Abstract
Objectives:
The purpose of this pilot study was to evaluate the usefulness of magnetic resonance lymphography (MRL) with superparamagnetic iron oxide (SPIO) in sentinel lymph node (SLN) mapping of clinically N0 early oral cancer, and to conduct a comparative study of this MRL with CT lymphography (CTL).
Methods:
CTL and MRL were performed for SLN mapping before surgery for 20 patients with clinically N0 early oral cancer. The detection rate, number, and location of SLNs in CTL and MRL were evaluated. Furthermore, optimal scanning/imaging timing in MRL was examined.
Results:
SLNs were detected by CTL in 18 (90%) patients, and the total and mean number of SLN were 35 and 1.8, respectively. All SLNs could be detected 2 min and 3.5–5 min after contrast medium injection. In all patients, SLNs were detected by MRL at 10 min after SPIO injection, and the total and mean number of SLN was 53 and 2.7, respectively. MRL at 30 min after the injection showed additional 18 secondary lymph nodes.
Conclusion:
MRL with SPIO is safe and useful imaging for the detection of SLNs in clinically N0 early oral cancer, and the optimal imaging timing is 10 min after SPIO injection.
Keywords: early oral cancer, magnetic resonance lymphography, metastasis, sentinel lymph node, superparamagnetic iron oxide
Introduction
Cervical lymph node metastasis is an important prognostic factor in oral cancer. Because occult metastasis is found during observation after primary surgery in 20–30% of patients with N0 early oral cancer,1 some studies recommend prophylactic neck dissection (ND). Nonetheless, 70–80% of patients with early oral cancer who underwent ND may experience complications such as facial nerve paralysis or shoulder dysfunction. Therefore, the concept of the sentinel lymph node (SLN), which is the first lymph node to receive drainage from a primary tumor, has recently been applied in detecting early lymph node metastasis in oral cancer patients,1–12 and SLN biopsy (SLNB) has been performed to be less invasive than prophylactic ND. Although SLN detection using radioisotope (RI) tracers is commonly performed,4,5,8–14 RI confers hazards to the patient and staff and cannot be used in certain institutions due to restrictions regarding the handling and disposal of radioactive material.2,15 Furthermore, SLN detection is difficult when the SLN is close to the site of RI injection, due to shine-through artifacts.2 Another method for visualizing SLNs and lymphatics is CT lymphography (CTL), which does not require special equipment and has recently been applied in melanoma, breast, esophageal, gastric, and oral cancer.2,16–24 However, CTL cannot be performed for patients with iodine allergy to an iodinated contrast medium, and the use of CT has radiation exposure as with RI. Therefore, other method with nonradioactive and non-allergenic tracers for SLN mapping is required.15 Although interstitial magnetic resonance lymphography (MRL) with gadolinium or superparamagnetic iron oxide (SPIO) has recently been applied for SLN mapping of breast or esophageal cancer,15,25 there are few reports of interstitial MRL for SLN mapping of N0 early oral cancer.26,27 The purpose of this pilot study was to evaluate the usefulness of MRL with SPIO in SLN mapping of clinically N0 early oral cancer, and to conduct a comparative study of this MRL with CTL.
Methods and materials
Between January 2017 and December 2018, 20 early oral cancer patients without cervical lymph node metastasis were enrolled in our study. There were 12 males and 8 females with a median age of 61.1 (range, 23–86) years. The primary tumour site was the tongue in 19 of 20 patients, and only one patient had cancer of the floor of the mouth. In total, 13 patients had clinical T1 and 7 patients had clinical T2. All patients had primary cancer without prior surgery, chemotherapy and/or radiotherapy. Primary cancer and cervical lymph nodes before surgery were assessed using four modalities: enhanced-computed tomography (CT), magnetic resonance imaging (MRI), 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) and ultrasonography (US). The criteria for a diagnosis of N0 oral cancer at our institutions can be summarized as follows: (i) minimum axial diameter of the node <10 mm and no rim enhancement on enhanced CT; (ii) maximum standardized uptake <2.5 on PET/CT; and (iii) presence of hilar echoes on US. TNM staging was classified according to the Union for International Cancer Control staging system (eighth edition). This study was approved by the institutional review board of our university (No. B200500002) and was conducted according to the Declaration of Helsinki.
