Case Report
A 39-year-old female patient, without medical history, presented symptoms of holocranial headache and vomiting for 2 months before a single tonic-clonic seizure. In the postictal period, she presented with left hemiparesis that completely resolved over a couple of weeks without medical therapy other than phenytoin. The neurologic examination was unremarkable after that.
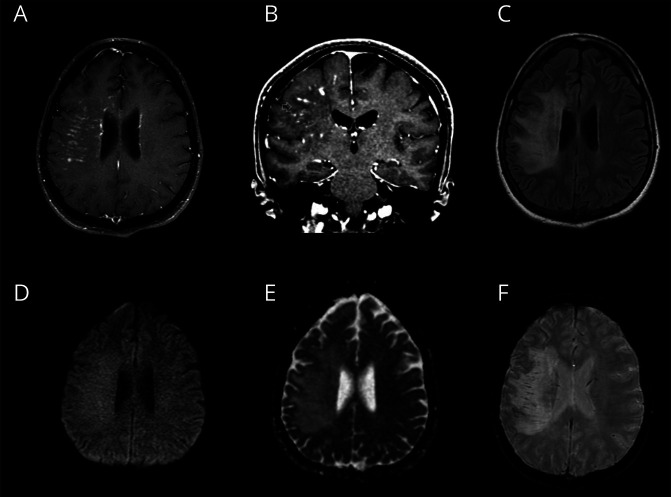
Brain MRI revealed subcortical and periventricular white matter lesions in the right frontoparietal and insular lobes, with a perivascular punctate and curvilinear enhancement, with no restricted diffusion, associated with edema without significative mass effect (figure 1). MRI angiography, including vessel wall sequences, did not show vascular stenosis or signs of vasculitis. CSF analysis showed slightly elevated protein levels (49 mg/dL) and cytology with 5 white blood cells; there were no oligoclonal bands, and protein electrophoresis was normal. Infectious screening of CSF was negative for herpes simplex virus I/II, Cytomegalovirus, Adenovirus, Mycobacterium tuberculosis, Varicella zoster virus, human herpesvirus 6/7, and Enterovirus. In addition, neoplastic cells were not detected in CSF. The investigation was also negative for Treponema pallidum, HIV, and hepatitis B and C. The screening for systemic autoimmunity and neoplastic diseases, including FDG PET-CT, was unremarkable.
Figure 1. MRI.
Perivascular enhancement, occasionally assuming a nodular configuration, in periventricular and subcortical right frontoparietal white matter (A and B). Extension to the insula and edema are also seen (C). No restricted diffusion is demonstrated (D and E). Mild enlarged vascular structures are seen in correspondence to enhancement zones in susceptibility imaging (F).
The patient underwent neuronavigation-guided open biopsy of a contrast-enhancing region in the inferior frontal gyrus. Samples were sent for neuropathologic analysis and flow cytometry. Immunophenotyping was negative for abnormal hematologic cells. The neuropathologic study revealed leptomeningeal and perivascular inflammation with parenchymal infiltration consisting of CD4 reactive T lymphocytes and occasional CD8-, C20-, and CD86-positive lymphocytes (figures e-1 and e-2, links.lww.com/NXI/A463 and links.lww.com/NXI/A464, respectively). There were no lesions on vessel walls and no granulomas, malignant cells, or myelin loss. The patient was treated with oral prednisone (60 mg/d) for 6 weeks, followed by a taper. She remained asymptomatic during treatment. Posttreatment MRI revealed resolution of the gadolinium-enhancing lesions (figure e-3, links.lww.com/NXI/A465).
Discussion
The original description of CLIPPERS emphasizes the involvement of the pons,1 and the most recent set of criteria2 require pontocerebellar involvement. However, more than half of patients with CLIPPERS have supratentorial involvement with imaging patterns similar to those seen in the brainstem, as shown by the largest cohort to date.3 In addition, in another study where autopsy and high-field 7T MRI were performed in patients with CLIPPERS, the authors suggest that there may be a more widespread perivascular inflammation, with a demonstration of supratentorial involvement that was not detected on 3T MRI.4 Although 3 similar cases have previously been reported presenting as an exclusively supratentorial inflammatory disorder with curvilinear enhancement on MRI responsiveness to steroids, and perivascular T lymphocyte infiltrate on biopsy; they were published in abstract form with no images available on the brain MRI or neuropathology.5,6 The disorder described was remarkably similar to CLIPPERS, with the exception that there was no pontocerebellar involvement. The authors suggested that these cases were a CLIPPERS variant and proposed to name it “supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids (SLIPPERS).”
Our patient, similarly to the SLIPPERS cases reported, had a chronic perivascular lymphocytic inflammatory disorder that was remarkably responsive to steroids but lacked the pontocerebellar involvement to fulfill the CLIPPERS criteria. Histopathology ruled out lymphoproliferative disorders and vasculitis, which are commonly described as CLIPPERS mimics.3 Although not tested for antiglial fibrillary acidic protein (GFAP) antibodies, the clinical presentation, CSF profile, histopathology in our case was not typical of the recently described autoimmune GFAP astrocytopathy.7
CLIPPERS is currently regarded as a syndrome, and evidence is not robust enough to consider it a distinctive disease. Hypotheses that have been contemplated include that (1) it is prestage or unusual presentation of well-determined diseases such as autoimmune gliopathies or vasculitis; (2) it is a prelymphoma state that could progress to lymphoma (i.e., primary CNS lymphoma); or (3) it is a manifestation of a disease still not fully understood.3 In keeping with this rationale, it is conceivable that SLIPPERS may have physiopathologic mechanisms akin to that of CLIPPERS and may represent another end of a spectrum of disorders with perivascular enhancement and responsiveness to steroids.
