Abstract
Background
Atherosclerosis cardiovascular disease (ASCVD) is the main cause of morbidity and mortality in type 2 diabetes mellitus (T2DM). As most diabetic patients with ASCVD are asymptomatic, it is most neglected in clinical practice. For this reason, identifying high-risk ASCVD population with intensified treatment is very important. In recent years, the relationship between diabetic retinopathy (DR) and ASCVD has caused much academic concern, but the results are inconsistent. Moreover, whether all grades of DR increase the risk of ASCVD remains controversial. Most importantly, very few data can be found in China.
Objective
Our aim is to discuss whether all grades of DR increase the risk of ASCVD after adjustment for the traditional cardiovascular risk factors and to assess the independent contribution of DR to cardiovascular events in patients with T2DM, hoping to provide more evidence for early identification of ASCVD.
Research design and methods
A total of 425 T2DM patients with complete physical and biochemical data were included in the study. The grade of DR was assessed with two 45 color digital retinal images. Based on the presence of history of ASCVD, 425 T2DM patients were divided into 2 groups: ASCVD group and non-ASCVD group.
Results
ASCVD patients were older and had a significantly higher fasting plasma glucose (FPG) and glycated haemoglobin (HbA1c) and proportion of history of ASCVD. At the same time, they were more likely to be females, and had lower level of alcohol and calculated glomerular filtration rate (eGFR) than non-ASCVD patients. Their trend to develop DR with ASCVD was significantly higher than patients with non-ASCVD (χ2 = 5.805, P = 0.016). DR was an independent statistical indicator of the presence of ASCVD [odds ratio (OR) (95% CI): 2.321 (1.152–4.678), P = 0.018]. Furthermore, when DR was divided into non-proliferative retinopathy (NPDR) and proliferative retinopathy (PDR) according to its severity, only PDR was significantly associated with incident ASCVD [OR (95% CI): 8.333 (1.813–38.304), P = 0.006]. After adjusting for traditional ASCVD risk factors, such an association still existed [OR (95% CI): 7.466 (1.355–41.137), P = 0.021].
Conclusion
DR associates strongly with ASCVD in the Chinese population with T2DM. With the increasing severity of DR, the risk of ASCVD also increases. After adjustment for traditional risk factors, PDR is still an independent risk marker for ASCVD.
Introduction
Diabetic retinopathy (DR) is one of the most common and severe microvascular complications of diabetes mellitus (DM). WHO studies have found that the number of diabetic patients on a global scale reached 366 million in 2011, and this figure is projected to increase even further to over 500 million by the year 2025, and approximately one in three of those sufferers will develop DR [1]. Mounting DR severity has a positive correlation with vision impairment or loss as well as other vision-threatening proliferative diseases [2].
Defined by raised glycemic levels, DM is a major contributor to atherosclerosis cardiovascular disease (ASCVD), the leading cause of death among adults with diabetes mellitus [3]. For this reason, DM is widely seen as an ASCVD risk equivalent. Likewise, of all contributing factors of mortality and morbidity among the DM population, ASCVD tops the list, making up 70% of all deaths [4, 5]. However, DM patients are more likely to suffer from silent myocardial ischemia and myocardial infarction (MI), as up to one-third of those without any manifestation of chest pain experience an acute MI [6]. Worse still, these patients often fail to be treated timely and effectively in cases of emergency, which leads to soaring fatality rates. As a result, early recognition of such high-risk ASCVD population is of top importance.
The association between DR and ASCVD in patients with type 2 DM (T2DM) has drawn considerable international attention, as traditional risk factors for ASCVD, such as hypertension, hyperlipidemia, duration of hyperglycemia and magnitude of glycemia control are well known for the progression and development of DR [7]. There have been a great number of pathophysiological mechanisms that underlie ASCVD in diabetes, but few have been studied [8–13]. However, similar pathophysiological processes may contribute to ASCVD and DR. Previous research indicated that the presence of DR increases the risk of ASCVD, such as stroke [14, 15] and coronary heart disease (CHD) [16, 17]. However, other studies [18, 19] showed that this correlation subsides after adjustment for traditional ASCVD risk factors. What remains disputed is whether each stage of DR is associated with increased risk of ASCVD. Furthermore, present studies focus mainly on European and American people, leading to limited data on Asian people, especially Chinese. The aim of this study is to discuss whether the presence or severity of DR is associated with ASCVD independent of traditional cardiovascular risk factors and to evaluate the independent effect of DR on cardiovascular events in patients with T2DM.
Research design and methods
Study population
Participants of this study were diagnosed T2DM patients from geriatric and endocrine wards in Beijing Tongren Hospital, chosen between January 2018 and June 2020. 447 participants aged 50 or above who were willing to participate and subsequently signed an informed consent received examinations including a physical examination, blood glucose and lipid measurements, renal function tests and ophthalmic examination. After excluding subjects with cataracts, glaucoma, age-related retinopathy or other eye diseases, impaired renal function [calculated glomerular filtration rate (eGFR) < 60 ml/min], cancer, chronic obstructive pulmonary disease (COPD), T1DM, secondary diabetes and chronic pancreatitis, 425 participants with T2DM were divided into two groups (65 with ASCVD and 360 without) for a follow-up comparative study.
