Abstract
Objective
To examine social, economic, and migratory influences on the health of racial and ethnic minority groups in Canada, with a special focus on Caribbean immigrants.
Methods
Combined annual cycles (2011–2016) of the Canadian Community Health Survey (CCHS) data totaling over 300,000 adult Canadian residents were aggregated. Descriptive statistics and multivariable logistic regression models were used to examine the prevalence and associated factors of (1) cardiovascular disease diagnosed by a healthcare professional, and (2) self-rated general health among racial and ethnic groups.
Results
Caribbeans in general, Black and other non-White Canadians had significantly higher odds (adjusted for age/sex) of reporting any cardiovascular disease compared with White Canadians. Only non-Caribbean Blacks had higher odds of self-rated fair or poor general health compared with White Canadians. Multivariate logistic regression models revealed that after controlling for social and demographic factors, immigration status and years since migration, Caribbean non-Blacks and Black Caribbeans were at higher odds of having a doctor-reported cardiovascular health condition compared with White Canadians. Caribbean non-Blacks also had higher odds of fair or poor self-rated health than White Canadians.
Conclusion
The results of this study highlight the need for additional investigations of other potential influences on physical health statuses, especially among migrants and those of African ancestry who might be more prone to adverse health outcomes.
Keywords: Social and economic factors, Race/ethnicity, Migration, Physical health
Résumé
Objectif
Examiner les influences socioéconomiques et migratoires sur la santé des minorités raciales et ethniques au Canada, en particulier les immigrants caribéens.
Méthode
Les données des cycles annuels combinés (2011-2016) de l’Enquête sur la santé dans les collectivités canadiennes (ESCC) totalisant plus de 300 000 résidents canadiens adultes ont été regroupées. Des statistiques descriptives et des modèles de régression logistique multivariée ont été utilisés pour examiner la prévalence et les facteurs connexes 1) des maladies cardiovasculaires diagnostiquées par un professionnel des soins de santé et 2) de la santé générale autoévaluée au sein de groupes raciaux et ethniques.
Résultats
Les Caribéens en général, les Noirs et les autres Canadiens non blancs présentaient une probabilité sensiblement plus élevée (ajustée selon l’âge et le sexe) de déclarer n’importe quelle maladie cardiovasculaire que les Canadiens blancs. Seuls les Noirs non caribéens présentaient une probabilité supérieure de faire état d’une santé générale autoévaluée passable ou mauvaise que les Canadiens blancs. Les modèles de régression logistique multivariée ont révélé qu’en tenant compte des facteurs sociodémographiques, du statut d’immigration et du nombre d’années depuis la migration, les Caribéens non noirs et les Caribéens noirs présentaient une probabilité plus élevée d’avoir un trouble de santé cardiovasculaire déclaré par un médecin que les Canadiens blancs. Les Caribéens non noirs présentaient aussi une probabilité plus élevée de faire état d’une santé autoévaluée passable ou mauvaise que les Canadiens blancs.
Conclusion
Les résultats de l’étude soulignent la nécessité de pousser la recherche sur les autres facteurs susceptibles d’influencer l’état de santé physique, surtout chez les migrants et les personnes d’origine africaine qui pourraient être plus sujets à des résultats sanitaires indésirables.
Mots-clés: Facteurs socioéconomiques, race/ethnicité, migration, santé physique
Introduction
Canada is a multiethnic nation gaining an international reputation for its diverse racial and ethnic group composition, high average standard of living, and universal healthcare (Banks 2017; Kobayashi et al. 2008; Raphael 2009). Despite continued efforts to promote multiculturalism and equality among individuals within the country, there are noted inequalities that may contribute to disparities in health outcomes (Ramraj et al. 2016; Veenstra and Patterson 2015). Among the populations in Canada vulnerable to these experiences are migrants, including those from the Caribbean region who are at risk for cardiovascular health problems (e.g., hypertension, heart disease, diabetes) and poor health conditions (Creatore et al. 2010; Chiu et al. 2010). The Caribbean population since the 1960s has increasingly expanded over the years, now representing one of the largest non-European ethnic groupings (Chiu et al. 2010). But like other racial and ethnic groups in Canada, their representation in health studies has been sparse. This study examined the influence of social, economic, and migratory factors among and between the health statuses of racial and ethnic groups in Canada.
Although not consistent, research reveals ethnocultural differences in health across social domains in Canada (Ramraj et al. 2016; Veenstra and Patterson 2015; Gushulak et al. 2011; Lindsay 2007). These differences are often driven by social, economic, and migratory factors (Kobayashi et al. 2008; Raphael 2009; Khan et al. 2011; Quan et al. 2013; Veenstra 2011; Newbold 2005). Structural theory suggests a duality approach that provides an understanding of how these factors can enable, while simultaneously restricting opportunities that may promote positive health behaviours. While recognizing that social influences can provide access to care, healthy diet, and other lifestyle choices, it also suggests that potential stressful factors, including unemployment, under-education, and discrimination within the social and economic structures can negatively affect the health of racial and ethnic minorities. The social determinants of health (SDOH) framework further asserts that macro-level factors such as socio-demographic factors and socio-economic status (SES) are linked to health, and access to health resources and health risks are shaped by factors such as age, gender, race, ethnicity, income, education, employment, housing, and other environmental factors (Newbold 2005; Hammond and Maddox 2019; Dawson et al. 2019). Individuals with advantageous attributes and greater access to resources are more likely to have better health outcomes (Hammond and Maddox 2019). By contrast, persons with disadvantaged status have greater exposure to stress and are linked to poor health status. In many instances, low-income and immigrant groups residing in racially segregated urban enclaves (e.g., poor air quality and waste disposal, high voltage electric grid exposures, etc.) are susceptible to poor health outcomes (Nazroo and Williams 2006).
Studies have generally recognized that health risks are linked to age, and increase over the life course (Quan et al. 2013). By and large, research across ethnocultural groups has found that the prevalence of cardiovascular and other chronic conditions tends to be higher in the older age group (Quan et al. 2013). While also recognizing the high prevalence of diabetes among recent younger immigrants, researchers found that by age 65, one third of men and women had diabetes in Canada (Creatore et al. 2010; Lindsay 2007). The few studies examining the health status of individuals of African and Caribbean descent in Canada has established a similar pattern and found that the risk for cardiovascular disease, diabetes, and self-perceived poor general health increases with age within this population (Quan et al. 2013; Galabuzi 2001).
