Abstract
Although Alzheimer’s disease (AD) is primarily a neurocognitive disorder, it also results in prominent neuropsychiatric symptoms (NPS). Much literature has investigated the NPS of apathy and depression in association with AD, but relatively less is known regarding anxiety, the third most common NPS in this disorder. The prevalence of anxiety symptoms in AD is about 40%, and it can be a prelude of AD. Anxiety can be especially present among patients with mild cognitive impairment, mild dementia, or early-onset forms of the disease, and can promote progression or conversion to Alzheimer’s clinical syndrome. A number of studies have established that anxiety is associated with positive amyloid scans, mesial temporal changes with atrophy and hypometabolism in the entorhinal region, and neurofibrillary tangles present on pathological examination of this region. In addition to psychosocial factors, proposed neurobiological mechanisms for increased anxiety in AD include decreased sensorimotor gating, relatively increased activation of amygdalae or the Salience Network, and the presence of comorbid pathology, particularly Lewy bodies. Having management strategies for anxiety in patients with AD is important as anxiety can worsen cognitive deficits. Interventions involve psychological support, behavioral management, and the judicious use of the psychiatric armamentarium of medications.
Keywords: Alzheimer’s disease, anxiety
INTRODUCTION
Alzheimer’s disease (AD) is the leading cause of dementia, with a worldwide prevalence that continues to rise as populations age. Currently there are almost six million people in the U.S. with AD and many others experience mild cognitive impairment (MCI), which can be a prelude to the Alzheimer’s clinical syndrome [1, 2]. Recent advances in AD have targeted the identification of risk factors and biomarkers. Risk factors for the disorder include advanced age, hypertension, diabetes, smoking, obesity, depression, traumatic brain injury, air pollution, excessive alcohol consumption, hearing impairment, low education, and limited social contact [3]. Additional considerations are the presence of sleep disorders and genetic factor such as having one or more apolipoprotein E (APOE) ɛ4 allele. In addition, there have been significant advances in the clinical diagnosis of AD with cerebrospinal fluid (CSF) and new neuroimaging biomarkers for amyloid and tau [4]. Research and advances are particularly lacking for understanding the neuropsychiatric symptoms (NPS) of AD, especially the role of anxiety.
Most clinicians know AD as a disorder affecting declarative, episodic memory or new learning and other spheres of cognition. Indeed, the typical late onset AD appears as a progressive amnestic disorder with additional deficits in word-finding and language, spatial and visuoperceptual processing, and executive abilities [2]. About 5–6%of patients with AD have an early-onset (EOAD) before age 65 [5], and these patients include a high percentage of variants with predominant language or visuospatial impairments [5].
Regardless of age of onset, AD also results in signi-ficant non-cognitive neuropsychiatric symptoms (NPS) [6], including apathy, depression, anxiety, agitation, aggression, and psychosis [7]. Beyond apathy, depression and anxiety disorders are the most common NPS in AD [8], present in up to 75%of patients with AD [9]. The presence of depression and anxiety have important implications for the patients’ quality of life, caregiver well-being, and likelihood for hospitalizations, institutionalization, and overall mortality [7, 10]. This review focuses on what is known about the relationship of anxiety with AD.
METHODS
A systematic review of the literature was initiated by searching the following electronic databases: PubMed and Google-Scholar. The search consisted of the following terms: “dementia,” “Alzheimer’s disease,” “mild cognitive impairment,” AND “anxiety,” “nervousness,” “psychiatric,” “neuropsychiatric,” “behavior,” “behavioral.” The literature search began October 1, 1995 and concluded October 1, 2020, a span of 25 years. Inclusion criteria for this report were papers available in English and including the following: 1) the inclusion of patients with AD rather than dementia in general; and 2) the presence of anxiety or related words such “nervousness” or “neuroticism”. Using these criteria, the initial search of 237 publications yielded 75 studies for this review. The following discussion focuses on an interpretation of these studies, rather than a comprehensive review of each individual publication.
PREVALENCE OF ANXIETY IN AD
Among the NPS of AD, there have been many investigations of depression [11, 12], but relatively few on anxiety. Yet, the presence of anxiety significantly exacerbates the cognitive impairments of AD, making its early recognition and management particularly important [13]. The prevalence estimates for anxiety in dementia range from 5–21%for anxiety disorders without depression and from 8–90%for significant anxiety symptoms at some time in their course [14–17]. Anxiety may be particularly associated with AD [14, 18–21]. A meta-analysis of 48 studies using the Neuropsychiatric Inventory (NPI) reports a pooled prevalence estimate for anxiety in AD of 39%(95%CI 32–46%) [22]. Anxiety in AD tends to be generalized anxiety with no clear association with demographic factors such as sex, education, or ethnicity [18, 20, 23].
