Abstract
The 2012 Berlin definition of acute respiratory distress syndrome (ARDS) provided validated support for three levels of initial arterial hypoxaemia that correlated with mortality in patients receiving ventilatory support. Since 2015, high-flow nasal oxygen (HFNO) has become widely used as an effective therapeutic support for acute respiratory failure, most recently in patients with severe COVID-19. We propose that the Berlin definition of ARDS be broadened to include patients treated with HFNO of at least 30 L/min who fulfil the other criteria for the Berlin definition of ARDS. An expanded definition would make the diagnosis of ARDS more widely applicable, allowing patients at an earlier stage of the syndrome to be recognised, independent of the need for endotracheal intubation or positive-pressure ventilation, with benefits for the testing of early interventions and the study of factors associated with the course of ARDS. We identify key questions that could be addressed in refining an expanded definition of ARDS, the implementation of which could lead to improvements in clinical practice and clinical outcomes for patients.
Introduction
Definitions of clinical syndromes are not immutable and should be updated as needed to match the needs of patients, clinicians, and investigators. The definition of acute respiratory distress syndrome (ARDS) has been revised several times since its original description in 1967.1, 2 In 1988, Murray and colleagues3 proposed an expanded definition of ARDS that specified a four-point lung injury score (ranging from 0 to 4) that included the degree of hypoxaemia, static respiratory compliance, the level of positive end-expiratory pressure (PEEP), and the extent of radiographic pulmonary infiltrates. In 1994, the American–European Consensus Conference provided a revised definition of ARDS that designated patients with a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen (PaO2/FiO2) of 300 mm Hg or less as having acute lung injury, and reserved the term ARDS for patients with more severe hypoxaemia (PaO2/FiO2 ≤200 mm Hg).4 In 2012, the Berlin definition of ARDS recommended that the term be expanded to include patients with an initial PaO2/FiO2 of 201–300 mm Hg who were receiving invasive or non-invasive ventilation with a tight-fitting mask and PEEP or continuous positive airway pressure (CPAP) of at least 5 cm H2O; this group was designated as having mild ARDS. PaO2/FiO2 of 101–200 mm Hg defined moderate ARDS and PaO2/FiO2 of 100 mm Hg or less was termed severe ARDS.5 This recommendation was validated in a patient-level meta-analysis of 4188 patients, in which mortality was 27%, 35%, and 45% in the mild, moderate, and severe PaO2/FiO2 groups,5 and has since been prospectively confirmed.6 The Berlin definition also specified the following criteria: first, that respiratory failure should have developed within 1 week of a known clinical insult; second, that respiratory failure should not be fully explained by cardiac failure, with the recommendation for additional testing such as echocardiography to exclude hydrostatic oedema, if needed; and third, that chest imaging should include bilateral opacities not fully explained by effusions, atelectasis, or nodules. In 2016, Riviello and colleagues7 proposed the Kigali modification of the Berlin definition, to respond to patient needs in resource-limited settings. This modification specified that bilateral opacities could be documented by either ultrasonography or chest radiograph, and that oxygenation criteria could be met with a pulse oximetric oxygen saturation (SpO2)/FiO2 ratio of less than or equal to 315 without the requirement for PEEP.
Key messages.
-
•
Definitions of ARDS have evolved since the first description of the syndrome in 1967: key advances include the 1988 proposal of an acute lung injury score, which provided a semi-quantitative scoring of lung injury that was useful for clinical research; and the 1994 American–European Consensus Conference definition of ARDS, which was used in several successful clinical trials, including those of lung-protective ventilation, prone positioning, and a fluid-conservative management strategy
-
•
The 2012 Berlin definition of ARDS simplified the terminology, clarified several criteria, and provided validated support for three strata of initial arterial hypoxaemia (PaO2/FiO2 categories of ≤100, 101–200, and 201–300 mm Hg), which correlated with mortality (45%, 35%, and 27%, respectively)
-
•
Since 2015, HFNO has become widely used as an effective therapeutic support for acute respiratory failure, most recently in patients with severe COVID-19
-
•
We propose that the Berlin definition of ARDS be broadened to include patients treated with HFNO of at least 30 L/min who fulfil the other criteria for the Berlin definition of ARDS
-
•
This broadened definition would make the diagnosis of ARDS more widely applicable, focusing on patients with sufficient clinical lung injury to require high levels of oxygen support, independent of the need for endotracheal intubation or positive-pressure ventilation
-
•
An expanded definition of ARDS, including HFNO, would be valuable in addressing the needs of patients in clinical practice and through clinical research, including clinical trials
ARDS=acute respiratory distress syndrome. HFNO=high-flow nasal oxygen. PaO2/FiO2=ratio of partial pressure of arterial oxygen to fraction of inspired oxygen.
