Abstract
Objective:
This study estimated the percentage of age 35 and 55 adults reporting using medical marijuana intended for someone else (diverted use) and compared demographics and health status of such users with respondents reporting recommended use (i.e., individuals with a medical marijuana recommendation for their own health conditions) and to respondents using marijuana not intended for medical use (nonmedical marijuana [NMM] use).
Method:
Cross-sectional analyses were conducted using complex sample survey data collected from 2013 to 2018 from 12,138 adults (6,998 women) at modal ages 35 or 55 participating in the U.S. national Monitoring the Future study.
Results:
Diverted use was reported by 72.9% [95% CI, 66.4, 79.4] and 64.3% [56.0, 72.7] of age 35 and 55 past-12-month medical marijuana users, respectively. Age 35 diverted users were more likely than recommended users to not work full time and have no postsecondary education. Age 55 recommended users were more likely than NMM users to be retired. Age 35 diverted users were less likely than recommended users to report poor physical health (odds ratio [OR] = 0.40 [0.17, 0.94]). Age 55 diverted users were less likely than recommended users to report three or more poor health conditions (OR = 0.22 [0.09, 0.55]) and any qualifying conditions (OR = 0.21 [0.08, 0.58]). Prevalence of these conditions was similar between diverted and NMM users.
Conclusions:
Results indicated a substantial degree of nonmedical (i.e., recreational) marijuana use. Diverted and NMM users reported generally similar levels of health conditions, whereas diverted users had fewer indicators of poor health than recommended users.
Medical marijuana use has increased among U.S. adults, both in states that have made such use legal as well as states in which such use remains illegal (Han et al., 2018). Individuals may use marijuana (a colloquial term for the cannabis plant and its derivatives; in the current article, the terms marijuana and cannabis are used interchangeably) for self-medication regardless of state laws or doctor recommendations (Park & Wu, 2017). Yet, similarities between individuals using marijuana for medical versus recreational purposes in outcomes including psychological problems and Addiction Severity Index Drug Use composite scores (Roy-Byrne et al., 2015) suggest that some individuals use medical marijuana for recreational purposes (Compton et al., 2017). Such recreational use may involve diverting medical marijuana from intended users via giving, sharing, trading, or selling to users without medical use recommendations. Use of someone else’s prescription medication meets the definition of prescription drug misuse (National Institute on Drug Abuse [NIDA], 2018). Substances considered high risk for prescription misuse and diversion include opioids, central nervous system depressants, and stimulants (NIDA, 2018; Wood, 2015). Although some studies have examined marijuana diversion prevalence among subgroups such as adult psychiatric inpatients (Nussbaum et al., 2015), the degree to which medical marijuana is diverted to unintended users among the general population is unknown.
Medical marijuana diversion may reflect medical and/or recreational use motivations; research indicates that recreational motivations may be likely. Regarding medical motivations, individuals may use diverted medical marijuana because of (a) running out of or not being able to access their own supply, (b) living in states without medical marijuana legislation, (c) an inability to find medical professionals willing to provide use recommendations, or (d) a desire to treat medical condition(s) not covered by state medical marijuana policy. Regarding recreational motivations, individuals may use diverted marijuana simply to get high. Research has linked increases in adult marijuana use and use disorder with implementation of some state medical marijuana laws (Hasin et al., 2017; Wen et al., 2015). Such increases would be understandable among medical users who typically report near daily/daily use (Bohnert et al., 2018; Bonn-Miller et al., 2014; Haug et al., 2017; Kepple & Freisthler, 2018); increased marijuana use prevalence and frequency have been found among those using for medical purposes in states with medical marijuana laws (Han et al., 2018). Adult nonmedical or illicit marijuana use also increased significantly after state medical marijuana law implementation (Cerdá et al 2012; Hasin et al., 2017), indicating connections between diverted medical marijuana and recreational use, possibly driven by availability (Hasin, 2018; Hasin et al., 2017). There is public discussion about medical marijuana black market diversion (Verywell Health, 2019) and resulting associations with outcomes including substance treatment need (Salomonsen-Sautel et al., 2012; Thurstone et al., 2011). One analytical approach to examining recreational versus medical factors underlying medical marijuana diversion would be to examine health condition similarities between those reporting use of diverted medical marijuana versus medical marijuana recommended for themselves. To the degree that diverted medical marijuana users report lower health condition prevalence than users of medical marijuana recommended for their own health conditions, recreational motivations may be more likely to drive diversion.
The number of registered medical marijuana participants is highest across ages 30–60 years, and in many states the largest number of registered participants is in their 50s (Fairman, 2016). Yet, medical marijuana use is higher among those ages 30–49 than 50 and older (Han et al., 2018). There do not appear to be meaningful age differences in the degree to which adults report medical use only versus nonmedical use only or both medical and nonmedical use (Compton et al., 2017). Questions concerning medical marijuana diversion prevalence and how diversion relates to medical need are relevant for all adults but particularly so for those ages 30–60, who are most likely to be registered medical marijuana participants (Fairman, 2016), who experience increased health concerns, and among whom marijuana use has strongly increased (Han et al., 2017).
This study contributes to the medical marijuana literature by examining (a) the prevalence of using medical marijuana intended for someone else, using medical marijuana intended for the user, and using marijuana not intended for medical use and (b) whether health condition prevalence indicators differ by such use patterns. Three research questions guided this cross-sectional analysis:
(a) What proportion of adults at modal ages 35 and 55 reported using medical marijuana intended for someone else versus using either medical marijuana intended for their own use, or using marijuana not intended for medical use?
(b) To what extent do sociodemographic characteristics differentiate use types?
(c) How is use type associated with self-reported overall physical health and specific health condition prevalence (including conditions identified as qualifying for treatment in many state medical marijuana laws)?
Method
Sample
Data were obtained from adults participating in the 2013–2018 Monitoring the Future (MTF) longitudinal study at modal ages 35 and 55. Detailed methods are presented elsewhere (Bachman et al., 2015; Miech et al., 2019; Schulenberg et al., 2019). In brief, MTF surveys annual, nationally representative cross-sectional samples of approximately 15,000 12th grade students (modal age 18) from 130 public and private schools in the coterminous United States (school samples are revised annually). A representative subsample of approximately 2,450 students is selected from each annual sample for longitudinal follow-up with oversampling of drug users. Six biennial follow-up surveys are conducted between 12th grade and modal age 30; thereafter, follow-up surveys are conducted every 5 years. The modal age (hereafter referred to simply as “age”) 55 respondents included here were drawn from the 1976–1981 12th grade cohorts; age 35 respondents were drawn from the 1996–2001 cohorts (data were not available from the same individuals at both ages 35 and 55 because of the recency of medical marijuana use measures). A University of Michigan Institutional Review Board approved the study, including consent procedures. Data were collected using mailed questionnaires; follow-up response rates averaged 36.7% and 49.8% for ages 35 and 55, respectively. Of the 5,404 cases who responded at age 35, 125 (2.3%) were removed because of conflicting or missing data on marijuana measures (past-12-month use, past-30-day use, and medical use), leaving a total of 5,279 for analysis. Respective numbers for age 55 respondents were 7,144 total respondents, with 285 (4.0%) removed because of conflicting/missing data on marijuana indicators, leaving 6,859 for final analysis. Attrition adjustments are discussed below (see Analyses).
Measures
Marijuana use.
