Abstract
Study objective
We describe how the coronavirus disease 2019 (COVID-19) pandemic affected the economics of emergency department care (ED).
Methods
We conducted an observational study of 136 EDs from January 2019 to September 2020, using 2020-to-2019 3-week moving ratios for ED visits, complexity, revenue, and staffing expenses. We tabulated 2020-to-2019 staffing ratios and calculated hour and full-time-equivalent changes.
Results
Following the COVID-19 pandemic’s onset, geriatric (age ≥65), adult (age 18 to 64), and pediatric (age <18) ED visits declined by 43%, 40%, and 73%, respectively, compared to 2019 visits and rose thereafter but remained below 2019 levels through September. Relative value units per visit rose by 8%, 9%, and 18%, respectively, compared to 2019, while ED admission rates rose by 32%. Both fell subsequently but remained above 2019 levels through September. Revenues dropped sharply early in the pandemic and rose gradually but remained below 2019 levels. In medium and large EDs, staffing and expenses were lowered with a lag, largely compensating for lower revenue at these sites, and barely at freestanding EDs. Staffing and expense reductions could not match revenue losses in smaller EDs. During the pandemic, emergency physician and advanced practice provider clinical hours and compensation fell 15% and 27%, respectively, corresponding to 174 lost physician and 193 lost advanced practice provider full-time-equivalent positions.
Conclusion
The COVID-19 pandemic adversely impacted the economics of ED care, with large drops in overall and, in particular, low-acuity ED visits, necessitating reductions in clinical hours. Staffing cutbacks could not match reduced revenue at small EDs with minimum emergency physician coverage requirements.
Editor’s Capsule Summary.
What is already known on this topic
Emergency department (ED) census throughout the US dramatically declined as a result of the COVID-19 pandemic and has remained below typical levels.
What question this study addressed
This retrospective observational study assesses the change in ED visit numbers and case complexity during the COVID-19 pandemic, and the resultant economic impact.
What this study adds to our knowledge
The COVID-19 pandemic adversely impacted the economics of US EDs, resulting in decreases in provider staffing hours and consequent decreased compensation for ED clinicians.
How this is relevant to clinical practice
Findings demonstrate the vulnerability of a fee-for-service system serving as the ultimate public safety net, and suggest the need to consider alternative payment models for EDs.
Introduction
Background
In early 2020, the coronavirus disease 2019 (COVID-19) pandemic spread throughout the world. In the United States and other countries, there were reports of substantial numbers of people delaying or avoiding necessary emergency care early in the pandemic.1 Avoidance of emergency care was driven by many factors, including stay-at-home orders, concerns the health care system would be overwhelmed by COVID-19 cases, and personal concerns about risks of viral transmission in emergency departments (EDs).2 Starting in mid-March, there was a precipitous decline in US ED visits. Visit rates reached a low point in the second week of April, at 58% of 2019 volumes.3 , 4 ED visits declined for both low-acuity and high-acuity conditions, including acute myocardial infarction, stroke, heart failure, and substance use disorders.5 , 6 Since that time, ED visit rates have partially recovered, but they remain substantially below 2019 levels. Potential contributors to fewer ED visits include less communicable disease and injury due to public health measures, including social distancing, mask wearing, and school/business closures. In addition, some care may have shifted to other venues, specifically telemedicine.7 , 8
Importance
Medical care delivered by emergency physicians and advanced practice providers in EDs is primarily reimbursed by payers on a fee-for-service basis for each visit based on the complexity of care, commonly measured as relative value units (RVUs).9 Hospitals and ED practice organizations use different models to pay clinicians for clinical work, including fixed hourly rates, payments for generating RVUs, or a combination of hourly pay plus RVU incentives. As a result, the economics of ED practice organizations depend directly on patient volumes and, to a lesser degree, on care complexity.10 Practice organizations staff EDs to meet volume and complexity demands, including adjusting staffing with workload changes. When volumes fall, as occurred with the COVID-19 pandemic, the economic viability of EDs and emergency clinician practice organizations, as well as the salaries and jobs of ED clinicians, become threatened. Understanding the economic changes in emergency care during the COVID-19 pandemic may help inform potential shifts to new alternative payment models in emergency medicine.11 To our knowledge, no studies have quantified the economic impact of the COVID-19 pandemic on EDs or ED clinicians and discussed the implications for the economic viability of the delivery of US emergency care.
Goals of This Investigation
We describe how visit numbers and case complexity changed during the COVID-19 pandemic and how this impacted the economics of EDs, ED clinicians, and their practice organizations.
Methods
Study Design and Settings
We conducted an observational study of visit rates from January to September 2020, compared to the same period during 2019, in 136 continuously staffed EDs that contracted with a national ED practice organization for emergency physician and advanced practice provider services. The study relied on patient data that were extracted directly into a data warehouse from electronic health records at each contracted site. Data on staffing, reimbursement, and expenses were collected from shift reports (ShiftAdmin, Columbia, SC) and internal billing data. Missing data were rare (less than 1% of visits). Our study team has published several studies using this database (<1%).5 , 6 , 10 , 12 , 13
Facilities included small- (<30,000 visits per year, n=40), medium- (30,000 to 59,999 visits per year, n=56) and large-hospital based EDs (≥60,000 visits per year, n=16) and freestanding EDs (n=24). Freestanding ED volumes were comparable to those of small-hospital based EDs, but we examined freestanding EDs separately given their different organizational structure. The included facilities were geographically diverse, located in 18 states (ED counts by state can be found in Table E1, available at http://www.annemergmed.com). Of the 112 hospital-based EDs, 104 (93%) were nonacademic community hospitals. This study was determined to not be human subjects research by the Institutional Review Board at Allegheny Health Network.