The pathogenesis of CLIPPERS and its predisposition for the pontine region remain unknown. Our description of the hemispheric pattern of involvement of a CLIPPERS-like disease suggests an autoimmune etiology. Long-term follow-up is necessary to exclude malignant transformation and to reach consistent conclusions. Despite that, we strongly believe that this description, and those previously named as SLIPPERS, supports the idea that all of them are a CLIPPERS-variant presentation with isolated supratentorial involvement. Therefore, we suggest the acronym extra pontine CLIPPERS, to stress the similarities between them, until more comprehensive understanding of this disorder is reached.
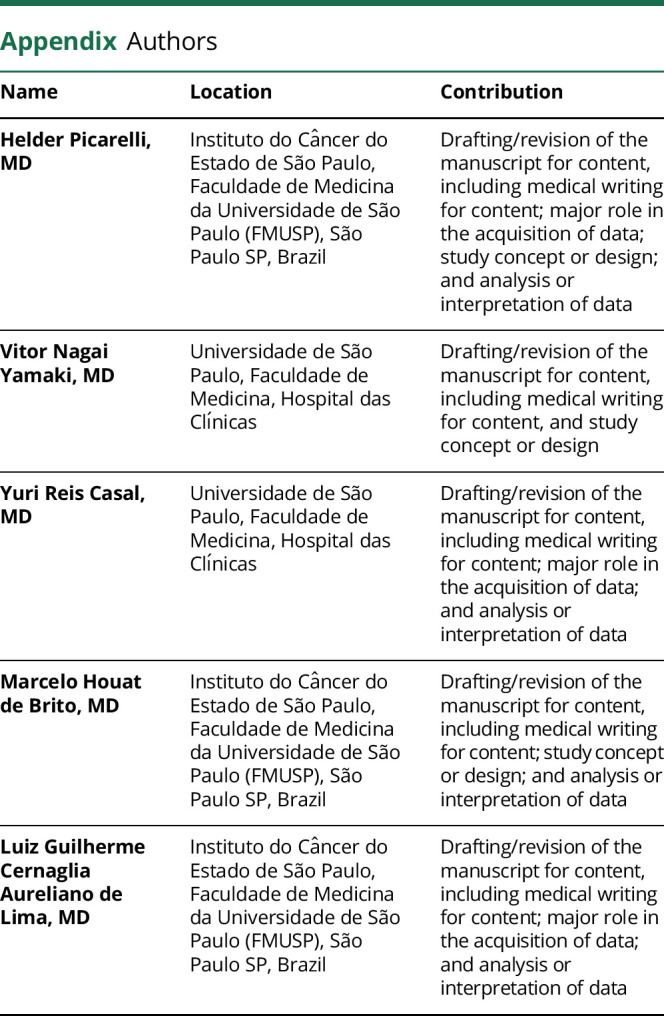
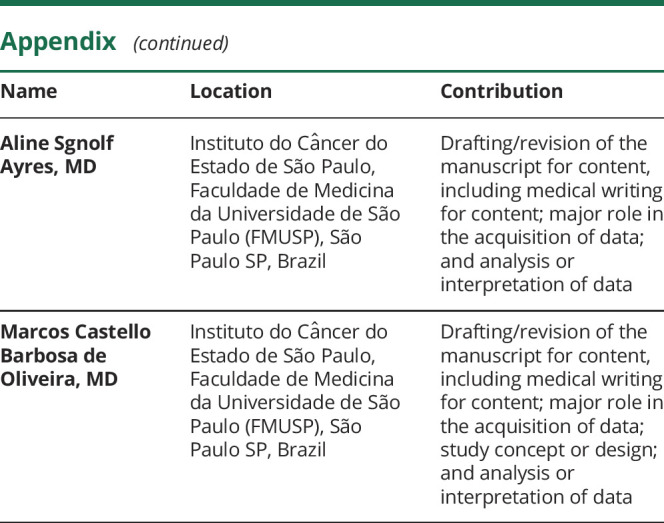
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
The authors report no competing interests. Go to Neurology.org/NN for full disclosures.
References
- 1.Pittock SJ, Debruyne J, Krecke KN, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain 2010;133:2626–2634. [DOI] [PubMed] [Google Scholar]
- 2.Tobin WO, Guo Y, Krecke KN, et al. Diagnostic criteria for chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain 2017;140:2415–2425. [DOI] [PubMed] [Google Scholar]
- 3.Taieb G, Mulero P, Psimaras D, et al. CLIPPERS and its mimics: evaluation of new criteria for the diagnosis of CLIPPERS. J Neurol Neurosurg Psychiatry 2019;90:1027–1038. [DOI] [PubMed] [Google Scholar]
- 4.Blaabjerg M, Ruprecht K, Sinnecker T, et al. Widespread inflammation in CLIPPERS syndrome indicated by autopsy and ultra-high-field 7T MRI. Neurol Neuroimmunol Neuroinflammation 2016;3:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Armand C, Graber J, Lado F, LaSala P, Weidenheim K. SLIPPERS: supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids: a case report (P5.118). Neurology 2015;84:P5.118. [Google Scholar]
- 6.Horng S, Crary J, Fabian M. A case of SLIPPERS (supratentorial lymphocytic inflammation with parenchymal perivascular enhancement responsive to steroids) presenting with isolated cognitive dysfunction. (P1.336). Neurology 2017;88:336. [Google Scholar]
- 7.Kunchok A, Zekeridou A, McKeon A. Autoimmune glial fibrillary acidic protein astrocytopathy. Curr Opin Neurol 2019;32:452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]