ANXIETY AS A RISK FACTOR FOR AD
A number of recent studies have indicated that anxiety can be a risk factor for AD independent of the presence of depression [24, 25]. In a large longitudinal (4.5 year), community-based study of over four thousand dementia-free persons ≥55 years of age, there was a significant association between anxiety at baseline and eventual AD [25]. In another study of over twelve thousand cognitively asymptomatic participants, anxiety, along with depression and sleep disturbance, independently and as a comorbid factor, was associated with the development of AD [26]. In a third cross-sectional study of 1,417 older adults the majority of whom were cognitively normal, the number of comorbid NPS, including anxiety, was associated with a threefold increased risk of dementia and a twofold increased risk of MCI [27]. Finally, in a large study and meta-analysis of personality studies, participants with high scores on neuroticism, a construct that includes anxiety, and low conscientiousness, showed a threefold increased risk of developing AD on follow-up [28].
ANXIETY AS AN INITIAL OR PRODROMAL SYMPTOM OF AD
Anxiety may be an early manifestation of AD, even heralding the initial stages of cognitive decline [9, 13, 14, 29–35]. Anxiety is particularly present among those with MCI or mild dementia, compared to those with more advanced dementia, especially if they have retained insight into their condition [14, 36–38]. Multiple studies indicate that the presence of anxiety can increase the rate for conversion from MCI to dementia [39–42]. Indeed, longitudinal studies of non-demented patients with positive amyloid scans report that elevated anxiety levels are associated with a more rapid decline, particularly in memory [43–45]. In a comparison of 104 cognitively unimpaired and 53 MCI patients followed for up to 4 years who had anxiety on the Hospital Anxiety and Depression Scale, anxiety was related to amyloid-β (Aβ) deposition on flutemetamol amyloid positron emission tomography (PET) imaging [45]. In this study, the presence of anxiety also predicted cognitive decline and interacted with amyloid status to predict faster cognitive deterioration [45]. But the presence of anxiety among mild AD patients followed for up to 5 years may not predict progression as well as other NPS symptoms on the NPI, such as delusions, agitation, and aberrant motor behavior [46]. Nevertheless, the occurrence of anxiety appears most associated with early AD.
Initial or prodromal anxiety may be most prominent among patients with the early-onset forms of AD that begin at < 65 years of age (EOAD) [14, 18, 47, 48]. EOAD differs from the usual late onset disorder in its high prevalence of nonamnestic phenotypic variants that spare the hippocampi but have greater tau burden in posterior neocortices. In a comparison of 23 EOAD and 22 late-onset AD (LOAD) patients, significantly more EOAD patients reported anxiety on the NPI Anxiety subscale than the LOAD patients (70%versus 27%, respectively) [14]. In another NPI comparison of EOAD (n = 24) and LOAD (n = 56) participants with mild dementia, the EOAD patients had greater prevalence of all NPS except apathy, and they were significantly worse on anxiety (p = 0.03) as well as irritability (p = 0.01) and sleep (p < 0.01) subscales [49]. Others have found equal amounts of NPS on the NPI, including anxiety, among EOAD (n = 35) and LOAD (n = 35) patients [50]. In fact, LOAD patients do experience anxiety, but often as the dementia progresses and in association with comorbid psychiatric and behavioral symptoms [30, 51, 52]. The anxiety in middle or late stages of AD may manifest as agitation and signs of emotional distress, with inappropriate or excessive vocal or motor activity.
ASSOCIATION WITH NEUROPATHOLOGY
Much of the literature has suggested that anxiety is due to AD neuropathology, rather than hippocampal damage due to anxiety-induced mechanisms, such as elevated cortisol levels [42]. Although MRI studies have not found an association between anxiety in AD and gray matter changes [53–55], some investigators have shown increased white matter hyperintensities associated with anxiety, suggesting a vascular component [56]. In another MRI study, the presence of anxiety was associated with greater rates of decrease in entorhinal cortex volume on regions of interest analysis [42]. On fluorodeoxyglucose PET imaging, when investigators controlled for cognitive decline, they showed higher anxiety correlates with lower metabolism in bilateral entorhinal cortex, bilateral anterior parahippocampal gyrus, left anterior superior temporal gyrus, and left insula [57]. After further controlling for other NPS, their results were still significant in the right entorhinal cortex and parahippocampal gyrus. An older study looking at regional cerebral blood flow additionally suggested decreased parietal hypometabolism [58]; however, they were not able to confirm this finding in a subsequent study [57]. In sum, anxiety may be associated with involvement of the mesial temporal lobe, particularly the entorhinal region [42, 57, 59].
