Abstract
Objectives:
Infants who are HIV exposed but uninfected (HEU) compared to HIV unexposed uninfected (HUU) have increased risk of adverse birth outcomes, morbidity and hospitalization. In the era of universal maternal antiretroviral treatment, there are few insights into patterns of neonatal morbidity specifically.
Design:
Prospective cohort.
Methods:
We compared neonatal hospitalizations among infants who were HEU (n=463) vs HUU (n=466) born between 2017 and 2019 to a cohort of pregnant women from a large antenatal clinic in South Africa. We examined maternal and infant factors associated with hospitalization using logistic regression.
Results:
Hospitalization rates were similar between neonates who were HEU and HUU (13% vs. 16%; p=0.25). Overall, most hospitalizations occurred directly after birth (87%); infection-related causes were identified in 34%. The most common reason for hospitalization unrelated to infection was respiratory distress (25%). Very preterm birth (<32w) (29% vs. 11%; p=0.01) as well as very low birthweight (<1500 g) (34% vs. 16%; p=0.02) occurred more frequently among hospitalized neonates who were HEU. Of those hospitalized, risk of intensive care unit (ICU) admission was higher in neonates who were HEU (53%) compared to HUU (27%) (RR=2.1; 95% CI 1.3–3.3). Adjusted for very preterm birth, the risk of ICU admission remained higher among neonates who were HEU (aRR=1.8; 95% CI 1.1–2.9).
Conclusions:
Neonates who were HEU (vs. HUU) did not have increased all-cause or infection-related hospitalization. However, very preterm birth, very low birthweight and ICU admission were more likely in hospitalized neonates who were HEU, indicating increased severity of neonatal morbidity.
Keywords: HIV, Exposed Uninfected, Infant, Newborn, Hospitalization, Morbidity
Introduction
Substantial progress has been made in the provision of antiretroviral treatment (ART) to pregnant women living with HIV with subsequent reduction in vertical transmission across sub-Saharan Africa. In South Africa, where antenatal HIV prevalence is high (31%) [1] and rates of early vertical transmission are low (<3%) [2], children who are HIV exposed but uninfected (HEU) form a growing population. In 2018, there were an estimated 15 million children who are HEU globally, 13 million resident in sub-Saharan Africa [3].
Infants who are HEU are more likely than those HIV unexposed uninfected (HUU) to be born preterm [4–8], have lower birthweight or be small-for-gestational age [5,9,10]. Preterm birth in turn is a risk factor for infant morbidity and mortality [11]. Maternal ART regimen and timing of initiation may be associated with preterm birth and mortality [12]. Higher rates of preterm birth have been reported in several studies among pregnant women on protease inhibitor(PI)-based ART [13,14] but also in pregnant women on efavirenz or dolutegravir [15]. Increased preterm birth risk may be associated with conception on ART vs. ART initiation after conception [5,16,17], particularly in low- and middle-income countries [18]. While ART is clearly essential to prevent vertical transmission and for maternal heath, safety of ART exposure during pregnancy and conception is not fully established; concerns include possible toxicity and teratogenicity of antiretrovirals [15]. Furthermore, it is difficult to disentangle the effects of HIV vs. ART exposure on fetal development and birth outcomes. Adverse birth outcomes in infants who are HEU are poorly understood but likely to influence health outcomes beyond birth [19].
Infants who are HEU compared to HUU have increased risk of hospitalization in the first year of life [8,20–22], particularly due to infectious morbidity during the first 3–6 months [23–25], and higher mortality, predominantly from infectious causes [26]. Meta-analysis showed that infants who are HEU compared to HUU have a 50% and 70% increased risk of diarrhea and pneumonia, respectively, in the first 6 months of life [27]. Increased risk of infectious morbidity and hospitalization in infants who are HEU is associated with lower maternal CD4 counts [23,28], ART initiation during pregnancy vs. pre-conception [21], elevated delivery maternal viral load (VL) [29,30], poorer maternal education and suboptimal immunization and breastfeeding [22,24,31,32].
More accurate evaluation of the health risks and needs of children who are HEU, particularly in resource-limited settings, has been identified as a research priority [33]. In the pre-ART era, neonatal hospitalization rates differed significantly between infants who were HEU and HUU [34] but in the universal ART era there are few insights into patterns of morbidity, specifically during the neonatal period. We aimed to describe hospitalization patterns in a cohort of neonates who were HEU and HUU and examine maternal and infant factors associated with hospitalization, preterm birth and mortality.
Methods
Study population
We conducted a prospective cohort study of pregnant women and their infants at a large primary maternity care facility (Gugulethu Midwife Obstetric Unit) in a low-income area in Cape Town, South Africa. Between January 2017 and July 2018, consecutive pregnant women aged ≥18 years, with and without HIV, were screened for participation after completing routine antenatal visits. Women were eligible if: (1) they were attending their first antenatal visit during the current pregnancy at the facility (before onset of labor); (2) their HIV status was confirmed through routine testing either previously or at the current visit; (3) they planned to reside with their infants in Cape Town until at least 1 year postpartum; and (4) they provided informed consent to participate and allow researchers to access medical records.
Study procedures
Sources of data included: (1) interview-based measures; (2) clinical assessments; (3) information abstracted from routine electronic data, including laboratory test results; and (4) medical record reviews of hospital admissions. Gestational age at first antenatal visit was estimated, in order of priority, from ultrasound, first date of last menstrual period or symphysis-fundal height. Study visits occurred around routinely scheduled antenatal and postnatal clinic visits and included up to 3 visits during the antenatal period (<28; 28–32; and 34–38 weeks, as allowed by gestation at presentation), and 4 postnatal visits (≤7 days; 10 weeks; 6 months; and 12 months). At the first visit, study counsellors interviewed participants about: previous medical history, including HIV and ART history; gravidity and parity; level of education; type of housing and access to basic household amenities; and alcohol and drug usage. Infant feeding history was assessed at postnatal visits.
Hospitalization of infants was tracked through the provincial hospital admissions system, facilitated by the Western Cape Provincial Health Data Centre (WCPHDC), a health information system which links individuals via a unique health identifier to a range of datasets, including outpatient visits, pharmacy records, laboratory results and hospitalizations [35]. The unique identifier, referred to as the Patient Master Index (PMI), is issued to infants at birth and linked to the maternal PMI, allowing linkage of maternal and infant data and enabling public-sector hospitalizations within the province to be identified electronically. The WCPHDC established an electronic alert system for all enrolled infants, whereby we were notified in real time via daily, automated email alerts of hospitalizations linked to the PMI. Because intention to reside in Cape Town was an inclusion criterion for the study, we anticipated that the majority of hospitalizations would occur in hospitals in Cape Town or surrounding areas. After infants were discharged home, the study doctor reviewed medical records related to hospitalizations among the infant cohort at provincial hospitals. We collected detailed data on reasons for admission and severity of illness using standardized case report forms, which incorporated standardized tools [36–39]. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Cape Town [40,41].
The study was approved by the Western Cape Department of Health’s Provincial Health Research Committee (REF WC_2016RP6_286) and ethics approval was granted by the Human Research Ethics Committee at the University of Cape Town (REF 541/2015 and 749/2015).
Definitions
The primary outcome was hospitalization that commenced during the neonatal period, defined from birth (day 0) up to and including day 28 of life. Although all pregnant women in the study enrolled at the Gugulethu Midwife Obstetric Unit for antenatal care, they delivered their infants at a variety of facilities. In our setting, pregnant women are triaged to different levels of care, from primary care units through to tertiary hospitals, depending on obstetric risk factors, complications and gestational age. Mothers and their neonates routinely stay at birthing facilities for a minimum of 6 hours after uncomplicated vaginal delivery and 48–72 hours after uncomplicated caesarean section. Such periods of routine post-delivery observation are not recorded by the hospital admissions system as infant hospitalizations and were not included in the study as hospitalizations. Well neonates who were in hospital due to maternal conditions/complications were not included as neonatal hospitalizations. In our setting, neonates <35 weeks gestation and <1800g are usually admitted to neonatal units for support, monitoring and/or treatment for possible infection; such periods are recorded as hospitalizations.
