Abstract
Following the introduction of a novel pathological concept of usual interstitial pneumonia (UIP) by Liebow and Carrington in 1969, diffuse interstitial pneumonia has evolved into UIP, nonspecific interstitial pneumonia (NSIP), and interstitial lung abnormality (ILA); the histopathological and CT findings of these conditions reflect the required multidisciplinary team approach, involving pulmonologists, radiologists, and pathologists, for their diagnosis and management. Concomitantly, traction bronchiectasis and bronchiolectasis have been recognized as the most persistent and important indices of the severity and prognosis of fibrotic lung diseases. The traction bronchiectasis index (TBI) can stratify the prognoses of patients with ILAs. In this review, the evolutionary concepts of UIP, NSIP, and ILAs are summarized in tables and figures, with a demonstration of the correlation between CT findings and pathologic evaluation. The CT-based UIP score is being proposed to facilitate a better understanding of the spectrum of pulmonary fibrosis, from ILAs to UIP, with emphasis on traction bronchiectasis/bronchiolectasis.
Keywords: Usual interstitial pneumonia (UIP), Interstitial lung abnormality (ILA), Traction bronchiectasis, Pulmonary fibrosis, Traction bronchiectasis index (TBI)
INTRODUCTION
The history of usual interstitial pneumonia (UIP) dates back to 1969 when Liebow and Carrington [1], pathologists at Yale University, defined it as “the largest group, the most heterogeneous in terms of structure and causation, corresponding to the classic, undifferentiated” or “usual” description. It results from the failed resolution of lesions caused by injury to the alveolar lining cells, the capillary endothelium, or both, while the basement membrane is relatively intact. Hyaline membrane formation and the most variegated proteinaceous and cellular exudate may persist for several years. In 1994, Katzenstein and Fiorelli [2] defined nonspecific interstitial pneumonia (NSIP) as “characterized by varying proportion of interstitial inflammation and fibrosis that appeared to be occurring over a single time span (i.e., the process was temporally uniform)” with a better prognosis and different treatment options. The concept of UIP and NSIP evolved within the pathology domain until the 1990s when Nishimura et al. in 1992 [3], Müller and Coiby in 1997 [4], and Johkoh et al. in 1999 [5] reported the histopathologic-radiologic correlation of UIP using high-resolution CT (HRCT). The American Thoracic Society (ATS)/European Respiratory Society (ERS) International Multidisciplinary Consensus Classification on Idiopathic Interstitial Pneumonia published in 2002 reflected the trend of the multidisciplinary approach by pulmonologists, radiologists, and pathologists [6]. The concept and definition of UIP continued to evolve with pathologic and CT criteria in addition to the ATS/ERS/Japanese Respiratory Society (JRS)/Latin American Thoracic Association (ALAT) Guidelines in 2011 [7] and 2018 [8] and the Fleischner Society White Paper in 2018 [9]. In 2020, the Fleischner Society Position Paper on Interstitial Lung Abnormality (ILA), which defined the abnormality as lung lesions detected incidentally on CT, was published with its subcategorizations of non-subpleural ILA, subpleural non-fibrotic ILA, and subpleural fibrotic ILA based on data from multiple large investigational cohort studies including thousands of CT scans [10]. It is expected that ILAs, particularly the subpleural fibrotic, include earlier or subclinical forms of fibrotic lung diseases. Throughout the course of concept evolution from UIP to ILA via NSIP, histopathology and CT have become a partner and they have played an important role in the multidisciplinary team approach. At the same time, traction bronchiectasis/bronchiolectasis is recognized as the most persistent and important index of severity for fibrosis and prognosis [11,12]. A recent report by Hida et al. [13] indicated that the Traction Bronchiectasis Index (TBI) helps stratify the prognoses of subjects with ILA. In this review, the evolutionary concepts of UIP, NSIP, and ILA are summarized using tables, figures, and CT-pathologic correlation. Finally, the proposal of CT-based UIP scoring was proposed to facilitate a better understanding of the spectrum from ILA to UIP with attention to traction bronchiectasis.
Brief History of Fibrotic Lung Disease, UIP, and Traction Bronchiectasis
Liebow and Carrington [1] first defined UIP in 1969; chronic interstitial pneumonia was classified into five histopathological categories: UIP, desquamative interstitial pneumonia (DIP), bronchiolitis obliterans interstitial pneumonia and diffuse alveolar damage (BIP), lymphocytic interstitial pneumonia (LIP), and giant cell interstitial pneumonia (GIP). NSIP was first defined as a category of pulmonary fibrosis in 1994 by Katzenstein and Fiorelli [2]. Acute interstitial pneumonia (AIP), respiratory bronchiolitis-interstitial lung disease (RB-ILD), and bronchiolitis obliterans with organizing pneumonia (BOOP) as a substitute for bronchiolitis with interstitial pneumonia were also added to the category of idiopathic interstitial pneumonias [4,14,15]. GIP was considered idiopathic and excluded from the category of idiopathic interstitial pneumonia [4,16,17]. Both pathological and clinical classifications of idiopathic pulmonary fibrosis (IPF; pathologic counterpart, UIP) were reviewed [18]. In 2001, the classification evolved into the diagnostic criteria for IPF by the ATS with consensus [6]; the characteristic HRCT features were as follows: patterns of honeycombing and reticular opacities and the distribution of bilateral and symmetric basal or subpleural predominance (Table 1, Fig. 1).
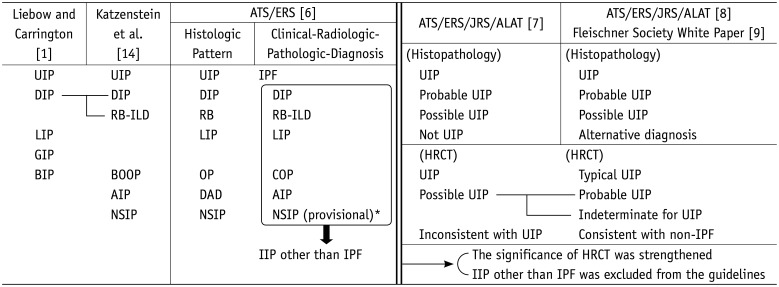
Table 1. Transition of Classification of Interstitial Pneumonia.
*This group represents a heterogeneous group with poorly characterized clinical and radiologic features that needs further study. AIP = acute interstitial pneumonia, ALAT = Latin American Thoracic Association, ATS = American Thoracic Society, BIP = bronchiolitis obliterans interstitial pneumonia and diffuse alveolar damage, BOOP = bronchiolitis obliterans-organizing pneumonia, COP = cryptogenic organizing pneumonia, DAD = diffuse alveolar damage, DIP = desquamative interstitial pneumonia, ERS = European Respiratory Society, GIP = giant cell interstitial pneumonia, HRCT = high-resolution CT, IIP = idiopathic interstitial pneumonia, IPF = idiopathic interstitial fibrosis, JRS = Japan Respiratory Society, LIP = lymphocytic interstitial pneumonia, NSIP = nonspecific interstitial pneumonia, OP = organizing pneumonia, RB = respiratory bronchiolitis, RB-ILD = respiratory bronchiolitis-interstitial pneumonia, UIP = usual interstitial pneumonia
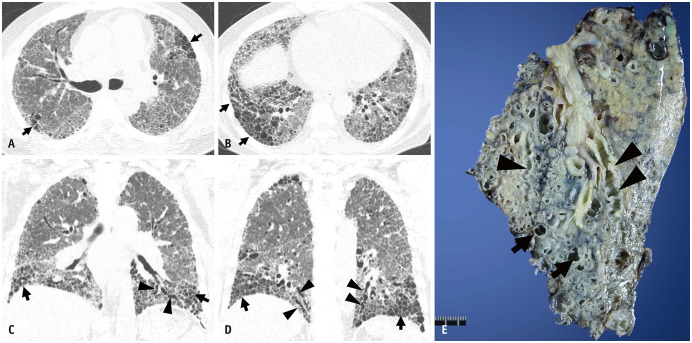
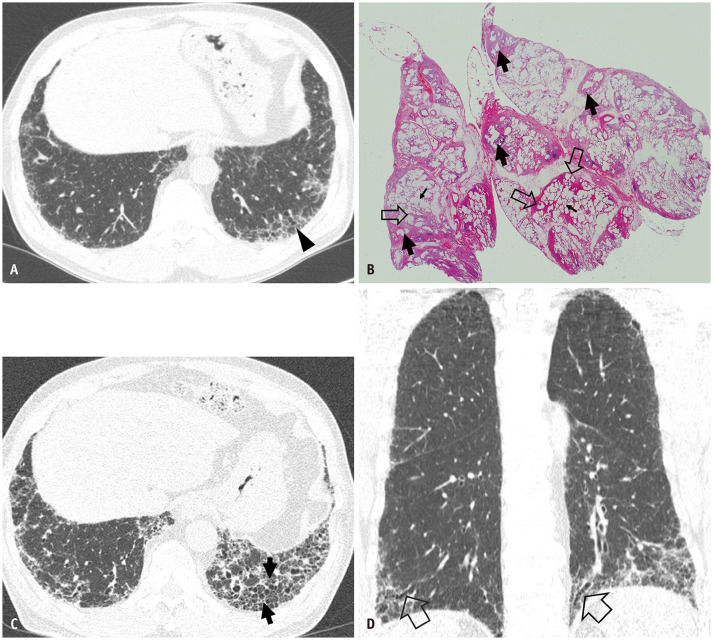
Fig. 1. End-stage pulmonary fibrosis and lung transplantation in a 62-year-old man with usual interstitial pneumonia.
