Abstract
Background
Non-regular workers are steadily increasing on account of improving corporate productivity. They are classified as non-permanent, part-time, or non-typical workers. Non-regular work has a negative impact on workers' physical and mental health. This study analyzed the relationship between non-permanent, part-time and non-typical work and insomnia among Korean wage workers, and investigated the differences and interactions between different work patterns.
Methods
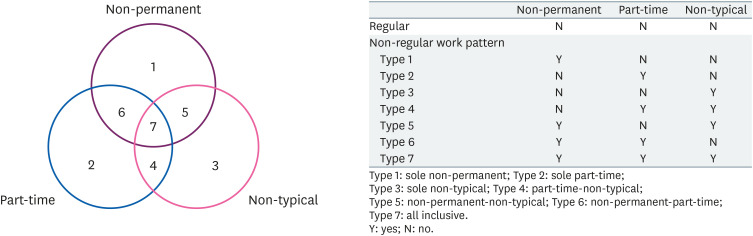
The Fifth Korean Working Conditions Survey was used in this study. Non-regular work patterns were classified into 7 types: type 1, sole non-permanent; type 2, sole part-time; type 3, sole non-typical; type 4, part-time-non-typical; type 5, non-permanent-non-typical; type 6, non-permanent-part-time; type 7, all inclusive. Insomnia was measured on a scale from “normal sleep” to “insomnia” based on the 3-item Minimal Insomnia Symptom Scale. Multiple logistic regression was used to analyze the association between non-regular work patterns and insomnia among wage workers.
Results
After multivariate adjustment, a significantly increased odds ratio (OR) for insomnia was found in types 1, 2, 3, 4, 5, 6, and 7 of non-regular work patterns compared to regular work patterns. After stratification for shift and night work, the OR of the group with shift and night work was higher than that of the group without shift and night work.
Conclusions
Insomnia was significantly associated with non-regular work patterns. This association was prominent in workers with shifts and night work. This finding suggests that proper work patterns may be needed to reduce the risk of insomnia among Korean wage workers and workers who initially had insomnia should consider these results before placement.
Keywords: Non-regular worker, Work patterns, Insomnia, Minimal Insomnia Symptom Scale, Korean Working Condition Survey
BACKGROUND
After the 1997 financial crisis, South Korean companies tried to reduce labor costs and gain employment flexibility for productivity, which resulted in an increase in non-regular workers [1,2]. According to the 2018 additional survey of the economically active population by Statistics Korea, the number of non-regular workers in Korea has steadily increased (6,308,000 in 2015; 6,481,000 in 2016; 6,578,000 in 2017; and 6,614,000 in 2018).
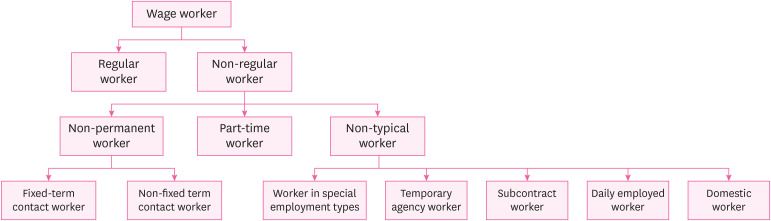
There is no internationally established standard definition for non-regular workers. However, in Korea, non-regular workers include all workers except regular workers who are employed by a single employer, work standard hours, and have no limit on the period of employment. Non-regular workers can primarily be divided into non-permanent workers, part-time workers and non-typical workers [3].
Non-permanent workers are those who have a limited working contract period or work only through repeated contract renewal. Part-time workers are workers whose work hours are at least 1 hour shorter than those of regular workers who perform the same type of work at the same workplace. This is usually the case when workers are scheduled to work for less than 36 hours per week. Non-typical workers are those workers whose employment contract relationship is different from that of a regular worker and include workers in special employment types, temporary agency workers, subcontract workers, domestic workers, and daily employed workers.
These non-regular workers are exposed to more risk than regular workers, which can influence their health negatively. A survey on the subcontracted industrial accidents conducted in 2016 by the Korea Occupational Safety and Health Institute found that the rate of death incidents due to work accidents was higher among subcontract workers than among original contractors [4]. Comparing the injuries caused by industrial accidents during 2017, only 21% of the regular workers experienced industrial accidents, while 38% of non-regular workers (nearly twice as many as regular workers) experienced industrial accidents. Job satisfaction among non-regular workers was also lower compared to regular workers [5]. In addition, non-regular workers showed significantly worse results in physical health such as mortality, obesity prevalence, chronic disease, and mental health, such as depression and insomnia, than regular workers [6,7,8].
Insomnia is defined as a complaint of sleep disturbances even though there is enough opportunity to sleep in an appropriate environment [9]. According to the age-based mental health disease statistics released by the Korea Health Insurance Review and Assessment Service in 2017, 123,898 patients received inpatient treatment for insomnia in 2017, an increase of 48.3% from 83,556 in 2013 [10,11]. Insomnia not only causes personal loss and suffering at the individual level but also affects society negatively.
At the individual level, insomnia can be accompanied by various diseases such as depression. Forty to fifty percent of patients with chronic insomnia have mental disorders, such as bipolar disorder, depressive disorder, and anxiety disorder [12,13,14]. Insomnia can lead to a decrease in cognitive/physical functioning, which reduces the quality of life [15,16]. It also increases the risk of physical diseases, such as cardiovascular diseases (e.g., hypertension) [17,18].
At the social level, a study showed that insomnia increases the risk of traffic accidents, absenteeism, and decreases productivity [19]. In other studies, workers who suffered from insomnia were 7 times more likely to have accidents in their workplaces and more than twice as likely to be involved in car accidents [20]. Research shows that frequent absenteeism and inefficiency of workers suffering from sleep problems reduce productivity, resulting in socioeconomic losses [21].
As mentioned above, previous studies have reported that the physical and mental health of non-regular workers is affected more negatively compared to regular workers [22,23]. These studies classified non-regular workers based on the following criteria: continuity of employment contract (non-permanent workers), working hours (part-time workers), and labor provision method (non-typical workers) [24]. In Europe, studies have classified non-regular workers based on the continuity of employment contract and working hours, and found a difference in job dissatisfaction and workplace stress in each work pattern [25]. However, because the definitions of non-regular workers in Europe and Korea are different, it is necessary to comprehensively examine non-regular workers in Korea. In addition, no studies have analyzed the effects and interactions of the continuity of employment contract, working hours, and labor provision method.
