Abstract
Introduction
Between early March 2020 and the end of May 2020, Italy issued strict measures to limit further spread of coronavirus disease 2019 (COVID-19) and became the first European country that imposed a lockdown on the population. The aim of this study was to assess the impact of these restricted conditions on the activity of the Poison Control Center (PCC) of Policlinico Umberto I Hospital-Sapienza University of Rome.
Methods
This was a retrospective analysis of calls received by the PCC during the lockdown period March 9, 2020 through May 31, 2020 compared to the same time period in year 2019 (reference).
Results
We observed a reduction in calls from hospitals and emergency departments and an increase in calls from private citizens about exposures to products or intoxications during the lockdown. There were increases in unintentional exposures and exposures to hand and surface sanitizers among household and cleaning products. There was a decrease in calls concerning medications, which were mostly from hospitals and emergency departments. We observed increases in exposures requiring clinical observations among adults and referral to the emergency department among pre-school children.
Conclusions
Public health protection measures against COVID-19 to improve hygiene and maintain clean environments can increase exposures to hazardous products in the domestic environment. We observed an increase in unintentional exposures to household and cleaning products during the lockdown and an increase in ED referrals for pre-school children compared to the previous year. Our data suggest the need for improvements in public campaigns that promote safer handling of household products and prevent unnecessary exposures during a lockdown. The public health promotion activity can benefit the community after the pandemic and prepare the community for lockdowns in the future.
Keywords: Lockdown, Poison Control Center, Toxic exposures, Household products, COVID-19
Introduction
In early 2020, Italy became the first epicenter for the coronavirus disease 2019 (COVID-19) in Europe. The enormous pressure on the national healthcare system during the quickly escalating COVID-19 outbreak has prompted authorities to implement radical emergency measures. A so-called lockdown was first imposed exclusively in northern regions, where the outbreak started, and then extended to the whole country on March 10th [1]. To promote physical distancing, gatherings in public and open places were forbidden, and the population encouraged to stay home. Schools and retailers were closed, with the exception of pharmacies and basic needs stores. Tele-working and online learning for students were arranged where feasible. A further restriction on travelling outside the current municipality was also applied later on. By May 18th, these strict containment measures were gradually loosened, and travelling across regions was again permitted starting June 3rd. To slow the transmission of COVID-19, the Italian Health Department recommended good personal hygiene through the use of alcohol-based hand sanitizers and chlorine disinfectant solutions for disinfection of surfaces.
Several articles have pointed out peculiar intoxication trends or changes in patterns of healthcare use during the COVID-19 emergency [2–5]. Indeed, the limitations and physical distancing have confined people in the home environment and exposed to a variety of potential threats to safety. Alarming news on television and the social media can contribute to engage in unsafe or erroneous domestic behaviors (e.g., overuse or improper storage of household and cleaning products and mixing of chemical agents). In addition to the above items, there is the potential effect on hospital admissions by the new priorities at the emergency department (ED) and the concerns for excessive wait time and increased risk for contracting COVID-19 by people seeking care [6, 7].
The emergency network in Lazio region is organized in structures by levels of complexity and articulated in catchment areas, each with a level II ED as a reference for level I EDs and first aid points. The Poison Control Center (PCC) of Policlinico Umberto I Hospital-Sapienza University of Rome (a level II ED hub) mainly operates at the regional level, with 70% of calls from the city of Rome and the Lazio region. It serves, along with two other independent PCCs, a population of approximately 6 million people, including about 300,000 pre-school children and 1.2 million aged 65 years or older. Penetrance of this PCC is on average 0.4/1000 residents per year. During the lockdown period, the PCC has not modified its operating protocol.
The aim of this study is to assess the impact of the lockdown on the activity of the PCC. We will provide a descriptive analysis of the calls received during the lockdown period compared to the same time period in the previous year.
