Abstract
A case of regenerative endodontics: (a) before treatment; (b) post‐treatment Xray; (c) follow‐up at 6 months; (d) follow‐up at 12 months.
Keywords: Mineral Trioxide Aggregate, Necrotic immature teeth, Regenerative endodontics, Root canal irrigants
Key Clinical Message
The present report demonstrates that desiccant agent Hybenx cleanser could be used successfully in necrotic teeth with incomplete root development and apical lesion to realize single appointment regenerative endodontic therapy.
CLINICAL RELEVANCE
Scientific rationale for the study: Patients with immature necrotic teeth could be treated in a single appointment.
Principal Finding: The present report demonstrates that desiccant agent Hybenx cleanser could be used successfully in necrotic teeth with incomplete root development and apical lesion.
Practical implications: The present report documents two successful single appointment regenerative endodontic therapy using desiccant agent Hybenx cleanser in necrotic teeth with incomplete root development and apical lesion.
1. INTRODUCTION
Regenerative endodontic treatment is one of the most innovative challenges for the clinician in the management of necrotic teeth with immature apices. In the past apexification with calcium hydroxide or placement of a mineral trioxide aggregate (MTA), apical plug yielded satisfactory outcomes in terms of resolving the patients’ clinical signs and symptoms and periapical radiolucent lesions.1, 2, 3 Although they were predicable, these traditionally treatment protocols for immature nonvital teeth often did not promote either the roots development or the pulp‐dentin complex and its functions. Regenerative endodontic procedure (REPs) or revascularization procedures were introduced nearly fifteen years ago4 to overcome the arrest of root formation and dentin‐pulp complex development.5 The principles of REPs were borrowed from tissue engineering: mesenchymal stem cells derived from the laceration of apical papilla (SCAPs), a suitable 3‐dimensional (3‐D) matrix scaffold for appropriate organization of stem cells, and growth factors that could influence and act on the stem cells environment.6 The interaction of these three elements permits the continue root formation and the restoration of immune and sensory function within the pulpal space.7
Complete root development allows a favorable crown to root ratio and improvement of dentinal wall thickness and it promotes the development of biological tissue in the root canal, all of which could contribute to reducing the risk of root fractures that can occur after MTA and/or calcium hydroxide apexification procedures.1, 8, 9 The biological balance between the efficient eradication of preoperative root canal infections10, 11 and the survival of stem cell and bioactive properties of root dentin11, 12 heavily influences the success of REPs.
A low concentration of sodium hypochlorite (NaOCl) 1.5% and the subsequent use of 17% EDTA have a minimal effect on stem cells survival and promote the release of bioactive molecules from dentinal matrix.13 Early case reports of revascularization/regenerative endodontics describe the successful use of an antibiotic mixture as intracanal/interappointment medication to improve the eradication of root canal infections in necrotic teeth with immature root development.4, 14, 15 Triple (TAP) or double (DAP) antibiotic past consisting of ciprofloxacin, and metronidazole with or without minocycline commonly used in REPs, has a toxic effect on SCAPs at high concentration.12, 16
As in the apexification procedure, the use of interappointment medications in REPs did not permit a single visit procedure, thereby further increasing microbial contamination from oral cavity with a negative impact on the vitality of the apical papilla.17 There are only a few case reports of successful single‐visit regenerative endodontic treatment that used irrigant solutions alone to manage the intracanal infection.18, 19
Recently, a new desiccant agent, HYBENX® cleanser (EPIEN Medical Inc, St. Paul, MN, USA), was introduced for endodontic therapy; the manufacturer recommended the use of HYBENX® cleanser as an adjunctive rinse for root canal systems. HYBENX® cleanser (EPIEN Medical Inc, St. Paul, MN, USA) is a mixture of hydroxybenzenesulfonic and hydroxymethoxybenzene acids. It is a debriding solution for plaque and oral biofilm control in periodontal and endodontic disease.20, 21
It was successfully used for the treatment of chronic periodontitis to enhance the efficacy of traditional therapy (scaling and root planing), and it reduces pathogens of periodontal socket biofilm.22, 23 Consistent results were described in a case report for the treatment of an acute periodontal abscess.24
The present report describes 2 regenerative endodontic treatment using HYBENX® cleanser as antibiofilm agent in two immature necrotic teeth with periapical radiolucency.
