Abstract
Introduction
Despite acute respiratory infections (ARIs) being the single largest reason for antibiotic use in under-5 children in Bangladesh, the prevalence of antibiotic use in the community for an ARI episode and factors associated with antibiotic use in this age group are unknown.
Methods
We analysed nationally representative, population-based, household survey data from the Bangladesh Demographic and Health Survey 2014 to determine the prevalence of antibiotic use in the community for ARI in under-5 children. Using a causal graph and multivariable logistical regression, we then identified and determined the sociodemographic and antibiotic source factors significantly associated with the use of antibiotics for an episode of ARI.
Results
We analysed data for 2 144 children aged <5 years with symptoms of ARI from 17 300 households. In our sample, 829 children (39%) received antibiotics for their ARI episode (95% CI 35.4% to 42.0%). Under-5 children from rural households were 60% (adjusted OR (aOR): 1.6; 95% CI 1.2 to 2.1) more likely to receive antibiotics compared with those from urban households, largely driven by prescriptions from unqualified or traditional practitioners. Private health facilities were 50% (aOR: 0.5; 95% CI 0.3 to 0.7) less likely to be sources of antibiotics compared with public health facilities and non-governmental organisations. Age of children, sex of children or household wealth had no impact on use of antibiotics.
Conclusion
In this first nationally representative analysis of antibiotic use in under-5 children in Bangladesh, we found almost 40% of children received antibiotics for an ARI episode. The significant prevalence of antibiotic exposure in under-5 children supports the need for coordinated policy interventions and implementation of clinical practice guidelines at point of care to minimise the adverse effects attributed to antibiotic overuse.
Keywords: infections, diseases, disorders, injuries, public health, child health, respiratory infections
Key questions.
What is already known?
Emergence of antimicrobial resistance due to inappropriate use of antibiotics is a global public health threat. A recent meta-analysis across eigth low-income and middle-income countries (LMICs) showed that up to 80% of under-5 children in health facilities received antibiotic therapy for acute respiratory infections (ARIs), often unnecessarily.
Although some estimates of the number of under-5 children in Bangladesh exposed to antibiotic treatment for ARIs are available from small samples, patterns of antibiotic use at a population level, particularly in the community, remain unknown.
What are the new findings?
In this first nationally representative population-based analysis, we find that 39% of under-5 children received antibiotics for an ARI episode in the community.
Additionally, we demonstrate that children in rural households were more likely to receive antibiotics compared with those from urban households and this was largely driven by over-the-counter antibiotic purchases in rural settings from unqualified medicine vendors and inequitable access to formal healthcare practitioners.
In contrast to some previous literature, we reported that private health facilities were less likely to be the source of antibiotics for under-5 children with ARI compared with public health facilities and non-governmental organisations.
Key questions.
What do the new findings imply?
Our findings suggest an alarmingly high level of inappropriate antibiotic use for ARIs in the community which may act as a major driving force behind the growth of antimicrobial resistance in LMICs such as Bangladesh. Our data provides baseline information on antibiotic use for childhood ARI and will help evaluate effectiveness of any public health intervention designed to improve antimicrobial stewardship in Bangladesh.
Introduction
Globally, acute respiratory infections (ARIs) are the leading cause of morbidity and mortality in children aged below 5 years.1 The burden is significantly higher in low-income and middle-income countries (LMICs) where they contribute to one third of all deaths among under-5 children.1 WHO estimates that every year over 1 million under-5 children die from ARIs around the globe with over 75% of this burden concentrated in sub-Saharan Africa and South-East Asia.1 2 In Bangladesh, a country in South-East Asia and home to one of the most densely populated cities in the world, ARIs, including pneumonia, are the leading cause of under-5 deaths claiming the lives of over 50 000 children annually.3 Consistent with countries around the world, the aetiology of ARIs in this age group of children in Bangladesh is predominantly viral.4 Clinical Practice Guidelines (CPGs) consistently advise against routine antibiotic use in ARIs due to insufficient evidence of any marginal benefit.5 Despite this, 80% of children with ARIs are treated with antibiotics in LMICs.6 Such unrestricted use of antibiotics raise significant concerns for the continued rise of antimicrobial resistance (AMR). As the COVID-19 pandemic, caused by novel SARS-CoV-2, spreads across Bangladesh and other LMICs, there are reports of widespread empirical antibiotic use due to uncertainty surrounding the disease,7 which may further contribute to AMR.
The exponential growth of AMR worldwide is one of our greatest public health threats of this century and is largely propelled by excessive and inappropriate use of antibiotics. During 2000–2010, total global antibiotic consumption grew 36% with LMICs accounting for 76% of this increase.8 Systematic factors implicated in the growth of antibiotic use in LMIC include increased morbidity and mortality of illnesses, significant patient volumes, limited access to investigations and attitudes of both patients and healthcare providers.6 However, the impact of patient specific factors have been inconsistent.6 9 Under-5 children have the highest consumption of antibiotics compared with other age groups and ARIs are the single largest reason for antibiotics prescription in LMICs.10 This presents a particularly concerning combination as it inflates healthcare system costs while also exposing individual patients to unnecessary risks of life threatening adverse effects, drug toxicity and developmental consequences.11 Importantly, there is an established body of evidence demonstrating the effectiveness of simple and cost-effective interventions in changing antibiotic prescribing practices in LMICs.12
In Bangladesh, there remains a critical gap in the literature on antibiotic consumption patterns for childhood ARI, specifically at a population level. Evaluating the extent and pattern of antibiotic use for ARI has policy implications in terms of designing targeted interventions to promote appropriate antibiotic stewardship and curtail the emergence of AMR. Therefore, we used nationally representative population-based sample survey data to examine the prevalence and factors associated with antibiotic use in under-5 children with ARIs.
Methods
Data sources and procedures
We analysed data extracted from the latest available Bangladesh Demographic and Health Survey (BDHS) 2014, conducted between June and November 2014 and published in March 2016. BDHS is a nationally representative cross-sectional household survey that is typically implemented every 5 years by the National Institute of Population Research and Training of the Ministry of Health and Family Welfare.13 As with the Demographic and Health Surveys (DHS) implemented across other LMICs, the dataset is publicly available to researchers on request. The tools of data collection and study methodology are described in the survey report and the DHS website.13 Briefly, the survey uses a two-stage cluster sampling procedure where clusters are enumeration areas (EAs) composed of a number of households. In the first stage, 600 EAs were chosen with probability proportional to EA size. Then, based on a systematic sampling approach, 30 households were selected from each of the EAs and surveyed a total of 18 000 residential households, and 17 300 residential houses were successfully interviewed, representing 0.05% of total households in Bangladesh. In these households, 18 245 ever-married women aged 15–49 were approached and 17 863 consenting participants were successfully interviewed with a response rate of 98%. Mothers were asked about any recent illness episodes of their under-5 children including any illness with symptoms of cough, fever, runny nose or diarrhoea in the 2 weeks preceding the survey with response options ‘yes’, ‘no’ or ‘don’t know’. If answered ‘yes’, mothers were also asked further details of any treatment sought; including, place of treatment, type of facility and type of drugs used.
