Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has impacted various aspects of daily living and has influenced the life of every individual in a unique way. Acute myocardial infarction (AMI) is associated with high morbidity and mortality; thus, timely treatment is crucial to prevent poor prognosis. Therefore, an immediate emergency department (ED) visit is required; however, no domestic studies have reported the effect of COVID-19 on ED visits by patients with AMI. Therefore, this study aimed to assess the changes in the pattern of ED visits by patients with AMI by comparing visits during the COVID-19 outbreak period to those during two control periods.
Methods
This nationwide, retrospective study used registry data of the National Emergency Department Information System. The ‘outbreak period’ was defined as the period between February 21, 2020 and April 1, 2020, while the ‘control period’ was defined as the same time period in the preceding two years (2018 and 2019). The primary outcome of our study was the number of patients admitted to the ED owing to AMI during the outbreak and control periods. Secondary outcomes were time from symptom onset to ED visit, length of ED stay, and 30-day mortality following admission.
Results
During the outbreak period, 401,378 patients visited the ED; this number was lower than that during the control periods (2018: 577,548; 2019: 598,514). The number of patients with AMI visiting the ED was lower during the outbreak period (2,221) than during 2018 (2,437) and 2019 (2,591).
Conclusion
The COVID-19 pandemic has caused a reduction in ED visits by patients with AMI. We assume that this could likely be caused by misinterpretation of AMI symptoms as symptoms of respiratory infection, fear of contracting severe acute respiratory syndrome coronavirus 2, and restrictions in accessing emergency medical care owing to overburdened healthcare facilities. This study sheds light on the fact that healthcare and emergency medical staff members must work towards eliminating hurdles due to this pandemic for patients to receive timely emergency care, which in turn will help curb the growing burden of mortality.
Keywords: COVID-19, Emergency Care, Myocardial Infarction
Graphical Abstract
INTRODUCTION
Coronavirus disease 2019 (COVID-19) was first reported in China in December, 2019. It then spread globally, following which the World Health Organization declared COVID-19 a pandemic on March 12, 2020. As of November 29, 2020, there have been over 61.8 million cases and over 1.4 million deaths reported globally.1 In Korea, the first case of COVID-19 was reported on January 20, 2020, and as of December 8, there have been 38,755 confirmed cases of COVID-19 with approximately 552 deaths.2
Such epidemics influence various aspects of daily living and cause changes in the pattern and number of medical visits. These changes were observed during the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) outbreaks; relevant findings have been reported. During the SARS outbreak, there was a decrease in the total number of emergency department (ED) visits, primarily of patients presenting with respiratory symptoms. Some studies reported that changes in healthcare utilization differed across age groups, while other studies reported a reduction in the number of ED visits alone.3,4
As many studies investigated the changes in trends of ED visits during the MERS outbreak, it has been reported that South Korea had similar experiences during the MERS epidemic in 2015. While the total number of ED visits decreased, the change was more evident for pediatric and non-emergency cases.5 Another study reported a similar finding wherein the total number of ED visits decreased with marked changes with respect to non-emergency cases; however, the same study reported that there were no grave changes observed in regard to severe illnesses and ED mortality.6 Additionally, a study reported an increasing trend in ED visits owing to fever.7
Studies are now reporting that COVID-19 is also causing a shift in healthcare utilization. A study conducted in the United States that retrospectively analyzed data from the National Center for Immunization and Respiratory Diseases stated that a decrease in the total number of ED visits raised concerns regarding severely ill patients not being able to visit hospitals.8
In Korea, a study reported a decrease in the number of outpatient and ED visits by patients with spinal disorders; however, no changes were observed in the number of surgeries performed.9 While another study reported decreased healthcare utilization in patients with rheumatoid arthritis.10
Acute myocardial infarction (AMI) is a critical disease with high rates of mortality and morbidity, and this condition requires timely treatment. Therefore, an immediate ED visit is required; however, no domestic studies have reported the effect of COVID-19 on ED visits by patients with AMI.
We investigated the effect of the COVID-19 pandemic on ED visits due to AMI and the prognosis of myocardial infarction when compared with those during the control period.