At ages 35 and 55, marijuana use was measured using the question, “On how many occasions (if any) have you used marijuana (weed, pot) or hashish (hash, hash oil) during the last 12 months?” (response options used a 7-point scale of 0 occasions, 1–2, 3–5, 6–9, 10–19, 20–39, and 40 or more occasions). A dichotomy indicating any use (versus none) was coded.
At age 35, respondents were asked, “If you used marijuana in the last 12 months, did you get any of it from (a) . . . a medical marijuana prescription in your name? (b) . . . someone else’s medical marijuana prescription?” (response options of yes, no, did not use). At age 55, respondents were asked, “If you used marijuana in the last 12 months, how much came from (a) . . . your own medical marijuana prescription? (b) . . . someone else’s medical marijuana prescription?” (response options of none, a little, some, most, all). Responses at both ages were dichotomized as any versus none. Readers should be aware that the MTF measures use the term prescription as a colloquialism to refer to the typical way in which patients discuss medications with their medical providers. Although many states have legalized the medical use of marijuana for specific conditions, cannabis remains a Schedule I substance under federal law (Controlled Substances Act, 1970), with no accepted medical use. A decision by the Ninth Circuit Court of Appeals (Conant v. Walters, 2002) clarified that although physicians may not actually prescribe or dispense marijuana, they are able to issue either written or oral recommendations for marijuana use.
Based on responses to the any use and medical marijuana use items, the following multi-categorical measure of 12-month marijuana use was coded at both ages 35 and 55: (a) no marijuana use, (b) nonmedical marijuana use only (NMM Use), (c) diverted use of medical marijuana intended for others with no use of marijuana medically intended for the users themselves (Diverted MM Use), (d) recommended medical marijuana use involving marijuana medically recommended for the user themselves with no diverted use (Recommended MM Use), and (e) both diverted and recommended medical marijuana use (D+RMM Use).
Health measures.
Overall physical health was asked at both ages as, “Overall, relative to other people your age, do you think your physical health over the past year has been . . . much poorer than average, somewhat poorer, about average, somewhat better, much better than average.” Responses were coded as a dichotomy of 1 = much/somewhat poorer versus 0 = average/somewhat better/much better.
At age 55 only, respondents were asked, “Has a doctor or other medical professional ever told you that you have . . .” followed by a listing of 30 medical conditions with yes/no response options (see Supplemental Table 1 for full wording of all conditions). (Supplemental material appears as an online-only addendum to this article on the journal’s website.) The medical condition list was developed to examine a range of midlife health concerns, not to specifically examine qualifying medical marijuana conditions. Based on review of all current state medical marijuana laws as of December 2018 (Compassionate Certification Centers, 2017), 10 conditions were identified as qualifying conditions in at least one state: skin cancer, lung cancer, other cancers, cirrhosis of the liver, HIV/AIDs, autoimmune disorder, migraine headaches, arthritis or other joint condition, other chronic pain condition, and posttraumatic stress disorder (PTSD). In addition to dichotomous yes/no measures for specific conditions, three dichotomous yes/no summary measures were coded as follows: (a) prevalence of one or more of the 30 health conditions regardless of condition type, (b) prevalence of three or more health conditions regardless of condition type, and (c) prevalence of one or more of the 10 identified medical marijuana qualifying conditions. Sensitivity analyses examining the definition of qualifying conditions were conducted by coding a second qualifying condition measure comprising three additional conditions frequently reported as being relevant for medical marijuana use: general anxiety, panic, or phobias; major depressive disorder; and memory impairment (Bonn-Miller et al., 2014; Canadian Agency for Drugs and Technologies in Health, 2019; Haug et al., 2017; Kepple & Freisthler, 2018). No significant differences were observed in associations between marijuana use type and the two qualifying condition measures.
Covariates
Covariates included the following demographic characteristics previously found to differentiate between individuals using marijuana for medical versus nonmedical purposes (Compton et al., 2017; Han et al., 2018): sex (male/female), race/ethnicity (Black, Hispanic, White, other race/ethnicity), current marital status (married/not married), employment (age 35: employed full time/other; age 55: employed full time, retired, other), previous year income assistance (any unemployment or governmental assistance vs. none), and postsecondary education (any education past 12th grade vs. none).
Analyses
All analyses used SAS 9.4 (SAS Institute Inc., Cary, NC) and incorporated age-specific attrition weights based on extensive information available from 12th grade measures. Multiple imputation (PROC MI with fully conditional specification; 20 multiply imputed data sets) was conducted using all sample data to address missing data on non-marijuana use measures (see Supplemental Correlation Table for correlation coefficient matrixes). Given the use of complex sample survey data (Heeringa et al., 2017), all models accounted for the design of individuals within MTF sampling units with unequal probability of selection using Taylor series linearization for variance estimation (SAS Institute Inc., 2013). Subpopulation estimates accounted for the number of subgroup observations; subpopulation estimate standard errors were calculated based on all cases (e.g., the DOMAIN procedure; SAS Institute Inc., 2013; Institute for Digital Research and Education, n.d.). For descriptive statistics, SURVEYFREQ and SURVEYMEANS procedures were used. For logistic regression models, SURVEYLOGISTIC was used to regress (a) marijuana use types on sociodemographic characteristics, and (b) health conditions on marijuana use types based on the basic model of  in which π is the binary response probability modeled, α is the intercept parameter, x is the row vector of explanatory variables, and β is the vector of slope parameters for individual i within MTF sampling unit h. Synthesis of analytic results across the 20 multiply imputed data sets for statistical inference was conducted using PROC MIANALYZE (Berglund & Heeringa, 2014). Sensitivity analyses compared results of complete case versus multiple imputation regression models; results indicated either no meaningful differences or fewer meaningful findings with multiple imputation models (see Supplemental Tables 2–4).
in which π is the binary response probability modeled, α is the intercept parameter, x is the row vector of explanatory variables, and β is the vector of slope parameters for individual i within MTF sampling unit h. Synthesis of analytic results across the 20 multiply imputed data sets for statistical inference was conducted using PROC MIANALYZE (Berglund & Heeringa, 2014). Sensitivity analyses compared results of complete case versus multiple imputation regression models; results indicated either no meaningful differences or fewer meaningful findings with multiple imputation models (see Supplemental Tables 2–4).
Results
Sample description
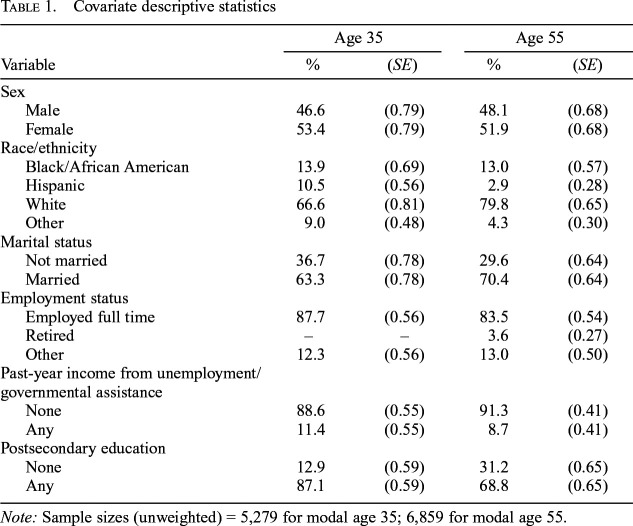
Table 1 presents covariate descriptive statistics. At both ages 35 and 55, respondents were roughly evenly divided by sex; more than four fifths were employed full time, and approximately 10% reported any past-year unemployment or governmental assistance income. Age 55 respondents were more likely than age 35 respondents to be White, currently married, and to report no postsecondary education.