CTL was performed with a 128 multi-detector row CT scanner (Siemens SOMATOM Definition AS+; Siemens Healthcare GmbH, Erlangen, Germany) to detect SLNs 2 days before resection of the primary tumour and SLNB. Patients were placed in the supine position and CT scanning was performed with the following parameters: tube voltage of 80 kVp, 400 mAs, the helical thickness of 0.6 mm, the field of view of 220 mm, and rotation time of 1.0 s. First, non-contrast CT images of the oral cavity and neck were obtained. After local anaesthesia, a total of 2.0 ml of iopamidol (Iopamiron 300; Bayer Yakuhin Co., Ltd., Osaka, Japan) was injected submucosally into four points around the tumour with a 27-gauge needle, and the injected sites were massaged. CT scanning was performed in all patients at 2, 3.5, and 5 min after administration of iopamidol. SLNs were identified as the first enhancing lymph node in the lymphatic flow from the sites of injection of the contrast medium, and the CT images with three-dimensional (3D) reconstruction were analysed on the day of the procedure. The 3D reconstruction was performed using the cinematic volume rendering technique with syngo.via imaging software (Siemens Healthcare GmbH, Erlangen, Germany).
MRL was performed with a 3 Tesla MRI system (Discovery MR750w; GE Healthcare, Chicago, US) in the supine position the day before resection of the primary tumour and SLNB. Resovist® (FUJIFILM RI Farma Co., LTD., Kobayashi, Tokyo, Japan) was used as an SPIO agent, and it contains 540 mg ferucarbotran per millilitre (27.9 mg iron/ml), containing hydrophilic carboxydextran-covered SPIO particles. Iron oxide nanoparticles are incorporated into macrophages and other phagocytic cells, and have been used as “negative contrast agents”, that is, their active uptake by normal lymph nodes results in a homogeneous decrease in signal intensity on T2*-weighted images. After local anaesthesia, a total of 0.4 ml Resovist® (ferucarbotran) was injected submucosally for four-point around the tumour with a 27-gauge needle as same as CTL, and the injected sites were massaged. Imaging was performed 10 and 30 min after SPIO injection by some sequences; axial MERGE (Multiple Echo Recombined Gradient Echo) which is developed by GE Healthcare and is a spoiled T2*-weighted sequence and equipped with the option of 3D acquisition, axial T1-weighted, and T2-weighted MR images of FS (FatSat). After MRL, we analysed the MR images on the day of the procedure, and LNs with SPIO uptake from direct lymphatic drainage of the injection site were considered as SLNs.
The detection rate, number, and location of SLNs in CTL and MRL were evaluated by two observers. Furthermore, optimal scanning/imaging timing in MRL was examined.
Results
In CTL as well as MRL, each SLN mapping (the location and number) which were performed by two observers was in complete agreement.
SLNs were detected by CTL in 18 (90%) of the 20 patients (Figure 1). The number of SLNs was 0 in two patients (10%), 1 in six patients (30%), 2 in eight patients (40%), 3 in three patients (15%), and 4 in one patient (5%). The total number and the mean number of SLNs were 35 and 1.8, respectively. All SLNs could be detected 2 min and 3.5–5 min after contrast medium (iopamidol) injection.
Figure 1.
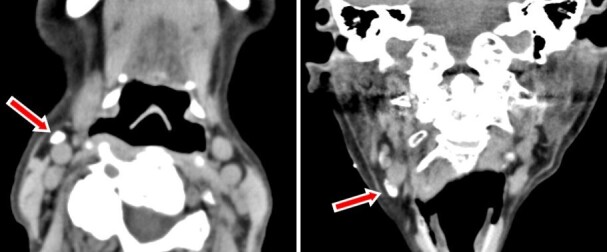
CT lymphography 2 min after iopamidol. A: Axial image, B: coronal image, Arrows indicate sentinel lymph node.
In all 20 patients (100%), SLNs were detected by MRL at 10 min after injection of ferucarbotran (Figure 2), and the total and mean number of SLNs was 53 and 2.7, respectively. MRL at 30 min after the injection showed additional 18 secondary lymph nodes. The number of SLNs was one in four patients (20%), two in six patients (30%), three in five patients (25%), four in four patients (20%), and 7 in one patient (5%).