A, B. Lung window images of CT scans obtained at the levels of the right upper lobar bronchus (A) and liver dome (B) show reticular lesions and patchy areas of honeycombing (arrows) in both lungs. C, D. Coronal reformatted images demonstrate areas of honeycombing (arrows) and traction bronchiectasis (arrowheads). E. Gross pathologic specimen of explanted left lung showing areas of honeycombing (arrows) and traction bronchiectasis (arrowheads).
Traction bronchiectasis was described as a finding of CT UIP in the 2011 statement, which was subsequently added as a criterion of probable CT UIP pattern in the 2018 statement [8,9]. In the 1950s, traction bronchiectasis was initially regarded as the progression of cystic changes in the lungs [19]. A comparison between the pathologic and chest radiographic features of end-stage fibrosis was performed by Genereux [20], and in this study, the possible relationship between traction bronchiectasis and pulmonary fibrosis was highlighted. The association between pathological and radiological traction bronchiectasis was reported by Westcott and Cole [21]. They considered the mechanism of traction bronchiectasis as the response to abnormal intraluminal pressure caused by increased elasticity and mechanical distortion of the bronchi. Radiological bronchiectasis was described in 2009 [22]; traction bronchiectasis was described as a frequently accompanying feature of UIP. Traction bronchiectasis is now defined as irregular and bronchiolar dilation caused by surrounding retractile pulmonary fibrosis (Fig. 1) [23].
Overview of NSIP
Kitaichi [24] was the first to report the cases of idiopathic interstitial pneumonia that were not covered by the previous classification of idiopathic interstitial pneumonia, including UIP and DIP. The concept of NSIP was developed by Katzenstein and Fiorelli [2]. They reported that NSIP had pathological features of inflammation and pulmonary fibrosis, the proportion of which could help classify NSIP into subtypes [2]. Fibrotic and cellular patterns are included in the classification of NSIP [2,18,25,26,27]. Cellular NSIP mainly consists of inflammatory cell infiltration [2,25]. The typical pathological features of fibrotic NSIP (fNSIP) are characterized by homogeneous and diffuse fibrosis with interstitial deposition of collagen and chronic inflammatory cells [24,27]. The fNSIP had a larger architectural distortion than the cellular NSIP; it was smaller than that of UIP [18,25]. Fibroblastic foci, myogenesis, and honeycombing in pathology, which are pathognomonic of UIP, are not usually observed in fNSIP [18,28,29]. In addition to pathological viewpoints, NSIP was also different from UIP based on the following clinical characteristics: younger age, susceptibility to steroid therapy, longer overall survival, and relatively preserved pulmonary function [2,18,27,28,30]. NSIP is associated with connective tissue disease more frequently than UIP. This relationship with connective tissue disease can influence the overall survival of patients depending on the type of underlying connective tissue disease (Tables 1, 2) [31,32].
Table 2. Histopathological Criteria for UIP and NSIP.
| UIP* | Probable UIP* | Indeterminate UIP* | Alternative Diagnosis* |
|---|---|---|---|
| Dense fibrosis with architectural distortion (i.e., destructive scarring and/or honeycombing) | Some histologic features from UIP (column 1) are present but to an extent that preludes a definite diagnosis of UIP/IPF | Fibrosis with or without architectural distortion with features favoring either a pattern other than UIP or features favoring UIP secondary to another cause | Features of other histologic patterns of IIPs (e.g., absence of fibroblast foci or loose fibrosis) in all biopsies |
| Predominantly subpleural and/or paraseptal distribution of fibrosis | AND | ||
| Absence of features to suggest an alternate diagnosis | Histologic findings indicative of other diseases (e.g., hypersensitivity pneumonitis, Langerhans cell histiocytosis, sarcoidosis, LAM) | ||
| Some histologic features from UIP (column 1), but with other features suggesting an alternative diagnosis | |||
| Patchy involvement of lung parenchyma by fibrosis | OR | ||
| Honeycombing only | |||
| Fibroblast foci | |||
| Absence of features to suggest an alternate diagnosis | |||
| Fibrosing NSIP† | Cellular NSIP† | ||
| Key Features | Pertinent Negative Factors | Key Features | Pertinent Negative Factors |
| Dense or loose interstitial fibrosis with uniform appearance | Temporal heterogeneity | Mild to moderate interstitial chronic inflammation | Dense interstitial fibrosis |
| Fibroblastic foci with dense fibrosis | Prominence of organizing pneumonia | ||
| Type II pneumocyte hyperplasia in areas of inflammation | |||
| Frequent preservation of lung architecture | |||
| Findings above are especially important in case with patchy involvement and subpleural or paraseptal distribution | Diffuse severe alveolar septal inflammation | ||
| Mild or moderate interstitial chronic inflammation | |||
*Raghu et al. Am J Respir Crit Care Med 2018;198:e44-e68 [8], †Travis et al. Am J Respir Crit Care Med 2008;177:1338-1347 [37]. IIP = idiopathic interstitial pneumonia, IPF = idiopathic interstitial fibrosis, LAM = lymphangioleiomyomatosis, NSIP = nonspecific interstitial pneumonia, UIP = usual interstitial pneumonia
HRCT is useful for identifying NSIP; a 78% diagnostic accuracy was reported by Silva et al. [33]. Typical features of fNSIP on HRCT are subpleural-dominant ground-glass opacities and reticular lesions sometimes with mild traction bronchiectasis. The lesions may show a distribution along the bronchovascular bundles and subpleural lungs (Fig. 2). In fNSIP related to connective tissue disease, the lesions demonstrated a lower lung zone predominance (Fig. 3). Honeycombing in fNSIP is rarely observed on HRCT and during pathological evaluations (Figs. 2, 3) [34,35,36,37]. On the other hand, the presence of ground-glass opacities is insufficient for CT distinction between fNSIP and UIP [5,11,36,38]; interobserver variation was also not negligible [5]. Therefore, pathological examination is often required to confirm the diagnosis of fNSIP [5,11,38,39]. However, radiologic UIP features can overlap with those of fNSIP, with subpleural fibrosis accompanying traction bronchiectasis/bronchiolectasis. Similarly, UIP can overlap with fNSIP with patchy involvement and a subpleural or paraseptal distribution of fibrosis [5,11,29,30,34,35,36,37,38]. The interobserver agreement between radiological and pathological observations can also be a problem [11,30,39,40]. Additionally, the distinction between cellular NSIP and fNSIP, as well as NSIP and chronic hypersensitivity pneumonitis, based on HRCT is often difficult [33]. Regardless of these issues, radiological assessments of fNSIP are important because of the difference between patient management approaches and patient survival (effective corticosteroid and cytotoxic drug use and longer overall survival in fNSIP, compared with UIP) [30,41].
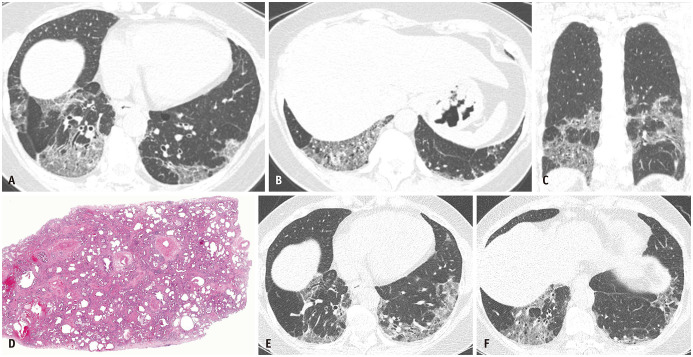
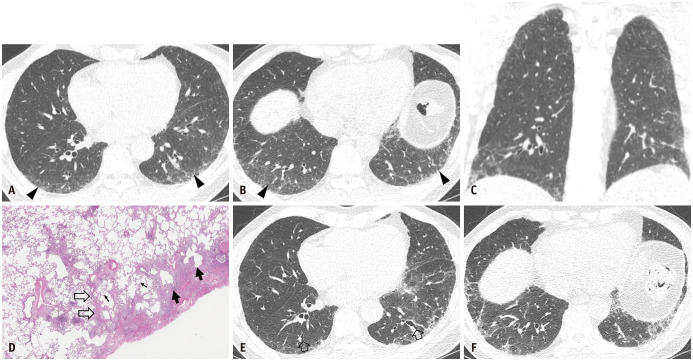
Fig. 2. Fibrotic nonspecific interstitial pneumonia in a 60-year-old woman with Sjogren's syndrome.
A, B. Lung window images of CT scans obtained at the levels of the liver dome (A) and suprahepatic inferior vena cava (B) show mixed areas of ground-glass opacities and reticular lesions with a patchy distribution. C. Coronal reformation image demonstrates lower lung zone predominance of lesions. D. Low-magnification (hematoxylin-eosin staining, × 10) pathological specimen shows chronologically homogeneous (same age) interstitial fibrosis. Uniform thickening of the alveolar septa and the preservation of the lung architecture are noticeable. E, F. Lung window images of CT scans obtained at similar levels to and six years after (A) and (B) without specific treatment show a minimal progression of interstitial lung diseases.
Fig. 3. Fibrotic nonspecific interstitial pneumonia in a 69-year-old man.
A, B. Lung window images of CT scans obtained at the levels of the right inferior pulmonary vein (A) and liver dome (B) show reticular lesions in the subpleural portion of both lungs. C. A high-magnification (hematoxylin-eosin staining, x 100) pathologic specimen obtained from the right middle lobe shows temporally uniform and homogeneous pulmonary fibrosis. D, E. Lung window images of CT scans obtained at similar levels to and four years after (A) and (B) with azathioprine therapy for one and a half years show a minimal progression of pulmonary fibrosis. In addition, the development of traction bronchiolectasis is observable (arrowheads in E).