Table 1.
Covariate descriptive statistics
| Variable | Age 35 |
Age 55 |
||
| % | (SE) | % | (SE) | |
| Sex | ||||
| Male | 46.6 | (0.79) | 48.1 | (0.68) |
| Female | 53.4 | (0.79) | 51.9 | (0.68) |
| Race/ethnicity | ||||
| Black/African American | 13.9 | (0.69) | 13.0 | (0.57) |
| Hispanic | 10.5 | (0.56) | 2.9 | (0.28) |
| White | 66.6 | (0.81) | 79.8 | (0.65) |
| Other | 9.0 | (0.48) | 4.3 | (0.30) |
| Marital status | ||||
| Not married | 36.7 | (0.78) | 29.6 | (0.64) |
| Married | 63.3 | (0.78) | 70.4 | (0.64) |
| Employment status | ||||
| Employed full time | 87.7 | (0.56) | 83.5 | (0.54) |
| Retired | – | – | 3.6 | (0.27) |
| Other | 12.3 | (0.56) | 13.0 | (0.50) |
| Past-year income from unemployment/governmental assistance | ||||
| None | 88.6 | (0.55) | 91.3 | (0.41) |
| Any | 11.4 | (0.55) | 8.7 | (0.41) |
| Postsecondary education | ||||
| None | 12.9 | (0.59) | 31.2 | (0.65) |
| Any | 87.1 | (0.59) | 68.8 | (0.65) |
Note: Sample sizes (unweighted) = 5,279 for modal age 35; 6,859 for modal age 55.
Marijuana use prevalence
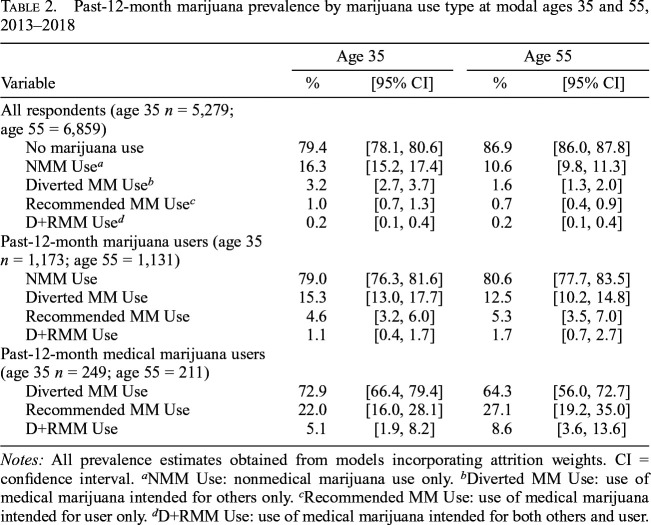
Table 2 presents marijuana use prevalence estimates. For age 35 and 55 respondents, respectively, 20.6% and 13.1% reported any past-12-month marijuana use; 4.4% and 2.5% reported any medical marijuana use. Among those reporting any past-12-month marijuana use, any medical marijuana use was reported by 21.0% and 19.5% of age 35 and 55 respondents, respectively. Among respondents reporting any past-12-month medical marijuana use, approximately one fourth reported Recommended MM Use (22.0% age 35; 27.1% age 55), whereas the clear majority reported Diverted MM Use (72.9% age 35; 64.3% age 55). Very few respondents reported D+RMM Use (n < 20); these respondents were excluded from further analysis.
Table 2.
Past-12-month marijuana prevalence by marijuana use type at modal ages 35 and 55, 2013–2018
| Variable | Age 35 |
Age 55 |
||
| % | [95% CI] | % | [95% CI] | |
| All respondents (age 35 n = 5,279; age 55 = 6,859) | ||||
| No marijuana use | 79.4 | [78.1, 80.6] | 86.9 | [86.0, 87.8] |
| NMM Usea | 16.3 | [15.2, 17.4] | 10.6 | [9.8, 11.3] |
| Diverted MM Useb | 3.2 | [2.7, 3.7] | 1.6 | [1.3, 2.0] |
| Recommended MM Usec | 1.0 | [0.7, 1.3] | 0.7 | [0.4, 0.9] |
| D+RMM Used | 0.2 | [0.1, 0.4] | 0.2 | [0.1, 0.4] |
| Past-12-month marijuana users (age 35 n = 1,173; age 55 = 1,131) | ||||
| NMM Use | 79.0 | [76.3, 81.6] | 80.6 | [77.7, 83.5] |
| Diverted MM Use | 15.3 | [13.0, 17.7] | 12.5 | [10.2, 14.8] |
| Recommended MM Use | 4.6 | [3.2, 6.0] | 5.3 | [3.5, 7.0] |
| D+RMM Use | 1.1 | [0.4, 1.7] | 1.7 | [0.7, 2.7] |
| Past-12-month medical marijuana users (age 35 n = 249; age 55 = 211) | ||||
| Diverted MM Use | 72.9 | [66.4, 79.4] | 64.3 | [56.0, 72.7] |
| Recommended MM Use | 22.0 | [16.0, 28.1] | 27.1 | [19.2, 35.0] |
| D+RMM Use | 5.1 | [1.9, 8.2] | 8.6 | [3.6, 13.6] |
Notes: All prevalence estimates obtained from models incorporating attrition weights. CI = confidence interval.
NMM Use: nonmedical marijuana use only.
Diverted MM Use: use of medical marijuana intended for others only.
Recommended MM Use: use of medical marijuana intended for user only.
D+RMM Use: use of medical marijuana intended for both others and user.
Sociodemographic differences in marijuana use types
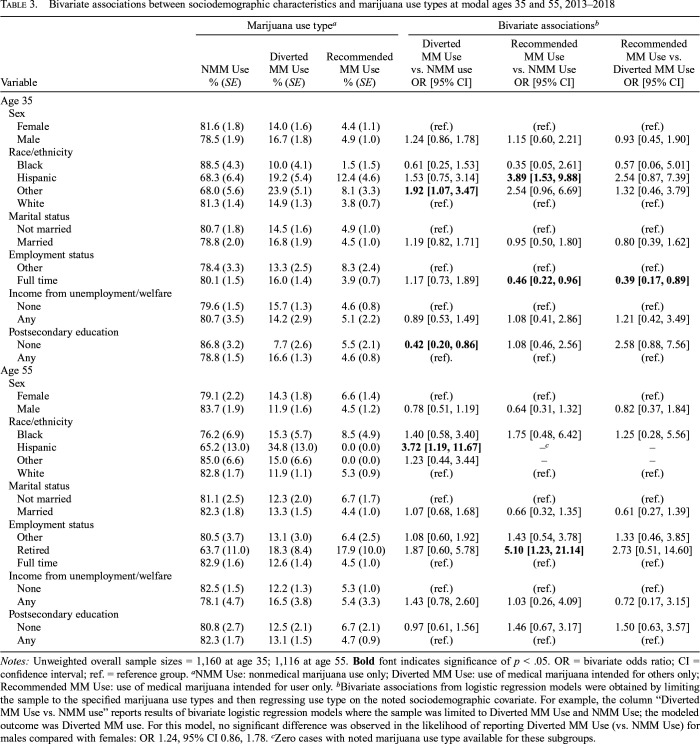
Bivariate logistic regression models examined marijuana use type differences by sociodemographic characteristics of sex, race/ethnicity, marital and employment status, past-year income from governmental assistance, and education achievement (Table 3). Associations were found for race/ethnicity, employment, and education.
Table 3.
