Abstract
Objective
To investigate the feasibility and the accuracy of the coronary CT angiography (CCTA)-derived Registry of Crossboss and Hybrid procedures in France, the Netherlands, Belgium and United Kingdom (RECHARGE) score (RECHARGECCTA) for the prediction of procedural success and 30-minutes guidewire crossing in percutaneous coronary intervention (PCI) for chronic total occlusion (CTO).
Materials and Methods
One hundred and twenty-four consecutive patients (mean age, 54 years; 79% male) with 131 CTO lesions who underwent CCTA before catheter angiography (CA) with CTO-PCI were retrospectively enrolled in this study. The RECHARGECCTA scores were calculated and compared with RECHARGECA and other CTA-based prediction scores, including Multicenter CTO Registry of Japan (J-CTO), CT Registry of CTO Revascularisation (CT-RECTOR), and Korean Multicenter CTO CT Registry (KCCT) scores.
Results
The procedural success rate of the CTO-PCI procedures was 72%, and 61% of cases achieved the 30-minutes wire crossing. No significant difference was observed between the RECHARGECCTA score and the RECHARGECA score for procedural success (median 2 vs. median 2, p = 0.084). However, the RECHARGECCTA score was higher than the RECHARGECA score for the 30-minutes wire crossing (median 2 vs. median 1.5, p = 0.001). The areas under the curve (AUCs) of the RECHARGECCTA and RECHARGECA scores for predicting procedural success showed no statistical significance (0.718 vs. 0.757, p = 0.655). The sensitivity, specificity, positive predictive value, and the negative predictive value of the RECHARGECCTA scores of ≤ 2 for predictive procedural success were 78%, 60%, 43%, and 87%, respectively. The RECHARGECCTA score showed a discriminative performance that was comparable to those of the other CTA-based prediction scores (AUC = 0.718 vs. 0.665–0.717, all p > 0.05).
Conclusion
The non-invasive RECHARGECCTA score performs better than the invasive determination for the prediction of the 30-minutes wire crossing of CTO-PCI. However, the RECHARGECCTA score may not replace other CTA-based prediction scores for predicting CTO-PCI success.
Keywords: Coronary artery disease, Coronary angiography, Percutaneous coronary intervention, Computed tomography angiography
INTRODUCTION
Coronary chronic total occlusion (CTO) percutaneous coronary intervention (PCI) is associated with lower procedural success (CTO vs. non-CTO, 55–80% vs. 90–99%) and higher complication rates (CTO vs. non-CTO, 1.6% vs. 0.8%) than non-CTO-PCI [1]. Compared with failed CTO-PCI, successful PCI has been associated with improvement in angina, left ventricular function, and increased survival [2,3]. Procedural success is associated with several CTO lesion morphological characteristics and surgeon experience [1]. A pre-procedural evaluation of CTO lesion characteristics may facilitate better clinical decision making and procedural planning [4], which will increase the likelihood of overall success of CTO-PCI [5]. Some predictive scoring tools based on catheter angiography (CA) findings, such as the Multicenter CTO Registry of Japan (J-CTO) score [6,7], clinical and lesion-related score (CL-score) [8], Prospective Global Registry for the study of Chronic Total Occlusion Intervention (PROGRESS) score [9], and Registry of Crossboss and Hybrid procedures in France, the Netherlands, Belgium and United Kingdom (RECHARGE) score [10], have been introduced to describe the complexity of the CTO lesion for appropriate patient selection and pre-procedural intervention planning of CTO-PCI. As the RECHARGE score is based on hybrid CTO procedures, it has demonstrated better capacity for predicting the technical outcomes and the feasibility of different levels of surgery than the J-CTO and PROGRESS scores [5,10].
Coronary CT angiography (CCTA), a non-invasive imaging technique, can characterize the features of the CTO segment, which is a notable advantage over CA for the assessment of longer and more tortuous CTO lesions, as well as segments distal to a CTO lesion [11]. Moreover, it can provide prognostic information beyond CA [12,13,14,15,16,17], and it has been investigated as an alternative pre-procedural imaging method for CTO-PCI [18]. However, it is unclear whether the RECHARGE score can be calculated using CCTA data.
Thus, the aim of the present study was to investigate the feasibility and predictive value of the CCTA-derived RECHARGE score (RECHARGECCTA) and compare it with CA (RECHARGECA) and other pre-procedural tools for predicting procedural success and guidewire crossing within 30-minutes in CTO-PCI.