For classification of the most common reasons for neonatal hospitalization, we used several case definitions and guidelines developed by the Global Alignment of Immunization Safety Assessment in Pregnancy (GAIA) project, coordinated by the Brighton Collaboration Foundation [36–38]. Each case definition has three levels of evidence which reflect diagnostic certainty (not grades of clinical severity). Level 1 is highly specific for the condition, with a stepwise increase of sensitivity (and reduction in specificity) from level 1 to level 3 (definite/probable/possible). Because our setting has sufficient laboratory diagnostic resources to assess events, we restricted our use of the case definitions to levels 1 and 2. We used GAIA definitions to assign diagnoses of neonatal infections, which includes 3 separate definitions for blood stream infections, meningitis and lower respiratory tract infections [36]. We also used GAIA case definitions for neonatal respiratory distress and neonatal encephalopathy [37,38].
For other infection-related diagnoses not included in GAIA neonatal infections definitions, we used the Pediatric Infectious Event Tool, used in a previous study of infants who were HEU [39]. The tool includes case definitions for classification and grading of infectious diagnoses, including diarrheal disease, skin and mucocutaneous infections, invasive bacterial infections and congenital infections. Case definitions are largely based on criteria from the World Health Organization Integrated Management of Childhood Illnesses and the Division of AIDS Grading of Adult and Paediatric Adverse Events (see supplementary material for definitions).
We defined the following adverse birth outcomes: miscarriage as pregnancy loss <20 weeks gestation; stillbirth as infants born with no signs of life ≥ 20 weeks gestation; preterm birth as infants born alive <37 completed weeks gestation; and very preterm birth as <32 completed weeks gestation. We defined low birthweight as <2500g and very low birthweight as <1500g. We reported on congenital anomalies listed by the Centers for Disease Control and Prevention as ‘major congenital defects,’ tracked by the Metropolitan Atlanta Congenital Defects Program [42].
Maternal CD4 counts were recorded as the result closest to delivery date, within 12 months before or after delivery date. Maternal VL measurement during pregnancy, or within 7 days after delivery, and nearest to delivery date was recorded. Infant polymerase chain reaction (PCR) testing for HIV conducted within the first 7 days of life was regarded as ‘birth PCR’.
Data analysis
We compared characteristics and pregnancy outcomes of women living with and without HIV, as well as characteristics of neonates who are HEU vs. HUU, using the two-sample Z-test for proportions or Fisher’s Exact test if expected cell frequencies were <5. We used the two-sample T-test to compare means between groups. We described non normally distributed data using medians and interquartile ranges (IQR); and used the Wilcoxon sum rank test to compare medians. Among hospitalized infants, we calculated Risk Ratios (RR) for preterm birth, very preterm birth and intensive care unit (ICU) admission. RR confidence intervals were calculated using the Chi-Square test. To assess the effects of multiple pregnancy, preterm birth, low birthweight and twin status on ICU admission, we used the Mantel-Haenszel test to calculate adjusted RRs (aRR). We examined associations of HIV exposure and maternal HIV-related factors with hospitalization-related outcomes, preterm birth and mortality using logistic regression. Maternal age, socio-economic conditions (housing and education) and multiple pregnancy were assigned a priori as potential confounders and were adjusted for in logistic regression models. We excluded: (1) second-born twins and neonates with severe congenital diseases that required urgent surgical intervention from all RR and logistic regression analyses; (2) neonates born in other provinces from analysis of hospitalization-related risks/associations. We performed sensitivity analyses of ICU risks and association with HIV exposure which excluded neonates <650g or <800g (determined by delivery facility and facility-specific eligibility criteria for ICU care). Analyses were performed using Stata 14 (College Station, TX: StataCorp LP).
Results
We enrolled 991 eligible pregnant women (487 living with HIV and 504 without) (Fig. 1). Median gestational age at enrolment was 19 weeks (IQR 13–24). Miscarriage and stillbirth did not differ between women with HIV vs. without (1% vs. 2%, p=0.28; and 2% vs. 3%, p=0.46 respectively). In each group, 3% of mother-infant pairs were lost to follow-up, including women with unknown pregnancy outcomes; and with live births but untraceable infant PMIs (therefore electronic tracking was not possible). Relocation to another province was reported for 70% of those lost to follow-up.
Figure 1: Flow diagram of pregnant women enrolled, pregnancy losses and infants followed up from birth.
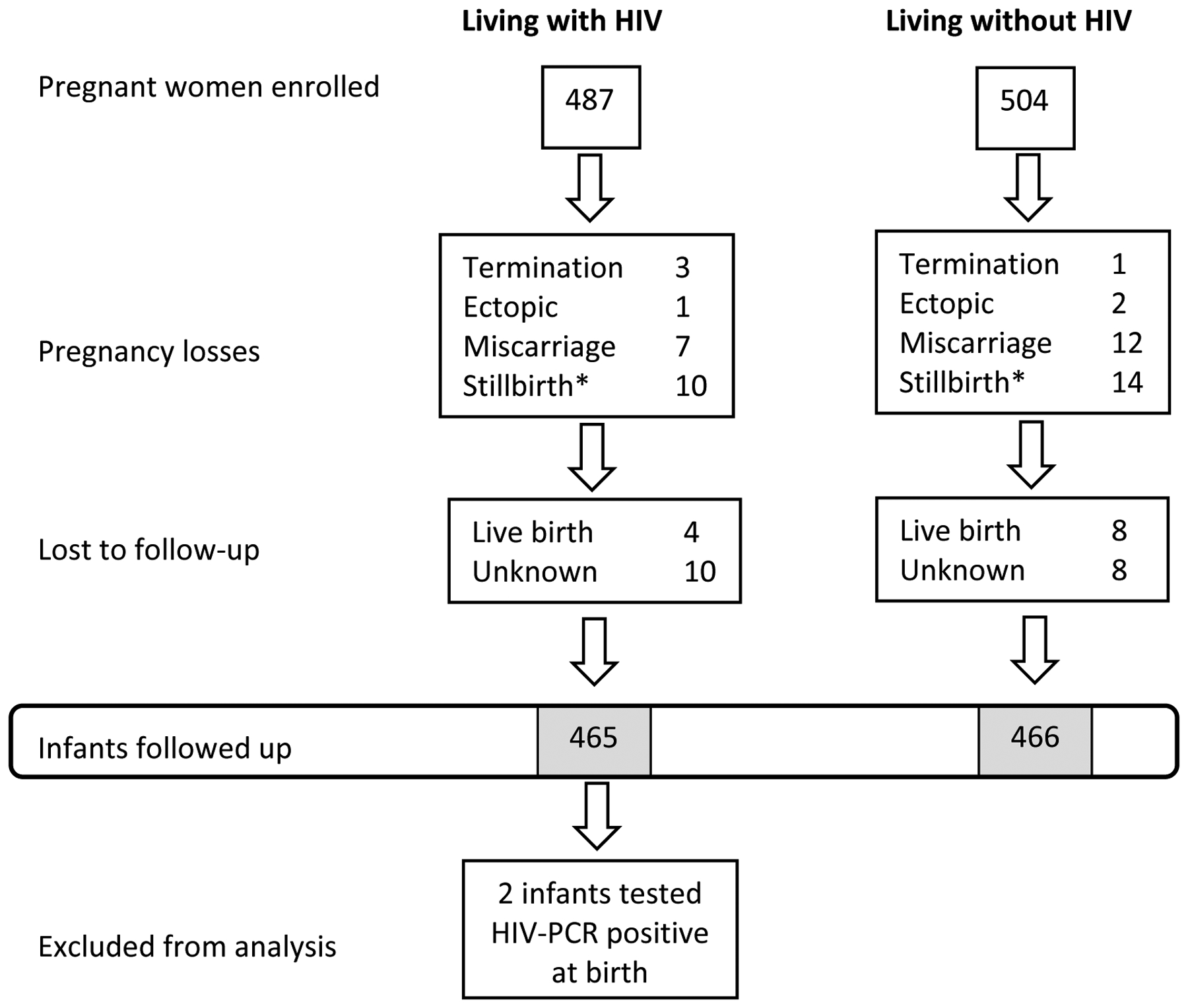
* One woman in each group had a multiple pregnancy that resulted in one twin born alive and the other twin stillborn.
