Abstract
Angiosarcoma is a rare form of malignant endothelial cell tumour characterised by rapidly infiltrating anaplastic cells of vascular or lymphatic origin. We report an uncommon case of cutaneous angiosarcoma (cAS) manifesting as rapidly progressive unilateral periorbital oedema. Due to the acute onset of disease, the patient was initially treated with antibiotics for presumed periorbital cellulitis. The lack of response to conservative management raised the suspicion of a more serious condition, which eventually revealed the diagnosis of angiosarcoma through skin biopsy. As suggested by several previous case reports, the subtle manifestation of cAS made it a great mimicker of benign skin conditions. This case report serves as a reminder to the aggressive nature of angiosarcoma which can lead to marked facial swelling within several weeks. As the tumour was not resectable by the time of diagnosis, the patient was offered palliative radiotherapy.
Keywords: Angiosarcoma, Eyelid, Periorbital, Oedema
Introduction
Angiosarcomas are a rare form of malignant endothelial cell tumour characterised by rapidly infiltrating anaplastic cells of vascular or lymphatic origin. They are responsible for 2% of all soft tissue sarcomas, occurring only at the rate of 2–5 cases per 1,000,000 per year [1]. Cutaneous angiosarcoma (cAS) − a subtype of this sarcoma, predominantly affect the elderly (average age of 65–70 years) with a predilection for males compared to females (2:1) and fair-skinned individuals [2]. While certain predisposing factors, including trauma, long-standing lymphoedema, radiation and toxin exposure, were postulated, most reported cAS were primary with no overt aetiology [3].
In this report, we narrated an uncommon case of cAS manifesting as rapidly progressive unilateral periorbital oedema. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Case Presentation
A 91-year-old Caucasian man presented to a general practice clinic in rural Victoria, Australia with a 4-week history of progressive facial oedema primarily affecting his right upper and lower eyelid, associated with a gritty sensation and clear discharge from his affected eye (Fig. 1). The onset of oedema was subacute in nature as it was not noticeable when he was in the clinic for a routine check-up exactly 1 month previously. He denied any itch or pain over the affected area or any visual changes. He had no fever, recent trauma, or symptoms of rhinosinusitis. There was no previously documented allergy. On examination, there was no increased warmth or tenderness over the affected area. Inspection of both eyes revealed no significant abnormalities as the cornea and conjunctivae appeared normal. Visual acuity without correction was 6/7.5 for the right and 6/6 for the left, which were normal for him. Periorbital cellulitis was presumed to be the primary diagnosis and cephalexin was prescribed for 6 days.
Fig. 1.
Right unilateral periorbital oedema.
Six weeks later, he returned with worsening facial oedema. His eyelid was so swollen that he was unable to open his right eye. Leading up to this date, he had two full courses of cephalexin and amoxycillin/clavulanate, topical corticosteroids, as well as trials of warm compression. Unfortunately, these treatments did little to slow down the progression of disease. An urgent computed tomography (CT) scan was ordered. The CT of the head/orbit/sinus showed mild to moderate inflammatory change involving the paranasal sinuses and soft tissue swelling overlying the right orbit and right nasal bone. Given the persistence of facial swelling despite treatment, an incisional biopsy was performed, revealing areas of solid proliferation and abnormal mitotic activity, which suggested underlying squamous cell carcinoma (SCC). However, there were also vascular spaces lined by plump atypical endothelial cells infiltrating the entire dermis. The stains were positive with immunohistochemical vascular markers ERG, CD31, and CD34, and a high proliferation index with Ki67, revealing the diagnosis of extensive cAS (Fig. 2, 3).
Fig. 2.
Angiosarcoma (on the right) adjacent to SCC (on the left) with intervening normal sebaceous glands. The tumour consists of irregular anastomosing channels lined by markedly pleomorphic cells. The vessels dissect through the dermis, and the tumour is poorly circumscribed. This is a relatively well-differentiated area, so you can see the obvious vascular nature of the tumour.
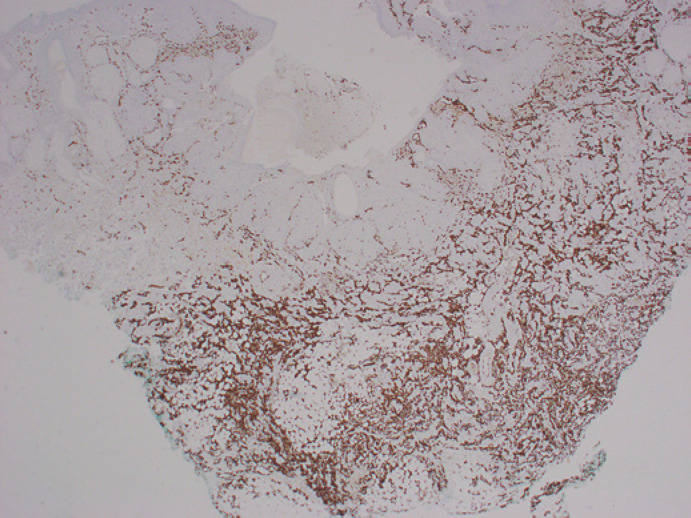
Fig. 3.
