Abstract
Background:
Previous research has demonstrated that heavy alcohol consumption and maladaptive eating behaviors co-occur among college students, but less is known about patterns of these behaviors in a more diverse community-dwelling emerging adult sample. The purpose of this study was to: 1) identify classes of emerging adults by their reported alcohol consumption patterns, food addiction symptoms, and body mass index; and 2) determine whether these classes differed on behavioral economic reinforcer pathology indices (e.g., environmental reward deprivation, impulsivity, alcohol demand).
Method:
Emerging adult participants recruited as part of a study on risky alcohol use (n = 602; 47% white, 41.5% Black; mean age = 22.63, SD = 1.03) completed anthropometric measures and indices of alcohol and food-related risk factors.
Results:
Latent profile analysis suggested a four-profile solution: a moderate alcohol severity, overweight profile (Profile 1; n = 424, 70.4%), moderate alcohol severity, moderate food addiction + obese profile (Profile 2; n = 93, 15.4%), high alcohol severity, high food addiction + obese profile (Profile 3; n = 44, 7.3%), and high alcohol severity, overweight profile (Profile 4; n = 41, 6.8%). Individuals in Profile 1 reported significantly lower levels of environmental reward deprivation compared to both Profile 2 and 3 and participants in Profile 3 reported significantly higher environmental reward deprivation compared to those in Profile 4 (p < .001). Profile 4 demonstrated significantly higher alcohol demand intensity and Omax and lower demand elasticity compared to Profile 1, Profile 2, and Profile 3. Profile 4 also demonstrated significantly greater proportionate substance-related reinforcement compared to Profile 1 (p < 001) and Profile 2 (p = .004).
Conclusion:
Maladaptive eating patterns and alcohol consumption may share common reinforcer pathology risk factors including environmental reward deprivation, impulsivity, and elevated alcohol demand.
Keywords: alcohol use, food addiction, emerging adults, obesity, behavioral economics
Introduction
Heavy episodic drinking (defined as 4+/5+ alcohol drinks in a single occasion for women/men) tends to peak between ages 18 to 25, with approximately 33% of U.S. college students and 28% of noncollege same aged peers reporting heavy episodic drinking in the past two weeks (Schulenberg et al., 2018). These patterns of drinking are associated with a range of acute consequences (Hingson et al., 2017), including poor academic and career outcomes (Jennison, 2004) and an increased likelihood of developing an alcohol use disorder in the future (Prince et al., 2019). Heavy drinking often co-occurs with other health-risk behaviors which increases risk for health problems and early mortality (Myint et al., 2009). For example, about half of adults who engage in risky drinking have also reported problematic eating behaviors (Bahji et al., 2019). The co-occurrence of heavy drinking and overeating is particularly important because both have been linked to chronic illnesses such as cardiovascular disease, diabetes, cancer, and obesity (Hruby et al., 2016; Zhou et al., 2016).
Given the developmental, physiological, and neurobiological similarities that predict the onset and course of both alcohol use and overeating (Volkow and Baler, 2014), some researchers have argued for the inclusion of food addiction (FA) in the Diagnostic and Statistical Manual of Mental Disorders (DSM). FA is characterized by an addictive cycle of compulsive overconsumption of highly palatable foods (Shell and Firmin, 2017). There is substantial overlap in the behaviors and symptoms exhibited by individuals with substance use disorders and overeating. Because of this overlap, FA measures such as the Yale Food Addiction Scale 2.0 (Gearhardt et al., 2016) were developed and adapted directly from the DSM-5 criteria for substance use. Despite the etiological and behavioral similarities, no research to date has examined patterns of severity of FA along with patterns of alcohol use, alcohol-related problems, and obesity-related outcomes in a community-based emerging adult sample.
Overall, there is evidence that increased alcohol consumption is associated with greater maladaptive eating behaviors among college students (Kelly-Weeder and Edwards, 2011; Martin et al., 2015; Pedrelli et al., 2011; Rush et al., 2009, 2016), particularly for women (Kelly-Weeder and Edwards, 2011). However, a subgroup of college student drinkers has also been identified who engage in compensatory behaviors, such as restrictive eating, to counteract calories consumed from drinking (Wilkerson et al., 2017). Thus, it is possible that patterns of relationships between these health risk behaviors may vary by individuals. However, previous research that examined risk factors for alcohol and food-related pathology among emerging adults has relied on traditional variable-centered approaches, which produce a single set of averaged parameters based on the assumption that the population is homogeneous. In contrast, person-centered approaches empirically identify relatively homogenous subgroups of individuals characterized by similar constellations of risk and may thus determine whether specific classes of emerging adults exist with similar patterns of alcohol use, problems, maladaptive eating behaviors, and obesity. Further, given that previous research has been conducted among college students and not a broader sample of emerging adults, generalizability is limited. This limitation is especially important because although college students tend to report higher levels of drinking, attainment of a 4-year degree is ultimately protective against long-term alcohol use disorder symptoms and obesity (Crum et al., 1993; Ogden et al., 2018). In light of these limitations, there is a need for person-centered data analytic approaches that identify classes of alcohol use/problems and eating behaviors/body mass index (BMI)/body composition in a large, diverse sample of college and non-college emerging adults and to identify how these classes differ on important theoretically-driven risk factors for both behaviors.
Shared Behavioral Economic Risk Factors for Maladaptive Eating and Risky Drinking
Behavioral economic models have been applied to both alcohol use and obesity but to date no studies have applied these models to understand how patterns of these co-occurring health risk behaviors differ by BE risk factors (Carr and Epstein, 2020; Vuchinich and Tucker, 1983). Behavioral Economic (BE) Theory integrates operant psychology and microeconomics and posits that individuals make choices based on the perceived costs and benefits of a given behavior or commodity compared to the available alternatives (Carr and Epstein, 2020; Epstein et al., 2018). Both calorie dense foods and alcohol require little effort to obtain/consume and generate immediate and potent experiences of reward, which make them powerful reinforcers (Bickel et al., 2018; Carr et al., 2011). According to BE, both excessive substance use and food overconsumption result from a “reinforcer pathology” processes that is driven by a tendency to sharply devalue delayed outcomes (e.g., health and other rewards) in favor of immediate rewards such as food and alcohol ((Bickel et al., 2011, 2014; Temple et al., 2008)). Elevated demand refers to strong motivation to consume a substance even in the presence of a high price or response cost. Importantly, strong preference for immediately available reinforcers such as alcohol and highly palatable food is most likely to develop in contexts that are devoid of other sources of reward such as healthy recreational or leisure activities, and thus environmental reward deprivation is a risk factor for both alcohol use disorder and obesity (Buscemi et al 2014; Joyner et al 2016).
Reinforcing value for both alcohol and food has been measured via purchase tasks which generate demand curves that plot consumption and associated expenditures as a function of price (Murphy et al., 2009; Murphy and MacKillop, 2006) or through reinforcement surveys which measure the reinforcement value of the substance based on the product of the frequency of engagement in and enjoyment of a particular substance (Buscemi et al., 2014; Murphy et al., 2005). Individual differences in reward value can also be impacted by factors such as delay discounting (DD), which describes a preference for immediate rewards as opposed to delayed rewards and is related to impulsivity. Behavioral economic researchers have developed the reinforcer pathology model to describe how elevated reward value interacts with steep DD to generate excessive preference for immediately available and high potency rewards such as palatable foods and alcohol/drugs (Bickel et al., 2014, 2011; Temple et al., 2008). Thus, individuals who highly value alcohol/palatable foods AND have difficulty delaying rewards are at highest risk for overconsumption. Results from studies investigating BE constructs have been fairly consistent, such that reward, DD, and impulsivity assessed by measures such as the Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency, Impulsive Behavior Scale (UPPS-P; Whiteside and Lynam, 2001), predict use and problems for alcohol (Acuff et al., 2018; Murphy and Dennhardt, 2016), overeating (Epstein and Saelens, 2000; Raynor and Epstein, 2003), and obesity (Epstein et al., 2010; Saelens and Epstein, 1996). However, it is unknown how these constructs differ across classes of emerging adults based on alcohol use and problems, maladaptive eating patterns, and objective measures of obesity.