MATERIALS AND METHODS
Study Population
This single-center study was approved by the local Institutional Review Board, and written informed consent was obtained from each patient (IRB No. LS2018-001). The study was performed in compliance with the HIPAA regulations. One hundred and twenty-four patients (mean age, 54 years; 79% male, 131 CTO lesions) who underwent CCTA before elective interventional CTO recanalization at the institution were retrospectively enrolled in this study. CTO was defined as a native coronary artery occlusion (antegrade flow of the Thrombolysis in Myocardial Infarction [TIMI] = 0) that had lasted for ≥ 3 months. The exclusion criteria included previous reaction to iodine contrast media, renal failure (glomerular filtration rate < 30 mL/min/1.73 m2), pregnancy, and previously implanted stents located at the occlusion site. Covariates, including cardiac risk factors and patient baseline characteristics, were obtained from the medical records.
CCTA Acquisition Protocol
A dual-source CT scanner (Somatom Definition FLASH, Siemens Healthineers) or a 256-slice CT scanner (Revolution CT, GE Healthcare) was used for imaging. For the prospectively ECG-triggered CCTA, the patients with body mass index (BMI) of < 24 kg/m2 were scanned at 100 kV and those with BMIs of ≥ 24 kg/m2 were scanned at 120 kV. The tube current was modulated by automatic exposure control. The acquisition window was performed within the 70% R-R interval for heart rates (HRs) of < 60 bpm, 40–70% R-R interval for HRs of 60–80 bpm, or 30–40% R-R interval for HRs of > 80 bpm. Bolus-tracking was performed with the region of interest placed in the root of the aorta, and image acquisition was automatically started 6 seconds after a predefined threshold of 100 Hounsfield units was reached. The scanning range was set from the tracheal bifurcation to 1 cm below the diaphragm. The contrast agent was injected with a dual-head power injector (Stellant D, Medrad) through an 18–20-gauge intravenous needle placed in the right antecubital vein. Fifty to seventy milliliters of contrast agent (Ultravist, iopromide 370 mg iodine/mL, Bayer AG) was injected, followed by 30 mL of saline as a bolus chaser with an injection rate of 4.5–5 mL/s for all the phases.
CCTA Data Analysis and Assessment of RECHARGE Score
All the CCTA data showed diagnostic quality, and they were included for further analysis. The image data were reconstructed using a dual-source CT (0.6 mm section thickness, 0.4 mm increment) and a 256-slice CT scanner (0.625 mm section thickness, 0.4 mm increment). Multi-planar reconstructions (MPRs), maximum intensity projections, and curved precision-recall (CPR) were obtained. CCTA post-processing was performed on a dedicated workstation (Vitrea, Canon). For all CTOs, the vessel lumen and vessel diameters were measured on orthogonal images, and the lengths were measured on CPR or MPRs.
For the CCTA-derived RECHARGE (RECHARGECCTA) score, the following parameters were recorded: 1, a blunt stump; 2, severe calcification in the CTO segment, i.e., a calcified area of ≥ 50% of the vessel cross-sectional area [14,17]; 3, tortuosity, defined as a bend of > 45° within the CTO body; 4, occlusion length of ≥ 20 mm; 5, diseased distal landing zone, defined as the presence of significant coronary artery disease (lumen stenosis > 50%) distal to the occluded segment, and/or a distal lumen diameter of < 2 mm; 6, previous bypass graft of CTO vessel [10]. Each variable was assigned one score point, which allowed the grading of CTO lesion complexity from 0 to 6 points. Two independent radiologists who were blinded to the CA results calculated the RECHARGECCTA score, J-CTOCT score [12], CT-RECTOR [14], and KCCT scores [19]. Interobserver disagreements were resolved by consensus in a joint session.
Catheter Angiography and Assessment of RECHARGE Score
CA and PCI were performed in all the 124 patients with 131 CTO lesions by interventional cardiologists with experience in the use of hybrid techniques who perform a mean number of ≥ 70 CTO procedures annually. A preoperative angiographic study was performed in each case to determine the CTO lesion complexity. In each case, the CTO lesion complexity was evaluated using the J-CTO scores. Hybrid strategies were applied: antegrade escalation and antegrade dissection and re-entry; retrograde escalation and retrograde dissection and re-entry. Two experienced cardiologists who were blinded to the RECHARGECCTA score independently calculated the RECHARGE score using CA data, as previously described [10]. Interobserver disagreements were resolved by consensus. Procedural success was defined as successful CTO revascularization with the achievement of < 20% residual diameter stenosis within the stented segment and the restoration of a TIMI = 3.