Cross-cultural studies generally indicate the advantageous health standing of women in comparison with men, irrespective of their social status in society (Quan et al. 2013). Some researchers have argued that this may be partly due to a healthier diet, and better health-seeking behaviours and preventive screening measures (Veenstra and Patterson 2015; Quan et al. 2013; Veenstra 2011; Newbold 2005; Hammond and Maddox 2019; Dawson et al. 2019; Lofters et al. 2017). However, it has been noted that among some racial and ethnic groups, women might be predisposed to poorer health conditions due to greater exposure to stressors resulting from role strain and double jeopardy (race and gender status) situation, which might be associated with hypertension (Karlsen and Nazroo 2002). For other cardiovascular conditions such as diabetes, however, it has been found that the rates tend to be higher among men (Quan et al. 2013).
Research reveals that SES is a consistent contributor in shaping the health of individuals within populations, with those occupying the lower strata of the economic ladder generally at greater risk for poorer health outcomes (Creatore et al. 2010; Nazroo and Williams 2006; Macdonald and Kennedy 2004; Karlsen and Nazroo 2002; Mutambudzi 2017; Mattu 2002). There are multiple pathways through which socio-economic factors can affect the health of individuals. Lower income, for instance, can have immediate and direct effects because of the barriers of access to quality medical and healthcare professionals, supplementary support care facilities, the purchasing of prescription drugs, and adopting healthy behaviours (Newbold 2005). Even with a universal healthcare system in Canada, health disparities are becoming more apparent and may be at least partly attributable to the growing income inequality and increased poverty rates in the country (Karlsen and Nazroo 2002; Mutambudzi 2017). While poverty is thought to be less concentrated in Canada in comparison with other high-income nations such as the United States, it has generally been problematic for those living in large urban areas, placing individuals at greater risk for poor health dispositions (Lofters et al. 2010; Mattu 2002). Research has found that individuals living in the poorest 20% of neighbourhoods are more likely to die from just about every illness, including cancer, diabetes, heart disease, and respiratory diseases than those in better-off locations (Galabuzi 2001; Nuru-Jeter et al. 2018; Lynch et al. 2004). Studies further show that income inequality and poverty are associated with lower life expectancy (Mutambudzi 2017; Robert and House 2000; Dinca-Panaitescu et al. 2011; Dunn and Dyck 2000).
Immigrants and racial/ethnic minorities in Canada are likely to suffer from poor health conditions due to generally lower incomes (after arrival) and residence in poor core areas. Some scholars have noted that SES is more important in explaining health inequalities among racial/ethnic and immigrant groups in comparison with Whites (Veenstra and Patterson 2015; Lacey et al. 2019). Among immigrants, individuals with lower levels of education and those not in the labour force are more likely to be unhealthy (Branker 2017; Lindsay 2007). However, socio-economic circumstances might be compounded with their status in society which exposes them to stressful discriminatory practices, resulting in limited access to quality of care and resources, and in turn, influencing poorer health outcomes (Dinca-Panaitescu et al. 2011; Lacey et al. 2019; Wu et al. 2005; Bryant et al. 2011; Ezeh et al. 2017; Allen and Allen 2015; Wilkins et al. 1989).
This is demonstrated by a growing body of research revealing more advantaged health standings of immigrants immediately upon arrival, but progressively deteriorating with time within host countries (Creatore et al. 2010; Veenstra 2011; Robert and House 2000; Lacey et al. 2019; Ezeh et al. 2017; Allen and Allen 2015; Qi 2012). For example, since the time of arrival, the highest prevalence of diabetes was found for men and women living in Canada for 15 years or more compared with those living in Canada 5–9 years, with greater increases among individuals from the Caribbean and Sub-Saharan Africa (Creatore et al. 2010; Quan et al. 2013; Galabuzi 2001; Ezeh et al. 2017). In particular, one study found that immigrants either had better or similar health statuses compared with Canadian-born adults with respect to mental health, chronic conditions, and disability (Khan et al. 2011; Quan et al. 2013). First-generation immigrants were also more likely than their Canadian-born counterparts to report poorer health, but this association was dependent on their country of origin (Briggs 2018; De Maio and Kemp 2010; Gee et al. 2007). Thus, it is still unclear how specific racial/ethnic groups, such as those of Caribbean descent, fare in comparison with other racial and ethnic groups with respect to health outcomes in Canada.
This study explored physician-diagnosed cardiovascular disease (i.e., diabetes, heart disease, hypertension, stroke) and the self-rated fair or poor general health of racial and ethnic groups in Canada, with a focus on Caribbean immigrants. We further examine the contributions of social, economic, and years since migration on the health of racial and ethnic populations relative to the dominant group in order to ultimately develop preventive and intervention programs and approaches to assist those racial/ethnic groups who may be at risk for poorer health conditions than others.
Methods
Data
Data for this study are from the Canadian Community Health Survey (CCHS). Since 2008, CCHS data are released annually. This annual cycle survey collects data on the general health of participants 12 years or older living in private dwellings in provinces and territories, obtaining information on health determinants, disease status, and socio-demographic characteristics. Every 2 years, a file combining the 2 years’ sample is also released. The survey sample represents approximately 97–98% of the Canadian population aged 12 and over (Gee et al. 2007). Residents of Indian reserves, Crown lands, institutions, certain remote areas, and full-time members of the Canadian Armed Forces were excluded from the sampling frame. Data were collected using two computer-assisted interviewing applications, one for telephone interviews (CATI) and one for personal interviews (CAPI). In the most recent cycle, about 80% of interviews were conducted by CATI. Interviews were primarily conducted in the official languages (French and English) of Canada. Interpreters were available for participants who spoke other languages and were unable to communicate in either of the official languages (Gee et al. 2007; Siddiqi et al. 2017). For the purposes of this study, data on participants 18 years and older from three combined annual files (2011–2012, 2013–2014, 2015–2016) were used. Those three datasets were combined and analyzed to attain sample sizes large enough to yield reasonable estimates. Each cycle contributed approximately one third of the study participants. The original sampling weights were adjusted by a factor of three (because three cycles were combined) to represent the Canadian population (Ng et al. 2011). The combined estimates do not represent the population of any particular year; rather, they reflect the average Canadian household population across the 2011 to 2016 period (Statistics Canada 2009). The response rates for the combined cycles were 67% (2011–2012), 66% (2013–2014), and 60% (2015–2016), respectively. In total, the sample consisted of 305,958 participants: 1052 Caribbean Blacks, 1512 Caribbean non-Blacks, 3213 non-Caribbean Blacks, 23,564 other non-White Canadians including Indigenous and other visible minority people, and 276,617 White Canadians. Caribbean Blacks are defined as first-generation individuals of African descent who migrated from Caribbean countries (see countries listed in footnote to Table 1). Caribbean non-Blacks are non-Black individuals who migrated from Caribbean countries. Non-Caribbean Blacks are defined as individuals of African descent who did not migrate from Caribbean countries. Other non-White Canadians are defined as respondents who did not identify as Caribbean descendants but were considered either a visible minority or Indigenous peoples in the country. White Canadians are defined as those who self-identified as Caucasian and having European ancestral roots. Respondents who reported multiple racial/cultural origins (0.8% of the sample) were excluded from the analysis. The secondary data used for this study were collected by the Canadian government; ethics committee approval was not required. Statistics Canada’s protection of respondents is based on the Statistics Act and Privacy Act.