Measurement of variables
Outcome variable
The outcomes of interest were the proportion of under-5 children who received antibiotics for a recent episode of ARI (in the preceding 2 weeks).
For our analysis, we defined an episode of ARI in an under-5 child as the presence of any two symptoms as reported by their mothers including cough, fever or nasal discharge (runny nose) in the preceding 2 weeks. This definition for ARI has been previously validated in Bangladesh.14 However, some previous studies in Bangladesh included breathing difficulty as a presenting symptoms for ARI while a more recent study used our definition for upper respiratory tract infections.15 16 We chose not to include breathing difficulty as a necessary symptom as we aimed to capture a broader range of ARIs including both mild and severe manifestations. Using our definition, milder ARIs that usually do not present with difficulty breathing would not be excluded while more severe ARIs such as pneumonia would be included as fever or cough usually accompany difficulty in breathing as a presenting symptom in the paediatric population. All children who had an ARI episode within the preceding 2 weeks and were given antibiotics for that illness episode were included in our study.
Explanatory variable
All the explanatory variables were chosen based on existing literature and are defined in table 1. The explanatory variables were classified as socio-demographic factors including child’s age, sex, parental age, parent education and occupation, place of residence, division (province), household wealth; child’s nutritional status which includes stunting (height-for-age), wasting (weight-for-height) and underweight (weight-for-age); drug prescriber factors including healthcare professional/workers, unqualified/traditional practitioner; drug sources including public sector, non-governmental organisation (NGO) sector, private medical sector and others. Child nutritional status was measured by anthropometric z-scores based on the WHO child growth standards that take into account sex, age, height in centimetres and weight in kilograms.13 Household wealth was measured by a wealth index calculated using household assets data via principal component analysis as per the DHS guideline and categorised into five equal categories where each was comprising 20% of the population.13
Table 1.
Measurement of explanatory variables
| Variables | Description |
| Age of mother (in year) | Using child’s line no in household and mother’s line no—age of the mother was grouped into 15–19 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years, 40–44 years, 45–49 years. |
| Age of father (in year) | Using child’s line no in household and father’s line no- age of father was grouped into less and equal to 19 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years, 40–44 years, 45–49 years, 50–54 years, more than and equal to 55 years. |
| Age of child (in month) | Age of children was grouped into less than 6 months, 6–10 months, 12–23 months, 24–35 months, 36–47 months, 48–59 months. |
| Sex of child | Sex of children was categorised into male–female. |
| Place of residence | Place of residence was categorised into rural and urban. |
| Division (Province) | The divisional residence of the respondents were categorised into: Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur, Sylhet. |
| Wealth index | Campsite score of household possession using principal component analysis and was categorised into quintiles; poorest: q1- poorer: q2- middle: q3- richer: q4; and richest: q5. |
| Father education | Father education was categorised into no education; primary (up to grade 5)—secondary (up to grade 10)—higher (grade 11 or above). |
| Father occupation | Profession of the father of the child was categorised into five composite categories· Land owner, farmer, agriculture workers, fishermen, poultry raising, cattle raising were grouped into Agriculture· Similarly, unskilled and semiskilled worker (rickshaw driver, brick breaking, domestic servant, factory worker, carpenter, mason, transport workers), professional work (doctor, lawyer, dentist, accountant, other employed), businessmen (big businessman, small business/trader), other (unemployed/ student, retired, others) were composite categories made. |
| Mother education | Mother education was categorised into no education; primary (up to grade 5)—secondary (up to grade 10)—higher (grade 11 or above). |
| Mother occupation | Using child’s line no in household and mother’s line no- mother occupation was grouped into: currently working and not working. |
| Child malnutrition status | Stunted categorised into Severe if height/age SD was less than—300; moderate if height/age SD was between −300 and −201; well-nourished if height/age SD was above −200. Similarly, wasted-underweight categorised into severe-to-moderate and well nourished. |
| Health professional/worker | This composite variable was created form the frequency of prescribing drug by a qualified doctor or nurse/midwife/ paramedics or family welfare visitor or community skilled birth attendants or medical assistant or community healthcare provider or health assistant· This variable was coded into yes-no. |
| Unqualified/ traditional practitioner | Unqualified/ traditional practitioner was a composite variable and compilation of the variables such as drug prescribed by family welfare assistant—NGO worker—trained traditional birth attendant- untrained traditional birth attendant-unqualified doctor–drug seller—homoeopathic doctor—other· This composite variable was grouped into yes-no. |
| Public sector | Public sector as a source of antibiotics was also a composite variable and created by compiling the following variables: district hospital-Mother and Child Welfare Centre (MCWC)-Upazila Health Complxes (UHC) and Union Health and Family Welfare Centres (UHFWCs) UH and FWC-Expanded Program on Immunization (EPI) outreach-Family Welfare Assistant (FWA)· It was grouped into yes-no. |
| Private sector | A composite variable was created to express the private sector as the source of Antibiotic by considering the following variables: private hospital/clinic-qualified doctor—other private—pharmacy-unqualified doctor-shop· It was coded into yes- no. |
| NGO sector | The variables used to express the NGO sector as a source of Antibiotic were NGO static clinic-NGO satellite clinic-NGO depot holder-NGO field worker-another NGO sector· It was also coded into yes-no. |
| Other | Another source of antibiotics was dummy variables with categories yes and no. |
NGO, non-governmental organisation.
Statistical analysis
We used Stata V.15 software (StataCorp) for our analysis. We conducted descriptive statistics to describe sociodemographic characteristics of the children and caregivers. We performed univariate binary logistic regression to assess the crude relationship between receiving antibiotics for ARI among under-5 children and selected explanatory variables. To find out potential covariates for multivariate analysis, conceptual framework technique was used, which displayed the potential causal pathway and link between explanatory variables and the outcome of interest (figure 1). Causal graphs have been explained in detail by Jewell.17 Briefly, a single arrow represented the direct effect of the explanatory variables while the indirect effect was illustrated by one or more prevailing variables on the trail of the outcome. The total effect of an explanatory variable was the combined effect of its direct effect and indirect effect. For instance, for place of residence, we identified several confounders including nutritional status, other drug sources and age of the child, and adjusted for these confounders in the multivariable logistic regression model. We similarly conducted multivariable logistic regression analysis for other explanatory variables.