METHODS
Study design and data source
This was a nationwide, retrospective study. The registry data of the National Emergency Department Information System (NEDIS) managed by the National Emergency Medical Center (NEMC) were used. NEDIS is a prospective collection of data on the demographic and baseline clinical characteristics of patients from all emergency healthcare facilities. Since 2016, all emergency healthcare facilities in Korea have been required to adopt the NEDIS-based registration system that is utilized in the evaluation of emergency healthcare facilities and payment systems. The number of emergency healthcare facilities participating in the NEDIS registry is 408 out of 413 in 2016(98.8%), 413 out of 416 in 2017(99.3%), 399 out of 401 in 2018(99.5%), 401 out of 402(99.8%) in 2019, and 403 out of 403(100%) in 2020. Detailed information about types and numbers of facilities was presented in Supplementary Table 1. Healthcare providers and administrators in regional emergency medical centers are required to input data related to the NEDIS system and to hire coordinators from the NEMC to be in charge of hospital-based monitoring and feedback.
The registry data consist of approximately 60 items that can be divided according to the following factors: demographics including age, gender, identification number, address, type of medical insurance; baseline characteristics including symptom onset time, route of visit, mode of visit, ED visit time, ED discharge time, chief complaint, KTAS level, ICD-10 based diagnosis, vital signs at presentation, and ED disposition.11,12
Study period
The period between February 21, 2020, and April 1, 2020, which was amidst the COVID-19 outbreak, was defined as the ‘outbreak period,’ and the same time periods during 2018 and 2019 were defined as the ‘control period’ to compare patients during the two periods. The start date of the outbreak period was defined as the first day when the number of patients occurred more than 100 per day. The end date of the outbreak period is defined as the first date on which the daily number of patients is maintained at or below 100 until one week after the end date. The dates corresponding to the criteria were from February 21 to April 1, 2020 in Korea.
Data collection
In this study, we obtained the following codes: date of visit, time of visit, age group, sex, date of onset, time of onset, route of visit, mode of visit, systolic blood pressure (SBP) at visit, diastolic blood pressure (DBP) at visit, pulse rate at visit, breathing rate at visit, body temperature at visit, oxygen saturation at visit, outcome of emergency care, date of discharge, time of discharge, post-admission outcomes, diagnosis code at discharge, diagnosis category code at discharge, procedural code at ED, and procedural code after admission from the NEDIS data for analysis.
Operational definitions of AMI patients
Health insurance data or NEDIS data are collected for claims or emergency medical system monitoring purposes and thus do not contain detailed clinical information such as clinical data, which may undermine the accuracy of the study. To address this shortcoming, operational definitions of each disease should be utilized, as they will reduce potential overestimations or underestimations.13 According to Ahn,13 a more stable incidence estimation can be obtained using an operational definition that simultaneously utilizes disease codes and procedural codes when computing the incidence of AMI, which is less influenced by other conditions and changes in the claims-related system.14
In the present study, patients with ICD code I21 (AMI) as the primary or secondary diagnosis at discharge from the ED or hospital were selected from the NEDIS data. Regarding the procedural code, patients given a code for AMI-related procedures as the procedure in the ED or after admission were selected from the NEDIS data. The AMI-related procedure codes were determined based on a previous report.13 Detailed information about procedure codes was presented in Supplementary Table 2.
Patients who met both the criteria of the disease code and procedure code were defined as patients with AMI.
Primary outcome
The primary outcome was defined as the number of patients admitted to the ED due to AMI during the control and outbreak periods. Further, to assess the reduction in ED visits, the percentage of ED visits in 2020 compared with those in the same periods in 2018 and 2019 was calculated as follows:
Secondary outcome
In addition to the primary outcome, the following three outcomes were analyzed as secondary outcomes: time from symptom onset to ED visit, length of ED stay, and mortality within 30 days of admission.
Statistical analysis
Nominal variables consisting of two categories were analyzed using the Pearson χ2 test or Fisher's exact test, and the results are expressed as frequencies and percentages. For continuous variables, we determined normality based on the shape of the graph, the comparison between the mean and median values, skewness, and kurtosis. Variables with normal distribution were analyzed using Student's t-test and expressed as means and standard deviations. Skewed variables were tested using the Wilcoxon rank-sum test and expressed as the median and interquartile range. Data analysis was conducted using SAS (version 9.4; SAS Institute, Inc., Cary, NC, USA).
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of the NEMC (No.NMC-2007-026). The requirement of informed consent was waived owing to the retrospective nature of the study.