Table 1 shows characteristics of mothers whose infants were followed up (451 living with HIV; 460 without). Women living with HIV were older, fewer had completed secondary schooling, they had higher gravidity and parity, and a larger proportion previously had tuberculosis. Socio-economic conditions, in terms of type of housing, access to household amenities and self-reported use of alcohol and illicit drugs were similar for both groups.
Table 1:
Characteristics of the maternal cohort (n; %)
| Without HIV | With HIV | Total | p-value | ||
|---|---|---|---|---|---|
| Number of mothers | 460 | 451 | 911 | ||
| Age at delivery (mean; 95% CI) | 28.1 (27.6–28.7) | 31.2 (30.6–31.7) | 29.6 (29.2–30.0) | <0.001 | |
| Age <21 years at delivery | 57 (12%) | 13 (3%) | 70 (8%) | <0.001 | |
| Primigravid (n=458; 451) | 121 (26%) | 65 (14%) | 186 (20%) | <0.001 | |
| Parity ≥2 at enrolment (n=458; 451) | 164 (36%) | 223 (49%) | 387 (43%) | <0.001 | |
| Multiple pregnancy (current pregnancy) | 7 (1%) | 13 (3%) | 21 (2%) | 0.161 | |
| Completed secondary schooling (n=457;451) | 182 (40%) | 133 (29%) | 315 (35%) | 0.001 | |
| Resides in shack/informal housing (n=458; 451) | 233 (51%) | 256 (57%) | 489 (54%) | 0.075 | |
| Toilet inside the house (n=458;451) | 152 (33%) | 126 (28%) | 278 (31%) | 0.086 | |
| Running water inside the house (n=458; 451) | 216 (47%) | 190 (42%) | 406 (45%) | 0.127 | |
| Electricity in the house (n=458; 451) | 440 (96%) | 433 (96%) | 873 (96%) | 0.962 | |
| Self-reported alcohol use (at enrolment) (n=457; 450) | Never | 413 (90%) | 407 (90%) | 820 (90%) | 0.867 |
| <5 times/month | 40 (9%) | 41 (9%) | 81 (9%) | ||
| 2–3 times/week | 3 (1%) | 1 (<1%) | 4 (<1%) | ||
| ≥4 times/week | 1 (<1%) | 1 (<1%) | 2 (<1%) | ||
| Self-reported consumption of ≥6 alcoholic drinks on regular occasions (n=456; 449) | Never | 429 (94%) | 422 (94%) | 851 (94%) | 0.981 |
| Monthly or less | 20 (4%) | 20 (4%) | 40 (4%) | ||
| Weekly | 5 (1%) | 5 (1%) | 10 (1%) | ||
| Daily or almost daily | 2 (<1%) | 2 (<1%) | 4 (<1%) | ||
| Self-reported illicit drug use (at enrolment) (n=457; 450) | Never | 456 (99%) | 450 (100%) | 906 (99%) | 0.321 |
| Previous history of tuberculosis (n=458; 451) | 13 (3%) | 79 (18%) | 92 (10%) | <0.001 | |
| ART initiation | Pre-conception | 240 (53%) | |||
| During pregnancy | 122 (27%) | ||||
| ‘Resumed’ during pregnancy | 87 (19%) | ||||
| Post-delivery* | 2 (<1%) | ||||
| CD4 count category (cells/μl) (n=430) | CD4 <200 | 41 (10%) | |||
| CD4 200–349 | 84 (20%) | ||||
| CD4 350–500 | 108 (25%) | ||||
| CD4 >500 | 197 (46%) | ||||
| Time from nearest CD4 to delivery date (days) | (mean; 95% CI) | 136 (131–142) | |||
| Viral load category (copies/ml) (n=432) | VL<40 | 320 (74%) | |||
| VL 40–399 | 60 (14%) | ||||
| VL 400–999 | 8 (2%) | ||||
| VL ≥1000 | 44 (10%) | ||||
| Time from nearest viral load to delivery date (days) | (median; IQR) | 42 (15–69) | |||
Abbreviations – CI: confidence interval; ART: antiretroviral treatment
2 women were HIV-negative at enrolment but tested positive at 6 weeks postpartum: they are included as women with HIV and their infants as HIV exposed)
Among women with HIV: 53% were on ART at conception; 27% initiated ART for the first time at enrolment (during pregnancy); and 19% had evidence of previous ART use but were no longer on treatment, all of whom ‘resumed’ ART during pregnancy. Among women not on ART at conception, 24% commenced/resumed ART in the first trimester, 69% in the second trimester and 7% in the third trimester. The majority of women were taking non-nucleoside reverse transcriptase inhibitors (NNRTIs; 91% efavirenz and 4% nevirapine); whereas 5% were taking PI-based ART at enrolment (5% lopinavir/ritonavir and <0.5% atazanavir). Among women with VL available (96%), 88% had VL<400 copies/ml at the measurement nearest to delivery; mean CD4 count was 492 cells/μl (95% CI 469–514). Fewer women with VL ≥400 copies/ml near delivery had completed secondary schooling compared to those with VL <400 copies/ml (15% vs. 31%; p=0.02). Among the subset of women who resumed ART during pregnancy, compared to those who maintained ART from before conception, fewer had VL<400 copies near delivery (82% vs. 89%; p=0.07), fewer had completed secondary schooling (22% vs. 29%; p=0.19) and more lived in informal housing (60% vs. 55%; p=0.48), without indoor toilets (75% vs. 69%; p=0.30) and without indoor running water (60% vs. 56%; p=0.53).
Table 2 shows the characteristics of neonates with known PMIs (HEU=463; HUU=466), born between February 2017 and January 2019 and followed up from birth. Birth HIV-PCR was recorded in 96% of neonates born to women with HIV. Two neonates tested PCR-positive at birth and were excluded from analysis. Of the 19 HIV-exposed infants who did not have birth PCR testing, 16 had subsequent PCR testing confirming their status as HIV-uninfected, 2 had early neonatal deaths and 1 infant was not tested during the first year of life.