ERG showing the tumour dissecting through the dermis into the subcutaneous fat. Note the above SCC does not stain for this marker, allowing clear distinction.
A multidisciplinary approach was taken in managing this patient's condition with the general practitioner playing the central role. Aiming to provide symptomatic relief and improve quality of life, the patient was referred to radiation oncology at the nearest regional hospital for palliative radiotherapy. The palliative care team in the local community was also involved in the end-of-life discussion, which was held in the presence of the patient and his family members. Follow-up with the radiation oncologist was scheduled once every 6 months with regular follow-ups with the general practitioner as required. Up until the time of writing, the patient has had no severe, debilitating symptoms other than gradual progressive facial swelling and discomfort, which was managed with simple analgesia.
Discussion
Differential Diagnosis
The differential diagnosis for unilateral eyelid erythema and oedema is broad, which can be widely categorised into infection, benign skin dermatoses, and tumour. A unilateral swollen red eye often signals infections. Cellulitis was first considered as an initial diagnosis as they are common, but the swelling without pain and no clinical response to antibiotics made this diagnosis unlikely. There was slight crusting seen superior to his right nasolabial fold, but there were no vesicles and erosion suggestive of herpes infection. Benign skin dermatoses, including rosacea, contact or allergic dermatitis, and blepharitis were unconvincing as they are self-limiting and should improve with topical steroids, warm compression, and oral antibiotics. Angioedema was also considered but no potential trigger was identified. All these benign conditions also usually present symmetrically on both sides, which was not demonstrated in this patient.
This patient presented with signs and symptoms that appeared to be benign in nature. Therefore, it was justifiable that tumour was not heavily deliberated as one of the potential causes of swelling. However, given the facial oedema that this patient had was rapidly progressive and acutely debilitating, a soft tissue malignancy should be considered.
Presentation
The case study discussed above highlighted uncommon manifestations of cAS. A rapidly enlarging bruise, erythematous patch, and persistent ulceration are the hallmark presentations of this soft tissue malignancy. With ill-defined ecchymoses or facial oedema being the only initial tell-tale signs, it often progresses within a short period into indurated nodules, haemorrhage, or ulcerations. However, cAS is notoriously known to be a great mimicker of benign skin conditions, thus delaying diagnosis. While xanthelasma-, rosacea-, and alopecia-like lesions were reported in the past, it could also disguise as rhinophyma- or angioedema-like features and eyelid swelling, as narrated in this case.
Cases of cAS affecting the eyelids are rare and it is even rarer for cAS to present so subtly but rapidly with minimal erythema and violaceous lesions. From the list of reported eyelid cAS over the years, there are only 6 published cases in the English literature presenting as non-erythematous non-violaceous eyelid swelling (Table 1) [4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17]. To our knowledge, this is the first case that has the shortest duration of symptoms with an unusual presentation that would have been easily missed. This case served as a reminder of the need for further investigations in patients with suspicious signs, especially in the absence of other infective and inflammatory signs.
Table 1.