Outcomes and Study Data
Outcomes included visit numbers, visit complexity (RVUs per visit), hospital admission rates (inpatient admissions plus observation stays), clinical revenue, direct salary expenses for clinicians, clinician hours worked, and clinician full-time equivalents. RVUs were chosen as a measure of visit complexity because they are attributed to visits and clinicians through standardized coding across all sites.10 Full-time-equivalents were calculated based on 108 hours worked per clinician per month, which is the minimum required to obtain benefits in this ED practice organization. We used data from the practice organization’s data warehouse for EDs that remained open and staffed continuously in both 2019 and 2020 (balanced panel) but noted that 5 additional freestanding EDs were closed during some or all of this period due to reduced visit volumes.
Variables collected included weekly total visits and admissions by patient age categories (≥65, 18 to 64, and <18 years) and payer sources (commercial, Medicare, Medicaid, and self-pay), ED clinician revenue from patient care (sum of payer reimbursement and patient responsibility [eg, deductibles, copayments, and coinsurance]), direct clinical expenses (salary payments to clinicians for clinical responsibilities), and clinician hours worked. Revenue data for the study referred to expected revenue once all payments are received. This is because actual revenue had not been fully collected for the 2020 study period given typical delays in collections at the time the data analysis was conducted, especially for direct billing to patients. Expected revenue was estimated using the practice organization’s revenue cycle management functions. Historically, these estimates have tracked accurately against ultimate actual revenue.
Methods of Measurement and Data Analysis
Outcomes and study data were aggregated to the facility-week level for January through September of 2019 and 2020 (39 weeks in each year). All reported weeks began on Sunday and ended on Saturday. Data on direct clinical expenses were collected at the facility-month level. We created 3-week moving averages for each variable (ie, we reported for week t the average of weeks t-2, t-1, and t) for each ED. We then computed a 2020:2019 ratio by dividing the 2020 moving average by the moving average for the corresponding weeks in 2019. We dropped the partial weeks of January 1 to January 4, 2020 and January 1 to January 5, 2019. Thus, week 4 was the first week for which a full 3-week rolling average was available for ratio calculations. We winsorized ratios at the 1st and 99th percentiles to reduce the influence of outliers. We then plotted means and 95% confidence intervals for the ratios, stratified by patient age, insurance status, and ED size. We separated children (age <18 years) from nonelderly adults (age 18 to 64 years) because prior work has demonstrated large differences in the impact of COVID-19 and other pandemics on pediatric versus adult ED visit rates.14 , 15 We studied older adults (age ≥65 years) separately because they have greater COVID-19 mortality and complications and have heeded stay-at-home orders more stringently than younger people.16 , 17
We examined means and ratios during several time periods related to the COVID-19 pandemic. The prepandemic time period consisted of weeks 2 to 11 (January 5, 2020 to March 14, 2020). With the exception of the last 2 days of week 11, this time period fell prior to the national emergency declaration on March 13. We considered the next 6 weeks of the pandemic (March 15 to April 25) as the “early” COVID-19 period, when many states imposed stay-at-home orders, closing schools and nonessential businesses. Note that the week 12 moving average (ending March 21) and week 13 moving average (ending March 28) included both prepandemic and during-pandemic data. The third period (weeks 18 to 39) aligned with general reopening and increased social mobility and gradual recovery in ED visit volumes. We chose the length of the middle period based on visual observation of the visit trends shown in Figure 1 . We used Stata 16 (College Station, TX) for analysis.
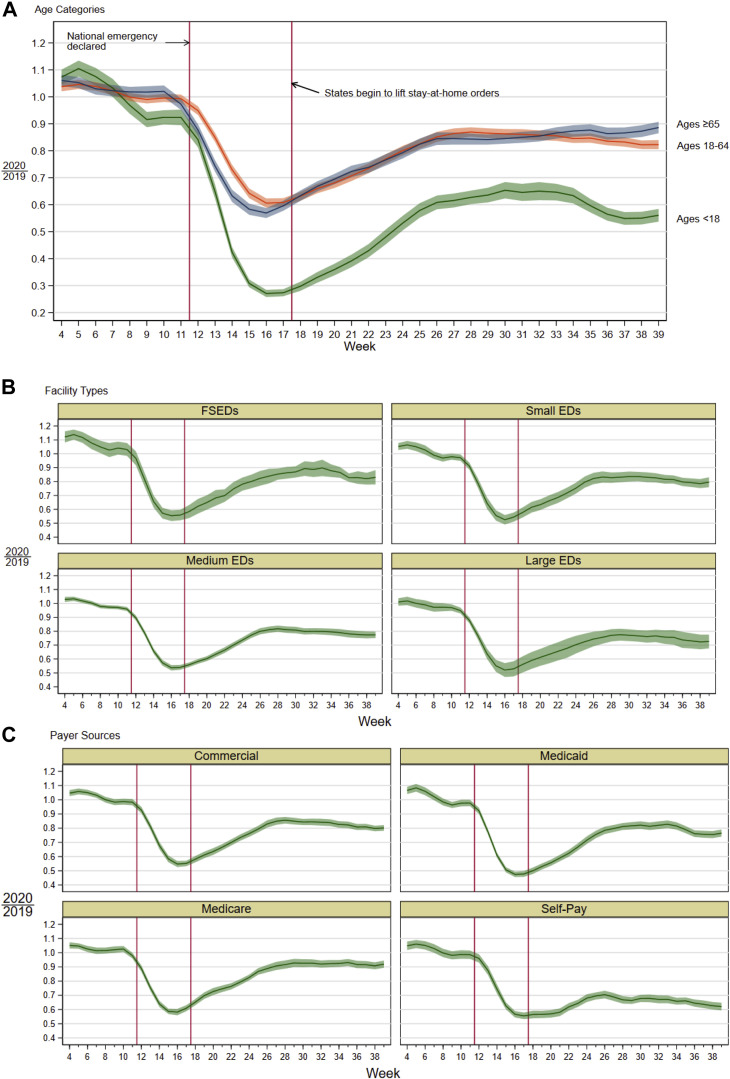
Figure 1.