Patients receiving HFNO
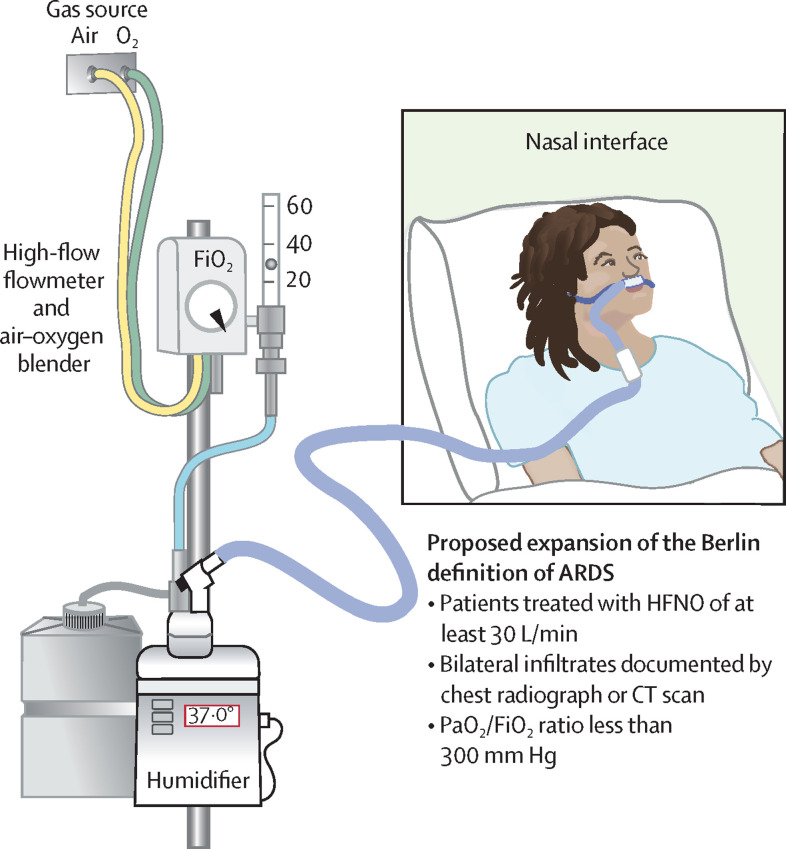
Now, in 2021, we propose a further modification to the clinical definition of ARDS to include patients treated with high-flow nasal oxygen (HFNO) who otherwise meet the Berlin criteria for ARDS. Since the landmark study by Frat and colleagues,8 HFNO has become widely used in critically ill patients to provide support for hypoxaemic respiratory failure that was not previously feasible with supplemental oxygen supplied by face mask or standard nasal cannula. HFNO provides heated and humidified oxygen that can be delivered at high flow rates, ranging from 10 to 60 L/min, thus increasing FiO2 to levels in the range of 80–90% (figure ). In addition, in most patients, HFNO provides a modest flow-dependent level of end-expiratory airway pressure (2–5 cm H2O) that inflates atelectatic distal airspaces similar to low levels of PEEP in mechanically ventilated patients.9, 10 HFNO also increases carbon dioxide excretion and diminishes work of breathing.8, 11, 12, 13, 14 During the COVID-19 pandemic, HFNO has been widely used to support patients with bilateral pulmonary infiltrates and hypoxaemia due to SARS-CoV-2 pneumonia,15, 16, 17 including those managed in resource-limited settings18 and patients with severe COVID-19-associated ARDS managed in the prone position,19 who typically meet all other Berlin diagnostic criteria for ARDS other than the requirement for invasive or non-invasive mechanical ventilation.
Figure.
Proposed expansion of the Berlin definition of ARDS
ARDS=acute respiratory distress syndrome. HFNO=high-flow nasal oxygen. PaO2/FiO2=ratio of partial pressure of arterial oxygen to fraction of inspired oxygen.