Reported cases of cAS with eyelid involvement as initial presentation
| Study | Year | Description | Duration of symptoms | Initial diagnosis prior to biopsy |
|---|---|---|---|---|
| Mackenzie [4] | 1985 | Recurrent firm swelling and new nodules | 30 years | Cellulitis |
| Gunduz et al. [5] | 1998 | Bruise-like maculopapular lesions, subcutaneous nodules, and diffuse oedema | Not documented | Not documented |
| Tay and Ong [6] | 2000 | Recurrent, episodic swelling | 6 months | Angioedema |
| Conway et al. [7] | 2003 | Multifocal, red-blue maculopapular lesions | 9 months | Not documented |
| Hiemstra et al. [8] | 2004 | Red, painless swelling | 6 weeks | Not documented |
| Sluzevich et al. [9] | 2007 | Violaceous, minimally infiltrating plaque | 4 months | Not documented |
| Ettl et al. [10] | 2008 | Diffuse and erythematous painless swelling | 6 months | Allergic dermatitis |
| Papalas et al. [11] | 2010 | Nodular growth and swelling | 6 months | Not documented |
| Wiwatwongwana et al. [12] | 2010 | Erythematous, elevated lesion and poorly defined violaceous papules | 6 weeks | Not documented |
| Cox et al. [13] | 2013 | Slowly progressive swelling | 3 months | Cellulitis |
| Choi et al. [14] | 2013 | Progressive swelling with erythema and induration | 11 months | Angioedema, allergies and autoimmune disorders |
| Ferguson et al. [15] | 2018 | Progressive erythematous swelling | 36 months | Morbihan disease |
| Milman et al. [16] | 2018 | Progressive swelling, blepharoptosis, and nodule | 5 months | Ocular adnexal lymphoma or basal cell carcinoma |
| Chiu et al. [17] | 2020 | Bilateral periorbital oedema | 6 months | Not documented |
Management
The cornerstone treatment for localised cAS was complete resection with wide surgical margins (>1 cm). Owing to a high incidence of widespread local infiltration, resection should be combined with preoperative or postoperative radiotherapy in order to limit locoregional spread. Several retrospective studies showed the efficacy of this combination regime with a prolonged median survival time (36 months compared to 9 months) and improvement in 5-year survival rates (45% compared to 20%) [3].
Patients who have metastatic or unresectable cAS should be considered for chemotherapy. Doxorubicin used to be the chemotherapeutic agent of choice, but in recent times, taxanes such as paclitaxel have emerged as the first-line treatment for advanced cAS. With time, more options for systemic treatments are becoming available, including immunotherapy such as eribulin mesylate (anticancer for breast cancer), trabectedin (histone deacetylase inhibitor), bevacizumab (vascular endothelial growth factor receptor inhibitor), and pazopanib (multityrosine kinase inhibitor) [1].
Among the numerous ongoing studies, the role of propranolol in advanced cAS is being investigated. A case series suggested a reduction of 34% in the proliferative index after 1 week of propranolol monotherapy. Although the evidence of propranolol is currently not as robust as the other systemic therapies, its effectiveness as either a combination therapy or monotherapy in β-adrenergic receptors ADRB1-, ADRB2-, and ADRB3-positive tumours is promising [18] . In this case report, propranolol may be a viable option considering its accessibility and excellent side effect profile.
Prognosis
Due to the frequent misdiagnosis and inherent aggressive nature of this sarcoma, the prognosis has remained poor despite the greater understanding of the intrinsic biologic properties of cAS in the past few years. Approximately 50% of all cAS had distant metastases upon diagnosis. While the mean survival rate for all other types of sarcomas was roughly 65%, the 5-year survival rate of cAS varied between 12 and 35% with advanced age (>65 years), larger tumour size (>5 cm), and cAS of the head being the predictors of poor prognosis [1]. Patients with isolated eyelid involvement had a better survival (100% at 3.2 years) compared with patients with diffuse disease (57% at 3.3 years), albeit true isolated angiosarcoma of the eyelid is extremely rare [11].
Learning Points
Angiosarcoma is a rare form of malignant endothelial cell tumour characterised by rapidly infiltrating anaplastic cells of vascular or lymphatic origin.
The subtle manifestation of cAS made it a great mimicker of benign skin conditions, including rosacea, dermatitis, and cellulitis.
Rapidly progressive facial oedema should warn clinicians of more sinister conditions, including malignancy when other benign conditions seem unlikely.
Conclusion
This case report emphasised the variations in the manifestation of cAS. The prognosis is very poor, particularly when diagnosed late. Owing to that, it is of paramount importance for clinicians to consider this aggressive sarcoma as one of the many differential diagnoses. Curative surgery with or without radiotherapy should always be recommended in localised cAS. Despite the growing number of systemic modalities for advanced cAS in recent years, further research trials are warranted to determine the most efficacious regimen.
Statement of Ethics
The guardian of the subject gave their written informed consent to publish this case, including the publication of images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have no external funding sources to report.
Author Contributions
K.Y.C. is the main author of this case report. He contributed to the literature review, data collection, and writing of the manuscript. S.K. and Q.W.M.A. contributed to reviewing the data and revising the manuscript.
Acknowledgements
The authors would like to extend their gratitude to Dr. Catherine Uzzell, anatomical pathologist, for her contribution in the histopathology reports.