Figure 2.
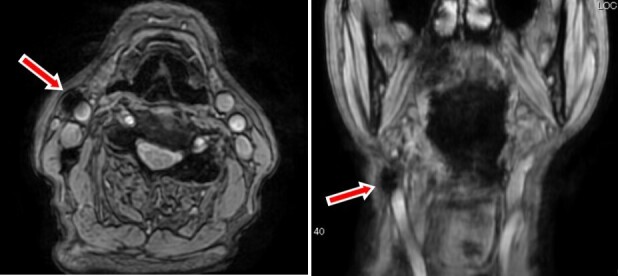
MR lymphography in a spoiled T2*-weighted sequence (Multiple Echo Recombined Gradient Echo) 10 min after ferucarbotran. A: Axial image, B: coronal image, Arrows indicate sentinel lymph node.
SLN location and the number of MRL and CTL in N0 early oral cancer patients were shown in Table 1. In both imaging, only one SLN (level IB) was located on the contralateral side. Although CTL showed two SLNs were lingual lymph nodes in two patients, MRL could not detect lingual lymph nodes for an artefact of ferucarbotran injected into the primary site. The other 33 of 35 SLNs enhanced by CTL could be detected by MRL.
Table 1.
SLN location and number of MRL and CTL in oral cancer patients
| SLN location | SLN number | |
|---|---|---|
| MRL | CTL | |
| IA | 2 | 1 |
| IB | 23 | 14 |
| IIA | 27 | 17 |
| IIB | 1 | 1 |
| Lingual lymph node | 0 | 2 |
CTL, computed tomography lymphography; MRL, magnetic resonance lymphography; SLN, sentinel lymph node
Discussion
Because occult cervical lymph node metastasis during observation after primary surgery is found in 20–30% of patients with N0 early oral cancer and commonly occurs at level I to III, supraomohyoid ND has been recommended.28,29 However, minimally invasive surgery such as SLNB is required to avoid the complications that can occur after ND, such as facial nerve paralysis. SLNB, which benefits patients without lymph node metastasis by avoiding unnecessary lymph node dissection, has been performed in the treatment of various cancers such as melanoma, breast and gastric cancer.16–22 SLNB using RI is a standard procedure and has been recently applied in oral cancer.9,10,14 However, the main disadvantages of RI method are radiation exposure to patients and physicians, and short half-life, availability, handling, and disposal of RI.30 It cannot be performed in hospitals that do not have the required equipment and systems, thereby preventing its widespread use.1 Therefore, preoperative mapping of SLNs without RI is required for the widespread application of SLNB and the reliable detection of SLNs.
As an alternative method for preoperative visualization of SLNs and lymphatics, CTL without requiring special equipment can be performed at many hospitals with conventional CT scanners and has recently been applied in melanoma, breast, esophageal and gastric cancer.16–21 CTL has clarified, with high resolution, the detailed arrangement of lymphatics along the route in various malignant tumours when visualizing multiple lymph nodes. This then helped determine whether or not these were secondary lymph nodes or lymph nodes from separate channels, thus facilitating more accurate SLN identification.19 Therefore, CTL without the shine-through effect is recommended for the accurate identification of SLNs and better topographical 3D orientation before SLNB,19 and the reported detection rate of SLNs is 99 to 100% in breast cancer [16–18]. However, the imaging protocol for CTL is not clear,2,23,24 because there are few reports of SLN mapping using CTL for N0 early oral cancer. In a study of CTL for SLN mapping in patients with N0 early tongue cancer, Honda et al2,24 injected 1.5 ml iopamidol (Iopamiron 370) into the peritumoural area. SLNs were detected by CTL in 88.9–90.3% of patients. The number of SLNs was 0 in 9.7–11.1% of patients, 1 in 35.5–44.4% of patients, 2 in 35.5–38.9% of patients and 3 in 5.6–19.4% of patients (mean 1.6–1.8). In 28 patients, the detection rates of SLNs at 1, 3, 5, 10 min after contrast injection were 7.1%, 53.6%, 17.9%, and 21.4%, respectively.2 Their studies required four separate CT scans for SLN mapping in tongue cancer patients. In contrast, in our CTL study involving the injection of 2 ml of Iopamiron 300 into the peritumoural area of early oral cancer patients, the SLN detection rate was 90% and the mean number of SLNs was slightly higher 1.8 (range, 1–4). SLNs could be identified by two separate CT scans (2 min and 3.5–5 min after contrast injection) and with lower radiation exposure. However, CTL cannot be performed for oral cancer patients with iodine allergy to iodinated contrast medium.