Therefore, this study investigated the relationship between non-regular work patterns and insomnia and analyzed the interactions of non-regular work patterns with the risk of insomnia. This study is intended to help improve the mental health of workers by identifying the work patterns that are most related to insomnia.
METHODS
Study participants
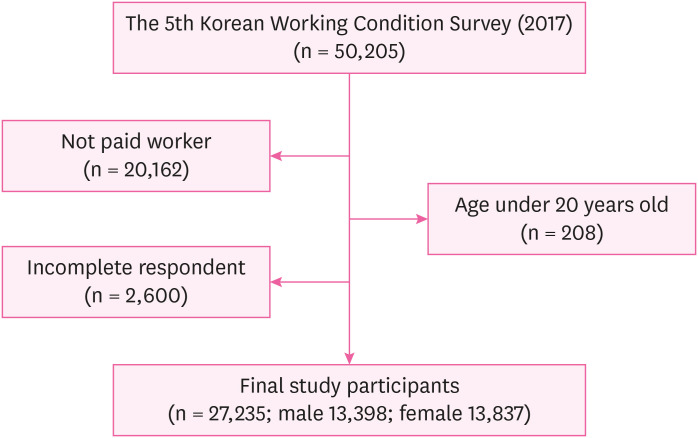
This study used data from the fifth Korean Working Conditions Survey (KWCS). The KWCS has been conducted since 2006, and 5 surveys have been conducted. The fifth KWCS was conducted by the Korea Occupational Safety and Health Research Institute in 2017. The survey identifies the degree of workers' exposure to risk factors by occupation, industry, and type of work, and uses the findings as a basis for establishing occupational safety and health policies. The survey participants were individuals aged 15 or older from all households residing in Korea. Approximately 50,000 households were sampled. The survey was developed based on the European Working Conditions Survey and the British Labor Force Survey. Professional interviewers visited the participants' households and interviewed them individually. In this study, only wage workers were analyzed, and 27,235 (13,398 men and 13,837 women) individuals were included in the final analysis, except for 2,600 respondents who had provided incomplete responses and 208 respondents aged below 20 years (Fig. 1).
Fig. 1. Flow diagram depicting study population.
Variables
Non-regular work patterns
Non-regular work patterns were classified based on the “Composition of Workers by Work Type” in the Statistics Korea's “2018 Supplementary Survey by Work Type of Economically Active Population Workers” (Fig. 2).
Fig. 2. Classification of Korean wage workers.
Non-regular workers were classified into 3 types, namely non-permanent, part-time, and non-typical workers, depending on the definition. Other wage workers were regarded as regular workers.
Non-permanent workers are non-regular workers classified on the basis of “continuity of employment contract” and are categorized into those who have a fixed period of work contract (fixed-term contract workers) or those who have not set a fixed period but continue to work because of repeated contract renewal and those who cannot expect to continue working for involuntary reasons (non-fixed term contract workers). Fixed-term contract workers were defined using the question, “Did you set an continuity of employment contract when you were hired?” Respondents responded to the above questions as “determined,” “not determined,” “unknown,” or “no.” In this study, the response of “determined” was defined as fixed-term contract workers. Non-fixed term contract workers were defined using the question: “If the running of the company becomes very difficult and the company is likely to go out of business or make adjustments to employment or if you do not make certain mistakes, can you continue to work for as long as you want?” Follow-up questions for the non-fixed term contract workers were “Why did you answer ‘Yes’ (can keep going)?” or “Why did you answer ‘No’ (can’t keep going)?” Respondents who answered “yes” to the above question and answered “Because the contract was repeatedly renewed” were classified as non-fixed term contract workers. In the question “Why did you answer ‘no’ (can't keep going)?”, respondents who answered “Because the previously set term of the employment contract expires,” “Because implicitly and customarily, the contract will be terminated,” “Because the employee was hired on the condition of quitting anytime if the employer asked,” “Because the current job (project) is finished,” “Because the person who previously worked at the current job returns,” “Because I can only work in certain seasons,” and “Because of business reasons at work,” were defined as non-fixed term contract workers.
Part-time workers are non-regular workers classified on the basis of “working hours,” and include workers who have working hours that are even 1 hour shorter than the 1-week working hours of regular workers. Part-time workers were defined using the question, “What is the type of employment in your main workplace?” Respondents answered the above questions with “full-time work,” “part-time work,” “unknown/no-response,” and “declined.” In this study, those who gave the response of “part-time work” were defined as part-time workers.
Non-typical workers are non-regular workers classified on the basis of the “labor provision method,” and include workers in special employment types, temporary agency workers, subcontract workers, domestic workers, and daily employed workers.
Workers in special employment types are workers who have no separate office, store, or workplace but work on a contractual basis for an employer. They directly meet their clients, provide goods or services to them, and receive payments (fee, service fee, allowance, etc.) according to their performance. They determine the methods of delivering their labor, working hours, etc., by themselves, such as insurance consultants, home-study teachers, quick service delivery agents, caddies, door-to-door sales persons, chauffeurs, and body scrubbers. Workers in special employment types were defined using the question “Was the job (work) you worked last week as a type of personally seeking or receiving customers, providing goods or services, and earning income for the amount of work (according to your performance) done by you? (e.g., insurance planner, workbook teacher, courier, quick-service delivery engineer, golf course assistant, truck driver, etc.)” Responses to the above question were “Yes,” “No,” “Don't know/No response,” and “Rejected.” In this study, a “yes” response to the above question was defined as a worker in a special employment type.
Temporary agency workers are workers dispatched to another company to perform their duties while employed by their own companies. Their wages or working status are managed by their employer, while their duties are supervised and directed by the company where they are dispatched. Temporary agency workers were defined using the question “Did you get wages from the workplace you worked for or from a dispatcher or service provider?” Individuals responding to the “dispatch company” were defined as dispatch workers.
Subcontract workers are workers who are employed by a subcontracting firm and work at other establishments' working sites, and receive direction and supervision on wages, employment status, work orders, and guidance from the subcontracting firm (e.g., cleaning services, security services, etc.). In this study, subcontract workers were defined using the question “Did you get wages from the workplace you worked for or from a dispatcher or service provider?” Individuals responding to the “contractor company” were defined as subcontract workers.