Figure 1.
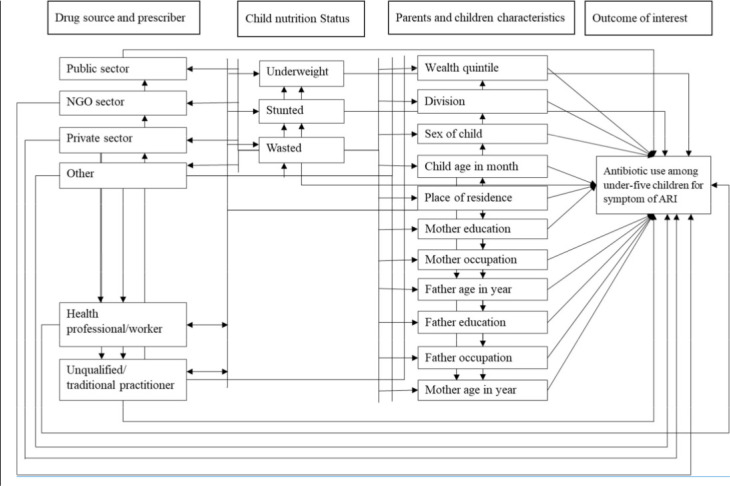
Conceptual framework used to inform multivariable logistic regression analysis to identify the influence of associated factors on antibiotic consumption among under-5 age children for symptom of ARI, Bangladesh 2014. ARI, acute respiratory infection; NGO, non-governmental organisation.
Adjusted ORs (aOR) with 95% CIs and p value for each model were estimated to identify the statistically significant association of explanatory variable with the outcome of interest. All tests were two tailed and were considered significant at alpha value of 5%. We performed all analysis by considering sampling design, sampling strata and weight.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or disseminating of this research as this was a secondary analysis of nationally representative data.
Results
BDHS surveyed 7 754 under-5 children, of which 2 144 children (28%) had an episode of ARI in the preceding 2 weeks and were included in our analysis. The median age of our study population was 26 months (IQR 12–42) and more than half of them were female. The sociodemographic characteristic of our study cohort is presented in table 2.
Table 2.
Demographic and sociodemographic characteristics—child malnutrition status—antibiotic prescribers-sources of drug of the children who had symptoms of ARI at any time in the 2 weeks preceding the survey and prevalence of their antibiotic use, BDHS 2014 (N=2144)
| Characteristics | Children under 5 years of age who had symptoms of ARI | Children of age under 5 years who took antibiotic for symptoms of ARI | |||||
| No of children who had symptoms of ARI | Percentage of children who had symptoms of ARI | No of children who received antibiotics | Percentage of children who received antibiotics | Prevalence of receiving antibiotic | 95% CI | P value | |
| Overall | 2146 | 100 | 829 | 100 | 38.7 | (35.4 to 42.0) | |
| Age of mother (year) | |||||||
| Median (IQR: 25th, 75th) | 24 (21–29) | 25 (21–30) | |||||
| 15–19 | 336 | 15.7 | 125 | 15.1 | 37.1 | (31.4 to 43.2) | 0.756 |
| 20–24 | 762 | 35.5 | 283 | 34.2 | 37.2 | (32.7 to 41.9) | |
| 25–29 | 541 | 25.2 | 207 | 25.0 | 38.3 | (32.7 to 44.3) | |
| 30–34 | 351 | 16.4 | 146 | 17.6 | 41.5 | (32.6 to 51.0) | |
| 35–39 | 118 | 5.5 | 51 | 6.2 | 43.6 | (31.4 to 56.6) | |
| 40–44 | 24 | 1.1 | 12 | 1.5 | 52.4 | (31.9 to 72.1) | |
| 45–49 | 14 | 0.7 | 4 | 0.5 | 31.6 | (10.3 to 64.8) | |
| Age of father (year) | |||||||
| Median (IQR: 25th, 75th) | 32 (28–38) | 32 (28–39) | |||||
| ≤24 | 124 | 5.8 | 46 | 5.5 | 37.0 | (28.1 to 46.9) | 0.181 |
| 25–29 | 519 | 24.2 | 180 | 21.7 | 34.7 | (29.6 to 40.3) | |
| 30–34 | 490 | 22.8 | 177 | 21.3 | 36.0 | (31.0 to 41.4) | |
| 35–39 | 502 | 23.4 | 212 | 25.5 | 42.2 | (35.2 to 49.5) | |
| 40–44 | 268 | 12.5 | 100 | 12.1 | 37.4 | (30.9 to 44.3) | |
| 45–49 | 136 | 6.3 | 65 | 7.8 | 47.6 | (34.0 to 61.7) | |
| 50–54 | 52 | 2.4 | 21 | 2.6 | 40.9 | (26.7 to 56.7) | |
| ≥55 | 55 | 2.6 | 29 | 3.5 | 52.5 | (39.3 to 65.3) | |
|
Age of child (months) | |||||||
| Median (IQR: 25th, 75th) | 27(13–42) | 29 (14–43) | |||||
| <6 | 178 | 8.3 | 64 | 7.7 | 36.0 | (26.2 to 47.2) | 0.254 |
| 6–11 | 308 | 14.3 | 95 | 11.5 | 31.0 | (24.3 to 38.5) | |
| 12–23 | 482 | 22.5 | 180 | 21.7 | 37.3 | (32.2 to 42.6) | |
| 24–35 | 414 | 19.3 | 161 | 19.4 | 38.9 | (33.0 to 45.1) | |
| 36–47 | 405 | 18.9 | 173 | 20.8 | 42.6 | (36.5 to 48.9) | |
| 48–59 | 357 | 16.7 | 157 | 18.9 | 43.9 | (33.0 to 55.4) | |
| Sex of child | |||||||
| Male | 1133 | 52.8 | 425 | 51.3 | 37.5 | (33.4 to 41.8) | 0.425 |
| Female | 1012 | 47.2 | 404 | 48.7 | 39.9 | (35.4 to 44.6) | |
| Place of residence | |||||||
| Urban | 520 | 24.2 | 163 | 19.6 | 31.3 | (26.3 to 36.8) | 0.006 |
| Rural | 1625 | 75.8 | 666 | 80.4 | 41.0 | (37.2 to 44.9) | |
| Wealth index | |||||||
| Poorest | 502 | 23.4 | 203 | 24.5 | 40.5 | (34.8 to 46.5) | 0.459 |
| Poorer | 390 | 18.2 | 163 | 19.6 | 41.6 | (35.0 to 48.6) | |
| Middle | 466 | 21.7 | 186 | 22.5 | 40.0 | (33.1 to 47.2) | |
| Richer | 412 | 19.2 | 147 | 17.8 | 35.8 | (29.9 to 42.1) | |
| Richest | 375 | 17.5 | 129 | 15.6 | 34.5 | (28.3 to 41.2) | |
| Divisions | |||||||
| Barisal | 138 | 6.4 | 57 | 6.8 | 41.0 | (33.0 to 49.5) | 0.070 |
| Chittagong | 506 | 23.6 | 171 | 20.6 | 33.8 | (28.3 to 39.8) | |
| Dhaka | 657 | 30.6 | 247 | 29.8 | 37.6 | (31.5 to 44.1) | |
