Abstract
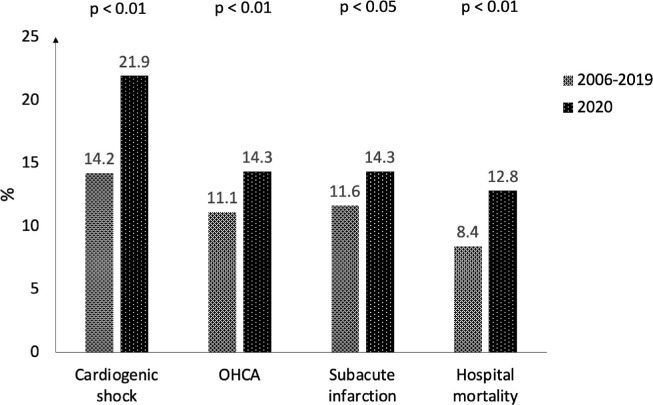
Impact of COVID-19 pandemic and pandemic-related social restrictions on clinical course of patients treated for acute ST-elevation myocardial infarction (STEMI) is unclear. In the present study presentation and outcome of patients with STEMI in the year 2020 were compared with the years before in a German registry that includes all patients hospitalized for acute STEMI in a region with approximately 1 million inhabitants. In the year 2020 726 patients with STEMI were registered compared with 10.226 patients in the years 2006 to 2019 (730 ± 57 patients per year). No significant differences were observed between the groups regarding age, gender and medical history of patients. However, in the year 2020 a significantly higher rate of patients admitted with cardiogenic shock (21.9% vs 14.2%, p <0.01) and out-of-hospital cardiac arrest (OHCA) (14.3% vs 11.1%, p <0.01) was observed. The rate of patients with subacute myocardial infarction (14.3% vs 11.6%, p <0.05) was elevated in 2020. Hospital mortality increased by 52% from the years 2006 to 2019 (8.4%) to the year 2020 (12.8%, p <0.01). Only 4 patients (0.6%) with STEMI in the year 2020 had SARS-CoV-2 infection, none of those died in-hospital. In conclusion, in the year 2020 a highly significant increase of STEMI-patients admitted to hospital with advanced infarction and poor prognosis was observed. As the structure of the emergency network to treat patients with STEMI was unchanged during the study period, the most obvious reason for these changes was COVID-19 pandemic-related lockdown and the fear of many people to contact medical staff during the pandemic.
Since December 2019, a new viral pneumonia caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its clinical manifestation, named coronavirus disease 2019 (COVID-19), spread to a global pandemic.1, 2, 3 The pandemic-related “lockdown” with social distancing restrictions and the fear of many people to contact medical staff should have implications on the incidence and characteristics of patients admitted to hospital with cardiovascular diseases. In the last months researchers from many countries worldwide reported a decrease of hospital admissions due to cardiac emergencies.4, 5, 6, 7, 8, 9, 10 In patients with ST-elevation myocardial infarctions (STEMIs) an increase of mortality has been described.11
We therefore aimed to analyze presentation and outcome of consecutive patients with STEMI in the “corona-year” 2020 compared with the years before, using data of large German STEMI registry.
Methods
The Bremen STEMI registry (BSR) includes data from all patients with STEMI in a region of one million inhabitants in Northwest Germany since the year 2006. All patients which are admitted to the Bremen Heart Centre with the diagnosis STEMI are documented in the registry. Emergency services and regional hospitals are closely connected by telephone and fax with the interventional centre for rapid communication to enable urgent percutaneous coronary interventions (PCI). Documentation for the BSR is done via data sheets completed by the responsible interventional cardiologist and/or through patient records after a cardiologist has confirmed the diagnosis. Data about age, gender, concomitant diseases, severity of STEMI, acute medical or interventional treatment, as well as laboratory parameters at admission and during the hospital stay are recorded. After discharge major adverse cardiac and cerebral events as well as bleeding events are documented through follow-up examination performed after 1, 5, and 10 years by a telephone interview. Before inclusion of patient records in the database, a written consent on study participation was obtained. The BSR was approved by the ethical committee of the Ärztekammer Bremen, Germany. Studies about methods and results from the BSR have been previously published elsewhere.12, 13, 14
For the present analysis all consecutive patients with STEMI documented in the BSR in the year 2020 were compared with the patients in the years before (2006 to 2019). The groups were compared regarding clinical presentation, treatment and hospital outcome of the patients.