Data collection
All participants received a standardized examination. Data regarding age, smoking, alcohol consumption, physical activity, educational level, and history of diabetes, hypertension and ASCVD were obtained with detailed medical records. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Waist circumference (WC) was measured at the level of the umbilicus in cm. Blood pressure (BP) was measured 3 times when participants were seated, and the average of the last 2 measurements was adopted. Blood samples were collected after an overnight fast for the determination of plasma glucose, HbA1c, total cholesterol (TC), triglycerides (TG), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C) concentrations and serum creatinine (Scr). GFR was estimated by using the modified MDRD formula for Chinese patients [20]: eGFR (ml/min/1.73m2) = 175 × Scr−1.234 × age−0.179 × 0.79 (if female).
Definition of clinical and biochemical variables
Various non-fatal ASCVD were determined according to a patient’s self-report. CHD can be defined with a history of myocardial infarction, at least one coronary stenosis more than 50% by coronary angiography or coronary CTA, a surgical history of revascularization (including percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)). The definition of stroke included a history of language or physical dysfunction continuing for more than 24 h and ischemic or hemorrhagic stroke diagnosed using imaging examination [computed tomography or magnetic resonance imaging]. ASCVD referred to a history of CHD or stroke, as defined above. Diagnosis of hypertension was based on meeting any of three criteria: systolic blood pressure (SBP) of ≥ 140 mmHg, diastolic blood pressure (DBP) of ≥ 90 mmHg or current use of antihypertensive drugs [21]. Central obesity was based on WC cutoff ≥ 80 cm in women and ≥ 90 cm in men according to the IDF ethnicity-specific definitions for Asian [22]. Overweight and obesity were respectively identified as BMI 24–28 kg/m2 and BMI equal to or over 28 kg/m2 according to the Working Group on Obesity in China (WGOC) (2002) [23]. Smokers were defined as those who had smoked ≥ 1 cigarette/day for at least 1 year. Drinkers were defined as those who had consumed ≥ 30 g of alcohol/week on average for at least 1 year. Regular leisure-time physical activity was defined as participation in moderate or vigorous activity for 30 min or more per day at least 3 days a week. Educational level was also recorded and categorized into two groups: low (illiteracy, primary, and secondary education), and high (high school education, college or university education). The family history of ASCVD went for first-degree relatives (biological mother, father, brothers, or sisters).
Assessment of retinopathy
All participants received eye examinations by an ophthalmologist and had a bilateral retinal photograph taken of the fundus through dilated pupils. Two 45u color digital images of the retina were taken of each eye by a technologist using a Topcon TRC-NW7SF fundus camera (Topcon, Tokyo, Japan), an ophthalmic digital imaging system. The first image was centered on the macula, and the second on the optic nerve. The photographs were graded by two qualified ophthalmologists from the Eye Center of Capital Medical University, Beijing Tongren Hospital according to the international clinical diabetic retinopathy severity scale [24]: (i) no diabetic retinopathic changes (NDR); (ii) mild non-proliferative diabetic retinopathy (NPDR); (iii) moderate NPDR; (iv) severe NPDR; and (v) proliferative diabetic retinopathy (PDR). The degree of DR was determined according to the grading in the most affected eye. The ophthalmologists grading the photographs were blinded to the patients’ characteristics.
Statistical analysis
All statistical analyses were conducted with the software package SPSS version 22.0 for Windows. For the continuous variables with a normal distribution, mean ± SD was reported and the independent t-test was used to compare subjects with no diabetic retinopathy (NDR) with any stage of diabetic retinopathy (DR). For the discrete variables or the continuous variables without a normal distribution, the median (P25–P75) was reported, and a Mann–Whitney rank test was used to examine the differences between the groups. In the meantime, distribution of discrete/qualitative variables was compared by Pearson chi-square test. Multivariable logistic regression analysis was used to estimate crude and adjusted odds ratios (ORs) (95% CIs) to allow for differences between groups with respect to demographic and risk factors and control for potentially confounding variables. A p-value of less than 0.05 was considered statistically significant.
Results
A total of 425 T2DM patients with (n = 65) or without (n = 360) ASCVD comprised the study groups. There were 165 men and 260 women, with an average age of 58.72 ± 6.82. The total prevalence of DR was 11.29%, 9.65% with NPDR and 1.64% with PDR respectively.
The demographic and biochemical parameters of the two groups are shown in Table 1. Compared with the non-ASCVD group, patients with ASCVD were older, with higher levels of FPG and HbA1c and higher proportion of female and family history of ASCVD, while their level of eGFR and proportion of alcohol were lower. At the same time, there were no statistical differences between the two groups in duration of diabetes, the proportion of smoking, high educational level, physical activity, central obesity, generalized obesity, hypertension and the levels of SBP, DBP, TC, TG, HDL-C, LDL-C (Table 1).
Table 1.
