
| PPD Digilego | BCT | User Need |
| “My Diary” | 2.3- Self-monitoring of behavior 5.4- Monitoring of emotional consequences 15.4- Self talk |
Tailored support based on medical history/unique needs Support for unique pregnancy experiences |
| “Mom Talk” | 3.1- Social support (unspecified) 6.2 - Social comparison 6.3- Information about other’s approval | Feeling part of a community environment |
| “Library” | 9.1- Credible source | Support for unique pregnancy experiences |
| “My Care” | 2.2- Feedback on Behavior | Open and timely communication with providers Tools to overcome information silos in the care setting |
| “How am I doing today?” | 2.3- Self-monitoring of behavior | Tools to overcome barriers when seeking mental health care |
Technology Development
Recent wireframes for components of “Mom Mind” are illustrated in Figure 2. The left screen shows the main landing page for the user, where our Digilego blocks are highlighted. This main screen provides recent notifications to the user, and a main menu is also accessible at the bottom of the page. The center screen illustrates the “My Diary” journal feature, personalized with the user’s name and with a listing of recent entries. The right-most screen shows the PHQ-2 screening integrated into the “How am I doing today?” Digilego.
Figure 2.
“Mom Mind” Wireframes
Initial Evaluation
Feature Comparisons
A comparison of features between our proposed MomMind digital platform and consumer apps dedicated to PPD was conducted. Six PPD apps were examined in this analysis: “Little Mother’s Helper”, “MomentHealth”, “PPD ACT”, “MGHPDS”, “Postpartum Depression”, and “Post Pregnancy Recovery” [33-38]. These apps are free and available in the Apple App Store and/or the Google Play Store. They are targeted exclusively to new mothers (postpaturm) and contain a range of features such as PPD information and screening. Table 6 summarizes the comparison of features between MomMind and the examined apps. Two of the six apps (PPD Act and MGHPDS) are research-based and therefore have a theoretical framework behind their features. The other four are consumer-driven. The common features that we have found in both our Digilego blocks and these apps are: social hubs, self-reporting surveys, and education about PPD. Personalization features such as bidirectional communication with providers, journal, and treatment summary were not present in any of the selected apps for comparison. Further, the average number of BCT techniques incorporated in the apps was four, while our Mom Mind has a total of eight BCT techniques. In terms of PEF adoption, we found that the highest level of PEF category reached among the apps was Empower Me. This was identified in two of the apps, due to their inclusion of screening tools for symptom assessment. Our proposed Digilego blocks, on the other hand, are able to reach the category of “Support my e-Community” due to the provision of communication with providers and peers. This indicates that our usage of BIT (through which we incorporate BCTs) and PEF models has allowed us to develop an engaging product that optimizes the care coordination and self-management of PPD.
Table 6.
Comparison of MomMind and Consumer Apps
| Digital Feature |
Little Mother’s Helper |
Moment Health |
PPD Act |
MGHPDS | Postpartum Depression |
Post Pregnancy Recovery |
MomMind |
| Journaling | x | x | x | x | x | x | ✓ |
| Social Hub | x | ✓ | x | x | x | x | ✓ |
| Education | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Question Corner | x | x | x | x | x | x | ✓ |
| Appointment Reminders | x | x | x | x | x | x | ✓ |
| Treatment summary | x | x | x | x | x | x | ✓ |
| Alerts | x | x | x | x | x | x | ✓ |
|
Physician Communication |
x | x | x | x | x | x | ✓ |
| Caregiver Profile | x | x | x | x | x | x | ✓ |
| Survey | x | ✓ | ✓ | ✓ | x | x | ✓ |
Limitations and Future Work
Our needs analysis is limited to focus groups discussions of women who are pregnant and of low socioeconomic status, but not necessarily diagnosed with PPD. Inclusion of other PPD stakeholders, such as clinicians, in our needs analysis will also be done for holistic development of the MomMind ecosystem. Our digital prototypes are partially implemented and have gone through limited usability evaluations. Next steps in our research program will be:
a) Mixed-mode needs assessment: Continuation of needs analysis, with more focus groups with different participants (including clinicians). Our needs analysis will also harness additional methodologies through synthesis of existing literature knowledge and data from social media content [20, 21]. For example, content of online forums dedicated to PPD will be analyzed in order to include different sources of data. While the focus of this paper has been to customize the MomMind platform to socioeconomically disadvantaged women, this work will help us understand the needs of the general population as well.