| Khulna | 138 | 6.4 | 47 | 5.6 | 33.8 | (26.5 to 42.0) | |
| Rajshahi | 216 | 10.1 | 83 | 10.1 | 38.5 | (32.0 to 45.5) | |
| Rangpur | 232 | 10.8 | 94 | 11.4 | 40.7 | (34.0 to 47.8) | |
| Sylhet | 258 | 12 | 130 | 15.7 | 50.4 | (38.6 to 62.1) | |
| Father education | |||||||
| No education | 572 | 26.7 | 221 | 26.6 | 38.6 | (31.2 to 46.5) | 0.547 |
| Primary | 653 | 30.5 | 274 | 33.1 | 42.0 | (34.9 to 49.5) | |
| Secondary | 637 | 29.7 | 235 | 28.3 | 36.8 | (32.5 to 41.5) | |
| Higher | 281 | 13.1 | 99 | 12.0 | 35.3 | (28.8 to 42.5) | |
| Father occupation | |||||||
| Agriculture | 557 | 26 | 224 | 27.0 | 40.2 | (34.7 to 45.9) | 0.868 |
| Unskilled and semiskilled worker | 982 | 45.8 | 377 | 45.4 | 38.4 | (33.8 to 43.2) | |
| Professional work | 112 | 5.2 | 42 | 5.0 | 37.4 | (28.2 to 47.5) | |
| Businessmen | 443 | 20.7 | 171 | 20.6 | 38.7 | (32.6 to 45.1) | |
| Others | 50 | 2.3 | 16 | 1.9 | 31.8 | (21.0 to 45.0) | |
| Mother education | |||||||
| No education | 367 | 17.1 | 144 | 17.3 | 39.2 | (30.9 to 48.1) | 0.853 |
| Primary | 650 | 30.3 | 262 | 31.6 | 40.3 | (34.4 to 46.4) | |
| Secondary | 939 | 43.8 | 355 | 42.8 | 37.8 | (33.6 to 42.1) | |
| Higher | 190 | 8.9 | 69 | 8.3 | 36.2 | (28.2 to 45.1) | |
| Mother occupation | |||||||
| Not working | 1588 | 74.0 | 615 | 74.2 | 38.7 | (34.8 to 42.8) | 0.902 |
| Working | 557 | 26.0 | 214 | 25.8 | 38.4 | (33.8 to 43.2) | |
| Child malnutrition status | |||||||
| Stunted | |||||||
| Severe | 263 | 87 | 98 | 12.4 | 37.1 | (28.6 to 46.6) | 0.746 |
| Moderate | 538 | 254 | 219 | 27.9 | 40.7 | (34.6 to 47.0) | |
| Well Nourished | 1217 | 1677 | 469 | 59.7 | 38.5 | (34.6 to 42.7) | |
| Wasted | |||||||
| Severe | 204 | 10.1 | 20 | 2.5 | 22.7 | (13.1 to 36.3) | 0.048 |
| Moderate | 528 | 26.1 | 105 | 13.4 | 41.2 | (33.9 to 49.0) | |
| Well Nourished | 1286 | 63.7 | 661 | 84.1 | 39.4 | (35.9 to 43.1) | |
| Underweight | |||||||
| Severe | 204 | 10.1 | 74 | 9.4 | 36.2 | (25.0 to 49.1) | 0.813 |
| Moderate | 528 | 26.1 | 210 | 26.7 | 39.8 | (35.0 to 44.9) | |
| Well Nourished | 1286 | 63.7 | 502 | 63.8 | 39.0 | (35.0 to 43.1) | |
| Drug prescribed | |||||||
| Healthcare professional/worker | |||||||
| Yes | 733 | 34.1 | 275 | 33.1 | 37.5 | (31.1 to 44.3) | 0.649 |
| No | 1413 | 65.9 | 555 | 66.9 | 39.3 | (35.7 to 42.9) | |
| Unqualified/traditional practitioner | |||||||
| Yes | 970 | 50.8 | 457 | 55.2 | 47.1 | (42.9 to 51.4) | 0.022 |
| No | 938 | 49.2 | 371 | 44.8 | 39.5 | (34.0 to 45.2) | |
| Drug sources | |||||||
| Public sector | |||||||
| Yes | 234 | 10.9 | 103 | 12.4 | 43.9 | (36.3 to 51.8) | 0.176 |
| No | 1912 | 89.1 | 727 | 87.6 | 38.0 | (34.5 to 41.7) | |
| NGO sector | |||||||
| Yes | 18 | 0.9 | 11 | 1.3 | 59.6 | (30.2 to 83.4) | 0.147 |
| No | 2126 | 99.1 | 818 | 98.7 | 38.5 | (35.4 to 41.7) | |
| Private sector | |||||||
| Yes | 1511 | 70.7 | 615 | 74.3 | 40.7 | (36.5 to 45.1) | 0.056 |
| No | 628 | 29.3 | 213 | 25.7 | 33.9 | (29.1 to 39.1) | |
| Others | |||||||
| Yes | 90 | 4.2 | 68 | 8.2 | 76.0 | (62.9 to 85.6) | <0.001 |
| No | 2055 | 95.8 | 761 | 91.8 | 37.0 | (33.6 to 40.6) | |
Bolded Values indicate statistical significance where the p-value is <0.05.
ARIs, acute respiratory infections; BDHS, Bangladesh Demographic and Health Survey; NGO, non-governmental organisation.
Prevalence of antibiotic consumption for ARI
The prevalence of antibiotic consumption for ARI among the under-5 children was 39% (829/2144) (table 2). We found an association in our univariable analysis between the prevalence of using antibiotics for children with ARI and their place of residence. The prevalence of antibiotic use in rural areas was 41% which was significantly higher than 31% antibiotic use for children with ARI living in urban regions. We also found significant differences in the proportion of antibiotic use among wasted children, children for whom unqualified or traditional practitioner prescribed antibiotic and children who received antibiotics from sources other than public, private or NGO sectors. The prevalence of antibiotics prescribed by a qualified health professional was 38%, which was significantly lower than antibiotic prescription rates for ARI of unqualified or traditional practitioner (47%). Considering sources of antibiotic prescription, the proportion of children with ARI symptoms received antibiotics were highest from other sources (76%) and lowest from the public sector (40%).