Several studies have shown an association of anxiety with biomarkers of AD pathology. Among patients with MCI or AD, there is a significant correlation between NPS and an increased CSF t-tau/Aβ42 ratio, a biomarker of AD neuropathology [38]. A number of amyloid PET investigations report increased anxiety measures with positive amyloid PET imaging and faster cognitive decline [35, 43–45]. In another amyloid PET study of 270 community-dwelling, cognitively normal elderly individuals followed for 1–5 years, steeper rates of increase for anxiety-concentration scores were associated with higher Pittsburgh Compound B PET-binding for amyloid [35]. These results persisted despite adjusting for depression history and intellectual background on a reading test, consistent with increasing anxiety with increasing Aβ burden over time [35]. In an autopsy study, postmortem interviews of informants for a cohort to 455 cases revealed that Braak I/II pathology (neurofibrillary tangles in transentorhinal/entorhinal region), significantly increased the odds of having anxiety, agitation, appetite changes, depression, and sleep disturbances, compared to controls, but there was no increased odds for anxiety with Aβ pathology or with worsening Braak stages [60]. Together, these findings suggest that anxiety is associated with early neurofibrillary tangle pathology in the entorhinal region in the presence of minimal cortical pathology [60].
POTENTIAL MECHANISMS FOR ANXIETY IN AD
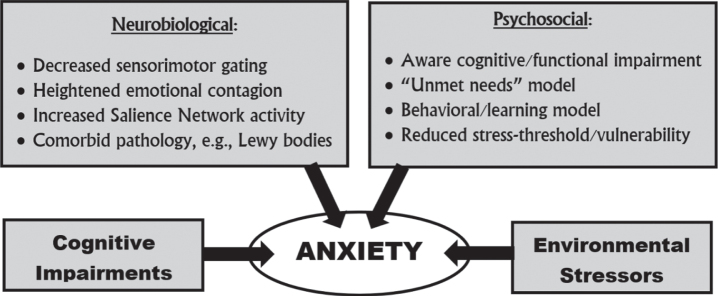
There are several possible neurobiological reasons for an association of anxiety with AD (see Fig. 1). First, anxiety in mild AD may result from a widening attentional refocusing to (potentially threatening) socioemotional stimuli from decreased sensorimotor gating of environmental stimuli, a process suggested by a failure to inhibit an acoustic startle response with a preceding softer noise (“prepulse inhibition”) [61]. AD pathology in the entorhinal cortex may lead to decreased sensorimotor gating with larger initial orienting responses than normal, indicating enhanced perceptual processing of significant environmental stimuli [47, 62]. Second, in MCI and AD, early neurodegeneration in right mesial temporal lobes, with entorhinal involvement and relatively preserved amygdala, may lead to amygdalar hyperactivity and heightened emotional contagion [9, 47]. Emotional contagion is a primitive, rapid, and automatic synchronization of emotional and physiological states with another person [9, 63]. Third, anxiety may be secondary to a release of emotion generating structures in the salience network (SN) (an anterior insula-anterior cingulate predominant network). Increased SN activity results in increased visceromotor responsivity and emotional upregulation [9]. Finally, anxiety may be related to the presence of comorbid neuropathology, such as vascular changes or the presence of Lewy bodies. Anxiety is a common and early manifestation in dementia with Lewy bodies, and Lewy bodies are a frequent comorbidity of AD neuropathology [64–66].
Fig. 1.
Potential mechanisms for anxiety in Alzheimer’s disease.
Beyond potential neurobiological explanations, there are possible psychosocial reasons for an association of anxiety with AD. Among patients with sufficient insight, the presence of anxiety could reflect a psychological reaction to their cognitive impairments early in the course of their disease. This anxiety is worse with caregiver separation and observing their performance on neurocognitive testing [14], and it is facilitated if there is preservation of right frontal and anterior cingulate regions involved in self-criticism [67]. In this last case, decreasing the threat posed by psychological symptoms may be one avenue for possibly delaying the onset of dementia due to AD [26]. As dementia progresses, there is further anxiety from the accumulation of cognitive and associated functional impairments and the inability to cope with environmental stressors [68, 69]. Importantly, AD patients have “unmet needs”, such as physical discomforts and socioemotional difficulties, which they cannot effectively communicate and may go unrecognized [69–71]. One model of behavioral symptoms in dementia stresses the progressive inability to handle stress from discomforts or difficulties [69, 70]. Patients with advanced AD may even learn to use disruptive behaviors, such as shouting or aggression, in order to gain attention to themselves and their discomforts or difficulties [71].