Domestic workers are workers who work in the home, not in the workplace provided by the business, such as telecommuting or the domestic handicraft industry. Domestic workers were defined using the question “Where did you usually work last week?" Respondents who answered “at home” were defined as domestic workers.
Daily employed workers are workers who work irregularly on a day-to-day basis and receive daily wages, such as construction workers, event assistants, housekeepers, and daily employed workers were defined using the question “Are your jobs working days or weeks only when jobs are available? (e.g., daytime construction worker, housekeeper, caregiver.)” In this study, the individual responding “yes” was defined as a daily employed worker.
In summary, non-permanent work means “continuity of employment contract”, part-time work means “working hours”, and non-typical work means “labor provision method”. Considering the overlap of non-regular workers as non-permanent, part-time, and non-typical workers, the “non-regular work patterns” were classified into 7 types (sole non-permanent, sole part-time, sole non-typical, non-permanent-part-time, non-permanent-non-typical, part-time-non-typical, and all-inclusive) (Fig. 3).
Fig. 3. Classification of non-regular workers.
Insomnia
Insomnia was assessed using the Minimal Insomnia Symptom Scale (MISS) [26]. MISS is a tool developed for screening insomnia for individuals aged 20–64 years. However, recently it has been reported that MISS is suitable as an insomnia screening tool even for those above 65 years. Therefore, this study targeted workers aged over 20 years [27,28]. “How often have you had the following problems with sleep in the last 12 months?” The MISS items consist of 3 sub-items: (A) Difficulty falling asleep; (B) Waking up repeatedly while sleeping; (C) Waking up feeling exhausted or extremely tired. In response to each question, respondents answered “every day,” “sometimes a week,” “sometimes a month,” “rarely,” “not at all,” “don't know,” or “decline.”
In this study, the scores of each sub-item, consisting of 0 (“not at all”) to 4 (“every day”) points, were summed according to the MISS scoring method. The calculated values between 0 and 12 were applied to the criteria suggested in the previous study, defining 6 or more points as insomnia and less than 6 points as a normal sleeping pattern. Cronbach's alpha was 0.73. In addition, the MISS showed sufficient specificity and sensitivity to screen patients with insomnia who met the International Classification of Diseases, Tenth Revision criteria. When comparing the sensitivity and specificity of MISS and other insomnia screening scales (Insomnia severity index [ISI]; Pittsburgh sleep quality index [PSQI]), the ISI has 94% sensitivity and 94% specificity [29], while PSQI has a sensitivity of 89.6% and specificity of 86.5% [30]. MISS showed similar percentages with 82% sensitivity and 86% specificity as a result of using 6 points as cut-offs in previous studies.
Other variables
In this study, variables known to be related to non-regular work and insomnia were included in the analysis, and the definitions of each variable are as follows.
In this study, sex, age, health status, education and income were included in the control variables as the study participants' general characteristics.
The ages were categorized as 15–19, 20–29, 30–39, 40–49, 50–59, and 60 above. The state of health was defined using the question “What is your state of health in general?” Respondents who answered “very good” or “good” were categorized as “good,” and those who answered “normal,” “bad,” or “very bad” were categorized as “not good.” Education levels were categorized into below elementary school graduation, middle school graduation, high school graduation, and junior college graduation. The income levels were classified into 0–1.00 million Korean won (KRW) group, 1.00–1.99 million KRW group, 2.00–2.99 million KRW group, and more than 3 million KRW group based on the average monthly income received from the company.
In addition, the occupational risk factors of insomnia presented in previous studies [31,32,33,34] were used as control variables. This included occupations, shifts, night work, working environment satisfaction, job stress, colleague support, and working hours. Each variable was defined as follows.
Occupations were categorized into 5 groups based on the response to the question “Which of the following classifications are best for your job?” [35] The first group was defined as the management/professional group, which included managers, experts, technicians, and paraprofessionals. The second group was defined as the white-collar group and the third group as the service/sales group. The fourth group was defined as the blue-collar group, which included skilled agricultural and forestry, fishery workers and equipment, machine operation, and assembly workers. The fifth group was defined as the simple labor group. Shift work refers to a case in which workers or groups of workers are swapped for the same work according to a time schedule in the same workplace. In this study, the case of answering “yes” to the question “Do you work shift work?” was set as shift work. Night work was defined based on the response to the question, “How many days do you work at night when working at least 2 hours from 10 pm to 5 am?” Respondents who answered “at least once a month” were defined as “night work.” Work environment satisfaction was defined using the question, “What do you generally think about the work environment in which you do your work?” Respondents who answered “not very satisfied” and “not satisfied at all” were defined as “not satisfied” with the working environment, while those who answered “satisfied” and “very satisfied” were defined as “satisfied.” In terms of job stress, the answers “not very” and “not at all” to the question “Do you feel stressed at work?” were classified as “None,” while the answer “always yes,” “mostly yes,” and “sometimes yes” were categorized as “Yes.” Regarding colleagues’ support, the responses “not very” and “not at all” to the question “Do your colleagues help and support you?” were classified as “None,” while the responses “always yes,” “mostly yes,” and “sometimes yes” were classified as “Yes.” Working hours were classified into “more than 52 hours/week” and “52 hours/week or less” based on weekly working hours.
Statistical analysis
In this study, a χ2 test was conducted to identify the general and occupational characteristics of participants with insomnia. The χ2 test was used to determine the distribution of work patterns according to insomnia, and logistic regression analysis was performed to determine the association between work patterns and insomnia. Odds ratios (ORs) were calculated for models without correction of control variables, models with correction of only general characteristics, and models with correction of all control variables including occupational characteristics.
The fifth KWCS provides a weight variable for their data to represent the working population across the country. The design weight of the fifth KWCS was calculated from the sample design and then adjusted by applying the weight of post-stratification and the weight based on the item non-response method. The weight variable was used for the statistical analysis.
Logistic regression analysis was performed by stratifying night and shift work to confirm the difference according to night and shift work. All the statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and the statistical significance level was set at p < 0.05.
Ethics statement
The Institutional Review Board (IRB) of Seoul National University Hospital waived the need for written informed consent to exempt the review of this study (IRB No. E-2004-037-1116).
RESULTS
General and Occupational characteristics
The general and occupational characteristics of the participants with insomnia are shown in Table 1.
