Introduction
The COVID-19 pandemic has increased the use of remote telehealth evaluations of sports medicine injuries and shoulder injuries [30,35]. The improvement of web-based videoconferencing platforms has allowed for more user-friendly, face-to-face interactions between patients and clinicians [15]. Both patients and providers have been forced to welcome telehealth as an alternative because of recent required social distancing and restrictions on in-person visits. There have been several studies across various medical specialties that have shown telehealth visits have similar patient satisfaction levels compared with in-person visits. In addition, telehealth visits have shown decreased overall visit times, wait times, and health care costs [2,29,32,42,43]. While the use of telehealth had increased in some medical specialties, before the COVID-19 crisis, it had not had a significant role in most orthopedic surgery or sports medicine practices [25]. As we return to a new normal, most musculoskeletal care providers recognize telehealth as an alternative. This becomes particularly relevant because patients and providers have an increasing demand for convenience and proficiency [25,27,30,35]. A common belief among musculoskeletal clinicians is that telemedicine has a limited ability to provide accurate and through physical examination—the keystone of clinical orthopedic evaluation [8,9,17,18,38,39]. Specifically, many providers feel that in a telehealth visit, it is too difficult to perform exam maneuvers that require manual motor testing for strength, motion assessment, and provocative testing for pain. There is a recent study describing basic physical examination components [35]; in addition we have recently pubilshed an overview of the telehealth examination of the shoulder and knee elsewhere [24]. Here, we provide a basic overview.
The purpose of this article is to arm clinicians with a comprehensive shoulder physical examination for the telehealth visit, including easy-to-understand verbal instructions and checklists for documentation.
Preparation for Telehealth Visit
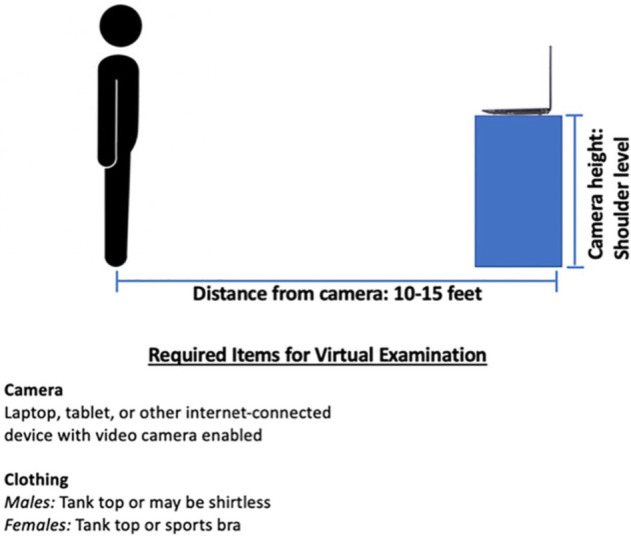
To maximize the efficiency of the telehealth visit, patients should complete all paperwork, including specific questions related to the history of present illness, past histories, and review of systems. Supplemental Table 1 provides specific instructions and guidelines on clothing, patient positioning, exam room setup, camera positioning, and any required common household items. In addition, patients should familiarize themselves with the instructions on how to set up their camera and review the guidelines on microphone settings and proper camera positioning, location, and lighting. At the beginning of the visit, the patient should be seated with the camera at eye level. Throughout the physical exam, the patient and camera will need to reposition, depending on the exam maneuver that the patient is being asked to perform. The position and angle of the camera will change depending on the camera type and patient position. In addition, it is important that the patient is dressed in appropriate clothing for the visit. It is also essential to have available support from the information technology department throughout the visit for help with technical difficulties.
Virtual Shoulder Examination
In most instances, a comprehensive shoulder exam can be divided into a basic core exam and a pathology-specific special testing. The basic core exam can be performed on all patients presenting with shoulder pain and includes palpation, inspection, motor testing, range of motion testing, peripheral vascular exam, and sensory testing. Depending on a patient’s specific pathology, further special pathology-specific testing can then be tailored by the clinician [17,18,38,39]. Special testing can be performed as needed based on the patient’s history and core shoulder exam.
