Abstract
Objective:
This article aims to appraise how scientific evidence related to CBCT has changed over the years, based on levels of evidence and diagnostic efficacy.
Methods:
A general search strategy was used in different databases (Pubmed, Embase, and Web of Science) to identify systematic reviews (SRs) on CBCT until November of 2020. The SRs included were divided according to different specialties of dentistry. A critical review of the articles was made, describing the level of evidence and efficacy.
Results:
In total, 75 articles were selected. There was an increase in the number of SRs on CBCT from 2014 onwards, as 83% of the SRs on this topic were published after 2013, and 72% between 2016 and to date. Twenty SRs (27%) performed meta-analysis. Only 28% of the SRs provided a detailed description of CBCT protocols. According to SR evidence, almost all specialties of dentistry have advanced concomitantly with the introduction of CBCT. The majority of SRs were related to clinical applications (level 2 of efficacy), followed by technical parameters (level 1 of efficacy). Only some CBCT models were mentioned in the SRs selected.
Conclusion:
Over the course of 20 years, SRs related to CBCT applications for a broad range of dental specialties have been published, with the vast majority of studies at levels 1 and 2 of diagnostic efficacy. Not all CBCT models available on the market have been scientifically validated. At all times, one should remain cautious as such not to simply extrapolate in vitro results to the clinical setting. Also, considering the wide variety of CBCT devices and protocols, reported results should not be overstated or generalized, as outcomes often refer to specific CBCT devices and protocols.
Keywords: cone-beam computed tomography, radiology, systematic review, meta-analysis
Introduction
Since the development of the first cone-beam CT (CBCT) device dedicated to dentomaxillofacial imaging in 1998,1 a remarkable increase in the availability of models occurred, particularly in the last 10 years. In 2008, 23 models were available1 and in 2013, there were 43.2 Recently, 279 models were catalogued, in spite of CBCT being considered a generic term that covers a wide variety of technical specifications and models.3 Over the course of these years, an increasing number of articles scrutinizing aspects related to CBCT have also been verified. However, the dissemination and growth of CBCT technology may have moved faster than the methods for acquisition of evidence related to their application.4
An advanced search in Pubmed database on September 2020 using the terms “Cone-beam computed tomography AND (dental OR oral)” enabled the retrieval of 8,731 publications, with an exponential increase on publication from 2012 onwards. This extremely high number of articles reinforces the need for an evidence-based method for analysing published data regarding CBCT.
Thus, it is of paramount importance to obtain evidence-based guidelines for CBCT imaging. There are important publications available for the guidance of clinicians, based on position papers prepared by internationally recognized associations and consensus group statements.5–10 In 2012, the SEDENTEXCT project published evidence-based indications for CBCT used in the different clinical fields.11 Their recommendations were and are still used worldwide. However, an update of these recommendations is needed, considering the advances in research in the last 10 years.
It is important to mention that radiological studies are graded according to varying levels of efficacy evidence,12 hence a six-tiered hierarchical model of the efficacy of diagnostic imaging was introduced in 1991.13 These levels comprise technical aspects of the new technologies (level 1), diagnostic accuracy (level 2), diagnostic thinking (level 3), treatment choice and outcome (levels 4 and 5, respectively), and a cost/benefit analysis of its value to society at large scale (level 6).
The levels of evidence may vary according to the type of study and can provide a way to visualize both the quality of evidence and the amount of evidence available. Traditionally, as a type of study that critically appraises and synthesizes the findings of primary studies, the systematic review (SR) is considered to be at the top of the pyramid of evidence.14 Thus, SRs can be a good source of information when endeavoring to analyze the knowledge generated over the years with regard to a specific topic. Smith et al. (2011)15 proposed a methodology for conducting an SR of previously published SRs. This methodology unites the evidence relative to a topic and may be useful to clinicians in the decision-making process. However, when working with broad themes, this type of methodology may not be feasible.
Although a recent publication presented an inventory of all CBCT units available worldwide and listed their technical features,3 it is of paramount importance to look for the evidence concerning this imaging technique. Therefore, the aim of the present article was to appraise how scientific evidence related to CBCT has changed over the last two decades by analyzing SRs. Secondary objectives were to critically analyze all SRs, and to assess their level of evidence and diagnostic efficacy, for diagnostic and treatment planning applications in various dental specialties and a wide variety of CBCT devices available on the market.
Methods
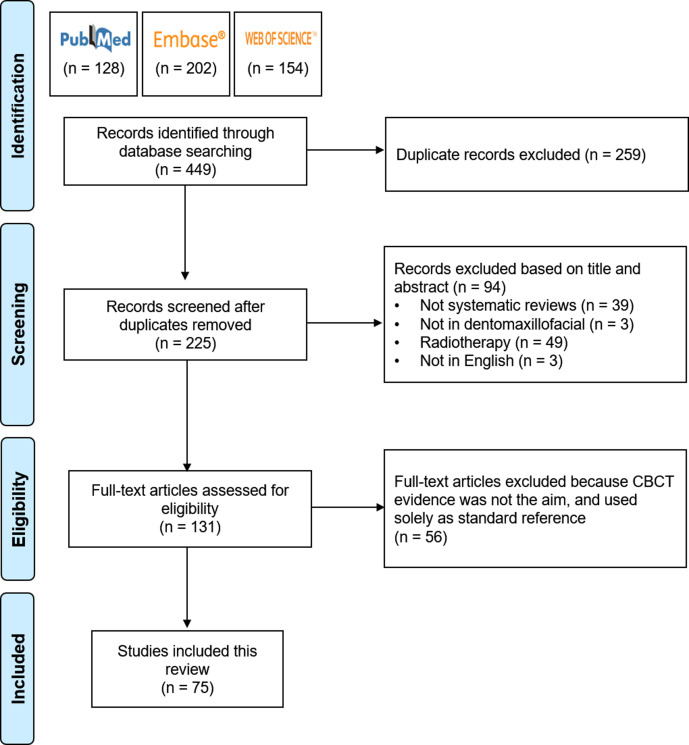
A general search strategy was used in different databases (Pubmed, Embase, and Web of Science), to identify SRs on CBCT up to September 2020. For this purpose, the keywords “cone-beam computed tomography”, “CBCT”, and “systematic review” were used. The search results were exported to a reference manager (Mendeley Desktop, version 1.19.4, Mendeley Ltd., London, UK), and all duplicates were manually removed by one observer (HGA). A second exclusion process, based on the title and abstract of the studies, was performed by three observers (HGA, AFL, KFV). In consensus, they removed the articles that addressed radiotherapy, CBCT applications in body parts other than the dentomaxillofacial complex, studies that were not specifically SRs (i.e., narrative reviews), those that used CBCT solely as reference-standard to assess different outcomes (e.g., alveolar bone changes caused by orthodontic treatment), and articles published in languages other than English.
After the exclusion process, the remaining articles were divided according to the following specialties of dentistry: Endodontics, Implant Dentistry, Orthodontics, Oral and Maxillofacial Surgery (including Orthognathic Surgery), Pathology, Pediatric Dentistry, Periodontology, Radiology, and Temporomandibular Joint (TMJ) Imaging. The same three observers independently analyzed the SRs included, and extracted information such as the year of publication, main objective of the SR, types of CBCT units reported and description of CBCT protocols, conclusions, and level of evidence based on the six-tiered hierarchical model introduced by Fryback and Thornbury.13 The findings were descriptively expressed in a chronological sequence within each specialty.
Results
A total of 484 articles were retrieved during the initial screening. Two hundred and fifty-nine duplicates were removed, resulting in 225 articles. After further analysis, 49 were excluded because they were related to CBCT by on board imager in radiotherapy equipment, 39 studies were not SRs, 56 studies used CBCT as a reference standard to assess different outcomes, three studies were in German, and three studies were not related to the dentomaxillofacial complex. In total, 75 articles were selected (Figure 1). The articles included were divided according to the specialty: Endodontics (n = 16), Implant Dentistry (n = 7), Orthodontics (n = 15), Oral and Maxillofacial Surgery (n = 10), Pathology (n = 3), Paediatric Dentistry (n = 1), Periodontology (n = 10), Radiology (n = 9), and TMJ Imaging (n = 4).