Table 1. General and occupational characteristics of the participants according to insomnia and normal sleep.
| Variables | Total | Normal sleep | Insomnia | p | |
|---|---|---|---|---|---|
| Total | 27,235 (100) | 25,181 (100) | 2,054 (100) | ||
| Sex | < 0.0001 | ||||
| Male | 13,398 (49.2) | 12,486 (49.6) | 912 (44.4) | ||
| Female | 13,837 (50.8) | 12,695 (50.4) | 1,142 (55.6) | ||
| Age (years) | < 0.0001 | ||||
| 20–29 | 3,570 (13.1) | 3,295 (13.1) | 275 (13.4) | ||
| 30–39 | 6,510 (23.9) | 6,094 (24.2) | 416 (20.3) | ||
| 40–49 | 7,192 (26.4) | 6,676 (26.5) | 516 (25.0) | ||
| 50–59 | 6,190 (22.7) | 5,681 (22.6) | 509 (24.8) | ||
| ≥ 60 | 3,773 (13.9) | 3,435 (13.6) | 338 (16.5) | ||
| Health condition | < 0.0001 | ||||
| Not good | 7,557 (27.8) | 6,801 (27.0) | 756 (36.8) | ||
| Good | 19,678 (72.2) | 18,380 (73.0) | 1,298 (63.2) | ||
| Education | < 0.0001 | ||||
| Elementary school or below | 1,302 (4.8) | 1,172 (4.7) | 130 (6.3) | ||
| Middle school | 1,817 (6.7) | 1,665 (6.6) | 152 (7.4) | ||
| High school | 9,266 (34.0) | 8,476 (33.7) | 790 (38.5) | ||
| College or above | 14,850 (54.5) | 13,868 (55.0) | 982 (47.8) | ||
| Income (× 10,000 KRW/month) | < 0.0001 | ||||
| < 100 | 2,011 (7.3) | 1,860 (7.4) | 151 (7.4) | ||
| 100–199 | 7,532 (27.7) | 6,916 (27.5) | 616 (30.0) | ||
| 200–299 | 12,684 (46.6) | 11,839 (47.0) | 845 (41.1) | ||
| ≥ 300 | 5,008 (18.4) | 4,566 (18.1) | 442 (21.5) | ||
| Type of occupation | < 0.0001 | ||||
| Management/professional | 4,395 (16.1) | 4,112 (16.3) | 283 (13.8) | ||
| White collar | 6,659 (24.4) | 6,248 (24.8) | 411 (20.0) | ||
| Service/sale | 7,776 (28.6) | 7,088 (28.2) | 688 (33.5) | ||
| Blue collar | 4,357 (16.0) | 4,046 (16.1) | 311 (15.1) | ||
| Simple labor | 4,048 (14.9) | 3,687 (14.6) | 361 (17.6) | ||
| Shift work | < 0.0001 | ||||
| No | 23,857 (87.6) | 22,132 (87.9) | 1,725 (84.0) | ||
| Yes | 3,378 (12.4) | 3,049 (12.1) | 329 (16.0) | ||
| Night work | 0.0154 | ||||
| No | 24,686 (90.6) | 22,855 (90.8) | 1,831 (89.1) | ||
| Yes | 2,549 (9.4) | 2,326 (9.2) | 223 (10.9) | ||
| Working condition satisfaction | < 0.0001 | ||||
| Not satisfied | 6,182 (22.7) | 5,380 (21.4) | 802 (39.0) | ||
| Satisfied | 21,053 (77.3) | 19,801 (78.6) | 1,252 (61.0) | ||
| Job stress | < 0.0001 | ||||
| No | 5,075 (18.6) | 4,832 (19.2) | 243 (11.8) | ||
| Yes | 22,160 (81.4) | 20,349 (80.8) | 1,811 (88.2) | ||
| Colleague support | 0.1232 | ||||
| No | 1,457 (5.3) | 1,332 (5.3) | 125 (6.1) | ||
| Yes | 25,778 (94.7) | 23,849 (94.7) | 1,929 (93.9) | ||
| Working hour (hours per week) | 0.0195 | ||||
| ≤ 52 | 23,471 (86.2) | 21,736 (86.3) | 1,735 (84.5) | ||
| > 52 | 3,764 (13.8) | 3,445 (13.7) | 319 (15.5) | ||
Values are presented as number (%).
Of the 27,235 participants, 13,398 (49.2%) were male and 13,837 (50.8%) were female. According to the MISS, insomnia was found in 912 men and 1,142 women. There were significant differences in the general and occupational characteristics between normal sleep and experiencing insomnia. Insomnia was more likely related with being female, older and having negative health condition, and having lower education. In terms of job aspects, participants with insomnia were more likely to work in service/sale, simple labor, shift and night work and to experience more stress from the job and less job satisfaction.
Work patterns and insomnia
The distribution of each non-regular work pattern in relation to insomnia is shown in Table 2. Among the regular workers, 16,923 (94.0%) had normal sleep, while 1,075 (6.0%) had insomnia. For non-regular workers, 8,258 (88.1%) had normal sleep and 979 (11.9%) had insomnia. There is a higher incidence of insomnia among non-regular workers than among regular workers. Among the non-regular workers, sole non-permanent workers showed a higher incidence of insomnia than sole part-time workers and sole non-typical workers and the difference was statistically significant (p <0.001).
Table 2. Job classification of the participants according to sleeping pattern.
| Non-regular work patterns | Total | Normal sleep | Insomnia | p | ||||
|---|---|---|---|---|---|---|---|---|
| Regular | 17,998 (100.0) | 16,923 (94.0) | 1,075 (6.0) | < 0.0001 | ||||
| Non-regular | Non-per. | Part. | Non-typ. | 9,237 (100.0) | 8,258 (88.1) | 979 (11.9) | ||
| Type 1 | ∘ | - | - | 2,778 (100.0) | 2,443 (87.9) | 335 (12.1) | ||
| Type 2 | - | ∘ | - | 1,061 (100.0) | 995 (93.8) | 66 (6.2) | ||
| Type 3 | - | - | ∘ | 2,527 (100.0) | 2,315 (91.6) | 212 (8.4) | ||
| Type 4 | - | ∘ | ∘ | 663 (100.0) | 606 (91.4) | 57 (8.6) | ||
| Type 5 | ∘ | - | ∘ | 763 (100.0) | 656 (86.0) | 107 (14.0) | ||
| Type 6 | ∘ | ∘ | - | 1,043 (100.0) | 908 (87.1) | 135 (12.9) | ||
| Type 7 | ∘ | ∘ | ∘ | 402 (100.0) | 335 (83.3) | 67 (16.7) | ||
Values are presented as number (%).