Factor associated with antibiotic consumption
In our multivariable analysis (online supplemental data 1), we found children living in rural areas were 1.6 times (95% CI 1.2 to 2.1) as likely to receive antibiotics for an episode for ARI than those living in an urban area. We similarly found a statistically significant difference in antibiotic consumption in participants who used private sector drug sources (aOR=0.5; 95% CI 0.3 to 0.7) and other drug sources (aOR=5.3; 95% CI 2.7 to 10·4). The factors associated with antibiotic consumption are presented in table 3.
Table 3.
Bivariable and multivariable analysis to explore factors associated with antibiotic consumption for ARI episode among children of aged less than 5 years, Bangladesh 2014
| Received antibiotic for ARI episode | ||||
| uOR (95% CI) | p-value | aOR (95% CI) | p-value | |
| Mother age (year)* | ||||
| 15–19 (ref) | 1 | |||
| 20–24 | 1.0 (0.7 to 1.4) | 0.988 | 0.9 (0.7 to 1.3) | 0.732 |
| 25–29 | 1.1 (0.7 to 1.5) | 0.777 | 0.9 (0.6 to 1.4) | 0.789 |
| 30–34 | 1.2 (0.8 to 1.9) | 0.432 | 1.1 (0.6 to 1.7) | 0.829 |
| 35–39 | 1.3 (0.7 to 2.3) | 0.364 | 1.0 (0.5 to 1.9) | 0.959 |
| 40–44 | 1.9 (0.8 to 4.6) | 0.177 | 2.0 (0.7 to 5.8) | 0.218 |
| 45–49 | 0.8 (0.2 to 3.1) | 0.727 | 1.0 (0.3 to 3.9) | 0.960 |
| Age of father (year)† | ||||
| ≤24 | 1 | |||
| 25–29 | 0.9 (0.6 to 1.5) | 0.682 | 0.7 (0.4 to 1.2) | 0.203 |
| 30–34 | 1 (0.6 to 1.5) | 0.855 | 0.8 (0.5 to 1.3) | 0.353 |
| 35–39 | 1.2 (0.8 to 2) | 0.381 | 1 (0.6 to 1.7) | 0.928 |
| 40–44 | 1 (0.6 to 1.7) | 0.952 | 0.7 (0.4 to 1.4) | 0.352 |
| 45–49 | 1.6 (0.8 to 3.1) | 0.221 | 1.2 (0.6 to 2.4) | 0.675 |
| 50–54 | 1.2 (0.5 to 2.7) | 0.701 | 0.8 (0.3 to 2) | 0.617 |
| ≥55 | 1.9 (0.9 to 3.7) | 0.07 | 1.6 (0.7 to 3.7) | 0.251 |
| Age of child (month)‡ | ||||
| <6(ref) | 1 | |||
| 6–11 | 0.8 (0.5 to 1.4) | 0.428 | 0.8 (0.5 to 1.4) | 0.531 |
| 12–23 | 1.1 (0.6 to 1.8) | 0.841 | 1.1 (0.7 to 1.9) | 0.661 |
| 24–35 | 1.1 (0.7 to 2.0) | 0.662 | 1.3 (0.7 to 2.3) | 0.352 |
| 36–47 | 1.3 (0.8 to 2.2) | 0.276 | 1.4 (0.8 to 2.4) | 0.189 |
| 48–59 | 1.4 (0.6 to 3.1) | 0.414 | 1.6 (0.8 to 3.2) | 0.161 |
| Sex§ | ||||
| Female(ref) | 1 | |||
| Male | 0.9 (0.7 to 1.2) | 0.425 | 1.0 (0.7 to 1.3) | 0.756 |
| Type of place of residence¶ | ||||
| Urban (ref) | 1 | |||
| Rural | 1.5 (1.1 to 2.0) | 0.005 | 1.6 (1.2 to 2.1) | 0.004 |
| Divisions** | ||||
| Barisal (ref) | 1 | |||
| Chittagong | 0.7 (0.5 to 1.1) | 0.161 | 0.6 (0.4 to 1.0) | 0.055 |
| Dhaka | 0.9 (0.6 to 1.3) | 0.528 | 0.9 (0.5 to 1.5) | 0.621 |
| Khulna | 0.7 (0.5 to 1.2) | 0.220 | 0.7 (0.4 to 1.2) | 0.161 |
| Rajshahi | 0.9 (0.6 to 1.4) | 0.657 | 0.8 (0.5 to 1.2) | 0.250 |
| Rangpur | 1.0 (0.6 to 1.5) | 0.961 | 0.7 (0.4 to 1.2) | 0.188 |
| Sylhet | 1.5 (0.8 to 2.6) | 0.205 | 1.3 (0.7 to 2.2) | 0.438 |
| Wealth quintile†† | ||||
| Poorest (ref) | 1 | |||
| Poorer | 1.0 (0.7 to 1.5) | 0.793 | 1.1 (0.8 to 1.6) | 0.556 |
| Middle | 1.0 (0.7 to 1.4) | 0.900 | 1.0 (0.6 to 1.7) | 0.869 |
| Richer | 0.8 (0.6 to 1.2) | 0.269 | 0.9 (0.6 to 1.3) | 0.629 |
| Richest | 0.8 (0.5 to 1.1) | 0.187 | 0.8 (0.5 to 1.3) | 0.341 |
| Father education‡‡ | ||||
| No education(ref) | 1 | |||
| Primary | 1.2 (0.7 to 1.9) | 0.558 | 1.1 (0.7 to 1.8) | 0.597 |
| Secondary | 0.9 (0.6 to 1.4) | 0.705 | 0.9 (0.6 to 1.4) | 0.793 |
| Higher | 0.9 (0.6 to 1.4) | 0.536 | 0.9 (0.5 to 1.5) | 0.675 |
| Father occupation§§ | ||||
| Agriculture (ref) | 1 | |||
| Unskilled and semiskilled worker | 0.9 (0.7 to 1.2) | 0.603 | 1.0 (0.7 to 1.4) | 0.978 |
| Professional work | 0.9 (0.5 to 1.4) | 0.625 | 0.9 (0.5 to 1.7) | 0.855 |
| Businessmen | 0.9 (0.6 to 1.4) | 0.733 | 1.0 (0.7 to 1.6) | 0.835 |
| Other | 0.7 (0.4 to 1.3) | 0.230 | 1.0 (0.5 to 2.0) | 0.987 |
| Mother education¶¶ | ||||
| No education (ref) | 1 | |||
| Primary | 1.0 (0.7 to 1.5) | 0.807 | 1.0 (0.6 to 1.6) | 0.988 |
| Secondary | 0.9 (0.6 to 1.4) | 0.791 | 0.9 (0.6 to 1.5) | 0.816 |
| Higher | 0.9 (0.5 to 1.5) | 0.628 | 0.9 (0.5 to 1.7) | 0.767 |
| Mother occupation*** | ||||