2020:2019 ratios of number of visits to 136 EDs. Figure 1 shows 2020:2019 ratios for 24 freestanding EDs, 40 small EDs (<30,000 visits/year), 56 medium EDs (30,000 to 59,999 visits/year), and 16 large EDs (>60,000 visits/year). Vertical lines divide the prepandemic, early pandemic, and later pandemic periods. Shaded areas around lines are 95% confidence intervals.
Results
Study Sample
Weekly visit and financial data from 136 EDs in 18 states (24 freestanding EDs and 112 hospital-based EDs) were collected during the study period. Of approximately 6 million ED visits, 16% were from patients aged <18 years, 62% from patients 18 to 64 years, and 22% from patients >65 years. Approximately 28% of the visits were from commercial payers, 29% from Medicaid, 29% from Medicare, and 15% from self-pay. The average RVUs per visit were 3.9 (standard deviation [SD] 0.4), and the average hospital admission rate (excluding freestanding EDs) was 20.1% (SD 9.4%).
Pandemic Impact on ED Visit Volumes and Complexity
In Figure 1, we present trends in overall ED visit volumes by patient age, ED size, and payer type. Starting in mid-March (week 11), the 2020:2019 visit ratio declined sharply for all 3 groups, nadiring at approximately 0.6 for the 2 adult groups and 0.3 for children by mid-April (week 16) (Figure 1A). The adult ED visit ratio then gradually increased to between 0.8 and 0.9 for adults and roughly leveled off. Starting in August, visit ratios for adults ages 18 to 64 declined slightly, while visit ratios for adults 65 and older increased. The pediatric visit ratio also rose to between 0.6 and 0.7 by mid-July, flattened, and then fell again in the later part of our sample period. Overall, 2020:2019 visit ratios followed similar trends for EDs of different sizes (Figure 1B). By mid-April (week 16), visit ratios in all 4 size groups fell to between 0.5 and 0.6 before rebounding by late June, to about 0.8 at freestanding EDs and small and medium EDs and 0.7 at large EDs. Visit ratios then plateaued and declined somewhat through the end of September. Visit ratios for commercial, Medicaid, and Medicare patients followed a similar trend, falling to between 0.5 to 0.6 during the early pandemic and then rebounding to approximately 0.8 in the June to July period (Figure 1C). Self-pay patients fell by similar amounts early but had a more limited rebound, to approximately 0.6. Mean weekly visit counts and ratios by facility size and age category for the prepandemic (through mid-March), early pandemic (mid-March through end of April), and later pandemic periods can be found in Table E2 (available at http://www.annemergmed.com).
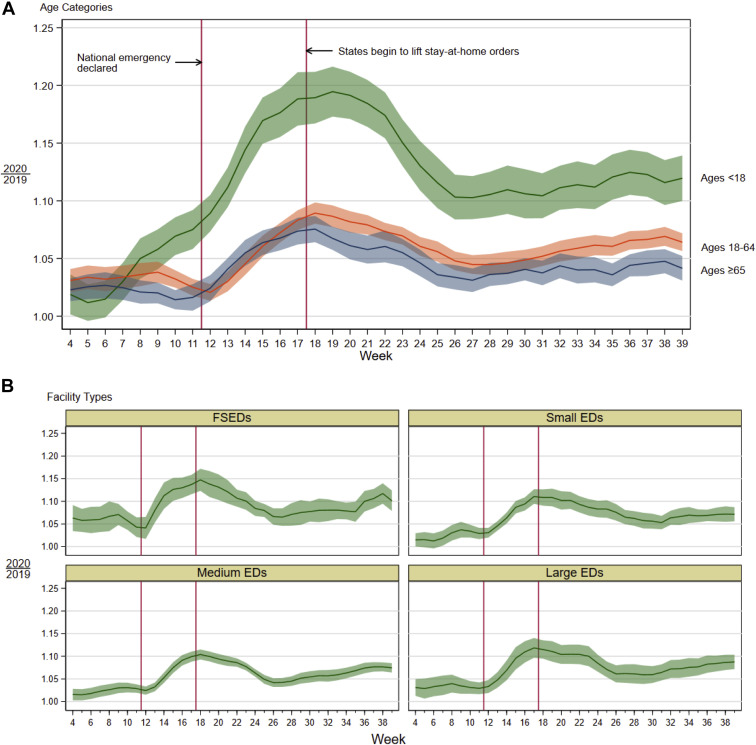
Figure 2 shows the impact of the COVID-19 pandemic on visit complexity (RVUs per visit) for the patients who presented to the ED. As visit rates fell in the early pandemic period, the 2020:2019 ratio of RVUs per visit increased for both adults and children (Figure 2A), reaching approximately 1.2 for children and just less than 1.1 for adults by the end of April. Both ratios declined (to approximately 1.1 for children and to 1.04 for adults) by the end of June and then began to slowly rise again. Trends in complexity, for adults and children combined, were similar across the 4 ED groups (Figure 2B).
Figure 2.