RESULTS
Characteristics of study subjects
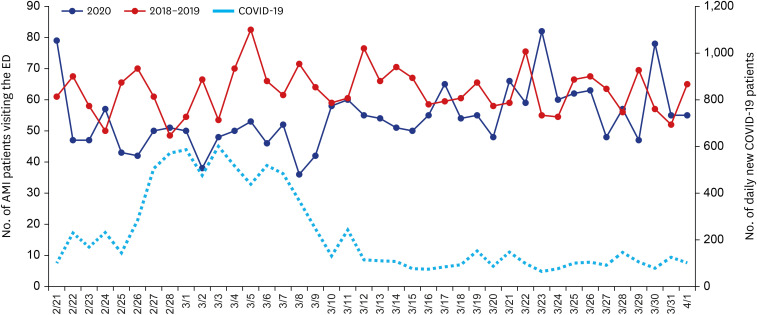
A total of 1,577,440 patients visited the ED during the study period. During the outbreak period, 401,378 patients visited the ED, which was lower than that in both 2018 (577,548 patients) and 2019 (598,514 patients). Additionally, the number of AMI patients presenting to the ED during the outbreak (2,221) was also lower than that in 2018 (2,437 patients) and 2019 (2,591 patients) (Fig. 1).
Fig. 1. Trend of daily COVID-19 confirmed patients, AMI patients visiting ED in outbreak, control period.
AMI = acute myocardial infarction, ED = emergency department, COVID-19 = coronavirus disease 2019.
Demographic and clinical differences between the control period and outbreak period
There were no significant differences in age and sex between the patients during the outbreak and control periods. The percentage of patients transferred from another hospital decreased by 3.35% during the outbreak period. There were no marked differences in SBP, DBP, pulse rate, breathing rate, body temperature, and oxygen saturation between the two groups (Table 1).
Table 1. Demographic and clinical differences between control period and outbreak period.
| Variables | Control perioda | Outbreak periodb | P value | |
|---|---|---|---|---|
| Age, yr | 65.15 ± 13.25 | 64.65 ± 13.31 | 0.137 | |
| Male | 3,757 (74.72) | 1,699 (76.50) | 0.106 | |
| Transportation by ambulance | 2,776 (55.21) | 1,219 (54.89) | 0.797 | |
| Transferred from other hospitals | 1,907 (37.93) | 768 (34.58) | 0.007** | |
| Coronary angiography or percutaneous coronary intervention | 3,215 | 1,187 | ||
| Vital signs at ED presentation | ||||
| SBP, mmHg | 136.38 ± 31.01 | 137.48 ± 30.99 | 0.182 | |
| DBP, mmHg | 81.42 ± 18.43 | 82.67 ± 19.06 | 0.012* | |
| PR, beats/min | 82.29 ± 21.86 | 83.43 ± 21.96 | 0.048* | |
| RR, breaths/min | 20.02 ± 3.50 | 19.84 ± 3.32 | 0.054 | |
| Temperature, °C | 36.38 ± 0.62 | 36.34 ± 0.62 | 0.011* | |
| SpO2 | 96.56 ± 5.28 | 96.57 ± 5.41 | 0.921 | |
Data are shown as mean ± standard deviation or number (%).
ED = emergency department, SBP = systolic blood pressure, DBP = diastolic blood pressure, PR = pulse rate, RR = respiratory rate.
aFebruary 21 to April 1 in 2018–2019; bFebruary 21 to April 1 in 2020.
*P < 0.05, **P < 0.01.
Primary outcome: ratio of ED visits by AMI patients
The ratio of ED visits by AMI patients during the outbreak period was 88.35%, which was reduced by approximately 10% when compared with that in 2018 (96.94%) and 2019 (103.06%). The ratio was the lowest for women under the age of 60 (76.68%) and the highest for men over the age of 80 (97.9%). While the number of AMI patients visiting the ED during the outbreak period was lower than that during the control period, the proportion of ED visits by AMI patients was higher at 0.55% than that in 2018 (0.42%) and 2019 (0.43%) (Fig. 1 and Table 2).