Methods
Data were extracted from the database of the PCC and analyzed retrospectively. Each telephone call was managed complying with the internal operating procedures and using a standard data collection form. The primary objective of the study was to compare the characteristics of calls received in the period March 9th–May 31st of year 2020 (lockdown) and the same time period in year 2019 (reference). Secondary objective was to compare the management of the calls between the two periods of interest. The following variables were considered: (i) age group, (ii) caller site (private citizens [PV] or from Hospitals/ED [H/ED]), (iii) type of call (information request or actual exposures, which included intoxications), (iv) agent category, (v) reason for exposure, (vi) site of exposure, (vii) route of exposure, and (viii) PCC recommended management. A medical toxicologist reviewed the data for consistency and for errors in categorization. The inter-rater reliability score, assessed with the Cohen’s kappa statistic, was 0.85 for the variables considered. For any missing data on age (about 1%), the related archived paper form was retrieved and examined to determine an age group assignment. No cases had missing data on the other variables considered.
Comparative statistical analysis was performed using Pearson chi-square tests for categorical variables. When significant (p < .05), z-tests on relative proportions (percentage of total) with Bonferroni correction were conducted as post-hoc tests. IBM SPSS Statistics version 20 was used for the data analysis. Ninety-five percent confidence intervals (CI) for proportions were calculated with the Clopper–Pearson method.
Subject-identifying information were obscured in the database, therefore not extracted and not available to the investigators. This study was determined to be exempt by the Institutional Review Board at our institution.
Results
Between March 9th and May 31st in 2020, there were a decrease in calls from H/ED (14.0%, 95% CI 11.0–17.4% vs 33.5%, 95% CI 29.6–37.6%; p < .001) and an increase in calls from PV (86.0%, 95% CI 82.5–89.0% vs 66.5%, 95% CI 62.4–70.4%) compared to 2019 (Fig. 1). Analysis on type of calls revealed an increase in the proportion of exposures during lockdown (79.3%, 95% CI 75.1–82.7% vs 72.0%, 95% CI 68.1–75.6%) and a reduction in simple information requests.
Fig. 1.
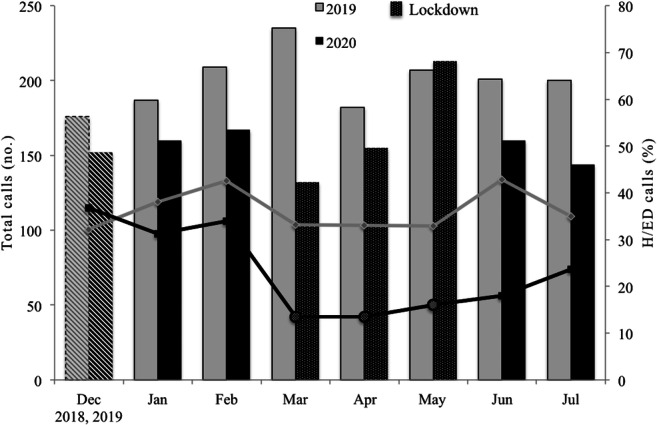
Monthly distribution of total calls and percentage of hospital and emergency department (H/ED) calls received by the PCC from December 2019 to July 2020 and compared to the same period in the previous year. The lockdown period was from March 9, 2020, to May 31, 2020. Total number of calls in the lockdown period was 463 and in the same period in 2019 (reference) was 567
Exposures
During the lockdown, the distribution of calls by agent category was different from the previous year (p < .001) (Table 1). For example, the proportion of calls concerning exposures to medications was lower than those in 2019 (18.7%, 95% CI 14.7–22.9% vs 39.5%, 95% CI 34.7–44.4%). On the contrary, the calls for exposures to household and cleaning products (35.9%, 95% CI 30.9–40.9% vs 26.7%, 95% CI 22.5–31.3%) and to pesticides (6.0%, 95% CI 3.8–9.0% vs 2.2%, 95% CI 1.0–4.1%) were higher than their respective categories in 2019. The total number of calls progressively increased by month during the lockdown, while the proportion of calls by site remained essentially unchanged (Fig. 1 and Table 1). Exposures mainly occurred at home (89.3% vs 85.5%). In the lockdown period, however, unintentional exposure increased (76.4%, 95% CI 71.8–80.8% vs 57.1%, 95% CI 52.1–62.0%; p < .001), while intentional intoxications and administration errors decreased (Table 1).