In sum, previous literature is limited in the following ways: 1) no studies to date have utilized person-centered approaches to identify classes of emerging adults based on alcohol use/problems and eating behaviors/BMI/body composition; and 2) no studies to date have investigated how BE indices differ based on patterns of co-occurring health risk behaviors. Further, most research exploring relations between alcohol use and maladaptive eating in emerging adults have been limited to relatively homogeneous college student sample. Thus, the purpose of the current study was to 1) identify classes of emerging adults by their alcohol consumption patterns/problems and FA/BMI/body composition; and 2) determine whether these classes differed by BE indices (e.g., environmental reward deprivation, impulsivity, and alcohol demand). We hypothesized that higher-risk profiles (e.g., higher alcohol use and higher BMI/food addiction scores) would have higher levels of alcohol-related reward and impulsivity and higher levels of environmental reward deprivation. Findings from the current study will inform the etiological models to incorporate co-occurrence of these two highly common health risk behaviors.
Materials and Methods
Participants
Eligible participants (n = 602; 47% white, 41.5% Black, mean age 22.63, 57.3% female) were between the ages of 21.5 and 24.99 and reported drinking at least 3 or 4 alcoholic drinks for women or men, respectively, on two or more occasions in the past month. Individuals were ineligible if they were currently in alcohol or drug use treatment, reported a psychotic disorder, or were not fluent in English.
Procedures
Participants were recruited as a part of a larger longitudinal study between September of 2017 and February of 2019. Recruitment methods included: social media advertisements, flyers, departmental research pools, emails, and in-person recruitment at various events (e.g., concerts, sporting events). All interested participants were screened for eligibility prior to providing informed consent to participate. Participants provided written informed consent and completed an individual in-person testing session that lasted 2 hours in duration for which they were compensated $40. During the session, eligible participants completed anthropometric measures and various measures on demographics, alcohol use, and psychosocial risk factors related to substance use. All procedures received approval from the University of Memphis’ Institutional Review Board (project #4320).
Measures
Latent Profile Indicator Measures.
Alcohol Misuse.
Typical drinks per week.
Alcohol consumption was measured using the Daily Drinking Questionnaire (Collins et al., 1985), which asks participants to report the average number of standard drinks consumed on each day of a typical week in the last month. Consumption across the week was summed to obtain the typical drinks per week.
Alcohol problems.
The Young Adult Alcohol Consequences Questionnaire (YAACQ; Read et al., 2006) asks participants to report whether or not they have experienced 48 problems commonly associated with drinking. These items are summed to create a total score, with higher scores indicating a greater number of past month problems. Internal consistency was excellent in the current sample (α = .93).
Alcohol use disorder (AUD).
Participants endorsed whether or not they had experienced each of the 11 symptoms of AUD over the past year as defined in the DSM-5 (American Psychiatric Association, 2013).
Body Composition and Eating Behavior.
Food Addiction.
The Yale Food Addiction Scale 2.0 (Gearhardt et al., 2016) is a 35-item measure reflecting symptoms of food addiction found in the DSM-5. Respondents report how often each statement applied to them in the past year on an 8-point scale (0 – Never to 7 – Every day). The items are recoded into the 11 equivalent symptoms of substance use disorder (range of scores is 0–11).
Body Composition.
Body composition indices were measured using a TBF 105 (Tanita Corporation, Tokyo, Japan). The measurements were performed in a standing position, with electrodes in contact with soles and heels of both feet. Biological impedance was measured with 4 terminals; a sine wave current with frequency 50Hz and 0.80 mA was applied via sourced electrodes on both feet, and the voltage drop was compared with the heel electrodes. Outputs included in the current analysis are weight, percent body fat, visceral fat, basal metabolic rate (BMR) and muscle mass. Body mass index (BMI) was calculated as weight/(height2).
Outcomes Measures.
Reward Functioning.
The Reward Probability Index (RPI; Carvalho et al., 2011) is a 20-item measure assessing reward access and engagement in one’s environment. Participants report how much each statement reflects their experience in the past month on a 4-point rating scale (1 – strongly disagree to 4 – strongly agree). Items load onto two factors: the reward probability factor (α = .87), which measures whether the individual experiences a broad range of situations and events that will be rewarded and reinforced (higher scores indicate greater reward probability); and the environmental suppressors factor (α = .84), which measures the availability of reinforcers in an individual’s environment and exposure to punishing or aversive experiences (with higher scores indicating greater environmental reward deprivation). Previous research indicates that AUD symptoms are associated with greater environmental reward deprivation (Joyner et al., 2016). Internal consistency was good for reward probability factor and the environmental suppressors factor (α = .84).
Alcohol Reinforcing Value.
Alcohol demand was measured with an alcohol purchase task, in which participants reported the number of standard drinks they would purchase at each price in a series of 30 escalating prices ($0.00 - $40.00 per drink). The current study examined three observed indices: intensity (consumption with no constraint, or when drinks are free), breakpoint (price at which consumption reaches zero), and Omax (maximum expenditure). We also derived elasticity (the rate of change in consumption as a function of price) using the exponentiated equation (Koffarnus et al., 2015). Greater elasticity means a greater impact of price on consumption, thus reflecting lower alcohol demand. In the current study, k was tested at rates of 2, 3, and 4 to determine the greatest variance accounted for in the data by the equation, and k was held constant across participants at 4. Data was cleaned using the Stein macro (Stein et al., 2015) based on the following criteria: (1) trend (detection limit for ΔQ < 0.025); (2) bounce (detection limit for B = 0.10); (3) reversal from zero (detection limit number for reversals = 2 or more). Responding on hypothetical purchase tasks are correlated with actual purchasing behavior (Amlung and MacKillop, 2015), and test-retest reliability for alcohol purchase tasks are robust (Acuff and Murphy, 2017).
Reinforcing value of substance-related relative to substance-free activities was measured with the Activity Level Questionnaire (Meshesha et al., 2020). Participants reported the frequency (0 times to 4 – More than once a day) and enjoyment (0 – Unpleasant or neutral to 4 - Extremely pleasant) of 37 activities while both under the influence of any substances and while sober. Frequency and enjoyment ratings for substance-related and substance-free activities are multiplied together to create a cross product representing substance-related (Cronbach’s alpha [α] = .93) and substance-free reinforcement (α = .88). Next, a ratio (r-ratio) was created representing substance-related reinforcement relative to total reinforcement (substance-related reinforcement / [substance-free reinforcement + substance-related reinforcement). Similar reinforcement survey measures of reinforcement ratio have demonstrated good reliability and validity among young adult drinkers (Hallgren et al., 2016).
Delay Discounting.
The Effective Delay – 50 (ED-50) measure (Koffarnus and Bickel, 2014) is a 5-item discounting procedure used to assess intertemporal choice behavior. Participants choose between larger, later and smaller sooner rewards (e.g., “Would you rather have $1000 in 3 weeks or $500 now?”). Items titrate based on participant responses to determine the indifference point (point at which the choice shifts from delayed to immediate choices). For example if the participant chooses the delayed choice in the option above, the delay will increase until the participant chooses the immediate choice; alternatively, if the participant chooses the immediate choice above, the delay will decrease until the participant shifts to the delay.