According to international guidelines, STEMI was defined as persistent angina pectoris for ≥ 20 minutes in conjunction with a ST segment elevation in two contigous leads of ≥ 0.25 mV in men below the age of 40 years, ≥ 0.2 mV in men over the age of 40 years, or ≥ 0.15 mV in women in leads V2-V3 and/or ≥ 0.1 mV in all other leads or new left bundle branch block (LBBB).15
Subacute STEMIs were defined as STEMIs with >12 hours between first symptoms and first medical contact and/or signs of a subacute myocardial infarction in the ECG at admission. As the period between symptoms and first medical contact was not known in some cases, especially in patients with out-of-hospital cardiac arrests (OHCA) and cardiogenic shock that died during hospital course, signs of subacute myocardial infarction in the ECG were included in the definition of subacute STEMIs to make the diagnosis when symptom-to-medical contact time was not available.
Baseline characteristics of patients were described by mean values and standard deviations for continuous variables. Absolute numbers and percentages were reported for categorical variables. Data were tested for normal distribution by Kruskal-Wallis testing and distribution analysis. For continuous variables comparison between the groups was done by t-tests (if data were normally distributed) or Mann-Whitney-U-tests (if data were not normally distributed). For categorical variables groups were compared by chi-square tests and Fisher's exact tests (if events were rare). A p value < 0.05 was considered as statistically significant. All calculations were done with SPSS (IBM, version 22).
Results
In the year 2020 726 patients with STEMI were documented in the BSR. In the 14 years before, a mean of 730 ± 57 patients per year, with a total of 10.226 patients between 2006 and 2019, was registered in the BSR. Comparing the both groups, no significant differences were observed regarding age (64.8 ± 12.3 years vs 64.1 ± 13.3 years, p = n.s.), gender (74.9% vs 72.2% male, p = n.s.) and medical history of the patients, such as prior myocardial infarction, diabetes mellitus or active smoking (Table 1 ).
Table 1.
Patients admitted with STEMI in the year 2020 versus 2006 to 2019
| Parameter | 2020 (n = 726) | 2006-2019 (n = 10.226) |
|---|---|---|
| Age (years), MV ± SD | 64.8 ± 12.3 | 64.1 ± 13.3 |
| Men | 544 (74.9%) | 7379 (72.2%) |
| Prior myocardial infarction | 97 (13.4%) | 1134 (11.1%) |
| Diabetes mellitus | 155 (21.3%) | 1992 (19.5%) |
| Active smokers | 282 (38.8%) | 4183 (40.9%) |
| Admission data: | ||
| Cardiogenic shock = Killip IV | 159 (21.9%)⁎⁎ | 1456 (14.2%)⁎⁎ |
| Killip III | 12 (1.7%) | 161 (1.6%) |
| Killip II | 8 (1.1%) | 147 (1.4%) |
| No signs of HF = Killip I | 547 (75.3%)⁎⁎ | 8462 (82.7%)⁎⁎ |
| Out-of-hospital cardiac arrest | 104 (14.3%)⁎⁎ | 1133 (11.1%)⁎⁎ |
| Subacute myocardial infarction | 104 (14.3%)* | 1182 (11.6%)* |
p <0.05,
p <0.01 between the groups
MV ± SD indicates mean value ± standard deviation
HF indicates heart failure;
Subacute myocardial infarction indicates >12 hours between first symptoms and first medical contact and/or signs of a subacute myocardial infarction in the ECG at admission.
However, in the year 2020 a highly significant increase of patients that were admitted with cardiogenic shock (21.9% vs 14.2%, p <0.01) and after OHCA (14.3% vs 11.1%, p <0.01) was observed. The proportion of patients without any clinical signs of heart failure (Killip class I) at admission was significantly lower in the year 2020 than in the years before (75.3% vs 82.7%, p <0.01). The rate of patients with subacute myocardial infarction was elevated by 23% in the year 2020 (14.3% vs 11.6%, p <0.05) (Table 1).