Table 1.
Characteristics of exposure calls received by the Poison Control Center of Policlinico Umberto I Hospital-Sapienza University of Rome, Italy, in 2020 vs 2019 (9th March–31st May).
| Lockdown (2020) | Reference (2019) | ||
|---|---|---|---|
| n (%) | n (%) | p | |
| All cases | 366 | 408 | |
| Caller site | < .001 | ||
| PVa | 308 (84.0)* | 251 (61.5) | |
| H/EDb | 58 (16.0)* | 157 (38.5) | |
| Age group (years) | .363 | ||
| ≤ 6 | 112 (30.7) | 121 (29.7) | |
| 7–18 | 21 (5.5) | 32 (7.8) | |
| ≥ 19 | 233 (63.8) | 255 (62.5) | |
| Site of exposure | .287 | ||
| Home | 327 (89.3) | 349 (85.5) | |
| Public and open spaces | 25 (6.9) | 37 (9.1) | |
| Workplace and community | 14 (3.8) | 22 (5.4) | |
| Agent category | < .001 | ||
| Medications | 68 (18.7)* | 161 (39.5) | |
| Household and cleaning products | 131 (35.9)* | 109 (26.7) | |
| Pesticides | 22 (6.0)* | 9 (2.2) | |
| Solvents and fuels | 20 (5.4) | 24 (5.9) | |
| Substances of abuse | 4 (1.1) | 4 (1.0) | |
| Food | 14 (3.8) | 19 (4.7) | |
| Mushrooms and plants | 13 (3.7) | 10 (2.4) | |
| Animal bites and stings | 30 (8.1) | 23 (5.6) | |
| HMPc and CAMd | 15 (4.1) | 9 (2.2) | |
| Other toxic products | 15 (4.0) | 11 (2.7) | |
| Non-toxic products | 34 (9.2) | 29 (7.1) | |
| Reason of exposure | < .001 | ||
| Unintentional | 280 (76.4)* | 233 (57.1) | |
| Intentional | 39 (10.7)* | 74 (18.1) | |
| Adverse reactions | 3 (0.8) | 8 (2.0) | |
| Administration error | 42 (11.5)* | 87 (21.3) | |
| Unknown | 2 (0.6) | 6 (1.5) | |
| Route of exposure | .185 | ||
| Ingestion | 228 (62.3) | 291 (71.3) | |
| Inhalation | 50 (13.7) | 39 (9.6) | |
| Inoculation | 14 (3.8) | 14 (3.4) | |
| Bites | 19 (5.2) | 10 (2.5) | |
| Dermal | 18 (4.9) | 16 (3.9) | |
| Oral mucosa | 22 (6.0) | 22 (5.4) | |
| Ocular | 12 (3.3) | 9 (2.2) | |
| Other and unknown | 3 (0.8) | 7 (1.7) |
*z-test with Bonferroni correction (p < .05)
aPV private citizens
bH/ED hospitals and emergency department
cHMP herbal medicinal products
dCAM complementary and alternative medicine
During the lockdown, 86.3% of all household and cleaning products exposures were unintentional (86.2% in 2019) and mainly involved adults (65.6% vs 59.6%) rather than children ≤ 6 years old (30.5% vs 34.9%). Although home monitoring was usually recommended by the PCC for calls from PVs, there was a trend for increased referral to the ED for pre-school children (≤ 6 years old) during the lockdown compared to the prior year (26.5%, 95% CI 12.9–44.4% vs 15.8%, 95% CI 3.4–39.6) (Table 2). Among the children sent to the ED, most of them were exposed by ingestion (66.7%). Sodium hypochlorite containing products (19%), acid cleaners and degreasers (18%), and hand and surface sanitizers (without sodium hypochlorite) (18%) were common exposures for household and cleaning products, and there was an increase in calls for the latter item from 2019 (6.3%).
Table 2.