Significance of Classifying ILD Depending on the Presence of Traction Bronchiectasis
An international consensus statement about interstitial pneumonia was first made in 2002 [6]. Interstitial pneumonia was classified based on the pathological pattern and the categorization of IPF or non-IPF. The radiologic features of interstitial pneumonia were also based on previous studies that reported a high diagnostic performance of HRCT [37,42]. Quadrelli et al. [43] reported that the performance of HRCT and pathological assessments in diagnosing IPF were comparable. Thus, differentiating between pathological and radiological patterns was considered important for the diagnosis of interstitial lung disease (ILD). An official ATS/ERS/JRS/ALAT statement in 2011 addressed the efficacy of the radiological approach [7]. The statement established the CT criteria of UIP patterns where “UIP pattern,” “Possible UIP pattern,” and “Inconsistent with UIP Pattern” were included. A possible UIP pattern was determined to meet the three following features: subpleural and basal predominance, reticular abnormality, and the absence of the feature of “Inconsistent with UIP Pattern.” Therefore, lung biopsy can be exempted for the definite diagnosis of IPF after the confirmation of the CT “UIP Pattern” (Table 3).
Table 3. Recategorization of Possible UIP Pattern on High-Resolution CT: Excerpt from an Official ATS/ERS/JRS/ALAT Guideline in 2011 and 2018, and a Fleischner Society White Paper in 2018.
| Distribution | Features | |
|---|---|---|
| Typical UIP (2018) [8, 9] | Subpleural predominant and basal predominant (occasionally diffuse) | Honeycombing |
| Reticular pattern with peripheral traction bronchiectasis or bronchiolectasis | ||
| Often heterogeneous | ||
| Probable UIP (2018) [8, 9] | Subpleural and basal predominant | Reticular pattern with peripheral traction bronchiectasis or bronchiolectasis |
| Often heterogeneous | ||
| May have mild GGO | ||
| Absence of honeycombing | ||
| Absence of features to suggest an alternative diagnosis | ||
| Indeterminate for UIP (2018) [8, 9] | Subpleural and basal predominant | Subtle reticulation |
| May have mild GGO or distortion | ||
| Some inconspicuous features suggestive of non-UIP pattern | ||
| Most consistent with non-IPF diagnosis (2018) [8, 9] | Upper-lung or mid-lung predominant fibrosis | Any of the following: predominant consolidation, extensive pure ground glass opacity (without acute exacerbation), extensive mosaic attenuation with extensive sharply defined lobular air trapping on expiration, diffuse nodules or cysts |
| Peribronchovascular predominance with subpleural sparing | ||
| UIP (2011) [7] | Subpleural and basal predominant | Reticular abnormality |
| Honeycombing with or without traction bronchiectasis | ||
| Absence of features listed as inconsistent with UIP pattern | ||
| Possible UIP (2011) [7] | Subpleural and basal predominant | Reticular abnormality |
| Absence of features listed as inconsistent with UIP pattern | ||
| Inconsistent with UIP (2011) [7] (any of seven features) | Upper or mid-lung predominance | Extensive ground glass abnormality (extensive reticular abnormality) |
| Peribronchovascular predominance | Profuse micronodules (bilateral, predominantly upper lobes) | |
| Discrete cysts (multiple, bilateral, away from areas of honeycombing) | ||
| Diffuse mosaic attenuation/air-trapping (bilateral, in three or more lobes) | ||
| Consolidation in bronchopulmonary segment(s)/lobe(s) |
ALAT = Latin American Thoracic Association, ATS = American Thoracic Society, ERS = European Respiratory Society, GGO = ground-glass opacities, IPF = idiopathic interstitial fibrosis, JRS = Japan Respiratory Society, UIP = usual interstitial pneumonia
Sumikawa et al. [11] reported that survival curves are affected by HRCT patterns of chronic fibrotic ILD; cases with UIP patterns show significantly shorter overall survival than those with possible UIP patterns and fNSIP patterns (mean overall survival times of typical UIP, possible UIP, and fNSIP: 33.5, 73.0, and 140.2 months, respectively). Regarding the cases with fNSIP patterns, significant differences in survival curves stratified by pathological patterns were observed [30]. Several previous studies have shown an association between HRCT patterns and the histopathological pattern of UIP [8,38,44,45]. Raghu et al. [46] reported that in an appropriate clinical setting, surgical lung biopsy may not be necessary for diagnosing IPF if the CT “possible UIP pattern” can be assessed by CT-reading experts.
Because 80% or more of patients with CT “probable UIP pattern” proved to have histopathological UIP, Chung et al. [45] insisted that the CT “possible UIP pattern” should be classified into probable and indeterminate UIP patterns on HRCT to maintain consistency with the pathological UIP classification. Brownell et al. [47] reported that the addition of traction bronchiectasis to the CT “possible UIP pattern” can increase the positive predictive value for histopathologic UIP diagnosis (Fig. 4).
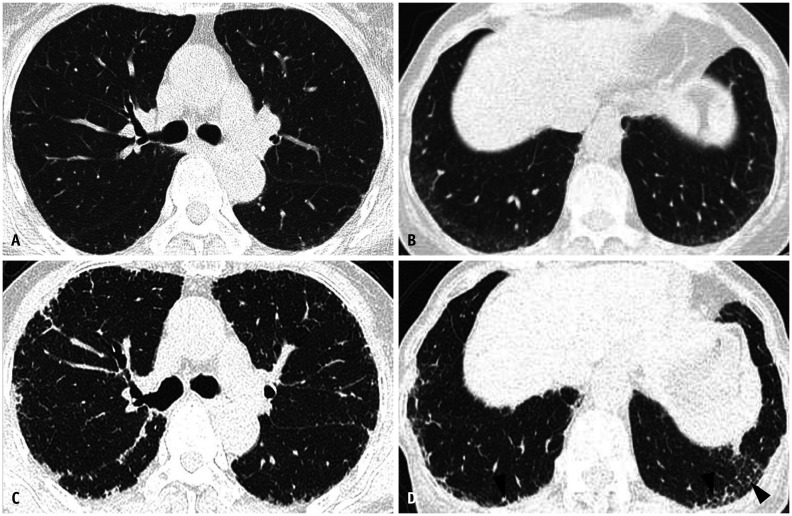
Fig. 4. Pathologic usual interstitial pneumonia manifesting as probable usual interstitial pneumonia pattern on CT in a 62-year-old man.
A. Lung window CT scan image obtained at the level of the liver dome shows reticular lesions in the subpleural portions of the basal lungs. In addition, traction bronchiolectasis (arrowhead) is noticeable. B. Low-magnification (hematoxylin-eosin staining, × 50) pathologic specimen obtained from the right lower lobe discloses interstitial lung disease of temporal heterogeneity composed of areas of microscopic honeycombing (arrows), interstitial fibrosis, and chronic inflammation (open arrows) and normal lungs (small arrows). C. Seven-year follow-up CT scan obtained at a level similar to that in (A) demonstrates the progression of pulmonary fibrosis with new areas of honeycombing (arrows) in the left lower lobe. D. Coronal reformatted image obtained at the same time as (C) shows reticular lesions in the lower lung zones with traction bronchiectasis (open arrows).
Therefore, the statement was modified and published as a clinical practice guideline in 2018 [8]. A possible UIP pattern can be replaced with a probable UIP pattern based on the presence of traction bronchiectasis/bronchiolectasis (Figs. 4, 5). Traction bronchiectasis was also indicated as an important feature of interstitial fibrosis in the Fleischner Society White Paper [9]. The distinction between traction bronchiectasis and honeycombing based on HCRT is often difficult, and adding multi-planar (coronal or sagittal reformation) images may facilitate a somewhat easier reading for the distinction. However, the importance of such a distinction cannot be emphasized more because the probable UIP pattern on HRCT shows a strong correlation with pathologic UIP [45].
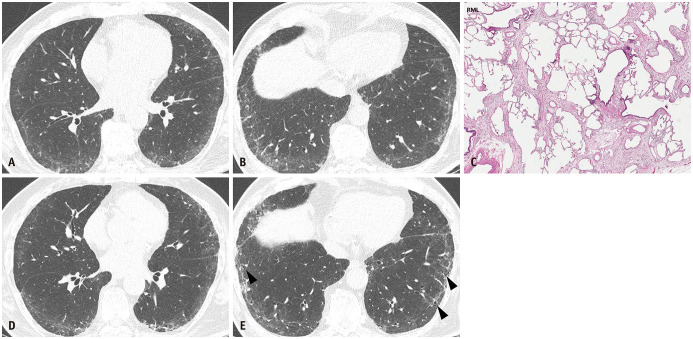
Fig. 5. Pathologic usual interstitial pneumonia manifesting as probable usual interstitial pneumonia pattern on CT in a 61-year-old man.
A, B. Lung window images of CT scans obtained at the levels of the right inferior pulmonary vein (A) and liver dome (B) show reticular lesions in subpleural areas in both lungs, particularly in dependent lungs. Traction bronchiectasis/bronchiolectasis is also observable (arrowheads, visible bronchioles within 2 cm from pleural surfaces). C. Coronal reformatted image demonstrates reticular lesions with subpleural distribution in both lungs. D. High-magnification (hematoxylin-eosin staining, × 200) pathologic specimen obtained from the right lower lobe shows mixed areas of microscopic honeycombing (arrows), interstitial fibrosis, and chronic inflammation (open arrows) and normal lung (small arrows). E, F. Four-year follow-up CT images obtained at similar levels to (A) and (B) and with Pirfenidone (antifibrotic drug) therapy demonstrated a minimal progression of pulmonary fibrosis. In addition, areas of traction bronchiectasis are noticeable (open arrows in E).