MANAGEMENT AND TREATMENT
The treatment of anxiety in AD and dementia usually consists of a combination of reassurance and support associated with limited use of pharmacotherapy. Removing precipitating or anxiety-producing triggers, responding to potential unmet needs, and maintaining a calm environment and steady routine can be most effective in managing anxiety and resultant agitation in AD. Treating anxiety includes managing intercurrent factors and comorbid conditions such as medication side-effects, sleep disturbances, and intercurrent medical conditions. Additional non-pharmacological techniques, such as visual arts, music, exercise programs, and aromatherapy should be considered [70, 71], and cognitive intervention therapy such as cognitive rehabilitation may be especially helpful for alleviating anxiety among those with MCI or mild dementia [69]. If behavioral or environmental intervention is insufficient, short-term use of benzodiazepines or the initiation of a selective serotonin reuptake inhibitor, are the drugs of choice. Low dose trazodone, particularly at bedtime, is an alternative when poor sleep or nocturnal agitation are factors. There can be psychoactive effects of the dementia medications, with acetylcholinesterase inhibitors occasionally worsening anxiety in some patients and memantine producing anxiety in others. Finally, if anxiety is severe and associated with agitation or physical aggression, clinicians may need to administer an atypical antipsychotic, despite the presence of a black-box warning label of increased morbidity and mortality with antipsychotic use in dementia.
CONCLUSIONS
AD manifests as a cognitive disorder; however, NPS are equally a part of the disease. Much literature has explored the apathy and depression associated with AD, but relatively less is known regarding anxiety, which is present in about 40%of AD patients. Anxiety often occurs early in the course of AD, especially among patients with MCI, mild dementia, or early-onset forms of the disease, and can promote progression and conversion from MCI to dementia. Anxiety is associated with positive amyloid scans and with mesial temporal changes in the entorhinal region, including atrophy, hypometabolism, and the presence of neurofibrillary tangles. The proposed mechanisms for anxiety in AD range from the neurobiological to the psychosocial and include contributions from cognitive impairments and environmental stressors. The management strategies for anxiety in patients with AD are important as anxiety can worsen cognitive deficits. Interventions involves psychological support, behavioral management, environmental changes, and, if necessary, the careful use of psychoactive medications.
CONFLICT OF INTEREST
The author has no conflict of interest to report.
ACKNOWLEDGMENTS
This work is supported by US National Institute on Aging Grant 1RF1AG050967.
REFERENCES
- [1]. Rabinovici GD (2019) Late-onset Alzheimer disease. Continuum (Minneap Minn) 25, 14–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr., Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7, 263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimaki M, Larson EB, Ogunniyi A, Orgeta V, Ritchie K, Rockwood K, Sampson EL, Samus Q, Schneider LS, Selbaek G, Teri L, Mukadam N (2020) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Jack CR Jr., Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, Holtzman DM, Jagust W, Jessen F, Karlawish J, Liu E, Molinuevo JL, Montine T, Phelps C, Rankin KP, Rowe CC, Scheltens P, Siemers E, Snyder HM, Sperling R, Contributors (2018) NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement 14, 535–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Mendez MF (2019) Early-onset Alzheimer disease and its variants. Continuum (Minneap Minn) 25, 34–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Fernandez M, Gobartt AL, Balana M, COOPERA Study Group (2010) Behavioural symptoms in patients with Alzheimer’s disease and their association with cognitive impairment. BMC Neurol 10, 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Lyketsos CG, Carrillo MC, Ryan JM, Khachaturian AS, Trzepacz P, Amatniek J, Cedarbaum J, Brashear R, Miller DS (2011) Neuropsychiatric symptoms in Alzheimer’s disease. Alzheimers