Non-per.: non-permanent worker; Part.: part-time worker; Non-typ.: non-typical worker.
Association between non-regular work patterns and insomnia stratified by shift and night work
Table 3 shows the logistic regression model's estimates of the effect of non-regular work patterns on insomnia. In the crude model, non-regular workers had a high risk of insomnia. After controlling for covariates, non-regular workers had a statistically significant increased risk of insomnia. Non-regular workers were approximately 1.23–2.87 times more likely to have insomnia compared to regular workers. The risk of insomnia increased when the non-regular work patterns overlapped. Compared to regular workers, sole non-permanent and non-typical workers had greater risk of insomnia (OR: 1.72–1.23). The effect increased with non-regular work patterns overlapping, followed by part-time-non-typical, non-permanent-non-typical, and non-permanent-part-time. When all 3 overlapped, the risk of insomnia was the highest (OR: 2.87).
Table 3. Odds ratios for insomnia according to the non-regular work patterns.
| Non-regular work patterns | Crude | Model Ia | Model IIb | ||||
|---|---|---|---|---|---|---|---|
| Regular | 1.00 | 1.00 | 1.00 | ||||
| Non-regular | Non-per. | Part. | Non-typ. | ||||
| Type 1 | ∘ | - | - | 1.78 (1.50–2.11) | 1.74 (1.47–2.07) | 1.72 (1.45–2.05) | |
| Type 2 | - | ∘ | - | 0.96 (0.69–1.34) | 0.90 (0.64–1.27) | 1.04 (0.72–1.50) | |
| Type 3 | - | - | ∘ | 1.35 (1.11–1.64) | 1.30 (1.06–1.58) | 1.23 (1.00–1.53) | |
| Type 4 | - | ∘ | ∘ | 1.69 (1.18–2.43) | 1.58 (1.09–2.29) | 1.74 (1.17–2.58) | |
| Type 5 | ∘ | - | ∘ | 2.58 (1.97–3.39) | 2.48 (1.87–3.30) | 2.23 (1.64–3.04) | |
| Type 6 | ∘ | ∘ | - | 1.94 (1.44–2.60) | 1.90 (1.40–2.57) | 2.48 (1.78–3.46) | |
| Type 7 | ∘ | ∘ | ∘ | 2.43 (1.71–3.46) | 2.36 (1.63–3.40) | 2.87 (1.91–4.32) | |
Values are presented as odds ratio (95% confidence interval).
Non-per.: non-permanent worker; Part.: part-time worker; Non-typ.: non-typical worker.
aAdjusted for sex, age and health condition; bAdjusted for model I + education, income, occupational type, shift work, night work, job satisfaction, job stress, colleague support, working hour.
To investigate the association between non-regular work patterns and insomnia among participants with shift and night work, stratified analyses were applied, as shown in Table 4. After stratification by shift and night work, the effect of non-regular work patterns on insomnia remained. In addition, in the crude model, shift and night workers had a higher OR for insomnia compared to non-shift and non-night workers. Similarly, in models I and II, the OR was higher in shift and night workers than in non-shift and non-night workers.
Table 4. Odds ratios for insomnia stratified by shift work and night work according to the non-regular work patterns.
| Nonregular work patterns | Crude | Model Ia | Model IIb | |||||
|---|---|---|---|---|---|---|---|---|
| Shift work (−) | ||||||||
| Regular | 1.00 | 1.00 | 1.00 | |||||
| Non-regular | Non-per. | Part. | Non-typ. | |||||
| Type 1 | ∘ | - | - | 1.73 (1.44–2.09) | 1.68 (1.39–2.03) | 1.66 (1.37–2.02) | ||
| Type 2 | - | ∘ | - | 1.00 (0.67–1.50) | 0.94 (0.62–1.41) | 1.10 (0.71–1.69) | ||
| Type 3 | - | - | ∘ | 1.37 (1.11–1.68) | 1.30 (1.05–1.60) | 1.19 (0.95–1.50) | ||
| Type 4 | - | ∘ | ∘ | 1.75 (1.18–2.58) | 1.60 (1.07–2.38) | 1.71 (1.11–2.61) | ||
| Type 5 | ∘ | - | ∘ | 2.83 (2.06–3.89) | 2.65 (1.90–3.69) | 2.43 (1.71–3.46) | ||
| Type 6 | ∘ | ∘ | - | 1.77 (1.34–2.35) | 1.72 (1.27–2.33) | 2.23 (1.56–3.20) | ||
| Type 7 | ∘ | ∘ | ∘ | 2.28 (1.55–3.35) | 2.15 (1.44–3.21) | 2.56 (1.63–4.03) | ||
| Shift work (+) | ||||||||
| Regular | 1.00 | 1.00 | 1.00 | |||||
| Non-regular | Non-per. | Part. | Non-typ. | |||||
| Type 1 | ∘ | - | - | 1.96 (1.30–2.98) | 2.02 (1.31–3.10) | 1.87 (1.18–2.96) | ||
| Type 2 | - | ∘ | - | 0.71 (0.40–1.29) | 0.75 (0.40–1.41) | 1.14 (0.60–2.16) | ||
| Type 3 | - | - | ∘ | 1.30 (0.74–2.29) | 1.36 (0.76–2.43) | 1.55 (0.84–2.88) | ||
| Type 4 | - | ∘ | ∘ | 1.32 (0.48–3.61) | 1.40 (0.51–3.88) | 1.66 (0.55–5.01) | ||
| Type 5 | ∘ | - | ∘ | 1.64 (0.99–2.72) | 1.83 (1.08–3.08) | 1.90 (1.05–3.42) | ||
| Type 6 | ∘ | ∘ | - | 2.20 (1.01–4.79) | 2.37 (1.14–4.91) | 3.53 (1.78–7.00) | ||
| Type 7 | ∘ | ∘ | ∘ | 2.83 (1.21–6.65) | 3.16 (1.30–7.68) | 3.96 (1.59–9.83) | ||
| Night work (−) | ||||||||
| Regular | 1.00 | 1.00 | 1.00 | |||||
| Non-regular | Non-per. | Part. | Non-typ. | |||||
| Type 1 | ∘ | - | - | 1.80 (1.51–2.16) | 1.77 (1.48–2.12) | 1.74 (1.45–2.09) | ||
| Type 2 | - | ∘ | - | 0.88 (0.61–1.27) | 0.82 (0.56–1.19) | 0.95 (0.64–1.41) | ||
| Type 3 | - | - | ∘ | 1.37 (1.11–1.68) | 1.32 (1.07–1.63) | 1.22 (0.97–1.53) | ||
| Type 4 | - | ∘ | ∘ | 1.67 (1.12–2.47) | 1.57 (1.04–2.35) | 1.66 (1.08–2.56) | ||
| Type 5 | ∘ | - | ∘ | 2.82 (2.09–3.82) | 2.71 (1.98–3.70) | 2.50 (1.79–3.49) | ||
| Type 6 | ∘ | ∘ | - | 1.97 (1.45–2.68) | 1.95 (1.42–2.69) | 2.49 (1.75–3.55) | ||
| Type 7 | ∘ | ∘ | ∘ | 2.11 (1.45–3.08) | 2.08 (1.40–3.08) | 2.51 (1.61–3.90) | ||
| Night work (+) | ||||||||
| Regular | 1.00 | 1.00 | 1.00 | |||||
| Non-regular | Non-per. | Part. | Non-typ. | |||||