Clinical characteristic of studied subjects with and without ASCVD
| Total | Non-ASCVD | ASCVD | P value | |
|---|---|---|---|---|
| Number (%) | 425 | 360 (84.71) | 65 (15.29) | |
| Age (years) | 58.72 ± 6.82 | 58.27 ± 6.68 | 61.21 ± 7.12 | 0.001 |
| Female (%) | 260 (61.2) | 212 (58.9) | 48 (73.8) | 0.023 |
| Smoking, n (%) | 112 (26.4) | 101 (28.1) | 11 (16.9) | 0.061 |
| Alcohol, n (%) | 125 (29.4) | 114 (31.7) | 11 (16.9) | 0.016 |
| High educational level, n (%) | 26 (6.1) | 22 (6.1) | 4 (6.2) | 0.989 |
| Physical activity, n (%) | 332 (78.1) | 281 (78.1) | 51 (78.5) | 0.942 |
| Family history of ASCVD, n (%) | 187 (44.0) | 150 (41.7) | 37 (56.9) | 0.023 |
| Central obesity, n (%) | 311 (73.2) | 257 (71.4) | 54 (83.1) | 0.050 |
| General obesity | 0.890 | |||
| Overweight, n (%) | 191 (44.9) | 162 (45.0) | 29 (44.6) | |
| Obesity, n (%) | 132 (31.1) | 113 (31.4) | 19 (29.2) | |
| Duration of DM (years) | 10.39 ± 3.24 | 10.34 ± 3.16 | 10.69 ± 3.70 | 0.416 |
| FPG (mmol/l) | 8.61 ± 2.64 | 8.50 ± 2.58 | 9.22 ± 2.95 | 0.042 |
| HbA1c (%) | 7.36 ± 1.75 | 7.25 ± 1.68 | 7.94 ± 2.04 | 0.004 |
| Hypertension, n (%) | 328 (77.2) | 275 (76.4) | 53 (81.5) | 0.363 |
| SBP (mmHg) | 150.56 ± 20.17 | 150.30 ± 20.20 | 152.06 ± 20.11 | 0.518 |
| DBP (mmHg) | 87.16 ± 11.19 | 87.37 ± 11.25 | 85.98 ± 10.86 | 0.360 |
| TC (mmol/l) | 5.37 ± 1.14 | 5.37 ± 1.13 | 5.37 ± 1.19 | 0.977 |
| TG (mmol/l) | 2.31 ± 1.96 | 2.33 ± 2.05 | 2.19 ± 1.36 | 0.588 |
| LDL-C (mmol/l) | 2.71 ± 0.54 | 2.71 ± 0.53 | 2.73 ± 0.59 | 0.802 |
| HDL-C (mmol/l) | 1.45 ± 0.29 | 1.45 ± 0.29 | 1.47 ± 0.32 | 0.589 |
| eGFR (ml/min/1.73 m2) | 92.42 ± 17.68 | 93.31 ± 17.73 | 87.53 ± 16.69 | 0.015 |
Data are means ± SE or raw numbers (%). Continuous data were used for univariate general linear models and categorical data were analyzed by χ2 tests.
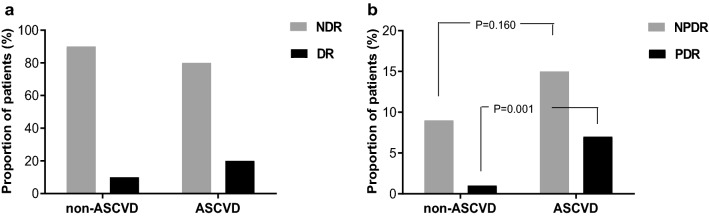
Of the 360 subjects without ASCVD, 35 (9.7%) had DR. However, 13 cases (20.0%) were registered in the ASCVD group of 65 subjects, showing that the trend to DR in ASCVD group was significantly higher than in non-ASCVD group (Pearson χ2 = 5.805, P = 0.016), as is illustrated in Fig. 1a. Furthermore, when DR was divided into NPDR and PDR based on its severity, a higher proportion of subjects with NPDR (9, 13.8%) and PDR (4, 6.2%) were found in the ASCVD group than from non-ASCVD group [32 subjects (9.0%) with NPDR (Pearson χ2 = 1.975, P = 0.160) and 3 subjects (0.9%) with PDR (Pearson χ2 = 10.368, P = 0.001)], and the difference of prevalence of PDR in two groups was statistically significant (Fig. 1b).
Fig. 1.