Comparing the admission data of 2020 with each year from 2006 to 2019, the rates of cardiogenic shock, OHCA and subacute myocardial infarction in the year 2020 were higher than that of any year from 2006 to 2019 (Supplemental Table 1).
The maximum creatine kinase levels did not differ significantly between the groups; however, a higher rate of patients with coronary 3-vessel disease (37.0% vs 31.7%, p <0.01) was observed in patients that were admitted in the year 2020 (Table 2 ).
Table 2.
Hospital course of patients with STEMI in the year 2020 versus 2006-2019
| Parameter | 2020 (n = 726) | 2006-2019 (n = 10.226) |
|---|---|---|
| Clinical findings and treatment: | ||
| Coronary 3-vessel diseasea | 264 (37.0%)⁎⁎ | 3215 (31.7%)⁎⁎ |
| Revascularization therapy by primary PCI | 658 (90.6%) | 9201 (90.0%) |
| Door-to-balloon-time, minutes MV ± SD | 39 ± 15⁎⁎ | 45 ± 22⁎⁎ |
| Revascularization therapy by emergency CABG | 35 (4.8%) | 494 (4.8%) |
| No revascularization therapy | 33 (4.5%) | 531 (5.2%) |
| Maximum CK-levels, U/l MV ± SD | 1915 ± 3860 | 1910 ± 3075 |
| Outcome: | ||
| Reinfarction | 2 (0.3%) | 83 (0.8%) |
| Stroke | 2 (0.3%) | 55 (0.5%) |
| In-hospital cardiac arrest | 46 (6.3%)* | 481 (4.7%)* |
| Mortality | 93 (12.8%)⁎⁎ | 864 (8.4%)⁎⁎ |
p <0.05,
p <0.01 between the groups.
In 84 patients (n = 12 in the year 2020, n = 72 in the years 2006 to 2019) patients died before coronary status could be obtained.
MV ± SD indicates mean value ± standard deviation; CK = creatine kinase; CABG = coronary artery bypass grafting; PCI = percutaneous coronary intervention.
Rate of revascularization therapy was not different between the groups; only 4.5% vs. 5.2% (p = n.s.) did not receive revascularization therapy (PCI or emergency CABG), because they died before revascularization therapy could be performed or coronary artery disease was treated conservatively. Door-to-balloon-time of interventionally treated patients was lower in the year 2020 compared with the years before (Table 2).
A low rate of reinfarctions or strokes was observed during hospital course without significant difference between the groups (Table 2). However, in the year 2020 an increased rate of in-hospital cardiac arrests (6.3% vs 4.7%, p <0.05) was documented. Hospital mortality increased by 52% from the years 2006 to 2019 (8.4%) to the year 2020 (12.8%, p <0.01) (Figure 1).
Figure 1.
Major differences between patients with STEMI admitted to hospital in the year 2020 versus 2006-2019. OHCA indicates out-of-hospital cardiac arrest.
Analyzing the results of SARS-CoV-2 testings in patients hospitalized due to STEMI, only 4 patients (0.6%) had positive tests, while 624 patients had negative tests. In 98 patients at the begin of the year 2020 no SARS-CoV-2 tests were performed (because in the first weeks of the year 2020 no serial SARS-CoV-2 testings were performed). None of the SARS-CoV-2 positive STEMI-patients died in-hospital.
Discussion
The main result of the present study was that in the “corona-year” 2020 patients with STEMI presented with a 54% increased rate of cardiogenic shock and a 29% increased rate of OHCA. Hospital mortality was elevated by 52% compared with the years before. The most obvious reason for these changes was COVID-19 pandemic-related lockdown and the fear of many people to contact medical staff and clinics during the pandemic.