Several studies have reported that non-ventilated patients who otherwise meet the diagnostic criteria for ARDS have characteristics and outcomes similar to those of patients with ARDS. For example, Kangelaris and colleagues20 reported that non-ventilated patients who otherwise met the criteria for ARDS had the same 60-day mortality outcomes as ventilated patients with ARDS. Another study found that patients with hypoxaemia and bilateral infiltrates who were treated with HFNO had patterns of elevated plasma biomarkers of inflammation and injury similar to those of patients with ARDS who were mechanically ventilated.21 Additionally, Coudroy and colleagues22 reported that almost all patients with bilateral pulmonary infiltrates and a PaO2/FiO2 of 300 mm Hg or less under standard oxygen support fulfilled ARDS criteria by oxygenation and chest radiographic criteria without meeting the Berlin criteria for positive-pressure ventilation. These studies and others suggest that the severity of hypoxaemia is more important than the method used for oxygen delivery, supporting the concept that the diagnosis of ARDS should not depend on the presence of an endotracheal tube or positive-pressure ventilation in adults23, 24, 25, 26 or in children.27
An expanded definition of ARDS
We propose that the use of HFNO at a rate of at least 30 L/min be added as an additional criterion for the diagnosis of ARDS. There are other modifications that could be considered (panel ). Given the more indolent progression of hypoxaemia and respiratory failure in COVID-19 compared with other causes of ARDS,17 a revised definition of ARDS could also consider a latency longer than 7 days from identification of the ARDS risk factor, as specified by the Berlin definition, perhaps up to 14 days. Oxygenation and radiographic criteria for the diagnosis of ARDS would be the same as in the Berlin definition, although the addition of SpO2/FiO2 of less than or equal to 315 should be considered, as in the Kigali modification,7 given its increasing use both clinically and in research settings since it was originally validated.28 Would it be reasonable to consider a wider range of patients who have severe hypoxaemia on high FiO2 delivered with lower flow rates, as suggested decades ago, before the HFNO era?29 Should the radiographic criteria for bilateral opacities be reconsidered? One recent study indicated that mechanically ventilated patients from the LUNG SAFE study had the same mortality with opacities in two quadrants, independent of whether the infiltrates were bilateral or unilateral.30
Panel. Questions to address in considering an expanded definition of ARDS.
The proposal to include patients receiving HFNO in an expanded definition of ARDS could be evaluated in several forums. Areas of uncertainty and other potential modifications to the Berlin definition are listed below. These questions could be addressed in randomised controlled trials or observational studies that include patients recruited at an early stage of respiratory failure.
-
•
Is an HFNO cutoff of 30 L/min optimal?
-
•
Should the latency period for the inciting clinical disorder be increased to 14 days rather than 7 days, a point that is especially relevant to viral pneumonia and COVID-19?
-
•
Should the use of a SpO2/FiO2 ratio of less than or equal to 315 be formally integrated as an oxygenation criterion?
-
•
Should the radiographic criteria be modified to include two quadrants, independent of whether the infiltrates are bilateral or unilateral?
ARDS=acute respiratory distress syndrome. HFNO=high-flow nasal oxygen. SpO2/FiO2=ratio of pulse oximetric oxygen saturation to fraction of inspired oxygen.
What would be the advantages of adding HFNO of at least 30 L/min to the definition of ARDS? First, the addition would explicitly recognise that many HFNO-supported patients have acute respiratory failure and acute lung injury from a non-cardiogenic cause of pulmonary oedema, regardless of the presence of an endotracheal tube. Second, it would emphasise that these patients are excellent candidates for the testing of treatments for acute lung injury and ARDS in an earlier phase of respiratory failure, allowing treatment to begin before the patient is intubated and mechanically ventilated. This approach is being taken in the US I-SPY COVID trial (NCT04488081)31—a national, randomised, platform trial that is testing several pharmacological agents for COVID-19-associated ARDS in patients who meet the Berlin definition either with mechanical ventilation or with HFNO support—and with other trials that are being designed as part of ACTIV-3 (NCT04501978) in the US National Institutes of Health Operation Warp Speed.32, 33 Third, because HFNO provides end-expiratory support of 2–5 cm H2O, our proposal would be concordant, to an extent, with the current criterion in the Berlin definition that requires at least 5 cm H2O PEEP or CPAP. Fourth, from an epidemiological perspective, the inclusion of these patients would more comprehensively identify those with ARDS at an earlier stage of the syndrome, and would include more patients in resource-limited settings, as was recommended with the Kigali modification of the Berlin definition of ARDS.7 Fifth, the addition of HFNO would make the definition of ARDS more widely applicable by focusing on all patients who have sufficient clinical lung injury to require high levels of oxygen support. Sixth, although the optimum use of HFNO and the optimum timing of intubation for ARDS remain unclear, randomised trials with a broader definition of ARDS would help to determine whether the use of HFNO reduces the use of invasive mechanical ventilation.15 Finally, other investigators have already concluded that ARDS is present in many patients being treated with HFNO, suggesting that this modification is already overdue.21, 24, 25
Challenges and opportunities
Are there disadvantages to expanding the Berlin definition of ARDS to include HFNO? Conceivably, some patients might be included who would not meet the criterion of a PaO2/FiO2 ratio of less than 300 mm Hg, since FiO2 can only be estimated with HFNO. However, this would be unlikely if a simple bedside estimate of FiO2 were included along with a measure of either PaO2, as was done in the trial of Frat and colleagues,8 or SpO2.28
Expanding the definition to include HFNO should not obscure the need to rule out left heart failure or a primary pulmonary process such as an autoimmune disease or acute eosinophilic pneumonia.34 The need to make these diagnostic distinctions would be the same whether the patient was being mechanically ventilated or being treated with HFNO. Also, some patients treated with HFNO might have declined intubation and mechanical ventilation or have a do-not-resuscitate restriction. However, such patients might have ARDS and their personal preference for limits on further respiratory support, such as intubation, should not impede an appropriate diagnosis.