b) Culmination of digital platform development: this includes technical implementation of new features, adaptation of existing Digilego blocks for MomMind, and content curation. This will be accomplished through software tools including proto.io [39] and Flutter [40]. The content selection and final curation will be based on expert input from an interdisciplinary group of clinicians and health researchers, with particular focus on the specialties of OB/GYN, Psychiatry, and Health Disparities. The content will be selected from reliable sources (i.e. PubMed, PsychInfo). We then plan to use storytelling tools such as Videoscribe [41] to summarize content in a user-friendly comprehensible format for hosting in MomMind, while considering health literacy aspects.
c) Interoperability assurance: Ensuring that MomMind is compliant to Fast Healthcare Interoperable Resources (FHIR) standards [23].
d) Evaluation of digital platform by patients and providers: once the development stage is culminated, patients and providers will be presented with our platform to assess its acceptability and usability. This can be achieved through evaluation techniques such as having end users do a walkthrough of the platform while developers use the Nielsen -Shneiderman Heuristics tool to annotate platform usability [42, 43].
Conclusion
Peripartum depression is a condition that produces significantly adverse public health outcomes, yet there are still not enough efficient digital tools to advance its diagnosis and management. In this study, we describe information needs of young pregnant women to deal with conditions like PPD. We adapt a digital health framework to translate patient needs to theory-driven, engaging, and evidence-based digital features. Particularly, our work describes the technology needs of an underexplored population; young demographic who are accustomed to communicating in a digital environment, where information is sent and received in an instant manner. Therefore, a digital platform that is agile, personable, and adaptive is a suitable solution to increasing patient engagement in their management of the PPD condition. Further, a care coordination ecosystem optimized for clinicians with synchronized features in terms of case management and patient-provider communication across multiple specialties is much needed for conditions such as PPD. In summary, our work is the first step towards a digital health ecosystem that facilitates interdisciplinary care coordination and self-health management that would allow PPD patients to have trusted information sources readily available with personalized, theoretically-aligned, and sustainable digital pathways for enhanced self-monitoring.
Acknowledgements
We would like to thank the patients who participated in this study for their time and insights. We would also like to thank all of the staff at the UTPhysician’s Women’s Center at TMC who helped with the coordination of the focus group interviews. Research reported in this publication was partly supported by the National Library of Medicine of the National Institutes of Health under award numbers 1R01LM012974-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Figures & Table
References
- 1.Kaiser Family Foundation What are the current costs and outcomes related to mental health and substance use disorders? 2015. ; Accessed from: https://www.healthsystemtracker.org/chart-collection/current-costs-outcomes-related-mental-health-substance-abuse-disorders/#item-start .
- 2.Hubner-Liebermann B, Hausner H, Wittmann M. Recognizing and treating peripartum depression. Deutsches Ärzteblatt International. 2012 Jun;109(24):419. doi: 10.3238/arztebl.2012.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . Arlington: American Psychiatric Association; 5th ed. 2013. Diagnostic and statistical manual of mental disorders; p. 1520. p. Available from: https://doi.org/10.1176/appi.books.9780890425596 . [Google Scholar]
- 4.Centers for Disease Control and Prevention Depression among women. 2020. May, . Accessed from: https://www.cdc.gov/reproductivehealth/depression/index.htm .