Figure 1.
Diagram flowchart of the selection of the included studies.
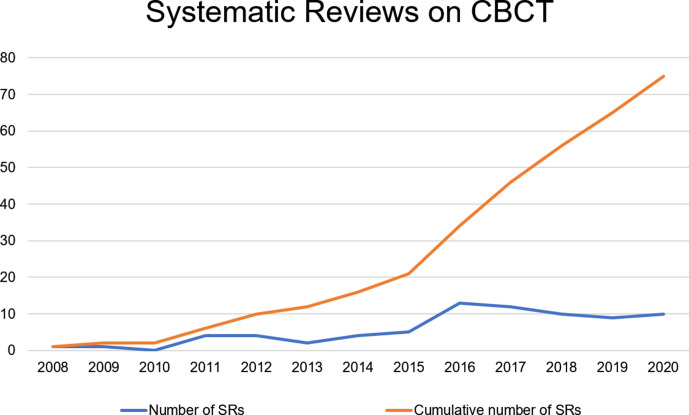
The first SR included in the present study dated back to 2008. There was a more significant increase in the number of SRs on CBCT from 2014 onwards. In other words, 84% of the SRs on CBCT were published after 2013, and 72% between 2016 and 2020 (Figure 2). Out of all the SRs selected, only 20 SRs (27%) performed meta-analysis. Considering the period since the first published SR on CBCT, it could be noted that the majority of SRs were related to clinical applications and diagnostic accuracy, followed by technical parameters (levels 2 and 1 of the six-tiered hierarchical model, respectively). Only 21 SRs (28%), provided a detailed description of CBCT protocols. Furthermore, 25 SRs provided a partial description of the protocols, mainly CBCT voxel size. As regards the CBCT units reported in the SRs, 52 models made by 20 manufacturers were identified, as described in Table 1. The majority of the CBCT models were reported in radiology SRs (30%), followed by endodontics (21%). The CBCT units manufactured by KaVo/Imaging Science International (i-CAT models, USA), Quantitative Radiology, Cefla Dental Group (NewTom models, Italy), and J. Morita (Accuitomo models, Japan) were the predominant types.
Figure 2.
Number of systematic reviews included for analysis per year.
Table 1.
Cone-beam CT manufacturers and respective models reported by systematic reviews according to dentistry specialties
| Manufacturer | Model | Endodontics | Implant | Orthodontics | OMFS | Pathology | Paediatric dentistry | Periodontology | Radiology | TMJ Imaging |
Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 3M IMTEC (USA) | ILUMA | 116 | 117 | 118 | - | - | - | - | 419–22 | - | 7 |
| Acteon (France) | Whitefox | - | - | - | 123 | - | - | 120 | - | 2 | |
| Asahi Roentgen (Japan) | Alphard VEGA | - | - | 124 | - | - | - | 225,26 | - | - | 3 |
| PSR9000 | - | 117 | 127 | 128 | 123 | - | - | - | - | 4 | |
| 0 | 1 | 2 | 1 | 1 | 0 | 2 | 0 | 0 | 7 | ||
| Carestream/Kodak (France) | Kodak 9000 | 229,30 | - | - | - | - | 131 | 325,32,33 | 419–22 | - | 10 |
| CS8100 | 130 | - | - | - | - | - | - | - | - | 1 | |
| CS9300 | - | - | - | - | - | - | 125 | 220,34 | - | 3 | |
| CS9500 | - | 117 | - | - | - | - | 225,33 | 319,20,22 | - | 6 | |
| 3 | 1 | 0 | 0 | 0 | 1 | 6 | 9 | 0 | 20 | ||
| Dentsply Sirona (Germany) | Galileos | 330,35,36 | 117 | 224,37 | - | - | 131 | - | 219,38 | 139 | 10 |
| Galileos Compact | - | 140 | - | - | - | - | 225,32 | - | - | 3 | |
| Galileos Comfort | 141 | - | - | - | - | - | 142 | 220,21 | - | 4 | |
| Orthophos XG 3D | - | - | - | - | - | - | - | 219,38 | - | 2 | |
| 4 | 2 | 2 | 0 | 0 | 1 | 3 | 6 | 1 | 19 | ||
| HDX Will (Republic of Korea) | Dinnova | - | - | - | - | - | - | - | 120 | - | 1 |
| Hitachi (Japan) | CB MercuRay | - | - | 618,24,27,37,43,44 | 228,45 | - | 131 | - | 719–22,34,38,46 | - | 16 |
| CB Throne | - | - | - | - | - | - | - | 138 | - | 1 | |
| 0 | 0 | 6 | 2 | 0 | 1 | 0 | 8 | 0 | 17 | ||
| J Morita (Japan) | 3D Accuitomo | 716,29,35,36,47–49 | 317,40,50 | 124 | 145 | - | 131 | 725,26,33,42,51–53 | 620–22,38,46,54 | - | 26 |
| 3D Accuitomo FPD 80 | 141 | 155 | - | - | - | - | 525,26,32,51,52 | 119 | - | 8 | |
| 3D Accuitomo 170 | 816,30,35,36,41,47,49,56 | 217,50 | 127 | 145 | - | 131 | 125 | 121 | - | 15 | |
| Veraviewepocs | 329,30,48 | - | - | - | - | - | - | 219,20 | - | 5 | |
| 19 | 6 | 2 | 2 | 0 | 2 | 13 | 10 | 0 | 54 | ||
| KaVo Kerr (USA) | 3D eXam | 141 | - | 224,44 | - | - | - | - | 619–22,34,54 | - | 9 |
| KaVo/Imaging Science International (USA) | i-CAT | 829,30,35,36,41,47,48,57 | 317,40,50 | 718,24,27,37,43,44,58 | 628,45,59–62 | 123 | 131 | 725,26,32,33,42,51,52 | 519,21,34,38,54 | 163 | 39 |
| i-CAT Classic | 130 | 117 | - | - | - | 131 | - | 219,20 | - | 5 | |
| i-CAT Next Generation | 416,30,35,36 | 317,40,55 | 118 | - | - | 131 | - | 219,20 | 139 | 12 | |
| i-CAT FLX | - | - | - | - | - | - | - | 219,21 | - | 2 | |
| 13 | 7 | 8 | 6 | 1 | 3 | 7 | 11 | 2 | 58 | ||
| KaVo/Instrumentarium (Finland) | OP300 | - | - | - | - | - | 131 | - | - | - | 1 |
| KaVo/Soredex (Finland) | Cranex 3D | - | - | - | - | - | - | - | 220,21 | - | 2 |
| Scanora 3D | 330,35,36 | - | - | 345,59,60 | - | 131 | 425,26,33,42 | 519–22,54 | - | 16 | |
| 3 | 0 | 0 | 3 | 0 | 1 | 4 | 7 | 0 | 18 | ||
| MyRay (Italy) | Skyview | - | - | - | - | - | - | - | 219,20 | - | 2 |
| PiXAMED (Thailand) | DentiiScan | - | - | - | - | - | - | - | 120 | - | 1 |
| Planmeca (Finland) | ProMax 3D | 336,41,56 | 117 | - | - | - | - | 425,33,42,52 | 519–22,54 | - | 13 |
| ProMax 3D Classic | - | - | - | - | 123 | - | - | - | - | 1 | |
| ProMax 3D S | 229,30 | - | - | - | - | - | 152 | - | - | 3 | |
| ProMax 3D Max | 130 | 140 | - | - | - | 131 | - | - | - | 3 | |
| 6 | 2 | 0 | 0 | 1 | 1 | 5 | 5 | 0 | 20 | ||
| PreXion (Japan) | PreXion 3D | 230,56 | - | - | - | - | - | - | 219,38 | - | 4 |
| Quantitative Radiology/Cefla Dental Group (Italy) | NewTom | - | - | 143 | 160 | - | - | - | - | - | 2 |
| NewTom 9000 | - | 117 | 327,44,58 | 162 | - | 131 | 242,52 | 419,20,34,38 | - | 12 | |
| NewTom 3G | 716,29,35,36,41,47,48 | 240,50 | 418,24,27,58 | 345,50,59 | - | 131 | 325,33,52 | 619–22,34,38 | - | 26 | |
| NewTom 5G | 130 | - | - | - | - | - | - | 220,21 | - | 3 | |
| NewTom VG | 241,47 | - | - | - | - | - | 325,26,52 | 219,22 | - | 7 | |
| NewTom VGi | - | 240,55 | 144 | - | - | - | - | 219,20 | - | 5 | |
| 10 | 5 | 9 | 5 | 0 | 2 | 8 | 16 | 0 | 55 | ||
| Vatech (Republic of Korea) | DCT Pro | - | - | - | 162 | - | - | - | 119 | - | 2 |
| PaX-Uni 3D | - | - | - | - | - | - | - | 219,20 | - | 2 | |
| PaX-Duo 3D | - | 140 | - | - | - | - | - | 119 | - | 2 | |
| Picasso Duo | - | - | - | - | - | - | - | 120 | - | 1 | |
| Picasso Trio | 156 | 240,50 | - | - | - | - | - | 319–21 | - | 6 | |
| Master 3D | 156 | - | 327,43,44 | - | - | - | - | 119 | - | 5 | |
| PaX-i3D | 130 | - | - | - | - | - | - | - | - | 1 | |
| PaX Reve 3D | - | - | 124 | - | - | - | - | - | - | 1 | |
| PaX Zenith | - | - | 124 | - | - | - | - | - | - | 1 | |
| 3 | 3 | 5 | 1 | 0 | 0 | 0 | 9 | 0 | 21 | ||
| Xoran Technologies (USA) | DentoCAT | - | - | - | - | - | - | - | 138 | - | 1 |
| MiniCAT | - | - | 127 | - | - | - | - | - | - | 1 | |
| 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | ||
| Yoshida (Japan) | FineCube | 229,30 | - | - | - | - | - | 120 | - | 3 | |
| TOTAL | 67 | 28 | 38 | 20 | 4 | 13 | 48 | 100 | 3 | 321 | |
OMFS, Oral and maxillofacial surgery; TMJ, temporomandibular joint.