Management of exposure cases by age group in the lockdown period (March 9, 2020, to May 31, 2020) vs the reference period (March 9, 2019, to May 31, 2019).
| Total exposures | ≤6 years | 7–18 years | ≥ 19 years | |||||
|---|---|---|---|---|---|---|---|---|
| Lockdown | Reference | Lockdown | Reference | Lockdown | Reference | Lockdown | Reference | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| All cases | 366 | 408 | 112 | 121 | 21 | 32 | 233 | 255 |
| Management | ||||||||
| None | 118 (32.1)* | 164 (40.2) | 43 (38.4) | 58 (47.9) | 7 (30.0) | 12 (37.5) | 68 (29.2) | 94 (36.9) |
| Home monitoring and clinical observationa | 174 (47.7)* | 143 (35.0) | 51 (45.5) | 48 (39.7) | 11 (55.0) | 10 (31.2) | 112 (48.1)* | 85 (33.3) |
| Referral to a specialistb | 11 (3.0)* | 27 (6.6) | 2 (1.8) | 3 (2.5) | 1 (5.0) | 5 (15.6) | 8 (3.4) | 19 (7.5) |
| Referral to EDc | 40 (11.0) | 31 (7.6) | 13 (11.6)* | 3 (2.5) | 2 (10.0) | 2 (6.3) | 25 (10.7) | 26 (10.2) |
| Other | 23 (6.2) | 43 (10.6) | 3 (2.8) | 9 (7.4) | 0 | 3 (9.4) | 20 (8.6) | 31 (12.1) |
*z-test with Bonferroni correction (p < .05) following Pearson chi-square test (p < .01)
a“Home monitoring” may be suggested for private calls, “clinical observation” for hospital and emergency departments calls
b“Referral to a specialist” may be suggested for (i) private cases requiring a delayed specialist consultation or (ii) cases already admitted to hospital and emergency departments prior to Poison Control Center consultation that require additional specialist evaluation
cED emergency department
Ninety-five percent of exposures to pesticides happened at home during the lockdown, and pyrethroids were commonly involved in these calls (49.6%). All these exposures were unintentional in nature, and ingestion was a common route of exposure (32.1%). There was an increase in home monitoring or clinical observation for these exposures compared to 2019 (52.4% vs 16.1%). No exposure in children ≤ 6 years old required referral to ED.
Among all exposures during the lockdown, there was an increase in referrals to the ED for pre-school children (≤ 6 years old) compared to the prior year (11.6%, 95% CI 6.3–19.0% vs 2.5%, 95% CI 0.5–7.1%; p = .001) (Table 2). In addition, there was an increase in home monitoring or clinical observation for adults (48.1%, 95% CI 41.5–54.7% vs 33.3%, 95% CI 27.6–39.5%).
Information requests
During the lockdown, nearly all information requests were from PV (92.8%), and the distribution of calls by agent category was similar to the calls for exposures (Table 3).
Table 3.
Characteristics of information requests received by the Poison Control Centre of Policlinico Umberto I University Hospital in Rome Italy in 2020 vs 2019 (9th March–31st May).
| Lockdown (2020) | Reference (2019) | ||
|---|---|---|---|
| n (%) | n (%) | p | |
| All cases | 97 | 159 | |
| Caller site | .004 | ||
| PVa | 90 (92.8)* | 126 (79.2) | |
| H/EDb | 7 (7.2)* | 33 (20.8) | |
| Age group (years) | .155 | ||
| ≤ 6 | 5 (5.5) | 13 (8.1) | |
| 7–18 | 0 (0.0) | 7 (4.4) | |
| > 18 | 92 (94.5) | 139 (87.5) | |
| Agent category | .036 | ||
| Medications | 28 (29.2)* | 71 (44.7) | |
| Household and cleaning products | 16 (15.5) | 9 (5.7) | |
| Pesticides | 6 (6.3)* | 1 (0.6) | |
| Solvents and fuels | 2 (2.1) | 2 (1.3) | |
| Substances of abuse | 6 (6.3) | 8 (5.0) | |
| Food | 15 (15.5) | 21 (13.2) | |
| Mushrooms and plants | 0 | 3 (1.9) | |
| Animal bites and stings | 4 (4.2) | 12 (7.5) | |
| HMPc and CAMd | 4 (4.2) | 5 (3.2) | |
| Other toxic products | 7 (7.3) | 14 (8.8) | |
| Non-toxic products | 9 (9.4) | 13 (8.1) |
*z-test with Bonferroni correction (p < .05)
aPV private citizens
bH/ED hospitals and emergency department
cHMP herbal medicinal products
dCAM complementary and alternative medicine
Discussion
There were three main findings in this retrospective analysis. First, during the months of the 2020 lockdown, compared to 2019, there was an important reduction in calls to the PCC from healthcare facilities. Second, among exposures, the most frequent scenario was an unintentional exposure to household and cleaning products. Hand and surface sanitizers were more frequently involved than in the previous year. Third, during lockdown, there was an increase in referral to the ED for pre-scholar children (≤ 6 years old).
