Abstract
Advanced breast cancer with skin ulceration, bleeding, and odor is associated with impaired quality of life (QoL). In patients with metastatic breast cancer, treatment aims to relieve symptoms, improve QoL, and slow the progression of cancer. Occasionally, it is extremely difficult to alleviate symptoms and improve QoL in patients with breast cancer and skin ulceration, especially elderly patients. Since patient age, patient preferences, and the expected survival benefit from treatment are factors that influence the selection of therapy, physicians should provide an optimal treatment for patients with metastatic disease depending on the situation. In this study, we report the case of an elderly patient with metastatic breast cancer who had substantial skin ulceration. In this patient, multidisciplinary treatment including chemotherapy, radiotherapy, and surgery resulted in significantly improved QoL.
Keywords: Skin ulceration, Metastatic breast cancer, Quality of life
Introduction
Approximately 3–8% of patients with breast cancer have metastatic disease at initial presentation [1]. The role of the primary breast tumor and its impact on distant metastatic disease and patient survival are controversial. Growing evidence from retrospective studies and meta-analyses suggests that surgical treatment of the primary breast tumor has a positive impact on survival [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]. However, some prospective studies are ongoing, and one study indicated that locoregional treatment of the primary tumor conferred no overall survival advantage in patients with metastatic breast cancer [15].
Conversely, some experts insist that symptom palliation is the only indication for locoregional treatment of the primary tumor in patients with metastatic breast cancer because skin ulceration, bleeding, and odor reduce patients' quality of life (QoL). However, it is also uncertain whether resection of the primary tumor leads to improvements in QoL because advances in systemic therapies and targeted therapies as well as a better understanding of tumor biology might lead to significant effects on locoregional disease control and QoL.
In this study, we observed significant improvements in QoL following multidisciplinary treatment in an elderly patient with metastatic breast cancer who had substantial skin ulceration and fungation.
Case Report
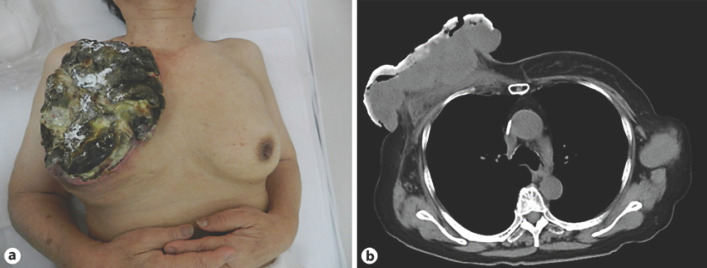
An 80-year-old woman was diagnosed with right breast cancer and multiple lung metastases at a previous institute a few months after she had noticed a right breast lump with progressive skin invasion. Chemotherapy was provided for 4 years. However, she was referred to our institute in December 2017 because the breast tumor progressed despite systemic treatment. She had a right breast lump with 15 cm of skin ulceration as well as bleeding, fungation, and odor at presentation (Fig. 1a). Breast biopsy revealed invasive ductal carcinoma, and immunohistochemistry of the tumor confirmed the following findings: HER2 1+, estrogen receptor-negative, progesterone receptor-negative, and Ki-67 = 40%. Computed tomography revealed a right breast tumor with skin ulceration, bilateral axillary lymph node metastases (Fig. 1b), and multiple lung metastases. The results of blood tests indicated slight anemia and mild elevation of white blood cell counts, and the levels of carcinoembryonic antigen reached 603 ng/mL. The symptoms of the breast tumor, such as bleeding, odor, and pain, impaired her QoL, and the Eastern Cooperative Oncology Group performance score was 0. Additionally, it was difficult for the patient to change bandages and clean the lesion by herself. The aim of treatment at this time was to alleviate intolerable symptoms considering her age and desire to survive without bleeding and odor from the breast tumor.
Fig. 1.
a Appearance of the breast mass at presentation. Image of the breast lesion illustrating the fungating breast ulcer on a large and irregularly shaped right breast mass. b Computed tomography image at presentation revealing a large right breast tumor with skin ulceration and bilateral axillary lymph node metastases.
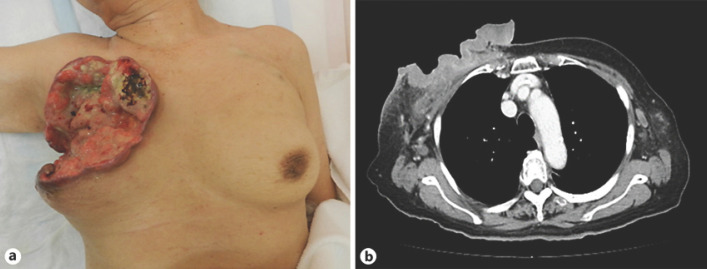
Mohs' paste was applied to the bleeding tumor, and subsequently reduced-dose bevacizumab and paclitaxel were administered, relieving the patient's bleeding and odor. The size of the tumor decreased after 3 months, resulting in a partial response. Six months after the administration of bevacizumab and paclitaxel, tumor regrowth was observed, leading to the diagnosis of disease progression even though the primary tumor was smaller than its initial size at presentation (Fig. 2).