Cells are filled according to the number of systematic reviews that reported that CBCT unit.  : none;
: none; :1 time;
:1 time;  : from 2 to 5 times;
: from 2 to 5 times;  : more than six times.
: more than six times.
Findings regarding specific specialties
Endodontics
Sixteen of the SRs concerned endodontic applications of CBCT, mostly related to root fracture detection,16,35,36,41,47,56,57 and periapical lesions or periapical tissue evaluation.29,48,49,64,65 Other subjects of study were the value of CBCT for root canal morphology,30 establishing the working length,66 detection of external root resorption,67 and one SR focused on the overall diagnostic efficacy of CBCT in Endodontics.68
Relative to periapical lesion detection, in 2012 one SR concluded that CBCT was more sensitive for this task when compared with periapical radiography.48 In 2015, a six-level efficacy model showed that the majority of studies on this subject were in vitro studies on the diagnostic accuracy level (level 2 of efficacy).29 The following SRs (from 2018 and 2020) showed higher accuracy for CBCT when compared with 2D methods in both in vitro and in vivo studies.49,64,65
Several SRs addressed CBCT indication for root fracture detection.16,35,36,41,47,56,57 All of them pointed out the higher accuracy of CBCT for this diagnostic task, however, with limited diagnostic value in the presence of high-density materials.16,35,36,47,56,57 The heterogeneity and low number of in vivo primary studies were also considered limitations.
One SR showed a higher diagnostic accuracy of CBCT in detecting external root resorptions when compared with conventional radiographic methods.67 In 2019, CBCT was indicated as being a reliable tool, at least as accurate as an electronic apex locator, for determining the working length.66 Recently, CBCT was described as being as accurate as micro-computed tomography for in vitro root canal morphology assessment.30 Once again, the inclusion of in vitro studies for all the aforementioned tasks limited the possibility of drawing clinical inferences with regard to the results.
The accuracy of CBCT imaging for endodontic purposes was clearly extracted from the selected 16 SRs. However, the heterogeneity of primary studies related to different study designs and CBCT models should be emphasized. Although several models were tested (Table 1), the performance of one CBCT cannot be extrapolated to another. Moreover, CBCT accuracy may be directly jeopardized in the presence of artefacts.
Implant dentistry
Seven SRs were identified in the implant dentistry field. An overview of guidelines, indications, and radiation dose risks related to CBCT use was published in 2014.69 At that time, the majority of the guidelines did not offer strong evidence-based statements to support the recommendations, indications, and contraindications of CBCT for this purpose. The development of patient-oriented CBCT protocols was recommended in order to reduce the radiation dose whenever possible.
In 2018, a SR demonstrated high accuracy and reliability of CBCT for linear measurement of bone, even when a lower resolution was selected, and therefore it was recommended for preoperative planning of implant placement.17
The usefulness of CBCT for post-operative evaluation of peri-implant bone was investigated by 3 SRs.40,50,55 One SR showed a similar accuracy between intraoral radiographs and CBCT for peri-implant bone defect assessments.50 The other SRs focused on CBCT peri-implant bone loss analyses compared to direct measurements40 and 2D images.55 Despite CBCT presenting good accuracy for fenestration-type and circumferential infra bony peri-implant defects, the last two SRs reported a low level of evidence to support the use of CBCT as a standard method for peri-implant bone level assessment, mainly due to the presence of metal-related artefacts. Moreover, the lack of clinical studies was reported in these SRs.
The same aforementioned limitations were reported in two evidence-based guidelines published in 2020, addressing the contribution of CBCT to implant planning70 and treatment outcomes.71 They stated that CBCT was of paramount importance for preoperative assessment.70 Nevertheless, due to artefacts arising from the implant, for postoperative assessment, CBCT should be used for some specific cases, such as in patients with postoperative sensory abnormalities.71
The accuracy of CBCT for preoperative implant assessment is well established in the literature (level 2 of efficacy). However, further investigations are required in order to assess whether this 3D imaging method would significantly impact the decision-making process and level of confidence during patient treatment. Considering the broad variety of CBCT models available on the market3 there were reports on only a few devices in the SRs related to implant dentistry (Table 1). Although CBCT imaging appears to be of limited use for postoperative planning due to artefacts, this effect may vary according to each CBCT device.
Orthodontics
Fifteen SRs were found related to the applicability of CBCT in orthodontics.18,24,27,37,43,44,58,72–79 In 2012, one SR showed no high-quality evidence regarding the benefits of CBCT used in this field, in spite of observing the potential of CBCT in treatment planning.74
Assessment of the upper airway using CBCT and its validation were considered research questions in a few SRs. While one SR considered CBCT an accurate and reliable tool when compared with 2D evaluation,18 the other found a divergent result.43 However, it is important to highlight that most of the selected studies differed in acquisition parameters and these were not fully described. More recently, CBCT demonstrated moderate-to-excellent intra- and interobserver reliability for volume and minimum cross-sectional area assessment, but the findings should be interpreted with caution, as most studies included in this SR were conducted under artificially controlled conditions.27 Furthermore, two SRs showed the applicability of CBCT for predicting airway volume77 and assessing patients that had undergone rapid maxillary expansion.76 When considering CBCT imaging for orthodontic and orthognathic treatment planning and follow-up, the assessment of the soft tissues is of vital importance. It is generally recommended to have the patient in an upright position as such to allow accurate appraisal of the soft tissues in a natural head position.76,77 In a supine position, facial contour and airway dimensions may indeed change. Fortunately, most CBCT devices allow for upright patient positioning.3 Although, lesser movement artifacts may be expected in patients laying down during scanning.