Dement 7, 532–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Woolley JD, Khan BK, Murthy NK, Miller BL, Rankin KP (2011) The diagnostic challenge of psychiatric symptoms in neurodegenerative disease: Rates of and risk factors for prior psychiatric diagnosis in patients with early neurodegenerative disease. J Clin Psychiatry 72, 126–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Sturm VE, Yokoyama JS, Seeley WW, Kramer JH, Miller BL, Rankin KP (2013) Heightened emotional contagion in mild cognitive impairment and Alzheimer’s disease is associated with temporal lobe degeneration. Proc Natl Acad Sci U S A 110, 9944–9949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Garcia-Alberca JM, Cruz B, Lara JP, Garrido V, Lara A, Gris E (2012) Anxiety and depression are associated with coping strategies in caregivers of Alzheimer’s disease patients: Results from the MALAGA-AD study. Int Psychogeriatr 24, 1325–1334. [DOI] [PubMed] [Google Scholar]
- [11]. Burke AD, Goldfarb D, Bollam P, Khokher S (2019) Diagnosing and treating depression in patients with Alzheimer’s disease. Neurol Ther 8, 325–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Galts CPC, Bettio LEB, Jewett DC, Yang CC, Brocardo PS, Rodrigues ALS, Thacker JS, Gil-Mohapel J (2019) Depression in neurodegenerative diseases: Common mechanisms and current treatment options. Neurosci Biobehav Rev 102, 56–84. [DOI] [PubMed] [Google Scholar]
- [13]. Seignourel PJ, Kunik ME, Snow L, Wilson N, Stanley M (2008) Anxiety in dementia: A critical review. Clin Psychol Rev 28, 1071–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Kaiser NC, Liang LJ, Melrose RJ, Wilkins SS, Sultzer DL, Mendez MF (2014) Differences in anxiety among patients with early- versus late-onset Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 26, 73–80. [DOI] [PubMed] [Google Scholar]
- [15]. Lyketsos CG, Steinberg M, Tschanz JT, Norton MC, Steffens DC, Breitner JC (2000) Mental and behavioral disturbances in dementia: Findings from the Cache County Study on Memory in Aging. Am J Psychiatry 157, 708–714. [DOI] [PubMed] [Google Scholar]
- [16]. Garcia-Alberca JM, Lara JP, Berthier ML, Cruz B, Barbancho MA, Green C, Gonzalez-Baron S (2011) Can impairment in memory, language and executive functions predict neuropsychiatric symptoms in Alzheimer’s disease (AD)? Findings from a cross-sectional study. Arch Gerontol Geriatr 52, 264–269. [DOI] [PubMed] [Google Scholar]
- [17]. Craig D, Mirakhur A, Hart DJ, McIlroy SP, Passmore AP (2005) A cross-sectional study of neuropsychiatric symptoms in 435 patients with Alzheimer’s disease. Am J Geriatr Psychiatry 13, 460–468. [DOI] [PubMed] [Google Scholar]
- [18]. Porter VR, Buxton WG, Fairbanks LA, Strickland T, O’Connor SM, Rosenberg-Thompson S, Cummings JL (2003) Frequency and characteristics of anxiety among patients with Alzheimer’s disease and related dementias. J Neuropsychiatry Clin Neurosci 15, 180–186. [DOI] [PubMed] [Google Scholar]
- [19]. Mintzer JE, Brawnman-Mintzer O, Mirski DF, Barkin K (2000) Anxiety in the behavioral and psychological symptoms of dementia. Int Psychogeriatr 12, 139–142. [Google Scholar]
- [20]. Teri L, Ferretti LE, Gibbons LE, Logsdon RG, McCurry SM, Kukull WA, McCormick WC, Bowen JD, Larson EB (1999) Anxiety of Alzheimer’s disease: Prevalence, and comorbidity. J Gerontol A Biol Sci Med Sci 54, M348–352. [DOI] [PubMed] [Google Scholar]
- [21]. Tractenberg RE, Patterson M, Weiner MF, Teri L, Grundman M, Thomas RG, Thal LJ (2000) Prevalence of symptoms on the CERAD behavior rating scale for dementia in normal elderly subjects and Alzheimer’s disease patients. J Neuropsychiatry Clin Neurosci 12, 472–479. [DOI] [PubMed] [Google Scholar]
- [22]. Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, Xu W, Li JQ, Wang J, Lai TJ, Yu JT (2016) The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: Systematic review and meta-analysis. J Affect Disord 190, 264–271. [DOI] [PubMed] [Google Scholar]
- [23]. Ownby RL, Harwood DG, Barker WW, Duara R (2000) Predictors of anxiety in patients with Alzheimer’s disease. Depress Anxiety 11, 38–42. [DOI] [PubMed] [Google Scholar]