The association of ASCVD with DR or different degree of DR. a Comparison of prevalence of DR between ASCVD and non-ASCVD group. The trend to DR in the ASCVD group was significantly higher than in the non-ASCVD group (Pearson χ2 = 5.805, P = 0.016). b Prevalence (%) of patients with different degrees of DR (NPDR and PDR) in relation to ASCVD. When DR was divided into NPDR and PDR according to its severity, the prevalence of NPDR between ASCVD and non-ASCVD group had no statistical difference (Pearson χ2 = 1.975, P = 0.160). However, a higher proportion of subjects with PDR were found in the ASCVD group than from non-ASCVD group (Pearson χ2 = 10.368, P = 0.001)
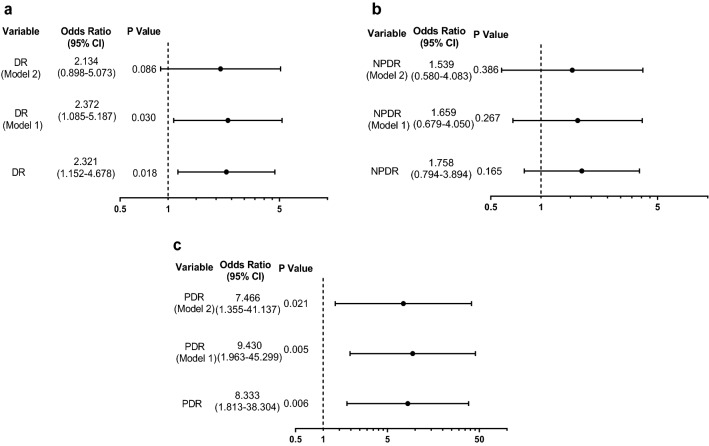
Logistic regression analysis was performed to identify the risk factors of ASCVD. Age [odds ratio (OR) (95% CI): 1.814 (1.257–2.616), P = 0.001], female sex [OR (95% CI): 1.971 (1.091–3.562), P = 0.025], family history of ASCVD [OR (95% CI): 1.850 (1.085–3.155), P = 0.024] and HbA1c [OR (95% CI): 1.198 (1.050–1.368), P = 0.007] were relative risk factors and alcohol [OR (95% CI): 0.440 (0.222–0.872), P = 0.019], eGFR [OR (95% CI): 0.990 (0.827–0.980), P = 0.015] was relative protection factors of ASCVD (Table 2). Next, we found that DR [OR (95% CI): 2.321 (1.152–4.678), P = 0.018] was significantly associated with ASCVD, and such a link was only true for PDR [OR (95% CI): 8.333 (1.813–38.304), P = 0.006] when DR was divided into NPDR and PDR. With an adjustment for age, sex, family history of ASCVD and duration of DM, PDR was significantly associated with and an independent risk factor for ASCVD [OR (95% CI): 9.430 (1.963–45.299), P = 0.005]. Moreover, the association was not affected by an additional adjustment for smoking, alcohol, educational level, physical activity, obesity (central or general obesity), history of hypertension, SBP, DBP, HbA1c, LDL-C and eGFR [OR (95% CI): 7.466 (1.355–41.137), P = 0.021] (Fig. 2).
Table 2.
Odds ratios of metabolic factors for ASCVD
| B | SE | Wald | OR | 95% CI | P value | |
|---|---|---|---|---|---|---|
| Age (per 10 years) | 0.595 | 0.187 | 10.141 | 1.814 | 1.257–2.616 | 0.001 |
| Sex (f/m) | 0.679 | 0.302 | 5.053 | 1.971 | 1.091–3.562 | 0.025 |
| Smoking (y/n) | − 0.649 | 0.351 | 3.423 | 0.522 | 0.263–1.039 | 0.064 |
| Alcohol (y/n) | − 0.822 | 0.350 | 5.526 | 0.440 | 0.222–0.872 | 0.019 |
| High education (y/n) | 0.007 | 0.561 | 0.000 | 1.007 | 0.335–3.026 | 0.989 |
| Physical activity (y/n) | 0.024 | 0.327 | 0.005 | 1.024 | 0.539–1.946 | 0.942 |
| Family history of ASCVD (y/n) | 0.615 | 0.272 | 5.103 | 1.850 | 1.085–3.155 | 0.024 |
| Central obesity (y/n) | 0.677 | 0.351 | 3.723 | 1.967 | 0.989–3.913 | 0.054 |
| General obesity | ||||||
| Overweight (y/n) | − 0.111 | 0.334 | 0.110 | 0.895 | 0.466–1.721 | 0.740 |
| Obesity (y/n) | − 0.174 | 0.363 | 0.228 | 0.841 | 0.412–1.714 | 0.633 |
| Duration of DM (y/n) | 0.031 | 0.039 | 0.661 | 1.032 | 0.957–1.113 | 0.416 |
| FPG (per 1 mmol/l) | 0.158 | 0.090 | 3.068 | 1.171 | 0.981–1.396 | 0.080 |
| HbA1c (per 1 %) | 0.181 | 0.068 | 7.174 | 1.198 | 1.050–1.368 | 0.007 |
| Hypertension (y/n) | 0.311 | 0.343 | 0.824 | 1.365 | 0.697–2.674 | 0.364 |
| SBP (per 10 mmHg) | 0.051 | 0.066 | 0.597 | 1.052 | 0.925–1.197 | 0.440 |
| DBP (per 5 mmHg) | − 0.037 | 0.060 | 0.368 | 0.964 | 0.857–1.085 | 0.544 |
| TC (≥ 4.68 mmol/l) | − 0.080 | 0.302 | 0.071 | 0.923 | 0.510–1.668 | 0.790 |
| TG (≥ 1.70 mmol/l) | − 0.029 | 0.274 | 0.011 | 0.971 | 0.568–1.660 | 0.915 |
| LDL-C (≥ 2.60 mmol/l) | 0.622 | 0.362 | 2.959 | 1.864 | 0.917–3.788 | 0.085 |
| HDL-C (m ≤ 1.00 mmol/l; f ≤ 1.30 mmol/l) | 0.217 | 0.323 | 0.453 | 1.243 | 0.660–2.341 | 0.501 |
| eGFR (per 10 ml/min/1.73 m2) | − 0.105 | 0.043 | 5.910 | 0.900 | 0.827–0.980 | 0.015 |
Binary univariate logistic regression was conducted to assess the association of ASCVD with different variables using the Entry method; odds ratios (ORs) and the 95% confidence intervals (CIs) given
Fig. 2.