- 5.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant behavior & development. 2010 Feb;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. doi:10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitelson E, Kim S, Baker AS, Leight K. Treatment of postpartum depression: clinical, psychological and pharmacological options. International journal of women’s health. 2010 Dec;3:1–14. doi: 10.2147/IJWH.S6938. doi:10.2147/IJWH.S6938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ko JY, Rockhill KM, Tong VT, Morrow B, Farr SL. Trends in Postpartum Depressive Symptoms — 27 States, 2004, 2008, and 2012. MMWR Morb Mortal Wkly Rep. 2017 Feb;66:153–158. doi: 10.15585/mmwr.mm6606a1. . DOI: http://dx.doi.org/10.15585/mmwr.mm6606a1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vigod SN, Wilson CA, Howard LM. Depression in pregnancy. BMJ. 2016 Mar;352:i1547. doi: 10.1136/bmj.i1547. [DOI] [PubMed] [Google Scholar]
- 9.Lee DTS, Chung THK. Postnatal depression: an update. Best Practice & Research Clinical Obstetrics & Gynaecology. 2007 Apr;21(2):183–191. doi: 10.1016/j.bpobgyn.2006.10.003. . https://doi.org/10.1016/j.bpobgyn.2006.10.003 . [DOI] [PubMed] [Google Scholar]
- 10.Dennis C, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: A Qualitative Systematic Review. Birth. 2006 Dec;(33):323–331. doi: 10.1111/j.1523-536X.2006.00130.x. doi:10.1111/j.1523-536X.2006.00130.x. [DOI] [PubMed] [Google Scholar]
- 11.Gjerdingen DK, Yawn BP. Postpartum depression screening: importance, methods, barriers, and recommendations for practice. The Journal of the American Board of Family Medicine. 2007 May 1;20(3):280–8. doi: 10.3122/jabfm.2007.03.060171. [DOI] [PubMed] [Google Scholar]
- 12.Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal depression treatment cascade: baby steps toward improving outcomes. The Journal of Clinical Psychiatry. 2016 Sep;77(9):1189–2000. doi: 10.4088/JCP.15r10174. doi:10.4088/JCP.15r10174. [DOI] [PubMed] [Google Scholar]
- 13.Rafferty J, Mattson G, Earls MF, Yogman MW. Incorporating recognition and management of perinatal depression into pediatric practice. Pediatrics. 2019 Jan;143(1) doi: 10.1542/peds.2018-3260. . doi:10.1542/peds.2018-3260. [DOI] [PubMed] [Google Scholar]
- 14.Lee EW, Denison FC, Hor K, Reynolds RM. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC pregnancy and childbirth. 2016 Feb;16(38) doi: 10.1186/s12884-016-0831-1. . doi:10.1186/s12884-016-0831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hollis C, Morriss R, Martin J, Amani S, Cotton R, Denis M, et al. Technological innovations in mental healthcare: harnessing the digital revolution. British Journal of Psychiatry. 2015 Apr;206(4):263–265. doi: 10.1192/bjp.bp.113.142612. doi:10.1192/bjp.bp.113.142612. [DOI] [PubMed] [Google Scholar]
- 16.Pineros-Leano M, Tabb KM, Sears H, Meline B, Huang H. Clinic staff attitudes towards the use of mHealth technology to conduct perinatal depression screenings: a qualitative study. Family Practice. 2015 Apr;32(2):211–215. doi: 10.1093/fampra/cmu083. . https://doi.org/10.1093/fampra/cmu083 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osma J, Barrera A, Ramphos E. Are pregnant and postpartum women interested in health-related apps? implications for the prevention of perinatal depression. Cyberpsychology, Behavior and Social Networking. 2016 Jun;19(6):412–415. doi: 10.1089/cyber.2015.0549. . https://doi.org/10.1089/cyber.2015.0549 . [DOI] [PubMed] [Google Scholar]
- 18.Sprenger M, Mettler T, Osma J. Health professionals’ perspective on the promotion of e-mental health apps in the context of maternal depression. PloS one. 2017 Jul;12(7):e0180867. doi: 10.1371/journal.pone.0180867. doi:10.1371/journal.pone.0180867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broom MA, Ladley AS, Rhyne EA, Halloran DR. Feasibility and perception of using text messages as an adjunct therapy for low-income, minority mothers with postpartum depression. JMIR mental health. 2015 Mar;2(1):e4. doi: 10.2196/mental.4074. doi:10.2196/mental.4074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myneni S, Rogith D, Franklin A. In International Conference on Social Computing, Behavioral-Cultural Modeling and Prediction and Behavior Representation in Modeling and Simulation. Cham: Springer; 2018 Jul 10. Digilego: A standardized analytics-driven consumer-oriented connected health framework; pp. 263–273. [Google Scholar]