- [24]. Santabarbara J, Lopez-Anton R, de la Camara C, Lobo E, Gracia-Garcia P, Villagrasa B, Bueno-Notivol J, Marcos G, Lobo A (2019) Clinically significant anxiety as a risk factor for dementia in the elderly community. Acta Psychiatr Scand 139, 6–14. [DOI] [PubMed] [Google Scholar]
- [25]. Santabarbara J, Villagrasa B, Lopez-Anton R, Olaya B, Bueno-Notivol J, de la Camara C, Gracia-Garcia P, Lobo E, Lobo A (2019) Clinically relevant anxiety and risk of Alzheimer’s disease in an elderly community sample: 4.5 years of follow-up. J Affect Disord 250, 16–20. [DOI] [PubMed] [Google Scholar]
- [26]. Burke SL, Cadet T, Alcide A, O’Driscoll J, Maramaldi P (2018) Psychosocial risk factors and Alzheimer’s disease: The associative effect of depression, sleep disturbance, and anxiety. Aging Ment Health 22, 1577–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Mortby ME, Burns R, Eramudugolla R, Ismail Z, Anstey KJ (2017) Neuropsychiatric symptoms and cognitive impairment: Understanding the importance of co-morbid symptoms. J Alzheimers Dis 59, 141–153. [DOI] [PubMed] [Google Scholar]
- [28]. Terracciano A, Sutin AR, An Y, O’Brien RJ, Ferrucci L, Zonderman AB, Resnick SM (2014) Personality and risk of Alzheimer’s disease: New data and meta-analysis. Alzheimers Dement 10, 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Pocnet C, Rossier J, Antonietti JP, von Gunten A (2013) Personality traits and behavioral and psychological symptoms in patients at an early stage of Alzheimer’s disease. Int J Geriatr Psychiatry 28, 276–283. [DOI] [PubMed] [Google Scholar]
- [30]. Hynninen MJ, Breitve MH, Rongve A, Aarsland D, Nordhus IH (2012) The frequency and correlates of anxiety in patients with first-time diagnosed mild dementia. Int Psychogeriatr 24, 1771–1778. [DOI] [PubMed] [Google Scholar]
- [31]. Van der Mussele S, Le Bastard N, Vermeiren Y, Saerens J, Somers N, Marien P, Goeman J, De Deyn PP, Engelborghs S (2013) Behavioral symptoms in mild cognitive impairment as compared with Alzheimer’s disease and healthy older adults. Int J Geriatr Psychiatry 28, 265–275. [DOI] [PubMed] [Google Scholar]
- [32]. Duchek JM, Balota DA, Storandt M, Larsen R (2007) The power of personality in discriminating between healthy aging and early-stage Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci 62, P353–361. [DOI] [PubMed] [Google Scholar]
- [33]. Sollberger M, Stanley CM, Wilson SM, Gyurak A, Beckman V, Growdon M, Jang J, Weiner MW, Miller BL, Rankin KP (2009) Neural basis of interpersonal traits in neurodegenerative diseases. Neuropsychologia 47, 2812–2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34]. Rosenberg PB, Mielke MM, Appleby BS, Oh ES, Geda YE, Lyketsos CG (2013) The association of neuropsychiatric symptoms in MCI with incident dementia and Alzheimer disease. Am J Geriatr Psychiatry 21, 685–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35]. Donovan NJ, Locascio JJ, Marshall GA, Gatchel J, Hanseeuw BJ, Rentz DM, Johnson KA, Sperling RA, Harvard Aging Brain S (2018) Longitudinal association of amyloid beta and anxious-depressive symptoms in cognitively normal older adults. Am J Psychiatry 175, 530–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36]. Calleo JS, Kunik ME, Reid D, Kraus-Schuman C, Paukert A, Regev T, Wilson N, Petersen NJ, Snow AL, Stanley M (2011) Characteristics of generalized anxiety disorder in patients with dementia. Am J Alzheimers Dis Other Demen 26, 492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37]. Derouesne C, Thibault S, Lagha-Pierucci S, Baudouin-Madec V, Ancri D, Lacomblez L (1999) Decreased awareness of cognitive deficits in patients with mild dementia of the Alzheimer type. Int J Geriatr Psychiatry 14, 1019–1030. [PubMed] [Google Scholar]
- [38]. Scaricamazza E, Colonna I, Sancesario GM, Assogna F, Orfei MD, Franchini F, Sancesario G, Mercuri NB, Liguori C (2019) Neuropsychiatric symptoms differently affect mild cognitive impairment and Alzheimer’s disease patients: A retrospective observational study. Neurol Sci 40, 1377–1382. [DOI] [PubMed] [Google Scholar]
- [39]. Stella F, Radanovic M, Balthazar ML, Canineu PR, de Souza LC, Forlenza OV (2014) Neuropsychiatric symptoms in the prodromal stages of dementia. Curr Opin Psychiatry 27, 230–235. [DOI] [PubMed] [Google Scholar]