Odds ratios for ASCVD with/without DR and different degree of DR. Binary logistic regression was conducted to assess the association of ASCVD with DR (a) and different degrees of DR: NPDR (b) and PDR (c) using the Entry method; adjusted odds ratios (ORs) and the 95% confidence intervals (CIs) given. Adjustment variables included the basic confounders (age, sex, family history of ASCVD and duration of DM) in Model 1. In Model 2, smoking, alcohol, educational level, physical activity, obesity (central or general obesity), history of hypertension, SBP, DBP, HbA1c, LDL-C and eGFR were also considered other adjustment variables and were thus added to Model 1
Discussion
In this study, the prevalence of ASCVD was 15.29% in T2DM patients. Age, female sex, the family history of ASCVD and hyperglycemia were risk factors of ASCVD, similar to previous research results. Coexisting diseases with T2DM, such as hypertension and hyperlipidemia are defined ASCVD risk factors, while DM itself is considered a CAD risk equivalent. ASCVD is the main cause of morbidity and mortality in diabetic patients, contributing to the biggest burden of DM directly or indirectly. The 2007–2008 China National Diabetes and Metabolic Disorders Study reported that the defined total of ASCVD prevalence was 1.44%, including 0.83% of stroke and 0.63% of CHD in Chinese adults over 20 years of age [25]. The Da Qing impaired glucose tolerance (IGT) and Diabetes Study found that the leading cause of death for patients with diabetes is ASCVD after a 23-year follow-up study [26].
It is of great importance for ASCVD to be accurately detected and timely intervened. Due to the fact that the sensory nerve becomes insensitive and even lost in patients with diabetes, symptoms of ASCVD become asymptomatic or atypical. A number of cardiovascular risk assessment tools proposed to assess the risk of developing ASCVD are available, such as Framingham risk score (FRS), Adult Treatment Panel III (ATP-III), EURO—the Systematic Coronary Risk Evaluation (SCORE), Reynolds risk score (RRS), QRISK2 and the Chinese ten-year appraisal method for ischemic cardiovascular disease (ICVD). However, the suitability of these screening assessment tools are limited due to great disparities in terms of ethnicity, geography, environment and lifestyle of patients. Moreover, computed tomography (CT) and angiography can detect the evidence of stenosis or occlusion of vasculars directly, but such clinical applications can result in radiation exposure and sometimes unnecessary invasive diagnosis and treatment. Therefore, it is necessary to look for simple and non-invasive approaches to identify ASCVD early in clinical practices.
In spite of growing controversy, more evidence has revealed a predictive value of microvascular diseases in T2DM on developing ASCVD. In other words, micro- and macrovascular complications of T2DM have a “common soil”. Since the Framingham Heart Study and the Framingham Eye Study had identified the association between DR and the occurrence of cardiovascular events, the importance of DR beyond visual damage was gradually realized by doctors, researchers and the general public. The Atherosclerosis Risk in Communities (ARIC) study also found that DR was associated with an increased risk of ischemic stroke [hazard ratio (HR), 2.34; 95% confidence interval (CI), 1.13 to 4.86] over a follow-up period of 7.8 years on average in middle-aged diabetic patients, independent of other risk factors [14]. Another ARIC study [27] showed that after controlling for traditional cardiovascular risk factors, participants with retinopathy were 2.5 times as likely to develop heart failure (HF) as those without the condition (HR 2.71; 95% CI 1.46 to 5.05). Significant association still existed following further adjustments for glycemic control, carotid atherosclerosis, and serum markers of endothelial dysfunction (HR 2.20, 95% CI 1.08 to 4.47). A recent meta-analysis showed that patients with DR were more liable to develop stroke [risk ratio (RR), 1.74; 95% CI 1.35 to 2.24], compared with those without. Furthermore, DR was associated with an increased risk of HF in patients with DM (RR 2.24; 95% CI 0.98 to 5.14), although marginally [15]. Retinopathy proved to be an independent risk marker for CVD in patients with T2DM [28].