The diagnostic efficacy of (3D) cephalometric landmarks was the topic of 3 SRs73,75,79 The majority of the studies included had a moderate level of evidence according to the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool. The authors highlighted the need for standardized methodology79 and improvement in the reliability of landmarks.75 Digital linear dental measurements performed on models generated from CBCT images were shown to be accurate and reliable in two SRs.37,58
Due to the lack of diagnostic studies, one SR did not find sufficient accuracy and reliability of CBCT for diagnosing transverse deficiencies of the maxilla,44 whereas CBCT has proven to be reliable for comparing hard tissue changes by image superimposition,24 and accurate for detecting alveolar bone alterations caused by orthodontic tooth movement.78
In 2019, one SR recognized CBCT as a remarkable tool for some orthodontic tasks in a pediatric population. However, this study pointed out a lack of evidence for both CBCT optimization and justification in this population.72
CBCT imaging has been demonstrated to be a reliable, reproductible and accurate tool for a few orthodontic applications. Further studies reporting levels 3 to 6 of efficacy are still lacking. Moreover, there is not enough research-based evidence on 3D cephalometric analyses for clinical use. The limited number of tested CBCT models (Table 1) may be related to the need for using a large FOV for many orthodontic purposes.
Oral and maxillofacial surgery (including orthognathic surgery)
Ten SRs were related to orthognathic and oral maxillofacial surgery.28,45,59–62,80–83 In 2011, a scarcity of diagnostic accuracy studies was verified, specifically for the purpose of evaluating impacted third molars by using CBCT.61 Furthermore, in 2011, two other SRs were retrieved. One demonstrated the influence of various parameters, such as windowing settings, plane definition, number and thickness of cross-sections in bone grafts measurements.28 While the other SR showed the accuracy of CBCT-based fusion models used for orthodontic and orthognathic treatment planning and follow-up.83
In 2014, the applicability of 3D imaging was demonstrated for assessing hard and soft tissues in patients with cleft-lip and/or palate.82 Three years later, one SR showed that CBCT could be considered an accurate and reliable tool to assess anatomical changes, followed by surgically assisted rapid palatal expansion. However, there was no consensus on dental and skeletal landmarks.60
In 2019, one SR concluded that additional analysis of CBCT images did not have the potential to change preoperative planning and the surgical approach to mandibular third molar extraction.59 In line with this previous study, another SR that included randomized clinical trials, showed that CBCT evaluation had no impact on the reduction of temporary paresthesia after third molar extraction or preventing inferior alveolar nerve injury, and therefore, should not be considered as a routine imaging method for this task considering the higher radiation dose compared to panoramic imaging.80 Nevertheless, the cited SR highlighted that the potential benefit of CBCT over panoramic radiograph was assessed for only one of the possible post-operative complications, and no inferences could be drawn about the other types (e.g., trismus). Based on the 6-level efficacy model, another SR demonstrated that the localization of impacted maxillary canines was more reliable and accurate when CBCT images are used (level 2 of efficacy).45
In regards to the use of CBCT for condyle assessment, two SRs were retrieved, both dated 2020.62,81 In one SR, different methods for assessing condylar remodeling (i.e., image registration, condyle segmentation, and analysis protocols) were discussed,62 whereas another SR showed that each method had its advantages and disadvantages, especially as regards the question of being time-consuming. Although the semi-automatic segmentation method was shown to be highly reliable, there were few studies to allow conclusive statements to be made on its accuracy.81
Therefore, CBCT has been demonstrated to be a reliable and accurate tool for several surgical procedures. Nevertheless, there is still not enough evidence to allow the indication of CBCT for all surgical cases; and there is a scarcity of evidence of the benefits of CBCT at the last levels (patient outcome and societal efficacy levels). In addition, based on the selected SRs, only 10 CBCT models were investigated (Table 1).
Pathology
Three SRs with an approach to the field of pathology were identified.23,84,85 One review indicated that radiomorphometric indices and CBCT-derived radiographic density should be promising tools for differentiating individuals with osteoporosis from individuals with normal bone mineral density, however, the review also pointed out the scarcity of studies on this topic.23
Considering the inconsistency of imaging techniques in the detection of bone invasion in oral cancer patients, the aim of two SRs (from 2018 and 2019) was to quantify CBCT accuracy for this purpose.84,85 Both SRs demonstrated high diagnostic accuracy of CBCT in detecting bone invasion in patients with oral cancer. However, there is still a lack of studies on the detection of bone marrow invasion in patients with oral cancer.85
Paediatric dentistry
One SR was dedicated to the application of CBCT in paediatric dentistry, with an overall focus on indications and contra indications of CBCT relative to its diagnostic efficacy.31 In general, CBCT could be advantageous for the localization of dental structures and surgical planning in the paediatric population. A relevant limitation was the almost complete absence of in vivo studies of the paediatric population to be included for analysis, and therefore, it was necessary to include ex vivo studies as well. Moreover, considering the six-level model of efficacy, no studies were found for assessing patient outcome efficacy.
Periodontology
Ten SR were found related to the applicability of CBCT in periodontology.25,26,32,33,42,51–53,86,87 In 2016, a low level of evidence was found regarding the accuracy and precision of CBCT for the measurement of periodontal defects.86 In the same year, another SR revealed that there was no scientific evidence to justify the use of CBCT for the diagnosis and/or treatment planning of infrabony and furcation defects.42 Furthermore, no studies were found to address the therapeutic and patient outcome efficacy data (levels 4 and 5). Another SR from 2016 that included few studies, showed limited evidence for CBCT assessment of horizontal and angular bone loss, and furcation involvement.51 In 2017, another SR reinforced this limitation.26
Two years later, an SR showed the superiority of CBCT images for assessing periodontal structures and pathologies when compared with other imaging modalities 87 while another showed no difference between in situ and CBCT measurements of periodontal bone defects.52 In the same year, an SR demonstrated that CBCT was a valuable tool in periodontal surgery, especially considering regenerative surgeries and maxillary molar furcation therapy, with the studies included presenting a low risk of bias.32
Recently, one SR and meta-analysis stated that measurements of bone height and thickness made on CBCT images did not differ from gold-standard references found in both in vivo and in vitro studies.53 In 2020, two SRs were published showing an increased level of evidence for the use of CBCT in the detection of periodontal defects25 and the benefits of CBCT in periodontal therapy.33
Therefore, there is scientific evidence for the use of CBCT for some periodontal procedures, including bone measurement and periodontal surgical planning. There are a few studies in the highest levels of efficacy that have been published in the field of periodontology, nevertheless, further studies are recommended.33
TMJ imaging
Four SRs related to CBCT and TMJ imaging were found.19,20,38,46 In 2008, an SR pointed out the potential benefits of CBCT when compared with other imaging modalities (e.g., helical CT) for assessing TMJ and diagnosis of erosions and osteophytes.88 In 2016, another SR (with meta-analysis) confirmed the high diagnostic accuracy of CBCT for the detection of bony changes in the TMJ.20
In the same year, a SR with only three studies, including 12 patients, verified the applicability of image registration (using MRI, CT, and CBCT) for TMJ assessment.19 The small amount of data precluded robust conclusions, but a tendency towards a higher degree of accuracy could be noted, for diagnosing erosions and osteophytes in the TMJ when different imaging techniques were combined.19
A more recent study indicated CBCT for the diagnosis of degenerative disorders, with an emphasis on progression of the disease over time. However, CBCT may not be used as a screening method, due to its low specificity.38 The low number of studies and CBCT models tested (Table 1) suggested limited evidence for CBCT use in TMJ assessment.
Radiology – Technical parameters
Nine SRs were dedicated to oral radiology and the technical parameters of CBCT.4,21,22,34,39,54,63,88,89 In 2009, a review of the general literature on CBCT was performed.34 Out of the 176 articles initially selected, 86 dealt with clinical applications of CBCT imaging in the oral and maxillofacial field, 65 were related to technique, 16 articles were related to radiation dose, and 26 were article summaries. At that time, the evidence-based use of CBCT was not possible. There was a lack of evidence regarding radiation dose, inconsistencies related to the terminology, settings, and technical properties of the devices.