A neurologic cause should be ruled out in a patient who presents with undifferentiated shoulder and neck pain [17,18,40,41,48]. In the setting of cervical disk disease, the Spurling test can be helpful [17,40,41].
Core Shoulder Exam
Once the patient is appropriately positioned in front of the camera, the clinician should inspect the bilateral shoulders and should evaluate for obvious atrophy, deformity, incisions, scars, rashes, swelling, ecchymosis, or erythema. The clinician can also ask the patient to turn to the side and then to turn so their back faces the camera to visualize the entire shoulder and allow for a thorough inspection. This can help identify specific findings including atrophy of the rotator cuff muscle bellies. The location of maximal pain can be pointed out by the patient using 1 finger. Range of motion should be performed looking for symmetry and pain. Shoulder forward flexion should be visualized with the patient facing the side. External rotation and abduction can be evaluated with the patient directly facing the camera. Internal rotation can be assessed with the patient’s back to the camera. In addition, technology can be used to assist in acquiring objective information during the physical exam. These include evaluating shoulder range of motion virtual using goniometers, smart-phone applications, and motion sensing technologies like accelerometers and gyroscopes [6,46,48]. A majority of the strength testing can be performed using common household items [35]. The patient can independently do a peripheral vascular exam and sensory testing. These exams can also be compared by the patient with the other side. Scapular positioning and dynamic scapular motion can often accompany shoulder pathologies [4,18,28,36]. Bilateral scapulae can be assessed with the patient’s back facing the camera. Bilateral scapular motion can be evaluated by having the patient elevate their arms in the scapular and sagittal planes [23].
Special Testing
Pathology-specific special testing can be broken down into subtesting for biceps-labrum complex (BLC) disease, glenohumeral instability, acromioclavicular (AC) joint arthrosis, impingement/rotator cuff pathology, generalized ligamentous laxity, and thoracic outlet syndrome [17,18,38,39]. Most of the shoulder special testing can be completed by the patient with minor alterations to the originally described techniques (Fig. 1). The use of an additional remote examiner can help facilitate some provocative maneuvers but is not a prerequisite. We have included the sensitivities, specificities, and likelihood ratios for the in-person version of these exams or test/maneuvers.
Fig. 1.
Schematic of virtual shoulder examination.
Rotator Cuff and Impingement
The Neer and Hawkins tests are excellent screening tests to identify rotator cuff pathology. The patient can also use their contralateral arm and hand for assistance to perform some of the maneuvers [16,17,20,26,29,38]. Strength testing of the rotator cuff can be assessed using household items. Our modification of strength testing involves using a combination of 2 plastic grocery bags and multiple cans of soup or beans (each weighing approximately 16 ounces each). Adding or removing cans to the plastic grocery bag allows the provider to do a modified strength testing as the resistance increases or decreases. This modifications allows for a modified assessment of a strength grade. Furthermore, the handles on the plastic grocery bag allow for strength testing to be performed while the thumb is pointed upward or downward. This allows the clinician to perform a Jobe test with modification. This modification to the Jobe test is completed with the patient holding the grocery bag with soup cans with the thumb pointed down at the shoulder level in the scapular plane [16,17,20,26,29,38]. With the patient facing the camera, additional rotator cuff–specific testing can be completed including testing of the teres minor using the hornblower test or Patte test [11,16,44]. With the patient facing their affected side to the camera, the subscapularis can be tested using the belly press and liftoff tests [3,16,20,34,47]. These maneuvers can be performed almost completely by the patient (Supplemental Table 2).
Acromioclavicular Joint
Tenderness to palpation directly over the AC joint is an excellent screening tool to identify AC joint pathology. Palpation and localization of pain over the AC joint can be completed by the patient using their uninvolved contralateral side [16,17,38,45]. In addition, with the patient facing the camera, a cross-body adduction test can also be completed [10,16,45] (Supplemental Table 3).