Emerging Therapies for UIP and Emerging Concept of ILA
Several clinical trials have been performed to prove the benefit of selected drug therapy. The importance of monotherapy with corticosteroids was demonstrated only in a retrospective study [48]. The effect of corticosteroids on acute exacerbation of IPF was also unclear, although they were commonly prescribed [49]. The combination of corticosteroids and immunosuppressants was considered equivocal [50,51]. Rituximab and cyclophosphamide were significantly effective for progressive ILD other than IPF in previous studies [52,53]. However, pharmacotherapy for IPF has no conclusive evidence [7]. Some studies have shown that lung transplantation can improve the overall survival of patients with IPF [54]. Recently, the introduction of pirfenidone, an oral antifibrotic drug, and nintedanib, a tyrosine kinase inhibitor, has gained increasing attention. Both pirfenidone and nintedanib proved to be effective in controlling declining lung function or improving overall survival in phase III clinical trials (Fig. 5) [55,56,57]. Previous studies reported that immediate treatment with antifibrotic drugs can improve the overall survival and quality of life in patients with IPF [58,59]. Therefore, the need for early detection of IPF has become pressing.
Subclinical and early ILD has been recognized broadly in several reports [60,61,62,63,64]. Rosas et al. [60] identified the radiological features of asymptomatic ILD with CT features such as subpleural ground-glass opacities and reticulation or peribronchovascular thickening. Similar findings of pulmonary interstitial changes, which may be collectively called ILA, were reported in subclinical older adults, smokers, and rheumatoid arthritis-related ILD [61,62,63,64,65]. The radiological features of ILA are defined as nondependent lung changes on CT affecting more than 5% of any lung zone, including non-dependent ground-glass opacities or reticular abnormalities, architectural distortion, diffuse centrilobular nodularity, nonemphysematous cysts, honeycombing, and traction bronchiolectasis [66,67,68]. The Fleischner Society White Paper also highlighted that ILA may be a crucial predictor of ILD [9]. In 2020, the Fleischner Society Position Paper on ILAs was published. ILAs are defined radiologically as incidental non-dependent abnormalities, including ground-glass opacities or reticular abnormalities, architectural distortion, traction bronchiolectasis, honeycombing, and nonemphysematous cysts involving at least 5% of a lung zone in individuals without suspected ILD [10]. ILAs were further subclassified as non-subpleural, subpleural non-fibrotic, and subpleural fibrotic (Table 4) (Figs. 6, 7). There has been a debate on the treatment of early fibrotic ILD or fibrotic ILA with antifibrotic drugs, which is based on the idea that early fibrotic ILD or fibrotic ILA eventually evolves and progresses to overt fibrotic ILD. Early treatment with antifibrotic drugs may prevent the ongoing progression of pulmonary fibrosis and help maintain healthy lives.
Table 4. Definition and Subcategories of ILA (Modified from Hatabu et al. Lancet Respir Med 2020;8:726-737 [10]).
| Definitions and subcategories of interstitial lung abnormalities |
| What are ILAs? |
| • Incidental identification of non-dependent abnormalities, including ground-glass or reticular abnormalities, lung distortion, traction bronchiectasis, honeycombing, and non-emphysematous cysts |
| • Involving at least 5% of a lung zone (upper, middle, and lower lung zones are demarcated by the levels of the inferior aortic arch and right inferior pulmonary vein |
| What are not ILAs? |
| Imaging findings restricted to: |
| • Dependent lung atelectasis |
| • Focal paraspinal fibrosis in close contact with thoracic spine osteophytes |
| • Smoking-related centrilobular nodularity in the absence of other findings |
| • Mild focal or unilateral abnormality |
| • Interstitial oedema (e.g., in heart failure) |
| • Findings of aspiration (patchy ground-glass, tree in bud) |
| Subcategories of ILAs |
| • Non-subpleural: ILAs without predominant subpleural localisation |
| • Subpleural non-fibrotic: ILAs with a predominant subpleural localisation and without evidence of fibrosis* |
| • Subpleural fibrotic: ILAs with a predominant subpleural localisation and with evidence of pulmonary fibrosis* |
*Fibrosis is characterised by the presence of architectural distortion with traction bronchiectasis or honeycombing (or both). ILAs = interstitial lung abnormalities
Fig. 6. Subcategorization of Interstitial Lung Abnormalities (Table 4).
A. Non-subpleural and non-fibrotic. CT shows bilateral patchy areas of ground-glass opacities with non-subpleural distribution. B. Subpleural non-fibrotic. CT predominantly shows subpleural ground-glass opacity and linear abnormality without evidence of fibrosis. C. Subpleural fibrosis, traction bronchiectasis, and architectural distortion with predominant subpleural distribution.
Fig. 7. Evolution of fibrotic interstitial lung abnormality in both lungs during follow-up of eight years in a 70-year-old woman.
A, B. Lung window images of CT scans obtained at the levels of the right upper lobar bronchus (A) and liver dome (B) show fine reticular lesions in the subpleural portion of both lungs. C, D. Eight-year follow-up CT scans obtained at similar levels to (A) and (B) demonstrate a slow progression of pulmonary fibrosis in both lungs; these are interstitial lung diseases. In addition, areas of traction bronchiolectasis are noticeable (arrowheads in D).
How Do We Understand the Whole Gamut of the ILD Spectrum from ILA to UIP with a Special Focus on Traction Bronchiectasis/Bronchiolectasis?
The radiologic features of ILA overlap with those of NSIP, except for the relative paucity of clinical symptoms in the former [10,34,35,36,66,67,68]. NSIP can be diagnosed based on pathologic and clinical characteristics, whereas ILA can be diagnosed based on incidental findings on CT [10,68]. ILAs are associated with smoking, old age, declining pulmonary function, increased mortality, and a positive mucin 5B (MUC5B) gene [10,66,67,68,69,70,71,72]. Some of these associated factors of ILAs are similar to those of IPF [7,8,9,10,66,67,68,69,70,71,72,73]. During long-term follow-up, the radiological findings of ILAs may evolve depending on the background and degree of lung disease [11,12,71,72,74,75,76,77].
An increase in the extent of architectural distortion or honeycombing, as well as the decrease in the extent of ground-glass opacities, is often detected on the HRCT of pathologically diagnosed fNSIP patients [11,74]. In approximately 30% of cases with a suggested diagnosis of NSIP on initial CT examination, the disease shows progression, which was suggestive of IPF on follow-up CT in a previous study [74]. For ILAs and other ILDs, several studies have reported the progression of lung abnormalities on HRCT [12,71,72,75,76,77]. NSIP, ILA, and ILD are considered to belong to the same spectrum as IPF based on their progressions [78,79]. ILAs and early interstitial fibrosis are not necessarily interchangeable because ILAs are frequently observed with advanced age and associated with smoking and environmental pollution [80]. However, early diagnosis or more careful follow-up of ILAs may be required with the possibility of progression in mind. Increased comorbidities, such as lung cancer and other respiratory diseases, should also be considered during follow-up (Table 5) [72,81,82,83,84].
Table 5. Key Features according to Different UIP Category on High-Resolution CT with Its Correspondence to ILA/NSIP.
| Typical UIP [8, 9] | Probable UIP [8, 9] | Indeterminate for UIP [8, 9] | Most consistent with non-IPF [8, 9] | |
|---|---|---|---|---|
| Basal and subpleural predominant distribution | + | + | −; Variable/diffuse | |
| Heterogeneity | + | + | ||
| Distortion | + | + | Subtle | |
| GGO | ± | ± | ||
| Peripheral traction bronchiectasis or bronchiolectasis | + | + | - | |
| Honeycombing | + | - | - | |
| ILA defined by CT [10] | Subpleural | Subpleural | Non-Subpleural | |
| Fibrotic ILA | Non-Fibrotic ILA | ILA | ||
| NSIP defined by pathology [37] | Progressive NSIP | Fibrosing NSIP | Cellular NSIP |
GGO = ground-glass opacities, ILA = interstitial lung abnormality, IPF = idiopathic pulmonary fibrosis, NSIP = nonspecific interstitial pneumonia, UIP = usual interstitial pneumonia
The onset of pulmonary fibrosis may indicate a dysfunction of epithelial cells. The release of profibrotic mediators and the acquisition of the features of mesenchymal cells occurred subsequently. The release of profibrotic mediators may lead to the activation of mesenchymal cells, an increase in the extracellular matrix, the differentiation of fibroblasts, and apoptosis of epithelial cells. The repetitive and complicated mechanism, including the aforementioned processes, was considered to cause interstitial fibrosis or alveolar wall collapse [73,85]. Simultaneously, lung remodeling occurs as an aberrant process. Injury to epithelial cells induces the activation of basal airway cells and causes aberrant re-epithelization or bronchiolization [85,86]. These are considered to result in traction bronchiectasis or honeycombing. However, there are problems in clinical settings related to the discordance between radiologic and pathologic features; the difficulty in distinguishing microcystic honeycombing from traction bronchiectasis may cause a discrepancy [9,87,88]. Indeed, histopathological honeycombing does not necessarily coincide with radiological honeycombing owing to the difference in their definitions [88]. On the other hand, traction bronchiectasis is closely related to honeycombing pathologically and radiologically. Staats et al. [89] reported that the degree of histopathological traction bronchiolectasis correlates with the degree of honeycombing on HRCT and honeycombing on HRCT correlates with histopathological traction bronchiolectasis after an explanted lung evaluation. This implied that lung remodeling was associated with the spectrum spanning traction bronchiectasis to honeycombing [84,89,90]. This observation was also consistent with that of a previous study; the extent of traction bronchiectasis and reticulation was associated with the severity of pulmonary fibrosis [91]. Jacob et al. [92] reported that the progression of traction bronchiectasis in IPF patients is the most significant factor associated with mortality. Therefore, identifying the presence, extent, and progression of traction bronchiectasis on HRCT is considered important for the diagnosis and prognostic predictions of IPF.