In 2013, an SR with ex vivo studies noted a tendency towards the appearance of more accurate results for diagnosis when smaller voxel sizes were selected (i.e., higher resolution), however no general protocol for CBCT examination could be defined.89
Three SRs were performed with regard to radiation dose.21,22,88 The first dated from 2015, in which a broader variety of effective dose data among CBCT devices were described, considering different measurement methods and scanning protocols.21 A poor description of scanning protocols throughout the studies included was highlighted as being a limitation. Later on, one study showed that it was possible to optimize CBCT imaging by reducing kilovoltage, tube current, and/or exposure time product without a negative impact on diagnostic accuracy.88 Nonetheless, these results may differ among CBCT devices and diagnostic tasks. The third SR demonstrated that patient-related factors and technical parameters could reduce effective doses in CBCT.22
The increasing use of CBCT in parallel with the growing amount of published data on this topic has allowed the development of evidence-based guidelines over the course of the years. In 2015, an SR identified all published guidelines for clinical use of CBCT and objectively appraised their quality by using the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument. The quality of publications was frequently low and lacked evidence of adequate methodology. There was broad agreement between publications on clinical use of CBCT.4
Motion artifacts in CBCT images were the aim of one SR in 2016.63 The average incidence of patient movement and the pattern of the artifacts generated were described in in vivo studies. However, the characteristics of patient movements and their prevalence could not be specified.
In the following year, an SR was conducted on quality assurance phantoms for CBCT imaging.54 Twenty-five phantoms were described in the literature, of which only two fulfilled the possibility of evaluating the most relevant parameters. The authors recommended the development of a phantom capable of measuring all parameters, with one exposure, and selecting a small field of view.
Recently an SR assessed superimposition techniques of 3D volumes with the purpose of evaluating morphological changes in the craniofacial skeletal structures.39 Landmark-based superimposition seems to be inferior to the voxel-based and surface-based techniques. However, due to the lack of studies and high heterogeneity among them, no clear recommendations could be given.
Considering the number of technical studies in dentomaxillofacial radiology, this was the specialty with the highest number of CBCT models tested (Table 1). However, it must be emphasized that only few devices were mentioned in the SRs selected, when compared with the huge number and variety of models available on the market,3 and the fact that technical outcomes are CBCT model dependent.
Discussion
An appraisal of the scientific evidence of CBCT was performed, based on a critical review of the SRs published on this topic. In total, 75 SRs were selected for this purpose. Although this article demonstrated the contribution of CBCT to several specialties of dentistry, the majority of studies addressed the clinical applicability and diagnostic accuracy of this imaging modality, level 2 of efficacy according to Fryback and Thornbury.13 A significant number of SR articles were observed from 2014 onwards, probably related to the increasing number of new CBCT models and data provided by primary studies. However, only few models were mentioned in the selected SRs. Within the limitations of our method, it would appear that some models available on the market have not been sufficiently, or even ever been investigated for many tasks. Therefore, studies with the aim of achieving higher levels of diagnostic efficacy and including a higher number of CBCT models are highly recommended.
This approach to appraise scientific evidence was adopted in order to limit the number of studies selected, and at the same time, provide a high level of evidence on this topic. Some of the steps proposed by Smith et al. (2011)15 for compiling an SR of SRs could be followed in the present appraisal, however, in order to strictly follow their methodology, the authors would have needed to narrow the research question to include only one clinical application, or assessed one outcome. However, given the broad scope of the theme and heterogeneity of SRs with regard to CBCT, the authors opted to perform an appraisal of the scientific evidence on CBCT that covered all aspects related to this imaging modality in the different specialties of dentistry.
The primary studies included in the SRs reviewed in the present study, had heterogeneous methodological designs and focused mainly on levels 1 and 2 of the six-tiered efficacy-model.13 In line with this model, CBCT should be further investigated, not only to confirm its contribution to diagnosis, but also to assess its capacity to influence decisions on patient therapy, increase the chance of favorable treatment outcomes, and maintain a beneficial cost/benefit ratio to society as a whole.12 In addition, the limitations associated with metal and patient-related artefacts should be critically considered, because the primary studies included in these SRs usually were ex vivo studies.
The high and increasing number of level two articles may be related to the enormous challenges involved in designing studies comprising levels 3 to 6. Furthermore, level two studies are of more interest, as they provide guidelines on protocols for the use of CBCT. In 2015, an SR was performed to objectively assess the quality of available guidelines on the clinical use of CBCT.4 Although the development of guidelines should be defined on evidence-based methods, the reporting of CBCT guidelines was often poorly presented at that time. The authors stated that objective methods based upon SRs of the literature were promoted, based on the premise that they had the best chance of avoiding the influence of individual opinion and bias. As this aforementioned study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for SR and meta-analysis, it was included in the present appraisal of CBCT scientific evidence. However, an update of the clinical guidelines for the use of CBCT is needed, considering the evidence published since 2015.
Another common limitation of primary studies pointed out by the SRs was the poor reporting of the CBCT protocols used. As previously demonstrated,3 CBCT devices have a wide range of technical parameters that affect image quality, and scientific evidence cannot simply be extrapolated from one CBCT to another. Therefore, in future studies, an effort should be made to describe the full protocol used. This would allow professionals to make more conclusive statements about the benefits of using different protocols for image acquisition in the different tasks and strengthen future guidelines on the use of CBCT. Although the aim of several primary studies was to study the technical parameters of CBCT, this aim was not constantly the motivation for performing the SRs.
Although this strategy was successful for limiting the amount of data analysed, the selection of only SRs had limitations. SRs have the primary function of systematically synthesizing the data present in the literature. Although traditionally present at the top of the pyramid of evidence, this classification can be questioned, and this type of study may have its own level depending on the inclusion criterion. It could be argued that syntheses are too varied to be confined to only one level. Syntheses of observational studies are unlikely to be equivalent to syntheses of randomized clinical trials or syntheses of multiple guidelines on the same topic.90
Some relevant topics within the specialties of dentistry may not have been covered in our review, as they have not yet been addressed in SRs. Moreover, the applications of CBCT are not restricted to oral health care; for example, applications such as radiation biology, ears, nose and throat, and ophthalmology were excluded. Furthermore, CBCT was used in many reviews as a tool for measuring or achieving different purposes, and was considered the gold/reference-standard. However, as these SRs did not exactly evaluate the scientific evidence of the imaging method itself (i.e., CBCT), they were not included in the present SR.
In conclusion, over the course of 20 years, SRs related to CBCT for all the specialties of dentistry have been published, with a vast majority of studies at levels 1 and 2 of diagnostic efficacy. Not all models available on the market were mentioned in the SRs. Therefore, studies with the aim of achieving the top levels of diagnostic as well as treatment efficacy are recommended. In any case, one cannot simply extrapolate in vitro results to the clinical setting. Also, considering the wide variety of CBCT devices and protocols, reported results should not be overstated or generalized, as outcomes may often refer to specific CBCT devices and protocols.
Footnotes
Acknowledgment: The authors declare no conflict of interest.
Contributor Information
Hugo Gaêta-Araujo, Email: hugogaeta@hotmail.com.
André Ferreira Leite, Email: andreleite@unb.br.
Karla de Faria Vasconcelos, Email: karlafav13@gmail.com.
Reinhilde Jacobs, Email: reinhilde.jacobs@kuleuven.be.