1.1. Cases report
1.1.1. Case 1
A 15‐year‐old boy presented to the Endodontics Clinic of the Unit of Dentistry of the Careggi University Hospital in June 2018; he was referred for evaluation of right second mandibular premolar. The patient had no significant medical history or known drug allergies. The parents reported a previous episode of pain and swelling for which his dentist prescribed antibiotic therapy (amoxicillin) for 6 days before performing a pulpotomy and a temporary restoration.
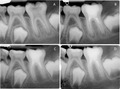
During the first visit, extra‐oral examinations were within normal limit, and the second mandibular premolar was coronally restored with Cavit (3M ESPE, St Paul, MN). It was sensitive to percussion and palpation and not responsive to cold pulp testing when compared to the contralateral tooth; no mobility and a normal periodontal probing depth were recorded. Radiographic examinations showed a periapical radiolucent area and a radiopaque intracanal medication; root length, thickness of canal walls, and the opening of the apex confirmed the incomplete root development (Figure 1A). After discussing the possible treatment options, patient's parents approved the regenerative endodontics therapy and provided informed written consent.
FIGURE 1.
Treatment of second mandibular right premolar. (A) Diagnostic radiograph that showed the presence of radiopaque intracanal and coronal filling associated with periapical radiolucent lesion. (B) Radiograph of tooth to check the placement of MTA barrier. (C) Six‐month radiographic follow‐up showing the complete resolution of periapical radiolucent lesion. (D) Twelve‐month radiographic follow‐up
The study design was approved by the Ethical Committee of the Careggi University Hospital (Permission no. SPE 16.302). The study was conducted in full accordance with the World Medical Association Declaration of Helsinki on experimentation involving human subjects, as revised in 2008.
The second mandibular premolar was anesthetized with 3% mepivacaine (Scadonest Septodont; Cedex, France) without vasoconstrictor in order to obtain an inferior alveolar nerve block. The tooth was isolated with rubber dam, and Cavit was removed. The entire procedure was performed under surgical microscope: The access was refinished using an ultrasonic tip, Start‐X 3 (Dentsply Maillefer Ballaigues, Suisse). The canal was copiously irrigated with sterile water and dried for inspection; no apical vital tissue was detected. The working length (WL) was determined by placing a size #80 hand K‐file at the end of the root canal under magnification and was confirmed with a periapical radiograph. The canal was irrigated with 2.5% of NaOCl and gently dried with paper points; 2ml of HYBENX® cleanser (Epien Medical, Inc, St. Paul, USA) was introduced into the canal using a capillary tip 2 mm shorter than the WL. A paper point was inserted into the canal 2‐mm short WL with an up‐and‐down movement for 30 seconds to favor a homogeneous distribution on the root canal walls. The HYBENX® cleanser was completely removed using 5 ml of sterile water as the final irrigant and sterile paper points were used to dry the root canals and to confirm no sign of bleeding or exudate for the entire WL. The bleeding was induced over‐instrumenting with a #30 hand K‐file beyond the apex. Hemostasis was promoted with a sterile cotton pellet at the level of the cementoenamel junction, 3 mm of Pro‐Root MTA (Dentsply Tulsa Dental, Tulsa, OK) was placed over the formed blood clot to seal the coronal portion of the root canal, and a radiograph was taken (Figure 1B).
About 3 mm RelyX™ Unicem Self‐Adhesive Universal Resin Cement (3M ESPE, Seefeld, Germany) was used to cover the MTA plug, and in the same appointment, the tooth was coronally restored with self‐etch adhesive cement associated with composite resin.