Bivariate associations between sociodemographic characteristics and marijuana use types at modal ages 35 and 55, 2013–2018
| Variable | Marijuana use typea |
Bivariate associationsb |
||||
| NMM Use % (SE) | Diverted MM Use % (SE) | Recommended MM Use % (SE) | Diverted MM Use vs. NMM use OR [95% CI] | Recommended MM Use vs. NMM use OR [95% CI] | Recommended MM Use vs. Diverted MM Use OR [95% CI] | |
| Age 35 | ||||||
| Sex | ||||||
| Female | 81.6 (1.8) | 14.0 (1.6) | 4.4 (1.1) | (ref.) | (ref.) | (ref.) |
| Male | 78.5 (1.9) | 16.7 (1.8) | 4.9 (1.0) | 1.24 [0.86, 1.78] | 1.15 [0.60, 2.21] | 0.93 [0.45, 1.90] |
| Race/ethnicity | ||||||
| Black | 88.5 (4.3) | 10.0 (4.1) | 1.5 (1.5) | 0.61 [0.25, 1.53] | 0.35 [0.05, 2.61] | 0.57 [0.06, 5.01] |
| Hispanic | 68.3 (6.4) | 19.2 (5.4) | 12.4 (4.6) | 1.53 [0.75, 3.14] | 3.89 [1.53, 9.88] | 2.54 [0.87, 7.39] |
| Other | 68.0 (5.6) | 23.9 (5.1) | 8.1 (3.3) | 1.92 [1.07, 3.47] | 2.54 [0.96, 6.69] | 1.32 [0.46, 3.79] |
| White | 81.3 (1.4) | 14.9 (1.3) | 3.8 (0.7) | (ref.) | (ref.) | (ref.) |
| Marital status | ||||||
| Not married | 80.7 (1.8) | 14.5 (1.6) | 4.9 (1.0) | (ref.) | (ref.) | (ref.) |
| Married | 78.8 (2.0) | 16.8 (1.9) | 4.5 (1.0) | 1.19 [0.82, 1.71] | 0.95 [0.50, 1.80] | 0.80 [0.39, 1.62] |
| Employment status | ||||||
| Other | 78.4 (3.3) | 13.3 (2.5) | 8.3 (2.4) | (ref.) | (ref.) | (ref.) |
| Full time | 80.1 (1.5) | 16.0 (1.4) | 3.9 (0.7) | 1.17 [0.73, 1.89] | 0.46 [0.22, 0.96] | 0.39 [0.17, 0.89] |
| Income from unemployment/welfare | ||||||
| None | 79.6 (1.5) | 15.7 (1.3) | 4.6 (0.8) | (ref.) | (ref.) | (ref.) |
| Any | 80.7 (3.5) | 14.2 (2.9) | 5.1 (2.2) | 0.89 [0.53, 1.49] | 1.08 [0.41, 2.86] | 1.21 [0.42, 3.49] |
| Postsecondary education | ||||||
| None | 86.8 (3.2) | 7.7 (2.6) | 5.5 (2.1) | 0.42 [0.20, 0.86] | 1.08 [0.46, 2.56] | 2.58 [0.88, 7.56] |
| Any | 78.8 (1.5) | 16.6 (1.3) | 4.6 (0.8) | (ref). | (ref.) | (ref.) |
| Age 55 | ||||||
| Sex | ||||||
| Female | 79.1 (2.2) | 14.3 (1.8) | 6.6 (1.4) | (ref.) | (ref.) | (ref.) |
| Male | 83.7 (1.9) | 11.9 (1.6) | 4.5 (1.2) | 0.78 [0.51, 1.19] | 0.64 [0.31, 1.32] | 0.82 [0.37, 1.84] |
| Race/ethnicity | ||||||
| Black | 76.2 (6.9) | 15.3 (5.7) | 8.5 (4.9) | 1.40 [0.58, 3.40] | 1.75 [0.48, 6.42] | 1.25 [0.28, 5.56] |
| Hispanic | 65.2 (13.0) | 34.8 (13.0) | 0.0 (0.0) | 3.72 [1.19, 11.67] | –c | – |
| Other | 85.0 (6.6) | 15.0 (6.6) | 0.0 (0.0) | 1.23 [0.44, 3.44] | – | – |
| White | 82.8 (1.7) | 11.9 (1.1) | 5.3 (0.9) | (ref.) | (ref.) | (ref.) |
| Marital status | ||||||
| Not married | 81.1 (2.5) | 12.3 (2.0) | 6.7 (1.7) | (ref.) | (ref.) | (ref.) |
| Married | 82.3 (1.8) | 13.3 (1.5) | 4.4 (1.0) | 1.07 [0.68, 1.68] | 0.66 [0.32, 1.35] | 0.61 [0.27, 1.39] |
| Employment status | ||||||
| Other | 80.5 (3.7) | 13.1 (3.0) | 6.4 (2.5) | 1.08 [0.60, 1.92] | 1.43 [0.54, 3.78] | 1.33 [0.46, 3.85] |
| Retired | 63.7 (11.0) | 18.3 (8.4) | 17.9 (10.0) | 1.87 [0.60, 5.78] | 5.10 [1.23, 21.14] | 2.73 [0.51, 14.60] |
| Full time | 82.9 (1.6) | 12.6 (1.4) | 4.5 (1.0) | (ref.) | (ref.) | (ref.) |
| Income from unemployment/welfare | ||||||
| None | 82.5 (1.5) | 12.2 (1.3) | 5.3 (1.0) | (ref.) | (ref.) | (ref.) |
| Any | 78.1 (4.7) | 16.5 (3.8) | 5.4 (3.3) | 1.43 [0.78, 2.60] | 1.03 [0.26, 4.09] | 0.72 [0.17, 3.15] |
| Postsecondary education | ||||||
| None | 80.8 (2.7) | 12.5 (2.1) | 6.7 (2.1) | 0.97 [0.61, 1.56] | 1.46 [0.67, 3.17] | 1.50 [0.63, 3.57] |
| Any | 82.3 (1.7) | 13.1 (1.5) | 4.7 (0.9) | (ref.) | (ref.) | (ref.) |
Notes: Unweighted overall sample sizes = 1,160 at age 35; 1,116 at age 55. Bold font indicates significance of p < .05. OR = bivariate odds ratio; CI = confidence interval; ref. = reference group.
NMM Use: nonmedical marijuana use only; Diverted MM Use: use of medical marijuana intended for others only; Recommended MM Use: use of medical marijuana intended for user only.
Bivariate associations from logistic regression models were obtained by limiting the sample to the specified marijuana use types and then regressing use type on the noted sociodemographic covariate. For example, the column “Diverted MM Use vs. NMM use” reports results of bivariate logistic regression models where the sample was limited to Diverted MM Use and NMM Use; the modeled outcome was Diverted MM use. For this model, no significant difference was observed in the likelihood of reporting Diverted MM Use (vs. NMM Use) for males compared with females: OR 1.24, 95% CI 0.86, 1.78.
Zero cases with noted marijuana use type available for these subgroups.
At age 35, the prevalence of Recommended MM Use (vs. NMM Use) was higher for Hispanic than White respondents (OR = 3.89, 95% CI [1.53, 9.88]). Recommended MM Use prevalence (vs. either NMM or Diverted Use) was lower for respondents with full-time employment status than without (ORs = 0.46 [0.22, 0.96] and 0.39 [0.17, 0.89], respectively). Respondents without postsecondary education were less likely than those with such education to report Diverted MM Use (vs. NMM Use) (OR = 0.42 [0.20, 0.86]).