Preoperative SLN mapping of N0 early oral cancer has commonly been performed using lymphoscintigraphy and/or single-photon emission CT with CT (SPECT/CT), with a reported identification rate of 95 to 100%,9,12,13 and the most common location of SLNs was level I to III using RI.31 Regarding the location of SLNs detected by CTL, Honda et al2 reported SLNs at level I to III; in our study, SLNs were at level I to II and in the sublingual region. Although metastasis to the lingual lymph nodes is one of the crucial events in determining survival outcomes in cancer of the tongue and floor of the mouth, few reports about the lingual lymph node are available because of its small size and close location to the primary tumour.23 In 2012, Saito et al23 first reported that CTL revealed a lateral lingual lymph node as the SLN in a tongue cancer patient, and our study showed SLNs which was detected in the sublingual region. The lingual lymph nodes are not always present (incidence: 17.1 to 25.1%),32–34 and lingual lymph node metastasis in oral cancer is rare,33,35–40 with a reported incidence of 2.1 to 14.3%.32–34 Owing to the proximity to the primary tumour and the frequency of extracapsular invasion, lingual lymph node metastasis can be misdiagnosed as local recurrence.39 Therefore, lingual lymph node metastasis may occur more frequently than has previously been reported.39
Recently, interstitial MRL has also been applied for SLN mapping of breast, esophageal, and head and neck cancer.15,25,27,41–45 The reported detection rate of SLN is 90.9–100% in breast cancer.41,44 However, there are few reports of interstitial MRL for N0 early oral cancer.26,27 Gadolinium or SPIO has been used as a contrast medium of MRL,26,27,46 and contrast medium drains through the lymphatics and accumulates in the SLN after the interstitial injection. Loo et al27 performed interstitial MRL with gadolinium for seven oral cancer patients (five tongues and two buccal mucosae) and showed that the optimal dose of gadolinium which was diluted with an equal volume of sterile water and a small volume of 2% lidocaine (1:1:0.2–0.5 contrast:water: lidocaine) was 0.3–0.5 ml and optimal imaging time was 5–15 min after the interstitial injection. Although tongue cancer patients had 4–8 SLNs (mean, 5.3) at level II-IV, SLN cannot be detected in two patients with cancer of the buccal mucosa, and the detection rate of SLN was 71.4%. Bae et al27 reported interstitial MRL with gadolinium (0.3:1:0.2 contrast:water: lidocaine) for SLN mapping, and SLNs (mean, 1.7) were detected at level I-III in all 26 oral cancer patients. Mizokami et al26 performed a study on SLN detection by interstitial MRL with SPIO and 99mTc-radicoloid lymphoscintigraphy and SPECT/CT in three tongue cancer patients. MR images were acquired sequentially at 10 min, 30 min and 24 h after injection of SPIO (ferucarbotran), and 1–3 SLNs were visualized in the 10 min interstitial MRL images and were completely concordant with those visualized by lymphoscintigraphy and SPECT/CT. However, interstitial MRL 24 h after SPIO injection showed an additional 10 or more lymph nodes uptake including secondary lymph nodes, probably due to the smaller particle size (approximately 45–60 nm) and negative charge that may have resulted in increased phagocytosis.26 Moreover, the limitations of this study were the small number of patients (three patients) and different dosages of SPIO (0.1 ml, 0.15 ml, and 0.3 ml). In our study, MRL at 10 min after injection of SPIO (0.4 ml) showed the detection rate of SLNs was 100% in 20 oral cancer patients. Although the mean number of SLN was 2.7, the number was more than the number detected by CTL and was similar to the number reported in RI imaging.5,10,12 MRL at 30 min after the injection showed additional 18 secondary lymph nodes. From the above, the optimal imaging timing of interstitial MRL for SLN mapping seemed to be 10 min after SPIO injection. However, our MRL study showed lingual lymph nodes which enhanced by CTL could not be visualized by shine-through artifacts, as RI imaging. Although the incidence and metastasis of lingual lymph nodes in oral cancer patients are rare,32,33,35–40 the presence should be examined by ultrasonography47 before interstitial MRL because oral cancer patients with iodine allergy to iodinated contrast medium cannot undergo CTL.