Follow‐ups were advised every 6 months during a 12‐month period. No pain, swelling, or tooth discoloration was reported at any of the control visits. There was no mobility or response to thermal pulp tests, and probing depth was within normal limits.
At six months, radiographic examination of treated tooth showed an almost completely radiographic resolution of the initial periapical radiolucency; no root development was observed. An intracanal radiopaque area was detected under the MTA plug at baseline and at the 6‐month radiographic follow‐up (Figure 1C).
At 12 months in treated tooth, a complete resolution of the periapical radiolucent area has been observed; there was no improvement of root development with respect to the baseline and 6‐month radiographic follow‐up (Figure 1D).
1.1.2. Case 2
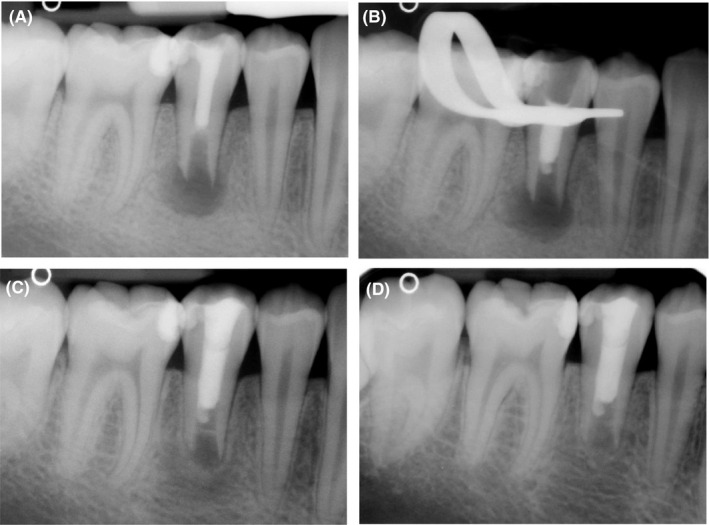
An 8‐year‐old boy was referred to Endodontics Clinic of the Unit of Dentistry of the Careggi University Hospital for examination of first mandibular left molar. The clinical examination during the first visit did not reveal signs of swelling, or pain to percussion and palpation. The first mandibular molar had a deep occlusal caries and no response to cold test; no pathologic periodontal probing depth or mobility was recorded. Radiographic examination revealed a large periapical radiolucency encompassing both the mesial and distal roots with incomplete root development in terms of length and thickness (Figure 2A). Pulp necrosis associated with asymptomatic apical periodontitis was diagnosed.
FIGURE 2.
Treatment of first left mandibular molar. (A) Preoperative radiograph of molar tooth. (B) Postoperative radiograph of first molar after treatment. (C) Six‐month radiographic follow‐up demonstrating the resolution of periapical lesion. (D) Twelve‐month follow‐up radiograph showing a partial apical closure of both roots
After discussing possible treatment options, the patient's mother opted for pulp revascularization and she gave her informed consent.
The study design was approved by the Ethical Committee of the Careggi University Hospital (Permission no. SPE 16.302). The study was conducted in full accordance with the World Medical Association Declaration of Helsinki on experimentation involving human subjects, as revised in 2008.
The tooth was anesthetized with 3% mepivacaine (Scadonest Septodont; Cedex, France) without vasoconstrictor, and it was then isolated with a rubber dam. After removing carious tissues, the endodontic access was completed using a diamond‐coated fissure bur (801 Komet, Milan, Italy) with copious sterile water; bleeding and exudate were observed. A total of 20 ml of irrigation with 2.5% NaOCl was used to manage the exudate and the bleeding from all roots canals. The residual necrotic pulp tissue was removed. The WL was determined with a periapical radiograph acquired by placing a size #60 K‐file at the end of both roots canals.