The results of previous studies suggested that traction bronchiectasis is also associated with prognosis in patients with ILD and chronic hypersensitivity pneumonitis [87,93,94]. Edey et al. [95] first reported that the quantification (with a three-point scale) of the severity of traction bronchiectasis is important for patient prognosis; in other words, increasing the severity of traction bronchiectasis is indicative of higher mortality irrespective of the HRCT pattern and disease extent. Walsh et al. [96] reported that there is a significant difference between the survival curves stratified by the severity of traction bronchiectasis in chronic hypersensitivity pneumonitis. However, the standard for the classification of the severity of traction bronchiectasis is not defined in these studies. Recently, traction bronchiectasis/bronchiolectasis proved to be the most influential factor associated with the progression of ILAs [78]. Thus, the association between ILAs and traction bronchiectasis/bronchiolectasis is gaining more attention.
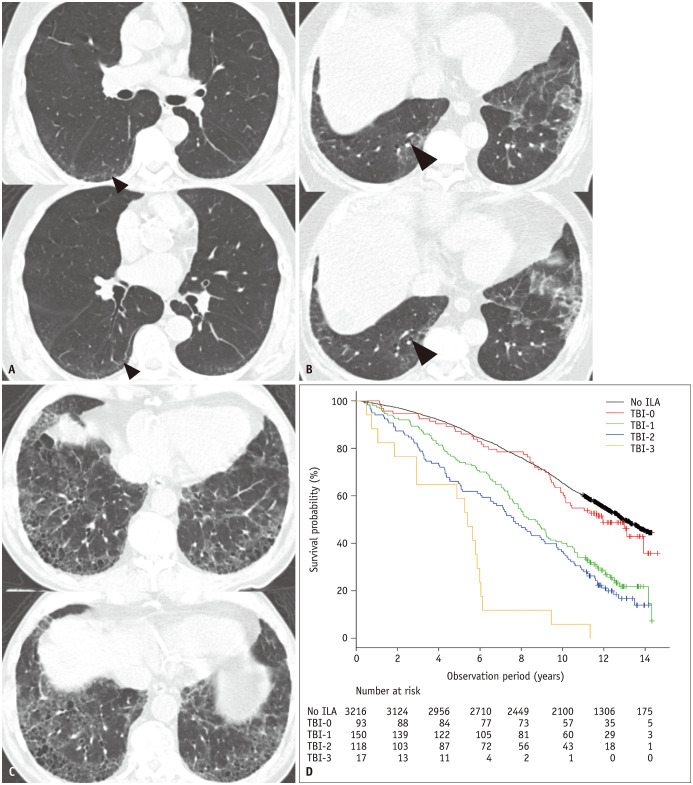
Hida et al. [13] classified ILA patients into 4 according to TBI. The four-point scales were based on the evaluation of the diameter of dilated bronchi or bronchioles on HRCT: TBI = 0, ILA without traction bronchiectasis or bronchiolectasis; TBI = 1, ILA with bronchiolectasis but without bronchiectasis or architectural distortion; TBI = 2, ILA with mild to moderate traction bronchiectasis; TBI = 3, ILA and severe traction bronchiectasis and/or honeycombing. As illustrated in Figure 8A, dilated airways in the subpleural area within 2 cm from the pleural or fissural surfaces with concurrent ILAs should be regarded indicative of bronchiolectasis, whereas dilated airways that are more proximal represent bronchiectasis, as shown in Figure 8B. They concluded that the extent of TBI is associated with overall survival or survival curves in ILA patients [13]. Traction bronchiolectasis on HRCT may be characterized by the results of interstitial inflammation, a non-fibrotic ILA, or gravity-dependent phenomena because the radiologic-pathologic correlation on the nature of the presumed traction bronchiolectasis has not been established. However, TBI on HRCT may be indicative of a substantial degree of interstitial pulmonary fibrosis (Fig. 8).
Fig. 8. TBI stratifies prognosis among the subjects with ILA. Reproduced from Hida et al. Eur J Radiol 2020;129:109073 [13].
A. TBI = 1. CT images demonstrate subpleural ground-glass and reticular opacities, indicating the presence of ILA. The dilatation of bronchioles (arrowheads) without obvious architectural distortion in the area of the subpleural opacities of the ILA is shown. B. TBI = 2. CT images demonstrate ground-glass and reticular opacities with subpleural and basilar distributions, indicating the presence of an ILA. Itis characterized by mild bronchiectasis (arrowheads) associated with architectural distortion in the area of subpleural opacities of an ILA. C. TBI = 3. CT images demonstrate ground-glass and reticular opacities with subpleural and basilar distributions, indicating the presence of an ILA. Severe bronchiectasis associated with architectural distortion as well as honeycombing is shown. D. Kaplan-Meier survival curves showing percent survival probability of participants with ILA stratified by TBI = 0, 1, 2, and 3 and those without ILA over years. ILA = interstitial lung abnormality, TBI = traction bronchiectasis index
ILAs have been reported to progress at several yearly intervals [12,71,77]. Jin et al. [77] reported the relationship between fibrotic ILAs and their progression. Putman et al. [12] reported that ILA progression is associated with the following radiological features: subpleural reticulation, lower lung zone predominance, and traction bronchiectasis/bronchiolectasis. Traction bronchiectasis/bronchiolectasis may be predictive not only of the degree of pulmonary fibrosis but also the progression of ILAs. On the other hand, serial changes in traction bronchiectasis/bronchiolectasis, which are frequently observed in clinical settings, have been mentioned only in a few studies [33,92]. Silva et al. [33] showed changes in lung abnormalities in patients with NSIP on HRCT. Several cases showed an increase in the severity of traction bronchiectasis. Further assessment will be necessary to confirm the presence and extent of traction bronchiectasis in fibrotic ILDs or ILAs as radiological biomarkers for pulmonary fibrosis.
A Proposal of UIP Score Based on CT with a Special Focus on Traction Bronchiectasis/Bronchiolectasis
In this article, we have reviewed the history and evolution of the concepts and classification of UIP and traction bronchiectasis based on the tremendous work of several pathologists, pulmonologists, radiologists, and investigators on ILA and TBI. Naturally, we may derive a simple scoring system for UIP based on CT findings with special emphasis on traction bronchiectasis/bronchiolectasis (Table 6) (Figs. 9, 10).
Table 6. UIP Score Defined by CT Findings with Emphasis on Presence and Extent of TB/Bronchiolectasis (Hatabu and Lee).
| ATS/ERS/JRS/ALAT | ILA [10] | TBI [13] | TB | UIP Score |
|---|---|---|---|---|
| Typical UIP | 3 | +++ (severe) and/or honeycombing | 4 | |
| Probable UIP (82.4% UIP/probable UIP) [45] | Subpleural fibrotic | 2 | + or ++ (mild to moderate) | 3 |
| Indeterminate UIP (54.2% UIP/probable UIP) [45] | Subpleural non-fibrotic | 1 | Bronchiolectasis only | 2 |
| Subpleural non-fibrotic | 0 | - (none) | 1 | |
| Inconsistent | Non-subpleural | 0 |
ALAT = Latin American Thoracic Association, ATS = American Thoracic Society, ERS = European Respiratory Society, ILA = interstitial lung abnormality, JRS = Japanese Respiratory Society, TBI = traction bronchiectasis index, UIP = usual interstitial pneumonia
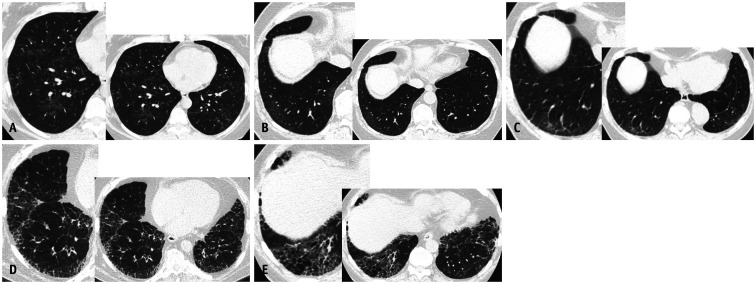
Fig. 9. UIP score defined by CT findings with emphasis on the presence and extent of traction bronchiectasis/bronchiolectasis (Hatabu and Lee as defined in Table 6).
A. UIP score = 0; non-subpleural ILA, TBI = 0, inconsistent for UIP. B. UIP score = 1; subpleural non-fibrotic ILA, TBI = 0, indeterminate UIP. C. UIP score = 2; subpleural non-fibrotic ILA, TBI = 1, indeterminate UIP. D. UIP score = 3; subpleural fibrotic ILA, TBI = 2, probable UIP. E. UIP score = 4; subpleural fibrotic ILA, TBI = 3, typical UIP. ILA = interstitial lung abnormalities, TBI = traction bronchiectasis index, UIP = usual interstitial pneumonia
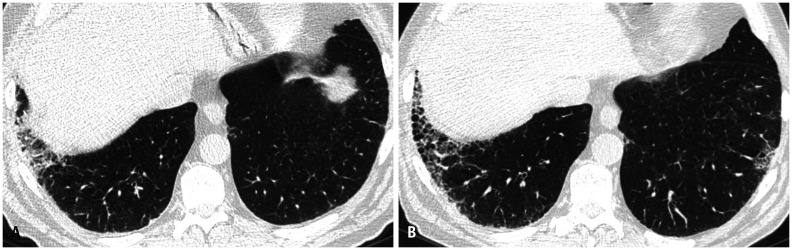
Fig. 10. Progression of fibrotic lung disease over 5 years.