The lockdown in Italy set an unprecedented experience for the population. The stringent measures imposed on such a scale, coupled with the global perception of the COVID-19-related health risk, exert a deep impact on people’s habits [8–11]. Among the behaviors possibly affected is the personal use of the healthcare system. In fact, a decline in ED visits by the general population has been reported elsewhere [12, 13]. Also, many large hospitals, including the one where our PCC operates, were re-adapted into facilities to treat COVID-19 patients during the epidemic, which can discourage people from seeking health care for other reasons. In this context, the observed decrease in calls to the PCC from H/ED in this study can be explained. Anyhow, even considering a drop in ED admissions for intoxications, one would have still expected greater requests for information. Indeed, COVID-19 posed new challenges also in the pharmacological management of patients already on medications for one or more underlying pathologies [14, 15]. Clinicians could therefore take advantage of PCCs knowledge and access to specific databases for potential drug–drug interactions and toxicity of new and old medications [16].
On the other hand, this PCC registered more PV calls pertaining to exposures, including intoxications, with respect to 2019 that were more often unintentional and happened in the home environment. Household and cleaning products, including those for personal hygiene (hand sanitizers) and disinfection, were more likely to be involved during lockdown, approximately in more than one-third of the cases. This is consistent with the increase in the number of consultations for cleaning products and disinfectants in North America [3, 17, 18] and Europe [19] in the same period. Misinformation spread by the media on hygiene practices could have played a significant role in this phenomenon [20–22], although we did not specifically evaluate this effect on our data. Also, public knowledge on safe and proper use of sanitizing chemicals has been questioned [23]. It is relevant to note that the restrictive measures applied in Italy to promote physical distancing may have on their own increased the chances of contact with household and cleaning products in the home setting. Misuse (or overuse) of these products could reflect the longer time spent in a confined environment, coupled with public announcements stressing the importance of personal hygiene and disinfection. The initial short supply of sanitizers and disinfectants might have contributed to the above phenomenon. In addition to reasons discussed for household products, pesticides exposures might have increased in the lockdown period as a consequence of living in a closed and confined environment.
In contrast to other reports [3, 17], we did not see an increase in child exposures to household and cleaning products. It should be noticed though that not all countries did enforce containment measures as strict as in Italy. With the shutdown of many activities and tele-working promoted at all levels, adults spent more time at home, possibly extending surveillance over children. Nevertheless, we report an increase in the proportion of exposures among children ≤ 6 years old who were referred to the ED, mostly following household and cleaning product ingestion. In addition, the data suggest that during lockdown, the increased exposure to these products accounted for the increased frequency of cases requiring clinical observation among adults. Because of loss to follow-up, it was not possible to establish if the increased perceived health risk actually corresponded to a more severe clinical course or prognosis.