The canals were dried with paper points, and 2ml of HYBENX® cleanser was introduced into the canal using a capillary tip 2 mm shorter than WL. A paper point was used with an up‐and‐down movement to promote a homogeneous distribution into both canals. The HYBENX® cleanser was completely removed using 5 ml of sterile water as the final irrigant; sterile paper points were used to dry the root canals and to confirm that there was no bleeding or exudate throughout WL. As described before, bleeding was induced; 3 mm of Pro‐Root MTA (Dentsply Tulsa Dental, Tulsa, OK) was placed and covered with RelyX™ Unicem and composite resin. A final postoperative radiographic examination was taken (Figure 2B).
At the 6‐ and 12‐month follow‐up visits, the patient reported no pain, swelling, and/or tooth discoloration; the treated tooth responded negatively to electric pulp test. Radiographic examination at 6‐month follow‐up showed a reduction of periapical radiolucency adjacent to the mesial and distal roots (Figure 2C). At 12 months, the treated mandibular molar showed a complete resolution of the periapical lesions, no development of roots has been detected in terms of thickness and length, and the roots showed a partial apical closure (Figure 2D).
2. DISCUSSION
Regenerative endodontic therapy considers various operative protocols to manage non‐vital permanent immature teeth. One of the differences between the proposed techniques consists of different irrigant protocols adopted to eradicate biofilm from canal spaces. Bacterial molecules or metabolites might hinder the survival and the differentiation process of stem cells,25 growth factors, and scaffold in order to achieve a predictable and successful outcome.11 The American Association of Endodontics recommended the use of antibiotics at low concentrations,5 even though a recent in vitro study documented that low concentrations of DAP were not able to ensure a complete eradication of biofilm and prevent the possible repopulation of residual bacterial from the oral cavity.26 Antibiotic eluting‐polymer nanofibers to deliver drugs to strengthen the antimicrobial effects of antibiotics on dentin biofilm and the ability of dental pulp stem cells to attach and proliferate on dentin surfaces have been recently tested in vitro.27
However, the disadvantages correlated with the use of antibiotic paste, such as discoloration and the length of the therapy due to interappointment medications,28, 29 have not been resolved.
The need for a single appointment protocol in regenerative endodontic treatments was supported by recent randomized clinical trial that compared results obtained after immediate and delayed induction for necrotic immature teeth.30
As suggested in a recent systematic review,31 the length of the treatment is strictly connected to the disinfection process as well as the maintenance of vitality of the apical papilla32: it is significantly longer in regenerative endodontic procedures than in the MTA apical technique. The review maintains that only after the use of intracanal medication, ranging from a few days to months, a blood clot associated with the MTA apical barrier may be used as scaffold.31 The biological principles of single visit REPs are based on the antibiofilm effect of irrigant solution to manage the intracanal infection of immature necrotic teeth. The importance of predictable disinfection protocol has been also stressed in a recent review.33 Tagelsir et al showed that only 5 minutes of 1.5% NaOCl has an antibiofilm effect comparable to 500 mg/mL of DAP and Ca(OH)2 with one‐week exposure: both strategies permit a complete eradication of Enterococcus Faecalis biofilm.26
In the present case reports, the efficacy of irrigants solutions was improved with the use of HYBENX® cleanser. The mechanism of actions of desiccant agents is not completely understood but it may be attributed to the high affinity of sulfonic/sulfuric acids to bind water present in the biofilm leading to its detachment and destruction.24, 34 The use of HybenX as oral tissue decontaminant in vital pulp therapy has been documented only in dogs, where it showed better odontoblast inductive properties than Ca(OH)2.35 In REPs, the use of desiccant agents can improve the antimicrobial actions of irrigant solutions during chemical decontamination of the root canal space. It may be very important because the bacteria biofilm in immature necrotic teeth is different than in mature teeth.36 In a recent study, Jacobs et al reported a more antibiotic‐resistant bacterial biofilm in immature teeth and that these teeth are more susceptible to bacterial repopulation than mature teeth.37 Bacterial resistance is one of the greatest challenges facing the scientific community.