Impulsivity.
The Short UPPS-P scale (Cyders et al., 2014) is a 20-item measure assessing various facets of impulsivity. Respondents indicate how much they agree with each statement on a 4-point scale (0 – agree strongly to 4 – Disagree strongly). The UPPS-P is made up of five scales: negative urgency (“When I feel bad, I will often do things I later regret in order to make myself feel better now”; α = .76), lack of perseverance (“I generally like to see things through to the end”; α = .70), lack of premeditation (“My thinking is usually careful and purposeful” α = .81), sensation seeking (“I quite enjoy taking risks”; α = .65), and positive urgency (“When I am in great mood, I tend to get into situations that could cause me problems”; α = .73).
Data Analysis
Latent profile analysis (LPA) was conducted using Mplus version 8 (Muthén, & Muthén, 2017), following the manual three-step BCH method (Bakk & Vermunt, 2015; Bolck, Croon, & Hagenaars, 2004). For all models, full-information maximum likelihood (FIML) was used to account for missing data and robust maximum likelihood estimation (MLR) was used to account for non-normal data. For the first step of the manual-BCH method, indicators for the LPA included standardized versions of alcohol problems, typical drinks per week, alcohol use disorder, food addiction, body fat, muscle mass, and BMI. We searched for the optimal class solution by comparing fit statistics across differing models with one to five profiles. For all models, we covaried alcohol indicators with one another, and we covaried all food-related variables with one another. Models were estimated using 1,500 random sets of start values with 50 iterations to avoid misidentification of a false local solution (Hipp & Bauer, 2006).
We assessed four fit indices to compare models and to determine the profile solution resulting in optimal fit. We reported the Akaike Information Criterion (AIC; Akaike, 1974) and Bayesian Information Criterion (BIC; Schwarz, 1978), with lower values indicative of better fitting models (McCutchen, 1987; Rose et al., 2007). We also reported the Lo-Mendell-Rubin (LMR; Lo, Mendell, & Rubin, 2001) test and Bootstrap Likelihood Ratio test (BLRT), which allows examining whether each model fits the data better than the previous model with k-1 profiles. Significant results indicate better fit for the model with an additional profile. Classification quality of competing models was assessed using entropy, which is an index that depicts the likelihood that participants are classified in the appropriate class (Magidson & Vermunt, 2002). Lastly, latent profile proportions were examined, as classes with less than 5% of the total sample may indicate data over-extraction (Berlin, Williams & Parra, 2014). Simulation studies have found that the BIC and BLRT are the most robust indices for identifying the correct number of latent classes (Nylund, Asparouhov, & Muthén, 2007).
Next, we examined the effect of the latent profile variable on a secondary auxiliary model that included both covariates and outcomes. Mean differences in theoretically relevant variables were examined as a function of profile membership. Wald chi-square tests (Asparohouv & Muthén, 2007; Wang, Brown, & Bandeen-Roche, 2005) demarcated mean differences across these outcomes after controlled for sex, race, college status, and income.
Results
Descriptive Statistics and Correlations Among Study Variables
See Table 1 for sample characteristics. Participants consumed an average of 17.06 (SD = 13.66) drinks per week in a typical month and reported 11.91 (SD = 9.31) past-month alcohol problems and 4.19 (SD = 4.75) binge drinking episodes. Participants reported an average of 1.93 (SD = 2.39) AUD symptoms, and 27.6% of the sample reported at least two AUD symptoms. Participants had an average weight of 82.03 kg (SD = 22.38) and an average BMI of 28.31 (SD = 7.20). Using established BMI cutoffs, 26.4% of the sample were overweight (BMI between 25 and 29.99) and 35.2% were obese (BMI 30 or greater). Participants reported an average of 1.59 (SD = 2.52) FA symptoms. We examined correlations between alcohol misuse variables and obesity-related factors. Typical drinks per week was significantly (p < .05) and positively correlated with weight (r = .10), visceral fat (r = .10), muscle mass (r = .17), and BMR (r = .17). Number of FA symptoms was positively correlated with alcohol problems (r = .25) and AUD (r = .24). Finally, alcohol problems were positively correlated with muscle mass (r = .09) and BMR (r = .09). Although statistically significant, the magnitude of these associations is small.
Table 1.
Descriptive Statistics
| Variable | M (SD) / % | Range |
|---|---|---|
| Age | 22.63 (1.03) | 21.5 – 24.99 |
| Sex (% women) | 57.3 | |
| Income | $30,000 – $45,000 | |
| Education | ||
| Less than Bachelor | 36.4 | |
| Currently receiving Bachelor’s | 25.6 | |
| Bachelor’s complete | 38.0 | |
| Intensity | 8.29 (5.71) | 2 – 35 |
| Omax | 22.17 (15.00) | 0 – 85 |
| Elasticity | .0044 (.0051) | .0004 – .0453 |
| r-ratio | .36 (.18) | .00 – 1.00 |
| UPPS – Negative Urgency | 9.28 (3.01) | 4 – 16 |
| UPPS – Lack of Perseverance | 6.28 (1.85) | 4 – 14 |
| UPPS – Lack of Premeditation | 6.76 (1.85) | 4 – 16 |
| UPPS – Sensation Seeking | 11.09 (2.84) | 4 – 16 |
| UPPS – Positive Urgency | 7.61 (2.66) | 4 – 16 |
| Delay Discounting | .0469 (.1105) | .0001 – .6000 |
| Reward Probability Factor | 36.40 (5.90) | 18 – 44 |
| Environmental Suppressors Factor | 23.83 (6.20) | 9 – 36 |
| Typical drinks per week | 17.06 (13.66) | 0 – 77 |
| Past Month Alcohol Problems | 11.91 (9.31) | 0 – 48 |
| Past Month Binge Drinking Occasions | 4.19 (4.75) | 0 – 22 |
| Alcohol Use Disorder Symptoms | 1.93 (2.39) | 0 – 11 |
| Food Addiction Symptom Count | 1.59 (2.52) | 0 – 11 |
| BMI | 28.31 (7.20) | 15.63 – 55.49 |
| Weight (kg) | 82.03 (22.38) | 40.50 – 162.00 |
| Percent Body Fat | 30.55 (12.50) | 6.30 – 77.00 |
| Visceral Fat | 5.93 (5.09) | 1.00 −28.00 |
| Muscle Mass | 52.29 (11.08) | 20.00 – 92.70 |
| BMR | 1711.14 (343.06) | 1119 – 3012 |
Note. M = Mean; SD = Standard Deviation; r-ratio = proportionate substance-related reinforcement; BMI = Body Mass Index; kg = kilograms; BMR = Basal Metabolic Rate
Latent Profile Characterization
Latent profile models, with 2 to 5 profiles, were extracted from the weight-related and alcohol-related variables. Models were estimated with profile variant means, and covariances were constrained to be equal across profiles as model fit was reduced when covariances were allowed to freely covary across profiles. Table 2 presents the class solutions, key fit indices, and conditional probabilities of the estimated models. Models did not converge beyond five classes. Selection of the optimal class solution relied on the LMR test and scree-plot inspection (Morin, Meyer, Creusier, & Biétry, 2016). The LMR test was significant through the three-profile model (p < .05), and then reached non-significance when the model was expanded to a four-profile solution. However, comparison of the plotted data suggests that three profiles are identical across the three-profile and four-profile solutions, with the inclusion of an additional small-sample higher-alcohol using profile in the four-profile solution. Thus, it was determined that the addition of a fourth profile provided additional meaningful information, therefore, the four-class solution was retained as the optimal model. We have provided the 3-class solution data in supplemental materials. The four-profile solution provided good classification certainty as reflected by entropy (0.95) and posterior probabilities for most likely class membership ranging from 0. 89 to 0.98.