| Not working (ref) | 1 | |||
| Working | 1.0 (0.8 to 1.3) | 0.902 | 0.9 (0.7 to 1.2) | 0.608 |
| Child nutrition status | ||||
| Stunted††† | ||||
| Well nourished (ref) | 1 | |||
| Moderate | 1.1 (0.8 to 1.5) | 0.576 | 1.1 (0.8 to 1.5) | 0.428 |
| Severe | 0.9 (0.6 to 1.4) | 0.753 | 1.0 (0.6 to 1.5) | 0.898 |
| Wasted‡‡‡ | ||||
| Well nourished (ref) | 1 | |||
| Moderate | 1.1 (0.8 to 1.5) | 0.654 | 1.0 (0.7 to 1.5) | 0.838 |
| Severe | 0.5 (0.2 to 0.9) | 0.024 | 0.5 (0.2 to 1.0) | 0.037 |
| Underweight§§§ | ||||
| Well nourished (ref) | 1 | |||
| Moderate | 1.0 (0.8 to 1.3) | 0.785 | 1.1 (0.8 to 1.4) | 0.596 |
| Severe | 0.9 (0.5 to 1.5) | 0.672 | 1.0 (0.5 to 2.0) | 0.886 |
| Drug prescriber | ||||
| Healthcare professional /worker¶¶¶ | ||||
| No (ref) | 1 | |||
| Yes | 0.9 (0.7 to 1.3) | 0.649 | 0.9 (0.6 to 1.4) | 0.756 |
| Unqualified/traditional practitioner**** | ||||
| No (ref) | 1 | |||
| Yes | 1.4 (1.0 to 1.8) | 0.022 | 1.3 (1.0 to 1.8) | 0.083 |
| Drug sources | ||||
| Public sector†††† | ||||
| No (ref) | 1 | |||
| Yes | 1.3 (0.9 to 1.8) | 0.176 | 1.2 (0.8 to 1.9) | 0.344 |
| NGO sector‡‡‡‡ | ||||
| No (ref) | 1 | |||
| Yes | 2.4 (0.7 to 7.8) | 0.159 | 2.1 (0.7 to 6.1) | 0.188 |
| Private sector§§§§ | ||||
| No (ref) | 1 | |||
| Yes | 1.3 (1.0 to 1.8) | 0.056 | 0.5 (0.3 to 0.7) | <0.001 |
| Others¶¶¶¶ | ||||
| No (ref) | 1 | |||
| Yes | 5.4 (2.8 to 10.4) | <0.001 | 5.3 (2.7 to 10.4) | <0.001 |
Bolded Values indicate statistical significance where the p-value is <0.05.
*Adjusted for wasted, unqualified practitioner, other sector, age of child, place of residence.
†Adjusted for wasted, unqualified practitioner, other sector, age of child, place of residence.
‡Adjusted for wasted, healthcare professional, unqualified practitioner, other sector.
§Adjusted for wasted, unqualified practitioner, other sector, age of child, place of residence.
¶Adjusted for wasted, other sector, age of child.
**Adjusted for wasted, unqualified practitioner, private medical sector, other sector, place of residence.
††Adjusted for wasted, unqualified practitioner, private medical sector, other sector, place of residence.
‡‡Adjusted for wasted, age of child, unqualified practitioner, other sector, place of residence.
§§Adjusted for wasted, age of child, unqualified practitioner, other sector, place of residence.
¶¶Adjusted for wasted, age of child, unqualifiedpractitioner, other sector, place of residence.
***Adjusted for wasted, age of child, unqualified practitioner, other sector, place of residence.
†††Adjusted for wasted, unqualified practitioner, other sector, place of residence.
‡‡‡Adjusted for unqualified practitioner, other sector, place of residence.
§§§Adjusted for wasted unqualified practitioner, other sector, place of residence.
¶¶¶Adjusted for public sector, other sector, place of residence.
****Adjusted for public sector, other sector, place of residence.
††††Adjusted for wasted, unqualified practitioner, place of residence.
‡‡‡‡Adjusted for wasted, unqualified practitioner, place of residence.
§§§§Adjusted for wasted, unqualified practitioner, place of residence.
¶¶¶¶Adjusted for wasted, place of residence.
aOR, adjusted OR; ARI, acute respiratory infection; NGO, non-governmental organisation; uOR, unadjusted OR.
bmjgh-2020-004010supp001.pdf (76KB, pdf)
Discussion
Our results, based on a nationally representative large sample survey data, suggest that almost 40% of children aged <5 years with ARI symptoms in Bangladesh are given antibiotics for an episode of ARI. If we extrapolate our results to Bangladesh’s population of under-5 children of 16·5 million, then 4·5 million children had symptoms of ARI, of which an estimated 1·7 million children were treated with antibiotics. This unacceptably high level of antibiotic usage for childhood ARI is not supported by any CPGs including Integrated Management of Childhood Illness guidelines.5 Additionally, this imposes financial burden on families and health systems while potentially contributing to the growth of AMR in Bangladesh.