2020:2019 ratios of RVUs per visit in 136 EDs. Figure 2 shows 2020:2019 ratios for 24 freestanding EDs, 40 small EDs (<30,000 visits/year), 56 medium EDs (30,000 to 59,999 visits/year), and 16 large EDs (>60,000 visits/year). Red vertical lines divide the prepandemic, early pandemic, and later pandemic time periods. Shaded area around lines are 95% confidence intervals.
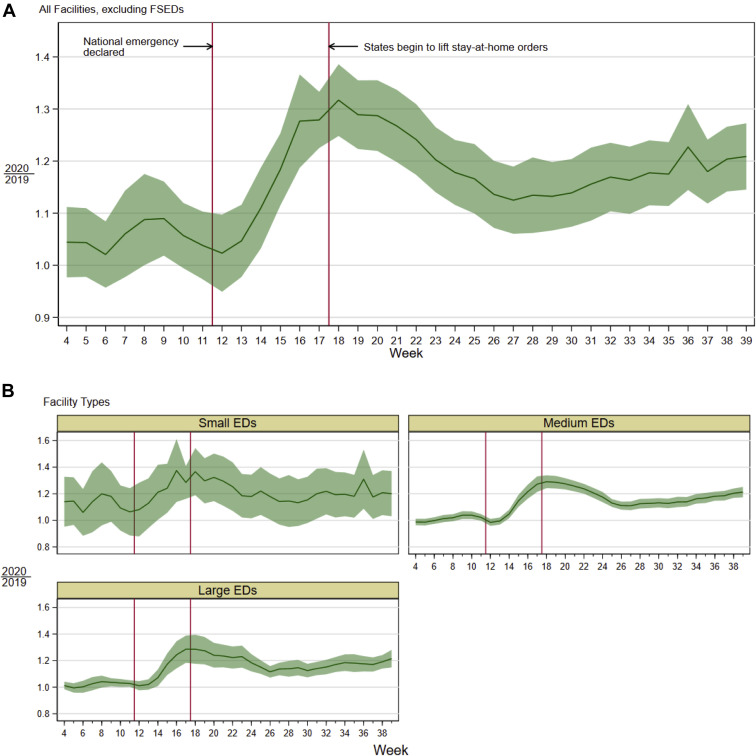
Figure 3 shows the impact of COVID-19 on admission rates at hospital-based EDs. Across all facilities (Figure 3A), admission rates followed a similar pattern to RVUs per visit, increasing during the early pandemic period, then declining as states began to lift stay-at-home orders. However, beginning in late June, admission rate ratios began to rise again. This general trend was present across all hospital-based ED types (Figure 3B).
Figure 3.
2020:2019 ratios of hospital admission rates for 136 EDs. Figure 3 shows 2020:2019 ratios for 24 freestanding EDs, 40 small EDs (<30,000 visits/year), 56 medium EDs (30,000 to 59,999 visits/year), and 16 large EDs (>60,000 visits/year). Red vertical lines divide the prepandemic, early pandemic, and later pandemic time periods. Shaded area around lines are 95% confidence intervals. Hospital admissions included inpatient admissions and observation unit admissions from the ED.
Pandemic Impact on Clinical Revenues and Expenses
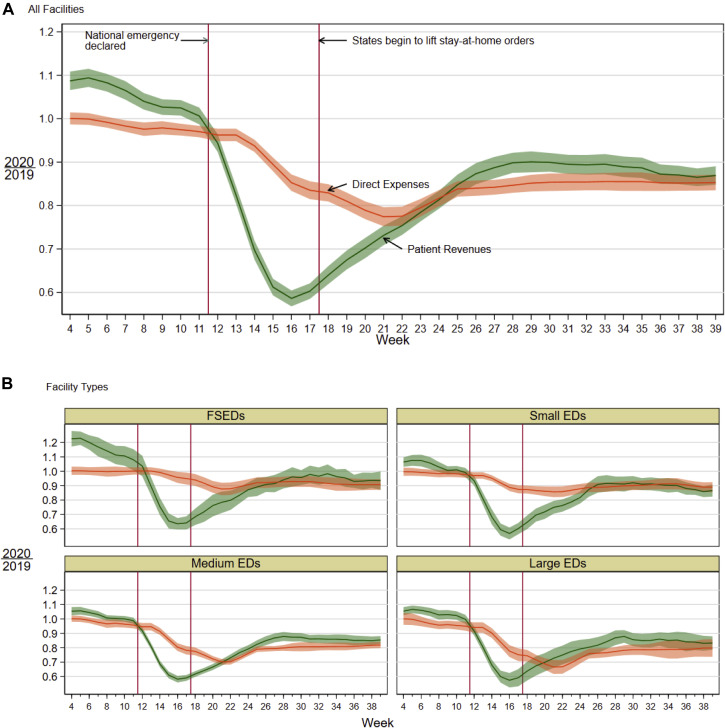
In Figure 4 , we present clinical revenues and expenses by ED size. During the early pandemic, 2020:2019 revenue ratios fell sharply (by similar percentages for all 4 ED types) to approximately 0.6 in mid-April; they then partly recovered, to approximately 0.9 across ED types. However, changes in clinical expenses varied greatly with ED size. For freestanding EDs and small EDs, expenses declined only modestly in the early pandemic period. There were larger initial drops in clinical expenses in medium and large EDs. The expense reductions lagged the drop in revenue by approximately 6 weeks. The rapid drop in revenue and slower change in expenses led to an initial large gap between revenues and expenses for all EDs. This closed gradually for medium and large EDs as revenue partially recovered in mid-2020 and staffing was reduced to more closely match volume. For medium and large EDs, 2020:2019 expense ratios decreased to 0.6 by mid-April but then increased to 0.9 by the end of September. In contrast, at smaller EDs, 2020:2019 direct expense ratios declined to approximately 0.9 by mid-May, with only a small improvement by the end of September.