However, there is insufficient evidence showing whether this association can be confirmed from consistent observation in Asian people, especially in Chinese. There exist differences in the epidemiologic and risk associations of ASCVD between white and Asian populations. For this reason, an ethnicity-specific risk model of ASCVD is potentially needed. Furthermore, it is still debatable whether each stage of DR is associated with increased risk of ASCVD. A Finnish report suggested that during a follow-up study lasting seven years, the risk of CHD events was significantly higher than patients without DR, but only in those with PDR at baseline (OR 2.31, 95% CI 1.21 to 4.40) [29]. However, the Japan Diabetes Complications Study (JDCS) [30] which consisted of 2033 patients with T2DM confirmed that the presence of DR was continuously associated with an increased risk of stroke and CHD based on 8 years of follow-up. Additionally, even mild to moderate NPDR triggered a higher risk of CHD (HR 1.69; 95% CI 1.17–2.97) and stroke (HR 2.69; 95% CI 1.03–4.86) after adjusting for traditional cardiovascular risk factors. In our research, those T2DM patients with an eGFR < 60 ml/min/1.73 m2 were excluded specifically to avoid the confounding factor of renal insufficiency, which was associated with an increased risk of atherosclerosis. We found that the presence of DR was significantly associated with an increased risk of ASCVD in Chinese with T2DM. Furthermore, the incidence of ASCVD increased along with the severity of DR. After adjustment for age, sex and other traditional risk factors, PDR rather than NPDR was significantly associated with and an independent risk factor for ASCVD. In the presence of PDR, risk of ASCVD was sevenfold in T2DM patients and PDR offered risk information beyond that provided by those established risk factors.
DR is closely related to ASCVD in epidemiology, and similar pathophysiological processes may also contribute to DR and diabetes-accelerated atherosclerosis. To elaborate, traditional risk factors for ASCVD, such as hypertension, hyperlipidemia, duration of hyperglycemia, magnitude of glycemic control and metabolic syndrome (MetS) are well-known for the progression and development of DR [7, 31]. Secondly, neovascularization (retinal angiogenesis) is a typical characteristic of PDR, while angiogenesis is also a common feature observed in advanced atherosclerotic lesions [32, 33]. Early pathological changes of macro- and microvascular have similarities, and chances are microcirculation change can quicken macrovascular lesions. In addition, increasing evidence indicates that unifying mechanisms play a major role in the pathogenesis of diabetic macrovascular, as well as microvascular, complications [34]. These mechanisms include hexosamine pathway, activation of protein kinase C, oxidative stress, pathological effects of the renin–angiotensin–aldosterone system (RAAS), advanced glycation end product (AGE) formation, inflammation and modification of circulating macromolecules, etc., which may influence not only the development of DR, but also the progress of atherosclerosis [35].
As mentioned above, we have elaborated on the usefulness of a simple and non-invasive evaluation of the ASCVD risk in diabetic patients through the research of DR. However, thanks to recent deployment and development of digital technologies, telemedicine has been increasingly applied in many clinical areas such as cardiovascular diseases and diabetes, alongside all its chronic complications, thus assuming an important role as a tool for a diagnosis of DR even at a great distance from doctors or specialist centers [36, 37].
Our study has several limitations that must be taken into account. First of all, it may have unpredictable selection bias. Secondly, ASCVD patients in this article are confirmed cases by hospitals, which means that some potential ASCVD patients may be missed. This might lead to an underestimation of the prevalence of ASCVD in T2DM patients. Thirdly, as these associations are cross-sectional, the study design is incapable of estimating a causal relationship directly; therefore, our findings may suggest that PDR is an indicator, but not predictor of ASCVD. Furthermore, participants are small in number for a cross-sectional study. The adverse effects of DR on ASCVD in Chinese population should be confirmed further in a larger cohort study with a broader spectrum of potential confounding factors. However, we have no reasons to believe these would substantially bias the associations reported herein.
In conclusion, all our data confirm that DR associates strongly with ASCVD in the Chinese population with T2DM. With the severity of DR increasing, the risk of ASCVD also increases. After adjustment for traditional risk factors, PDR is an independent risk marker for ASCVD. Retinal blood vessel is the only microvasculature that can be directly observed, and it would definitely be intriguing to assess whether the retinal microvasculature can be used as a ‘window’ into the state of the cardiovascular complications in patients with diabetes. DR is not only one of the most common microvascular complications of diabetes, but also a “warning sign” for ASCVD. Based on these research findings, we hope that clinicians pay more attention to systemic vascular risk of the patients with DR, especially PDR, and suggest incorporating PDR to clinical cardiovascular risk stratification in patients with diabetes.
Acknowledgements
Not applicable.
Abbreviations
- ASCVD
Atherosclerosis cardiovascular disease
- DR
Diabetic retinopathy
- NDR
No DR
- NPDR
Non-proliferative diabetic retinopathy
- PDR
Proliferative diabetic retinopathy
- DM
Diabetes mellitus
- BMI
Body mass index
- WC
Waist circumference
- FPG
Fasting plasma glucose
- HbA1c
Glycated haemoglobin
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- TC
Total cholesterol
- TG
Triglycerides
- HDL-C
High-density lipoprotein
- LDL-C
Low-density lipoprotein cholesterol
- eGFR
Calculated glomerular filtration rate
- OR
Odds ratio
- CI
Confidence interval
Authors’ contributions
LG designed the experiments, collected and analyzed the data before writing the manuscript. WZ did the experiments, and was a contributor in collecting data. JKY and MZQ also helped design the study and revise the manuscript. All authors read and approved the final manuscript.