Our findings are consistent with data from other LMICs18 19 which have also estimated community prevalence of antibiotic use for childhood ARI to be around 30%–40%. However, the prevalence of antibiotic use in our study was lower than what was documented in a recent cross-sectional study conducted in eight LMICs (Haiti, Kenya, Malawi, Namibia, Nepal, Senegal, Tanzania and Uganda).6 This study reported that 80% of children aged <5 years with respiratory illness were prescribed antibiotics. Unlike this study’s case definition, we did not include breathing difficulty as part of our ARI definition to capture of a broader spectrum of ARI cases, including milder ARIs without shortness of breath, which may explain our lower rate of antibiotic use. Importantly, unlike our community-based survey, this pooled analysis included children who attended healthcare facilities for illness episode which typically represent children with more severe symptoms of ARI, and therefore tend to have higher rates of antibiotic use. Indeed, a previous hospital-based study done in Bangladesh also estimated that >70% under-5 children attending hospital with ARI received antibiotics.20
Our analysis found under-5 children living in rural Bangladesh had a 60% higher exposure to antibiotics compared with urban areas for an episode of ARI which was particularly alarming as 70% of the nation’s population inhabit rural regions. This was consistent with prior literature in both high income countries21 and LMICs including neighbouring India22 where rural healthcare facilities were more likely to dispense antibiotics. In Bangladesh, this may be due to the shortage and inequitable distribution of trained health practitioners in rural areas which encourages overdependence on unqualified healthcare providers, including unlicensed village practitioners, medicine vendors in drug store, homoeopathic doctors and traditional healers (kabiraj). A study of around 20 000 healthcare providers in Bangladesh found that besides analgesics, antibiotics were most frequently prescribed by medicine vendors, who are more frequently the primary point of contact in rural areas.23 This is a significant source of non-judicial and unprescribed use of antibiotics in LMICs with one study in Nigeria finding 76% of children with ARI received unprescribed antibiotics directly from drug stores.24 Higher antibiotic use in rural Bangladesh may also be explained by patient factors including suboptimal knowledge, and attitudes of antibiotics and their indication in rural compared with urban areas. From a policy perspective, curtailing inappropriate antibiotic usage in rural areas presents a difficult challenge. However, investments in outreach education programmes, model pharmacy initiatives and stricter enforcement of regulations, including slowing down over the counter antibiotic purchases, coupled with patient education to reduce demand side pressures may be effective over the long term.
Our analysis found that private health facilities, which have grown to be one of Bangladesh’s largest services sector, were 50% less likely to supply antibiotics to under-5 children with ARI compared with the public facilities and NGOs. The prior body of evidence from LMICs has been inconclusive with some studies finding no difference between private or public sector antibiotic prescription rates while others finding a significant difference either way.25 26 In interpreting our results, we highlight that the private healthcare sector is highly heterogeneous in LMICs such as Bangladesh as they include both formally registered medical practitioners in private hospitals and clinics, and the informal sector of drug store employees and unqualified practitioners. In our analysis, the lower use of the private sector as a source of antibiotics for children with ARI only reached significance after adjusting for unqualified practitioners and place of residence (rural or urban). This may be due to the informal sources, which include drug store employees selling over-the-counter antibiotics, being the main contributor to inappropriate antibiotic supply from private health services compared with the formal private sector hospitals and clinics in urban Bangladesh. Moreover, when compared with public facilities, private facilities have higher out of pocket expenses, attract wealthier families, spend more time on consultations and investigations,27 and therefore, might be able to withhold prescribing unnecessary empirical antibiotics for ARIs as clinicians may have more confidence in their viral diagnosis and patients following up if symptoms worsen.
Finally, we found that nutritional status had no impact on antibiotic consumption patterns. Stunted, wasted or underweight children aged <5 years did not have any significant difference in the use of antibiotics for an episode of ARI. Our finding is theoretically inconsistent with studies showing that malnutrition was associated with increased incidence of ARI, particularly more severe lower respiratory tract infections such as pneumonia where more antibiotic may be indicated.28 Moreover, previous studies demonstrated that even mildly underweight children are at greater risk of mortality from illness and therefore both parents and clinicians might be more inclined to treat their illness with antibiotics.29 However, these findings may be influenced by other sociodemographic and environmental confounders such as parental education level, overcrowded living conditions or having a kitchen attached to the living room.28 While antibiotics are lifesaving when indicated, excessive inappropriate exposure in early childhood can not only result in short-term adverse events such as anaphylactic reactions and drug toxicity but also lead to detrimental development of their gut microbiota and obesity.11
Limitations
This manuscript has several important limitations. First, although BDHS data had a recall period of 2 weeks with a relatively low risk of error, it is still subject to some recall bias as a 2-week recall period was found to underestimate prevalence of illness compared with a 1-week period.30 Second, the data are from 2014. However, this was the most updated nationally representative population-based survey data available. Additionally, there has been no intervention at a national level in Bangladesh to improve antimicrobial stewardship and thus antibiotic prescribing practices remain largely unchanged, although it may have increased due to the COVID-19 pandemic. Third, we adopted a broader definition of ARI rather than cough and fast breathing or fever which correlate more with pneumonia (severe ARI) and exclude several milder ARIs. While this may make it more difficult to compare with previous studies that have inconsistent definitions, we believe our definition provides a more accurate measure of inappropriate antibiotic use in milder ARI. Fourth, the ARI cases were self-reported and not confirmed by a clinician, however, such syndromic approach of identifying ARI cases from community-based survey has been previously validated.31 We also did not have access to data detailing individual factors including patient attitudes and knowledge which limited our ability to explain our findings in greater and more accurate detail. There is a need for further study to explore this area. Finally, BDHS sample data lacked information on aetiology of ARI episodes which restricted us from determining the proportion of antibiotics that were appropriately prescribed according to CPG. However, even within hospital settings in Bangladesh, aetiology of ARI is not routinely confirmed and it is well established that >90% childhood ARI are of viral aetiology.4
Conclusion
Our study found antibiotics were used for around 40% of children aged <5 years with ARI in Bangladesh. While antibiotic consumption was similar across most social and economic factors, we found children in rural Bangladesh used antibiotics 60% more than those in urban regions, partly driven by antibiotics dispensed by unqualified/traditional practitioners. Targeted interventions including educational programmes for formal and non-formal medical sectors, availability of CPGs at point-of-care services, stricter policies prohibiting over the counter availability of antibiotics, enforcement of antibiotic prescription requirements and parental education will help improve antimicrobial stewardship and reduce the burden of inappropriate use of antibiotics in Bangladesh.
Acknowledgments
MZH, MAAJB, MAHK and FC are icddr, b employees. icddr, b is grateful to the Governments of Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support. NH is funded through Early Career Research Fellowship of the National Health and Medical Research Council of Australian Government.
Footnotes
Handling editor: Senjuti Saha
Contributors: MZH conceptualized the study. MZH, MRM and MAAJB equally contributed to this manuscript and are joint first authors as they contributed to study design, writing the first draft and performing the statistical analysis. FC and MAHK edited the manuscript and checked the data. JB and AJ critically apraised and edited the manuscript. NH devised the study, critically apraised and edited the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. The Demographic and Health Surveys are publicly available to researchers on request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
We did not require any ethical clearance as this study was based on secondary analysis of publicly available data.