Steps need to be taken to evaluate our proposal, to review it critically, and potentially to implement it in clinical research and clinical practice. We recognise the need for empirical validation of the optimum cutoff for HFNO flow rates. We have proposed 30 L/min partly because most of the beneficial effects of HFNO—including favourable effects on oxygenation, lung mechanics, end-expiratory lung volume, and respiratory drive—are achieved with flow of at least 30 L/min.12, 14 This and other uncertainties could be considered in several forums—including regional, national, or international conferences, or journals devoted at least in part to critical care medicine—and possibly at a consensus conference to address the scope and the specifics of an expanded definition of ARDS.
In conclusion, we recommend that the Berlin definition of ARDS be modified to include patients treated with HFNO of at least 30 L/min and propose that this would be an advance for patients with lung injury who require high levels of oxygen support, and for the clinicians and investigators caring for them. We welcome responses from the global community of investigators and clinicians caring for critically ill patients.
Declaration of interests
MAM receives fees as a consultant for Novartis and Citius Pharmaceuticals, outside of the present work. BTT receives fees as a consultant for Bayer, Novartis, and Thetis, outside of the present work. LBW receives fees as a consultant for Boehringer and Citius, outside of the present work.
Contributors
MAM wrote the original draft. BTT and LBW edited subsequent versions and contributed to the figure, panels, and selection of references.
References
- 1.Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;2:319–323. [Google Scholar]
- 2.Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. N Engl J Med. 2017;377:1904–1905. doi: 10.1056/NEJMc1711824. [DOI] [PubMed] [Google Scholar]
- 3.Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988;138:720–723. doi: 10.1164/ajrccm/138.3.720. [DOI] [PubMed] [Google Scholar]
- 4.Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 5.Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 6.Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 7.Riviello ED, Kiviri W, Twagirumugabe T, et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali modification of the Berlin definition. Am J Respir Crit Care Med. 2016;193:52–59. doi: 10.1164/rccm.201503-0584OC. [DOI] [PubMed] [Google Scholar]
- 8.Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 9.Ward JJ. High-flow oxygen administration by nasal cannula for adult and perinatal patients. Respir Care. 2013;58:98–122. doi: 10.4187/respcare.01941. [DOI] [PubMed] [Google Scholar]
- 10.Parke RL, Eccleston ML, McGuinness SP. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care. 2011;56:1151–1155. doi: 10.4187/respcare.01106. [DOI] [PubMed] [Google Scholar]
- 11.Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015;70:323–329. doi: 10.1111/anae.12923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–1215. doi: 10.1164/rccm.201605-0916OC. [DOI] [PubMed] [Google Scholar]
- 13.Goligher EC, Slutsky AS. Not just oxygen? Mechanisms of benefit from high-flow nasal cannula in hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1128–1131. doi: 10.1164/rccm.201701-0006ED. [DOI] [PubMed] [Google Scholar]
- 14.Mauri T, Alban L, Turrini C, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43:1453–1463. doi: 10.1007/s00134-017-4890-1. [DOI] [PubMed] [Google Scholar]
- 15.Demoule A, Vieillard Baron A, Darmon M, et al. High-flow nasal cannula in critically iII patients with severe COVID-19. Am J Respir Crit Care Med. 2020;202:1039–1042. doi: 10.1164/rccm.202005-2007LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McDonough G, Khaing P, Treacy T, McGrath C, Yoo EJ. The use of high-flow nasal oxygen in the ICU as a first-line therapy for acute hypoxemic respiratory failure secondary to coronavirus disease 2019. Crit Care Explor. 2020;2 doi: 10.1097/CCE.0000000000000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med. 2020;383:2451–2460. doi: 10.1056/NEJMcp2009575. [DOI] [PubMed] [Google Scholar]