- [40]. Li XX, Li Z (2018) The impact of anxiety on the progression of mild cognitive impairment to dementia in Chinese and English data bases: A systematic review and meta-analysis. Int J Geriatr Psychiatry 33, 131–140. [DOI] [PubMed] [Google Scholar]
- [41]. Somme J, Fernandez-Martinez M, Molano A, Zarranz JJ (2013) Neuropsychiatric symptoms in amnestic mild cognitive impairment: Increased risk and faster progression to dementia. Curr Alzheimer Res 10, 86–94. [DOI] [PubMed] [Google Scholar]
- [42]. Mah L, Binns MA, Steffens DC, Alzheimer’s Disease Neuroimaging Initiative (2015) Anxiety symptoms in amnestic mild cognitive impairment are associated with medial temporal atrophy and predict conversion to Alzheimer disease. Am J Geriatr Psychiatry 23, 466–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43]. Pietrzak RH, Lim YY, Neumeister A, Ames D, Ellis KA, Harrington K, Lautenschlager NT, Restrepo C, Martins RN, Masters CL, Villemagne VL, Rowe CC, Maruff P, Australian Imaging, Biomarkers, andLifestyle Research Group (2015) Amyloid-beta, anxiety, and cognitive decline in preclinical Alzheimer disease: A multicenter, prospective cohort study. JAMA Psychiatry 72, 284–291. [DOI] [PubMed] [Google Scholar]
- [44]. Pietrzak RH, Scott JC, Neumeister A, Lim YY, Ames D, Ellis KA, Harrington K, Lautenschlager NT, Szoeke C, Martins RN, Masters CL, Villemagne VL, Rowe CC, Maruff P, Australian Imaging, Biomarkers and Lifestyle Research Group (2014) Anxiety symptoms, cerebral amyloid burden and memory decline in healthy older adults without dementia: 3-year prospective cohort study. Br J Psychiatry 204, 400–401. [DOI] [PubMed] [Google Scholar]
- [45]. Johansson M, Stomrud E, Lindberg O, Westman E, Johansson PM, van Westen D, Mattsson N, Hansson O (2020) Apathy and anxiety are early markers of Alzheimer’s disease. Neurobiol Aging 85, 74–82. [DOI] [PubMed] [Google Scholar]
- [46]. Hallikainen I, Hongisto K, Valimaki T, Hanninen T, Martikainen J, Koivisto AM (2018) The progression of neuropsychiatric symptoms in Alzheimer’s disease during a five-year follow-up: Kuopio ALSOVA Study. J Alzheimers Dis 61, 1367–1376. [DOI] [PubMed] [Google Scholar]
- [47]. Joshi A, Jimenez E, Mendez MF (2017) Initial heart rate reactivity to socioemotional pictures in early-onset Alzheimer’s disease. J Alzheimers Dis 60, 1325–1332. [DOI] [PubMed] [Google Scholar]
- [48]. Brodaty H, Connors MH, Xu J, Woodward M, Ames D, PRIME study group (2015) The course of neuropsychiatric symptoms in dementia: A 3-year longitudinal study. J Am Med Dir Assoc 16, 380–387. [DOI] [PubMed] [Google Scholar]
- [49]. Baillon S, Gasper A, Wilson-Morkeh F, Pritchard M, Jesu A, Velayudhan L (2019) Prevalence and severity of neuropsychiatric symptoms in early- versus late-onset Alzheimer’s disease. Am J Alzheimers Dis Other Demen 34, 433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50]. Ferreira MDC, Abreu MJ, Machado C, Santos B, Machado A, Costa AS (2018) Neuropsychiatric profile in early versus late onset Alzheimer’s disease. Am J Alzheimers Dis Other Demen 33, 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51]. van Vliet D, deVugt ME, Aalten P, Bakker C, Pijnenburg YA, Vernooij-Dassen MJ, Koopmans RT, Verhey FR (2012) Prevalence of neuropsychiatric symptoms in young-onset compared to late-onset Alzheimer’s disease - part 1: Findings of the two-year longitudinal NeedYD-study. Dement Geriatr Cogn Disord 34, 319–327. [DOI] [PubMed] [Google Scholar]
- [52]. Tanaka H, Hashimoto M, Fukuhara R, Ishikawa T, Yatabe Y, Kaneda K, Yuuki S, Honda K, Matsuzaki S, Tsuyuguchi A, Hatada Y, Ikeda M (2015) Relationship between dementia severity and behavioural and psychological symptoms in early-onset Alzheimer’s disease. Psychogeriatrics 15, 242–247. [DOI] [PubMed] [Google Scholar]
- [53]. Serra L, Perri R, Cercignani M, Spano B, Fadda L, Marra C, Carlesimo GA, Caltagirone C, Bozzali M (2010) Are the behavioral symptoms of Alzheimer’s disease directly associated with neurodegeneration? J Alzheimers Dis 21, 627–639. [DOI] [PubMed] [Google Scholar]
- [54]. Horinek D, Petrovicky P, Hort J, Krasensky J, Brabec J, Bojar M, Vaneckova M, Seidl Z (2006) Amygdalar volume and psychiatric symptoms in Alzheimer’s disease: An MRI analysis. Acta Neurol Scand 113, 40–45. [DOI] [PubMed] [Google Scholar]