Table 1.
Sample characteristics
| Characteristics | Caribbean* Black (%) | Caribbean* non-Black (%) | Non-Caribbean Black (%) | Other non-White Canadians (%) | White Canadians (%) |
|---|---|---|---|---|---|
| Age (years) | 48.5 | 51.3 | 39.2 | 41.0 | 49.0 |
| Sex | |||||
| Men | 42.2 | 46.3 | 50.8 | 49.2 | 49.2 |
| Women | 57.8 | 53.7 | 49.2 | 50.8 | 50.8 |
| Education level | |||||
| Below high school | 14.5 | 12.7 | 8.4 | 8.4 | 13.7 |
| High school graduate | 17.6 | 21.3 | 20.9 | 19.0 | 21.0 |
| Post-secondary | 67.9 | 66.0 | 70.8 | 72.6 | 65.3 |
| Employment status | |||||
| Employed | 68.3 | 62.0 | 68.6 | 68.0 | 65.5 |
| Unemployed/not in labour force | 31.7 | 38.0 | 31.4 | 32.0 | 34.5 |
| Household income quintile | |||||
| Bottom quintile | 35.0 | 29.1 | 32.9 | 31.3 | 15.0 |
| Second quintile | 25.4 | 25.9 | 24.9 | 24.9 | 18.4 |
| Middle quintile | 20.2 | 19.1 | 19.3 | 18.2 | 20.9 |
| Fourth quintile | 11.4 | 14.7 | 14.0 | 14.2 | 22.0 |
| Highest quintile | 8.1 | 11.3 | 8.9 | 11.4 | 23.6 |
| Homeownership | |||||
| Yes | 54.5 | 61.9 | 59.4 | 64.5 | 76.1 |
| No | 45.5 | 38.1 | 40.6 | 35.5 | 23.9 |
| Years since migration† | |||||
| Born in Canada | 1.4 | 3.2 E | 27.0 | 21.9 | 88.2 |
| Up to 10 years | 18.7 | 17.1 | 28.7 | 30.9 | 1.8 |
| 11–20 years | 18.0 | 20.3 | 23.6 | 21.4 | 1.6 |
| More than 20 years | 63.4 | 62.7 | 20.7 | 25.8 | 8.4 |
| Region | |||||
| Atlantic | F | 0.8 E | 1.9 | 1.3 | 8.2 |
| Quebec | 28.9 | 13.6 | 10.6 | 13.5 | 26.2 |
| Ontario | 65.9 | 72.1 | 57.9 | 47.9 | 36.7 |
| Prairies | 3.2 | 9.0 | 16.5 | 15.9 | 17.7 |
| British Columbia | 1.8 | 4.4 | 13.0 | 21.4 | 11.9 |
| Territories | F | F | 0.1 E | 0.1 | 0.2 |
| Unweighted sample size | 1052 | 1512 | 3213 | 23,564 | 276,617 |
| Weighted N | 193,285 | 256,144 | 623,138 | 4,128,631 | 20,419,033 |
* Guyana, Anguilla, Antigua, Aruba, Bahamas, Barbados, Bermuda, Cuba, Dominica, Dominican Republic, Grenada, Guadeloupe, Haiti, Jamaica, Martinique, Netherlands Antilles, Puerto Rico, St. Kitts and Nevis, St. Lucia, St. Vincent and the Grenadines, Trinidad and Tobago, Virgin Islands
†Only among immigrants
E use with caution (CV between 16.6% and 33.3%)
F suppressed due to CV greater than 33.3%
Data source: Canadian Community Health Survey, 2011–2016
Measures
Socio-demographic indicators included age (in years), sex (men, women), household income quintile (bottom, second, middle, fourth, highest), employment status (employed, unemployed, not in the labour force), educational level (below high school, high school, post-secondary), homeownership (yes, no), and region (Atlantic, Quebec, Ontario, Prairies, British Columbia, Territories).
Migration years
Migration years represents the length of time since migration to Canada. For this study, these years were coded as follows: up to 10 years, 11 to 20 years, and above 20 years. Canadian-born respondents were assigned to a separate category, not any of the three migration year categories.
Cardiovascular disease
To measure cardiovascular disease, CCHS asked respondents about long-term conditions that had lasted or were expected to last 6 months or longer and had been diagnosed by a healthcare professional; these included diabetes, heart disease, hypertension, and stroke. Any cardiovascular disease is an additive combination of these conditions. Participants had to be diagnosed with at least one of the conditions listed to meet the criteria for any cardiovascular disease.
Self-rated general health
Self-rated general health reflects respondents’ evaluation of their overall health. They were asked, “In general, would you say your health is: excellent, very good, good, fair or poor?” For this analysis, we focused on fair or poor self-rated general health.
Analytic strategy
Descriptive statistics and multivariate logistic regression analytical procedures were conducted. Descriptive statistics presented included prevalence rates of cardiovascular conditions and fair and poor general health by race and ethnicity. Prevalence rates were also presented by age groups. In the initial analysis of logistic regressions, adjustments were made for age and sex. In the subsequent full model analyses (cardiovascular, fair/poor health), we conducted hierarchical modeling by entering relevant variables in different blocks. In block 1, we entered demographic variables (age, sex). In block 2, socio-economic variables (income, education) were added to the model. In block 3, immigration status and years since migration were included along with age and sex. In block 4, all variables were added to the model. We report odds ratio and confidence interval findings after the final entry. To account for the design effects of the survey, the bootstrap technique was used to calculate confidence intervals. A p value of less than 0.05 was used to determine statistical significance.