Figure 4.
2020:2019 ratios of patient revenues and direct expenses in 136 EDs. Figure 4 shows 2020:2019 ratios for 24 freestanding EDs, 40 small EDs (<30,000 visits/year), 56 medium EDs (30,000 to 59,999 visits/year), and 16 large EDs (>60,000 visits/year). Red vertical lines divide the prepandemic, early pandemic, and later pandemic time periods. Shaded area around lines are 95% confidence intervals.
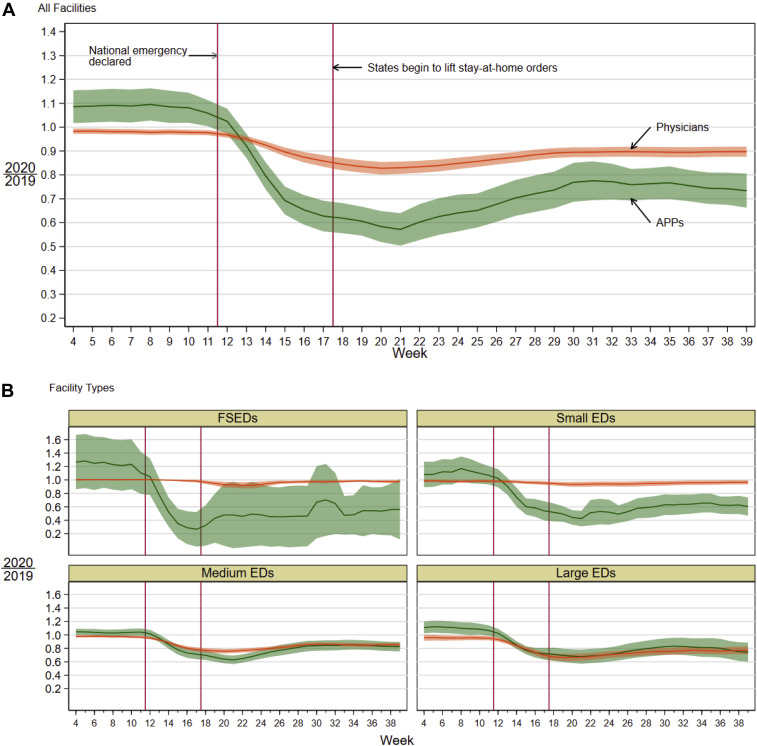
Pandemic Impact on Clinician Hours and Compensation
The impact of the COVID-19 pandemic on clinical hours worked by emergency physicians and advanced practice providers is presented in Figure 5 . The 2020:2019 physician hour ratio across all facility types declined to almost 0.8 and rebounded to 0.9, while the advanced practice provider hour ratio declined to 0.6 and rebounded to between 0.7 and 0.8 (Figure 5A). At freestanding EDs and small EDs, the physician hour ratio remained relatively steady at 1.0, indicating that there was no reduction in physician hours at those sites relative to 2019. In contrast, 2020:2019 advanced practice provider hour ratios declined significantly at those sites, falling to less than 0.3 at freestanding EDs and less than 0.5 at small EDs, before increasing to around 0.6 by the end of September. At medium and large EDs, in contrast, both emergency physician and advanced practice provider hours fell. The 2020:2019 physician hour ratios fell to less than 0.8 at medium EDs and less than 0.7 at large EDs by late April/early May (weeks 19 to 20) before increasing to 0.85 at medium EDs and 0.75 at large EDs by the end of September. Advanced practice provider hours also fell at these larger sites, by somewhat greater percentages for medium EDs and similar percentages for large EDs, although not to the extent seen in the smaller facilities (2020:2019 advanced practice provider hour ratios nadired at 0.6 and 0.7 at medium and large EDs, respectively).
Figure 5.
2020:2019 ratios of clinician hours in 136 EDs. Figure 5 shows 2020:2019 ratios for 24 freestanding EDs, 40 small EDs (<30,000 visits/year), 56 medium EDs (30,000 to 59,999 visits/year), and 16 large EDs (>60,000 visits/year). Red vertical lines divide the pre pandemic, early pandemic, and later pandemic time periods. Shaded area around lines are 95% confidence intervals.
In the Table , we quantify the total impact of the reductions in work hours during the COVID-19 period compared to the prepandemic period in 2020 (Jan 5 to March 14). Across all sites, emergency physician hours were reduced 15% and advanced practice provider hours 27% during the COVID-19 pandemic, translating to a similar percentage loss in clinical compensation. This would correspond to the loss of 174 emergency physician and 193 advanced practice provider full-time-equivalents. Physician hours were cut most significantly at large EDs (−26%) and medium EDs (−18%), while advanced practice provider hours were cut most significantly at freestanding EDs (−49%) and small EDs (−35%).
Table.