- 21.Myneni S, Amith M, Geng Y, Tao C. Towards an ontology-driven framework to enable development of personalized mHealth solutions for Cancer survivors’ engagement in healthy living. Studies in health technology and informatics. 2015 Aug;216:113. [PMC free article] [PubMed] [Google Scholar]
- 22.Carter L, Rogith D, Franklin A, Myneni S. NewCope: A Theory-Linked Mobile Application for Stress Education and Management. Stud Health Technol Inform. 2019 Aug 21;264:1150–1154. doi: 10.3233/SHTI190406. doi: 10.3233/SHTI190406. PMID: 31438105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mandel JC, Kreda DA, Mandl KD, Kohane IS, Ramoni RB. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. Journal of the American Medical Informatics Association. 2016 Sep 1;23(5):899–908. doi: 10.1093/jamia/ocv189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Villarreal V, Fontecha J, Hervas R, Bravo J. Mobile and ubiquitous architecture for the medical control of chronic diseases through the use of intelligent devices: Using the architecture for patients with diabetes. Future Gener. Comput. Syst. 2014 May;34:161–175. [Google Scholar]
- 25.Docksteader L, Benlamri R. Digital Information Management. Third International Conference on. IEEE; 2008. Mobile ontology-based reasoning and feedback health monitoring system; pp. 876–880. [Google Scholar]
- 26.Docksteader L, Benlamri R. MORF: A mobile health-monitoring platform. IT Prof. 2010;12(3):0018–0025. [Google Scholar]
- 27.Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The behavioral intervention technology model: an integrated conceptual and technological framework for eHealth and mHealth interventions. Journal of medical Internet research. 2014 Jun;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michie S, Yardley L, West R, Patrick K, Greaves F. Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. Journal of medical Internet research. 2017 Jun;19(6):e232. doi: 10.2196/jmir.7126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health psychology. 2008 May;27(3):379. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 30.HIMSS Patient Engagement Framework Center for Patient and Family-Centered Care. February 10 2014. (published). Last access July 7, 2020.
- 31.Smith MV, Gotman N, Lin H, Yonkers KA. Do the PHQ-8 and the PHQ-2 accurately screen for depressive disorders in a sample of pregnant women? Gen Hosp Psychiatry. 2010 Sep-Oct;32(5):544–8. doi: 10.1016/j.genhosppsych.2010.04.011. doi: 10.1016/j.genhosppsych.2010.04.011. Epub 2010 Jun 22. PMID: 20851275; PMCID: PMC2943487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kernot J, Olds T, Lewis LK, Maher C. Test-retest reliability of the english version of the edinburgh postnatal depression scale. Archives of women’s mental health. 2015 Apr 1;18(2):255–7. doi: 10.1007/s00737-014-0461-4. [DOI] [PubMed] [Google Scholar]
- 33.Egbert R. Little Mother’s Helper: A Postpartum Health Companion. Rsegbert & Assoc., LLC. 2016. Vers. 1.0.2. Google Play, https://play.google.com/store/apps/details?id=com.littlemothershelper.littlemothershelper&hl=en_US .
- 34.Moment Health. Health. 2018. Moment. Vers. 1.2.2. Google Play, https://play.google.com/store/apps/details?id=io.momenthealth.app&hl=en_US . [Google Scholar]
- 35.PPD ACT. University of North Carolina at Chapel Hill. 2017. Vers. 3.0.0.110. Google Play, https://play.google.com/store/apps/details?id=com.pactforthecure.app .
- 36.MGHPDS MGH Perinatal Depression Scale. 2017. Vers. 1.0.6. Apple App Store, https://apps.apple.com/us/app/mghpds/id1239621118 .
- 37.Postpartum Depression . Pinkdev. 2017. Vers. 1.3. Google Play, https://play.google.com/store/apps/details?id=postnatal.postpartum.depression&hl=en_US . [Google Scholar]
- 38.Post Pregnancy Recovery Hilltop_apps. 2018. Vers. 1.0. Google Play, https://play.google.com/store/apps/details?id=com.andromo.dev695852.app777161&hl=en_US .
- 39.Proto.io, Inc. 2019. Accessed from: https://proto.io/
- 40.Google. Flutter. 2020. Accessed from: https://flutter.dev/
- 41.Sparkol. Videoscribe. 2012. Available: https://www.videoscribe.co/en .
- 42.Nielsen J. Morgan Kaufmann; 1994. Nov, Usability Engineering (1 edition) [Google Scholar]
- 43.Zhang J, Johnson TR, Patel VL, Paige DL, Kubose T. Using usability heuristics to evaluate patient safety of medical devices. Journal of biomedical informatics. 2003 Feb 1;36(1-2):23–30. doi: 10.1016/s1532-0464(03)00060-1. [DOI] [PubMed] [Google Scholar]