Results
Sample characteristics
The sample distributions reveal that Caribbean non-Blacks on average were older than the other ethnic groups with a mean age of 51.3 years (see Table 1). Across cohorts, women represented the majority; a higher proportion was found among Caribbean Blacks (58.6%). The educational level of participants within the sample was relatively high, with a majority of participants across cohorts having some post-secondary education. Other non-White Canadians had the highest proportion in this category (72.6%). Sampled participants were also generally employed. The proportion of employed non-Caribbean Blacks (68.6%) was higher than other racial and ethnic groups. However, a higher proportion (35.0%) of Caribbean Blacks was represented in the lowest income quintile category. Twenty-four (23.6%) percent of Whites were represented in the highest quintile category. White Canadians also showed the highest rate of homeownership (76.1%). A majority (88.2%) of White participants were born in Canada; racial/ethnic minorities tended to have resided in the country for more than 20 years. Most participants across racial/ethnic groups also resided in the most populous province of Ontario, although Caribbean non-Black respondents (72.1%) were more highly represented in this category.
Physician-diagnosed cardiovascular conditions by race and ethnicity
Table 2 presents prevalence rates and the adjusted (age and sex) odds ratios of cardiovascular conditions and fair or poor self-rated general health conditions by racial groups relative to White Canadians. In general, rates of fair or poor self-rated general health were higher among Caribbean non-Blacks (17.1%) compared with Whites (11.7%). This was the same for physician-diagnosed diabetes and hypertension, where higher proportions were found among Caribbean non-Blacks (16.4%). For any cardiovascular disease, prevalence rates were higher among Caribbean Blacks (32.6%) and non-Blacks (36.9%) relative to Whites (25.4%). Only in the case of heart disease (5.7%) was the rate higher among Canadian Whites compared to most of the other racial/ethnic groups.
Table 2.
Physician-diagnosed cardiovascular conditions and self-rated fair or poor general health by race/ethnicity
| Caribbean Black | Caribbean non-Black | Non-Caribbean Black | Other non-White Canadians | White Canadians | |
|---|---|---|---|---|---|
| Fair or poor health | |||||
| Percent | 13.5 | 17.1* | 9.0* | 9.5* | 11.7 |
| Age/sex standardized odds ratios | 1.24 | 1.49 | 1.06 | 1.04 | 1.00 |
| (95% CI) | (0.94–1.64) | (1.21–1.85)*** | (0.88–1.27) | (0.96–1.12) | |
| Any cardiovascular disease or diabetes | |||||
| Percent | 32.6* | 36.9* | 17.9* | 18.0* | 25.4 |
| Age/sex standardized odds ratios | 1.82 | 1.79 | 1.37 | 1.14 | 1.00 |
| (95% CI) | (1.43–2.31)*** | (1.49–2.15)*** | (1.17–1.60)*** | (1.07–1.22)*** | |
| Diagnosed diabetes | |||||
| Percent | 13.3* | 16.4* | 8.2 | 6.2* | 7.1 |
| Age/sex standardized odds ratios | 2.48 | 2.65 | 2.23 | 1.42 | 1.00 |
| (95% CI) | (1.74–3.54)*** | (2.10–3.33)*** | (1.81–2.74)*** | (1.30–1.55)*** | |
| Diagnosed heart disease | |||||
| Percent | 2.7* | 4.5 | 2.2* | 2.7* | 5.7 |
| Age/sex standardized odds ratios | 0.54 | 0.73 | 0.75 | 0.80 | 1.00 |
| (95% CI) | (0.33–0.88)* | (0.49–1.10) | (0.56–1.00)* | (0.70–0.91)* | |
| Diagnosed hypertension | |||||
| Percent | 28.8* | 28.9* | 13.4 | 13.2 | 19.9 |
| Age/sex standardized odds ratios | 2.10 | 1.65 | 1.28 | 1.12 | 1.00 |
| (95% CI) | (1.63–2.70)*** | (1.37–1.98)*** | (1.08–1.52)** | (1.04–1.20)** | |
| Diagnosed stroke | |||||
| Percent | F | F | F | 0.6* | 1.3 |
| Age/sex standardized odds ratios | 0.92 | 1.56 | 0.80 | 0.83 | 1.00 |
| (95% CI) | (0.34–2.48) | (0.62–3.90) | (0.36–1.75) | (0.65–1.06) | |
White Canadians is the reference category
*p < 0.05; ** p < 0.01; ***p < 0.001
F suppressed due to CV greater than 33.3%
Data source: Canadian Community Health Survey, 2011–2016
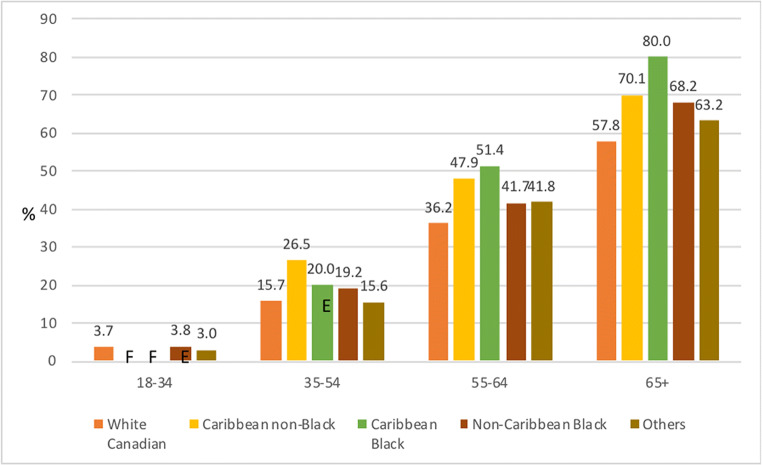
Any cardiovascular condition and self-rated general health of Canadians by age and race and ethnicity
With respect to any cardiovascular disease, prevalence rates increased with age for all groups (see Fig. 1). Even so, rates trended higher among Caribbeans within the older age categories in comparison with the other racial and ethnic groups. The highest rate was found among Caribbean Blacks (80.0%) and non-Caribbean Blacks (70.1%) in the oldest (65+) age group.
Fig. 1.