Table 2:
Characteristics of HIV uninfected neonates
| HUU | HEU | Total | p-value | |
|---|---|---|---|---|
| Number | 466 | 463 | 929 | |
| Male | 230 (49%) | 217 (47%) | 447 (48%) | 0.448 |
| Caesarean section delivery | 162 (35%) | 157 (34%) | 319 (34%) | 0.784 |
| Birthweight (g): median (IQR) (n=465;462) | 3200 (2900–3500) | 3110 (2730–3380) | 3160 (2820–3460) | <0.001 |
| Low birthweight (<2500g) (n=465;462) | 58 (12%) | 69 (15%) | 127 (14%) | 0.276 |
| Very low birthweight (<1500g) (n=465;462) | 12 (3%) | 21 (5%) | 33 (4%) | 0.107 |
| Preterm (GA 24–37 weeks) | 53 (11%) | 70 (15%) | 123 (13%) | 0.092 |
| Very preterm (GA <32 weeks) | 8 (2%) | 18 (4%) | 26 (3%) | 0.045 |
| Congenital anomalies | 5* (1%) | 8# (2%) | 13 (1%) | 0.396 |
| Twins | 13 (3%) | 25 (5%) | 39 (4%) | 0.045 |
| Received any breastmilk (n=412;408) | 410 (>99%) | 401 (98%) | 811 (99%) | 0.091 |
| Neonatal hospital admission | 75 (16%) | 62 (13%) | 137 (15%) | 0.245 |
| Neonatal infectious admission | 26 (6%) | 21 (5%) | 47 (5%) | 0.468 |
| Neonatal ICU admission | 20 (4%) | 33 (7%) | 53 (6%) | 0.062 |
| Neonatal ICU/death | 25 (5%) | 35 (8%) | 60 (6%) | 0.174 |
| Death | 7 (2%) | 6 (1%) | 13 (1%) | 0.789 |
Abbreviations - HUU: HIV unexposed uninfected; HEU: HIV exposed uninfected; IQR: interquartile range; GA: gestational age; ICU: intensive care unit
Cornelia de Lange Syndrome, intestinal atresia, thoracic scoliosis and 2 infants with talipes equinovarus
Cerebro-costo-mandibular Syndrome with cleft palate, hypospadias, polydactyly, Klinefelter Syndrome, VACTERL Syndrome, Trisomy 21 and 2 infants with myelomeningocele (one with concurrent talipes equinovarus); (Note: of the 2 HEU infants with neural tube defects: 1 mother used efavirenz at conception; the other stopped ART 3 months prior to conception and resumed efavirenz-based ART in the second trimester)
Median birthweight was lower among neonates who were HEU infants compared to HUU (3110g vs. 3200g; p<0.001). Preterm birth was more common among neonates who were HEU (15% vs. 11%; p=0.09) as well as very preterm birth (4% vs. 2%; p=0.05). Among all neonates born preterm, 63% were hospitalised. There were more twins amongst neonates who were HEU (5% vs. 3%; p=0.04). Among all twins, 68% had low birthweight, 66% were born preterm (24% very preterm), 50% were hospitalized and 11% died. Incidence of congenital defects did not differ between neonates who were HEU vs. HUU.
Overall proportions of all-cause hospitalization and infection-related hospitalization were similar between neonates who were HEU and HUU (13% vs. 16%; p=0.25; and 5% vs. 6%; p=0.47 respectively). Mortality rates did not differ significantly between groups; 11 infants died during hospitalization (2 preterm with major congenital defects and 9 very preterm; 1 low birthweight, 9 very low birthweight and 1 birthweight unknown).Two neonatal deaths were self-reported by mothers in preterm neonates who did not have low birthweight (exact dates and cause of death unknown). Of the 11 hospitalized neonates who died, 5 had infections (4 of whom were admitted to ICU); and 2 neonates without infections were admitted to ICU. Median age at death among hospitalized neonates was 2 days (IQR 0–11); all deaths occurred during the neonatal period except for one infant who was hospitalized since birth with birthweight <1000g and major congenital anomalies and died on day 53 of life.
Most hospitalized neonates were admitted directly after birth or during the post-delivery observation period (87%) (Table 3). Infections were identified in 34% of neonates who were HEU vs. 35% HUU (p=0.92). Most infection-related hospitalizations were associated with definite/probable bloodstream or respiratory infections (89%). Many neonates were documented with ‘presumed sepsis’ but did not meet case definitions for infection (29% HEU vs. 17% HUU; p=0.10). Neonatal respiratory distress was the most common indication for non-infectious hospitalization and did not differ between neonates who were HEU and HUU (41% vs. 35% of non-infectious admissions; p=0.51). Among hospitalized neonates, 29% HEU vs 11% HUU (p=0.01) were very preterm, 34% HEU vs. 16% HUU (p=0.02) were very low birthweight and 53% HEU vs. 27% HUU (p=0.002) required ICU admission. Among all neonates admitted to ICU, 36% were very preterm and 43% very low birthweight.
Table 3:
(A) Characteristics of hospitalized neonates and (B) reasons for hospitalization
| HUU | HEU | Total | p-value | |
|---|---|---|---|---|
| (A) Characteristics | ||||
| Neonatal admissions | 75 | 62 | 137 | |
| Male | 39 (52%) | 32 (52%) | 71 (52%) | 0.964 |
| Birthweight (g): median (IQR) (n=74;62) | 2228 (1655–3240) | 2265 (1340–3180) | 2243 (1503–3215) | 0.541 |
| Low birthweight (<2500g) (n=74;62) | 39 (53%) | 35 (56%) | 74 (54%) | 0.662 |
| Very low birthweight (<1500g) (n=74;62) | 12 (16%) | 21 (34%) | 33 (24%) | 0.017 |
| Preterm (24–37 weeks gestation) | 40 (53%) | 37 (60%) | 77 (56%) | 0.456 |
| Very preterm (<32 weeks gestation) | 8 (11%) | 18 (29%) | 26 (19%) | 0.006 |
| Extremely preterm (<28 weeks gestation) | 5 (7%) | 4 (6%) | 9 (7%) | - |
| Caesarean section delivery | 41 (55%) | 37 (60%) | 78 (57%) | 0.556 |
| Twins | 9 (12%) | 10 (16%) | 19 (14%) | 0.486 |
| Admission duration (days): median (IQR) | 7 (5–17) | 9 (5–28) | 8 (5–20) | 0.131 |
| Admission duration >5 days | 44 (59%) | 45 (73%) | 89 (65%) | 0.089 |
| Admitted on day of birth | 64 (85%) | 55 (89%) | 119 (87%) | 0.560 |
| Congenital abnormalities | 4 (5%) | 7 (11%) | 11 (8%) | 0.202 |
| Neonatal encephalopathy | 4 (5%) | 2 (3%) | 6 (4%) | 0.689 |
| Respiratory Distress of the Neonate | 34 (45%) | 32 (52%) | 66 (48%) | 0.464 |
| Jaundice requiring phototherapy | 19 (25%) | 19 (31%) | 38 (28%) | 0.489 |
| Supplemental oxygen given* | 37 (49%) | 37 (60%) | 74 (54%) | 0.227 |
| Continuous Positive Airway Pressure support given | 21 (28%) | 25 (40%) | 46 (34%) | 0.129 |
| Required intubation and ventilation | 3 (4%) | 4 (6%) | 7 (5%) | 0.701 |
| Received intravenous antibiotics | 41 (55%) | 39 (63%) | 80 (58%) | 0.330 |
| Infection-related hospitalization | 26 (35%) | 21 (34%) | 47 (34%) | 0.922 |
| Intensive Care Unit (ICU) admission (all-cause) | 20 (27%) | 33 (53%) | 53 (39%) | 0.002 |
| Infection-related ICU admission | 13 (17%) | 14 (23%) | 27 (20%) | 0.442 |
| Died during hospitalisation | 7 (9%) | 4 (6%) | 11 (8%) | 0.537 |
| ICU admission or death during hospitalization | 25 (33%) | 33 (53%) | 58 (42%) | 0.019 |
| (B) Reasons for hospitalization | ||||
| (i) Admissions that included an infectious diagnosis: | 26 (35%) | 21 (34%) | 47 (34%) | |
| Neonatal Bloodstream Infection^ | 18 (24%) | 14 (23%) | 32 (23%) | |
| Neonatal Bloodstream Infection^ and Neonatal Respiratory Infection^ | 3 (4%) | 3 (5%) | 6 (13%) | |
| Neonatal Respiratory Infection^ | 1 (1%) | 0 | 1 (1%) | |
| Neonatal Bloodstream Infection^ and Neonatal Meningitis^ | 0 | 1 (2%) | 1 (1%) | |