At age 55, Diverted MM Use prevalence (vs. NMM Use) was higher for Hispanic than White respondents (OR = 3.72 [1.19, 11.67]). At age 55, no Hispanic respondents reported Recommended MM Use. Compared with those employed full time, retired respondents at age 55 reported higher Recommended MM Use prevalence (vs. NMM Use) (OR = 5.10 [1.23, 21.14]).
Health condition differences based on marijuana use type
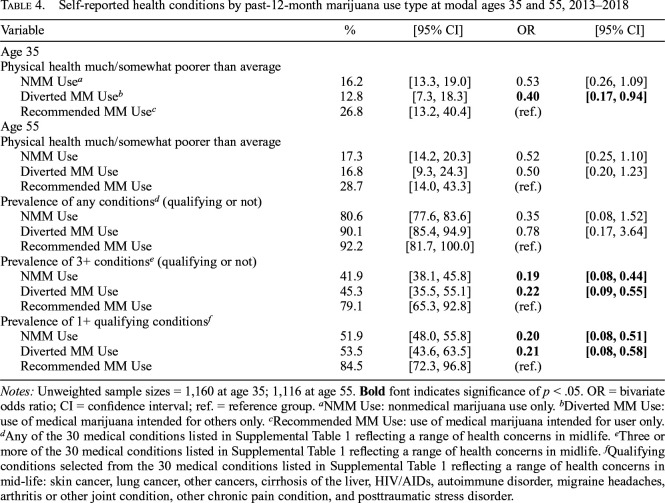
Table 4 presents bivariate estimates of cross-sectional differences by marijuana use type in four self-reported health prevalence conditions: (1) overall physical health, (2) any of the 30 health conditions, (3) three or more of the 30 conditions, and (4) any qualifying conditions.
Table 4.
Self-reported health conditions by past-12-month marijuana use type at modal ages 35 and 55, 2013–2018
| Variable | % | [95% CI] | OR | [95% CI] |
| Age 35 | ||||
| Physical health much/somewhat poorer than average | ||||
| NMM Usea | 16.2 | [13.3, 19.0] | 0.53 | [0.26, 1.09] |
| Diverted MM Useb | 12.8 | [7.3, 18.3] | 0.40 | [0.17, 0.94] |
| Recommended MM Usec | 26.8 | [13.2, 40.4] | (ref.) | |
| Age 55 | ||||
| Physical health much/somewhat poorer than average | ||||
| NMM Use | 17.3 | [14.2, 20.3] | 0.52 | [0.25, 1.10] |
| Diverted MM Use | 16.8 | [9.3, 24.3] | 0.50 | [0.20, 1.23] |
| Recommended MM Use | 28.7 | [14.0, 43.3] | (ref.) | |
| Prevalence of any conditionsd (qualifying or not) | ||||
| NMM Use | 80.6 | [77.6, 83.6] | 0.35 | [0.08, 1.52] |
| Diverted MM Use | 90.1 | [85.4, 94.9] | 0.78 | [0.17, 3.64] |
| Recommended MM Use | 92.2 | [81.7, 100.0] | (ref.) | |
| Prevalence of 3+ conditionse (qualifying or not) | ||||
| NMM Use | 41.9 | [38.1, 45.8] | 0.19 | [0.08, 0.44] |
| Diverted MM Use | 45.3 | [35.5, 55.1] | 0.22 | [0.09, 0.55] |
| Recommended MM Use | 79.1 | [65.3, 92.8] | (ref.) | |
| Prevalence of 1+ qualifying conditionsf | ||||
| NMM Use | 51.9 | [48.0, 55.8] | 0.20 | [0.08, 0.51] |
| Diverted MM Use | 53.5 | [43.6, 63.5] | 0.21 | [0.08, 0.58] |
| Recommended MM Use | 84.5 | [72.3, 96.8] | (ref.) |
Notes: Unweighted sample sizes = 1,160 at age 35; 1,116 at age 55. Bold font indicates significance of p < .05. OR = bivariate odds ratio; CI = confidence interval; ref. = reference group.
NMM Use: nonmedical marijuana use only.
Diverted MM Use: use of medical marijuana intended for others only.
Recommended MM Use: use of medical marijuana intended for user only.
Any of the 30 medical conditions listed in Supplemental Table 1 reflecting a range of health concerns in midlife.
Three or more of the 30 medical conditions listed in Supplemental Table 1 reflecting a range of health concerns in midlife.
Qualifying conditions selected from the 30 medical conditions listed in Supplemental Table 1 reflecting a range of health concerns in mid-life: skin cancer, lung cancer, other cancers, cirrhosis of the liver, HIV/AIDs, autoimmune disorder, migraine headaches, arthritis or other joint condition, other chronic pain condition, and posttraumatic stress disorder.
Only one health condition was measured at age 35: overall physical health. About one quarter (26.8%) of age 35 Recommended MM Users reported that their overall physical health was much/somewhat poorer than average, versus 12.8% of Diverted MM Users and 16.2% of NMM Users. Poor overall physical health was less prevalent among Diverted than Recommended MM Users (OR = 0.40 [0.17, 0.94]) but similar between other use types.
At age 55, prevalence of poor overall physical health followed a pattern similar to that observed at age 35 but with more similarity between use types (28.7% Recommended MM Users, 16.8% Diverted MM Users, 17.3% NMM Users). The percentages of respondents reporting one or more health conditions also were similar across use types. Having three or more conditions was less prevalent among both Diverted MM and NMM Users than Recommended MM Users (ORs = 0.22 [0.09, 0.55] and 0.19 [0.08, 0.44], respectively). Specifically, having three or more conditions was reported by 79.1% of Recommended MM Users, 45.3% of Diverted MM Users, and 41.9% of NMM Users. Having any qualifying conditions also was less prevalent among both Diverted MM and NMM Users than Recommended MM Users (ORs = 0.21 [0.08, 0.58] and 0.20 [0.08, 0.51], respectively). Having any qualifying condition was reported by 84.5% of Recommended MM Users versus 53.5% of Diverted MM and 51.9% of NMM Users. Additional models (not shown) found only one indication of health condition difference between age 55 NMM and Diverted MM Users: NMM Users had lower prevalence of one or more health conditions (80.6% vs. 90.1%; OR = 0.45 [0.26, 0.80]).