In the two reported cases, adequate bleeding and blood clots were obtained by pushing a K‐file beyond the apex, while no matrix was used to assist in the placement of MTA. Based on Botero et al observations,42 the intracanal bleeding can represent a crucial step in predicting the final results. Failure occurred after 3 months in the cases where intracanal bleeding cannot be established.30 Finally, the lack of interappointment medications such as the use of TAP/DAP or Ca(OH)2 prevents the risk of discoloration and bacterial regrowth within the root canal system,32, 38 enhancing the patient compliance.18 Neither case showed a continued root development except for a slight apical closure on the roots of #19 tooth associated with the resolution of the apical lesion and absence of clinical signs at the 12‐month follow‐ups. These findings are in agreement with the review by Torabinejad et al that reported a vary rate of root development varying from 21% to 100% and an average tooth follow‐up time of 16.7 months.31
In Case 1, tooth #20 showed an intracanal radiopaque line below the MTA plug. Although this radiopaque line may be similar to the calcific barrier reported by Song et al,39 it might not be revascularization‐associated intracanal calcification because it was already present at the end of the therapy.
The use of two‐dimensional images (endo‐oral radiographs) represented a limitation when interpreting the results of the present study even if a standardized angulation has been used in each follow‐up radiograph.
The proposed protocol consents a single appointment therapy, which is fundamental in young patients with poor compliance and difficult follow‐ups.
The results of the present study support the use of Hybenx® in regenerative endodontic therapy, even more microbiological studies are needed to set up the best protocol of disinfection to control the intracanal biofilm and contemporary preserve the vitality of stem cell in the apical papilla.
Further clinical studies with larger sample sizes are still required to support the successful outcome of regenerative endodontic treatment with Hybenx®.
AUTHORS’ CONTRIBUTIONS
Riccardo Pace: Data Curation—Investigation (equal)—Writing—original Draft preparation—Writing—Reviewing & Editing (equal). Giuliani Valentina: Investigation (equal)—Writing—Reviewing & Editing (equal). Luca Di Nasso: Writing—Reviewing & Editing (equal). Gabriella Pagavino: Supervisor—Writing—Reviewing and Editing (equal). Debora Franceschi: Writing—Reviewing & Editing (equal). Franchi Franchi: Supervisor—Writing—Reviewing and Editing (equal).
Funding
The study was self‐funded by the authors.
ETHICAL APPROVAL
The study was approved by the Ethical Committee, Area Biomedica University of Florence (2019).
ACKNOWLEDGMENTS
The authors declare that there are no conflicts of interest regarding the publication of this article.
Pace R, Giuliani V, Di Nasso L, Pagavino G, Franceschi D, Franchi L. Regenerative Endodontic Therapy using a New Antibacterial Root Canal Cleanser in necrotic immature permanent teeth: Report of two cases treated in a single appointment. Clin Case Rep. 2021;9:1870–1875. 10.1002/ccr3.3696
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, Giuliani Valentina, upon reasonable request.
REFERENCES
- 1.Jeeruphan T, Jantarat J, Yanpiset K, Suwannpan L, Khewsawi P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012;38:1330‐1336. [DOI] [PubMed] [Google Scholar]
- 2.Pace R, Giuliani V, Nieri M, Di Nasso L, Pagavino G. Mineral trioxide aggregate as apical plug in teeth with necrotic pulp and immature apices: a 10‐year case series. J Endod. 2014;40:1250‐1254. [DOI] [PubMed] [Google Scholar]
- 3.Cvek M. Endodontic management and the use of calcium hydroxide in traumatized permanent teeth. Textbook and color atlas of traumatic injuries to the teeth, 4th edn. Oxford: Blackwell; 2007:598‐657. [Google Scholar]
- 4.Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004;4:196‐200. [DOI] [PubMed] [Google Scholar]
- 5.American Association of Endodontists, AAE clinical considerations for a regenerative procedure. Revised 6–8‐16. Available at: https://www.aae.org/uploadedfiles/publications_and_research/research/currentregenerativeendodonticconsiderations.pdf. Accessed October 12, 2016.