Changes to the emergency medicine clinician workforce during the COVID-19 pandemic in 136 emergency departments.
| Emergency Department Type | Mean Hours Worked Per Week Prepandemic | Mean Hours Worked Per Week During Pandemic | Mean Change in Hours Worked Per Week | % Reduction in Hours Worked | Total Hours Reduced During Pandemic (28 Weeks) | Total Reduction in Full-Time-Equivalents |
|---|---|---|---|---|---|---|
| Physician workforce | ||||||
| Freestanding EDs | 4,057 | 3,909 | −148 | −3.6 | 4,144 | 5.5 |
| Small EDs | 6,397 | 6,158 | −239 | −3.7 | 6,692 | 8.9 |
| Medium EDs | 14,261 | 11,719 | −2,542 | −17.8 | 71,176 | 94.1 |
| Large EDs | 6,748 | 4,969 | −1,779 | −26.4 | 49,812 | 65.9 |
| Total | 31,463 | 26,755 | −4,708 | −15.0 | 131,824 | 174.4 |
| Advanced practice provider workforce | ||||||
| Freestanding EDs | 589 | 302 | −287 | −48.7 | 8,036 | 10.6 |
| Small EDs | 2,187 | 1,418 | −769 | −35.2 | 21,532 | 28.5 |
| Medium EDs | 11,089 | 8,379 | −2,710 | −24.4 | 75,880 | 100.4 |
| Large EDs | 5,738 | 4,286 | −1,452 | −25.3 | 40,656 | 53.8 |
| Total | 19,603 | 14,385 | −5,218 | −26.6 | 146,104 | 193.3 |
Note: Clinician hours worked show totals and means across 24 freestanding EDs, 40 small EDs (<30,000 visits/year), 56 medium EDs (30,000 to 59,999 visits/year), and 16 large EDs (>60,000 visits/year). Full-time-equivalents are defined at 108 hours worked/month (27 hours/week). Prepandemic refers to the first 11 weeks of 2020 (excluding week 1) through March 14. Pandemic period refers to the next 28 weeks, from March 15 to September 26, 2020.
Limitations
There are several study limitations. First is the generalizability of our findings outside of the 136 sites, which represent approximately 2% of US EDs. There was a broad recognition by ED practice organizations of the need to reduce clinical hours worked to match volume during the pandemic, but different organizations may have adopted different approaches. This ED practice organization group reduced hours but not per-hour compensation, although clinicians paid partly based on RVUs did suffer some decline in total hourly compensation. Lower clinical revenue due to lower volumes and was only modestly offset by higher complexity. Second, we used expected revenue because actual revenue collected lags visits by a substantial amount of time. While expected revenues track closely with actual revenue ultimately received based on historical experience, results could have differed during the pandemic period.
Third, we considered only clinical expenses (ie, gross margin) and did not account for management costs or employee benefits. The full cost for managing a large group of clinicians and billing revenue from payers and patients (when they have a deductible, copayment, or coinsurance) is considerably higher. Therefore, our results may overestimate the real marginal profitability of ED practice organizations, particularly from solely comparing clinical revenues and expenses. We also did not account for any stipends provided by hospitals to supplement ED clinician revenue, so our analysis may underestimate total payments to maintain each site. Fourthly, we were unable to conduct analyses by race/ethnicity. The pandemic may have impacted ED visits in different racial/ethnic groups differently.
Finally, these data did not account for the Coronavirus Aid, Relief, and Economic Security (CARES) Act federal funding that was provided to the health care system in general, including this ED practice organization, during the pandemic. There was a single large payment to the group from the CARES Act as well as funding payments for uninsured patients evaluated for COVID-19 or COVID-19 related symptoms. Together, this offset roughly 30% of the revenue declines experienced during 2020. We also did not account for revenues or costs related to the use of telemedicine, which increased during the pandemic. Telemedicine revenue represented much less than 1% of clinical revenue during the pandemic period and did not meaningfully affect the gross margin. However, it did marginally supplement clinician income for the 20% of physicians who provided at least some telemedicine services.
Discussion
Our data demonstrates the vulnerability of the economics of an emergency care system that nearly universally reimburses emergency clinician services through fee-for-service payments. During the pandemic period, there were large declines observed for both adult and, even more so, pediatric visits, which severely impacted revenue, early in the pandemic. Visit rates subsequently increased but have remained well below 2019 levels. Another relative decline in ED visits occurred in September. This was more dramatic for pediatric visits, likely because many schools remained remote. This may have reduced child activities that can lead to pediatric ED visits, including reduced spread of infectious disease and fewer accidental injuries.18
ED visits that still took place were of higher average complexity, reflected in higher RVUs per visit and hospital admission rates. Presumably, lower-complexity and lower-acuity patients had greater abilities to avoid ED care, either by at-home care or by seeking treatment through other pathways (eg, physician office visits and telemedicine). Higher-complexity visits increased clinical revenue on a per-visit level but did not make up for the overall volume drops, confirming the larger importance of volume over visit complexity in the current reimbursement system. Workload per patient for the remaining patients was considerably higher, particularly when viewed through the lens of the hospital admission rate, which peaked at 32% above 2019 volumes. As a result of the clinical revenue changes, ED practice organizations, including this one, reduced clinical hours where feasible to maintain economic viability. This adjustment occurred at medium and larger EDs with a roughly 6-week lag, leading to a substantial but time-limited reduction in gross margin during the early pandemic period.