Table 2. Primary outcomes between control period and outbreak period.
| Primary outcomes | 2018a | 2019a | 2020a | |
|---|---|---|---|---|
| Total | ||||
| Total ED visits | 577,548 | 598,514 | 401,378 | |
| AMI patients | 2,437 (0.42) | 2,591 (0.43) | 2,221 (0.55) | |
| Ratio of ED visits of AMI patients, % | 96.94 | 103.06 | 88.35 | |
| Male total | ||||
| Total ED visits | 296,982 | 307,414 | 210,019 | |
| AMI patients | 1,804 (0.6) | 1,953 (0.64) | 1,699 (0.81) | |
| Ratio of ED visits of AMI patients, % | 96.03 | 103.96 | 90.44 | |
| Male age, yr < 60 | ||||
| Total ED visits | 211,964 | 215,872 | 139,492 | |
| AMI patients | 745 (0.35) | 819 (0.38) | 730 (0.52) | |
| Ratio of ED visits of AMI patients, % | 95.27 | 104.73 | 93.35 | |
| Male age, 60 ≤ yr ≤ 79 | ||||
| Total ED visits | 67,364 | 71,941 | 54,763 | |
| AMI patients | 883 (1.31) | 930 (1.29) | 783 (1.43) | |
| Ratio of ED visits of AMI patients, % | 97.4 | 102.6 | 86.38 | |
| Male age, yr ≥ 80 | ||||
| Total ED visits | 17,654 | 19,601 | 15,764 | |
| AMI patients | 176 (0.1) | 204 (1.04) | 186 (1.08) | |
| Ratio of ED visits of AMI patients, % | 92.63 | 107.37 | 97.9 | |
| Female total | ||||
| Total ED visits | 280,566 | 291,100 | 191,359 | |
| AMI patients | 633 (0.23) | 638 (0.22) | 522 (0.27) | |
| Ratio of ED visits of AMI patients, % | 99.6 | 100.39 | 82.14 | |
| Female age, yr < 60 | ||||
| Total ED visits | 194,504 | 198,889 | 124,306 | |
| AMI patients | 110 (0.06) | 83 (0.04) | 74 (0.06) | |
| Ratio of ED visits of AMI patients, % | 113.99 | 86.01 | 76.68 | |
| Female age, 60 ≤ yr ≤ 79 | ||||
| Total ED visits | 59,892 | 63,188 | 44,902 | |
| AMI patients | 313 (0.52) | 347 (0.55) | 292 (0.65) | |
| Ratio of ED visits of AMI patients, % | 94.85 | 105.15 | 88.48 | |
| Female age, 80 ≤ yr | ||||
| Total ED visits | 26,170 | 29,023 | 22,151 | |
| AMI patients | 210 (0.8) | 208 (0.72) | 156 (0.7) | |
| Ratio of ED visits of AMI patients, % | 99.6 | 100.39 | 82.14 | |
Values are presented as number (%).
ED = emergency department, AMI = acute myocardial infarction.
aPeriod: February 21 to April 1.
Secondary outcomes
The median time from symptom onset to ED visit was 3.24 hours during the outbreak period and 3.15 hours during the control period, showing no significant differences. However, it showed a statistically significant difference in women under 60 (3.35 hours vs. 8.86 hours, P = 0.002). Meanwhile, the median length of ED visits during the control and outbreak periods showed a significant difference, however, not large (2.73 hours vs. 2.6 hours, P = 0.026). The rate of 30-day mortality after admission was 4.89% during the control period and 5.99% in the outbreak period, showing merely a 1% difference, which was not significant. In men aged 60 to 80 years of age, the difference in mortality within 30 days of admission in the outbreak period was statistically significant compared to the control period (4.03% vs. 6%) (Table 3).
Table 3. Comparison of secondary outcomes between control period and outbreak period.