| Neonatal Bloodstream Infection^ and Necrotising Enterocolitis** | 0 | 1 (2%) | 1 (1%) | |
| Neonatal Bloodstream Infection and Congenital Syphilis** | 0 | 1 (2%) | 1 (1%) | |
| Congenital Tuberculosis** | 0 | 1 (2%) | 1 (1%) | |
| Dysentery## | 1 (1%) | 0 | 1 (<1%) | |
| Urinary Tract Infection## | 1 (1%) | 0 | 1 (<1%) | |
| Acute Diarrhea^^ | 1 (1%) | 0 | 1 (<1%) | |
| Bacterial Skin Infection^^ | 1 (1%) | 0 | 1 (<1%) | |
| (ii) Admissions without an infectious diagnosis: | 49 (65%) | 41 (66%) | 90 (66%) | |
| Congenital anomalies requiring intervention | 1 (1%) | 3 (5%) | 4 (3%) | |
| Respiratory Distress in Term infants | 4 (5%) | 3 (5%) | 7 (5%) | |
| Respiratory Distress in Preterm infants | 13 (17%) | 14 (23%) | 27 (20%) | |
| Other concerns† in Preterm infants | 17 (23%) | 10 (16%) | 27 (20%) | |
| Other concerns† in Term infants | 14 (19%) | 11 (18%) | 25 (18%) |
Abbreviations – HUU: HIV unexposed uninfected; HEU: HIV exposed uninfected; IQR: interquartile range
excluding the first 10 minutes of life
Global Alignment of Immunization Safety Assessment (GAIA) case definitions of Neonatal Infections (Bloodstream/Respiratory/Meningitis): diagnostic certainty was level 2 in all cases, except for 2 infants that met criteria for level 1 infection (Klebsiella pneumonia cultured from blood in an HUU infant and Group B Streptococcus cultured from blood and cerebrospinal fluid in an HEU infant)
Pediatric Infectious Event Tool for Research case definitions and grading:
very severe,
severe,
mild/moderate
Other concerns include jaundice, hypoglycaemia and feeding difficulties
Excluding second-born twins (n=18) and infants with severe congenital anomalies (requiring urgent surgical intervention; n=5), hospitalized neonates who were HEU compared to HUU had twice the risk of ICU admission (RR=2.05; 95% CI 1.28–3.30). ICU admission risk remained higher among neonates who were HEU after separate adjustment for multiple pregnancy (aRR=2.05; 95% CI 1.27–3.30), preterm birth (aRR=2.05; 95% CI 1.28–3.30), very preterm birth (aRR=1.78; 95% CI 1.12–2.85), low birthweight (aRR=2.03; 95% 1.26–3.27) or very low birthweight (aRR=1.79; 95% CI 1.12–2.86). In sensitivity analyses which excluded two neonates <650g and one neonate <800g (as per facility-specific eligibility criteria for ICU care), ICU admission risk remained higher for neonates who were HEU (RR=1.97; 95% CI 1.23–3.15; adjusted for very preterm birth or very low birthweight aRR=1.55; 95% CI 1.00–2.41 and aRR=1.60; 95% CI 1.02–2.50 respectively). Hospitalized neonates who were HEU had increased risk of preterm birth (RR=1.17; 95% CI 0.84–1.62), very preterm birth (RR=2.31; 95% CI 1.05–5.10), low birthweight (RR=1.11; 95% CI 0.79–1.56) and very low birthweight (RR=2.01; 95% CI 1.03–3.93) but not death (RR=0.79; 95% CI 0.20–3.17).
We examined associations of HIV exposure and maternal HIV-related factors with hospitalization-related outcomes using logistic regression, including infants not hospitalised (Table 4). Adjusted for maternal age, education, housing and infant twin status, HIV exposure was not associated with significant increases in neonatal hospitalization (aOR=0.65; 95% CI 0.43–0.97), infection-related admission (aOR=0.65; 95% CI 0.33–1.25), ICU admission (aOR=1.50; 95% 0.79–2.85), death (aOR=0.90; 95% CI 0.23–3.42), preterm birth (aOR=1.12; 95% CI 0.73–1.73), very preterm birth (aOR=1.55; 95% CI 0.60–3.96), low birthweight (aOR=1.00; 95% CI 0.66–1.54) or very low birthweight (aOR=1.36; 95% CI 0.60–3.09). In sensitivity analysis which excluded neonates ineligible for ICU admission based on birthweight, the association of HIV exposure with ICU admission was unchanged (aOR=1.47; 95% 0.78–2.79). Among neonates who were HEU, increased odds of preterm birth were associated with maternal use of PI- vs. NNRTI-based regimens (aOR=5.08; 95% CI 1.90–13.58) and ART initiation/resumption in the first trimester vs. on ART at conception (aOR=3.38; 95% CI 1.37–8.33). Maternal viremia (VL>400 copies/ml) was associated with very preterm delivery (aOR=6.30; 95% CI 1.28–30.96).
Table 4:
Logistic regression models assessing (A) the association of HIV exposure with different outcomes of interest among neonates HIV exposed uninfected (HEU) and HIV unexposed uninfected and (B) the association of maternal HIV-related factors with different outcomes of interest among neonates HEU
| (A) | Neonatal admission (N=894)* |
Neonatal infection-related admission (N=894)* |
Neonatal ICU admission (N=894)* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| uaOR | 95% CI | aOR | 95% CI | uaOR | 95% CI | aOR | 95% CI | uaOR | 95% CI | aOR | 95% CI | |
| HIV exposure | 0.74 | (0.50–1.08) | 0.65 | (0.43–0.97) | 0.75 | (0.40–1.41) | 0.65 | (0.33–1.25) | 1.62 | (0.88–2.97) | 1.50 | (0.79–2.85) |
| Maternal age (years) | 1.03 | (0.99–1.06) | 1.03 | (1.00–1.07) | 1.02 | (0.97–1.07) | 1.02 | (0.97–1.08) | 1.01 | (0.96–1.06) | 1.00 | (0.94–1.05) |
| Maternal education (secondary schooling completed) | 0.95 | (0.64–1.43) | 0.95 | (0.63–1.44) | 0.83 | (0.43–1.63) | 0.79 | (0.40–1.56) | 0.81 | (0.43–1.54) | 0.84 | (0.43–1.63) |
| Reside in formal housing (vs informal) | 0.89 | (0.61–1.31) | 0.90 | (0.60–1.33) | 1.17 | (0.63–2.18) | 1.21 | (0.64–2.27) | 0.89 | (0.49–1.62) | 0.95 | (0.51–1.75) |
| Twin | 6.76 | (2.75–16.60) | 6.28 | (2.47–15.96) | 5.52 | (1.76–17.31) | 6.19 | (1.92–19.94) | 6.80 | (2.36–19.61) | 6.90 | (2.33–20.40) |
| Preterm birth (N=903)# |
Very preterm birth (N=903)# |
Death (N=903)# |
||||||||||
| uaOR | 95% CI | aOR | 95% CI | uaOR | 95% CI | aOR | 95% CI | uaOR | 95% CI | aOR | 95% CI | |
| HIV exposure | 1.35 | (0.90–2.02) | 1.12 | (0.73–1.73) | 1.82 | (0.76–4.39) | 1.55 | (0.60–3.96) | 1.03 | (0.30–3.57) | 0.90 | (0.23–3.42) |
| Maternal age (years) | 1.05 | (1.02–1.09) | 1.04 | (1.00–1.08) | 1.03 | (0.96–1.11) | 1.00 | (0.93–1.09) | 1.04 | (0.94–1.16) | 1.04 | (0.93–1.16) |
| Maternal education (secondary schooling completed) | 0.69 | (0.44–1.07) | 0.69 | (0.43–1.10) | 0.69 | (0.27–1.79) | 0.67 | (0.25–1.82) | 1.25 | (0.35–4.45) | 1.01 | (0.27–3.81) |
| Reside in formal housing (vs informal) | 1.05 | (0.70–1.56) | 1.16 | (0.76–1.76) | 1.17 | (0.50–2.72) | 1.36 | (0.56–3.31) | 4.72 | (1.00–22.36) | 5.11 | (1.04–25.06) |
| Twin | 15.28 | (5.95–39.24) | 13.25 | (5.01–35.01) | 17.034 | (5.56–52.23) | 17.56 | (5.49–56.13) | 12.19 | (2.42–61.51) | 13.42 | (2.47–73.02) |
| (B) | Preterm birth (N=402)# |
Very preterm birth (N=402)# |
Neonatal ICU admission (N=400)* |
|||||||||
| uaOR | 95% CI | aOR^ | 95% CI | uaOR | 95% CI | aOR† | 95% CI | uaOR | 95% CI | aOR† | 95% CI | |
| Maternal age (years) | 1.06 | (1.01–1.11) | 1.06 | (0.99–1.12) | 1.02 | (0.93–1.13) | 1.04 | (0.92–1.17) | 1.01 | (0.94–1.08) | 1.02 | (0.94–1.00) |
| Maternal education (secondary schooling completed) | 0.74 | (0.40–1.38) | 0.40 | (0.18–0.88) | 0.38 | (0.08–1.74) | 0.34 | (0.07–1.69) | 0.64 | (0.25–1.61) | 0.52 | (0.18–1.47) |