The ED practice organization had a lesser ability to reduce clinical expenses at small hospital-based EDs and freestanding EDs. Thus, small EDs and freestanding EDs were more vulnerable to sustained profitability loss than medium and large EDs. By the end of our study period, patient revenue exceeded clinical expenses at medium and large EDs and also at freestanding EDs, albeit with a smaller margin. However, gross margins remained negative at small EDs. Freestanding EDs and small EDs remain economically stressed because each facility must maintain 24/7/365 coverage by at least a single emergency physician, regardless of patient volume. This brings into question the long-term sustainability of these EDs without subsidies to offset negative margins. Four of the freestanding EDs managed by this ED practice organization closed for a short period during the height of the pandemic. Additionally, one freestanding ED has closed permanently. We excluded these facilities from our study to maintain a balanced panel. The impact of the pandemic on the viability of smaller EDs is of particular concern, considering they commonly serve rural or other underserved communities.19
The economic effects and the staffing responses to the pandemic differed by ED size. For smaller facilities and freestanding EDs, this ED practice organization was unable to meaningfully reduce emergency physician coverage given minimum staffing requirements and instead lowered costs primarily through reducing advanced practice provider hours. For medium and large facilities, there were reductions in both emergency physician and advanced practice provider staffing. A potential effect may be a long-term shift of ED advanced practice providers into other facilities or even other fields of medicine, given the ability of advanced practice providers to switch fields more easily than emergency physicians.20 For medium and large EDs, the reductions in staffing were sufficient, with a lag, to restore the prepandemic balance between revenue and expenses, although this national practice organization still suffered a large, one-time loss. However, these facilities have remained more economically viable than small EDs and freestanding EDs, but this came at the expense of clinician hours and compensation.
Our study results generate larger questions about the economic viability of some small EDs and freestanding EDs. Without external support, any ED needs a minimum patient volume to justify the cost of physician coverage at all times, even without considering the cost of administration and the physical and equipment costs of the ED space. In the current pandemic environment, a significant number of small hospital-based EDs do not appear to be viable without subsidies to practice organizations to offset staffing costs.
Lowered workforce needs translated to reduced clinician hours and resultant compensation. During the pandemic, there was a 15% decline in hours worked for emergency physicians and 27% for advanced practice providers to match the volume demands in the facilities managed by this national group. This translated to a corresponding loss of 174 emergency physician and 193 advanced practice provider full-time-equivalent positions, respectively. We separately observed an all-cause departure of 58 advanced practice providers and 62 emergency physicians from the national group since mid-March. This occurred simultaneously with 2020 and 2021 graduates of emergency medicine residency programs experiencing a challenging job market, as our data were consistent with national trends.21
These negative economic effects on ED clinicians and practice organizations occurred at the same time when the emergency medicine community served as the frontline during a national public health emergency. This included clinicians incurring personal risk through exposure to a novel virus with limited availability of personal protective equipment at some locations, especially in the early pandemic period.22 There was a planned 6% reduction in Medicare reimbursement for emergency physician clinical services in the physician fee schedule from the Centers for Medicare and Medicaid Services, which would have further worsened the economics of ED clinician practices.23 This was postponed in late 2020 but could occur at the end of 2021.24
Our data have implications for the funding of EDs and how ED practice organizations are managed in the longer term postpandemic. First, we demonstrated the vulnerability of a fee-for-service system in funding staffing for facilities that serve the public as the frontline during pandemics and other public health threats and as a safety net for the uninsured. Policymakers should consider our data when creating policies about how to ensure EDs both are properly staffed for everyday care and have surge capacity to handle public health emergencies like the COVID-19 pandemic. Second, special attention is needed for smaller hospital-based EDs, which often serve less populous and/or more rural areas. Reimbursement for readiness needs to be included in the payment model for emergency care to remain viable in smaller communities where clinical volumes may not justify the presence of a 24/7/365 emergency physician.
Finally, our data suggest consideration of alternative payment models for EDs. One example is the global budgets used in Maryland hospitals, which reduced hospitals’ susceptibility to the large volume shifts in the COVID-19 pandemic.25 , 26 A capitation-based model for ED clinician services could be worth exploring, with payment based on the population expected to be served. This could be either a full model for ED clinician revenue or a “floor” on revenue to cushion against financial shocks. Such a capitated model would need to also account for low-acuity visit rates and the role of EDs as a social and health care safety net due to Emergency Medical Treatment & Labor Act requirements. Low-acuity visits fell considerably during the pandemic and have remained depressed but may reappear as people return to prepandemic use patterns. Another consideration is that the return to ED care during the pandemic differed by insurance status, with less of a return for Medicaid and self-pay patients compared to Medicare and commercially insured patients. Given the substantial community benefit of EDs, capitation-based models will need to consider the acute care needs of the entire population served—regardless of insurance status. Models will also need to consider current placement of facilities, some of which are intended more to drive market share rather than fill gaps in care, such as freestanding EDs in wealthier areas.27 , 28
In conclusion, the COVID-19 pandemic has had a dramatic impact on the economics of ED care and the work hours and job prospects for emergency physicians and advanced practice providers. After a period of expenses exceeding clinical payments to emergency clinician groups, medium and large hospital-based EDs have been able to recover financially through lower ED staffing. Small hospital-based EDs and freestanding EDs have remained unprofitable or marginally broken even for emergency clinician groups. This brings into question their long-term viability, particularly if volumes remain depressed for a longer period of time without additional sources of funding beyond the fee-for-service system.
Acknowledgments
The US Acute Care Solutions Research Group acknowledges the broader contributions of Amer Aldeen, MD, Jason Shawbell, RN, MS, Paul Dietzen, BA, and Jesse Eterovich, MBA.
Footnotes
Please see page 488 for the Editor’s Capsule Summary of this article.
Supervising editor: Kristin L. Rising, MD, MS. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: JMP, MZ, BB, RK, PC, AM, and AV conceived of this study. JMP and AV supervised the study. MZ, BB, and AM provided statistical direction. MZ conducted the analysis and created the graphs. PC provided the data and performed data analyses and quality control. JMP and MS drafted the manuscript, and all authors contributed substantially to its revision. JMP takes responsibility for the paper as a whole.
All authors attest to meeting the 4 ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Fundingandsupport: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Readers: click on the link to go directly to a survey in which you can provide feedback to Annals on this particular article.
A podcast for this article is available at www.annemergmed.com.