Any cardiovascular disease by race/ethnicity and age. Note: E use with caution (CV between 16.6% and 33.3%), F suppressed due to CV greater than 33.3%. Data source: Canadian Community Health Survey, 2011–2016
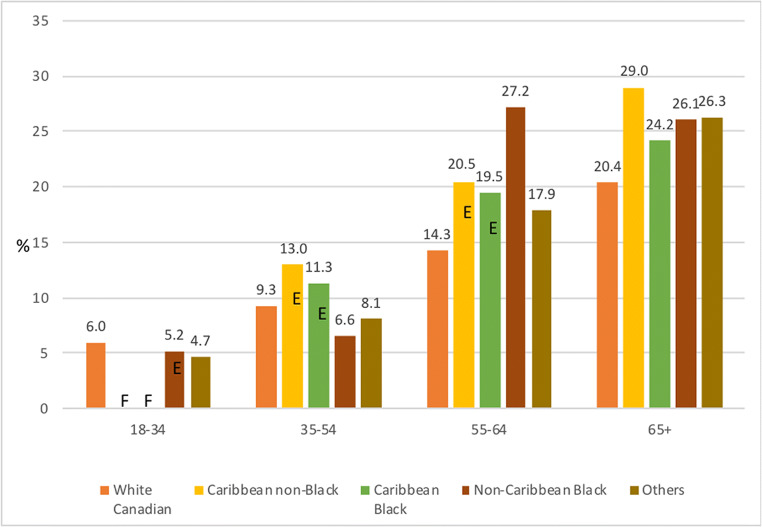
Figure 2 further reveals an increase with age in self-rated fair or poor general health by racial and ethnic characteristics. Within the oldest age group (65+), however, this was more apparent for Caribbean non-Blacks (29%).
Fig. 2.
Self-rated fair or poor general health by race/ethnicity and age. Note: E use with caution (CV between 16.6% and 33.3%), F suppressed due to CV greater than 33.3%. Data source: Canadian Community Health Survey, 2011–2016
Multivariate analysis examining social and economic factors and years of migration on any cardiovascular disease and self-rated fair or poor general health
Table 3 displays the results from the adjusted models on factors associated with any cardiovascular disease. The results indicated that after controlling for demographic factors such as age and sex, non-White groups were at higher odds than Whites of having any cardiovascular disease. In models where additional SES or immigrant variables were included, differences in odds of having any of cardiovascular conditions between Whites and each non-White group stayed significant. The final model, where demographic, socio-economic, and immigrant factors were taken into account, revealed that the odds for any cardiovascular disease significantly increased among Caribbean non-Blacks (AOR = 1.85, p < 0.001), Caribbean Black Canadians (1.82, p < 0.001), non-Caribbean Blacks (AOR = 1.43, p < 0.001), and Other non-White Canadians (AOR = 1.20, p < 0.001) relative to Whites.
Table 3.
Ethnic differences in any cardiovascular disease by social and economic factors and years of migration
| Caribbean Black | Caribbean non-Black | Non-Caribbean Black | Other non-White Canadians | White Canadians | |
|---|---|---|---|---|---|
| Model adjusted for | |||||
| Age and sex | 1.82 (1.43–2.31)*** | 1.79 (1.49–2.15)*** | 1.37 (1.17–1.60)*** | 1.14 (1.07–1.22)*** | 1.00 |
| + Income quintile, education level | 1.74 (1.37–2.20)*** | 1.75 (1.46–2.11)*** | 1.32 (1.13–1.53)*** | 1.01 (1.04–1.19)** | 1.00 |
| + Years of migration | 1.91 (1.50–2.43)*** | 1.89 (1.57–2.28)*** | 1.49 (1.26–1.75)*** | 1.23 (1.14–1.33)*** | 1.00 |
| All of the above | 1.82 (1.43–2.31)*** | 1.85 (1.53–2.24)*** | 1.43 (1.22–1.68)*** | 1.20 (1.12–1.30)*** | 1.00 |
To test the fitness of the models, Akaike information criterion (AIC) values for each model were obtained—the smaller values mean the better fit. It clearly indicates that model 2 and model 3 fit the data better than model 1 (smaller AIC values), and model 4 (full model) fits the data better than all previous models. Model 2 (age, sex + income, and education) fits the data better than model 3 (age, sex + years of migration)
White Canadians is the reference category
*p < 0.05; **p < 0.01; ***p < 0.001
Data source: Canadian Community Health Survey, 2011–2016
Table 4 shows the odds of reporting self-rated fair or poor general health among racial and ethnic groups in Canada. After controlling for demographic factors (age and sex), the odds of reporting fair or poor health were higher among Caribbean non-Blacks compared with White Canadians. Regression models including SES, immigration status, or years since immigration showed consistent results: higher odds among Caribbean non-Blacks. Other groups in this analysis did not show significant differences from Whites. The final model indicates Caribbean non-Blacks had 1.4 times higher odds than Whites to report self-rated fair or poor general health (AOR = 1.40, p < 0.01).
Table 4.
Ethnic differences in self-reported fair or poor general health by social and economic factors and years of migration
| Caribbean Black | Caribbean non-Black | Non-Caribbean Black | Other non-White Canadians | White Canadians | |
|---|---|---|---|---|---|
| Model adjusted for | |||||
| Age and sex | 1.24 (0.94–1.64) | 1.49 (1.21–1.85)*** | 1.06 (0.88–1.27) | 1.04 (0.96–1.12) | 1.00 |
| + Income quintile, education level | 1.03 (0.77–1.38) | 1.34 (1.06–1.69)* | 0.89 (0.73–1.07) | 0.90 (0.83–0.97)** | 1.00 |
| + Years of migration | 1.27 (0.95–1.69) | 1.54 (1.24–1.91)*** | 1.15 (0.95–1.40) | 1.13 (1.04–1.23)** | 1.00 |
| All of the above | 1.07 (0.79–1.45) | 1.40 (1.10–1.78)** | 1.00 (0.82–1.22) | 1.02 (0.93–1.11) | 1.00 |
To test the fitness of the models, Akaike information criterion (AIC) values for each model were obtained—the smaller values mean the better fit. It clearly indicates that model 2 and model 3 fit the data better than model 1 (smaller AIC values), and model 4 (full model) fits the data better than all previous models. Model 2 (age, sex + income, and education) fits the data better than model 3 (age, sex + years of migration)
White Canadians is the reference category
*p < 0.05; **p < 0.01; ***p < 0.001
Data source: Canadian Community Health Survey, 2011–2016
Discussion
This study used national Canadian data aggregated over several years to explore rates and contributing influences of physician-diagnosed cardiovascular disease and the self-rated fair or poor general health among specific racial and ethnic groups in Canada. Except for heart disease, prevalence rates tended to be higher among Caribbean descendants in Canada compared with their White counterparts. Specifically, Caribbean non-Black and Caribbean Black participants had higher rates of any overall cardiovascular disease, diabetes, and hypertension in comparison with White Canadians. Higher prevalence rates of self-rated fair or poor general health were also found among Caribbean non-Black Canadians compared with their White counterparts.