| Secondary outcomes | Control perioda | Outbreak periodb | P value | |
|---|---|---|---|---|
| Total | ||||
| Symptom onset to ED visit, hr | 3.15 (1–15.05) | 3.24 (1.10–14.43) | 0.264 | |
| EDLOS, hr | 2.73 (1.12–6.61) | 2.60 (1.05–5.80) | 0.026* | |
| Mortality within 30 day of hospitalization | 246 (4.89) | 133 (5.99) | 0.053 | |
| Male total | ||||
| Symptom onset to ED visit, hr | 2.92 (1–12.7) | 2.92 (1–12.31) | 0.420 | |
| EDLOS, hr | 2.48 (1.05–6.2) | 2.4 (1–5.6) | 0.129 | |
| Mortality within 30 day of hospitalization | 147 (3.91) | 88 (5.18) | 0.037* | |
| Male age, yr < 60 | ||||
| Symptom onset to ED visit, hr | 2.48 (0.92–10.43) | 2.51 (1–9) | 0.332 | |
| EDLOS, hr | 2.16 (0.93–5.75) | 2.01 (0.93–4.43) | 0.092 | |
| Mortality within 30 day of hospitalization | 30 (1.92) | 21 (2.88) | 0.147 | |
| Male age, 60 ≤ yr ≤ 79 | ||||
| Symptom onset to ED visit, hr | 2.95 (1–13.92) | 2.94 (1–13.36) | 0.769 | |
| EDLOS, hr | 2.6 (1.12–6.37) | 2.57 (1.03–6) | 0.374 | |
| Mortality within 30 day of hospitalization | 73 (4.03) | 47 (6) | 0.028* | |
| Male age, yr ≥ 80 | ||||
| Symptom onset to ED visit, hr | 4 (1.51–22.17) | 5.55 (1.5–27.56) | 0.191 | |
| EDLOS, hr | 3.17 (1.33–6.57) | 3.53 (1.52–7.68) | 0.301 | |
| Mortality within 30 day of hospitalization | 44 (11.58) | 20 (10.75) | 0.770 | |
| Female total | ||||
| Symptom onset to ED visit, hr | 4.7 (1.5–23.95) | 5.1 (2–23.91) | 0.191 | |
| EDLOS, hr | 3.38 (1.4–8) | 3.2 (1.38–6.65) | 0.054 | |
| Mortality within 30 day of hospitalization | 99 (7.79) | 45 (8.62) | 0.556 | |
| Female age, yr < 60 | ||||
| Symptom onset to ED visit, hr | 3.35 (1–17.32) | 8.86 (2.53–24.13) | 0.002** | |
| EDLOS, hr | 3.71 (1.73–8.41) | 3.38 (1.9–7.83) | 0.565 | |
| Mortality within 30 day of hospitalization | 7 (3.63) | 2 (2.7) | 1.000 | |
| Female age, 60 ≤ yr ≤ 79 | ||||
| Symptom onset to ED visit, hr | 4.31 (1.5–23.27) | 4.51 (1.9–23.7) | 0.642 | |
| EDLOS, hr | 3.09 (1.23–7.53) | 3.08 (1.34–6.08) | 0.239 | |
| Mortality within 30 day of hospitalization | 44 (6.67) | 17 (5.82) | 0.624 | |
| Female age, yr ≥ 80 | ||||
| Symptom onset to ED visit, hr | 6.03 (1.92–24.9) | 6 (2–23.91) | 0.704 | |
| EDLOS, hr | 3.53 (1.58–8.93) | 3.24 (1.31–8.55) | 0.449 | |
| Mortality within 30 day of hospitalization | 48 (11.48) | 26 (16.67) | 0.099 | |
Values are presented as median (interquartile range) or number (%).
AMI = acute myocardial infarction, ED = emergency department, EDLOS = Emergency Department Length Of Stay.
aFebruary 21 to April 1 in 2018–2019; bFebruary 21 to April 1 in 2020.
*P < 0.05, **P < 0.01.
DISCUSSION
This is the first nationwide study to analyze the impact of the COVID-19 pandemic on ED visits of patients with AMI. There have been multicenter studies that have investigated the effects of COVID-19 on healthcare utilization by patients with AMI or other circulatory diseases in other countries; however, none of the studies analyzed data from all emergency healthcare facilities in a country. In Korea, one study examined the effects of COVID-19 on outpatient department visits by patients with other diseases10; however, no study has reported its impact on the frequency of ED visits by AMI patients.
Changes in patterns of visiting the ED have been reported during previous outbreaks of SARS and MERS. Heiber and Lou3 reported that the number of ED visits decreased by about 21% during the SARS outbreak when compared with that during the same period in the two preceding years, with most marked changes observed among cases involving infants and toddlers (0–3 years); in contrast, ED visits by teenagers and adults (13–64 years) owing to respiratory diseases increased. Chen et al.4 reported that the percentage of patients in an urban ED in Taiwan decreased by 33.4% during the SARS outbreak.
Such reductions in ED visits have also been observed during the MERS outbreak in Korea. A study by Paek et al.5 revealed a decrease in the number of patients with non-urgent conditions and length of ED stay in one tertiary referral hospital, with the changes being more evident among cases involving children than adults. Lee et al.6 in their analysis of data of the National Health Information Database, reported that while the number of visits owing to non-urgent diseases markedly decreased, there were no notable changes observed in the number of visits owing to severe diseases and 7-day mortality after ED admission.