REFERENCES
- 1.Kau CH, Božič M, English J, Lee R, Bussa H, Ellis RK. Cone-Beam computed tomography of the maxillofacial region-an update. Int. J. Med. Robotics Comput. Assist. Surg. 2009; 5: 366–80. doi: 10.1002/rcs.279 [DOI] [PubMed] [Google Scholar]
- 2.Nemtoi A, Czink C, Haba D, Gahleitner A. Cone beam CT: a current overview of devices. Dentomaxillofac Radiol 2013; 42: 20120443. doi: 10.1259/dmfr.20120443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaêta-Araujo H, Alzoubi T. Vasconcelos K de F, Orhan K, Pauwels R, Casselman JW, et al. cone beam computed tomography in dentomaxillofacial radiology: a two-decade overview. Dentomaxillofacial Radiol 2020; 49: 20200145: 20200145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horner K, O'Malley L, Taylor K, Glenny A-M. Guidelines for clinical use of CBCT: a review. Dentomaxillofac Radiol 2015; 44: 20140225. doi: 10.1259/dmfr.20140225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scarfe WC. Clinical recommendations regarding use of cone beam computed tomography in orthodontic treatment. position statement by the American Academy of oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: 238–57. [DOI] [PubMed] [Google Scholar]
- 6.Hayashi T, Arai Y, Chikui T, Hayashi-Sakai S, Honda K, Indo H, Hayashi S, Kazuya S, Hiroko H, et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiol 2018; 34: 89–104. doi: 10.1007/s11282-018-0314-3 [DOI] [PubMed] [Google Scholar]
- 7.Jacobs R, Salmon B, Codari M, Hassan B, Bornstein MM. Cone beam computed tomography in implant dentistry: recommendations for clinical use. BMC Oral Health 2018; 18: 88. doi: 10.1186/s12903-018-0523-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matzen LH, Berkhout E. Cone beam CT imaging of the mandibular third molar: a position paper prepared by the European Academy of DentoMaxilloFacial radiology (EADMFR. Dentomaxillofac Radiol 2019; 48: 20190039. doi: 10.1259/dmfr.20190039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oenning AC, Jacobs R, Pauwels R, Stratis A, Hedesiu M, Salmon B. Cone-Beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr Radiol 2018; 48: 308–16. doi: 10.1007/s00247-017-4012-9 [DOI] [PubMed] [Google Scholar]
- 10.Patel S, Brown J, Semper M, Abella F, Mannocci F. European Society of Endodontology position statement: use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int Endod J 2019; 52: 1675–8. [DOI] [PubMed] [Google Scholar]
- 11. Radiation Protection 172: Cone Beam CT for Dental and Maxillofacial Radiology - Evidence-based Guidelines. Off Off Publ Eur Communities 2012; 156. [Google Scholar]
- 12.Geist JR. The efficacy of diagnostic imaging should guide oral and maxillofacial radiology research. Oral Surg Oral Med Oral Pathol Oral Radiol 2017; 124: 211–3. doi: 10.1016/j.oooo.2017.06.001 [DOI] [PubMed] [Google Scholar]
- 13.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: 10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 14.OCEBM Levels of Evidence Working Group The Oxford 2011 Levels of Evidence” [Internet. Oxford Centre for Evidence-Based Medicine. [Google Scholar]
- 15.Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 2011; 11: 15. doi: 10.1186/1471-2288-11-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baageel T, Allah E, Bakalka G, Jadu F, Yamany I, Jan A, et al. Vertical root fracture: biological effects and accuracy of diagnostic imaging methods. J Int Soc Prevent Communit Dent 2016; 6: 93. doi: 10.4103/2231-0762.189735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fokas G, Vaughn VM, Scarfe WC, Bornstein MM. Accuracy of linear measurements on CBCT images related to presurgical implant treatment planning: A systematic review. Clin Oral Implants Res 2018; 29(S16): 393–415. doi: 10.1111/clr.13142 [DOI] [PubMed] [Google Scholar]
- 18.Guijarro-Martínez R, Swennen GRJ. Cone-Beam computerized tomography imaging and analysis of the upper airway: a systematic review of the literature. Int J Oral Maxillofac Surg 2011; 40: 1227–37. doi: 10.1016/j.ijom.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 19.Al-Saleh MAQ, Alsufyani NA, Saltaji H, Jaremko JL, Major PW. Mri and CBCT image registration of temporomandibular joint: a systematic review. J Otolaryngol Head Neck Surg 2016; 45: 30. doi: 10.1186/s40463-016-0144-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma R-H, Yin S, Li G. The detection accuracy of cone beam CT for osseous defects of the temporomandibular joint: a systematic review and meta-analysis. Sci Rep 2016; 6: 34714. doi: 10.1038/srep34714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Okshi A, Lindh C, Salé H, Gunnarsson M, Rohlin M. Effective dose of cone beam CT (CBCT) of the facial skeleton: a systematic review. Br J Radiol 2015; 88: 20140658. doi: 10.1259/bjr.20140658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.da Silva Moura W, Chiqueto K, Pithon GM, Neves LS, Castro R, Henriques JFC. Factors influencing the effective dose associated with CBCT: a systematic review. Clin Oral Investig 2019; 23: 1319–30. doi: 10.1007/s00784-018-2561-4 [DOI] [PubMed] [Google Scholar]
- 23.Guerra ENS, Almeida FT, Bezerra FV, Figueiredo PTDS, Silva MAG, De Luca Canto G, et al. Capability of CBCT to identify patients with low bone mineral density: a systematic review. Dentomaxillofac Radiol 2017; 46: 20160475. doi: 10.1259/dmfr.20160475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ponce-Garcia C, Lagravere-Vich M, Cevidanes LHS, de Olivera Ruellas AC, Carey J, Flores-Mir C. Reliability of three-dimensional anterior cranial base superimposition methods for assessment of overall hard tissue changes: a systematic review. Angle Orthod 2018; 88: 233–45. doi: 10.2319/071217-468.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walter C, Schmidt JC, Rinne CA, Mendes S, Dula K, Sculean A. Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: systematic review update. Clin Oral Investig 2020; 24: 2943–58. doi: 10.1007/s00784-020-03326-0 [DOI] [PubMed] [Google Scholar]
- 26.Kim DM, Bassir SH. When is cone-beam computed tomography imaging appropriate for diagnostic inquiry in the management of inflammatory periodontitis? an American Academy of Periodontology best evidence review. J Periodontol 2017; 88: 978–98. doi: 10.1902/jop.2017.160505 [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman JN, Lee J, Pliska BT. Reliability of upper pharyngeal airway assessment using dental CBCT: a systematic review. Eur J Orthod 2017; 39: cjw079: cjw079. [DOI] [PubMed] [Google Scholar]
- 28.Spin-Neto R, Marcantonio E, Gotfredsen E, Wenzel A. Exploring CBCT-Based DICOM files. A systematic review on the properties of images used to evaluate maxillofacial bone grafts. J Digit Imaging 2011; 24: 959–66. doi: 10.1007/s10278-011-9377-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kruse C, Spin-Neto R, Wenzel A, Kirkevang L-L. Cone beam computed tomography and periapical lesions: a systematic review analysing studies on diagnostic efficacy by a hierarchical model. Int Endod J 2015; 48: 815–28. doi: 10.1111/iej.12388 [DOI] [PubMed] [Google Scholar]
- 30.Borges CC, Estrela C. Decurcio D de a, PÉcora JD, Sousa-Neto MD, Rossi-Fedele G. cone-beam and micro-computed tomography for the assessment of root canal morphology: a systematic review. Braz Oral Res 2020; 34: e056: e056. [DOI] [PubMed] [Google Scholar]
- 31.Horner K, Barry S, Dave M, Dixon C, Littlewood A, Pang CL. Diagnostic efficacy of cone beam computed tomography in paediatric dentistry: a systematic review. Eur Arch Paediatr Dent 2019;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woelber J, Fleiner J, Rau J, Ratka-Krüger P, Hannig C, et al. Accuracy and usefulness of CBCT in Periodontology: a systematic review of the literature. Int J Periodontics Restorative Dent 2018; 38: 289–97. doi: 10.11607/prd.2751 [DOI] [PubMed] [Google Scholar]
- 33.Assiri H, Dawasaz AA, Alahmari A, Asiri Z. Cone beam computed tomography (CBCT) in periodontal diseases: a systematic review based on the efficacy model. BMC Oral Health 2020; 20: 191. doi: 10.1186/s12903-020-01106-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Vos W, Casselman J, Swennen GRJ. Cone-Beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg 2009; 38: 609–25. doi: 10.1016/j.ijom.2009.02.028 [DOI] [PubMed] [Google Scholar]