| Reside in formal housing (vs informal) | 0.97 | (0.56–1.68) | 1.20 | (0.64–2.26) | 0.99 | (0.34–2.89) | 1.36 | (0.41–4.50) | 0.85 | (0.39–1.86) | 1.16 | (0.50–2.70) |
| Twin | 11.50 | (3.62–36.46) | 13.69 | (3.70–50.75) | 18.84 | (4.96–71.56) | 22.78 | (4.26–121.67) | 7.56 | (2.17–26.31) | 6.07 | (1.41–26.19) |
| Receiving ART at conception | 1 | 1 | 1 | |||||||||
| Initiated ART during pregnancy | 0.77 | (0.39–1.53) | 1.12 | (0.32–3.91) | 1.86 | (0.79–4.34) | ||||||
| Previous ART history, resumed ART during pregnancy | 1.52 | (0.79–2.94) | 1.23 | (0.31–4.86) | 1.19 | (0.41–3.47) | ||||||
| Receiving ART at conception | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| Initiated/resumed ART in first trimester | 2.10 | (0.99–4.44) | 3.38 | (1.37–8.33) | 2.95 | (0.83–10.48) | 3.80 | (0.79–18.28) | 3.13 | (1.16–8.40) | 2.68 | (0.83–8.62) |
| Initiated/resumed ART in second trimester | 0.71 | (0.36–1.38) | 0.76 | (0.35–1.67) | 0.72 | (0.18–2.81) | 0.65 | (0.15–2.86) | 1.27 | (0.52–3.09) | 1.13 | (0.42–3.00) |
| Initiated/resumed ART in third trimester | 1.62 | (0.43–6.05) | - | - | - | - | - | |||||
| CD4 ≥200 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| CD4 <200 | 1.60 | (0.70–3.65) | 0.90 | (0.30–2.66) | 0.78 | (0.10–6.17) | 0.33 | (0.04–3.04) | 1.78 | (0.58–5.45) | 0.99 | (0.25–3.90) |
| CD4>500 | 1 | 1 | 1 | |||||||||
| CD4 350–499 | 0.93 | (0.46–1.89) | 0.23 | (0.03–1.84) | 0.51 | (0.16–1.60) | ||||||
| CD4 200–349 | 1.10 | (0.52–2.29) | 0.88 | (0.23–3.38) | 0.65 | (0.21–2.03) | ||||||
| CD4 <200 | 1.59 | (0.66–3.83) | 0.59 | (0.07–4.86) | 1.40 | (0.44–4.49) | ||||||
| VL <400 before delivery | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| VL ≥400 before delivery | 1.31 | (0.58–2.95) | 2.29 | (0.84–6.20) | 2.08 | (0.56–7.72) | 6.30 | (1.28–30.96) | 0.91 | (0.27–3.15) | 1.40 | (0.36–5.51) |
| VL <40 before delivery | 1 | 1 | 1 | |||||||||
| VL 40–399 | 1.30 | (0.59–2.84) | - | 0.74 | (0.21–2.55) | |||||||
| VL 400–999 | 2.45 | (0.48–12.56) | 3.97 | (0.45–35.15) | 2.00 | (0.23–17.03) | ||||||
| VL ≥1000 | 1.19 | (0.47–3.01) | 1.36 | (0.29–6.34) | 0.68 | (0.15–3.02) | ||||||
| NNRTI-based regimen | 1 | 1 | - | - | ||||||||
| PI-based regimen | 4.57 | (1.89–11.10) | 5.08 | (1.90–13.58) | - | - | ||||||
Abbreviations - ICU: intensive care unit; uaOR: unadjusted odds ratio; CI: confidence interval; aOR: adjusted odds ratio; ART: antiretroviral treatment; VL: viral load; NNRTI: non-nucleoside reverse transcriptase inhibitor; PI: protease inhibitor
excluding neonates born in other provinces (n=7;2), second-born twins (n=6;12) and neonates with severe congenital anomalies requiring urgent surgical intervention (n=1;4: intestinal atresia; imperforate anus; 2 x myelomeningocele; cleft palate)
excluding second-born twins (n=6;12) and neonates with severe congenital anomalies requiring urgent surgical intervention (n=1;4)
third trimester ART initiation could not be included in the adjusted model as it predicted preterm delivery perfectly (zero events)
regimen type and third trimester ART initiation could not be included in the adjusted model as they predicted very preterm delivery and ICU admission perfectly (zero events)
Discussion
Among hospitalized neonates, those HEU had twice the risk of ICU admission compared to those HUU, even after adjustment for prematurity or birthweight; an indication of more severe morbidity in this group. While it is reassuring that in the entire cohort, neonates who were HEU did not have increased risk of all-cause or infection-related hospitalization, preterm birth, ICU admission or death, the increased ICU admission in hospitalized neonates may have important implications for health services, as an emerging very preterm HEU population would demand improved neonatal intensive care services, which are scarce in sub-Saharan Africa [43]. In our setting, high quality neonatal and particularly ICU care may have mitigated increased mortality despite increased morbidity, whereas in other resource-limited settings circumstances may differ [44].
Increased preterm birth and especially very preterm birth among neonates who are HEU may contribute to worse morbidity, as they are prone to complications from, for example, immature respiratory, gastrointestinal, metabolic and immune systems and may therefore require more advanced care, as reflected by the need for ICU admission, and longer duration of hospital stay, which places an increased burden on health services. Optimising maternal health by initiating ART before pregnancy and maintaining viral suppression during pregnancy may help mitigate against preterm birth. Whereas other studies have found an association with preterm birth and conception on ART [5,16–18], in this cohort, women who were on ART at conception were less likely to deliver preterm than women who initiated ART in the first trimester (but there were no significant differences if ART was initiated in the second trimester). The role of timing of ART initiation and optimal ART regimen warrants further study in larger cohorts, especially as dolutegravir use becomes widespread. Our finding that PI use is associated with preterm birth is similar to previous studies [13,14].
Improved health in women living with HIV may account for the observed reduction in neonatal hospitalization rates among those HEU in comparison with the pre-ART era, when neonatal period hospitalization rates differed significantly (IRR=1.5; 95% CI 1.2–2.0 for all-cause hospitalization; IRR=2.7; 95% CI 1.6 – 4.7 for lower respiratory tract infection hospitalizations) [34]. The causal mechanisms by which HIV and/or ART exposure predispose infants to adverse birth outcomes and worse morbidity should continue to be explored, although associations may be confounded. In the context of widespread, easily accessible maternal ART, women who are not on ART at conception, do not maintain suppressed VL and/or have stopped ART prior to pregnancy may have a range of other risk factors for poor birth outcomes independent of HIV and ART status, particularly those related to low socioeconomic status, such as lack of social support, domestic violence, smoking or other sexually transmitted infections [45]. While ART initiation and maintenance before pregnancy and interventions to improve adherence and viral suppression may directly, biologically improve infant outcomes, it is likely that broader support for other risk factors for poor outcomes in these women may be important for optimizing infant outcomes. Although differences in housing and access to indoor toilets and running water were not significant, women with HIV, and in particular the subset who resumed ART during pregnancy, had poorer living conditions and level of education. ART-related interventions alone may not address the range of risk factors for poor infant outcomes; addressing poverty and structural inequalities (education, housing etc.) will likely improve maternal and child health outcomes.