Table 2.
Fit Statistics for One to Five Profile Solutions and Posterior Profile Probabilities
| Fit Statistics | 1 Profile | 2 Profile | 3 Profile | 4 Profile | 5 Profile |
|---|---|---|---|---|---|
| Log-likelihood | −4167.79 | −4802.90 | −4683.70 | −4605.73 | −4533.74 |
| BIC | 10136.20 | 9804.20 | 9617.01 | 9512.27 | 9419.50 |
| Sample-size Adjusted BIC | 10063.18 | 9705.21 | 9493.19 | 9363.06 | 9244.89 |
| Entropy | N/A | .95 | .96 | .95 | .95 |
| LMR test | N/A | 375.85 | 233.84 | 152.95 | 141.22 |
| LMR, p-value | N/A | <.001 | <.001 | .13 | .78 |
| Four-class model | 1 | 2 | 3 | 4 | |
| 1, n = 424, 70.4% | .980 | .008 | .000 | .005 | |
| 2, n = 93, 15.4% | .042 | .948 | .004 | .006 | |
| 3, n = 44, 7.3% | .004 | .014 | .981 | .000 | |
| 4, n = 41, 6.8% | .104 | .011 | .000 | .885 | |
Note. BIC = Bayesian Information Criterion; LMR = Lo-Mendell-Rubin.
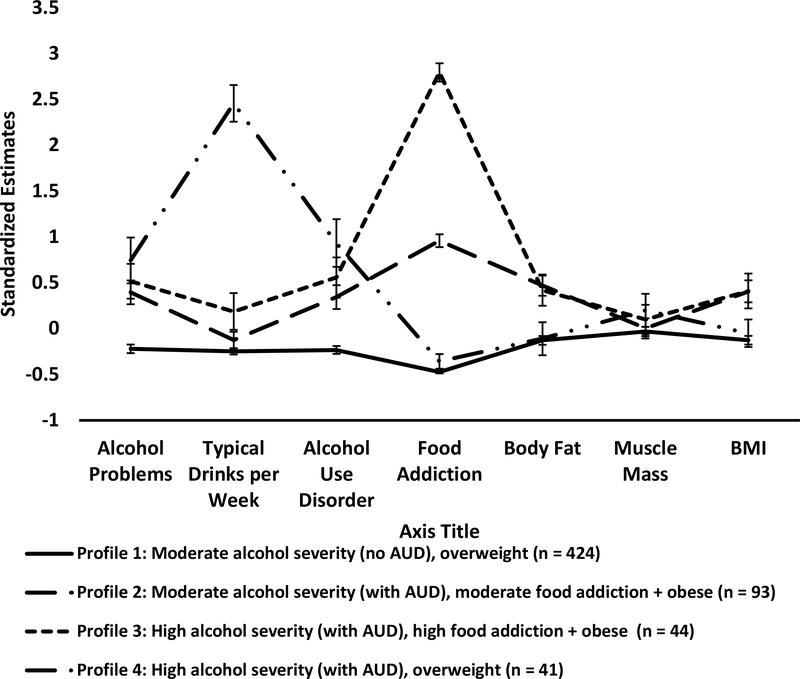
The final four-profile solution grouped participants in to a moderate alcohol severity (no AUD), overweight profile (Profile 1; n = 424, 70.4%), moderate alcohol severity (with AUD), moderate FA + obese profile (Profile 2; n = 93, 15.4%), high alcohol severity (with AUD), high FA + obese profile (Profile 3 n = 44, 7.3%), and high alcohol severity (with AUD), overweight (Profile 4 n = 41, 6.8%). Alcohol severity was classified using previously published cut offs (Read et al., 2015). Figure 1 depicts the standardized mean profiles of the four-profile solution, and unstandardized indicator means for each class can be found in Table 3.
Figure 1.
Empirically-derived latent profiles using alcohol misuse, food addiction, and body composition variables as indicators. Analyzes revealed a four class solution: Participants in Profile 2 (n = 96) demonstrated similar levels of alcohol use and muscle mass compared to Profile 1, but higher problematic use (alcohol problems and AUD symptoms), food addiction symptom count, and scores on body composition variables. Participants in Profile 3 (n = 96) demonstrated similar levels of alcohol use and muscle mass compared to Profiles 1 and 2, but higher problematic use (alcohol problems and AUD symptoms), food addiction symptom count, and scores on body composition variables, with the greatest difference occurring for the food addiction measure. Participants in Profile 1 (n = 462) demonstrated moderate alcohol misuse (moderate alcohol problems and typical drinks per week with an average AUD symptom count below the diagnostic criteria cutoff), an average food addiction symptom count below the diagnostic criteria cutoff, and moderate scores on body composition variables. Finally, those in Profile 4 demonstrated similar weight and food-related levels as those in Profile 1, similar AUD symptoms and alcohol problems as participants in Profile 2 and 3, but significantly higher levels of alcohol consumption compared to all other profiles. BMI = Body Mass Index
Table 3.
Means for Alcohol and Body Composition Indices for the four-class solution
| Variable | Profile 1 (n = 424) – Moderate Alcohol Severity (No AUD), overweight profile | Profile 2 (n = 93) – Moderate alcohol severity (with AUD), moderate food addiction + obese profile | Profile 3 (n = 44) – High alcohol severity (with AUD), High food addiction + obese profile | Profile 4 (n = 41) – High alcohol severity (with AUD), overweight |
|---|---|---|---|---|
| Demographics (M+SEM/Median) | ||||
| Age | 22.69 (0.05) | 22.66 (0.12) | 22.43 (0.16) | 22.47 (0.22) |
| Sex (% female) | 54.5% | 72.0% | 70.5% | 39.0% |
| Median Household Income | At least $30,000 but less than $45,000 | At least $30,000 but less than $45,000 | At least $30,000 but less than $45,000 | At least $30,000 but less than $45,000 |
| Race (% White/% Black) | 50.5%/39.2% | 37.6% / 50.5% | 27.3% / 52.3% | 53.7% / 34.1 |
| College Status (% College) | 67.9% | 64.5% | 45.5% | 51.2% |
|
Indicators | ||||
| Alcohol Problems | 9.74 (0.39) | 15.93 (1.13) | 16.74 (1.72) | 19.38 (1.6) |
| Drinks per Week | 13.30 (0.41) | 15.24 (1.13) | 19.77 (2.68) | 54.41 (1.89) |
| Alcohol Use Disorder Sxs | 1.33 (0.09) | 2.87 (0.28) | 3.26 (0.52) | 4.28 (0.46) |
| Food Addiction | 0.35 (0.03) | 4.15 (0.12) | 8.69 (0.2) | 0.67 (0.17) |
| Body Fat | 28.75 (0.6) | 36.74 (1.38) | 36 (2.03) | 29.55 (2.09) |
| Muscle Mass | 51.93 (0.56) | 52.47 (1.17) | 53.42 (1.74) | 54.48 (1.97) |
| BMI | 27.35 (0.34) | 31.48 (0.85) | 31.37 (1.29) | 28.09 (1.03) |
Note. BMI = Body Mass Index. College status refers to those enrolled or graduated from a 4-year University.