In interstitial MRL, gadolinium cannot help intraoperative detection of SLN during SLNB as RI method. However, interstitial MRL with SPIO can provide the preoperative mapping of SLN, and SLNs with SPIO can be detected by a handheld magnetometer (SentiMag®, Endomagnetics Ltd, UK), in the same way as the γ probe is used for detection of isotope-containing nodes.15,30,48–50 Several studies and reviews till now have shown the non-inferiority of SPIO over RI method for SLN detection in breast cancer.15,30,48–50 This RI-free method does not have the disadvantages of the standard method and is promising as a safe and effective alternative in the absence of nuclear medicine facilities.15 Another merit of MRL with SPIO is to enable SLN mapping in oral cancer patients with iodine allergy to iodinated contrast medium for which CTL cannot be performed. However, MRL with SPIO for SLN mapping cannot be performed in institutions without MRI or for patients with iron overload.
This study has some limitations such as a small number of patients, a single-centre study, and no comparison with RI imaging. Therefore, further prospective multicentre study with a larger number of patients and comparison with RI imaging is required to assess the usefulness of SLN mapping using MRL with SPIO in clinically N0 early oral cancer.
In conclusion, MRL with SPIO is safe and useful imaging for detection of SLNs in clinically N0 early oral cancer, and the optimal imaging timing was 10 min after SPIO injection.
REFERENCES
- 1.Hanai N, Asakage T, Kiyota N, Homma A, Hayashi R. Controversies in relation to neck management in N0 early oral tongue cancer. Jpn J Clin Oncol 2019; 49: 297–305. doi: 10.1093/jjco/hyy196 [DOI] [PubMed] [Google Scholar]
- 2.Honda K, Ishiyama K, Suzuki S, Oumi E, Sato T, Kawasaki Y, et al. Sentinel lymph node biopsy using computed tomographic lymphography in patients with early tongue cancer. Acta Otolaryngol 2015; 135: 507–12. doi: 10.3109/00016489.2015.1010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morton DL, Bostick PJ. Will the true sentinel node please stand? Ann Surg Oncol 1999; 6: 12–14. doi: 10.1007/s10434-999-0012-9 [DOI] [PubMed] [Google Scholar]
- 4.Rigual N, Loree T, Frustino J, Jayaprakash V, Cohan D, Sullivan M, et al. Sentinel node biopsy in lieu of neck dissection for staging oral cancer. JAMA Otolaryngol Head Neck Surg 2013; 139: 779–82. doi: 10.1001/jamaoto.2013.3863 [DOI] [PubMed] [Google Scholar]
- 5.Bilde A, von Buchwald C, Therkildsen MH, Mortensen J, Kirkegaard J, Charabi B, et al. Need for intensive histopathologic analysis to determine lymph node metastases when using sentinel node biopsy in oral cancer. Laryngoscope 2008; 118: 408–14. doi: 10.1097/MLG.0b013e31815d8e15 [DOI] [PubMed] [Google Scholar]
- 6.Bredell MG. Sentinel lymph node mapping by indocyanin green fluorescence imaging in oropharyngeal cancer - preliminary experience. Head Neck Oncol 2010; 2: 31. doi: 10.1186/1758-3284-2-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iwai T, Maegawa J, Hirota M, Tohnai I. Sentinel lymph node biopsy using a new indocyanine green fluorescence imaging system with a colour charged couple device camera for oral cancer. Br J Oral Maxillofac Surg 2013; 51: e26–8. doi: 10.1016/j.bjoms.2012.03.002 [DOI] [PubMed] [Google Scholar]
- 8.Miura K, Hirakawa H, Uemura H, Yoshimoto S, Shiotani A, Sugasawa M, et al. Sentinel node biopsy for oral cancer: a prospective multicenter phase II trial. Auris Nasus Larynx 2017; 44: 319–26. doi: 10.1016/j.anl.2016.07.008 [DOI] [PubMed] [Google Scholar]