Fig. 2.
a Appearance of the breast mass after the administration of bevacizumab and paclitaxel. b Computed tomography image after the use of Mohs' paste and the administration of bevacizumab and paclitaxel.
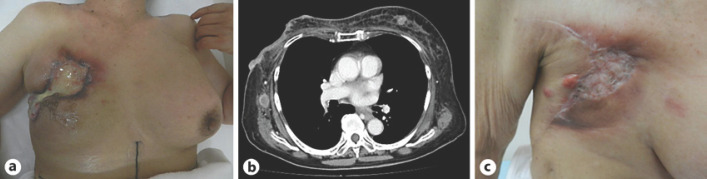
After disease progression, radiotherapy (51 Gy in 17 fractions) was delivered to the right breast and chest wall, followed by eribulin administration. Two months after the administration of eribulin, a partial response was obtained, although tumor effusion was still observed (Fig. 3a, b). However, as disease progression can result in acquired chemotherapy resistance, mastectomy and skin grafting were performed. Immunohistochemistry of the tumor confirmed the following findings: HER2 1+, estrogen receptor-negative, progesterone receptor-negative, and Ki-67 = 40%. After surgery, she experienced significant improvement in QoL based on the elimination of bleeding and odor, and she did not need to replace her bandages daily (Fig. 3c). Despite improvement in QoL and medical palliative care, the patient died from multiple lung metastases 12 months after surgery.
Fig. 3.
a Appearance of the breast mass after the administration of eribulin. b Computed tomography image after the use of Mohs' paste and the administration of eribulin. c Appearance of the breast mass after mastectomy and skin grafting.
Discussion
Metastatic breast cancer is considered an incurable disease, and the primary goals of treatment are prolongation of survival and palliation of symptoms. The primary treatment is systemic therapy including chemotherapy, endocrine therapy, and targeted agents. Traditionally, locoregional treatment such as surgery or radiation has only been used to alleviate symptoms related to breast tumor including bleeding and fungation. Some retrospective studies reported that locoregional treatment provided an overall survival benefit in patients with metastatic breast cancer [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14]. Other retrospective analyses did not describe any survival advantage after locoregional treatment [16, 17, 18, 19, 20]. A randomized trial found no evidence that locoregional treatment of the primary tumor improves overall survival in patients with metastatic breast cancer [15]. Additionally, the study suggested that surgical treatment of the primary tumor in patients with metastatic breast cancer could not be justified for achieving palliation and symptom control because only 10% of patients in the group that did not receive locoregional treatment required palliative surgery during follow-up.
However, some patients with metastatic breast cancer in the real world require or prefer locoregional treatment. The elderly patient in this case report is a representative of such patients. The most important finding in this case was that QoL was improved and her wishes were met using multidisciplinary treatment. Systemic therapy, radiotherapy, and Mohs' paste contributed to tremendous tumor regression. In addition, daily medical treatment such as gauze exchange and replacement as well as cleaning of the wound were temporarily unnecessary after treatment, resulting in improved QoL.
Statement of Ethics
The patient's son provided written informed consent for publication of this case, including images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have no funding source to report.
Author Contributions
R. Matsunuma and K. Yamaguchi wrote the manuscript. All authors critically reviewed the manuscript for content.
Acknowledgment
We would like to thank the staff and nurses for their kind cooperation. We would also like to thank the patient and her family.
References
- 1.Sant M, Allemani C, Berrino F, Coleman MP, Aareleid T, Chaplain G, et al. Breast carcinoma survival in Europe and the United States: a population-based study. Cancer. 2004;100((4)):715–22. doi: 10.1002/cncr.20038. [DOI] [PubMed] [Google Scholar]
- 2.Khan SA, Stewart AK, Morrow M. Does aggressive local therapy improve survival in metastatic breast cancer? Surgery. 2002;132((4)):620–7. doi: 10.1067/msy.2002.127544. [DOI] [PubMed] [Google Scholar]
- 3.Rapiti E, Verkooijen HM, Vlastos G, Fioretta G, Neyroud-Caspar I, Sappino AP, et al. Complete excision of primary breast tumor improves survival of patients with metastatic breast cancer at diagnosis. J Clin Oncol. 2006;24((18)):2743–9. doi: 10.1200/JCO.2005.04.2226. [DOI] [PubMed] [Google Scholar]
- 4.Fields RC, Jeffe DB, Trinkaus K, Zhang Q, Arthur C, Aft R, et al. Surgical resection of the primary tumor is associated with increased long-term survival in patients with stage IV breast cancer after controlling for site of metastasis. Ann Surg Oncol. 2007;14((12)):3345–51. doi: 10.1245/s10434-007-9527-0. [DOI] [PubMed] [Google Scholar]