| Type 1 | ∘ | - | - | 1.60 (0.93–2.75) | 1.49 (0.84–2.62) | 1.62 (0.89–2.92) | ||
| Type 2 | - | ∘ | - | 1.62 (0.71–3.71) | 1.71 (0.73–4.00) | 2.64 (1.10–6.33) | ||
| Type 3 | - | - | ∘ | 1.26 (0.71–2.26) | 1.11 (0.61–2.02) | 1.20 (0.63–2.27) | ||
| Type 4 | - | ∘ | ∘ | 1.95 (0.80–4.76) | 1.86 (0.78–4.42) | 2.42 (0.98–5.94) | ||
| Type 5 | ∘ | - | ∘ | 1.62 (0.88–2.97) | 1.31 (0.67–2.57) | 1.28 (0.61–2.69) | ||
| Type 6 | ∘ | ∘ | - | 1.81 (0.60–5.46) | 2.02 (0.69–5.91) | 2.80 (0.88–8.88) | ||
| Type 7 | ∘ | ∘ | ∘ | 7.05 (2.64–18.82) | 6.28 (2.18–18.08) | 6.35 (2.02–19.94) | ||
Values are presented as odds ratio (95% confidence interval).
Non-per.: non-permanent worker; Part.: part-time worker; Non-typ.: non-typical worker.
aAdjusted for sex, age and health condition; bAdjusted for model I + education, income, occupational type, shift work, night work (not in the stratified model), job satisfaction, job stress, colleague support, working hour.
DISCUSSION
Through this study, the following results were obtained. First, non-regular work patterns were associated with insomnia. Second, among non-regular workers, there was a difference in the association between insomnia and non-regular work patterns. Third, when 2 or more non-regular work patterns existed together, they showed an additive effect, which had a higher association with insomnia. Fourth, non-regular work patterns had an influence on insomnia among workers when adjusted for shift and night work.
The mechanism by which work patterns affect insomnia symptoms has not yet been clearly identified. However, previous studies have explained the effect of work patterns on workers' health using 2 mechanisms. The first mechanism is an economic factor. Non-regular workers often have lower wages than regular workers and are more likely to have an unstable income due to uncertain contract terms [36]. In addition, it is difficult to guarantee social insurance benefits for non-regular workers compared to regular workers [37]; however, non-regular workers are more likely to work in environments that are prone to exposure to hazards than their regular counterparts [38,39]. The second mechanism is a socio-psychological factor, such as employment insecurity. Employment anxiety created by the instability of a contract period and an uncertain future can be stressful and may create other stressors. In previous studies, when employment was unstable, the burnout experience and the risk of depression symptoms were significantly higher [23,40,41].
Currently, in Korea, non-regular workers are defined as workers even if they are only non-permanent workers, part-time workers, or non-typical workers, and these can overlap with each other. In other words, even for the same part-time worker, there are part-time workers who are indefinitely contracted, and on the contrary, there are part-time workers who are fixed-term contract workers. Therefore, this study compared the effects of each on insomnia by classifying them, and found that the more the overlap, the higher the effect. With type 1, type 2, and type 3, we compared which of the provision of “continuity of employment contract,” “working hours,” and “labor provision method” had a greater impact on insomnia. In this study, non-permanent work showed the highest association with insomnia, followed by non-typical work. The association between part-time work and insomnia was not significant. The result showed that the continuity of employment contract had the highest effect on insomnia, while working hours did not have a significant effect. These results can be explained by those of the existing studies. In Japan, a study showed that non-permanent workers were much more likely to be bullied [42], and in the Finnish study, non-permanent work was a risk factor for depressive disorder and delayed return to work [43].
In addition, when statistically insignificant results of non-regular work patterns were excluded, the study showed that the risk of insomnia was higher when 2 or more non-regular work (non-permanent, part-time, non-typical) existed together than when only one of them existed. From these results, it can be inferred that there would be interactions between non-regular work patterns when they coexist. Among non-regular workers, workers with more than one non-regular worker pattern are at risk of having worse mental health.
Based on the results, the risk of insomnia increased as the non-regular work patterns overlapped. Insomnia may be highly related to the continuity of employment contract. The risk of insomnia varied depending on the non-regular work pattern, probably due to the different effects of continuity of employment contract, labor provision method, and working hours on workers' health. These results can be used to evaluate the work fitness of workers with insomnia or to manage the risk of insomnia among non-regular workers. It can be argued that non-permanent workers, part-time workers, and non-typical workers are non-regular workers; however each has different characteristics. Therefore, it is necessary to distinguish them when determining the health impact of non-regular workers.