Boserup et al.8 raised concerns regarding reports showing a decrease in the total number of ED visits citing fear of contracting COVID-19 and patients' neglect of emergency symptoms. Multiple studies have reported a reduction in the number of patients with AMI visiting the ED during the COVID-19 outbreak.15,16,17 Although this was a preliminary analysis, a study reported an increased time component of ST-segment elevation myocardial infarction care (symptom onset to first medical contact, door to device, catheterization laboratory arrival to device).18
Previous studies investigating the impact of the COVID-19 on ED visits in patients with myocardial infarction have shown various results. Studies conducted in the U.S. and Italy reported a clear decrease in patients with AMI visiting the emergency room, but no change in Taiwan.17,19,20
In the present study, the total number of ED visits and ED visits by AMI patients were observed to be markedly decreased during the COVID-19 outbreak. The reason for the decrease in the number of AMI patients visiting the emergency room is estimated to be a result of two factors. First, the incidence of AMI patients remains unchanged, and the number of patients visiting the ED may decrease due to various reasons. Mafham et al.21 reported that the reduced number of AMI admissions is likely to have resulted in increases in out-of-hospital deaths and long-term complications of myocardial infarction. It is estimated that the following reasons are why patients hesitate to visit the ED. On the policy front, implementation of policies such as social distancing and quarantine to control the COVID-19 outbreak could possibly influence the comprehensive healthcare system for the treatment of AMI. From a patients' perspective, multiple factors may hinder the utilization of emergency care, these include misinterpreting the symptoms of myocardial infarction, such as chest discomfort and dyspnea, as symptoms of respiratory infection, fear of acquiring COVID-19, fear of not receiving proper treatment due to healthcare providers' fatigue or lack of resources, and efforts taken to not further burden the already overloaded emergency medical system, such as 119. Further, the restricted emergency medical system and shortage of quarantine facilities may stymie patient's ED visits.16,17 Given that women under the age of 60 have the longest time from symptom onset to ED visit and the lowest ratio of ED visits, one may think they have been most affected by the factors that hinder ED visits.
Second, although it is likely that the reduced number of AMI patients presenting to the ED is due to reduced ED visits by patients, as opposed to an actual reduction in the number of patients with AMI, the possibility that this may actually indicate a reduction in the incidence of AMI should be taken into account. There exists reported theoretical evidence supporting the rationale that COVID-19 may cause a decrease in the incidence of AMI, as a result of lifestyle changes in which people avoid physically straining exercise and reduce atmospheric contamination; although this has not been substantiated.22 After this period, we need to analyze trends of sudden cardiac arrest, cardiogenic shock, and cause of out of hospital cardiac arrest to distinguish the preceding two aspects.
Two aspects of Emergency Department Length Of Stay (EDLOS) reduction can be considered: During the epidemic, many infectious personnel and resources were required, but due to the decrease in emergency room patients and inpatients, other resources were more sufficient than usual, which would have enabled rapid treatment and hospitalization. In other respects, EDLOS may be a statistical coincidence due to an increase in the number of samples, given that there are no statistically significant groups in the subgroup analysis.
Although not statistically significant, the increase in mortality within 30 days of admission may be due to accidental findings or to infection preventive guidelines such as use of personal protective equipment before interventions begin.
AMI is associated with high mortality and morbidity and failing to receive timely treatment is highly likely to exacerbate the clinical progress, such as increase the risk of death and disabilities, highlighting the importance of a well-managed comprehensive care system. Healthcare providers and emergency medical systems must strive to maintain a comprehensive care system for AMI in strict compliance with disinfection measures to prevent any obstacles to ED visits by AMI patients during the COVID-19 pandemic.
This study had several limitations. First, this study utilized the NEDIS data, which are more like claims data, as opposed to in-depth hospital medical record review; therefore, there may be errors in the final diagnosis. Second, there is a possibility of recall bias due to the retrospective nature of the study. Third, we conducted this study under the premise that no other factors affected ED visits during the outbreak period. Thus, we cannot eliminate the possibility of factors other than COVID-19 affecting the study results during the outbreak period.
In conclusion, the COVID-19 outbreak has caused a reduction in ED visits by AMI patients, which is expected to influence the clinical course of the patients. Accordingly, the healthcare staff and emergency medicine personnel should work towards eliminating hurdles due to the COVID-19 pandemic for ensuring timely treatment of patients with AMI.
ACKNOWLEDGMENTS
The authors thank all the healthcare workers who are working on COVID-19 treatment.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Sung HK, Paik JH.