The Biceps-Labral Complex
Identification of pain to palpation over the bicipital groove can be completed by the patient using the patient’s contralateral arm. Good confirmatory test for proximal biceps pathology including the Speed and Yergason [5,14,17,19,23,38]. Both of these tests can be completed using modifications by the patient. The O’Brien test is also another screening test for BLC disease [37]. Our modification of the O’Brien test can be performed by the patient using a plastic grocery bag with addition or removal of soup cans (Supplemental Table 4).
Glenohumeral Instability
The anterior apprehension test is an excellent screening and confirmatory test for anterior shoulder instability [12,18,38]. The anterior apprehension test can be performed by asking the patient to place their involved extremity into a thrower’s position. Our modifications also allow the posterior stress test for posterior instability and sulcus test for inferior or multidirectional instability to be performed by the patient (Supplemental Table 5).
When completing a comprehensive shoulder exam, generalized joint hypermobility and evaluation for thoracic outlet syndrome should be completed. Facing the camera, the patient can independently complete the Beighton score and Roos test [7,21] (Supplemental Table 6).
Postoperative Shoulder Exam
A potential great application for the virtual visit is for postoperative appointments for patients who have had shoulder surgery. The purpose of the immediate postoperative virtual visit would be to identify any potential red flags that would prompt an in-person visit. Patient should be asked to position their camera to fully visualize their operative shoulder. This would allow for assessment of the incision, surrounding ecchymosis, drainage, and erythema. In addition, when appropriate, range of motion can be assessed as outlined above. Using technology like virtual goniometer or wearable technology can help facilitate and document the assessment of the change in range of motion between postoperative visits [13,35].
Discussion
After completing the “core shoulder exam,” additional pathology-specific special testing is performed, depending on the clinical suspicious and differential diagnoses. The pathology-specific special testing should be directed by the patient’s history of present illness, and core shoulder exam findings. Regardless of workflow or the exam approach of the physician, we have provided a standardized approach that is comprehensive to the virtual shoulder exam. This includes previsit setup, and modifications to in-person physical exam testing. As these modified exam maneuvers are used more, there will be improved standardization allowing for improved reliability and validity of these virtual exam maneuvers. While there are certain physical exam tests such as load and shift for glenohumeral instability that cannot be performed virtually, there are many portions of the shoulder physical exam that can be effectively be completed using a video-based Telehealth application. This does require physicians to expand their choice of exam maneuvers to include some minor modifications and alternatives to classic exam maneuvers, such as our modification to the Jobe test (Figure 2) [16,17,20,26,29,38]. Using these modifications, we are still able to acquire useful data through the virtual shoulder exam to allow for accurate and appropriate clinical decision making. After total joint arthroplasty, Sharareh and Schwarzkopf [33] reported that patients had increased patient satisfaction when compared with customary in-person outpatient clinic visits. This observation has been similar with the recent clinical experience, in the setting of a high-volume total shoulder arthroplasty, of the senior author (S.A.T.). When looking at postoperative patients after rotator cuff repair, Kane et al [22] showed in a randomized controlled trial that these patients received safe and effective postoperative follow-up care using telehealth when compared with traditional in-person outpatient postoperative clinic visits. In addition, postoperative wound complications and breakdowns can be easily identified during telehealth encounters [15]. The advancement, use, and access of video-based online applications have changed the way that telehealth visits are conducted. Over the last decade, there has been a drive to leverage new technologies to help better treat and understand patients [1]. As more video-based online platforms become accesible to patients, these tenchnologies can be further leveraged and modified to help standardize the virtual patient encounter. They can be potentially levereaged to identify at-risk patients, and to improve the reliability and validity of the virtual physical exam. A number of studies have assessed inter- and intra-observer reliability and validity of shoulder physical exam data points like acceleration, velocity, and range of motion [31]. Identification and sourcing of these data points have included the use of wearable accelerometers, gyroscopes, camera-based motion software, and inertial sensor monitoring units [31]. At some point in the future, we imagine a collaboration of motion sending technologies, video-based online applications, and data analytic software to help supplement and standardize the virtual visit and physical exam.
Fig. 2.