Funding
There is no funding for this study.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
The study was conducted with the approval from the Ethics Committee of Beijing Tongren Hospital, Capital Medical University, and adhered to the tenets of the Declaration of Helsinki. Written consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen XD, Gardner TW. A critical review: psychophysical assessments of diabetic retinopathy. Surv Ophthalmol. 2020 doi: 10.1016/j.survophthal.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):143–52. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 4.Conaway DG, O'Keefe JH, Reid KJ, Spertus J. Frequency of undiagnosed diabetes mellitus in patients with acute coronary syndrome. Am J Cardiol. 2005;96(3):363–5. doi: 10.1016/j.amjcard.2005.03.076. [DOI] [PubMed] [Google Scholar]
- 5.Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. 2018;34(5):575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Keefe JH, Carter MD, Lavie CJ. Primary and secondary prevention of cardiovascular diseases: a practical evidence-based approach. Mayo Clin Proc. 2009;84(8):741–57. doi: 10.1016/s0025-6196(11)60525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pradeepa R, Surendar J, Indulekha K, Chella S, Anjana RM, Mohan V. Relationship of diabetic retinopathy with coronary artery disease in Asian Indians with type 2 diabetes: the Chennai Urban Rural Epidemiology Study (CURES) Eye Study—3. Diabetes Technol Ther. 2015;17(2):112–8. doi: 10.1089/dia.2014.0141. [DOI] [PubMed] [Google Scholar]
- 8.Marfella R, Ferraraccio F, Rizzo MR, Portoghese M, Barbieri M, Basilio C, et al. Innate immune activity in plaque of patients with untreated and l-thyroxine-treated subclinical hypothyroidism. J Clin Endocrinol Metab. 2011;96(4):1015–20. doi: 10.1210/jc.2010-1382. [DOI] [PubMed] [Google Scholar]
- 9.Marfella R, D’Amico M, Di Filippo C, Siniscalchi M, Sasso FC, Ferraraccio F, et al. The possible role of the ubiquitin proteasome system in the development of atherosclerosis in diabetes. Cardiovasc Diabetol. 2007;6:35. doi: 10.1186/1475-2840-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sasso FC, Pafundi PC, Marfella R, Calabrò P, Piscione F, Furbatto F, et al. Adiponectin and insulin resistance are related to restenosis and overall new PCI in subjects with normal glucose tolerance: the prospective AIRE study. Cardiovasc Diabetol. 2019;18(1):24. doi: 10.1186/s12933-019-0826-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marfella R, Sasso FC, Siniscalchi M, Paolisso P, Rizzo MR, Ferraro F, et al. Peri-procedural tight glycemic control during early percutaneous coronary intervention is associated with a lower rate of in-stent restenosis in patients with acute ST-elevation myocardial infarction. J Clin Endocrinol Metab. 2012;97(8):2862–71. doi: 10.1210/jc.2012-1364. [DOI] [PubMed] [Google Scholar]
- 12.Torella D, Ellison GM, Torella M, Vicinanza C, Aquila I, Iaconetti C, et al. Carbonic anhydrase activation is associated with worsened pathological remodeling in human ischemic diabetic cardiomyopathy. J Am Heart Assoc. 2014;3(2):e000434. doi: 10.1161/jaha.113.000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cozzolino D, Sessa G, Salvatore T, Sasso FC, Giugliano D, Lefebvre PJ, et al. The involvement of the opioid system in human obesity: a study in normal weight relatives of obese people. J Clin Endocrinol Metab. 1996;81(2):713–8. doi: 10.1210/jcem.81.2.8636293. [DOI] [PubMed] [Google Scholar]
- 14.Cheung N, Rogers S, Couper DJ, Klein R, Sharrett AR, Wong TY. Is diabetic retinopathy an independent risk factor for ischemic stroke? Stroke. 2007;38(2):398–401. doi: 10.1161/01.str.0000254547.91276.50. [DOI] [PubMed] [Google Scholar]
- 15.Zhu XR, Zhang YP, Bai L, Zhang XL, Zhou JB, Yang JK. Prediction of risk of diabetic retinopathy for all-cause mortality, stroke and heart failure: evidence from epidemiological observational studies. Medicine. 2017;96(3):e5894. doi: 10.1097/md.0000000000005894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Um T, Lee DH, Kang JW, Kim EY, Yoon YH. The degree of diabetic retinopathy in patients with type 2 diabetes correlates with the presence and severity of coronary heart disease. J Korean Med Sci. 2016;31(8):1292–9. doi: 10.3346/jkms.2016.31.8.1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Targher G, Bertolini L, Zenari L, Lippi G, Pichiri I, Zoppini G, et al. Diabetic retinopathy is associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabet Med. 2008;25(1):45–50. doi: 10.1111/j.1464-5491.2007.02327.x. [DOI] [PubMed] [Google Scholar]