Because the lockdown measures have a pervasive impact on quality of life, decision-making, and public risk perception [24], further studies are warranted to disentangle the potential effect on PCC activity of the numerous variables involved. The future aims could be to (i) enact information campaigns that may prevent exposures to hazardous products in the household, (ii) educate both PV and healthcare personnel on the importance of PCCs as a source of drug information (including interactions with new drugs or when routine medications are unavailable) and initial treatment advice for potentially toxic exposures, and (iii) reduce the large number of patients arriving to EDs and healthcare facilities during the epidemic. Additionally, PCCs should continue to monitor for any change in the patterns of domestic use of hazardous products among the population in the months post-lockdown and in anticipation of future lockdowns.
To our knowledge, this paper is the first report of PCC data collected in a country that experienced a lockdown during the COVID-19 pandemic. There are some limitations to this report. The data presented here reflects the activity of a PCC at the regional level in Italy and may not be representative of the country. Also, given the small sample size, the findings might be an under representation of the actual situation in the community. Last, incomplete or inaccurate information about signs and symptoms can hinder the analysis and interpretation of the clinical presentation of the cases.
Conclusion
We showed an increase in unintentional exposures to household and cleaning products in the home environment during the lockdown and an increase in ED referrals for pre-school children compared to the previous year. Public health protection measures against COVID-19, such as physical distancing, good personal hygiene, and clean environments, can increase the exposure to hazardous products in the domestic environment. Our data suggest the need for a public campaign that promotes the prevention of exposures to these harmful products during a lockdown. Improving the population’s awareness through the use of preventive strategies will benefit the community after the pandemic and prepare the community for lockdowns in the future.
Sources of Funding
No funding was used for this project.
Author Contribution
All authors contributed to the study conception and design. Data acquisition was performed by Michele Stanislaw Milella, Paolo Boldrini, Gabriella Vivino, and Maria Caterina Grassi. Data analysis was performed by Michele Stanislaw Milella. The first draft of the manuscript was written by Michele Stanislaw Milella, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Declarations
Conflict of Interest
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Presidenza del Consiglio dei Ministri (DPCM). Misure urgenti in materia di contenimento e gestione dell'emergenza epidemiologica da COVID-19. [Urgent measures to contain COVID-19 and to deal with the emergency caused by the COVID-19 epidemiological situation]. Italian. 2020. Available from: http://www.governo.it/it/articolo/firmato-il-dpcm-9-marzo-2020/14276#.
- 2.Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J Pediatr. 2020;226:274–277. doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang A, Schnall AH, Law R, Bronstein AC, Marraffa JM, Spiller HA, Hays HL, Funk AR, Mercurio-Zappala M, Calello DP, Aleguas A, Borys DJ, Boehmer T, Svendsen E. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19—National Poison Data System, United States, January 1, 2020-March 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(16):496–498. doi: 10.15585/mmwr.mm6916e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le Roux G, Sinno-Tellier S, Descatha A. COVID-19: home poisoning throughout the containment period. Lancet Public Health. 2020;5(6):e314. doi: 10.1016/S2468-2667(20)30095-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodda LN, West KL, LeSaint KT. Opioid overdose-related emergency department visits and accidental deaths during the COVID-19 pandemic. J Urban Health. 2020;97:808–813. doi: 10.1007/s11524-020-00486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynn RM, Avis JL, Lenton S, Amin-Chowdhury Z, Ladhani SN. Delayed access to care and late presentations in children during the COVID-19 pandemic: a snapshot survey of 4075 paediatricians in the UK and Ireland. Arch Dis Child. 2020;106:e8. doi: 10.1136/archdischild-2020-319848. [DOI] [PubMed] [Google Scholar]