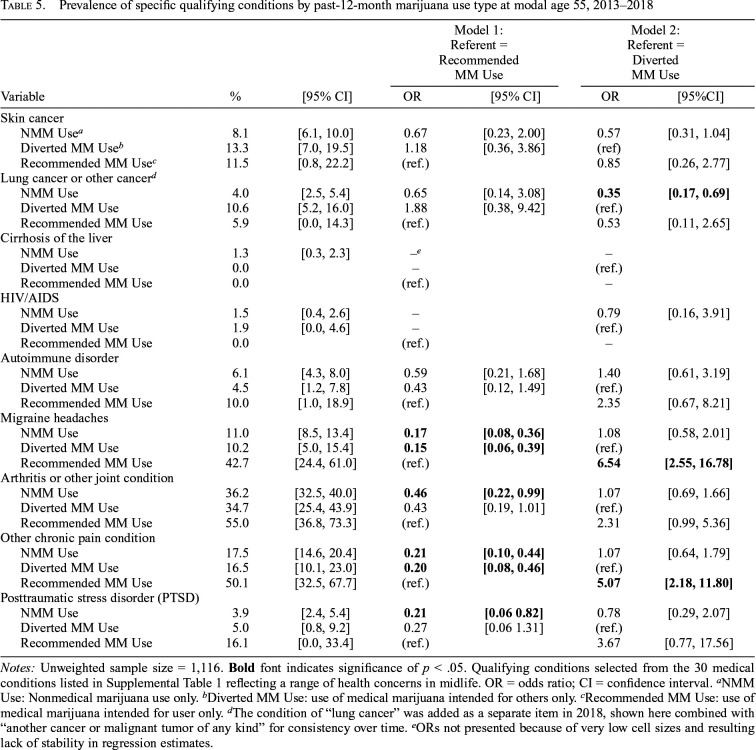
The models shown in Table 5 examined differences in the prevalence of each specific qualifying condition by marijuana use type. Diverted MM Users reported lower prevalence than Recommended MM users for migraine headaches (10.2% vs. 42.7%; OR = 0.15 [0.06, 0.39]), other chronic pain conditions (16.5% vs. 50.1%; OR = 0.20 [0.08, 0.46]). NMM users reported lower prevalence than Recommended MM users for migraine headaches (11.0% vs. 42.7%; OR = 0.17 [0.08, 0.36]), arthritis or other joint condition (36.2% vs. 55.0%; OR = 0.46 [0.22, 0.99]), other chronic pain conditions (17.5% vs. 50.1%; OR = 0.21 [0.10, 0.44]), and PTSD (3.9% vs. 16.1%; OR = 0.21 [0.06, 0.82]). NMM Users reported lower prevalence than Diverted MM Users for lung or other cancers (4.0% vs. 10.6%; OR = 0.35 [0.17, 0.69]).
Table 5.
Prevalence of specific qualifying conditions by past-12-month marijuana use type at modal age 55, 2013–2018
| Model 1: Referent = Recommended MM Use |
Model 2: Referent = Diverted MM Use |
|||||
| Variable | % | [95% CI] | OR | [95% CI] | OR | [95%CI] |
| Skin cancer | ||||||
| NMM Usea | 8.1 | [6.1, 10.0] | 0.67 | [0.23, 2.00] | 0.57 | [0.31, 1.04] |
| Diverted MM Useb | 13.3 | [7.0, 19.5] | 1.18 | [0.36, 3.86] | (ref) | |
| Recommended MM Usec | 11.5 | [0.8, 22.2] | (ref.) | 0.85 | [0.26, 2.77] | |
| Lung cancer or other cancerd | ||||||
| NMM Use | 4.0 | [2.5, 5.4] | 0.65 | [0.14, 3.08] | 0.35 | [0.17, 0.69] |
| Diverted MM Use | 10.6 | [5.2, 16.0] | 1.88 | [0.38, 9.42] | (ref.) | |
| Recommended MM Use | 5.9 | [0.0, 14.3] | (ref.) | 0.53 | [0.11, 2.65] | |
| Cirrhosis of the liver | ||||||
| NMM Use | 1.3 | [0.3, 2.3] | –e | – | ||
| Diverted MM Use | 0.0 | – | (ref.) | |||
| Recommended MM Use | 0.0 | (ref.) | – | |||
| HIV/AIDS | ||||||
| NMM Use | 1.5 | [0.4, 2.6] | – | 0.79 | [0.16, 3.91] | |
| Diverted MM Use | 1.9 | [0.0, 4.6] | – | (ref.) | ||
| Recommended MM Use | 0.0 | (ref.) | – | |||
| Autoimmune disorder | ||||||
| NMM Use | 6.1 | [4.3, 8.0] | 0.59 | [0.21, 1.68] | 1.40 | [0.61, 3.19] |
| Diverted MM Use | 4.5 | [1.2, 7.8] | 0.43 | [0.12, 1.49] | (ref.) | |
| Recommended MM Use | 10.0 | [1.0, 18.9] | (ref.) | 2.35 | [0.67, 8.21] | |
| Migraine headaches | ||||||
| NMM Use | 11.0 | [8.5, 13.4] | 0.17 | [0.08, 0.36] | 1.08 | [0.58, 2.01] |
| Diverted MM Use | 10.2 | [5.0, 15.4] | 0.15 | [0.06, 0.39] | (ref.) | |
| Recommended MM Use | 42.7 | [24.4, 61.0] | (ref.) | 6.54 | [2.55, 16.78] | |
| Arthritis or other joint condition | ||||||
| NMM Use | 36.2 | [32.5, 40.0] | 0.46 | [0.22, 0.99] | 1.07 | [0.69, 1.66] |
| Diverted MM Use | 34.7 | [25.4, 43.9] | 0.43 | [0.19, 1.01] | (ref.) | |
| Recommended MM Use | 55.0 | [36.8, 73.3] | (ref.) | 2.31 | [0.99, 5.36] | |
| Other chronic pain condition | ||||||
| NMM Use | 17.5 | [14.6, 20.4] | 0.21 | [0.10, 0.44] | 1.07 | [0.64, 1.79] |
| Diverted MM Use | 16.5 | [10.1, 23.0] | 0.20 | [0.08, 0.46] | (ref.) | |
| Recommended MM Use | 50.1 | [32.5, 67.7] | (ref.) | 5.07 | [2.18, 11.80] | |
| Posttraumatic stress disorder (PTSD) | ||||||
| NMM Use | 3.9 | [2.4, 5.4] | 0.21 | [0.06 0.82] | 0.78 | [0.29, 2.07] |
| Diverted MM Use | 5.0 | [0.8, 9.2] | 0.27 | [0.06 1.31] | (ref.) | |
| Recommended MM Use | 16.1 | [0.0, 33.4] | (ref.) | 3.67 | [0.77, 17.56] | |
Notes: Unweighted sample size = 1,116. Bold font indicates significance of p < .05. Qualifying conditions selected from the 30 medical conditions listed in Supplemental Table 1 reflecting a range of health concerns in midlife. OR = odds ratio; CI = confidence interval.
NMM Use: Nonmedical marijuana use only.
Diverted MM Use: use of medical marijuana intended for others only.
Recommended MM Use: use of medical marijuana intended for user only.
The condition of “lung cancer” was added as a separate item in 2018, shown here combined with “another cancer or malignant tumor of any kind” for consistency over time.
ORs not presented because of very low cell sizes and resulting lack of stability in regression estimates.
Discussion
Using data from national samples of U.S. adult high school graduates, this study found similar medical marijuana prevalence levels among marijuana users ages 35 and 55. About one fifth of past-12-month marijuana users used medical marijuana. More than two thirds of medical marijuana users reported that all the medical marijuana they had used was medically recommended for others, indicating a substantial degree of diversion. Some cross-sectional evidence indicated lower levels of illness and/or perceived poor health among Diverted MM versus Recommended MM Users, supporting the possibility of a meaningful degree of recreational (i.e., nonmedical) use.
Medical marijuana use was reported by 4.4% of age 35 respondents and 2.5% of age 55 respondents. These estimates are similar to those in prior national studies. Han et al. (2018) found that, in 2015, approximately 2% of U.S. adults age 18 and older reported medical marijuana use in the past 12 months. Among all past-12-month marijuana users, 11.5% reported medical marijuana use, including 7.6% who reported using only medical marijuana (Han et al., 2018). The current study extends such research by examining medical marijuana diversion: only one quarter of past-12-month medical marijuana users reported using marijuana medically solely recommended for themselves. These results may have important implications for links between state medical marijuana laws and increased illicit marijuana use (Cerdá et al., 2012; Hasin et al., 2017). For example, from 1991/92 to 2012/13, illicit marijuana use (i.e., use without medical recommendation or other than as recommended, such as to get high) increased more in states that had passed medical marijuana legislation than in other states (Hasin et al., 2017). Diverted medical marijuana use meets the definition of illicit use.