Profile Descriptions
Moderate alcohol severity (no AUD), overweight profile (Profile 1).
Participants in this profile demonstrated the lowest levels of alcohol problems, AUD symptoms, FA symptoms, body fat and BMI. However, levels of typical drinks per week and muscle mass were comparable to those in the other two profiles.
Moderate alcohol severity (with AUD), moderate FA + obese profile (Profile 2).
Participants in this profile demonstrated moderate levels of alcohol problems, AUD symptoms, food addiction symptoms, % body fat and BMI, to a degree that was higher than Profiles 1 but lower than 2. Levels of typical drinks per week and muscle mass were comparable to those in the other two profiles.
High alcohol severity (with AUD), high FA + obese profile (Profile 3).
Participants in this profile demonstrated high levels of alcohol problems, AUD symptoms, FA symptoms, percent body fat and BMI. The greatest increases were in the FA symptoms. However, levels of typical drinks per week and muscle mass were comparable to those in the other two profiles.
High alcohol severity (with AUD), overweight (Profile 4).
Participants in this profile demonstrated the highest levels of alcohol problems, AUD symptoms. However, levels of FA symptoms, percent body fat and BMI were comparable to those of Profile 1.
Table 3 also includes descriptive data for each class. Profile 2 and 3 were more likely to be female and Black. Those in Profile 3 were less likely to be enrolled in or have graduated from a 4-year university. Those in Profile 4 were more likely to be male and White. All four groups had similar median income levels.
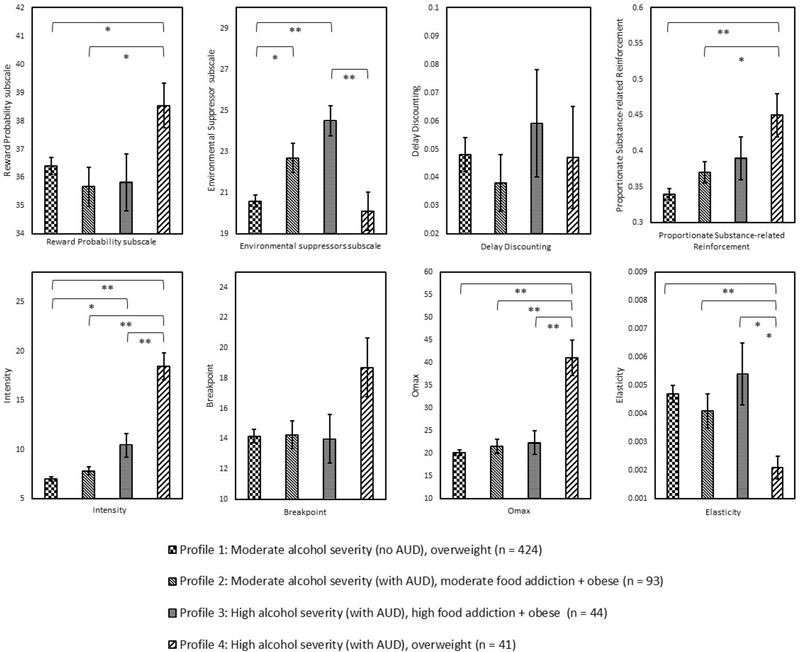
Differences in Reward, Impulsivity, and Alcohol Demand Variables Across Profiles
Significant differences in addiction-related risk factors were tested using Wald’s test (see Table 4 for means) using means adjusted for sex, race, college status, and income. Profile 4 demonstrated significantly greater scores on the reward probability subscale compared to those in Profile 2 (p = .008). There was a graded relationship between profile membership and mean levels of environmental reward deprivation, such that individuals in Profile 1 reported significantly lower levels of environmental reward deprivation compared to both Profile 2 (p = .008) and 3 (p < .001). Further, those in Profile 3 reported significantly higher environmental reward deprivation compared to those in Profile 4 (p < .001). Individuals in Profile 4 also demonstrated significantly higher alcohol demand intensity and Omax, and lower demand elasticity, compared to Profile 1, Profile 2, and Profile 3 (all p-values below .001 for intensity and Omax; p-values for elasticity Profile 4 comparison to Profile 1, 2, and 3 are <.001, .002, and .005 respectively). Intensity was also significantly lower for Profile 1 compared to Profile 3 (p < .001). Profile 4 also demonstrated significantly greater proportionate substance-related reinforcement compared to Profile 1 (p < 001) and Profile 2 (p = .004).
Table 4.
Means for Alcohol and Body Composition Indices for the four-class solution
| Variable | Profile 1 (n = 424) – Moderate Alcohol Severity (No AUD), overweight profile | Profile 2 (n = 93) – Moderate alcohol severity (with AUD), moderate food addiction + obese profile | Profile 3 (n = 44) – High alcohol severity (with AUD), High food addiction + obese profile | Profile 4 (n = 41) – High alcohol severity (with AUD), overweight |
|---|---|---|---|---|
| Reward Probability Scalec,e | 36.41 | 35.68 | 35.84 | 38.54 |
| Environmental Suppressor Scalea,b,f | 20.60 | 22.71 | 24.50 | 20.12 |
| Intensityb,c,e,f | 7.06 | 7.85 | 10.45 | 18.46 |
| Breakpoint | 14.16 | 14.25 | 13.98 | 18.71 |
| Omaxc,e,f | 20.25 | 21.57 | 22.43 | 41.08 |
| Elasticityc,e,f | 0.0047 | 0.0041 | 0.0054 | 0.0021 |
| Delay discounting | 0.048 | 0.038 | 0.059 | 0.047 |
| r-ratioc,e | 0.34 | 0.37 | 0.39 | 0.45 |
| UPPS – Neg Urga,b | 8.81 | 10.29 | 11.12 | 9.69 |
| UPPS - Lack of Perseverance | 6.27 | 6.23 | 6.65 | 6.1 |
| UPPS - Lack of Premeditationb | 6.57 | 6.82 | 7.65 | 7.49 |
| UPPS - Sensation Seeking | 11.11 | 10.76 | 10.84 | 11.96 |
| UPPS - Positive Urgencya,b | 7.24 | 8.2 | 9.04 | 8.48 |
Note. All significance tests use a p-value of .01.