Unique strengths of this study are the ability to examine: (1) the neonatal period specifically; (2) in contemporaneous cohorts of neonates who are HEU and HUU; (3) during the universal ART era; (4) with standardized outcome definitions applied systematically by a neutral observer and not relying on the treating clinicians’ diagnoses. Neonates who were HEU and HUU were hospitalized with similar frequency, therefore “over-hospitalization bias”, whereby HEU neonates may be hospitalized as a “precautionary measure”, is unlikely. As there is limited availability of neonatal ICU beds in our context [46], precautionary admission to ICU for neonates who are HIV-exposed is also extremely unlikely. A previous study similarly found that HIV-exposed preterm neonates have increased risk of invasive ventilation [47]. Antenatal recruitment of women reduced potential bias, compared to postnatal recruitment in which acutely ill neonates or those with serious adverse birth outcomes are more likely to be excluded. The 2 groups of pregnant women were comparable; all resided in the same area and in similar socio-economic conditions. We were able to track hospitalizations electronically within the province and therefore loss to follow-up and missing information on hospitalizations in the province was minimal. While we may have missed hospitalization/deaths that occurred in other provinces of South Africa and non-hospitalized deaths, this risk is likely small in the neonatal period as women were unlikely to leave Cape Town in such a short time window and because >99% of women deliver in facilities in our setting. Almost all pregnant women in our setting plan to deliver in a facility, which is very different from the rest of sub-Saharan Africa. Our findings are representative of urban South Africa but generalizability is limited as our setting is not representative of rural South Africa or other sub-Saharan African countries where access to neonatal intensive care services may be lacking. Timing and exclusiveness of breastfeeding were not examined. Precision of point estimates was limited as the study was originally powered to compare infant hospitalization frequency over 12 months, not neonatal events specifically. Crude increases observed in preterm birth, very preterm birth and ICU admission among neonates who were HEU vs. HUU were not shown as significant associations using logistic regression; this may be due to limited sample size.
Conclusion
Neonates who were HEU compared to HUU did not have increased overall preterm birth, all-cause hospitalization or infection-related hospitalization. However, very preterm birth, very low birthweight and ICU admission were more likely in hospitalized neonates who were HEU, indicating increased severity of morbidity during the neonatal period.
Supplementary Material
Acknowledgements
The mothers, infants and Western Cape service providers are acknowledged. We thank the Western Cape Provincial Health Data Centre for collating and sharing data.
Funding
The project was supported by Grant Number R01HD080465 from NIH (NICHD); PI: A Boulle.
Footnotes
Conflicts of Interest: No conflicts of interest are declared by the authors.
References
- 1.Woldesenbet SA, Kufa T, Lombard C, Manda S, Ayalew K, Cheyip M, et al. The 2017 National Antenatal Sentinel HIV Survey Key Findings, South Africa, National Department of Health [NICD website]. July 2019. Available at: https://www.nicd.ac.za/wp-content/uploads/2019/07/Antenatal_survey-report_24July19.pdf. Accessed August 12, 2020.
- 2.Sherman GG, Lilian RR, Bhardwaj S, Candy S, Barron P. Laboratory information system data demonstrate successful implementation of the prevention of mother-to-child transmission programme in South Africa. South African Med J 2014. January 20;104(3):235. [DOI] [PubMed] [Google Scholar]
- 3.Slogrove AL, Powis KM, Johnson LF, Stover J, Mahy M. Estimates of the global population of children who are HIV-exposed and uninfected, 2000–18: a modelling study. Lancet Glob Heal 2020. January 1;8(1):e67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans C, Humphrey JH, Ntozini R, Prendergast AJ. HIV-Exposed Uninfected Infants in Zimbabwe: Insights into Health Outcomes in the Pre-Antiretroviral Therapy Era. Front Immunol 2016. June 6;7:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen JY, Ribaudo HJ, Souda S, Parekh N, Ogwu A, Lockman S, et al. Highly active antiretroviral therapy and adverse birth outcomes among HIV-infected women in Botswana. J Infect Dis 2012. December 1;206(11):1695–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malaba TR, Phillips T, Le Roux S, Brittain K, Zerbe A, Petro G, et al. Antiretroviral therapy use during pregnancy and adverse birth outcomes in South African women. Int J Epidemiol 2017. October 1;46(5):1678–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wedi COO, Kirtley S, Hopewell S, Corrigan R, Kennedy SH, Hemelaar J. Perinatal outcomes associated with maternal HIV infection: a systematic review and meta-analysis. Lancet HIV 2016. January;3(1):e33–48. [DOI] [PubMed] [Google Scholar]
- 8.Labuda SM, Huo Y, Kacanek D, Patel K, Huybrechts K, Jao J, et al. Rates of Hospitalization and Infection-Related Hospitalization Among Human Immunodeficiency Virus (HIV)-Exposed Uninfected Children Compared to HIV-Unexposed Uninfected Children in the United States, 2007–2016. Clin Infect Dis 2020. July 11;71(2):332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dara JS, Hanna DB, Anastos K, Wright R, Herold BC. Low birth weight in human immunodeficiency virus–exposed uninfected infants in Bronx, New York. J Pediatric Infect Dis Soc 2018;7(2):E24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santosa WB, Staines-Urias E, Tshivuila-Matala COO, Norris SA, Hemelaar J. Perinatal outcomes associated with maternal HIV and antiretroviral therapy in pregnancies with accurate gestational age in South Africa. AIDS 2019;33(10):1623–33. [DOI] [PubMed] [Google Scholar]
- 11.Frey HA, Klebanoff MA. The epidemiology, etiology, and costs of preterm birth. Semin Fetal Neonatal Med 2016. April;21(2):68–73. [DOI] [PubMed] [Google Scholar]
- 12.Sebikari D, Farhad M, Fenton T, Owor M, Stringer JSA,Qin M, et al. Risk Factors for Adverse Birth Outcomes in the PROMISE 1077BF/1077FF Trial. J Acquir Immune Defic Syndr 2019;81(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powis KM, Kitch D, Ogwu A, Hughes MD, Lockman S, Leidner J, et al. Increased risk of preterm delivery among HIV-infected women randomized to protease versus nucleoside reverse transcriptase inhibitor-based HAART during pregnancy. J Infect Dis 2011. August 15;204(4):506–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sibiude J, Warszawski J, Tubiana R, Dollfus C, Faye A, Rouzioux C, et al. Premature Delivery in HIV-Infected Women Starting Protease Inhibitor Therapy During Pregnancy: Role of the Ritonavir Boost? Clin Infect Dis 2012. May 1;54(9):1348–60. [DOI] [PubMed] [Google Scholar]
- 15.Zash R, Jacobson DL, Diseko M, Mayondi G, Mmalane M, Essex M, et al. Comparative Safety of Antiretroviral Treatment Regimens in Pregnancy. JAMA Pediatr 2017. October 2;171(10):e172222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kourtis AP, Schmid CH, Jamieson DJ, Lau J. Use of antiretroviral therapy in pregnant HIV-infected women and the risk of premature delivery: a meta-analysis. AIDS 2007. March 12;21(5):607–15. [DOI] [PubMed] [Google Scholar]
- 17.Li N, Sando MM, Spiegelman D, Hertzmark E, Liu E, Sando D, et al. Antiretroviral Therapy in Relation to Birth Outcomes among HIV-infected Women: A Cohort Study. J Infect Dis 2016. April 1;213(7):1057–64. [DOI] [PubMed] [Google Scholar]