References
- 1.Williams BG, Gouws E, Boschi-Pinto C, et al. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis 2002;2:25–32. 10.1016/s1473-3099(01)00170-0 [DOI] [PubMed] [Google Scholar]
- 2.WHO . Ending preventable child deaths from pneumonia and diarrhoea by 2025. World Health organization, Published 2013. Available: https://apps.who.int/iris/bitstream/handle/10665/79200/9789241505239_eng.pdf;jsessionid=10F591E87AD598738D7D4C6A44C14AEF?sequence=1
- 3.icddr b . Pneumonia and other respiratory diseases, 2020. Available: https://www.icddrb.org/news-and-events/press-corner/media-resources/pneumonia-and-other-respiratory-diseases
- 4.Bhuyan GS, Hossain MA, Sarker SK, et al. Bacterial and viral pathogen spectra of acute respiratory infections in under-5 children in hospital settings in Dhaka City. PLoS One 2017;12:e0174488. 10.1371/journal.pone.0174488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . Handbook: IMCI integrated management of childhood illness. World Health organization, 2005. Available: https://apps.who.int/iris/handle/10665/42939
- 6.Fink G, D'Acremont V, Leslie HH, et al. Antibiotic exposure among children younger than 5 years in low-income and middle-income countries: a cross-sectional study of nationally representative facility-based and household-based surveys. Lancet Infect Dis 2020;20:179–87. 10.1016/S1473-3099(19)30572-9 [DOI] [PubMed] [Google Scholar]
- 7.Getahun H, Smith I, Trivedi K, et al. Tackling antimicrobial resistance in the COVID-19 pandemic. Bull World Health Organ 2020;98:442–442A. 10.2471/BLT.20.268573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis 2014;14:742–50. 10.1016/S1473-3099(14)70780-7 [DOI] [PubMed] [Google Scholar]
- 9.Zhang Z, Hu Y, Zou G, et al. Antibiotic prescribing for upper respiratory infections among children in rural China: a cross-sectional study of outpatient prescriptions. Glob Health Action 2017;10:1287334. 10.1080/16549716.2017.1287334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaz LE, Kleinman KP, Raebel MA, et al. Recent trends in outpatient antibiotic use in children. Pediatrics 2014;133:375–85. 10.1542/peds.2013-2903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shao X, Ding X, Wang B, et al. Antibiotic exposure in early life increases risk of childhood obesity: a systematic review and meta-analysis. Front Endocrinol 2017;8:170. 10.3389/fendo.2017.00170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davey P, Marwick CA, Scott CL, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 2017;2:CD003543. 10.1002/14651858.CD003543.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Research NIoP . Training - NIPORT/Bangladesh, Mitra, Associates, ICF International. Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh: NIPORT, Mitra and Associates, and ICF International, 2016. [Google Scholar]
- 14.Zaman K, Baqui AH, Yunus M, et al. Acute respiratory infections in children: a community-based longitudinal study in rural Bangladesh. J Trop Pediatr 1997;43:133–7. 10.1093/tropej/43.3.133 [DOI] [PubMed] [Google Scholar]
- 15.Homaira N, Luby SP, Hossain K, et al. Respiratory Viruses Associated Hospitalization among Children Aged <5 Years in Bangladesh: 2010-2014. PLoS One 2016;11:e0147982. 10.1371/journal.pone.0147982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brooks WA, Goswami D, Rahman M, et al. Influenza is a major contributor to childhood pneumonia in a tropical developing country. Pediatr Infect Dis J 2010;29:216–21. 10.1097/INF.0b013e3181bc23fd [DOI] [PubMed] [Google Scholar]
- 17.Jewell NP. Statistics for epidemiology. CRC Press, 2003. [Google Scholar]
- 18.Alkaff RN, Kamigaki T, Saito M, et al. Use of antibiotics for common illnesses among children aged under 5 years in a rural community in Indonesia: a cross-sectional study. Trop Med Health 2019;47:45. 10.1186/s41182-019-0173-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekram M, Abdel Khalek DMA-S. Acute respiratory tract infections in children under 5 years of age in upper Egypt. International Journal of Community Medicine and Public Health 2016;3:7. [Google Scholar]
- 20.Rashid MM, Chisti MJ, Akter D, et al. Antibiotic use for pneumonia among children under-five at a pediatric hospital in Dhaka City, Bangladesh. Patient Prefer Adherence 2017;11:1335–42. 10.2147/PPA.S140002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Jong J, Bos JHJ, de Vries TW, et al. Use of antibiotics in rural and urban regions in the Netherlands: an observational drug utilization study. BMC Public Health 2014;14:677. 10.1186/1471-2458-14-677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alvarez-Uria G, Zachariah S, Thomas D. High prescription of antimicrobials in a rural district hospital in India. Pharmacy Practice 2014;12:384. 10.4321/S1886-36552014000200003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed SM, Hossain MA, Chowdhury MR. Informal sector providers in Bangladesh: how equipped are they to provide rational health care? Health Policy Plan 2009;24:467–78. 10.1093/heapol/czp037 [DOI] [PubMed] [Google Scholar]
- 24.Ekwochi U, Chinawa JM, Osuorah CDI, et al. The use of unprescribed antibiotics in management of upper respiratory tract infection in children in Enugu, South East Nigeria. J Trop Pediatr 2014;60:249–52. 10.1093/tropej/fmt111 [DOI] [PubMed] [Google Scholar]
- 25.Siddiqi S, Hamid S, Rafique G, et al. Prescription practices of public and private health care providers in Attock district of Pakistan. Int J Health Plann Manage 2002;17:23–40. 10.1002/hpm.650 [DOI] [PubMed] [Google Scholar]
- 26.Haque M, Rahman NIA, Zulkifli Z, et al. Antibiotic prescribing and resistance: knowledge level of medical students of clinical years of university Sultan Zainal Abidin, Malaysia. Ther Clin Risk Manag 2016;12:413–26. 10.2147/TCRM.S102013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pongsupap Y, Van Lerberghe W. Choosing between public and private or between hospital and primary care: responsiveness, patient-centredness and prescribing patterns in outpatient consultations in Bangkok. Trop Med Int Health 2006;11:81–9. 10.1111/j.1365-3156.2005.01532.x [DOI] [PubMed] [Google Scholar]
- 28.Islam F, Sarma R, Debroy A, et al. Profiling acute respiratory tract infections in children from Assam, India. J Glob Infect Dis 2013;5:8–14. 10.4103/0974-777X.107167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caulfield LE, de Onis M, Blössner M, et al. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr 2004;80:193–8. 10.1093/ajcn/80.1.193 [DOI] [PubMed] [Google Scholar]
- 30.Overbey KN, Schwab KJ, Exum NG. Comparison of 1-week and 2-week recall periods for caregiver-reported diarrhoeal illness in children, using nationally representative household surveys. Int J Epidemiol 2019;48:1228–39. 10.1093/ije/dyz043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prinja S, Jeet G, Kumar R. Validity of self-reported morbidity. Indian J Med Res 2012;136:722–4. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-004010supp001.pdf (76KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. The Demographic and Health Surveys are publicly available to researchers on request.