A. Subpleural fibrotic interstitial lung abnormality (TBI = 2, UIP score 3, probable UIP). B. Subpleural fibrotic interstitial lung disease (TBI = 3, UIP score 4, typical UIP). TBI = traction bronchiectasis index, UIP = usual interstitial pneumonia
Future Directions and Conclusion
Traction bronchiectasis may facilitate a better understanding of the spectrum of ILD from ILA to IPF. The graded severity of traction bronchiectasis may facilitate the prediction of prognosis in ILAs. The progression of traction bronchiectasis is often observed in ILD patients during long-term follow-up evaluation. However, only a few studies have elaborated on the degree of or progression of traction bronchiectasis in ILD patients. Further studies are required to assess the exact extent of traction bronchiectasis from various viewpoints, including deep learning and artificial intelligence approaches, alternative approaches to quantitative analysis, and the correlation between radiology and pathology.
Acknowledgments
We are grateful for the librarians Myung-Ah Shim and Jaero Park for their dedicated support of manuscript formatting. Both librarians are working at the Samsung Medical Information & Media Services of Samsung Medical Center located in Seoul, South Korea.
Footnotes
Conflicts of Interest: Dr. Hatabu reports grants from Canon Medical Systems Inc, grants from Konica Minolta Inc, personal fees from Mitsubishi Chemical Co, personal fees from Canon Medical Systems Inc, outside the submitted work. Other authors have no potential conflicts of interest to disclose.
- Conceptualization: Takuya Hino, Kyung Soo Lee, Hiroto Hatabu.
- Data curation: Takuya Hino, Kyung Soo Lee.
- Investigation: Takuya Hino, Kyung Soo Lee.
- Project administration: Kyung Soo Lee, Hiroto Hatabu.
- Resources: Kyung Soo Lee, Hiroto Hatabu.
- Supervision: Kyung Soo Lee, Hiroto Hatabu.
- Visualization: Takuya Hino, Kyung Soo Lee, Joungho Han.
- Writing—original draft: Takuya Hino, Kyung Soo Lee, Joungho Han, Hiroto Hatabu.
- Writing—review & editing: Takuya Hino, Kyung Soo Lee, Joungho Han, Akinori Hata, Kosei Ishigami, Hiroto Hatabu.
References
- 1.Liebow AA, Carrington CB. The interstitial pneumonias. In: Simon M, Potchen EJ, LeMay M, editors. Frontiers of pulmonary radiology. 1st ed. New York: Grune & Stratton; 1969. pp. 102–141. [Google Scholar]
- 2.Katzenstein AL, Fiorelli RF. Nonspecific interstitial pneumonia/fibrosis. Histologic features and clinical significance. Am J Surg Pathol. 1994;18:136–147. [PubMed] [Google Scholar]
- 3.Nishimura K, Kitaichi M, Izumi T, Nagai S, Kanaoka M, Itoh H. Usual interstitial pneumonia: histologic correlation with high-resolution CT. Radiology. 1992;182:337–342. doi: 10.1148/radiology.182.2.1732946. [DOI] [PubMed] [Google Scholar]
- 4.Müller NL, Coiby TV. Idiopathic interstitial pneumonias: high-resolution CT and histologic findings. Radiographics. 1997;17:1016–1022. doi: 10.1148/radiographics.17.4.9225401. [DOI] [PubMed] [Google Scholar]
- 5.Johkoh T, Müller NL, Cartier Y, Kavanagh PV, Hartman TE, Akira M, et al. Idiopathic interstitial pneumonias: diagnostic accuracy of thin-section CT in 129 patients. Radiology. 1999;211:555–560. doi: 10.1148/radiology.211.2.r99ma01555. [DOI] [PubMed] [Google Scholar]
- 6.American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165:277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 7.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–e68. doi: 10.1164/rccm.201807-1255ST. [DOI] [PubMed] [Google Scholar]
- 9.Lynch DA, Sverzellati N, Travis WD, Brown KK, Colby TV, Galvin JR, et al. Diagnostic criteria for idiopathic pulmonary fibrosis: a Fleischner Society White Paper. Lancet Respir Med. 2018;6:138–153. doi: 10.1016/S2213-2600(17)30433-2. [DOI] [PubMed] [Google Scholar]
- 10.Hatabu H, Hunninghake GM, Richeldi L, Brown KK, Wells AU, Remy-Jardin M, et al. Interstitial lung abnormalities detected incidentally on CT: a Position Paper from the Fleischner Society. Lancet Respir Med. 2020;8:726–737. doi: 10.1016/S2213-2600(20)30168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sumikawa H, Johkoh T, Fujimoto K, Arakawa H, Colby TV, Fukuoka J, et al. Pathologically proved nonspecific interstitial pneumonia: CT pattern analysis as compared with usual interstitial pneumonia CT pattern. Radiology. 2014;272:549–556. doi: 10.1148/radiol.14130853. [DOI] [PubMed] [Google Scholar]
- 12.Putman RK, Gudmundsson G, Axelsson GT, Hida T, Honda O, Araki T, et al. Imaging patterns are associated with interstitial lung abnormality progression and mortality. Am J Respir Crit Care Med. 2019;200:175–183. doi: 10.1164/rccm.201809-1652OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hida T, Nishino M, Hino T, Lu J, Putman RK, Gudmundsson EF, et al. Traction bronchiectasis/bronchiolectasis is associated with interstitial lung abnormality mortality. Eur J Radiol. 2020;129:109073. doi: 10.1016/j.ejrad.2020.109073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katzenstein AL, Myers JL, Mazur MT. Acute interstitial pneumonia. A clinicopathologic, ultrastructural, and cell kinetic study. Am J Surg Pathol. 1986;10:256–267. [PubMed] [Google Scholar]
- 15.Myers JL, Veal CF, Jr, Shin MS, Katzenstein AL. Respiratory bronchiolitis causing interstitial lung disease. A clinicopathologic study of six cases. Am Rev Respir Dis. 1987;135:880–884. doi: 10.1164/arrd.1987.135.4.880. [DOI] [PubMed] [Google Scholar]
- 16.Ohori NP, Sciurba FC, Owens GR, Hodgson MJ, Yousem SA. Giant-cell interstitial pneumonia and hard-metal pneumoconiosis. A clinicopathologic study of four cases and review of the literature. Am J Surg Pathol. 1989;13:581–587. doi: 10.1097/00000478-198907000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Gibbs AR, Seal RM. Primary lymphoproliferative conditions of lung. Thorax. 1978;33:140–152. doi: 10.1136/thx.33.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katzenstein AL, Myers JL. Idiopathic pulmonary fibrosis: clinical relevance of pathologic classification. Am J Respir Crit Care Med. 1998;157:1301–1315. doi: 10.1164/ajrccm.157.4.9707039. [DOI] [PubMed] [Google Scholar]
- 19.Heppleston AG. The pathology of honeycomb lung. Thorax. 1956;11:77–93. doi: 10.1136/thx.11.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Genereux GP. The end-stage lung: pathogenesis, pathology, and radiology. Radiology. 1975;116:279–289. doi: 10.1148/116.2.279. [DOI] [PubMed] [Google Scholar]
- 21.Westcott JL, Cole SR. Traction bronchiectasis in end-stage pulmonary fibrosis. Radiology. 1986;161:665–669. doi: 10.1148/radiology.161.3.3786716. [DOI] [PubMed] [Google Scholar]
- 22.Cantin L, Bankier AA, Eisenberg RL. Bronchiectasis. AJR Am J Roentgenol. 2009;193:W158–W171. doi: 10.2214/AJR.09.3053. [DOI] [PubMed] [Google Scholar]
- 23.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 24.Kitaichi M. Pathologic features and the classification of interstitial pneumonia of unknown etiology. Bull Chest Dis Res Inst Kyoto Univ. 1990;23:1–18. [PubMed] [Google Scholar]
- 25.Nagai S, Kitaichi M, Itoh H, Nishimura K, Izumi T, Colby TV. Idiopathic nonspecific interstitial pneumonia/fibrosis: comparison with idiopathic pulmonary fibrosis and BOOP. Eur Respir J. 1998;12:1010–1019. doi: 10.1183/09031936.98.12051010. [DOI] [PubMed] [Google Scholar]
- 26.Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia. Am J Surg Pathol. 2000;24:19–33. doi: 10.1097/00000478-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR, et al. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;157:199–203. doi: 10.1164/ajrccm.157.1.9704130. [DOI] [PubMed] [Google Scholar]
- 28.Katzenstein AL, Mukhopadhyay S, Myers JL. Diagnosis of usual interstitial pneumonia and distinction from other fibrosing interstitial lung diseases. Hum Pathol. 2008;39:1275–1294. doi: 10.1016/j.humpath.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 29.Li X, Chen C, Xu J, Liu J, Yi X, Sun X, et al. Nonspecific interstitial pneumonia and usual interstitial pneumonia: comparison of the clinicopathologic features and prognosis. J Thorac Dis. 2014;6:1476–1481. doi: 10.3978/j.issn.2072-1439.2014.10.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, et al. Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001;164:1722–1727. doi: 10.1164/ajrccm.164.9.2103074. [DOI] [PubMed] [Google Scholar]