= significant comparison between Profile 1 and 2
= significant comparison between profiles 1 and 3
= significant comparison between Profile 1 and 4
= significant comparison between profiles 2 and 3
= significant comparison between profiles 2 and 4
= significant comparison between profiles 3 and 4. r-ratio = proportionate substance-related reinforcement
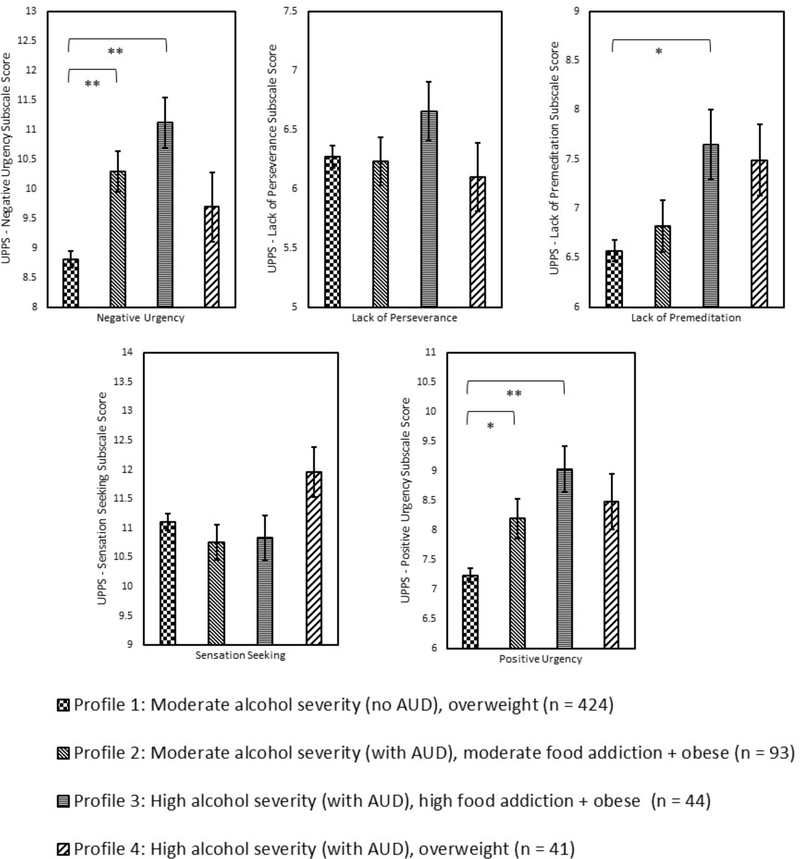
Those in Profile 1 demonstrated significantly lower negative urgency compared to those in Profile 2 (p < .001) and in Profile 3 (p < .001). Individuals in Profile 3 demonstrated significantly higher lack of premeditation compared to individuals in Profiles 1 (p < .001). Finally, those in Profile 3 demonstrated significantly lower positive urgency compared to those in Profile 1 (p < .001) and Profile 2 (p = .03). There were no statistically significant differences in delay discounting across the 4 profiles.
Discussion
The purpose of the current study was to 1) identify classes of emerging adult heavy drinkers by their patterns of alcohol use severity, FA, and BMI, and 2) determine whether these classes differed by behavioral economic and other related risk factors (e.g., reward availability, impulsivity, and alcohol demand). Our Latent Profile Analyses revealed four profiles: a moderate alcohol severity (no AUD), overweight profile (Profile 1); moderate alcohol severity (with AUD), moderate FA + obese profile (Profile 2); high alcohol severity (with AUD), high FA + obese profile (Profile 3); and high alcohol severity (with AUD), overweight (Profile 4). Overall, most of our participants’ patterns fell into the lowest risk profile. However, it is noteworthy that even Profile 1 participants had moderate alcohol problems just under the clinical threshold for a diagnosis of AUD. Participants in Profile 4 reported a mean of 54 drinks per week (range = 35–77) which was surprisingly high. Further, although Profiles 1 and 4 BMIs and body compositions were lower than Profiles 2 and 3, the mean BMI fell in the overweight range (Profile 1: M = 27.35, SD =0.34; Profile 4: M = 28.09, SD =1.03). Thus, all of the profiles had elevated health risk behaviors and anthropometric measures. This is likely due in part to the fact that this was a high-risk sample with respect to alcohol (all participants reported recent heavy episodic drinking) that was recruited from a community with a high prevalence of obesity.
These findings are consistent with previous variable-centered literature within college student samples that suggests a relation between heavy drinking and obesity-related factors such as maladaptive eating behaviors (Kelly-Weeder, 2011; Kelly-Weeder and Edwards, 2011; Martin et al., 2015; Pedrelli et al., 2011; Rush et al., 2016, 2009). Across our profiles of a more diverse (with respect to college status and race/ethnicity) emerging adult population, participants with higher levels of alcohol severity also tended to have higher levels of FA and body composition. Indeed, over 23% of our sample met criteria for AUD and participants in Profiles 2 and 3 had mean BMIs in the obese range. Although Profiles 1–3 were similar in terms of alcohol use, they differed in terms of BMI, FA, and AUD. This variation might be partially explained by the fact that food and alcohol are both sources of calorie and reward so if one values food over alcohol, that may result in a reduction of the rewarding value of alcohol (substitutes). On the other hand, given that there are shared risk factors for alcohol use and obesity (impulsivity, reward deprivation) one might also expect the behaviors to co-occur (complements). In terms of demographic differences, individuals in Profiles 2 and 3 were more likely to be female and Black, and those in Profile 3 were less likely to be enrolled in or have graduated from a 4-year university. Participants in Profile 4, the highest risk group in terms of AUD, were more likely to be male and white.
We found several differences in BE variables by profile group. Individuals in Profile 1 reported significantly lower levels of environmental reward deprivation compared to both Profile 2 (p = .008) and 3 (p < .001), and those in Profile 3 reported significantly higher environmental reward deprivation compared to those in Profile 4 (p < .001). However, Profile 4 did not differ from Profile 1. This suggests that environmental reward deprivation may be associated with maladaptive eating but not heavy drinking in our sample. Additionally, Profile 4 demonstrated significantly greater proportionate substance-related reinforcement compared to Profile 1 (p < 001) and Profile 2 (p = .004). These findings indicate that participants in the highest weight and alcohol severity groups were more likely to experience environmental reward deprivation. This finding is consistent with a robust laboratory and clinical/epidemiological literature linking high levels of environmental reward deprivation to alcohol and drug use (Acuff et al., 2019; Higgins et al., 2004; Tucker et al., 2009), including studies with emerging adults (Joyner et al., 2016). This finding is also generally consistent with previous research indicating that weight loss is more likely among individuals who reported greater levels of non-food related reinforcement (Buscemi et al., 2014). It is possible that high levels of environmental reward deprivation may partially explain differences in alcohol related consequences and AUD across profiles. Although the literature on environmental reward deprivation and alcohol use is robust (Acuff et al., 2019; Joyner et al., 2016; MacKillop, 2016), the literature on obesity and environmental reward deprivation is underdeveloped (Buscemi et al., 2014; Epstein et al., 2003). Future research should examine relations between environmental reward deprivation and FA and obesity among emerging adults, and future interventions for multiple health risk behaviors may consider targeting a reduction in environmental reward deprivation to reduce the severity of both alcohol use and obesity (Fazzino et al., 2019).
In addition to the profile differences in environmental reward deprivation, we found that individuals in Profile 1 demonstrated lower alcohol demand intensity (maximum consumption) compared to Profile 3 (p < .001). Intensity has been previously identified as a robust predictor of alcohol use problems in college samples (Murphy et al., 2015; Zvorsky et al., 2019). Our study extends these findings by identifying differences in intensity by integrated alcohol/obesity risk profiles. Profile 4 participants, who had the most AUD symptoms and self-reported alcohol-related problems, demonstrated significantly higher alcohol demand intensity and Omax, and lower demand elasticity compared to Profile 1, Profile 2, and Profile 3. Given that Profile 4 participants scored lower on the obesity-related variables, this profile allowed us to investigate how BE variables might differ in a group where obesity/eating behaviors were lower as compared to the other groups. Consistent with previous literature, we found that the highest alcohol risk profile also had the highest scores on BE risk factors for drinking. However, we might have expected to find more differences on BE-related factors between Profiles 1 and 3 given that Profile 3 also included participants with higher levels of consumption. This finding may suggest that BE indices play a more integral role for participants who drink heavily compared to more moderate drinking behavior and maladaptive eating. Future studies may further investigate the demand intensity of food in addition to alcohol to determine whether demand for food differs across groups of people with different levels of alcohol and obesity risk.