- 6.Langer R, Vacanti JP. Tissue engineering. Science. 1993;260:920‐926. [DOI] [PubMed] [Google Scholar]
- 7.Hargreaves KM, Diogenes A, Teixeira FB. Treatment options: biological basis of regenerative endodontic procedures. Pediatr Dent. 2013;35:129‐140. [PubMed] [Google Scholar]
- 8.Whitherspoon DE, Small JC, Regan JD, Nunn M. Retrospective analysis of open apex teeth obturated with mineral trioxide aggregate. J Endod. 2008;34:1171‐1176. [DOI] [PubMed] [Google Scholar]
- 9.Andreasen JO, Farik B, Munksgaard EC. Long‐term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134‐137. [DOI] [PubMed] [Google Scholar]
- 10.Fouad AF, Nosrat A. Pulp regeneration in previously infected root canal space. Endod Top. 2013;28:24‐37. [Google Scholar]
- 11.Diogenes A, Ruparel NB, Teixiera FB, Hargreaves KM. Translational science in disinfection for regenerative endodontics. J Endod. 2014;40:S52‐S57. [DOI] [PubMed] [Google Scholar]
- 12.Martin DE, De Almeida JF, Henry MA, et al. Concentration‐dependent effect of sodium hypochlorite on stem cells of apical papilla survival and differentiation. J Endod. 2014;40:51‐55. [DOI] [PubMed] [Google Scholar]
- 13.Galler KM, Krastl G, Simon S, et al. European society of endodontology position statement: revitalization procedures. Int Endod J. 2016;49:717‐723. [DOI] [PubMed] [Google Scholar]
- 14.Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001;17:185‐187. [DOI] [PubMed] [Google Scholar]
- 15.Petrino JA, Boda KK, Shambarger S, Bowles WR, McClanahan SB. Challenges in regenerative endodontics: a case series. J Endod. 2010;36:536‐541. [DOI] [PubMed] [Google Scholar]
- 16.Althumairy RI, Teixeira FB, Diogenes A. Effect of dentin conditioning with intracanal medicaments on survival of stem cells of apical papilla. J Endod. 2014;40:521‐525. [DOI] [PubMed] [Google Scholar]
- 17.McCabe P. Revascularization of an immature tooth with apical periodontitis using a visit protocol: a case report. Int Endod J. 2015;48:484‐497. [DOI] [PubMed] [Google Scholar]
- 18.Shin SY, Albert JS, Mortman RE. One step pulp revascularization treatment of an immature permanent tooth with chronic apical abscess: a case report. Int Endod J. 2009;42:1118‐1126. [DOI] [PubMed] [Google Scholar]
- 19.Topçuoğlu G, Topçuoğlu HS. Regenerative endodontic therapy in a single visit using platelet‐rich plasma and biodentine in necrotic and asymptomatic immature molar teeth: a case report of 3 cases. J Endod. 2016;42:1344‐1346. [DOI] [PubMed] [Google Scholar]
- 20.Antonelli A, Giovannini L, Baccani I, Giuliani V, Pace R, Rossolini GM. In vitro antimicrobial activity of the decontaminant hybenX(®) compared to chlorhexidine and sodium hypochlorite against common bacterial and yeast pathogens. Antibiotics (Basel). 2019;17(8):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ye WH, Fan B, Purcell W, et al. Anti‐biofilm efficacy of root canal irrigants against in‐situ enterococcus faecalis biofilms in root canals, isthmuses and dentinal tubules. J Dent. 2018;79:68‐76. [DOI] [PubMed] [Google Scholar]
- 22.Isola G, Matarese G, Williams RC, et al. The effects of a desiccant agent in the treatment of chronic periodontitis: a randomized, controlled clinical trial. Clin Oral Investig. 2017;22:791‐800. [DOI] [PubMed] [Google Scholar]
- 23.Lombardo G, Signoretto C, Corrocher G, et al. A topical desiccant agent in association with ultrasonic debridement in the initial treatment of chronic periodontitis: a clinical and microbiological study. New Microbiol. 2015;38:393‐407. [PubMed] [Google Scholar]