Modifications to common exam maneuvers for virtual shoulder exam: (a) Jobe’s test (thumbs down abduction) with soup cans in grocery bag for resistance. (b) Resisted external rotation testing. (c) Resisted internal rotation testing. (d) Hawkins test using contralaternal hand to push abducted shoulder into internal rotation. (e) Cross-body adduction using contralaternal arm. (f) O’Brien (active compression) test with the thumb pointed down and resistance provided by soup cans in grocery bag (Supplemental Table 7). (g) O’Brien test with thumb pointed up [24].
Conclusion
Telemedicine has the potential to change care delivery, increase health care savings, increase geographical expansion, and improve time-efficiency. While an in-person exam can be considered a gold-standard, we maintain that a majority of the customary in-person shoulder physical exam can be completed virtually with little to no modification of exam maneuvers. In addition, we maintain that the data points acquired from a virtual visit for shoulder pathology can allow for and enable the provider to make meaningful clinical decisions. We have provided a comprehensive description of the shoulder physical examination for sports medicine telehealth visits including (1) verbal instructions in layman’s terms, (2) annotated images of each exam maneuver that can be provided to patients via screen share options, and (3) a checklist for documentation. Additional studies need to be completed in the future to validate the virtual shoulder physical exam presented here.
Supplemental Material
Supplemental material, sj-pdf-2-hss-10.1177_1556331620975033 for The Virtual Shoulder Physical Exam by Samuel A. Taylor, Joseph D. Lamplot, Sridhar Pinnamaneni, Joseph D. Lamplot, Scott A. Rodeo, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Warren K. Young and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-pdf-3-hss-10.1177_1556331620975033 for The Virtual Shoulder Physical Exam by Samuel A. Taylor, Joseph D. Lamplot, Sridhar Pinnamaneni, Joseph D. Lamplot, Scott A. Rodeo, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Warren K. Young and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-zip-1-hss-10.1177_1556331620975033 for The Virtual Shoulder Physical Exam by Samuel A. Taylor, Joseph D. Lamplot, Sridhar Pinnamaneni, Joseph D. Lamplot, Scott A. Rodeo, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Warren K. Young and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Sridhar Pinnamaneni, MD; Joseph D. Lamplot, MD; Stephanie Swensen-Buza, MD; Cort D. Lawton, MD; and Warren K. Young, MD, declare they have no conflicts of interest. Scott A. Rodeo, MD, reports relationships with Advance Medical and Ortho RTI, outside the submitted work. Joshua Dines reports relationships with Arthrex Inc, Thieme Inc, Linvatec, Wolters Kluwer Health, American Shoulder and Elbow Surgeons, and the Journal of Shoulder and Elbow Surgeons, outside the submitted work. Samuel A. Taylor, MD, reports relationships with DJO Orthopedics and Mitek, outside the submitted work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
Supplemental Material: Supplemental material for this article is available online.
CME Credit: Please go to HSS eAcademy at https://bit.ly/HSSJCME to find all journal-related CME, complete the online post-test, and claim CME credit.