Semi-adjusted (age and sex) multivariate analysis further revealed higher odds of self-rated fair or poor general health among Caribbean non-Blacks relative to White Canadians. In a similar model, there were higher odds of any cardiovascular disease for all racial and ethnic minority groups compared with White Canadians. It is possible that post-migration challenges, including integration, cultural barriers, and limited access to services promoting positive health outcomes, can both directly and indirectly affect well-being and increase health risks (Lacey et al. 2019; Wilkins et al. 1989; Briggs 2018; Siddiqi et al. 2017; Ng et al. 2011; Lacey et al. 2015). Along with these challenges, it is commonly known that some immigrant and minority groups have lower rates of physician visits and health screening, which may serve as preventive measures for early-onset and treatment of chronic and poor health conditions.
Moreover, the possibility that barriers facing racial/ethnic groups, and immigrants, such as language and cultural barriers, fear of westernized medicine and doctors, and the lack of knowledge about seeking help for unmet health needs could have contributed to the poorer health standing among this group. This too could be a result of the generally high rate of cardiovascular disease among Caribbeans and other immigrant groups (Lynch and Kaplan 2000; Briggs 2018). Overall, this study showed that cardiovascular conditions and self-rated fair or poor general health increased with age but more so among immigrants and racial minorities, which has been supported by the literature (Lofters et al. 2017; Lynch and Kaplan 2000; Briggs 2018; Vang et al. 2015).
The fully adjusted multivariate models revealed increasing odds for any cardiovascular diseases among racial and ethnic minorities relative to Whites, with greater odds among Caribbean participants. At each step of the regression analysis, after controlling for social, economic, and immigration factors, non-White groups were found to have higher odds of cardiovascular disease compared with White Canadians. However, the effects seemed to be greater for Caribbean descendants (both Black and non-Black). While these results support the idea that membership in racial and ethnic minorities remains an important factor of health disposition, the result may also suggest potential structural and environmental influences that might affect the health outcomes of racialized groups. Some racial and ethnic and migrant groups may encounter additional stressors including underemployment and discrimination with years passed in host countries that might contribute to cardiovascular (health and chronic) conditions. The increased odds among Caribbean Blacks also signal that the health status of both non-Caribbean Black and Black Caribbeans in Canada may be influenced by both ethnicity and race.
A slightly different pattern was found concerning self-rated health. Caribbean non-Black Canadians were at higher odds to rate their health as fair or poor relative to Whites. No other minority groups showed differences in comparison with Whites when other confounding factors were considered. This finding among Caribbean non-Blacks may be attributed to the effect of perceptions of health which their vulnerable socio-economic standing and required adjustment to a new environment may impose. These relationships were found at certain stages of the analysis for other non-Whites but attenuated when all variables were considered.
Limitations and strengths
There were a number of weaknesses to this study that should be noted. First, while we explored the health of various groups in Canada, other racial and ethnic groups (e.g., Asian) were not highlighted or were lumped into one category that may mask other important differences that exist within this and other ethnic populations. Our focus was on racial and ethnic groups (Caribbean descendants, Blacks) that have been underexplored in research within Canada. Second, though we previously mentioned potential influences on health inequities among racial/ethnic groups, such as discrimination, these could not be included in the analysis due to data limitations. Third, cross-sectional data were used in this study, limiting the explanation of potential causal influences on health statuses. Though this analysis relied on the information of years since migration to measure the effects of respondents’ immigration experiences, future studies based on longitudinal information would provide a more meaningful assessment. This would allow for examining real changes in health (e.g., incidence of chronic conditions) as well as the changes in socio-economic status of immigrants over the course of their lives since immigration. Fourth, the study partly focused on physician-diagnosed conditions. Due to generally low rates of physician visits among immigrant and ethnic groups, the findings from this study may be under-estimated or may not adequately represent the health outcomes of the study populations. Finally, sample size issues among specific racial and ethnic groups prevented us from detecting meaningful relationships that may exist.
This study nonetheless provides important information on health differences in Canada by racial/ethnic groups that have gone largely underexplored. Notably, this is one of the first known studies to explore within racial and ethnic group health differences among individuals residing in Canada, particularly Blacks and Caribbean migrant populations that have been especially understudied. This study further permitted the examination of health differences between racial and ethnic groups within a specific population. Likewise, the study used population-based national data in the examination of rates and contributing factors to differential health outcomes among racial and ethnic groups. This is one of very few studies that take a national approach to understanding the health disposition of Caribbean and African descendants, where studies tend to be more regionally oriented.
Conclusion
Benefits aside, it is clear that additional research is necessary to explore other factors that may influence or explain health differences among groups despite the country’s universal healthcare. Although there are arguments surrounding the expanding income inequality, empirical examination of these circumstances is warranted among immigrant groups and individuals of African descent who may be at continuing risk for adverse health outcomes (Dunn and Dyck 2000; Briggs 2018; De Maio and Kemp 2010; Gee et al. 2007; Siddiqi et al. 2017; Ng et al. 2011; Lacey et al. 2015). More racial/ethnic group comparative research is necessary to better understand these continuing health differences (Veenstra and Patterson 2015). Additionally, given the persistent and suggested pervasive nature of racial inequality in the country, future empirical studies are necessary that include perceived and experienced racial/ethnic discrimination as sources of stress that can affect the health dispositions of Canadians (Veenstra and Patterson 2015; Ramraj et al. 2016; Gee et al. 2007; Siddiqi et al. 2017; Ng et al. 2011; Lacey et al. 2015; Vang et al. 2015; Rotermann 2011; Statistics Canada 2009; Williams and Sternthal 2010; Williams and Mohammed 2009; Thomas and Wannell 2009; Creatore et al. 2020). Finally, it might be instructive to revisit the use and meaning of self-rated indicators as valid assessments of individuals’ health status, given the differences found between this measure and the physician-diagnosed measures among some racial/ethnic groups. Despite its utility in highlighting the health of individuals, as evidenced in this study, perception is not always reality, especially when it comes to some immigrant groups.