- 9.Den Toom IJ, Heuveling DA, Flach GB, van Weert S, Karagozoglu KH, van Schie A, et al. Sentinel node biopsy for early-stage oral cavity cancer: the vu University medical center experience. Head Neck 2015; 37: 573–8. doi: 10.1002/hed.23632 [DOI] [PubMed] [Google Scholar]
- 10.Pedersen NJ, Jensen DH, Hedbäck N, Frendø M, Kiss K, Lelkaitis G, et al. Staging of early lymph node metastases with the sentinel lymph node technique and predictive factors in T1/T2 oral cavity cancer: a retrospective single-center study. Head Neck 2016; 38 Suppl 1(Suppl 1): E1033–40. doi: 10.1002/hed.24153 [DOI] [PubMed] [Google Scholar]
- 11.den Toom IJ, van Schie A, van Weert S, Karagozoglu KH, Bloemena E, Hoekstra OS, et al. The added value of SPECT-CT for the identification of sentinel lymph nodes in early stage oral cancer. Eur J Nucl Med Mol Imaging 2017; 44: 998–1004. doi: 10.1007/s00259-017-3613-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdul-Razak M, Chung H, Wong E, Palme C, Veness M, Farlow D, et al. Sentinel lymph node biopsy for early oral cancers: Westmead Hospital experience. ANZ J Surg 2017; 87(1-2): 65–9. doi: 10.1111/ans.13853 [DOI] [PubMed] [Google Scholar]
- 13.Khafif A, Schneebaum S, Fliss DM, Lerman H, Metser U, Ben-Yosef R, et al. Lymphoscintigraphy for sentinel node mapping using a hybrid single photon emission CT (SPECT)/CT system in oral cavity squamous cell carcinoma. Head Neck 2006; 28: 874–9. doi: 10.1002/hed.20434 [DOI] [PubMed] [Google Scholar]
- 14.Alkureishi LWT, Ross GL, Shoaib T, Soutar DS, Robertson AG, Thompson R, et al. Sentinel node biopsy in head and neck squamous cell cancer: 5-year follow-up of a European multicenter trial. Ann Surg Oncol 2010; 17: 2459–64. doi: 10.1245/s10434-010-1111-3 [DOI] [PubMed] [Google Scholar]
- 15.Wáng YXJ, Idée J-M. A comprehensive literatures update of clinical researches of superparamagnetic resonance iron oxide nanoparticles for magnetic resonance imaging. Quant Imaging Med Surg 2017; 7: 88–122. doi: 10.21037/qims.2017.02.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mokhtar M, Tadokoro Y, Nakagawa M, Morimoto M, Takechi H, Kondo K, et al. Triple assessment of sentinel lymph node metastasis in early breast cancer using preoperative CTLG, intraoperative fluorescence navigation and OSNA. Breast Cancer 2016; 23: 202–10. doi: 10.1007/s12282-014-0551-1 [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto S, Suga K, Maeda K, Maeda N, Yoshimura K, Oka M. Breast sentinel lymph node navigation with three-dimensional computed tomography-lymphography: a 12-year study. Breast Cancer 2016; 23: 456–62. doi: 10.1007/s12282-015-0584-0 [DOI] [PubMed] [Google Scholar]
- 18.Nakagawa M, Morimoto M, Takechi H, Tadokoro Y, Tangoku A. Preoperative diagnosis of sentinel lymph node (SLN) metastasis using 3D CT lymphography (CTLG. Breast Cancer 2016; 23: 519–24. doi: 10.1007/s12282-015-0597-8 [DOI] [PubMed] [Google Scholar]
- 19.Yasuta M, Sato S, Ishida T, Kiyohara T. Usefulness of CT-lymphography in sentinel lymph node navigation. Int J Clin Oncol 2014; 19: 557–62. doi: 10.1007/s10147-013-0582-1 [DOI] [PubMed] [Google Scholar]
- 20.Yuasa Y, Seike J, Yoshida T, Takechi H, Yamai H, Yamamoto Y, et al. Sentinel lymph node biopsy using intraoperative indocyanine green fluorescence imaging navigated with preoperative CT lymphography for superficial esophageal cancer. Ann Surg Oncol 2012; 19: 486–93. doi: 10.1245/s10434-011-1922-x [DOI] [PubMed] [Google Scholar]