- [55]. Poulin SP, Dautoff R, Morris JC, Barrett LF, Dickerson BC, Alzheimer’s Disease Neuroimaging Initiative (2011) Amygdala atrophy is prominent in early Alzheimer’s disease and relates to symptom severity. Psychiatry Res 194, 7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56]. Berlow YA, Wells WM, Ellison JM, Sung YH, Renshaw PF, Harper DG (2010) Neuropsychiatric correlates of white matter hyperintensities in Alzheimer’s disease. Int J Geriatr Psychiatry 25, 780–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57]. Hashimoto H, Monserratt L, Nguyen P, Feil D, Harwood D, Mandelkern MA, Sultzer DL (2006) Anxiety and regional cortical glucose metabolism in patients with Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 18, 521–528. [DOI] [PubMed] [Google Scholar]
- [58]. Sultzer DL, Mahler ME, Mandelkern MA, Cummings JL, Van Gorp WG, Hinkin CH, Berisford MA (1995) The relationship between psychiatric symptoms and regional cortical metabolism in Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 7, 476–484. [DOI] [PubMed] [Google Scholar]
- [59]. Victoroff J, Lin FV, Coburn KL, Shillcutt SD, Voon V, Ducharme S (2018) Noncognitive behavioral changes associated with Alzheimer’s disease: Implications of neuroimaging findings. J Neuropsychiatry Clin Neurosci 30, 14–21. [DOI] [PubMed] [Google Scholar]
- [60]. Ehrenberg AJ, Suemoto CK, Franca Resende EP, Petersen C, Leite REP, Rodriguez RD, Ferretti-Rebustini REL, You M, Oh J, Nitrini R, Pasqualucci CA, Jacob-Filho W, Kramer JH, Gatchel JR, Grinberg LT (2018) Neuropathologic correlates of psychiatric symptoms in Alzheimer’s disease. J Alzheimers Dis 66, 115–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61]. Ueki A, Goto K, Sato N, Iso H, Morita Y (2006) Prepulse inhibition of acoustic startle response in mild cognitive impairment and mild dementia of Alzheimer type. Psychiatry Clin Neurosci 60, 55–62. [DOI] [PubMed] [Google Scholar]
- [62]. Bradley MM (2009) Natural selective attention: Orienting and emotion. Psychophysiology 46, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63]. Rankin KP, Kramer JH, Miller BL (2005) Patterns of cognitive and emotional empathy in frontotemporal lobar degeneration. Cogn Behav Neurol 18, 28–36. [DOI] [PubMed] [Google Scholar]
- [64]. Segers K, Benoit F, Meyts JM, Surquin M (2020) Anxiety symptoms are quantitatively and qualitatively different in dementia with Lewy bodies than in Alzheimer’s disease in the years preceding clinical diagnosis. Psychogeriatrics 20, 242–246. [DOI] [PubMed] [Google Scholar]
- [65]. Bayram E, Shan G, Cummings JL (2019) Associations between comorbid TDP-43, Lewy body pathology, and neuropsychiatric symptoms in Alzheimer’s disease. J Alzheimers Dis 69, 953–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66]. Taragano FE, Allegri RF, Heisecke SL, Martelli MI, Feldman ML, Sanchez V, Garcia VA, Tufro G, Castro DM, Leguizamon PP, Guelar V, Ruotolo E, Zegarra C, Dillon C (2018) Risk of conversion to dementia in a mild behavioral impairment group compared to a psychiatric group and to a mild cognitive impairment group. J Alzheimers Dis 62, 227–238. [DOI] [PubMed] [Google Scholar]
- [67]. Shinagawa S, Babu A, Sturm V, Shany-Ur T, Toofanian Ross P, Zackey D, Poorzand P, Grossman S, Miller BL, Rankin KP (2015) Neural basis of motivational approach and withdrawal behaviors in neurodegenerative disease. Brain Behav 5, e00350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68]. Cohen-Mansfield J, Mintzer JE (2005) Time for change: The role of nonpharmacological interventions in treating behavior problems in nursing home residents with dementia. Alzheimer Dis Assoc Disord 19, 37–40. [DOI] [PubMed] [Google Scholar]
- [69]. Garcia-Alberca JM (2015) Cognitive intervention therapy as treatment for behaviour disorders in Alzheimer disease: Evidence on efficacy and neurobiological correlations. Neurologia 30, 8–15. [DOI] [PubMed] [Google Scholar]
- [70]. Cohen-Mansfield J (2001) Nonpharmacologic interventions for inappropriate behaviors in dementia: A review, summary, and critique. Am J Geriatr Psychiatry 9, 361–381. [PubMed] [Google Scholar]
- [71]. Cohen-Mansfield J (2018) Non-pharmacological interventions for persons with dementia: What are they and how should they be studied? Int Psychogeriatr 30, 281–283. [DOI] [PubMed] [Google Scholar]