Contributor Information
US Acute Care Solutions Research Group:
Supplementary Data
References
- 1.Czeisler M.É., Marynak K., Clarke K.E.N., et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong L.E., Hawkins J.E., Langness S., et al. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal Innov Care Deliv. 2020 doi: 10.1056/CAT.20.0193. [DOI] [Google Scholar]
- 3.Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeffery M.M., D'Onofrio G., Paek H., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180:1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pines JM, Zocchi MS, Black BS, et al. How emergency department visits for substance use disorders have evolved during the early COVID-19 pandemic. J Subst Abuse Treat. In press. [DOI] [PMC free article] [PubMed]
- 6.Pines J.M., Zocchi M.S., Black B.S., et al. The effect of the COVID-19 pandemic on emergency department visits for serious cardiovascular conditions. Am J Emerg Med. 2021;47:42–51. doi: 10.1016/j.ajem.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pines J.M. COVID-19, Medicare for all, and the uncertain future of emergency medicine. Ann Emerg Med. 2020;76:459–461. doi: 10.1016/j.annemergmed.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel S.Y., Mehrotra A., Huskamp H.A., et al. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181:388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henneman P.L., Nathanson B.H., Li H., et al. Is outpatient emergency department care profitable? Hourly contribution margins by insurance for patients discharged from an emergency department. Ann Emerg Med. 2014;63:404–411. doi: 10.1016/j.annemergmed.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 10.Pines J.M., Zocchi M.S., De Maio V.J., et al. The effect of operational stressors on emergency department clinician scheduling and patient throughput. Ann Emerg Med. 2020;76:646–658. doi: 10.1016/j.annemergmed.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Harish N.J., Miller H.D., Pines J.M., et al. How alternative payment models in emergency medicine can benefit physicians, payers, and patients. Am J Emerg Med. 2017;35:906–909. doi: 10.1016/j.ajem.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 12.Pines J.M., Penninti P., Alfaraj S., et al. Measurement under the microscope: high variability and limited construct validity in emergency department patient-experience scores. Ann Emerg Med. 2018;71:545–554. doi: 10.1016/j.annemergmed.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 13.Carlson J.N., Foster K.M., Pines J.M., et al. Provider and practice factors associated with emergency physicians’ being named in a malpractice claim. Ann Emerg Med. 2018;71:157–164. doi: 10.1016/j.annemergmed.2017.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pines J.M., Zocchi M.S., Black B.S., et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021;41:201–204. doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boutis K., Stephens D., Lam K., et al. The impact of SARS on a tertiary care pediatric emergency department. CMAJ. 2004;171:1353–1358. doi: 10.1503/cmaj.1031257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Driscoll M., Dos Santos G.R., Wang L., et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. 2021;590:140–145. doi: 10.1038/s41586-020-2918-0. [DOI] [PubMed] [Google Scholar]
- 17.Hutchins H.J., Wolff B., Leeb R., et al. COVID-19 mitigation behaviors by age group—United States, April–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1584–1590. doi: 10.15585/mmwr.mm6943e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee L., Mannix R., Guedj R., et al. Paediatric ED utilisation in the early phase of the COVID-19 pandemic. Emerg Med J. 2021;38:100–102. doi: 10.1136/emermed-2020-210124. [DOI] [PubMed] [Google Scholar]
- 19.Greenwood-Ericksen M.B., Kocher K. Trends in emergency department use by rural and urban populations in the United States. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pines J.M., Zocchi M.S., Ritsema T., et al. The impact of advanced practice provider staffing on emergency department care: productivity, flow, safety, and experience. Acad Emerg Med. 2020;27:1089–1099. doi: 10.1111/acem.14077. [DOI] [PubMed] [Google Scholar]
- 21.COVID-19 capsizes the physician job market: Trends you should know. Brendan Murphy. Accessed March 6, 2021. https://www.ama-assn.org/residents-students/transition-practice/covid-19-capsizes-physician-job-market-trends-you-should
- 22.Livingston E., Desai A., Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323:1912–1914. doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- 23.Revisions to Payment Policies under the Medicare Physician Fee Schedule, Quality Payment Program and Other Revisions to Part B for CY 2021. Centers for Medicare & Medicaid Services. Accessed March 6, 2021. https://www.cms.gov/medicaremedicare-fee-service-paymentphysicianfeeschedpfs-federal-regulation-notices/cms-1734-f
- 24.Major Crisis Averted (for Now): Rather than Medicare Payment Reductions, a Raise May be Coming Your Way In 2021. Davis J. Accessed March 6, 2021. https://www.acep.org/federal-advocacy/federal-advocacy-overview/regs–eggs/regs–eggs-articles/regs–eggs—january-7-2021/
- 25.Galarraga J.E., Black B., Pimentel L., et al. The effects of global budgeting on emergency department admission rates in Maryland. Ann Emerg Med. 2020;75:370–381. doi: 10.1016/j.annemergmed.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 26.Galarraga J.E., DeLia D., Wilhite D., et al. Emergency department care coordination strategies and perceived impact under Maryland's hospital payment reforms. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.12.048. [DOI] [PubMed] [Google Scholar]
- 27.Schuur J.D., Baker O., Freshman J., et al. Where do freestanding emergency departments choose to locate? A national inventory and geographic analysis in three states. Ann Emerg Med. 2017;69:383–392. doi: 10.1016/j.annemergmed.2016.05.019. [DOI] [PubMed] [Google Scholar]
- 28.Pines J.M. Maybe it's time to rethink freestanding emergency departments. Acad Emerg Med. 2019;26:1297–1299. doi: 10.1111/acem.13862. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.