References
- 1. Anoushiravani AA, Patton J, Sayeed Z, El-Othmani MM, Saleh KJ. Big data, big research: implementing population health-based research models and integrating care to reduce cost and improve outcomes. Orthop Clin North Am. 2016;47(4):717–724. [DOI] [PubMed] [Google Scholar]
- 2. Atanda A, Pelton M, Fabricant PD, Tucker A, Shah SA, Slamon N. Telemedicine utilisation in a paediatric sports medicine practice: decreased cost and wait times with increased satisfaction. J ISAKOS. 2018;3(2):94–97. [Google Scholar]
- 3. Barth JRH, Burkhart SS, De Beer JF. The Bear-Hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;22:1076–1084. [DOI] [PubMed] [Google Scholar]
- 4. Benjamin Kibler W, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20:364–372. [DOI] [PubMed] [Google Scholar]
- 5. Bennett WF. Specificity of the Speed’s test: arthroscopic technique for evaluating the biceps tendon at the level of the bicipital groove. Arthroscopy. 1998;14:789–796. [DOI] [PubMed] [Google Scholar]
- 6. Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21:29–35. [DOI] [PubMed] [Google Scholar]
- 7. Brantigan CO, Roos DB. Diagnosing thoracic outlet syndrome. Hand Clin. 2004;20:27–36. [DOI] [PubMed] [Google Scholar]
- 8. Bronstein RD, Schaffer JC. Physical examination of knee ligament injuries. J Am Acad Orthop Surg. 2017;25:280–287. [DOI] [PubMed] [Google Scholar]
- 9. Bronstein RD, Schaffer JC. Physical examination of the knee: meniscus, cartilage, and patellofemoral conditions. J Am Acad Orthop Surg. 2017;25(5):365–374. [DOI] [PubMed] [Google Scholar]
- 10. Chronopoulos E, Kim TK, Park HB, Ashenbrenner D, McFarland EG. Diagnostic value of physical tests for isolated chronic acromioclavicular lesions. Am J Sports Med. 2004;32:655–661. [DOI] [PubMed] [Google Scholar]
- 11. Collin P, Treseder T, Denard PJ, Neyton L, Walch G, Lädermann A. What is the best clinical test for assessment of the teres minor in massive rotator cuff tears? Clin Orthop Relat Res. 2015;473:2959–2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Farber AJ, Castillo R, Clough M, Bahk M, McFarland EG. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am. 2006;88:1467–1474. [DOI] [PubMed] [Google Scholar]
- 13. Ferriero G, Vercelli S, Sartorio F, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36:146–151. [DOI] [PubMed] [Google Scholar]
- 14. Gill HS, El Rassi G, Bahk MS, Castillo RC, McFarland EG. Physical examination for partial tears of the biceps tendon. Am J Sports Med. 2007;35:1334–1340. [DOI] [PubMed] [Google Scholar]
- 15. Grandizio LC, Foster BK, Klena JC. Telemedicine in hand and upper-extremity surgery. J Hand Surg Am. 2020;45(3):239–242. [DOI] [PubMed] [Google Scholar]
- 16. Hegedus EJ, Goode A, Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42:80–92. [DOI] [PubMed] [Google Scholar]
- 17. Hippensteel KJ, Brophy R, Smith MV, Wright RW. A comprehensive review of physical examination tests of the cervical spine, scapula, and rotator cuff. J Am Acad of Orthop Surg. 2019;27(11):385–394. [DOI] [PubMed] [Google Scholar]
- 18. Hippensteel KJ, Brophy R, Smith MV, Wright RW. Comprehensive review of provocative and instability physical examination tests of the shoulder. J Am Acad Orthop Surg. 2019;27(11):395–404. [DOI] [PubMed] [Google Scholar]
- 19. Holtby R, Razmjou H. Accuracy of the Speed’s and Yergason’s tests in detecting biceps pathology and slap lesions: comparison with arthroscopic findings. Arthroscopy. 2004;30:231–236. [DOI] [PubMed] [Google Scholar]
- 20. Hughes PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008;54:159–170. [DOI] [PubMed] [Google Scholar]
- 21. Juul-Kristensen B, Røgind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology. 2007;46:1835–1841. [DOI] [PubMed] [Google Scholar]
- 22. Kane LT, Thakar O, Jamgochian G, et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29(4):775–783. [DOI] [PubMed] [Google Scholar]
- 23. Kibler WB, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37:1840–1847. [DOI] [PubMed] [Google Scholar]
- 24. Lamplot JD, Pinnamaneni S, Swensen-Buza S, et al. The Virtual Shoulder and Knee Physical Examination. Orthop J Sports Med. October 2020. 10.1177/2325967120962869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Macdonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg. 2000;9:299–301. [DOI] [PubMed] [Google Scholar]