Finally, our profiles differed significantly by several impulsivity subscales. First, Profile 1 had significantly lower levels of negative urgency than Profiles 2 and 3. Negative urgency assesses how likely someone is to act urgently when feeling distressed (e.g., sample item, “When I feel bad, I will often do things I later regret in order to make myself feel better now”). Second, individuals in Profile 3, the most severe profile, demonstrated higher scores on lack of premeditation compared to individuals in Profile 1 and lower positive urgency compared to those in Profiles 1 and 2. The lack of premeditation and positive urgency findings were in the expected direction such that the higher risk profile had lower levels of planning and more risk behaviors when feeling positive emotions (respectively) than those in the lower risk profiles. Despite several differences in impulsivity across profiles, we did not find any differences in delay discounting across profiles. This finding is surprising, but it is consistent with some previous studies within similar emerging adult populations (Acuff et al., 2018; Dennhardt and Murphy, 2011). We did not find many differences between Profiles 3 and 4. This lack of findings may be due to the fact that Profile 3 was predominately female, and Profile 4 was predominately male, and we controlled for sex across our analyses. Our decision to control for sex was based on previously documented sex differences in drinking in the literature, but in this case, may have made it difficult for us to detect any differences between these two groups.
Our results should be interpreted within the context of our study limitations. First, we did not measure dietary intake, and our only dietary measure was one measuring FA. Future studies should consider assessing dietary intake via 24-hour dietary recalls to be able to measure specific eating behaviors and their relationship to FA, obesity, and alcohol use and problems. Second, our study was cross-sectional, so we are unable to identify the causal pathways linking reward, delay discounting, alcohol misuse, FA, and obesity. Additionally, to be eligible for this study, participants indicated recent heavy drinking episodes at screening. Although the high-risk sample is a strength in terms of understanding overlapping risk factors for elevated alcohol and food-related risk, it is possible the factors, and associations with risk factors, would be different in a general population sample of emerging adults. Further, we did not collect BE-related measures that were obesity specific or specific to maladaptive eating behaviors (e.g., food demand or food-free reward; Buscemi et al., 2014) or physical activity. Previous studies have measured delay discounting for food and food reward using validated measures (Epstein et al., 2010; Rasmussen et al., 2010). Such measures should be included in future studies investigating differences in these BE constructs across different health risk behavior profile groups. Finally, we acknowledge an important limitation to the literature that the term “food addiction” is problematic and stigmatizing. We used the term in this manuscript given that we were describing symptom counts on the YFAS which directly measures symptoms of “food addiction.” Thus, our mentioning of food addiction in our Profile labels corresponds directly to mean scores on that measure and does not indicate true “addiction.” Future research should consider a new term to describe maladaptive eating behavior that does not use the word “addiction.”
Despite its limitations, the current study was the first to identify profiles of low- to high-risk emerging adults based on alcohol- and obesity-related variables, and to examine theoretically informed “transdiagnostic” individual-level risk factors derived from the reinforcer pathology model (Bickel et al., 2014). Overall, Profile 4 participants had more risk factors across the board in terms of BE indices. In terms of environmental reward deprivation, individuals in Profile 1 reported significantly lower levels compared to both Profile 2 and 3, and those in Profile 3 reported significantly higher environmental reward deprivation compared to those in Profile 4. The fact that Profile 4 did not differ from Profile 1 may suggest that environmental reward deprivation may be primarily associated with maladaptive eating in our sample.
Our results are largely generalizable to higher risk community residing emerging adults from various socioeconomic and ethnic/racial minority groups. The co-occurrence of risking drinking and FA/obesity related factors in this sample is concerning and suggests that future intervention and prevention efforts consider targeting reward and impulsivity-related treatment mechanisms that confer risk for both of these health compromising behaviors.
Supplementary Material
Figure 2.
Difference in behavioral economic variables across the four empirically-derived latent profiles using alcohol misuse, food addiction, and body composition variables as indicators. Means and standard errors were calculated after controlling for sex, race, income, and college status.
Figure 3.
Difference in impulsivity variables across the four empirically-derived latent profiles using alcohol misuse, food addiction, and body composition variables as indicators. Means and standard errors were calculated after controlling for sex, race, income, and college status.
Acknowledgments
This work was supported by research grants from the National Institutes of Health (R01 AA020829, JM; 1F31AA027140-01A1, SFA). The funding source had no role other than financial support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health. Authors have no conflicts of interest to disclose.
References
- Acuff SF, Dennhardt AA, Correia CJ, Murphy JG (2019) Measurement of substance-free reinforcement in addiction: A systematic review. Clin Psychol Rev 70:79–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acuff SF, Murphy JG (2017) Further examination of the temporal stability of alcohol demand. Behav Processes 141:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acuff SF, Soltis KE, Dennhardt AA, Berlin KS, Murphy JG (2018) Evaluating behavioral economic models of heavy drinking among college students. Alcohol Clin Exp Res 42:1304–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) DSM-5, Diagnostic and statistical manual of mental disorders. Arlington, VA, American Psychiatric Publishing. [Google Scholar]
- Amlung MT, MacKillop J (2015) Further evidence of close correspondence for alcohol demand decision making for hypothetical and incentivized rewards. Behav Processes 113:187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahji A, Mazhar MN, Hudson CC, Nadkarni P, MacNeil BA, Hawken E (2019) Prevalence of substance use disorder comorbidity among individuals with eating disorders: A systematic review and meta-analysis. Psychiatry Res 273:58–66. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM (2011) The Behavioral Economics and Neuroeconomics of Reinforcer Pathologies : Implications for Etiology and Treatment of Addiction. Curr Psychiatr Reports 13:406–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG (2014) The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annu Rev Clin Psychol 10:641–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buscemi J, Murphy JG, Berlin KS, Raynor HA (2014) A behavioral economic analysis of changes in food-related and food-free reinforcement during weight loss treatment. J Consult Clin Psychol 82:659–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr KA, Epstein LH (2020) Choice is relative: Reinforcing value of food and activity in obesity treatment. Am Psychol 75:139–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho JP, Gawrysiak MJ, Hellmuth JC, McNulty JK, Magidson JF, Lejuez CW, Hopko DR (2011) The reward probability index: Design and validation of a scale measuring access to environmental reward. Behav Ther 42:249–262. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA (1985) Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psychol 53:189–200. [DOI] [PubMed] [Google Scholar]
- Crum RM, Helzer JE, Anthony JC (1993) Level of education and alcohol abuse and dependence in adulthood: A further inquiry. Am J Public Health 83:830–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, Karyadi KA (2014) Examination of a short version of the UPPS-P Impulsive Behavior Scale. Addict Behav 39:1372–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennhardt AA, Murphy JG (2011) Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychol Addict Behav 25:595–604. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Saelens BE (2000) Behavioral economics of obesity: Food intake and energy expenditure In: Reframing Health Behavior Change with Behavioral Economics (Bickel WK, Vuchinich RE eds), pp 293–311. Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Epstein LH, Salvy SJ, Carr KA, Dearing KK, Bickel WK (2010) Food reinforcement, delay discounting and obesity. Physiol Behav 100:438–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Stein JS, Paluch RA, MacKillop J, Bickel WK (2018) Binary components of food reinforcement: Amplitude and persistence. Appetite 120:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Truesdale R, Wojcik A, Paluch RA, Raynor HA (2003) Effects of deprivation on hedonics and reinforcing value of food. Physiol Behav 78:221–227. [DOI] [PubMed] [Google Scholar]