Statistical Analysis
All statistical analyses were performed using the MedCalc statistical software (MedCalc Software, version 15.8). Binary variables were presented as numbers with percentages (%), and continuous variables were presented as median with interquartile range (IQR) because of the non-normal distribution of the data. For comparisons of the RECHARGECCTA and the RECHARGECA scores, continuous variables were compared using both Mann-Whitney and Wilcoxon tests, and categorical variables were compared using the McNemar test. The prediction accuracies of the RECHARGECCTA, RECHARGECA, J-CTOCT, CT-RECTOR, and KCCT scores were evaluated using receiver operator characteristics (ROCs) curve analysis with the corresponding area under the curve (AUC). The method of DeLong et al. [20] was used to compare the ROC curves. The Optimal cut-off value of the RECHARGECCTA score was determined using the Youden index for predicting procedural success. Statistical significance was set at a p value of ≤ 0.05.
RESULTS
Patient Characteristics and Procedural Results
Of 124 patients, 33 (27%) had prior myocardial infarction and 13 (10%) had prior PCI. Further characteristics of the patients are presented in Table 1. Of the 131 lesions, final procedural success was obtained for 94 (72%), the 30-minutes wire crossing was achieved for 80 (61%), antegrade wire access was the preferred primary crossing strategy in 92 (70%), and a hybrid approach was performed in 39 (30%). The median J-CTO score was 2 (IQR 2–2) for all the patients, and it was higher in the failure group (2 [IQR 2–3] vs. 1.5 [IQR 1–2], p < 0.05). The median procedural time was 18 minutes (IQR 6–39 minutes) across the population. No severe complications occurred. Further characteristics of the CTO lesions and the procedural results are provided in Table 2.
Table 1. Baseline Data of Patients.
| Total | |
|---|---|
| Age (years) | 54 (43–60) |
| Sex (male/female) | 98/26 |
| Body mass index | 26 (25–28) |
| Diabetes | 32 (26) |
| Hypertension | 78 (63) |
| Dyslipidemia | 11 (9) |
| Prior MI | 33 (27) |
| Prior PCI | 13 (11) |
| Prior CABG | 0 (0) |
| Current smoker | 67 (54) |
| Echocardiographic LVEF% | 62 (58–62) |
Data presented as median with interquartile range or number (%). CABG = coronary artery bypass grafting, LVEF = left ventricular ejection fraction, MI = myocardial infarction, PCI = percutaneous coronary intervention
Table 2. Characteristics of CTO Lesions and Procedure Data.
| Lesion Characteristics | Total | Procedural Results | Guidewire Crossing Time | ||||
|---|---|---|---|---|---|---|---|
| Success | Fail | P | < 30 Minutes | > 30 Minutes | P | ||
| n = 94 | n = 37 | n = 80 | n = 51 | ||||
| J-CTO score | 2 (2–2) | 1.5 (1–2) | 2 (2–3) | 0.033 | 2 (1–2) | 2 (2–3) | 0.159 |
| Target vessel | 0.979 | 0.430 | |||||
| RCA | 61 (47) | 43 (33) | 18 (14) | 35 (27) | 26 (20) | ||
| LAD | 51 (39) | 37 (28) | 14 (11) | 30 (23) | 21 (16) | ||
| LCX | 17 (13) | 12 (9) | 5 (4) | 13 (10) | 4 (3) | ||
| Previous failed lesion | 14 (11) | 9 (7) | 5 (4) | 0.352 | 6 (5) | 8 (6) | 0.756 |
| Final crossing strategy | 131 (100) | 94 (72) | 37 (28) | 0.312 | 80 (61) | 51 (39) | 0.143 |
| Antegrade* | 116 (89) | 86 (66) | 30 (23) | 74 (56) | 42 (32) | ||
| Retrograde | 15 (11) | 8 (6) | 7 (5) | 6 (5) | 9 (7) | ||
| Hybrid approach | 39 (30) | 22 (17) | 17 (13) | 0.428 | 15 (11) | 24 (19) | 0.113 |
| Procedural time (minutes) | 18 (6–39) | 11.5 (4.75–26) | 43.5 (34–62) | 0.059 | 8 (4–15) | 44 (36–65) | 0.079 |
Data presented as median with interquartile range or number (%) of total 131 lesions (%). *Antegrade approach includes antegrade wire escalation and dissection re-entry. CTO = chronic total occlusion, LAD = left anterior descending branch, LCX = left circumflex branch, RCA = right coronary artery
Comparison of RECHARGE Scores Derived From CCTA and CA in Procedural Results
Both scores were significantly different for procedural success and failure (median RECHARGECA score: 2 vs. 3, p < 0.001; median RECHARGECCTA score: 2 vs. 3, p < 0.001), the 30-minutes wire crossing (median RECHARGECA score: 1.5 vs. 3, p = 0.001; median RECHARGECCTA score: 2 vs. 3, p = 0.001), and the antegrade crossing (median RECHARGECA score: 2 vs. 3, p = 0.044; median RECHARGECCTA score: 2 vs. 3, p = 0.040), respectively (Table 3, Figs. 1, 2).