- 35.Corbella S, Del Fabbro M, Tamse A, Rosen E, Tsesis I, Taschieri S. Cone beam computed tomography for the diagnosis of vertical root fractures: a systematic review of the literature and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 118: 593–602. doi: 10.1016/j.oooo.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 36.Talwar S, Utneja S, Nawal RR, Kaushik A, Srivastava D, Oberoy SS. Role of Cone-beam Computed Tomography in Diagnosis of Vertical Root Fractures: A Systematic Review and Meta-analysis. J Endod 2016; 42: 12–24. doi: 10.1016/j.joen.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 37.Luu NS, Nikolcheva LG, Retrouvey J-MM, Flores-Mir C, El-Bialy T, Carey JP. Linear measurements using virtual study models: a systematic review. Angle Orthod 2012; 82: 1098–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hilgenberg-Sydney PB, Bonotto DV, Stechman-Neto J, Zwir LF, Pachêco-Pereira C, Canto GDL, De Luca Canto G, et al. Diagnostic validity of CT to assess degenerative temporomandibular joint disease: a systematic review. Dentomaxillofac Radiol 2018; 47: 20170389. doi: 10.1259/dmfr.20170389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mai DD-P, Stucki S, Gkantidis N. Assessment of methods used for 3-dimensional superimposition of craniofacial skeletal structures: a systematic review. PeerJ 2020; 8: e9263. doi: 10.7717/peerj.9263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pelekos G, Acharya A, Tonetti MS, Bornstein MM. Diagnostic performance of cone beam computed tomography in assessing peri-implant bone loss: a systematic review. Clin Oral Implants Res 2018; 29: 443–64. doi: 10.1111/clr.13143 [DOI] [PubMed] [Google Scholar]
- 41.Long H, Zhou Y, Ye N, Liao L, Jian F, Wang Y, et al. Diagnostic accuracy of CBCT for tooth fractures: a meta-analysis. J Dent 2014; 42: 240–8. doi: 10.1016/j.jdent.2013.11.024 [DOI] [PubMed] [Google Scholar]
- 42.Nikolic-Jakoba N, Spin-Neto R, Wenzel A. Cone-Beam computed tomography for detection of Intrabony and Furcation defects: a systematic review based on a hierarchical model for diagnostic efficacy. J Periodontol 2016; 87: 630–44. doi: 10.1902/jop.2016.150636 [DOI] [PubMed] [Google Scholar]
- 43.Alsufyani NA, Flores-Mir C, Major PW. Three-Dimensional segmentation of the upper airway using cone beam CT: a systematic review. Dentomaxillofac Radiol 2012; 41: 276–84. doi: 10.1259/dmfr/79433138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sawchuk D, Currie K, Vich ML, Palomo JM, Flores-Mir C. Diagnostic methods for assessing maxillary skeletal and dental transverse deficiencies: a systematic review. Korean J Orthod 2016; 46: 331–42. doi: 10.4041/kjod.2016.46.5.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eslami E, Barkhordar H, Abramovitch K, Kim J, Masoud MI. Cone-Beam computed tomography vs conventional radiography in visualization of maxillary impacted-canine localization: a systematic review of comparative studies. American Journal of Orthodontics and Dentofacial Orthopedics 2017; 151: 248–58. doi: 10.1016/j.ajodo.2016.07.018 [DOI] [PubMed] [Google Scholar]
- 46.Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol 2008; 37: 63–71. doi: 10.1259/dmfr/16932758 [DOI] [PubMed] [Google Scholar]
- 47.Chang E, Lam E, Shah P, Azarpazhooh A. Cone-Beam computed tomography for detecting vertical root fractures in Endodontically treated teeth: a systematic review. J Endod 2016; 42: 177–85. doi: 10.1016/j.joen.2015.10.005 [DOI] [PubMed] [Google Scholar]
- 48.Petersson A, Axelsson S, Davidson T, Frisk F, Hakeberg M, Kvist T, et al. Radiological diagnosis of periapical bone tissue lesions in endodontics: a systematic review. Int Endod J 2012; 45: 783–801. doi: 10.1111/j.1365-2591.2012.02034.x [DOI] [PubMed] [Google Scholar]
- 49.Antony DP, Thomas T, Nivedhitha MS. Two-Dimensional periapical, panoramic radiography versus three-dimensional cone-beam computed tomography in the detection of periapical lesion after endodontic treatment: a systematic review. Cureus 2020; 12. doi: 10.7759/cureus.7736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bohner LOL, Mukai E, Oderich E, Porporatti AL, Pacheco-Pereira C, Tortamano P, et al. Comparative analysis of imaging techniques for diagnostic accuracy of peri-implant bone defects: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2017; 124: 432–40. doi: 10.1016/j.oooo.2017.06.119 [DOI] [PubMed] [Google Scholar]
- 51.Walter C, Schmidt JC, Dula K, Sculean A. Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: a systematic review. Quintessence Int 2016; 47: 25–37. [DOI] [PubMed] [Google Scholar]
- 52.Haas LF, Zimmermann GS, De Luca Canto G, Flores-Mir C, Corrêa M. Precision of cone beam CT to assess periodontal bone defects: a systematic review and meta-analysis. Dentomaxillofac Radiol 2018; 47: 20170084. doi: 10.1259/dmfr.20170084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Y, Deng S, Mei L, Li J, Qi M, Su S, et al. Accuracy of alveolar bone height and thickness measurements in cone beam computed tomography: a systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2019; 128: 667–79. doi: 10.1016/j.oooo.2019.05.010 [DOI] [PubMed] [Google Scholar]
- 54.de Oliveira MVL, Wenzel A, Campos PSF, Spin-Neto R. Quality assurance phantoms for cone beam computed tomography: a systematic literature review. Dentomaxillofac Radiol 2017; 46: 20160329. doi: 10.1259/dmfr.20160329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jacobs R, Vranckx M, Vanderstuyft T, Quirynen M, Salmon B. Cbct vs other imaging modalities to assess peri-implant bone and diagnose complications: a systematic review. Eur J Oral Implantol 2018; 11(Suppl 1): 77–92. [PubMed] [Google Scholar]
- 56.Salineiro FCS, Kobayashi-Velasco S, Braga MM, Cavalcanti MGP. Radiographic diagnosis of root fractures: a systematic review, meta-analyses and sources of heterogeneity. Dentomaxillofac Radiol 2017; 46: 20170400. doi: 10.1259/dmfr.20170400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ma RH, Ge ZP, Li G. Detection accuracy of root fractures in cone-beam computed tomography images: a systematic review and meta-analysis. Int Endod J 2016; 49: 646–54. doi: 10.1111/iej.12490 [DOI] [PubMed] [Google Scholar]
- 58.Ferreira JB, Christovam IO, Alencar DS, da Motta AFJ, Mattos CT, Cury-Saramago A. Accuracy and reproducibility of dental measurements on tomographic digital models: a systematic review and meta-analysis. Dentomaxillofac Radiol 2017; 46: 20160455. doi: 10.1259/dmfr.20160455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Araujo G de TT, Peralta-Mamani M, Silva a de FM dA, Rubira CMMFF, Honório HM, Rubira-Bullen IRFRF. Influence of cone beam computed tomography versus panoramic radiography on the surgical technique of third molar removal: a systematic review. Int J Oral Maxillofac Surg 2019; 48: 1340–7. [DOI] [PubMed] [Google Scholar]
- 60.Camps-Perepérez I, Guijarro-Martínez R, Peiró-Guijarro MA, Hernández-Alfaro F. The value of cone beam computed tomography imaging in surgically assisted rapid palatal expansion: a systematic review of the literature. Int J Oral Maxillofac Surg 2017; 46: 827–38. doi: 10.1016/j.ijom.2017.01.017 [DOI] [PubMed] [Google Scholar]
- 61.Guerrero ME, Shahbazian M, Elsiena Bekkering G, Nackaerts O, Jacobs R, Horner K. The diagnostic efficacy of cone beam CT for impacted teeth and associated features: a systematic review. J Oral Rehabil 2011; 38: 208–16. doi: 10.1111/j.1365-2842.2010.02141.x [DOI] [PubMed] [Google Scholar]
- 62.Verhelst PJ, Verstraete L, Shaheen E, Shujaat S, Darche V, Jacobs R, et al. Three-Dimensional cone beam computed tomography analysis protocols for condylar remodelling following orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg 2020; 49: 207–17. doi: 10.1016/j.ijom.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 63.Spin-Neto R, Wenzel A. Patient movement and motion artefacts in cone beam computed tomography of the dentomaxillofacial region: a systematic literature review. Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 121: 425–33. doi: 10.1016/j.oooo.2015.11.019 [DOI] [PubMed] [Google Scholar]