The rate of patients admitted with STEMI in the year 2020 was similar to the years before. This was in contrary to the rate of cardiac catheterizations for other diagnoses, such as unstable angina or chronic coronary syndrome, at the Bremen Heart Center, that decreased in the year 2020. However; this was in good accordance to the study of Stöhr et al., who reported a decrease in admissions for syncope and/or dizziness, heart failure or unstable angina, but not for unavoidable admissions, such as STEMIs, strokes or patients after resuscitations.6
Although the number of patients with STEMI did not change in the year 2020, the characteristics of patients with STEMI did dramatically. Our data demonstrate high rates of patients presenting with cardiogenic shock, after OHCA and with subacute myocardial infarction in the year 2020. In line with that, studies from Italy and the United States reported an increase of OHCAs with low rates of return of spontaneous circulation since the COVID-19 pandemic began.16, 17, 18 In a large survey of the European Society of Cardiology approximately 60% of all physicians reported that STEMI-patients presented later than usual and >40% of patients admitted to hospital presented beyond the optimal time window for PCI.10 Independent predictors of the reported higher rate of delayed STEMI presentation were a country in total lockdown, >100 COVID-19 cases admitted locally, and the complete restructuring of the local cardiology service.10
It was not surprising in the present study that the high rate of patients with cardiogenic shocks and after OHCA in the year 2020 resulted in a high rate of in-hospital cardiac arrests and mortality, because cardiogenic shock and OHCA are known to be strong predictors of impaired outcome.19 , 20 The high mortality of STEMI-patients was observed although door-to balloon-time improved in the year 2020.
As the structure of emergency catheterization in the analyzed cohort is monocentric and unchanged since many years, an external factor should have led to the changes in presentation and outcome of patients with STEMI: COVID-19 pandemic.
It might be argued that SARS-CoV-2 infection directly led to an increase of patients with advanced STEMI and to a poor prognosis, because numerous studies have shown deleterious effects of SARS-CoV-2 infection on the cardiovascular system.21 , 22 Different pathophysiological mechanisms of SARS-CoV-2 infection have been reported that induce or worsen cardiovascular diseases, such as inflammatory activation and cytokine storm leading to acute coronary syndromes, arrhythmias and heart failure, or coagulation abnomalities leading to thrombotic events.23 , 24 However, in our study less than 1% of all patients with STEMI had SARS-CoV-2 infection, the vast majority of STEMI-patients had negative SARS-CoV-2 tests, so that the impaired prognosis of STEMI-patients in the year 2020 was not directly caused by SARS-CoV-2 infection.
A much more conclusive explanation of the high rate of advanced myocardial infarctions at hospital admission in the year 2020 was the pandemic-related lockdown with social distancing rules and the fear of people of contracting the virus in clinics, that hampered people to seek medical help in case of cardiac symptoms.
In conclusion, the present study reports an alarming increase of STEMI-patients admitted with cardiogenic shock, OHCA and subacute myocardial infarction in the year 2020, leading to an elevation of hospital mortality by 52%. The most obvious explanation of these changes was pandemic-related lockdown and the fear of people to seek medical help during the pandemic. It is therefore crucial to inform people that the risk of untreated STEMI is much higher than the risk of contracting the virus in-hospital. If this public education will not be successful, a worsening of STEMI-prognosis is further to be expected, as a collateral damage of COVID-19 pandemic.
Credit Author Statement
Harm Wienbergen: Conceptualization, Methodology, Project administration, Data curation, Writing – Review & Editing.
Tina Retzlaff: Investigation, Data curation
Johannes Schmucker: Investigation, Data curation
Luis Albert Mata Marin: Investigation, Data curation
Stephan Rühle: Investigation, Data curation
Daniela Garstka: Investigation, Data curation
Rico Osteresch: Investigation, Project administration
Andreas Fach: Investigation, Project administration
Rainer Hambrecht: Conceptualization, Methodology, Project administration, Writing – Review & Editing.
Disclosures
The authors have no conflict of interest to declare.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.amjcard.2021.04.011.