- Data curation: Kang S, Sung HK.
- Formal analysis: Kang S, Lee YJ.
- Methodology: Kang S, Sung HK.
- Supervision: Kang S, Paik JH.
- Writing - original draft: Kang S.
- Writing - review & editing: Paik JH, Lee YJ.
SUPPLEMENTARY MATERIALS
Types and number of emergency healthcare facilities participating in the National Emergency Department Information System registry
Procedure codes related to acute myocardial infarction on National Emergency Department Information System
References
- 1.World Health Organization. Coronavirus disease (COVID-19) situation reports. [Updated 2020]. [Accessed December 15, 2020]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2.Korea Centers for Disease control and Prevention. Coronavirus disease-19 main website. [Updated 2020]. [Accessed December 15, 2020]. http://ncov.mohw.go.kr/en/
- 3.Heiber M, Lou WY. Effect of the SARS outbreak on visits to a community hospital emergency department. CJEM. 2006;8(5):323–328. doi: 10.1017/s148180350001397x. [DOI] [PubMed] [Google Scholar]
- 4.Chen WK, Cheng YC, Chung YT, Lin CC. The impact of the SARS outbreak on an urban emergency department in Taiwan. Med Care. 2005;43(2):168–172. doi: 10.1097/00005650-200502000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Paek SH, Kim DK, Lee JH, Kwak YH. The impact of Middle East respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017;32(10):1576–1580. doi: 10.3346/jkms.2017.32.10.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SY, Khang YH, Lim HK. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019;60(8):796–803. doi: 10.3349/ymj.2019.60.8.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeong H, Jeong S, Oh J, Woo SH, So BH, Wee JH, et al. Impact of Middle East respiratory syndrome outbreak on the use of emergency medical resources in febrile patients. Clin Exp Emerg Med. 2017;4(2):94–101. doi: 10.15441/ceem.16.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ham CH, Moon HJ, Kim JH, Park YK, Lee TH, Kwon WK. Coronavirus disease (COVID-19) outbreak and its impact on spinal daily practice : preliminary report from a single (regional) University Hospital in Republic of Korea. J Korean Neurosurg Soc. 2020;63(4):407–414. doi: 10.3340/jkns.2020.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y, Ahn E, Lee S, Lim DH, Kim A, Lee SG, et al. Changing patterns of medical visits and factors associated with no-show in patients with rheumatoid arthritis during COVID-19 pandemic. J Korean Med Sci. 2020;35(48):e423. doi: 10.3346/jkms.2020.35.e423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ryu JH, Min MK, Lee DS, Yeom SR, Lee SH, Wang IJ, et al. Changes in relative importance of the 5-level triage system, Korean triage and acuity scale, for the disposition of emergency patients induced by forced reduction in its level number: a multi-center registry-based retrospective cohort study. J Korean Med Sci. 2019;34(14):e114. doi: 10.3346/jkms.2019.34.e114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cha WC, Ahn KO, Shin SD, Park JH, Cho JS. Emergency department crowding disparity: a nationwide cross-sectional study. J Korean Med Sci. 2016;31(8):1331–1336. doi: 10.3346/jkms.2016.31.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahn S. Final report of health insurance big data-based monitoring of cardiovascular and cerebrovascular disease. Cheongju, Korea: Korea Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 14.Kim D. A study on the comparison of operational definitions of diseases based on health insurance claims data. Goyang, Korea: National Health Insurance Institute Ilsan Hospital; 2017. [Google Scholar]
- 15.Trabattoni D, Montorsi P, Merlino L. Late STEMI and NSTEMI patients' emergency calling in COVID-19 outbreak. Can J Cardiol. 2020;36(7):1161.e7–1161.e8. doi: 10.1016/j.cjca.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, et al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 20.Li YH, Huang WC, Hwang JJ Taiwan Society of Cardiology. No reduction of ST-segment elevation myocardial infarction admission in Taiwan during coronavirus pandemic. Am J Cardiol. 2020;131:133–134. doi: 10.1016/j.amjcard.2020.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niccoli G, Luescher TF, Crea F. Decreased myocardial infarction admissions during COVID times: what can we learn? Cardiovasc Res. 2020;116(10):e126–e128. doi: 10.1093/cvr/cvaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Types and number of emergency healthcare facilities participating in the National Emergency Department Information System registry
Procedure codes related to acute myocardial infarction on National Emergency Department Information System