Previous studies have found that shift and night work are related to insomnia [44]. In this study, shift and night work were also found to be associated with insomnia. It was analyzed through the stratification of shift and night work. The results of the analysis showed that the ORs of insomnia were higher in the group with shift and night work and lower in the group without shift and night work; however, it was significant in both cases. Considering that a relationship was found between non-regular work patterns and insomnia after stratification by shift and night work and that a higher OR was seen in the group with shift and night work, it could be inferred that non-regular work patterns may affect insomnia regardless of the effect of shift and night work.
This study has the following strengths. First, it is the first study to analyze the relationship between non-regular work patterns and insomnia and to compare the differences and interactions by subdividing the work patterns. Second, to define non-regular work patterns, the same criteria used in surveys conducted by the National Statistical Office and national agencies were used. The classification of work patterns using working hours, continuity of employment contracts, and labor provision method was the same as those used by the National Statistical Office and national agencies; therefore, it can be easily applied to future research or data analysis.
This study has several limitations. First, this study has limitations as a cross-sectional study that used the results obtained at a single time point. Although it was found that non-regular work patterns and insomnia were related, it was not possible to find causality. Longitudinal studies such as cohorts on work patterns may be helpful. Second, other factors related to insomnia were not considered. Factors such as a person's history of mental illness (e.g., major depressive disorder, anxiety disorder) or sleep apnea could influence current insomnia; however, this has not been identified. In addition, smoking, drinking, and obesity have been linked to insomnia in several studies [45]; however, there were no questions about smoking, drinking, and obesity in the fifth KWCS data used in this study. Therefore, it was impossible to include them as the control variables. More accurate results can be obtained if further investigations or questions are included in the future. Third, only workers who were working at the time of the survey were included in the fifth KWCS; therefore, it is possible that at the time of the survey, workers who already had severe insomnia or who took a break from work or quit completely for treatment were excluded. In addition, there is a difference in the definition of night work. In the fifth KWCS, night work was defined as “working more than 2 hours between 10 pm and 5 am;” however, according to Korea occupational safety and health agency, the definition of night work in Korea is “working more than 3 hours between 10 pm and 6 am.” This should be considered during interpretation.
CONCLUSIONS
This study found that, among Korean wage workers, non-regular workers were significantly associated with insomnia, especially non-permanent workers and workers with more than one non-regular worker pattern. Given the personal and social impact of insomnia, appropriate work patterns are needed to improve the health of non-regular workers while maintaining labor productivity and business efficiency. In addition, as there are various health promotion programs to prevent sleep disorders among shift workers, these programs will be needed for non-regular workers, especially non-permanent workers and workers with more than one non-regular worker pattern. Supervisors and managers should consider these findings when managing non-regular workers and workers with insomnia.
Acknowledgements
The authors appreciate the Occupational Safety and Health Research Institute (OSHRI) for offering raw data from the Korean Working Conditions Survey.
Abbreviations
- KWCS
Korean Working Conditions Survey
- ISI
Insomnia severity index
- MISS
Minimal Insomnia Symptom Scale
- Non-per.
non-permanent worker
- Non-typ.
non-typical worker
- OR
odds ratio
- Part.
part-time worker
- PSQI
Pittsburgh sleep quality index
Footnotes
Competing interests: The authors declare that they have no competing interests.
- Conceptualization: Kim HY, Lim HM.
- Data curation: Kim HY, Lim HM.
- Formal analysis: Kim HY, Lim HM, Choi J, Park C, Hong YC.
- Investigation: Kim HY, Lim HM, Choi J, Park C, Hong YC.
- Writing - original draft: Kim HY.
- Writing - review & editing: Hong YC.
References
- 1.Han JS. The conditions of non-regular workers and policy alternatives for social cohesion in Korea. J Peace Stud. 2015;16(3):151–174. [Google Scholar]
- 2.Yoo GJ, Kang CH. Effects of the 2007 Act on the protection of fixed-term and part-time employees on employment levels. Korean J Labor Econ. 2013;36(2):67–94. [Google Scholar]
- 3.Jang SC. A study on the definition of non-regular workers and its scale in Korea. Korean J Ind Relat. 2012;22(1):55–77. [Google Scholar]
- 4.Lee KY, Kim YS. Calculation of Integrated Statistics on Industrial Accidents of the Subcontractor. Ulsan: Korea Institute of Occupational Safety and Health; 2016. pp. 86–89. [Google Scholar]
- 5.National Human Rights Commission of Korea. Investigation of the Status of Indirect Employment Workers' Labor Human Rights. Seoul: National Human Rights Commission of Korea; 2018. [Google Scholar]
- 6.Kang YH, Kim HR. Socioeconomic mortality inequality in Korea: mortality follow-up of the 1998 National Health and Nutrition Examination Survey (NHANES) data. J Prev Med Public Health. 2006;39(2):115–122. [PubMed] [Google Scholar]
- 7.Yoo S, Cho HJ, Khang YH. General and abdominal obesity in South Korea, 1998-2007: gender and socioeconomic differences. Prev Med. 2010;51(6):460–465. doi: 10.1016/j.ypmed.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Kim IH, Muntaner C, Khang YH, Paek D, Cho SI. The relationship between nonstandard working and mental health in a representative sample of the South Korean population. Soc Sci Med. 2006;63(3):566–574. doi: 10.1016/j.socscimed.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C.: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Walsh JK, Coulouvrat C, Hajak G, Lakoma MD, Petukhova M, Roth T, et al. Nighttime insomnia symptoms and perceived health in the America Insomnia Survey (AIS) Sleep (Basel) 2011;34(8):997–1011. doi: 10.5665/SLEEP.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roth T, Coulouvrat C, Hajak G, Lakoma MD, Sampson NA, Shahly V, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69(6):592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 12.McCall WV. A psychiatric perspective on insomnia. J Clin Psychiatry. 2001;62(Suppl 10):27–32. [PubMed] [Google Scholar]