- Fazzino TL, Bjorlie K, Lejuez CW (2019) A systematic review of reinforcement-based interventions for substance use: Efficacy, mechanisms of action, and moderators of treatment effects. J Subst Abuse Treat 104:83–96. [DOI] [PubMed] [Google Scholar]
- Gearhardt AN, Corbin WR, Brownell KD (2016) Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav 30:113–121. [DOI] [PubMed] [Google Scholar]
- Hallgren KA, Greenfield BL, Ladd BO (2016) Psychometric properties of the adolescent reinforcement survey schedule-alcohol use version with college student drinkers. Subst Use Misuse 51:812–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Lussier JP (2004) Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol 55:431–461. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Smyth D (2017) Magnitude and Trends in Heavy Episodic Drinking, Alcohol-Impaired Driving, and Alcohol-Related Mortality and Overdose Hospitalizations Among Emerging Adults of College Ages 18 – 24 in the United States, 1998 – 2014. J Stud Alcohol Drugs 78:540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruby A, Manson JAE, Qi L, Malik VS, Rimm EB, Sun Q, Willett WC, Hu FB (2016) Determinants and consequences of obesity. Am J Public Health 106:1656–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennison KM (2004) The short-term effects and unintended long-term consequences of binge drinking in college: A 10-year follow-up study. Am J Drug Alcohol Abuse 30:659–684. [DOI] [PubMed] [Google Scholar]
- Joyner KJ, Pickover AM, Soltis KE, Dennhardt AA, Martens MP, Murphy JG (2016) Deficits in access to reward are associated with college student alcohol use disorder. Alcohol Clin Exp Res 40:2685–2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly-Weeder S (2011) Binge drinking and disordered eating in college students. J Am Acad Nurse Pract 23:33–41. [DOI] [PubMed] [Google Scholar]
- Kelly-Weeder S, Edwards E (2011) Co-occurring Binge Eating and Binge Drinking in College Women. J Nurse Pract 7:207–213. [Google Scholar]
- Koffarnus MN, Bickel WK (2014) A 5-trial adjusted delay discounting task: Accurate discount rates in less than 60 seconds. Exp Clin Psychopharmacol 22:222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Franck CT, Stein J, Bickel WK (2015) A modified exponential behavioral economic demand model to better describe consumption data. Exp Clin Psychopharmacol 23:504–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J (2016) The behavioral economics and neuroeconomics of alcohol use disorders. Alcohol Clin Exp Res 40:672–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JL, Groth G, Longo L, Rocha TL, Martens MP (2015) Disordered eating and alcohol use among college women: Associations with race and big five traits. Eat Behav 17:149–152. [DOI] [PubMed] [Google Scholar]
- Meshesha LZ, Soltis KE, Wise EA, Rohsenow DJ, Witkiewitz K, Murphy JG (2020) Pilot trial investigating a brief behavioral economic intervention as an adjunctive treatment for alcohol use disorder. J Subst Abuse Treat 113:108002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Correia CJ, Colby SM, Vuchinich RE (2005) Using behavioral theories of choice to predict drinking outcomes following a brief intervention. Exp Clin Psychopharmacol 13:93–101. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA (2016) The behavioral economics of young adult substance abuse. Prev Med (Baltim) 92:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Martens MP, Yurasek AM, Skidmore JR, MacKillop J, Mcdevitt-Murphy ME (2015) Behavioral economic predictors of brief alcohol intervention outcomes. J Counsulting Clin Psychol 83:1033–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J (2006) Relative reinforcing efficacy of alcohol among college student drinkers. Exp Clin Psychopharmacol 14:219–27. [DOI] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J, Skidmore JR, Pederson AA (2009) Reliability and validity of a demand curve measure of alcohol reinforcement. Exp Clin Psychopharmacol 17:396–404. [DOI] [PubMed] [Google Scholar]
- Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT (2009) Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years’ follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. BMJ 338:b349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, Li X, Freedman DS (2018) Prevalence of obesity among youths by household income and education level of head of household - United States 2011–2014. Morb Mortal Wkly Rep 67:186–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrelli P, Bitran S, Shyu I, Baer L, Guidi J, Tucker DD, Vitali M, Fava M, Zisook S, Farabaugh AH (2011) Compulsive alcohol use and other high-risk behaviors among college students. Am J Addict 20:14–20. [DOI] [PubMed] [Google Scholar]
- Prince MA, Read JP, Colder CR (2019) Trajectories of college alcohol involvement and their associations with later alcohol use disorder symptoms. Prev Sci 20:741–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen EB, Lawyer SR, Reilly W (2010) Percent body fat is related to delay and probability discounting for food in humans. Behav Processes 83:23–30. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Epstein LH (2003) The relative-reinforcing value of food under differing levels of food deprivation and restriction. Appetite 40:15–24. [DOI] [PubMed] [Google Scholar]
- Read JP, Haas AL, Radomski S, Wickham RE, Borish SE (2015) Identification of Hazardous Drinking With the Young Adult Alcohol Consequences Questionnaire: Relative Operating Characteristics as a Function of Gender. Psychol Assess 28:1276–1289. [DOI] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR (2006) Development and preliminary validation of the young adult alcohol consequences questionnaire. J Stud Alcohol 67:169–177. [DOI] [PubMed] [Google Scholar]
- Rush CC, Becker SJ, Curry JF (2009) Personality Factors and Styles Among College Students Who Binge Eat and Drink. Psychol Addict Behav 23:140–145. [DOI] [PubMed] [Google Scholar]
- Rush CC, Curry JF, Looney JG (2016) Alcohol expectancies and drinking behaviors among college students with disordered eating. J Am Coll Heal 64:195–204. [DOI] [PubMed] [Google Scholar]
- Saelens BE, Epstein LH (1996) Reinforcing value of food in obese and non-obese women. Appetite 27:41–50. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME, Schulenberg JE, Miech RA (2018) Monitoring the Future national survey results on drug use, 1975–2018: Volume II, College students and adults ages 19–60. Ann Arbor. [Google Scholar]
- Shell AG, Firmin MW (2017) Binge Eating Disorder and Substance Use Disorder: A Case for Food Addiction. Psychol Stud (Mysore) 62:370–376. [Google Scholar]
- Stein JS, Koffarnus MN, Snider SE, Quisenberry AJ, Bickel WK (2015) Identification and management of nonsystematic purchase task data: Toward best practice. Exp Clin Psychopharmacol 23:377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Legierski CM, Giacomelli AM, Salvy SJ, Epstein LH (2008) Overweight children find food more reinforcing and consume more energy than do nonoverweight children. Am J Clin Nutr 87:1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Roth DL, Vignolo MJ, Westfall AO (2009) A behavioral economic reward index predicts drinking resolutions: Moderation re-visited and compared with other outcomes 31:1713–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Baler RD (2014) Addiction science: Uncovering neurobiological complexity. Neuropharmacology 76 Part B:235–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuchinich RE, Tucker JA (1983) Behavioral theories of choice as a framework for studying drinking behavior. J Abnorm Psychol 92:408–416. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR (2001) The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Pers Individ Dif 30:669–689. [Google Scholar]
- Wilkerson AH, Hackman CL, Rush SE, Usdan SL, Smith CS (2017) “Drunkorexia”: Understanding eating and physical activity behaviors of weight conscious drinkers in a sample of college students. J Am Coll Heal 65:492–501. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Zheng J, Li S, Zhou T, Zhang P, Bin Li H (2016) Alcoholic beverage consumption and chronic diseases. Int J Environ Res Public Health 13:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvorsky I, Nighbor TD, Kurti AN, DeSarno M, Naudé G, Reed DD, Higgins ST (2019) Sensitivity of hypothetical purchase task indices when studying substance use: A systematic literature review. Prev Med (Baltim) 128:105789. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.