- 18.Uthman OA, Nachega JB, Anderson J, Kanters S, Mills EJ, Renaud F, et al. Timing of initiation of antiretroviral therapy and adverse pregnancy outcomes: a systematic review and meta-analysis. Lancet HIV 2017;4(1):e21–30. [DOI] [PubMed] [Google Scholar]
- 19.Goga A, Slogrove A, Wedderburn CJ, Feucht U, Wessels J, Ramokolo V, et al. The impact of health programmes to prevent vertical transmission of HIV. Advances, emerging health challenges and research priorities for children exposed to or living with HIV: Perspectives from South Africa. S Afr Med J 2019. December 5;109(11b):77–82. [DOI] [PubMed] [Google Scholar]
- 20.Slogrove A, Reikie B, Naidoo S, De Beer C, Ho K, Cotton M, et al. HIV-Exposed Uninfected Infants are at Increased Risk for Severe Infections in the First Year of Life. J Trop Pediatr 2012. December 1;58(6):505–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goetghebuer T, Smolen KK, Adler C, Das J, McBride T, Smits G, et al. Initiation of Antiretroviral Therapy Before Pregnancy Reduces the Risk of Infection-related Hospitalization in Human Immunodeficiency Virus–exposed Uninfected Infants Born in a High-income Country. Clin Infect Dis 2019. March 19;68(7):1193–203. [DOI] [PubMed] [Google Scholar]
- 22.Rupérez M, González R, Maculuve S, Quintó L, López-Varela E, Augusto O, et al. Maternal HIV infection is an important health determinant in non-HIV-infected infants. AIDS 2017. July;31(11):1545–53. [DOI] [PubMed] [Google Scholar]
- 23.Kuhn L, Kasonde P, Sinkala M, Kankasa C, Semrau K, Scott N, et al. Does Severity of HIV Disease in HIV-Infected Mothers Affect Mortality and Morbidity among Their Uninfected Infants? Clin Infect Dis 2005. December 1;41(11):1654–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.le Roux SM, Abrams EJ, Donald KA, Brittain K, Phillips TK, Zerbe A, et al. Infectious morbidity of breastfed, HIV-exposed uninfected infants under conditions of universal antiretroviral therapy in South Africa: a prospective cohort study. Lancet Child Adolesc Heal 2020. January 10; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.von Mollendorf C, von Gottberg A, Tempia S, Meiring S, de Gouveia L, Quan V, et al. Increased Risk for and Mortality From Invasive Pneumococcal Disease in HIV-Exposed but Uninfected Infants Aged <1 Year in South Africa, 2009–2013. Clin Infect Dis 2015. May 1;60(9):1346–56. [DOI] [PubMed] [Google Scholar]
- 26.Brennan AT, Bonawitz R, Gill CJ, Thea DM, Kleinman M, Useem J, et al. A meta-analysis assessing all-cause mortality in HIV-exposed uninfected compared with HIV-unexposed uninfected infants and children. AIDS 2016. September;30(15):2351–60. [DOI] [PubMed] [Google Scholar]
- 27.Brennan AT, Bonawitz R, Gill CJ, Thea DM, Kleinman M, Long L, et al. A Meta-analysis Assessing Diarrhea and Pneumonia in HIV-Exposed Uninfected Compared With HIV-Unexposed Uninfected Infants and Children. J Acquir Immune Defic Syndr 2019;82(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taron-Brocard C, Le Chenadec J, Faye A, Dollfus C, Goetghebuer T, Gajdos V, et al. Increased Risk of Serious Bacterial Infections Due to Maternal Immunosuppression in HIV-Exposed Uninfected Infants in a European Country. Clin Infect Dis 2014. November 1;59(9):1332–45. [DOI] [PubMed] [Google Scholar]
- 29.Weinberg A, Mussi-Pinhata MM, Yu Q, Cohen RA, Almeida VC, Amaral FR, et al. Factors Associated with Lower Respiratory Tract Infections in HIV-Exposed Uninfected Infants. AIDS Res Hum Retroviruses 2018;34(6):527–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yeganeh N, Watts DH, Xu J, Kerin T, Joao EC, Pilotto JH, et al. Infectious Morbidity, Mortality and Nutrition in HIV-Exposed, Uninfected, Formula Fed Infants. Pediatr Infect Dis J 2018. May 10;37:1271–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ásbjörnsdóttir KH, Slyker JA, Maleche-Obimbo E, Wamalwa D, Otieno P, Gichuhi CM, et al. Breastfeeding Is Associated with Decreased Risk of Hospitalization among HIV-Exposed, Uninfected Kenyan Infants. J Hum Lact 2016;32(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bork KA, Cournil A, Read JS, Newell M-L, Cames C, Meda N, et al. Morbidity in relation to feeding mode in African HIV-exposed, uninfected infants during the first 6 mo of life: the Kesho Bora study. Am J Clin Nutr 2014. December;100(6):1559–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mofenson LM. New challenges in the elimination of pediatric HIV infection: The expanding population of HIV-exposed but uninfected children [Editorial Commentary]. Clin Infect Dis 2015. May 1; 60:1357–60. [DOI] [PubMed] [Google Scholar]
- 34.Koyanagi A, Humphrey JH, Ntozini R, Nathoo K, Moulton LH, Iliff P, et al. Morbidity among human immunodeficiency virus-exposed but uninfected, human immunodeficiency virus-infected, and human immunodeficiency virus-unexposed infants in Zimbabwe before availability of highly active antiretroviral therapy. Pediatr Infect Dis J 2011. January;30(1):45–51. [DOI] [PubMed] [Google Scholar]
- 35.Boulle A, Heekes A, Tiffin N, Smith M, Mutemaringa T, Zinyakatira N, et al. Data Centre Profile: The Provincial Health Data Centre of the Western Cape Province, South Africa. Int J Popul Data Sci 2019. November 20;4(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vergnano S, Buttery J, Cailes B, Chandrasekaran R, Chiappini E, Clark E, et al. Neonatal infections: Case definition and guidelines for data collection, analysis, and presentation of immunisation safety data. Vaccine 2016;34(49):6038–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sweet LR, Keech C, Klein NP, Marshall HS, Tagbo BN, Quine D, et al. Respiratory distress in the neonate: Case definition & guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine 2017. December 4;35(48):6506–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sell E, Munoz FM, Soe A, Wiznitzer M, Heath PT, Clarke ED, et al. Neonatal encephalopathy: Case definition & guidelines for data collection, analysis, and presentation of maternal immunisation safety data. Vaccine 2017;35(48 Pt A):6501–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slogrove AL, Esser MM, Cotton MF, Speert DP, Kollmann TR, Singer J, et al. A Prospective cohort study of common childhood infections in South African HIV-exposed uninfected and HIV-unexposed infants. Pediatr Infect Dis J 2017;36(2):e38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009. April;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Metropolitan Atlanta Congenital Defects Program: MACDP 6-Digit Code Defect List [CDC website]. Available at: https://www.cdc.gov/ncbddd/birthdefects/macdp.html. Accessed July 17, 2020.
- 43.Argent AC. Critical care in Africa. South African J Crit Care 2009. July;25(1):4–8. [Google Scholar]
- 44.Dünser MW, Baelani I, Ganbold L. A review and analysis of intensive care medicine in the least developed countries. Critical Care Medicine 2006;34:1234–42. [DOI] [PubMed] [Google Scholar]
- 45.Eunice Kennedy Shriver National Institute of Child Health and Human Development. What are the risk factors for preterm labor and birth [NICHD website]? Available at: https://www.nichd.nih.gov/health/topics/preterm/conditioninfo/who_risk. Accessed November 4, 2020.
- 46.Lloyd LG, de Witt TW. Neonatal mortality in South Africa: How are we doing and can we do better? South African Med J 2013;103:518–9. [DOI] [PubMed] [Google Scholar]
- 47.Riemer LJ, Le Roux SM, Harrison MC, Tooke L. Short-term outcomes of HIV-exposed and HIV-unexposed preterm, very low birthweight neonates: a longitudinal, hospital-based study. J Perinatol 2020. March 31;40(3):445–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