- 24.Pini‐Prato G, Magnani C, Rotundo R. Treatment of acute periodontal abscesses using the biofilm decontamination approach: a case report study. Int J Periodontics Restorative Dent. 2016;36:55‐63. [DOI] [PubMed] [Google Scholar]
- 25.Vishwanat L, Duong R, Takimoto K, et al. Effect of bacterial biofilm on the osteogenic differentiation of stem cells of apical papilla. J Endod. 2017;43:916‐922. [DOI] [PubMed] [Google Scholar]
- 26.Tagleris A, Yassen GH, Gomez GF, Gregory RL. Effect of antimicrobials used in regenerative endodontic procedure on 3‐week‐old Enterococcus faecalis biofilm. J Endod. 2016;42:258‐262. [DOI] [PubMed] [Google Scholar]
- 27.Albuquerque MTP, Nagata J, Bottino MC. Antimicrobial efficacy of triple antibiotic–eluting polymer nanofibers against multispecies biofilm. J Endod. 2017;43:S51‐S56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheek CC, Heymann HO. Dental and oral discolorations associated with minocycline and other tetracycline analog. J Esthet Dent. 1999;11:43‐48. [DOI] [PubMed] [Google Scholar]
- 29.As L. Consideration for regeneration procedures. Pediatr. Dent. 2013;35:141‐152. [PubMed] [Google Scholar]
- 30.Botero TM, Tang X, Gardner R, Hu JCC, Boynton JR, Holland GR. Clinical evidence for regenerative endodontic procedures: immediate versus delayed induction? J Endod. 2017;43:S75‐S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torabinejad M, Nosrat A, Verma P. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta‐analysis. J Endod. 2017;43:1806‐1820. [DOI] [PubMed] [Google Scholar]
- 32.Kim J‐H, Kim Y, Shin S‐J, et al. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod. 2010;36:1086‐1091. [DOI] [PubMed] [Google Scholar]
- 33.Staffoli S, Plotino G, Nunez Torrijos BG, et al. Regenerative endodontic procedures using contemporary endodontic materials. Materials (Basel). 2019;19:908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Porter SR, Al‐Johani K, Fedele S, Moles DR. Randomized controlled trial of the efficacy of HybeniX in the symptomatic treatment of recurrent aphthous stomatitis. Oral Dis. 2009;15:155‐161. [DOI] [PubMed] [Google Scholar]
- 35.Rohrer MD, Prasad HS, Savord EG. A histologic assessment of a HYBENX® oral tissue decontaminant in vital pulp therapy in dogs. J Biol Regul Homeost Agents. 2016;30:189‐197. [PubMed] [Google Scholar]
- 36.Cvek M, Nord CE, Hollender L. Antimicrobial effect of root canal debridement in teeth with immature root. A clinical and microbiologic study. Odontol Revy. 1976;27:1‐10. [PubMed] [Google Scholar]
- 37.Jacobs JC, Troxel A, Ehrlich Y, et al. Antibacterial effects of antimicrobials used in regenerative endodontics against biofilm bacteria obtained from mature and immature teeth with necrotic pulps. J Endod. 2017;43:575‐579. [DOI] [PubMed] [Google Scholar]
- 38.Peters LB, van Winkelhoff AJ, Buijs JF, et al. Effects of instrumentation, irrigation and dressing with calcium hydroxide on infection in pulpless teeth with periapical bone lesions. Int Endod J. 2002;35:13‐21. [DOI] [PubMed] [Google Scholar]
- 39.Song M, Cao Y, Shin SJ, et al. Revascularization‐associated intracanal calcification: assessment of prevalence and contributing factors. J Endod. 2017;43:2025‐2033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Giuliani Valentina, upon reasonable request.