- 64.Leonardi Dutra K, Haas L, Porporatti AL, Flores-Mir C, Nascimento Santos J, Mezzomo LA, et al. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J Endod 2016; 42: 356–64. doi: 10.1016/j.joen.2015.12.015 [DOI] [PubMed] [Google Scholar]
- 65.Aminoshariae A, Kulild JC, Syed A. Cone-Beam computed tomography compared with intraoral radiographic lesions in endodontic outcome studies: a systematic review. J Endod 2018; 44: 1626–31. doi: 10.1016/j.joen.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 66.Sholapurkar A, Amin J, Lines J, Milosevic MP, Park A. Comparison of accuracy and reliability of working length determination using cone beam computed tomography and electronic apex locator: a systematic review. J Contemp Dent Pract 2019; 20: 1118–23. doi: 10.5005/jp-journals-10024-2651 [DOI] [PubMed] [Google Scholar]
- 67.Yi J, Sun Y, Li Y, Li C, Li X, Zhao Z. Cone-Beam computed tomography versus periapical radiograph for diagnosing external root resorption: a systematic review and meta-analysis. Angle Orthod 2017; 87: 328–37. doi: 10.2319/061916-481.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rosen E, Taschieri S, Del Fabbro M, Beitlitum I, Tsesis I. The diagnostic efficacy of cone-beam computed tomography in Endodontics: a systematic review and analysis by a hierarchical model of efficacy. J Endod 2015; 41: 1008–14. doi: 10.1016/j.joen.2015.02.021 [DOI] [PubMed] [Google Scholar]
- 69.Bornstein M, Scarfe W, Vaughn V, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants 2014; 29(Supplement): 55–77. doi: 10.11607/jomi.2014suppl.g1.4 [DOI] [PubMed] [Google Scholar]
- 70.Kim M-J, Lee S-S, Choi M, Yong HS, Lee C, Kim J-E, et al. Developing evidence-based clinical imaging guidelines of Justification for radiographic examination after dental implant installation. BMC Med Imaging 2020; 20: 102. doi: 10.1186/s12880-020-00501-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim M-J, Lee S-S, Choi M, Ha EJ, Lee C, Kim J-E, et al. Development of an evidence-based clinical imaging diagnostic guideline for implant planning: joint recommendations of the Korean Academy of oral and maxillofacial radiology and national evidence-based healthcare collaborating agency. Imaging Sci Dent 2020; 50: 45–52. doi: 10.5624/isd.2020.50.1.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.De Grauwe A, Ayaz I, Shujaat S, Dimitrov S, Gbadegbegnon L, Vande Vannet B, et al. Cbct in orthodontics: a systematic review on Justification of CBCT in a paediatric population prior to orthodontic treatment. Eur J Orthod 2019; 41: 381–9. doi: 10.1093/ejo/cjy066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sam A, Currie K, Oh H, Flores-Mir C, Lagravére-Vich M. Reliability of different three-dimensional cephalometric landmarks in cone-beam computed tomography: a systematic review. Angle Orthod 2019; 89: 317–32. doi: 10.2319/042018-302.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Vlijmen OJC, Kuijpers MAR, Bergé SJ, Schols JGJH, Maal TJJ, Breuning H, et al. Evidence supporting the use of cone-beam computed tomography in orthodontics. The Journal of the American Dental Association 2012; 143: 241–52. doi: 10.14219/jada.archive.2012.0148 [DOI] [PubMed] [Google Scholar]
- 75.Lisboa CdeO, Masterson D, Motta AFJ, Motta AT. Reliability and reproducibility of three-dimensional cephalometric landmarks using CBCT: a systematic review. J. Appl. Oral Sci. 2015; 23: 112–9. doi: 10.1590/1678-775720140336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Di Carlo G, Saccucci M, Ierardo G, Luzzi V, Occasi F, Zicari AM, et al. Rapid maxillary expansion and upper airway morphology: a systematic review on the role of cone beam computed tomography. Biomed Res Int 2017; 2017: 1–10. doi: 10.1155/2017/5460429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eslami E, Katz ES, Baghdady M, Abramovitch K, Masoud MI. Are three-dimensional airway evaluations obtained through computed and cone-beam computed tomography scans predictable from lateral cephalograms? A systematic review of evidence. Angle Orthod 2017; 87: 159–67. doi: 10.2319/032516-243.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mandelaris GA, Neiva R, Chambrone L. Cone-Beam computed tomography and interdisciplinary Dentofacial therapy: an American Academy of Periodontology best evidence review focusing on risk assessment of the dentoalveolar bone changes influenced by tooth movement. J Periodontol 2017; 88: 960–77. doi: 10.1902/jop.2017.160781 [DOI] [PubMed] [Google Scholar]
- 79.Pittayapat P, Limchaichana-Bolstad N, Willems G, Jacobs R. Three-Dimensional cephalometric analysis in orthodontics: a systematic review. Orthod Craniofac Res 2014; 17: 69–91. doi: 10.1111/ocr.12034 [DOI] [PubMed] [Google Scholar]
- 80.Del Lhano NC, Ribeiro RA, Martins CC, Assis NMSP, Devito KL. Panoramic versus CBCT used to reduce inferior alveolar nerve paresthesia after third molar extractions: a systematic review and meta-analysis. Dentomaxillofac Radiol 2020; 49: 20190265. doi: 10.1259/dmfr.20190265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim JJ, Nam H, Kaipatur NR, Major PW, Flores-Mir C, Lagravere MO, et al. Reliability and accuracy of segmentation of mandibular condyles from different three-dimensional imaging modalities: a systematic review. Dentomaxillofac Radiol 2020; 49: 20190150. doi: 10.1259/dmfr.20190150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kuijpers MAR, Chiu Y-T, Nada RM, Carels CEL, Fudalej PS. Three-Dimensional imaging methods for quantitative analysis of facial soft tissues and skeletal morphology in patients with orofacial clefts: a systematic review.editor.PLoS One 2014; 9: e93442. doi: 10.1371/journal.pone.0093442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Plooij JM, Maal TJJ, Haers P, Borstlap WA, Kuijpers-Jagtman AM, Bergé SJ. Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review. Int J Oral Maxillofac Surg 2011; 40: 341–52. doi: 10.1016/j.ijom.2010.10.013 [DOI] [PubMed] [Google Scholar]
- 84.Bombeccari GP, Candotto V, Gianni AB, Carinci F, Spadari F, .Department of Biomedical, Surgical and Dental Sciences, Maxillo-Facial and Dental Unit, Fondazione Ca' Granda IRCCS Ospedale Maggiore Policlinico Milan, University of Milan, Italy . Accuracy of the cone beam computed tomography in the detection of bone invasion in patients with oral cancer: a systematic review. Eurasian J Med 2019; 51: 298–306. doi: 10.5152/eurasianjmed.2019.18101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Qiao X, Liu W, Cao Y, Miao C, Yang W, Su N, et al. Performance of different imaging techniques in the diagnosis of head and neck cancer mandibular invasion: a systematic review and meta-analysis. Oral Oncol 2018; 86: 150–64. doi: 10.1016/j.oraloncology.2018.09.024 [DOI] [PubMed] [Google Scholar]
- 86.Anter E, Zayet M, El-Dessouky S. Accuracy and precision of cone beam computed tomography in periodontal defects measurement (systematic review. J Indian Soc Periodontol 2016; 20: 235–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Choi IGG, Cortes ARG, Arita ES, Georgetti MAP. Comparison of conventional imaging techniques and CBCT for periodontal evaluation: a systematic review. Imaging Sci Dent 2018; 48: 79. doi: 10.5624/isd.2018.48.2.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Goulston R, Davies J, Horner K, Murphy F. Dose optimization by altering the operating potential and tube current exposure time product in dental cone beam CT: a systematic review. Dentomaxillofac Radiol 2016; 45: 20150254. doi: 10.1259/dmfr.20150254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Spin-Neto R, Gotfredsen E, Wenzel A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: a systematic review. J Digit Imaging 2013; 26: 813–20. doi: 10.1007/s10278-012-9562-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shaneyfelt T. Pyramids are guides not rules: the evolution of the evidence pyramid. Evid Based Med 2016; 21: 121–2. doi: 10.1136/ebmed-2016-110498 [DOI] [PubMed] [Google Scholar]