Table 3. Comparison of RECHARGE Scores Derived From CCTA and CA in Procedural Results.
| CA-Derived | CCTA-Derived | P | |
|---|---|---|---|
| Procedural | |||
| Success | 2 (1–3) | 2 (1–3) | 0.084 |
| Failure | 3 (2–4) | 3 (3–4) | 0.429 |
| p | < 0.001 | < 0.001 | |
| 30-minutes crossing | |||
| Success | 1.5 (1–3) | 2 (1–3) | 0.001 |
| Failure | 3 (2–3) | 3 (2–4) | 0.336 |
| p | 0.001 | 0.001 | |
| Antegrade crossing | |||
| Success | 2 (1–3) | 2 (2–3) | 0.099 |
| Failure | 3 (2–3) | 3 (2–4) | 0.149 |
| p | 0.044 | 0.040 | |
| Retrograde crossing | |||
| Success | 2 (1–3) | 2 (2–3) | 0.146 |
| Failure | 2 (1–3) | 2.5 (2–3) | 0.037 |
| p | 0.677 | 0.275 | |
Data presented as median with interquartile range. CA = catheter angiography, CCTA = coronary CT angiography
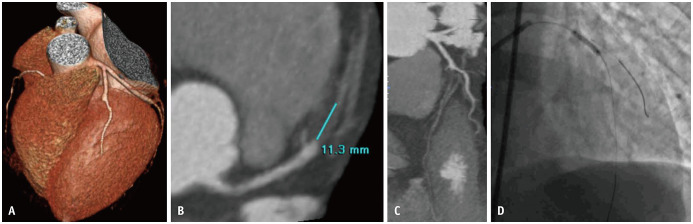
Fig. 1. A short non-calcified CTO lesion with a blunt-entry site in the mid-segment of the LAD.
A–C. The RECHARGECCTA score was 1. D. Invasive coronary angiography shows a successful recanalization of the LAD. CTO = chronic total occlusion, LAD = left anterior descending branch
Fig. 2. A long-calcified CTO lesion in the LAD with a blunt cap and non-relevant bending within the occlusion route and disease landing zone.
A–C. The RECHARGECCTA score was 4. D. Invasive coronary angiography shows a failed attempt of guidewire penetration for entering a true lumen of the LAD and overall failure of the procedure. CTO = chronic total occlusion, LAD = left anterior descending branch
No significant difference was observed between the RECHARGECCTA and RECHARGECA scores (median score: 2 vs. 2, p = 0.084) for procedural success. However, the RECHARGECCTA score was higher than the RECHARGECA score (median: 2 [IQR 1–3] vs. 1.5 [IQR 1–3], p = 0.001) for predicting the 30-minutes wire crossing (Table 3). In terms of the final crossing strategy, no significant difference was observed between the RECHARGECCTA and RECHARGECA scores for success or failure during the antegrade crossing. For the prediction of the failed final retrograde crossing, the RECHARGECCTA score was significantly higher than the RECHARGECA score (median: 2.5 [IQR 2–3] vs. 2 [IQR 1–3], p = 0.037).
Comparison of RECHARGE Scores Derived From CCTA and CA in CTO Lesions
The RECHARGECCTA score described higher levels of CTO calcification than the RECHARGECA score (p < 0.001). However, no significant difference was observed between the two RECHARGE scores regarding other morphological parameters (Table 4).
Table 4. Comparison of RECHARGE Scores Derived from CCTA and Catheter Angiography in CTO Lesions.
| CA-Derived | CCTA-Derived | P | |
|---|---|---|---|
| RECHARE score | 2 (1–3) | 2 (1–3) | 0.065 |
| Blunt stump | 82 (63) | 85 (65) | 0.838 |
| CTO calcification | 27 (21) | 81 (62) | < 0.001 |
| Tortuosity > 450 | 34 (26) | 39 (30) | 0.523 |
| CTO length (mm) | 14.2 (10.1–31) | 20 (9.3–29) | 0.739 |
| Diseased distal landing zone | 50 (38) | 51 (39) | 0.938 |
Data presented as median with interquartile range or number (%). CA = catheter angiography, CCTA = Coronary CT angiography, CTO = chronic total occlusion
Comparison of Prediction Accuracy between RECHARGE Scores Derived From CCTA and CA
The AUC for the ROC curve analysis for determining procedural success was 0.718 (95% confidence interval [CI] 0.633–0.793) for RECHARGECCTA and 0.757 (95% CI 0.661–0.840) for RECHARGECA. Similar results were observed for the 30-minutes wire crossing with an AUC of 0.708 (95% CI 0.622–0.784) for RECHARGECCTA and 0.705 (95% CI 0.603–0.793) for RECHARGECA. Neither of the comparisons of the RECHARGECCTA and RECHARGECA scores for predicting procedural success and 30-minutes wire crossing showed a significant difference (p = 0.655 and p = 0.984, respectively). The sensitivity, specificity, positive predictive value, and negative predictive value of the RECHARGECCTA scores of ≤ 2 for predicting procedural success were 78%, 60%, 43%, and 87%, respectively.
Comparison of RECHARGECCTA Score with Other Scores
AUC at ROC curve analysis for determining procedural success was 0.704 (95% CI 0.618–0.780) for J-CTOCT, 0.665 (95% CI 0.577–0.745) for CT-RECTOR, and 0.717 (95% CI 0.631–0.792) for KCCT scores, respectively. Similar results were observed for the 30-minutes wire crossing with an AUC of 0.673 (95% CI 0.586–0.752) for J-CTOCT, 0.643 (95% CI 0.544–0.724) for CT-RECTOR, and 0.703 (95% CI 0.617–0.780) for KCCT scores, respectively. There was no significant difference between the accuracies of the RECHARGECCTA score and other scores (including CT-RECTOR and KCCT scores) for predicting procedural success and the 30-minutes wire crossing (all p > 0.05) (Figs. 3, 4).
Fig. 3. ROC curves of CTA-derived scores for the prediction of procedural success.

ROC curves with AUCs for predicting procedural success are illustrated: 0.718 (95% CI 0.633–0.793) for RECHARGECCTA score, 0.704 (95% CI 0.618–0.780) for J-CTOCT, 0.665 (95% CI 0.577–0.745) for CT-RECTOR, and 0.717 (95% CI 0.631–0.792) for KCCT score. AUC = area under the curve, CI = confidence interval, CTA = CT angiography, ROC = receiver-operating characteristic
Fig. 4. ROC curves of CTA-derived scores for the prediction of the < 30-minutes guidewire crossing.

ROC curves with AUCs for 30-minutes guidewire crossing are illustrated: 0.708 (95% CI 0.622–0.784) for RECHARGECCTA score, 0.673 (95% CI 0.586–0.752) for J-CTOCT, 0.643 (95% CI 0.544–0.724) for CT-RECTOR, and 0.703 (95% CI 0.617–0.780) for KCCT score. AUC = area under the curve, CI = confidence interval, CTA = CT angiography, ROC = receiver-operating characteristic
DISCUSSION
This study demonstrates that the prediction accuracy of the CCTA-derived RECHARGE score for CTO-PCI success and wire crossing within 30 minutes was similar to that of the CA-derived RECHARGE score and other CTA-based scores (including J-CTOCT, CT-RECTOR, and KCCT scores). The overall procedural success rate was 72% in this population, which was similar to previous findings [21].
The RECHARGE score, as a novel and easy-to-use scoring tool, was developed from hybrid CTO procedures incorporating objective clinical and morphological parameters [5,10]. As the RECHARGE and J-CTO scores build on four common morphologic characteristics, their predictive powers were expected to be similar. Yet, compared with the J-CTO score, the “diseased distal landing zone” and “previous bypass graft on the CTO target vessel” are independent characteristics incorporated into the RECHARGE score, forming a 6-scale scoring tool. Maeremans et al. [10] demonstrated that the RECHARGECA score was not only more accurate than the J-CTO score (AUCRECHARGE = 0.711 vs. AUCJ-CTO = 0.676) in predicting overall procedural success; it was more suitable for different levels of surgery.
Several studies [12,16] have validated CCTA as a valuable and non-invasive imaging method for assessing pre-procedural characterization of CTO lesions and established it as a useful alternative to invasive angiography for certain indications. Recent investigations [12,22] concluded that the CCTA-derived J-CTO score has better predictive accuracy in predicting CTO-PCI success and the 30-minutes wire crossing, especially for complex cases. Similarly, the predictive accuracy of the RECHARGECCTA and RECHARGECA scores were compared in this study. Significantly higher RECHARGE scores (both CTA- and CA-derived) were observed for failed procedures, > 30-minutes guidewire crossing, and failure in final antegrade crossing, which indicates the predictive value of RECHARGE scores for procedural success and guidewire crossing within 30 minutes. However, the results also showed that the RECHARGECCTA score, which was not significantly better, was fairly comparable to the RECHARGECA score in predicting procedural success and the 30-minutes wire crossing. Furthermore, regarding that RECHARGE score focuses more on the “diseased distal landing zone,” the predictive performance of the CA- and CTA-derived scores were compared for the final retrograde crossing. The RECHARGECCTA score was significantly higher than the RECHARGECA for failed retrograde crossing. Yet, neither scores were significantly different for successful and failed retrograde crossing, mostly due to the limitations of the sample used for retrograde crossing.
Currently, some novel CCTA-based prediction tools have been demonstrated to be more accurate in predicting time-efficient guidewire crossing [14,19]. The CT-RECTOR score is a 6-variable predictive scoring system that exceeds the CA-based J-CTO score in prediction value [14,23]. Another novel CCTA-based predictive algorithm, the KCCT score (Korean Multicenter CTO CT Registry), showed higher predictive power than the other pre-procedural tools, including the CA-based J-CTO, PROGRESS-CTO, CL-score, and CT-based CT-RECTOR (c-statistics = 0.78 vs. 0.65–0.72, p < 0.001, all) [19]. Moreover, these studies showed that with an increasing CT-RECTOR or KCCT score, procedural success or the guidewire crossing duration decreased. In this study, the comparisons of the ROC curves of the RECHARGECCTA and other scores (J-CTOCT, CT-RECTOR, and KCCT scores) were not significantly different, indicating a similar predictive value of RECHARGECCTA for procedural outcomes.
Identifying the morphologic characteristics of CTO, using pre-procedural CCTA, may assist in determining procedural strategy, which may facilitate an increase in the rate of successful CTO-PCIs. Luo et al. [16] reported that the predictors of failed antegrade PCIs (including negative remodeling, lesion lengths of > 31.89 mm on CCTA, and ostial or bifurcation lesions on CA imaging) may prompt a switch to an early retrograde approach for appropriate patients and improve the chance of successful revascularization from 74% to 87%. Rolf et al. [17] reported that pre-procedural CCTA can significantly increase the success rate of CTO-PCI from 64% to 88%, although this was based on a relatively small patient cohort (30 patients with CCTA). Many CT-based studies consistently suggest the utility of severe calcification involving ≥ 50% of the vessel cross-sectional area for predicting CTO-PCI failure. In this study, the ability of CCTA to detect CTO calcification was significantly better than that of invasive angiograms (CCTA 62% vs. CA 21%, p < 0.001), which was discordant with the fact that the AUC for procedural success was higher for RECHARGECA (0.757 vs. 0.718), with similar AUC for the guidewire crossing time. In clinical practice, the success rate of the CTO intervention may be largely dependent on the surgeon's experience, but none of the RECHARGE scores incorporate procedure-related information. It may be one of the important reasons for this discordance.
Several limitations of this study need to be addressed. First, this was a single-center, retrospective, observational study with a relatively small sample size (124 CTO patients with 131 CTO lesions). The predictive value of the RECHARGECCTA score for procedural success and guidewire crossing within 30-minutes was found to be similar to those of other CTA-based scores; however, we did not analyze whether it was inferior to the other CTA-based scores due to the limitation of sample size. Our results also need to be further confirmed in a prospective multicenter study. Second, we only enrolled elective CTO-PCI patients who underwent CCTA before the procedure and had CTO lesions with intermediate complexity (median J-CTO score 2). The results of the current study require further validation before they can be generalized to patients with various lesions.
In conclusion, The predictive value of the RECHARGECCTA score for CTO-PCI success and guidewire crossing within 30-minutes was similar to those of the RECHARGECA score and other CTA-based scores. However, the RECHARGECCTA score may not be a viable replacement for other CTA-based scores for predicting performance. CCTA may serve as an alternative non-invasive imaging tool for guiding procedural strategies and predicting procedural outcomes.
Acknowledgments
The authors thank doctors from Cardiology and Radiology Departments for assistance in data collection.
Footnotes
This work was supported by Beijing Municipal Administration of Hospital Youth Program (Grant number: QML20160606); Beijing Municipal Science and Technology Project (Grant number: Z161100000516139); Beijing Lab for Cardiovascular Precision medicine, Beijing and China Cardiovascular Disease Alliance VG Youth Fund Project (Grant number: 2017-CCA-VG-046) and Capital Health Development Research Project (NO. 2018-2-2063).
Conflicts of Interest: The authors of this manuscript declare relationships with the following companies: Dr. Schoepf receives research support from Astellas, Bayer AG, GE Healthcare, and Siemens Healthineers and is a consultant for Bayer, Guerbet, HeartFlow Inc., and Siemens. All authors have no conflicts of interest to disclose.
- Conceptualization: Xiantao Song, Yi He.
- Data curation: Rui Wang, Yalei Chen, Jianan Li.
- Formal analysis: Jiahui Li, Rui Wang, Jonathan T. Pannell.
- Funding acquisition: Xiantao Song, Yi He.
- Investigation: Christian Tesche, U. Joseph Schoepf, Jonathan T. Pannell.
- Methodology: Xiantao Song, Rongchong Huang.
- Project administration: Jiahui Li, Rui Wang.
- Resources: Xiantao Li, Yi He.
- Software: Rui Wang, Christian Tesche, U. Joseph Schoepf.
- Supervision: Rongchong Huang, Yalei Chen, Jianan Li.
- Validation: Xiantao Song, Yi He, Christian Tesche, U. Joseph Schoepf, Jonathan T. Pannell.
- Visualization: Jiahui Li, Rui Wang, Yi He, Xiantao Song.
- Writing—original draft: Jiahui Li, Rui Wang.
- Writing—review & editing: Christian Tesche, Yi He, Rongchong Huang, Xiantao Song.
References
- 1.Brilakis ES, Banerjee S, Karmpaliotis D, Lombardi WL, Tsai TT, Shunk KA, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry) JACC Cardiovasc Interv. 2015;8:245–253. doi: 10.1016/j.jcin.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Grantham JA, Marso SP, Spertus J, House J, Holmes DR, Jr, Rutherford BD. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv. 2009;2:479–486. doi: 10.1016/j.jcin.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 3.Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010;160:179–187. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Staruch AD, Opolski MP, Slomka PJ, Staruch M, Kepka C, Witkowski A, et al. Automated quantitative plaque analysis for discrimination of coronary chronic total occlusion and subtotal occlusion in computed tomography angiography. J Thorac Imaging. 2016;31:367–372. doi: 10.1097/RTI.0000000000000223. [DOI] [PubMed] [Google Scholar]
- 5.Maeremans J, Walsh S, Knaapen P, Spratt JC, Avran A, Hanratty CG, et al. The hybrid algorithm for treating chronic total occlusions in Europe: the RECHARGE registry. J Am Coll Cardiol. 2016;68:1958–1970. doi: 10.1016/j.jacc.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 6.Christopoulos G, Wyman RM, Alaswad K, Karmpaliotis D, Lombardi W, Grantham JA, et al. Clinical utility of the Japan-chronic total occlusion score in coronary chronic total occlusion interventions: results from a multicenter registry. Circ Cardiovasc Interv. 2015;8:e002171. doi: 10.1161/CIRCINTERVENTIONS.114.002171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Alessandrino G, Chevalier B, Lefèvre T, Sanguineti F, Garot P, Unterseeh T, et al. A clinical and angiographic scoring system to predict the probability of successful first-attempt percutaneous coronary intervention in patients with total chronic coronary occlusion. JACC Cardiovasc Interv. 2015;8:1540–1548. doi: 10.1016/j.jcin.