To the extent that individuals reporting Diverted MM Use might be self-medicating, one would expect health condition prevalence levels to be similar between Diverted MM and Recommended MM Users, with noticeable differences between Diverted MM and NMM Users. The current study found that at age 35, poor overall physical health was less likely among Diverted MM than Recommended MM Users; at age 55, having three or more health conditions, as well as any qualifying conditions, was less likely among Diverted MM than Recommended MM Users. Self-reported general health was similar between Diverted MM and NMM Users; however, the prevalence of one or more health conditions was higher among Diverted MM Users, with lung and other cancers specifically more prevalent among Diverted MM Users. These results suggest that Diverted MM Users are more similar to NMM Users in terms of medical need than Recommended MM Users, but some Diverted MM Users likely use for medical needs, some for nonmedical needs, and some for both (Han et al., 2018; Park & Wu, 2017).
To whatever degree diverted medical marijuana is used medically, concerns exist related to “loaning” and/or “borrowing” medication for health purposes. Such behaviors are associated with negative consequences from abuse/disorder, and loss of medical warnings and instructions, which leads to increased risk of incorrect dosing and lack of effectiveness, overdose, side effects, etc. (Goldsworthy et al., 2008). Medical professionals need to proactively help patients manage medications safely, including active counseling and education about the dangers of sharing prescription medication and how to appropriately dispose of unused medication after treatment is discontinued (Ellis & Mullan, 2009). Real risks can arise from diverted marijuana use due to lack of knowledge about concentration levels and metabolism of medical marijuana products based on route of administration (ROA). For example, high-concentration ROAs such as dabbing are associated with acute harms such as psychotic episodes and severe impairment (Alzghari et al., 2017; Russell et al 2018). Edibles have delayed psychoactive effect onset, and users thus have a reduced ability to titrate dose and effects; medical marijuana edibles have been connected with overdoses, emergency department admissions, and poison control center calls (Russell et al., 2018; Wang et al., 2013).
Beyond diversion concerns, there is a great need for increased oversight and research regarding medical marijuana generally. There is a paucity of research supporting recommendations for appropriate dosing, strain, purity, and ROA for specific medical conditions, including the degree to which medical marijuana may actually exacerbate particular existing medical conditions (Bonn-Miller et al., 2014; MacCallum & Russo, 2018; Russel et al., 2018). There are very few resources that physicians can turn to to provide such information (MacCallum & Russo, 2018). There is also a great need for research on policies that can help increase public health and safety regarding medical marijuana use. In particular, there is a need for policies focusing on medical marijuana dispensaries to appropriately regulate the availability of items that may be particularly dangerous to uninformed or “marijuana-naive” users (pre-rolled joints; edibles) as well as high-concentration products that may contribute to dangerous heavy use (Keppel & Freisthler, 2018).
Strengths, limitations, and future directions
These results are subject to limitations. All data were cross-sectional; results cannot be viewed as causal. These analyses cannot determine the degree to which health-related problems may precede or follow nonmedical or medical marijuana use. Associations between health condition prevalence and marijuana use type observed in the current study should not be understood to provide definitive evidence regarding which conditions may or may not be appropriate for medical marijuana use. Subjects were limited to those at modal ages 35 and 55 who attended 12th grade. Results may not generalize across adulthood years or to individuals who drop out of school before 12th grade. Because school dropout is associated with higher marijuana use (Bachman et al., 2008; Tice et al., 2017), the marijuana use estimates reported here are likely conservative (i.e., low). The sample was also subject to attrition; use of weighting adjustments addressed the limitation of attrition in part. Although the list of health conditions used in the current study clearly does not encompass all of the conditions identified as qualifying for medical marijuana under existing state policies, it provided an opportunity to examine initial associations. These limitations notwithstanding, the current study provides needed data regarding prevalence of diverted use and differences between such use and recommended use using national samples of U.S. adults in middle adulthood.
Future research focusing on state policy-specific qualifying conditions would be of use, as would research exploring differences (if any) in the specific medical conditions for which individuals report recommended versus diverted use. Even patients with medical use recommendations have been reported to use medical marijuana for health conditions not included in state policy (Bonn-Miller et al., 2014). Also needed is research on factors beyond sociodemographic characteristics that differentiate recommended and diverted use, such as physical and socioeconomic proximity/access to medical marijuana products (i.e., physical distance and cost-related motivations for diversion) and social network characteristics.
Conclusions
About one fifth of age 35 and 55 past-12-month marijuana users in the United States used medical marijuana. More than two thirds of medical marijuana users reported that all the medically recommended marijuana they used was diverted from the intended person’s use. Diverted MM Users were more similar to NMM Users than those reporting that all medical marijuana they had used was intended for their own use.
Footnotes
This work was supported by National Institute on Drug Abuse (NIDA) Grants DA001411 and DA016575. NIDA had no further role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; nor in the decision to submit the paper for publication. The views expressed in this article are those of the authors and do not necessarily reflect the views of the funders.
References
- Alzghari S. K., Fung V., Rickner S. S., Chacko L., Fleming S. W. To dab or not to dab: Rising concerns regarding the toxicity of cannabis concentrates. Cureus. 2017;9 doi: 10.7759/cureus.1676. doi:10.7759/cureus.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachman J. G., Johnston L. D., O’Malley P. M., Schulenberg J. E., Miech R. A. The Monitoring the Future Project after four decades: Design and procedures (Monitoring the Future Occasional Paper No. 82) Ann Arbor, MI: Institute for Social Research, University of Michigan; 2015. Retrieved from http://monitoringthefuture.org/pubs/occpapers/mtf-occ82.pdf. [Google Scholar]
- Bachman J. G., O’Malley P. M., Schulenberg J. E., Johnston L. D., Freedman-Doan P., Messersmith E. E. The education-drug use connection: How successes and failures in school relate to adolescent smoking, drinking, drug use, and delinquency. NewYork, NY: Lawrence Erlbaum Associates/Taylor & Francis; 2008. [Google Scholar]
- Berglund P., Heeringa S. Multiple imputation of missing data using SAS. Cary, NC: SAS Institute Inc; 2014. [Google Scholar]
- Bohnert K. M., Bonar E. E., Arnedt J. T., Conroy D. A., Walton M. A., Ilgen M. A. Utility of the comprehensive marijuana motives questionnaire among medical cannabis patients. Addictive Behaviors. 2018;76:139–144. doi: 10.1016/j.addbeh.2017.08.001. doi:10.1016/j.addbeh.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Boden M. T., Bucossi M. M., Babson K. A. Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. American Journal of Drug and Alcohol Abuse. 2014;40:23–30. doi: 10.3109/00952990.2013.821477. doi:10.3109/00952990.2013.821477. [DOI] [PubMed] [Google Scholar]
- Canadian Agency for Drugs and Technologies in Health. Medical cannabis for the treatment of dementia: A review of clinical effectiveness and guidelines (CADTH rapid response report: summary with critical appraisal) Ottawa, Ontario: Author; 2019. [PubMed] [Google Scholar]
- Cerdá M., Wall M., Keyes K. M., Galea S., Hasin D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence. 2012;120:22–27. doi: 10.1016/j.drugalcdep.2011.06.011. doi:10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compassionate Certification Centers. List of qualifying health conditions for medical marijuana in each state. 2017. Retrieved from https://www.compassionatecertificationcenters.com/list-of-qualifying-health-conditions-for-medical-marijuana-in-each-state/ [Google Scholar]
- Compton W. M., Han B., Hughes A., Jones C. M., Blanco C. Use of marijuana for medical purposes among adults in the United States. JAMA. 2017;317:209–211. doi: 10.1001/jama.2016.18900. doi:10.1001/jama.2016.18900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conant v. Walters, 309 F.3d 629 (9th Cir., 2002) [Google Scholar]
- Controlled Substances Act 197021 U.S.C. 811 et seq.