Appendix. Supplementary materials
REFERENCES
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) WHO; Geneva, Switzerland: 2021. WHO coronavirus disease (COVID-19) dashboard.https://www.who.int (Accessed 30. March 2021) [Google Scholar]
- 4.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, Ambrosy AP, Sidney S, Go AS. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 5.De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omede P, Pennone M, Patti G, Mancone M, De Ferrari GM. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stoehr E, Aksoy A, Campbell M, Al Zaidi M, Ozturk C, Vorloeper J, Lange J, Sugiura A, Wilde N, Becher MU, Diepenseifen C, Heister U, Nickenig G, Zimmer S, Tiyerili V. Hospital admissions during Covid-19 lock-down in Germany: differences in discretionary and unavoidable cardiovascular events. PLoS One. 2020;15 doi: 10.1371/journal.pone.0242653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nef HM, Elsaesser A, Moellmann H, Abdel-Hadi M, Bauer T, Bruck M, Eggebrecht H, Ehrlich JR, Ferrari MW, Fichtlscherer S, Hink U, Holschermann H, Kacapor R, Koeth O, Korboukov S, Lamparter S, Laspoulas AJ, Lehmann R, Liebetrau C, Plucker T, Pons-Kuhnemann J, Schachinger V, Schieffer B, Schott P, Schulze M, Teupe C, Vasa-Nicotera M, Weber M, Weinbrenner C, Werner G, Hamm CW, Doerr O. Impact of the COVID-19 pandemic on cardiovascular mortality and catherization activity during the lockdown in central Germany: an observational study. Clin Res Cardiol. 2021;110:292–301. doi: 10.1007/s00392-020-01780-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dreger H, Bruch L, Maier B, Schuehlen H. Acute myocardial infarction admissions in Berlin during the COVID-19 pandemic. Dtsch Arztebl Int. 2020;117:597–598. doi: 10.3238/arztebl.2020.0597. [DOI] [PubMed] [Google Scholar]
- 9.Bugger H, Gollmer J, Pregartner G, Wunsch G, Berghold A, Zirlik A, von Lewinski D. Complications and mortality of cardiovascular emergency admissions during COVID-19 associated restrictive measures. PLoS One. 2020;15 doi: 10.1371/journal.pone.0239801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, Zamorano JL, Weidinger F, Achenbach S, Maggioni AP, Gale CP, Poppas A, Casadei B. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6:210–216. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gluckman TJ, Wilson MA, Chiu ST, Penny BW, Chepuri VB, Waggoner JW, Spinelli KJ. Case Rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020;5:1419–1424. doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmucker J, Wienbergen H, Seide S, Fiehn E, Fach A, Wuermann-Busch B, Gohlke H, Guenther K, Ahrens W, Hambrecht R. Smoking ban in public areas is associated with a reduced incidence of hospital admissions due to ST-elevation myocardial infarctions in non-smokers. Results from the Bremen STEMI Registry. Eur J Prev Cardiol. 2014;21:1180–1186. doi: 10.1177/2047487313483610. [DOI] [PubMed] [Google Scholar]
- 13.Backhaus T, Fach A, Schmucker J, Fiehn E, Garstka D, Stehmeier J, Hambrecht R, Wienbergen H. Management and predictors of outcome in unselected patients with cardiogenic shock complicating acute ST-segment elevation myocardial infarction: results from the Bremen STEMI Registry. Clin Res Cardiol. 2018;107:371–379. doi: 10.1007/s00392-017-1192-0. [DOI] [PubMed] [Google Scholar]
- 14.Fach A, Buenger S, Zabrocki R, Schmucker J, Conradi P, Garstka D, Fiehn E, Hambrecht R, Wienbergen H. Comparison of outcomes of patients with ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention analyzed by age groups (<75, 75 to 85, and >85 Years); (results from the Bremen STEMI Registry) Am J Cardiol. 2015;116:1802–1809. doi: 10.1016/j.amjcard.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 15.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119–177. doi: 10.1016/j.rec.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021;6:296–303. doi: 10.1001/jamacardio.2020.6210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S, Lombardia Cr. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shekhar AC, Effiong A, Ruskin KJ, Blumen I, Mann NC, Narula J. COVID-19 and the prehospital incidence of acute cardiovascular events (from the Nationwide US EMS) Am J Cardiol. 2020;134:152–153. doi: 10.1016/j.amjcard.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acharya D. Predictors of outcomes in myocardial infarction and cardiogenic shock. Cardiol Rev. 2018;26:255–266. doi: 10.1097/CRD.0000000000000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeFilippis EM, Singh A, Gupta A, Ayuba G, Biery D, Divakaran S, Collins BL, Qamar A, Fatima A, Hainer J, Klein J, Nasir K, Di Carli MF, Bhatt DL, Blankstein R. Long-term outcomes after out-of-hospital cardiac arrest in young patients with myocardial infarction. Circulation. 2018;138:2855–2857. doi: 10.1161/CIRCULATIONAHA.118.036506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17:543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quere I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.