- 13.Morin CM, Bélanger L, LeBlanc M, Ivers H, Savard J, Espie CA, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169(5):447–453. doi: 10.1001/archinternmed.2008.610. [DOI] [PubMed] [Google Scholar]
- 14.LeBlanc M, Beaulieu-Bonneau S, Mérette C, Savard J, Ivers H, Morin CM. Psychological and health-related quality of life factors associated with insomnia in a population-based sample. J Psychosom Res. 2007;63(2):157–166. doi: 10.1016/j.jpsychores.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5) Suppl:S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 16.Zammit GK, Weiner J, Damato N, Sillup GP, McMillan CA. Quality of life in people with insomnia. Sleep. 1999;22(Suppl 2):S379–85. [PubMed] [Google Scholar]
- 17.Suka M, Yoshida K, Sugimori H. Persistent insomnia is a predictor of hypertension in Japanese male workers. J Occup Health. 2003;45(6):344–350. doi: 10.1539/joh.45.344. [DOI] [PubMed] [Google Scholar]
- 18.Bonnet MH, Arand DL. Heart rate variability in insomniacs and matched normal sleepers. Psychosom Med. 1998;60(5):610–615. doi: 10.1097/00006842-199809000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10(4):427–438. doi: 10.1016/j.sleep.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Leger D, Quera-Salva MA, Philip P. Health-related quality of life in patients with insomnia treated with zopiclone. Pharmacoeconomics. 1996;10(Suppl 1):39–44. doi: 10.2165/00019053-199600101-00007. [DOI] [PubMed] [Google Scholar]
- 21.Woo JM, Hyun SY, Lee SH, Kang SG, Lee JS, Kim L, et al. Productivity time lost by sleep disturbance among workers in Korea. J Korean Neuropsychiatr Assoc. 2011;50(1):62–68. [Google Scholar]
- 22.Virtanen M, Kivimäki M, Joensuu M, Virtanen P, Elovainio M, Vahtera J. Temporary employment and health: a review. Int J Epidemiol. 2005;34(3):610–622. doi: 10.1093/ije/dyi024. [DOI] [PubMed] [Google Scholar]
- 23.Lewchuk W, Clarke M, de Wolff A. Working without commitments: precarious employment and health. Work Employ Soc. 2008;22(3):387–406. [Google Scholar]
- 24.Park J, Lee N, Yoon S, Choi B, Kim SS. A systematic review of the relationship between non-standard employment and health in South Korea. Health Soc Welf Rev. 2016;36(3):119–157. [Google Scholar]
- 25.Benavides FG, Benach J, Diez-Roux AV, Roman C. How do types of employment relate to health indicators? Findings from the second European survey on working conditions. J Epidemiol Community Health. 2000;54(7):494–501. doi: 10.1136/jech.54.7.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Broman JE, Smedje H, Mallon L, Hetta J. The Minimal Insomnia Symptom Scale (MISS): a brief measure of sleeping difficulties. Ups J Med Sci. 2008;113(2):131–142. doi: 10.3109/2000-1967-221. [DOI] [PubMed] [Google Scholar]
- 27.Hellström A, Hagell P, Fagerström C, Willman A. Measurement properties of the Minimal Insomnia Symptom Scale (MISS) in an elderly population in Sweden. BMC Geriatr. 2010;10(1):84. doi: 10.1186/1471-2318-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Westergren A, Broman JE, Hellström A, Fagerström C, Willman A, Hagell P. Measurement properties of the minimal insomnia symptom scale as an insomnia screening tool for adults and the elderly. Sleep Med. 2015;16(3):379–384. doi: 10.1016/j.sleep.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 29.Smith MT, Wegener ST. Measures of sleep: the insomnia severity index, medical outcomes study (MOS) sleep scale, Pittsburgh sleep diary (PSD), and Pittsburgh sleep quality index (PSQI) Arthritis Care Res (Hoboken) 2003;49(S5):S184–96. [Google Scholar]
- 30.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 31.Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med Clin. 2013;8(3):281–297. doi: 10.1016/j.jsmc.2022.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13(4):346–353. doi: 10.1016/j.sleep.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Utsugi M, Saijo Y, Yoshioka E, Horikawa N, Sato T, Gong Y, et al. Relationships of occupational stress to insomnia and short sleep in Japanese workers. Sleep. 2005;28(6):728–735. doi: 10.1093/sleep/28.6.728. [DOI] [PubMed] [Google Scholar]
- 34.de Souza Lopes C, Robaina JR, Rotenberg L. Epidemiology of insomnia: prevalence and risk factors. In: Sahoo S, editor. Can't Sleep? Issues of Being an Insomniac. London: IntechOpen; 2012. pp. 1–21. [Google Scholar]
- 35.Statistics Korea. Korean Standard Classification of Diseases, 7th Revision. Daejeon: Statistics Korea; 2017. [Google Scholar]
- 36.International Labour Organization. Policies and Regulations to Combat Precarious Employment. Paris: International Labour Organization; 2011. [Google Scholar]
- 37.Shin KY, Kong J. Why does inequality in South Korea continue to rise? Korean J Sociol. 2014;48(6):31–48. [Google Scholar]
- 38.Quinlan M. The implications of labour market restructuring in industrialized societies for occupational health and safety. Econ Ind Democr. 1999;20(3):427–460. [Google Scholar]
- 39.Benach J, Muntaner C. Precarious employment and health: developing a research agenda. J Epidemiol Community Health. 2007;61(4):276–277. doi: 10.1136/jech.2005.045237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Benach J, Vives A, Amable M, Vanroelen C, Tarafa G, Muntaner C. Precarious employment: understanding an emerging social determinant of health. Annu Rev Public Health. 2014;35:229–253. doi: 10.1146/annurev-publhealth-032013-182500. [DOI] [PubMed] [Google Scholar]
- 41.Sverke M, Hellgren J, Näswall K. No security: a meta-analysis and review of job insecurity and its consequences. J Occup Health Psychol. 2002;7(3):242–264. [PubMed] [Google Scholar]
- 42.Karthik L, Kumar G, Keswani T, Bhattacharyya A, Chandar SS, Bhaskara Rao KV. Protease inhibitors from marine actinobacteria as a potential source for antimalarial compound. PLoS One. 2014;9(3):e90972. doi: 10.1371/journal.pone.0090972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ervasti J, Vahtera J, Virtanen P, Pentti J, Oksanen T, Ahola K, et al. Is temporary employment a risk factor for work disability due to depressive disorders and delayed return to work? The Finnish Public Sector Study. Scand J Work Environ Health. 2014;40(4):343–352. doi: 10.5271/sjweh.3424. [DOI] [PubMed] [Google Scholar]
- 44.Kim YG, Yoon DY, Kim JI, Chae CH, Hong YS, Yang CG, et al. Health effects of shift work. Korean J Occup Environ Med. 2002;14(3):247–256. [Google Scholar]
- 45.LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32(8):1027–1037. doi: 10.1093/sleep/32.8.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]