- Ellis J., Mullan J. Prescription medication borrowing and sharing—risk factors and management. Australian Family Physician. 2009;38:816–819. [PubMed] [Google Scholar]
- Fairman B. J. Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug and Alcohol Dependence. 2016;159:72–79. doi: 10.1016/j.drugalcdep.2015.11.015. doi:10.1016/j.drugalcdep.2015.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsworthy R. C., Schwartz N. C., Mayhorn C. B. Beyond abuse and exposure: Framing the impact of prescription-medication sharing. American Journal of Public Health. 2008;98:1115–1121. doi: 10.2105/AJPH.2007.123257. doi:10.2105/AJPH.2007.123257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B., Compton W. M., Blanco C., Jones C. M. Trends in and correlates of medical marijuana use among adults in the United States. Drug and Alcohol Dependence. 2018;186:120–129. doi: 10.1016/j.drugalcdep.2018.01.022. doi:10.1016/j.drugalcdep.2018.01.022. [DOI] [PubMed] [Google Scholar]
- Han B. H., Sherman S., Mauro P. M., Martins S. S., Rotenberg J., Palamar J. J. Demographic trends among older cannabis users in the United States, 2006-13. Addiction. 2017;112:516–525. doi: 10.1111/add.13670. doi:10.1111/add.13670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology Reviews. 2018;43:195–212. doi: 10.1038/npp.2017.198. doi:10.1038/npp.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Sarvet A. L., Cerdá M., Keyes K. M., Stohl M., Galea S., Wall M. M. US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991-1992 to 2012-2013. JAMA Psychiatry. 2017;74:579–588. doi: 10.1001/jamapsychiatry.2017.0724. doi:10.1001/jamapsychiatry.2017.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug N. A., Padula C. B., Sottile J. E., Vandrey R., Heinz A. J., Bonn-Miller M. O. Cannabis use patterns and motives: A comparison of younger, middle-aged, and older medical cannabis dispensary patients. Addictive Behaviors. 2017;72:14–20. doi: 10.1016/j.addbeh.2017.03.006. doi:10.1016/j.addbeh.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa S. G., West B. T., Berglund P. A. Applied survey data analysis. Boca Raton, FL: CRC Press, Taylor and Francis Group: 2017. [Google Scholar]
- Institute for Digital Research and Education. (n.d.) Applied survey data analysis using SAS 9.4. UCLA Institute for Digital Research and Education Statistical Consulting; Retrieved from https://stats.idre.ucla.edu/sas/seminars/sas-survey/ [Google Scholar]
- Kepple N. J., Freisthler B. Who’s buying what and how much? Correlates of purchase behaviors from medical marijuana dispensaries in Los Angeles, California. Journal of Primary Prevention. 2018;39:571–589. doi: 10.1007/s10935-018-0528-5. doi:10.1007/s10935-018-0528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum C. A., Russo E. B. Practical considerations in medical cannabis administration and dosing. European Journal of Internal Medicine. 2018;49:12–19. doi: 10.1016/j.ejim.2018.01.004. doi:10.1016/j.ejim.2018.01.004. [DOI] [PubMed] [Google Scholar]
- Miech R. A., Johnston L. D., O’Malley P. M., Bachman J. G., Schulenberg J. E., Patrick M. E. Monitoring the Future national survey results on drug use, 1975-2018: Volume I, secondary school students. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2019. [Google Scholar]
- National Institute on Drug Abuse. Misuse of prescription drugs. 2018. Retrieved from https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/2609-misuse-of-prescription-drugs.pdf. [Google Scholar]
- Nussbaum A. M., Thurstone C., McGarry L., Walker B., Sabel A. L. Use and diversion of medical marijuana among adults admitted to inpatient psychiatry. American Journal of Drug and Alcohol Abuse. 2015;41:166–172. doi: 10.3109/00952990.2014.949727. doi:10.3109/00952990.2014.949727. [DOI] [PubMed] [Google Scholar]
- Park J.-Y., Wu L.-T. Prevalence, reasons, perceived effects, and correlates of medical marijuana use: A review. Drug and Alcohol Dependence. 2017;177:1–13. doi: 10.1016/j.drugalcdep.2017.03.009. doi:10.1016/j.drugalcdep.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy-Byrne P., Maynard C., Bumgardner K., Krupski A., Dunn C., West I. I., Ries R. Are medical marijuana users different from recreational users? The view from primary care. American Journal on Addictions. 2015;24:599–606. doi: 10.1111/ajad.12270. doi:10.1111/ajad.12270. [DOI] [PubMed] [Google Scholar]
- Russell C., Rueda S., Room R., Tyndall M., Fischer B. Routes of administration for cannabis use - basic prevalence and related health outcomes: A scoping review and synthesis. International Journal on Drug Policy. 2018;52:87–96. doi: 10.1016/j.drugpo.2017.11.008. doi:10.1016/j.drugpo.2017.11.008. [DOI] [PubMed] [Google Scholar]
- Salomonsen-Sautel S., Sakai J. T., Thurstone C., Corley R., Hopfer C. Medical marijuana use among adolescents in substance abuse treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:694–702. doi: 10.1016/j.jaac.2012.04.004. doi:10.1016/j.jaac.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® 13.1 user’s guide. Cary, NC: Author; 2013. Retrieved from https://support.sas.com/documentation/onlinedoc/stat/131/surveylogistic.pdf. [Google Scholar]
- Schulenberg J. E., Johnston L. D., O’Malley P. M., Bachman J. G., Miech R. A., Patrick M. E. Monitoring the Future national survey results on drug use, 1975-2018: Volume II, college students and adults ages 19-55. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2019. [Google Scholar]
- Thurstone C., Lieberman S. A., Schmiege S. J. Medical marijuana diversion and associated problems in adolescent substance treatment. Drug and Alcohol Dependence. 2011;118:489–492. doi: 10.1016/j.drugalcdep.2011.03.031. doi:10.1016/j.drugalcdep.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tice P., Lipari R. N., Van Horn S. L. Substance use among 12th grade aged youths, by dropout status. The CHBSQ Report: August 15. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. Retrieved from https://www.samhsa.gov/data/sites/default/files/report_3196/ShortReport-3196.pdf. [PubMed] [Google Scholar]
- Verywell Health. Abusing the medical marijuana law system: The temptation of profiting off of prescribed pot. New York: Dotdash; 2019. Retrieved from https://www.verywellhealth.com. [Google Scholar]
- Wang G. S., Roosevelt G., Heard K. Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatrics. 2013;167:630–633. doi: 10.1001/jamapediatrics.2013.140. doi:10.1001/jamapediatrics.2013.140. [DOI] [PubMed] [Google Scholar]
- Wen H., Hockenberry J. M., Cummings J. R. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. Journal of Health Economics. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. doi:10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Wood D. Drug diversion. Australian Prescriber. 2015;38:164–166. doi: 10.18773/austprescr.2015.058. doi:10.18773/austprescr.2015.058. [DOI] [PMC free article] [PubMed] [Google Scholar]