- 27. Massey PA, McClary K, Zhang AS, Savoie FH, Barton RS. Orthopaedic surgical selection and inpatient paradigms during the coronavirus COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:436–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Parker S, Prince A, Thomas L, et al. Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ Open. 2018;8(8):e019192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rao SS, Loeb AE, Amin RM, Golladay GJ, Levin AS, Thakkar SC. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020;6:617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rawashdeh SA, Rafeldt DA, Uhl TL. Wearable IMU for shoulder injury prevention in overhead sports. Sensors (Basel). 2016;16(11):1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rigamonti L, Albrecht UV, Lutter C, et al. Potentials of digitalization in sports medicine: a narrative review. Curr Sports Med Rep. 2020;19(4):157–163. [DOI] [PubMed] [Google Scholar]
- 33. Sharareh B, Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty. 2014;29(5):918–922.e911. [DOI] [PubMed] [Google Scholar]
- 34. Somerville LE, Willits K, Johnson AM, et al. Clinical assessment of physical examination maneuvers for rotator cuff lesions. Am J Sports Med. 2014;42:1911–1919. [DOI] [PubMed] [Google Scholar]
- 35. Tanaka MJ, Oh LS, Martin SD, Berkson EM. The orthopaedic forum telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102:e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tate AR, McClure P, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44:165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Taylor SA, Newman AM, Dawson C, et al. The “3-Pack” examination is critical for comprehensive evaluation of the biceps-labrum complex and the bicipital tunnel: a prospective study. Arthroscopy. 2017;33(1):28–38. [DOI] [PubMed] [Google Scholar]
- 38. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination part I: the rotator cuff tests. Am J Sports Med. 2003;31(1):154–160. [DOI] [PubMed] [Google Scholar]
- 39. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination: part II: laxity, instability, and superior labral anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31(2):301–307. [DOI] [PubMed] [Google Scholar]
- 40. Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine. 2002;27:156–159. [DOI] [PubMed] [Google Scholar]
- 41. Viikari-Juntura E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine. 1989;14:253–257. [DOI] [PubMed] [Google Scholar]
- 42. Vyas KS, Hambrick HR, Shakir A, et al. A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg. 2017;78(6):736–768. [DOI] [PubMed] [Google Scholar]
- 43. Vyas KS, Morrison SD, Vasconez HC, et al. Teledermatology: is it beneficial to patients? Ann Plast Surg. 2017;79(4):415–416. [DOI] [PubMed] [Google Scholar]
- 44. Walch G, Boulahia A, Calderone S, Robinson AHN. The “dropping” and “hornblower’s” signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80:624–628. [DOI] [PubMed] [Google Scholar]
- 45. Walton J, Mahajan S, Paxinos A, et al. Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am. 2004;86:807–812. [DOI] [PubMed] [Google Scholar]
- 46. Werner BC, Holzgrefe RE, Griffin JW, et al. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg. 2014;23:e275–e282. [DOI] [PubMed] [Google Scholar]
- 47. Yoon JP, Chung SW, Kim SH, Oh JH. Diagnostic value of four clinical tests for the evaluation of subscapularis integrity. J Shoulder Elbow Surg. 2013;22:1186–1192. [DOI] [PubMed] [Google Scholar]
- 48. Zulkarnain RF, Kim GY, Adikrishna A, Hong HP, Kim YJ, Jeon IH. Digital data acquisition of shoulder range of motion and arm motion smoothness using Kinect v2. J Shoulder Elbow Surg. 2017;26:895–901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-2-hss-10.1177_1556331620975033 for The Virtual Shoulder Physical Exam by Samuel A. Taylor, Joseph D. Lamplot, Sridhar Pinnamaneni, Joseph D. Lamplot, Scott A. Rodeo, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Warren K. Young and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-pdf-3-hss-10.1177_1556331620975033 for The Virtual Shoulder Physical Exam by Samuel A. Taylor, Joseph D. Lamplot, Sridhar Pinnamaneni, Joseph D. Lamplot, Scott A. Rodeo, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Warren K. Young and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-zip-1-hss-10.1177_1556331620975033 for The Virtual Shoulder Physical Exam by Samuel A. Taylor, Joseph D. Lamplot, Sridhar Pinnamaneni, Joseph D. Lamplot, Scott A. Rodeo, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Warren K. Young and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery