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Christopoulos G, Kandzari DE, Yeh RW, Jaffer FA, Karmpaliotis D, Wyman MR, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: the PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score. JACC Cardiovasc Interv. 2016;9:1–9. doi: 10.1016/j.jcin.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Maeremans J, Spratt JC, Knaapen P, Walsh S, Agostoni P, Wilson W, et al. Towards a contemporary, comprehensive scoring system for determining technical outcomes of hybrid percutaneous chronic total occlusion treatment: the RECHARGE score. Catheter Cardiovasc Interv. 2018;91:192–202. doi: 10.1002/ccd.27092. [DOI] [PubMed] [Google Scholar]
- 11.Magro M, Schultz C, Simsek C, Garcia-Garcia HM, Regar E, Nieman K, et al. Computed tomography as a tool for percutaneous coronary intervention of chronic total occlusions. EuroIntervention. 2010;6 Suppl G:G123–G131. [PubMed] [Google Scholar]
- 12.Fujino A, Otsuji S, Hasegawa K, Arita T, Takiuchi S, Fujii K, et al. Accuracy of J-CTO score derived from computed tomography versus angiography to predict successful percutaneous coronary intervention. JACC Cardiovasc Imaging. 2018;11:209–217. doi: 10.1016/j.jcmg.2017.01.028. [DOI] [PubMed] [Google Scholar]
- 13.Werner GS, Hecht H, Stone GW. Utility of CT angiography to guide coronary intervention of CTO. JACC Cardiovasc Imaging. 2015;8:814–816. doi: 10.1016/j.jcmg.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Opolski MP, Achenbach S, Schuhbäck A, Rolf A, Möllmann H, Nef H, et al. Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion: insights from the CT-RECTOR multicenter registry (Computed Tomography Registry of Chronic Total Occlusion Revascularization) JACC Cardiovasc Interv. 2015;8:257–267. doi: 10.1016/j.jcin.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Opolski MP, Achenbach S. CT angiography for revascularization of CTO: crossing the borders of diagnosis and treatment. JACC Cardiovasc Imaging. 2015;8:846–858. doi: 10.1016/j.jcmg.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 16.Luo C, Huang M, Li J, Liang C, Zhang Q, Liu H, et al. Predictors of interventional success of antegrade PCI for CTO. JACC Cardiovasc Imaging. 2015;8:804–813. doi: 10.1016/j.jcmg.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Rolf A, Werner GS, Schuhbäck A, Rixe J, Möllmann H, Nef HM, et al. Preprocedural coronary CT angiography significantly improves success rates of PCI for chronic total occlusion. Int J Cardiovasc Imaging. 2013;29:1819–1827. doi: 10.1007/s10554-013-0258-y. [DOI] [PubMed] [Google Scholar]
- 18.Opolski MP. Cardiac computed tomography for planning revascularization procedures. J Thorac Imaging. 2018;33:35–54. doi: 10.1097/RTI.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 19.Yu CW, Lee HJ, Suh J, Lee NH, Park SM, Park TK, et al. Coronary computed tomography angiography predicts guidewire crossing and success of percutaneous intervention for chronic total occlusion: Korean multicenter CTO CT registry score as a tool for assessing difficulty in chronic total occlusion percutaneous coronary intervention. Circ Cardiovasc Imaging. 2017;10:e005800. doi: 10.1161/CIRCIMAGING.116.005800. [DOI] [PubMed] [Google Scholar]
- 20.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 21.Patel VG, Brayton KM, Tamayo A, Mogabgab O, Michael TT, Lo N, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv. 2013;6:128–136. doi: 10.1016/j.jcin.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Li Y, Xu N, Zhang J, Li M, Lu Z, Wei M, et al. Procedural success of CTO recanalization: comparison of the J-CTO score determined by coronary CT angiography to invasive angiography. J Cardiovasc Comput Tomogr. 2015;9:578–584. doi: 10.1016/j.jcct.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Tan Y, Zhou J, Zhang W, Zhou Y, Du L, Tian F, et al. Comparison of CT-RECTOR and J-CTO scores to predict chronic total occlusion difficulty for percutaneous coronary intervention. Int J Cardiol. 2017;235:169–175. doi: 10.1016/j.ijcard.2017.02.008. [DOI] [PubMed] [Google Scholar]