- 31.du Bois R, King TE., Jr Challenges in pulmonary fibrosis × 5: the NSIP/UIP debate. Thorax. 2007;62:1008–1012. doi: 10.1136/thx.2004.031039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nunes H, Schubel K, Piver D, Magois E, Feuillet S, Uzunhan Y, et al. Nonspecific interstitial pneumonia: survival is influenced by the underlying cause. Eur Respir J. 2015;45:746–755. doi: 10.1183/09031936.00148613. [DOI] [PubMed] [Google Scholar]
- 33.Silva CI, Müller NL, Lynch DA, Curran-Everett D, Brown KK, Lee KS, et al. Chronic hypersensitivity pneumonitis: differentiation from idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia by using thin-section CT. Radiology. 2008;246:288–297. doi: 10.1148/radiol.2453061881. [DOI] [PubMed] [Google Scholar]
- 34.Kligerman SJ, Groshong S, Brown KK, Lynch DA. Nonspecific interstitial pneumonia: radiologic, clinical, and pathologic considerations. Radiographics. 2009;29:73–87. doi: 10.1148/rg.291085096. [DOI] [PubMed] [Google Scholar]
- 35.Kim TS, Lee KS, Chung MP, Han J, Park JS, Hwang JH, et al. Nonspecific interstitial pneumonia with fibrosis: high-resolution CT and pathologic findings. AJR Am J Roentgenol. 1998;171:1645–1650. doi: 10.2214/ajr.171.6.9843306. [DOI] [PubMed] [Google Scholar]
- 36.Mink SN, Maycher B. Comparative manifestations and diagnostic accuracy of high-resolution computed tomography in usual interstitial pneumonia and nonspecific interstitial pneumonia. Curr Opin Pulm Med. 2012;18:530–534. doi: 10.1097/MCP.0b013e3283568026. [DOI] [PubMed] [Google Scholar]
- 37.Travis WD, Hunninghake G, King TE, Jr, Lynch DA, Colby TV, Galvin JR, et al. Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Respir Crit Care Med. 2008;177:1338–1347. doi: 10.1164/rccm.200611-1685OC. [DOI] [PubMed] [Google Scholar]
- 38.MacDonald SL, Rubens MB, Hansell DM, Copley SJ, Desai SR, du Bois RM, et al. Nonspecific interstitial pneumonia and usual interstitial pneumonia: comparative appearances at and diagnostic accuracy of thin-section CT. Radiology. 2001;221:600–605. doi: 10.1148/radiol.2213010158. [DOI] [PubMed] [Google Scholar]
- 39.Hunninghake GW, Zimmerman MB, Schwartz DA, King TE, Jr, Lynch J, Hegele R, et al. Utility of a lung biopsy for the diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2001;164:193–196. doi: 10.1164/ajrccm.164.2.2101090. [DOI] [PubMed] [Google Scholar]
- 40.Sverzellati N, Wells AU, Tomassetti S, Desai SR, Copley SJ, Aziz ZA, et al. Biopsy-proved idiopathic pulmonary fibrosis: spectrum of nondiagnostic thin-section CT diagnoses. Radiology. 2010;254:957–964. doi: 10.1148/radiol.0990898. [DOI] [PubMed] [Google Scholar]
- 41.Lee HY, Lee KS, Jeong YJ, Hwang JH, Kim HJ, Chung MP, et al. High-resolution CT findings in fibrotic idiopathic interstitial pneumonias with little honeycombing: serial changes and prognostic implications. AJR Am J Roentgenol. 2012;199:982–989. doi: 10.2214/AJR.11.8192. [DOI] [PubMed] [Google Scholar]
- 42.Lynch DA, Newell JD, Logan PM, King TE, Jr, Müller NL. Can CT distinguish hypersensitivity pneumonitis from idiopathic pulmonary fibrosis? AJR Am J Roentgenol. 1995;165:807–811. doi: 10.2214/ajr.165.4.7676971. [DOI] [PubMed] [Google Scholar]
- 43.Quadrelli S, Molinari L, Ciallella L, Spina JC, Sobrino E, Chertcoff J. Radiological versus histopathological diagnosis of usual interstitial pneumonia in the clinical practice: does it have any survival difference? Respiration. 2009;79:32–37. doi: 10.1159/000225987. [DOI] [PubMed] [Google Scholar]
- 44.Yagihashi K, Huckleberry J, Colby TV, Tazelaar HD, Zach J, Sundaram B, et al. Radiologic-pathologic discordance in biopsy-proven usual interstitial pneumonia. Eur Respir J. 2016;47:1189–1197. doi: 10.1183/13993003.01680-2015. [DOI] [PubMed] [Google Scholar]
- 45.Chung JH, Chawla A, Peljto AL, Cool CD, Groshong SD, Talbert JL, et al. CT scan findings of probable usual interstitial pneumonitis have a high predictive value for histologic usual interstitial pneumonitis. Chest. 2015;147:450–459. doi: 10.1378/chest.14-0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raghu G, Lynch D, Godwin JD, Webb R, Colby TV, Leslie KO, et al. Diagnosis of idiopathic pulmonary fibrosis with high-resolution CT in patients with little or no radiological evidence of honeycombing: secondary analysis of a randomised, controlled trial. Lancet Respir Med. 2014;2:277–284. doi: 10.1016/S2213-2600(14)70011-6. [DOI] [PubMed] [Google Scholar]
- 47.Brownell R, Moua T, Henry TS, Elicker BM, White D, Vittinghoff E, et al. The use of pretest probability increases the value of high-resolution CT in diagnosing usual interstitial pneumonia. Thorax. 2017;72:424–429. doi: 10.1136/thoraxjnl-2016-209671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Flaherty KR, Toews GB, Lynch JP, 3rd, Kazerooni EA, Gross BH, Strawderman RL, et al. Steroids in idiopathic pulmonary fibrosis: a prospective assessment of adverse reactions, response to therapy, and survival. Am J Med. 2001;110:278–282. doi: 10.1016/s0002-9343(00)00711-7. [DOI] [PubMed] [Google Scholar]
- 49.Parambil JG, Myers JL, Ryu JH. Histopathologic features and outcome of patients with acute exacerbation of idiopathic pulmonary fibrosis undergoing surgical lung biopsy. Chest. 2005;128:3310–3315. doi: 10.1378/chest.128.5.3310. [DOI] [PubMed] [Google Scholar]
- 50.Collard HR, Ryu JH, Douglas WW, Schwarz MI, Curran-Everett D, King TE, Jr, et al. Combined corticosteroid and cyclophosphamide therapy does not alter survival in idiopathic pulmonary fibrosis. Chest. 2004;125:2169–2174. doi: 10.1378/chest.125.6.2169. [DOI] [PubMed] [Google Scholar]
- 51.Pereira CA, Malheiros T, Coletta EM, Ferreira RG, Rubin AS, Otta JS, et al. Survival in idiopathic pulmonary fibrosis-cytotoxic agents compared to corticosteroids. Respir Med. 2006;100:340–347. doi: 10.1016/j.rmed.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 52.Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354:2655–2666. doi: 10.1056/NEJMoa055120. [DOI] [PubMed] [Google Scholar]
- 53.Keir GJ, Maher TM, Ming D, Abdullah R, de Lauretis A, Wickremasinghe M, et al. Rituximab in severe, treatment-refractory interstitial lung disease. Respirology. 2014;19:353–359. doi: 10.1111/resp.12214. [DOI] [PubMed] [Google Scholar]
- 54.Mason DP, Brizzio ME, Alster JM, McNeill AM, Murthy SC, Budev MM, et al. Lung transplantation for idiopathic pulmonary fibrosis. Ann Thorac Surg. 2007;84:1121–1128. doi: 10.1016/j.athoracsur.2007.04.096. [DOI] [PubMed] [Google Scholar]
- 55.King TE, Jr, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2083–2092. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 56.Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 57.Collins BF, Raghu G. Antifibrotic therapy for fibrotic lung disease beyond idiopathic pulmonary fibrosis. Eur Respir Rev. 2019;28:190022. doi: 10.1183/16000617.0022-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lamas DJ, Kawut SM, Bagiella E, Philip N, Arcasoy SM, Lederer DJ. Delayed access and survival in idiopathic pulmonary fibrosis: a cohort study. Am J Respir Crit Care Med. 2011;184:842–847. doi: 10.1164/rccm.201104-0668OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Maher TM, Strek ME. Antifibrotic therapy for idiopathic pulmonary fibrosis: time to treat. Respir Res. 2019;20:205. doi: 10.1186/s12931-019-1161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosas IO, Ren P, Avila NA, Chow CK, Franks TJ, Travis WD, et al. Early interstitial lung disease in familial pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176:698–705. doi: 10.1164/rccm.200702-254OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Copley SJ, Wells AU, Hawtin KE, Gibson DJ, Hodson JM, Jacques AE, et al. Lung morphology in the elderly: comparative CT study of subjects over 75 years old versus those under 55 years old. Radiology. 2009;251:566–573. doi: 10.1148/radiol.2512081242. [DOI] [PubMed] [Google Scholar]
- 62.Lederer DJ, Enright PL, Kawut SM, Hoffman EA, Hunninghake G, van Beek EJ, et al. Cigarette smoking is associated with subclinical parenchymal lung disease: the Multi-Ethnic Study of Atherosclerosis (MESA)-lung study. Am J Respir Crit Care Med. 2009;180:407–414. doi: 10.1164/rccm.200812-1966OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gückel C, Hansell DM. Imaging the ‘dirty lung’--has high resolution computed tomography cleared the smoke? Clin Radiol. 1998;53:717–722. doi: 10.1016/s0009-9260(98)80312-7. [DOI] [PubMed] [Google Scholar]
- 64.Gochuico BR, Avila NA, Chow CK, Novero LJ, Wu HP, Ren P, et al. Progressive preclinical interstitial lung disease in rheumatoid arthritis. Arch Intern Med. 2008;168:159–166. doi: 10.1001/archinternmed.2007.59. [DOI] [PubMed] [Google Scholar]