- 5.Gnerlich J, Jeffe DB, Deshpande AD, Beers C, Zander C, Margenthaler JA. Surgical removal of the primary tumor increases overall survival in patients with metastatic breast cancer: analysis of the 1988–2003 SEER data. Ann Surg Oncol. 2007;14((8)):2187–94. doi: 10.1245/s10434-007-9438-0. [DOI] [PubMed] [Google Scholar]
- 6.Blanchard DK, Shetty PB, Hilsenbeck SG, Elledge RM. Association of surgery with improved survival in stage IV breast cancer patients. Ann Surg. 2008;247((5)):732–8. doi: 10.1097/SLA.0b013e3181656d32. [DOI] [PubMed] [Google Scholar]
- 7.Bafford AC, Burstein HJ, Barkley CR, Smith BL, Lipsitz S, Iglehart JD, et al. Breast surgery in stage IV breast cancer: impact of staging and patient selection on overall survival. Breast Cancer Res Treat. 2009;115((1)):7–12. doi: 10.1007/s10549-008-0101-7. [DOI] [PubMed] [Google Scholar]
- 8.Le Scodan R, Stevens D, Brain E, Floiras JL, Cohen-Solal C, De La Lande B, et al. Breast cancer with synchronous metastases: survival impact of exclusive locoregional radiotherapy. J Clin Oncol. 2009;27((9)):1375–81. doi: 10.1200/JCO.2008.19.5396. [DOI] [PubMed] [Google Scholar]
- 9.Ruiterkamp J, Ernst MF, van de Poll-Franse LV, Bosscha K, Tjan-Heijnen VC, Voogd AC. Surgical resection of the primary tumour is associated with improved survival in patients with distant metastatic breast cancer at diagnosis. Eur J Surg Oncol. 2009;35((11)):1146–51. doi: 10.1016/j.ejso.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen DH, Truong PT. A debate on locoregional treatment of the primary tumor in patients presenting with stage IV breast cancer. Expert Rev Anticancer Ther. 2011;11((12)):1913–22. doi: 10.1586/era.11.168. [DOI] [PubMed] [Google Scholar]
- 11.Pathy NB, Verkooijen HM, Taib NA, Hartman M, Yip CH. Impact of breast surgery on survival in women presenting with metastatic breast cancer. Br J Surg. 2011;98((11)):1566–72. doi: 10.1002/bjs.7650. [DOI] [PubMed] [Google Scholar]
- 12.Pérez-Fidalgo JA, Pimentel P, Caballero A, Bermejo B, Barrera JA, Burgues O, et al. Removal of primary tumor improves survival in metastatic breast cancer. Does timing of surgery influence outcomes? Breast. 2011;20((6)):548–54. doi: 10.1016/j.breast.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Rashaan ZM, Bastiaannet E, Portielje JE, van de Water W, van der Velde S, Ernst MF, et al. Surgery in metastatic breast cancer: patients with a favorable profile seem to have the most benefit from surgery. Eur J Surg Oncol. 2012;38((1)):52–6. doi: 10.1016/j.ejso.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Harris E, Barry M, Kell MR. Meta-analysis to determine if surgical resection of the primary tumour in the setting of stage IV breast cancer impacts on survival. Ann Surg Oncol. 2013;20((9)):2828–34. doi: 10.1245/s10434-013-2998-2. [DOI] [PubMed] [Google Scholar]
- 15.Badwe R, Hawaldar R, Nair N, Kaushik R, Parmar V, Siddique S, et al. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: an open-label randomised controlled trial. Lancet Oncol. 2015 Oct;16((13)):1380–8. doi: 10.1016/S1470-2045(15)00135-7. [DOI] [PubMed] [Google Scholar]
- 16.Babiera GV, Rao R, Feng L, Meric-Bernstam F, Kuerer HM, Singletary SE, et al. Effect of primary tumor extirpation in breast cancer patients who present with stage IV disease and an intact primary tumor. Ann Surg Oncol. 2006;13((6)):776–82. doi: 10.1245/ASO.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 17.Cady B, Nathan NR, Michaelson JS, Golshan M, Smith BL. Matched pair analyses of stage IV breast cancer with or without resection of primary breast site. Ann Surg Oncol. 2008;15((12)):3384–95. doi: 10.1245/s10434-008-0085-x. [DOI] [PubMed] [Google Scholar]
- 18.Hazard HW, Gorla SR, Scholtens D, Kiel K, Gradishar WJ, Khan SA. Surgical resection of the primary tumor, chest wall control, and survival in women with metastatic breast cancer. Cancer. 2008;113((8)):2011–9. doi: 10.1002/cncr.23870. [DOI] [PubMed] [Google Scholar]
- 19.Leung AM, Vu HN, Nguyen KA, Thacker LR, Bear HD. Effects of surgical excision on survival of patients with stage IV breast cancer. J Surg Res. 2010;161((1)):83–8. doi: 10.1016/j.jss.2008.12.030. [DOI] [PubMed] [Google Scholar]
- 20.Neuman HB, Morrogh M, Gonen M, van Zee KJ, Morrow M, King TA. Stage IV breast cancer in the era of targeted therapy: does surgery of the primary tumor matter? Cancer. 2010;116((5)):1226–33. doi: 10.1002/cncr.24873. [DOI] [PMC free article] [PubMed] [Google Scholar]