Acknowledgements
We thank Ms. Yvette Blackburn and Ms. Raquelle Forrester for their helpful editorial comments. We would also like to pay tribute to James S. Jackson, the senior author and mentor on this project, who passed away at the completion of this manuscript.
Authors’ contributions
K.K. Lacey was the lead author on this project. J. Park conducted the analyses. K.K. Lacey, A.Q. Briggs, J. Park, and J.S. Jackson all contributed to the conceptualization, interpretation of findings, and the writing of this research manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Human participation protection
Secondary data collected by the Canadian government were used for this study; ethics committee approval was not required. Statistics Canada’s protection of respondents is based on the Statistics Act and Privacy Act.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Allen J, Allen M. Health inequalities and the role of the physical and social environment. In: Barton H, Thompson S, Burgess S, Grant M, editors. The Routledge Handbook of Planning for Health and Well-Being. New York: Routledge; 2015. pp. 123–141. [Google Scholar]
- Banks JA. Citizenship education and global migration: Implications for theory, research, and teaching. Washington, DC: American Educational Research Association; 2017. [Google Scholar]
- Branker RR. Labour market discrimination: The lived experiences of English-speaking Caribbean immigrants in Toronto. Journal of International Migration and Integration. 2017;8(1):203–222. doi: 10.1007/s12134-016-0469-x. [DOI] [Google Scholar]
- Briggs AQ. Second generation Caribbean black male youths discuss obstacles to educational and employment opportunities: A critical race counter-narrative analysis. Journal of Youth Studies. 2018;21(4):533–549. doi: 10.1080/13676261.2017.1394997. [DOI] [Google Scholar]
- Bryant T, Raphael D, Schrecker T, Labonte R. Canada: A land of missed opportunity for addressing the social determinants of health. Health Policy. 2011;101(1):44–58. doi: 10.1016/j.healthpol.2010.08.022. [DOI] [PubMed] [Google Scholar]
- Chiu M, Austin PC, Manuel DG, Tu JV. Comparison of cardiovascular risk profiles among ethnic groups using population health surveys between 1996 and 2007. Canadian Medical Association Journal. 2010;182(8):E301–E310. doi: 10.1503/cmaj.091676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creatore MI, Moineddin R, Booth G, Doug MH, DesMeules M, McDermott S, et al. Age-and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. Canadian Medical Association Journal. 2010;182(8):781–789. doi: 10.1503/cmaj.091551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creatore MI, Booth GL, Manuel DG, Moineddin R, Glazier RH. A population-based study of diabetes incidence by ethnicity and age: Support for the development of ethnic-specific screening and prevention strategies. Canadian Journal of Diabetes. 2020;44(5):394–400. doi: 10.1016/j.jcjd.2019.12.001. [DOI] [PubMed] [Google Scholar]
- Dawson AZ, Rebekah JW, Gregory C, Egede LE. Relationship between social determinants of health and systolic blood pressure in United States immigrants. International Journal of Cardiology Hypertension. 2019;2:100011. doi: 10.1016/j.ijchy.2019.100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Maio F, Kemp E. The deterioration of health status among immigrants to Canada. Global Public Health. 2010;5(5):462–478. doi: 10.1080/17441690902942480. [DOI] [PubMed] [Google Scholar]
- Dinca-Panaitescu S, Dinca M, Bryant T, Daiski I, Pilkington B, Raphael D. Diabetes prevalence and income: Results of the Canadian Community Health Survey. Health Policy. 2011;99(2):116–123. doi: 10.1016/j.healthpol.2010.07.018. [DOI] [PubMed] [Google Scholar]
- Dunn JR, Dyck I. Social determinants of health in Canada’s immigrant population: Results from the National Population Health Survey. Social Science & Medicine. 2000;51(11):1573–1593. doi: 10.1016/s0277-9536(00)00053-8. [DOI] [PubMed] [Google Scholar]
- Ezeh A, Oyebode O, Satterthwaite D, Chen YF, Ndugwa R, Sartori J, et al. The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet. 2017;389(10068):547–558. doi: 10.1016/S0140-6736(16)31650-6. [DOI] [PubMed] [Google Scholar]
- Galabuzi, G. E. (2001). Canada’s creeping economic apartheid: The economic segregation and social marginalisation of racialised groups. Toronto: Centre for Social Justice Foundation for Research and Education.