- 18.Juutilainen A, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Retinopathy predicts cardiovascular mortality in type 2 diabetic men and women. Diabetes Care. 2007;30(2):292–9. doi: 10.2337/dc06-1747. [DOI] [PubMed] [Google Scholar]
- 19.Targher G, Bertolini L, Tessari R, Zenari L, Arcaro G. Retinopathy predicts future cardiovascular events among type 2 diabetic patients: the Valpolicella Heart Diabetes Study. Diabetes Care. 2006;29(5):1178. doi: 10.2337/diacare.2951178. [DOI] [PubMed] [Google Scholar]
- 20.Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–44. doi: 10.1681/asn.2006040368. [DOI] [PubMed] [Google Scholar]
- 21.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 22.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–45. doi: 10.1161/circulationaha.109.192644. [DOI] [PubMed] [Google Scholar]
- 23.Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96. [PubMed] [Google Scholar]
- 24.Wilkinson CP, Ferris FL, 3rd, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677–82. doi: 10.1016/s0161-6420(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 25.Yang ZJ, Liu J, Ge JP, Chen L, Zhao ZG, Yang WY. Prevalence of cardiovascular disease risk factor in the Chinese population: the 2007–2008 China National Diabetes and Metabolic Disorders Study. Eur Heart J. 2012;33(2):213–20. doi: 10.1093/eurheartj/ehr205. [DOI] [PubMed] [Google Scholar]
- 26.An Y, Zhang P, Wang J, Gong Q, Gregg EW, Yang W, et al. Cardiovascular and all-cause mortality over a 23-year period among Chinese with newly diagnosed diabetes in the Da Qing IGT and diabetes study. Diabetes Care. 2015;38(7):1365–71. doi: 10.2337/dc14-2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheung N, Wang JJ, Rogers SL, Brancati F, Klein R, Sharrett AR, et al. Diabetic retinopathy and risk of heart failure. J Am Coll Cardiol. 2008;51(16):1573–8. doi: 10.1016/j.jacc.2007.11.076. [DOI] [PubMed] [Google Scholar]
- 28.Gimeno-Orna JA, Faure-Nogueras E, Castro-Alonso FJ, Boned-Juliani B. Ability of retinopathy to predict cardiovascular disease in patients with type 2 diabetes mellitus. Am J Cardiol. 2009;103(10):1364–7. doi: 10.1016/j.amjcard.2009.01.345. [DOI] [PubMed] [Google Scholar]
- 29.Miettinen H, Haffner SM, Lehto S, Rönnemaa T, Pyörälà K, Laakso M. Retinopathy predicts coronary heart disease events in NIDDM patients. Diabetes Care. 1996;19(12):1445–8. doi: 10.2337/diacare.19.12.1445. [DOI] [PubMed] [Google Scholar]
- 30.Kawasaki R, Tanaka S, Tanaka S, Abe S, Sone H, Yokote K, et al. Risk of cardiovascular diseases is increased even with mild diabetic retinopathy: the Japan Diabetes Complications Study. Ophthalmology. 2013;120(3):574–82. doi: 10.1016/j.ophtha.2012.08.029. [DOI] [PubMed] [Google Scholar]
- 31.Gao L, Xin Z, Yuan MX, Cao X, Feng JP, Shi J, et al. High Prevalence of diabetic retinopathy in diabetic patients concomitant with metabolic syndrome. PLoS ONE. 2016;11(1):e0145293. doi: 10.1371/journal.pone.0145293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moreno PR, Purushothaman KR, Zias E, Sanz J, Fuster V. Neovascularization in human atherosclerosis. Curr Mol Med. 2006;6(5):457–77. doi: 10.2174/156652406778018635. [DOI] [PubMed] [Google Scholar]
- 33.Simo R, Carrasco E, Garcia-Ramirez M, Hernandez C. Angiogenic and antiangiogenic factors in proliferative diabetic retinopathy. Curr Diabetes Rev. 2006;2(1):71–98. doi: 10.2174/157339906775473671. [DOI] [PubMed] [Google Scholar]
- 34.Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615–25. doi: 10.2337/diabetes.54.6.1615. [DOI] [PubMed] [Google Scholar]
- 35.Ellis TP, Choudhury RH, Kaul K, Chopra M, Kohner EM, Tarr JM, et al. Diabetic retinopathy and atherosclerosis: is there a link? Curr Diabetes Rev. 2013;9(2):146–60. doi: 10.2174/1573399811309020006. [DOI] [PubMed] [Google Scholar]
- 36.Galiero R, Pafundi PC, Nevola R, Rinaldi L, Acierno C, Caturano A, et al. The importance of telemedicine during COVID-19 pandemic: a focus on diabetic retinopathy. J Diabetes Res. 2020;2020:9036847. doi: 10.1155/2020/9036847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sasso FC, Pafundi PC, Gelso A, Bono V, Costagliola C, Marfella R, et al. Telemedicine for screening diabetic retinopathy: the NO BLIND Italian multicenter study. Diabetes Metab Res Rev. 2019;35(3):e3113. doi: 10.1002/dmrr.3113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.