- 7.Jeffery MM, D'Onofrio G, Paek H, Platts-Mills TF, Soares WE, 3rd, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 States in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020. 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed]
- 9.Jia P, Liu L, Xie X, Yuan C, Chen H, Guo B, Zhou J, Yang S. Changes in dietary patterns among youths in China during COVID-19 epidemic: the COVID-19 Impact on Lifestyle Change Survey (COINLICS) Appetite. 2020;158:105015. doi: 10.1016/j.appet.2020.105015. [DOI] [PubMed] [Google Scholar]
- 10.Motta Zanin G, Gentile E, Parisi A, Spasiano D. A Preliminary evaluation of the public risk perception related to the COVID-19 health emergency in Italy. Int J Environ Res Public Health. 2020;17(9):3024. doi: 10.3390/ijerph17093024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Odone A, Lugo A, Amerio A, Borroni E, Bosetti C, Carreras G, et al. COVID-19 lockdown impact on lifestyle habits of Italian adults. Acta Biomed. 2020;91(9-S):87–89. doi: 10.23750/abm.v91i9-S.10122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV, National Syndromic Surveillance Program Community of Practice Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. National Syndromic Surveillance Program Community of Practice. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonnell T, McAuliffe E, Barrett M, Conlon C, Cummins F, Deasy C, et al. CUPID COVID-19: emergency department attendance by paediatric patients during COVID-19—project protocol. HRB Open Res. 2020. 10.12688/hrbopenres.13066.2. [DOI] [PMC free article] [PubMed]
- 14.Ghasemiyeh P, Mohammadi-Samani S. COVID-19 outbreak: challenges in pharmacotherapy based on pharmacokinetic and pharmacodynamic aspects of drug therapy in patients with moderate to severe infection. Heart Lung. 2020;49(6):763–773. doi: 10.1016/j.hrtlng.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roden DM, Harrington RA, Poppas A, Russo AM. Considerations for drug interactions on QTc interval in exploratory COVID-19 treatment. Heart Rhythm. 2020;17(7):e231–e232. doi: 10.1016/j.hrthm.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neumann NR, Chai PR, Wood DM, Greller HA, Mycyk MB. Medical toxicology and COVID-19: our role in a pandemic. J Med Toxicol. 2020;16(3):245–247. doi: 10.1007/s13181-020-00778-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenman KD, Reilly MJ, Wang L. Calls to a State Poison Center concerning cleaners and disinfectants from the onset of the COVID-19 pandemic through April 2020. Public Health Rep. 2020;136:27–31. doi: 10.1177/0033354920962437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yasseen Iii A, Weiss D, Remer S, Dobbin N, MacNeill M, Bogeljic B, et al. At-a-glance—increases in exposure calls related to selected cleaners and disinfectants at the onset of the COVID-19 pandemic: data from Canadian poison centres. Health Promot Chronic Dis Prev Can. 2020. 10.24095/hpcdp.41.1.03. [DOI] [PMC free article] [PubMed]
- 19.Babić Ž, Turk R, Macan J. Toxicological aspects of increased use of surface and hand disinfectants in Croatia during the COVID-19 pandemic: a preliminary report. Arh Hig Rada Toksikol. 2020;71(3):261–264. doi: 10.2478/aiht-2020-71-3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chary MA, Overbeek DL, Papadimoulis A, Sheroff A, Burns MM. Geospatial correlation between COVID-19 health misinformation and poisoning with household cleaners in the Greater Boston Area. Clin Toxicol (Phila). 2020;59:320–325. doi: 10.1080/15563650.2020.1811297. [DOI] [PubMed] [Google Scholar]
- 21.Hakimi AA, Armstrong WB. Hand sanitizer in a pandemic: wrong formulations in the wrong hands. J Emerg Med. 2020;59:668–672. doi: 10.1016/j.jemermed.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rivera JM, Gupta S, Ramjee D, El Hayek GY, El Amiri N, Desai AN, et al. Evaluating interest in off-label use of disinfectants for COVID-19. Lancet Digit Health. 2020;2(11):e564–e566. doi: 10.1016/S2589-7500(20)30215-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, Berling K, Mercante JW, Murphy JL, Garcia-Williams AG. Knowledge and practices regarding safe household cleaning and disinfection for COVID-19 prevention—United States, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):705–709. doi: 10.15585/mmwr.mm6923e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lohiniva A, Sane J, Sibenberg K, Puumalainen T, Salminen M. Understanding coronavirus disease (COVID-19) risk perceptions among the public to enhance risk communication efforts: a practical approach for outbreaks, Finland, February 2020. Euro Surveill. 2020;25. 10.2807/1560-7917.ES.2020.25.13.2000317. [DOI] [PMC free article] [PubMed]