- 65.Miller ER, Putman RK, Vivero M, Hung Y, Araki T, Nishino M, et al. Histopathology of interstitial lung abnormalities in the context of lung nodule resections. Am J Respir Crit Care Med. 2018;197:955–958. doi: 10.1164/rccm.201708-1679LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hatabu H, Hunninghake GM, Lynch DA. Interstitial lung abnormality: recognition and perspectives. Radiology. 2019;291:1–3. doi: 10.1148/radiol.2018181684. [DOI] [PubMed] [Google Scholar]
- 67.Washko GR, Lynch DA, Matsuoka S, Ross JC, Umeoka S, Diaz A, et al. Identification of early interstitial lung disease in smokers from the COPDGene Study. Acad Radiol. 2010;17:48–53. doi: 10.1016/j.acra.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Washko GR, Hunninghake GM, Fernandez IE, Nishino M, Okajima Y, Yamashiro T, et al. Lung volumes and emphysema in smokers with interstitial lung abnormalities. N Engl J Med. 2011;364:897–906. doi: 10.1056/NEJMoa1007285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hunninghake GM, Hatabu H, Okajima Y, Gao W, Dupuis J, Latourelle JC, et al. MUC5B promoter polymorphism and interstitial lung abnormalities. N Engl J Med. 2013;368:2192–2200. doi: 10.1056/NEJMoa1216076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Doyle TJ, Washko GR, Fernandez IE, Nishino M, Okajima Y, Yamashiro T, et al. Interstitial lung abnormalities and reduced exercise capacity. Am J Respir Crit Care Med. 2012;185:756–762. doi: 10.1164/rccm.201109-1618OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Araki T, Putman RK, Hatabu H, Gao W, Dupuis J, Latourelle JC, et al. Development and progression of interstitial lung abnormalities in the Framingham Heart Study. Am J Respir Crit Care Med. 2016;194:1517–1522. doi: 10.1164/rccm.201512-2523OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Putman RK, Hatabu H, Araki T, Gudmundsson G, Gao W, Nishino M, et al. Association between interstitial lung abnormalities and all-cause mortality. JAMA. 2016;315:672–681. doi: 10.1001/jama.2016.0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Richeldi L, Collard HR, Jones MG. Idiopathic pulmonary fibrosis. Lancet. 2017;389:1941–1952. doi: 10.1016/S0140-6736(17)30866-8. [DOI] [PubMed] [Google Scholar]
- 74.Silva CI, Müller NL, Hansell DM, Lee KS, Nicholson AG, Wells AU. Nonspecific interstitial pneumonia and idiopathic pulmonary fibrosis: changes in pattern and distribution of disease over time. Radiology. 2008;247:251–259. doi: 10.1148/radiol.2471070369. [DOI] [PubMed] [Google Scholar]
- 75.Tsushima K, Sone S, Yoshikawa S, Yokoyama T, Suzuki T, Kubo K. The radiological patterns of interstitial change at an early phase: over a 4-year follow-up. Respir Med. 2010;104:1712–1721. doi: 10.1016/j.rmed.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 76.Sverzellati N, Guerci L, Randi G, Calabrò E, La Vecchia C, Marchianò A, et al. Interstitial lung diseases in a lung cancer screening trial. Eur Respir J. 2011;38:392–400. doi: 10.1183/09031936.00201809. [DOI] [PubMed] [Google Scholar]
- 77.Jin GY, Lynch D, Chawla A, Garg K, Tammemagi MC, Sahin H, et al. Interstitial lung abnormalities in a CT lung cancer screening population: prevalence and progression rate. Radiology. 2013;268:563–571. doi: 10.1148/radiol.13120816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Putman RK, Rosas IO, Hunninghake GM. Genetics and early detection in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2014;189:770–778. doi: 10.1164/rccm.201312-2219PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hunninghake GM. Interstitial lung abnormalities: erecting fences in the path towards advanced pulmonary fibrosis. Thorax. 2019;74:506–511. doi: 10.1136/thoraxjnl-2018-212446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Antoniou KM, Tzilas V, Vasarmidi E, Symvoulakis EK, Tzouvelekis A, Bouros D. Interstitial lung abnormalities: ignotum per ignotius. Lancet Respir Med. 2019;7:376–378. doi: 10.1016/S2213-2600(19)30052-9. [DOI] [PubMed] [Google Scholar]
- 81.Hoyer N, Thomsen LH, Wille MMW, Wilcke T, Dirksen A, Pedersen JH, et al. Increased respiratory morbidity in individuals with interstitial lung abnormalities. BMC Pulm Med. 2020;20:67. doi: 10.1186/s12890-020-1107-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hoyer N, Wille MMW, Thomsen LH, Wilcke T, Dirksen A, Pedersen JH, et al. Interstitial lung abnormalities are associated with increased mortality in smokers. Respir Med. 2018;136:77–82. doi: 10.1016/j.rmed.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 83.Whittaker Brown SA, Padilla M, Mhango G, Powell C, Salvatore M, Henschke C, et al. Interstitial lung abnormalities and lung cancer risk in the National Lung Screening Trial. Chest. 2019;156:1195–1203. doi: 10.1016/j.chest.2019.06.041. [DOI] [PubMed] [Google Scholar]
- 84.Putman RK, Hunninghake GM, Dieffenbach PB, Barragan-Bradford D, Serhan K, Adams U, et al. Interstitial lung abnormalities are associated with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:138–141. doi: 10.1164/rccm.201604-0818LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wolters PJ, Collard HR, Jones KD. Pathogenesis of idiopathic pulmonary fibrosis. Annu Rev Pathol. 2014;9:157–179. doi: 10.1146/annurev-pathol-012513-104706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chilosi M, Poletti V, Murer B, Lestani M, Cancellieri A, Montagna L, et al. Abnormal re-epithelialization and lung remodeling in idiopathic pulmonary fibrosis: the role of deltaN-p63. Lab Invest. 2002;82:1335–1345. doi: 10.1097/01.lab.0000032380.82232.67. [DOI] [PubMed] [Google Scholar]
- 87.Mohning MP, Richards JC, Huie TJ. Idiopathic pulmonary fibrosis: the radiologist’s role in making the diagnosis. Br J Radiol. 2019;92:20181003. doi: 10.1259/bjr.20181003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Watadani T, Sakai F, Johkoh T, Noma S, Akira M, Fujimoto K, et al. Interobserver variability in the CT assessment of honeycombing in the lungs. Radiology. 2013;266:936–944. doi: 10.1148/radiol.12112516. [DOI] [PubMed] [Google Scholar]
- 89.Staats P, Kligerman S, Todd N, Tavora F, Xu L, Burke A. A comparative study of honeycombing on high resolution computed tomography with histologic lung remodeling in explants with usual interstitial pneumonia. Pathol Res Pract. 2015;211:55–61. doi: 10.1016/j.prp.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 90.Piciucchi S, Tomassetti S, Ravaglia C, Gurioli C, Gurioli C, Dubini A, et al. From “traction bronchiectasis” to honeycombing in idiopathic pulmonary fibrosis: a spectrum of bronchiolar remodeling also in radiology? BMC Pulm Med. 2016;16:87. doi: 10.1186/s12890-016-0245-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Johkoh T, Müller NL, Colby TV, Ichikado K, Taniguchi H, Kondoh Y, et al. Nonspecific interstitial pneumonia: correlation between thin-section CT findings and pathologic subgroups in 55 patients. Radiology. 2002;225:199–204. doi: 10.1148/radiol.2251011555. [DOI] [PubMed] [Google Scholar]
- 92.Jacob J, Aksman L, Mogulkoc N, Procter AJ, Gholipour B, Cross G, et al. Serial CT analysis in idiopathic pulmonary fibrosis: comparison of visual features that determine patient outcome. Thorax. 2020;75:648–654. doi: 10.1136/thoraxjnl-2019-213865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sumikawa H, Johkoh T, Colby TV, Ichikado K, Suga M, Taniguchi H, et al. Computed tomography findings in pathological usual interstitial pneumonia: relationship to survival. Am J Respir Crit Care Med. 2008;177:433–439. doi: 10.1164/rccm.200611-1696OC. [DOI] [PubMed] [Google Scholar]
- 94.Yamauchi H, Bando M, Baba T, Kataoka K, Yamada Y, Yamamoto H, et al. Clinical course and changes in high-resolution computed tomography findings in patients with idiopathic pulmonary fibrosis without honeycombing. PLoS One. 2016;11:e0166168. doi: 10.1371/journal.pone.0166168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Edey AJ, Devaraj AA, Barker RP, Nicholson AG, Wells AU, Hansell DM. Fibrotic idiopathic interstitial pneumonias: HRCT findings that predict mortality. Eur Radiol. 2011;21:1586–1593. doi: 10.1007/s00330-011-2098-2. [DOI] [PubMed] [Google Scholar]
- 96.Walsh SL, Sverzellati N, Devaraj A, Wells AU, Hansell DM. Chronic hypersensitivity pneumonitis: high resolution computed tomography patterns and pulmonary function indices as prognostic determinants. Eur Radiol. 2012;22:1672–1679. doi: 10.1007/s00330-012-2427-0. [DOI] [PubMed] [Google Scholar]