References
- 1.Ishida Y, Otsuka A, Kabashima K. Cutaneous angiosarcoma: update on biology and latest treatment. Curr Opin Oncol. 2018;30((2)):107–12. doi: 10.1097/CCO.0000000000000427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaballah AH, Jensen CT, Palmquist S, Pickhardt PJ, Duran A, Broering G, et al. Angiosarcoma: clinical and imaging features from head to toe. Br J Radiol. 2017;90((1075)):20170039. doi: 10.1259/bjr.20170039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Penel N, Marréaud S, Robin YM, Hohenberger P. Angiosarcoma: State of the art and perspectives. Crit Rev Oncol Hematol. 2011;80((2)):257–63. doi: 10.1016/j.critrevonc.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Mackenzie IJ. Angiosarcoma of the face. Arch Dermatol. 1985;((121)):549–550. [PubMed] [Google Scholar]
- 5.Gunduz K, Shields JA, Shields CL, et al. Cutaneous angiosarcoma with eyelid involvement. Am J Ophthalmol. 1998;125:870–871. doi: 10.1016/s0002-9394(98)00054-3. [DOI] [PubMed] [Google Scholar]
- 6.Tay YK, Ong BH. Cutaneous angiosarcoma presenting as recurrent angio-oedema of the face. Br J Dermatol. 2000;143:1346–1348. doi: 10.1046/j.1365-2133.2000.03933.x. [DOI] [PubMed] [Google Scholar]
- 7.Conway RM, Hammer T, Viestenz A, Holbach LM. Cutaneous angiosarcoma of the eyelids. Br J Ophthalmol. 2003;87:514. doi: 10.1136/bjo.87.4.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hiemstra CA, Mooy C, Paridaens D, et al. Excisional surgery of periocular angiosarcoma. Eye (Lond) 2004;18:738–739. doi: 10.1038/sj.eye.6700653. [DOI] [PubMed] [Google Scholar]
- 9.Sluzevich JC, Gloster HJ, Mutasim DF. A case of regressing central facial cutaneous angiosarcoma. J Am Acad Dermatol. 2008;58((51)):113–115. doi: 10.1016/j.jaad.2007.04.029. [DOI] [PubMed] [Google Scholar]
- 10.Ettl T, Kleinheinz J, Mehrotra R, et al. Infraorbital cutaneous angiosar- coma: a diagnostic and therapeutic dilemma. Head Face Med. 2008;4:18. doi: 10.1186/1746-160X-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiwatwongwana D, White VA, Dolman PJ. Two cases of periocular cutaneous angiosarcoma. Ophthal Plast Reconstr Surg. 2010;26((5)):365–366. doi: 10.1097/IOP.0b013e3181c0e180. [DOI] [PubMed] [Google Scholar]
- 12.Cox CA, Wein RO, Ghafouri R, et al. Angiosarcoma presenting with minor erythema and swelling. Case Rep Ophthalmol. 2013;4:59–63. doi: 10.1159/000346952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi WT, Stetsenko GY, Zhang J, et al. Cutaneous angiosarcoma clin- ically presenting as progressive solid facial edema in a 43-year-old male. Dermatol Online J. 2013;19:20409. [PubMed] [Google Scholar]
- 14.Ferguson DC, Mawn LA, Al-Rohil RN. Cutaneous Angiosarcoma of the Eyelid Mimicking Morbihan Disease. Am J Dermatopathol. 2018;40((8)):617–620. doi: 10.1097/DAD.0000000000001096. [DOI] [PubMed] [Google Scholar]
- 15.Milman T, Shields CL, Brooks JSJ, Lally SE, Shields JA, Tuluc M, et al. Primary Cutaneous Angiosarcoma of the Eyelid: A Diagnostic and Therapeutic Challenge. Ocul Oncol Pathol. 2018;4((4)):230–235. doi: 10.1159/000485427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiu LW, Yang TT, Chen GS. Cutaneous angiosarcoma with an initial presentation of bilateral periorbital swelling. Australas J Dermatol. 2020;1:1–2. doi: 10.1111/ajd.13381. [DOI] [PubMed] [Google Scholar]
- 17.Chow W, Amaya CN, Rains S, Chow M, Dickerson EB, Bryan BA. Growth attenuation of cutaneous angiosarcoma with propranolol-mediated β-blockade. JAMA Dermatology. 2015;151((11)):1226–1229. doi: 10.1001/jamadermatol.2015.2554. [DOI] [PubMed] [Google Scholar]
- 18.Papalas JA, Manavi CK, Woodward JA, Sangueza OP, Cummings TJ. Angiosarcoma of the eyelid a clinicopathologic comparison between isolated unilateral tumors and tumors demonstrating extrapalpebral involvement. Am J Dermatopathol. 2010;32((7)):694–9. doi: 10.1097/DAD.0b013e3181cf7813. [DOI] [PubMed] [Google Scholar]