- 18.Calligaro GL, Lalla U, Audley G, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: a multi-centre prospective observational study. EClinicalMedicine. 2020;28 doi: 10.1016/j.eclinm.2020.100570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raoof S, Nava S, Carpati C, Hill NS. High-flow, noninvasive ventilation and awake (nonintubation) proning in patients with coronavirus disease 2019 with respiratory failure. Chest. 2020;158:1992–2002. doi: 10.1016/j.chest.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kangelaris KN, Ware LB, Wang CY, et al. Timing of intubation and clinical outcomes in adults with acute respiratory distress syndrome. Crit Care Med. 2016;44:120–129. doi: 10.1097/CCM.0000000000001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.García-de-Acilu M, Marin-Corral J, Vázquez A, et al. Hypoxemic patients with bilateral infiltrates treated with high-flow nasal cannula present a similar pattern of biomarkers of inflammation and injury to acute respiratory distress syndrome patients. Crit Care Med. 2017;45:1845–1853. doi: 10.1097/CCM.0000000000002647. [DOI] [PubMed] [Google Scholar]
- 22.Coudroy R, Frat JP, Boissier F, Contou D, Robert R, Thille AW. Early identification of acute respiratory distress syndrome in the absence of positive pressure ventilation: implications for revision of the Berlin criteria for acute respiratory distress syndrome. Crit Care Med. 2018;46:540–546. doi: 10.1097/CCM.0000000000002929. [DOI] [PubMed] [Google Scholar]
- 23.Levitt JE, Bedi H, Calfee CS, Gould MK, Matthay MA. Identification of early acute lung injury at initial evaluation in an acute care setting prior to the onset of respiratory failure. Chest. 2009;135:936–943. doi: 10.1378/chest.08-2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chertoff J. High-flow oxygen, positive end-expiratory pressure, and the Berlin definition of acute respiratory distress syndrome: are they mutually exclusive? Am J Respir Crit Care Med. 2017;196:396–397. doi: 10.1164/rccm.201701-0005LE. [DOI] [PubMed] [Google Scholar]
- 25.Messika J, Ben Ahmed K, Gaudry S, et al. Use of high-flow nasal cannula oxygen therapy in subjects with ARDS: a 1-year observational study. Respir Care. 2015;60:162–169. doi: 10.4187/respcare.03423. [DOI] [PubMed] [Google Scholar]
- 26.Azoulay E, Lemiale V, Mokart D, et al. Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the HIGH randomized clinical trial. JAMA. 2018;320:2099–2107. doi: 10.1001/jama.2018.14282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flori HR, Glidden DV, Rutherford GW, Matthay MA. Pediatric acute lung injury: prospective evaluation of risk factors associated with mortality. Am J Respir Crit Care Med. 2005;171:995–1001. doi: 10.1164/rccm.200404-544OC. [DOI] [PubMed] [Google Scholar]
- 28.Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB. Comparison of the SpO2/FiO2 ratio and the PaO2/FiO2 ratio in patients with acute lung injury or ARDS. Chest. 2007;132:410–417. doi: 10.1378/chest.07-0617. [DOI] [PubMed] [Google Scholar]
- 29.Luhr OR, Antonsen K, Karlsson M, et al. Incidence and mortality after acute respiratory failure and acute respiratory distress syndrome in Sweden, Denmark, and Iceland. Am J Respir Crit Care Med. 1999;159:1849–1861. doi: 10.1164/ajrccm.159.6.9808136. [DOI] [PubMed] [Google Scholar]
- 30.Pham T, Pesenti A, Bellani G, et al. Outcome of acute hypoxaemic respiratory failure. Insights from the Lung Safe study. Eur Respir J. 2020 doi: 10.1183/13993003.03317-2020. [DOI] [PubMed] [Google Scholar]
- 31.Quantum Leap Healthcare Collaborative I-SPY COVID. 2019. https://www.quantumleaphealth.org/portfolio/i-spy-covid
- 32.Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2021;384:795–807. doi: 10.1056/NEJMoa2031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murray DD, Babiker AG, Baker JV, et al. Design and implementation of an international, multi-arm, multi-stage platform master protocol for trials of novel SARS-CoV-2 antiviral agents: Therapeutics for Inpatients with COVID-19 (TICO/ACTIV-3) medRxiv. 2021 doi: 10.1101/2020.11.08.20227876. published online April 8. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matthay MA, Zemans RL, Zimmerman GA, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019;5:18. doi: 10.1038/s41572-019-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]