- Gee EM, Kobayashi KM, Prus S. Ethnic inequality in Canada: Economic and health dimension—Wellesley Institution. Hamilton: Program for Research on the Social and Economic Dimensions of an Aging Population (SEDAP); 2007. [Google Scholar]
- Gushulak BD, Pottie K, Roberts JH, Torres S, DesMeules M. Migration and health in Canada: Health in the global village. Canadian Medical Association Journal. 2011;183:E952–E9588. doi: 10.1503/cmaj.090287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond G, Maddox KEJ. A theoretical framework for clinical implementation of social determinants of health. JAMA Cardiology. 2019;4(12):1189–1190. doi: 10.1001/jamacardio.2019.3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. American Journal of Public Health. 2002;92(4):624–631. doi: 10.2105/AJPH.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan NA, Wang H, Anand S, Jin Y, Campbell NRC, Pilote L, Quan H. Ethnicity and sex affect diabetes incidence and outcomes. Diabetes Care. 2011;34(1):96–101. doi: 10.2337/dc10-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi K, Prus S, Lin Z. Ethnic differences in self-rated and functional health: Does immigrant status matter? Ethnicity and Health. 2008;13(2):129–147. doi: 10.1080/13557850701830299. [DOI] [PubMed] [Google Scholar]
- Lacey KK, Sears KP, Govia IO, Forsythe-Brown I, Matusko, & N., Jackson, J.S. Substance use, mental disorders and physical health of Caribbeans at-home compared to those residing in the United States. International Journal of Environmental Research and Public Health. 2015;12(1):710–734. doi: 10.3390/ijerph120100710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacey, K. K., Park, J., Briggs, A. Q., & James, J. S. (2019). National origins, social context, timing of migration and the physical and mental health of Caribbeans living in and outside of Canada. Ethnicity & Health, 1–24. 10.1080/13557858.2019.1634183. [DOI] [PMC free article] [PubMed]
- Lindsay, C. (2007). The Caribbean community in Canada: Profiles of ethnic communities in Canada. Statistics Canada, 2001 Census of Canada. https://www150.statcan.gc.ca/n1/pub/89-621-x/89-621-x2007007-eng.htm. Accessed 16 November 2020
- Lofters AK, Hwang SW, Moineddin R, Glazier RH. Cervical cancer screening among urban immigrants by region of origin: A population-based cohort study. Preventive Medicine. 2010;51(6):509–516. doi: 10.1016/j.ypmed.2010.09.014. [DOI] [PubMed] [Google Scholar]
- Lofters AK, Schuler A, Slater M, Baxter NN, Persaud N, Pinto AD, et al. Using self-reported data on the social determinants of health in primary care to identify cancer screening disparities: Opportunities and challenges. BMC Family Practice. 2017;18:31. doi: 10.1186/s12875-017-0599-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- Lynch J, Smith GD, Harper SA, Hillemeier M, Ross N, Kaplan GA, et al. Is income inequality a determinant of population health? Part 1. A systematic review. The Milbank Quarterly. 2004;82(1):5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald JT, Kennedy S. Insights into the healthy immigrant effect: Health service use of immigrants to Canada. Social Science & Medicine. 2004;59:1613–1627. doi: 10.1016/j.socscimed.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Mattu P. A survey on the extent of substandard housing problems faced by immigrants and refugees in the Lower Mainland of British Columbia. Vancouver: Mosaic Publishers; 2002. [Google Scholar]
- Mutambudzi M. Association between workplace psychosocial factors and mental health in Black, Hispanic, and White women: Cross-sectional findings from the National Health Interview Survey. Women & Health. 2017;57(10):1129–1144. doi: 10.1080/03630242.2016.1263273. [DOI] [PubMed] [Google Scholar]
- Nazroo JY, Williams DR. The social determinant of ethnic/racial inequalities in health. In: Marmot M, Wilkinson RG, editors. Social determinants of health. 2. Oxford: Oxford University Press; 2006. [Google Scholar]
- Newbold KB. Self-rated health within the Canadian immigrant population: Risk and the healthy immigrant effect. Social Science & Medicine. 2005;60(6):1359–1370. doi: 10.1016/j.socscimed.2004.06.048. [DOI] [PubMed] [Google Scholar]
- Ng E, Pottie K, Spitzer D. Official language proficiency and self-reported health among immigrants to Canada. Health Reports. 2011;22(4):15–23. [PubMed] [Google Scholar]
- Nuru-Jeter AM, Michaels EK, Thomas MD, Reeves AN, Thorpe RJ, Jr, LaVeist TA. Relative roles of race versus socioeconomic position in studies of health inequalities: A matter of interpretation. Annual Review of Public Health. 2018;39:169–188. doi: 10.1146/annurev-publhealth-040617-014230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi Y. The impact of income inequality on self-rated general health: Evidence from a cross-national study. Research in Social Stratification and Mobility. 2012;30(4):451–471. doi: 10.1016/j.rssm.2012.07.002. [DOI] [Google Scholar]
- Quan H, Chen G, Walker RL, Wielgosz A, Dai S, Tu K, et al. Incidence, cardiovascular complications and mortality of hypertension by sex and ethnicity. Heart. 2013;99:715–721. doi: 10.1136/heartjnl-2013-303748. [DOI] [PubMed] [Google Scholar]
- Ramraj C, Shahidi FV, Darity W, Jr, Kawachi I, Zuberi D, Siddiqi A. Equally inequitable? A cross-national comparative study of racial health inequalities in the United States and Canada. Social Science & Medicine. 2016;161:19–26. doi: 10.1016/j.socscimed.2016.05.028. [DOI] [PubMed] [Google Scholar]
- Raphael, D. (2009). The social determinants of health: An overview of key issues and themes. In D. Raphael (Ed.), The social determinants of health: Canadian perspectives (2nd ed.). Toronto: Canadian Scholars Press Incorporated.
- Robert SA, House JS. Socioeconomic inequalities in health: An enduring sociological problem. In: Bird CE, Conrad P, Fremont AM, editors. Handbook of Medical Sociology. Upper Saddle River: Prentice Hall; 2000. [Google Scholar]
- Rotermann M. The impact of considering birthplace in analyses of immigrant health. Health Reports. 2011;22(4):37–43. [PubMed] [Google Scholar]
- Siddiqi A, Shahidi FV, Ramraj C, Williams DR. Association between race, discrimination and risk for chronic disease in a population-based sample from Canada. Social Science & Medicine. 2017;194:135–141. doi: 10.1016/j.socscimed.2017.10.009. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2009). Canadian Community Health Survey (CCHS) - Annual Component User Guide, 2009 Microdata Files. Retrieved from: https://www23.statcan.gc.ca/imdb-bmdi/pub/document/3226_D7_T9_V8-eng.pdf. Accessed 16 November 2020.
- Thomas S, Wannell B. Combining cycles of the Canadian Community Health Survey. Health Reports. 2009;20(1):53–58. [PubMed] [Google Scholar]
- Vang, Z., Sigouin, J., Flenon, A., Gagnon, A. (2015). The healthy immigrant effect in Canada: A systematic review. Population Change and Lifecourse Strategic Knowledge Cluster Discussion Paper Series/ Un Réseau stratégique de connaissances Changements de population et parcours de vie Document de travail, 3(1), 4.
- Veenstra, G. (2011). Race, gender, class, and sexual orientation: Intersecting axes of inequality and self-rated health in Canada. International Journal for Equity in Health, 10(3). 10.1186/1475-9276-10-3. [DOI] [PMC free article] [PubMed]
- Veenstra G, Patterson C. Health differences between Black and White Canadians: Revisiting Lebrun and LaVeist. Canadian Ethnic Studies. 2015;47(3):163–176. doi: 10.1353/ces.2015.0027. [DOI] [Google Scholar]
- Wilkins R, Adams O, Brancker A. Changes in mortality by income in urban Canada from 1971 to 1986. Health Reports. 1989;1(2):137–174. [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;2:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: Sociological contributions. Journal of Health and Social Behavior. 2010;51(S):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Penning MJ, Schimmele CM. Immigrant status and unmet health care needs. Canadian Journal of Public Health. 2005;95(6):369–373. doi: 10.1007/BF03404035. [DOI] [PMC free article] [PubMed] [Google Scholar]