- 21.Yoshida Y, Adachi K, Nakashima K, Yamane T, Yamamoto O. Difficulty to identify sentinel lymph nodes with computed tomography-lymphography in patients with cutaneous melanoma. Acta Derm Venereol 2011; 91: 465–6. doi: 10.2340/00015555-1057 [DOI] [PubMed] [Google Scholar]
- 22.Tsujimoto H, Yaguchi Y, Sakamoto N, Kumano I, Takahata R, Matsumoto Y, et al. Computed tomography lymphography for the detection of sentinel nodes in patients with gastric carcinoma. Cancer Sci 2010; 101: 2586–90. doi: 10.1111/j.1349-7006.2010.01706.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saito M, Nishiyama H, Oda Y, Shingaki S, Hayashi T. The lingual lymph node identified as a sentinel node on CT lymphography in a patient with cN0 squamous cell carcinoma of the tongue. Dentomaxillofac Radiol 2012; 41: 254–8. doi: 10.1259/dmfr/61883763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Honda K, Ishiyama K, Suzuki S, Kawasaki Y, Saito H, Horii A. Sentinel lymph node biopsy using preoperative computed tomographic lymphography and intraoperative indocyanine green fluorescence imaging in patients with localized tongue cancer. JAMA Otolaryngol Head Neck Surg 2019; 145: 735–40. doi: 10.1001/jamaoto.2019.1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ishiyama K, Motoyama S, Tomura N, Sashi R, Imano H, Ogawa J-ichi, Ogawa J, et al. Visualization of lymphatic Basin from the tumor using magnetic resonance lymphography with superparamagnetic iron oxide in patients with thoracic esophageal cancer. J Comput Assist Tomogr 2006; 30: 270–5. doi: 10.1097/00004728-200603000-00020 [DOI] [PubMed] [Google Scholar]
- 26.Mizokami D, Kosuda S, Tomifuji M, Araki K, Yamashita T, Shinmoto H, et al. Superparamagnetic iron oxide-enhanced interstitial magnetic resonance lymphography to detect a sentinel lymph node in tongue cancer patients. Acta Otolaryngol 2013; 133: 418–23. doi: 10.3109/00016489.2012.744143 [DOI] [PubMed] [Google Scholar]
- 27.Loo BW, Draney MT, Sivanandan R, Ruehm SG, Pawlicki T, Xing L, et al. Indirect Mr lymphangiography of the head and neck using conventional gadolinium contrast: a pilot study in humans. Int J Radiat Oncol Biol Phys 2006; 66: 462–8. doi: 10.1016/j.ijrobp.2006.05.045 [DOI] [PubMed] [Google Scholar]
- 28.Shah JP. Patterns of cervical lymph node metastasis from squamous carcinomas of the upper aerodigestive tract. Am J Surg 1990; 160: 405–9. doi: 10.1016/S0002-9610(05)80554-9 [DOI] [PubMed] [Google Scholar]
- 29.Byers RM, Weber RS, Andrews T, McGill D, Kare R, Wolf P. Frequency and therapeutic implications of "skip metastases" in the neck from squamous carcinoma of the oral tongue. Head Neck 1997; 19: 14–19. doi: [DOI] [PubMed] [Google Scholar]
- 30.Piñero-Madrona A, Torró-Richart JA, de León-Carrillo JM, de Castro-Parga G, Navarro-Cecilia J, Domínguez-Cunchillos F, et al. Superparamagnetic iron oxide as a tracer for sentinel node biopsy in breast cancer: a comparative non-inferiority study. Eur J Surg Oncol 2015; 41: 991–7. doi: 10.1016/j.ejso.2015.04.017 [DOI] [PubMed] [Google Scholar]
- 31.Mølstrøm J, Grønne M, Green A, Bakholdt V, Sørensen JA. Topographical distribution of sentinel nodes and metastases from T1-T2 oral squamous cell carcinomas. Eur J Cancer 2019; 107: 86–92. doi: 10.1016/j.ejca.2018.10.021 [DOI] [PubMed] [Google Scholar]
- 32.Fang Q, Li P, Qi J, Luo R, Chen D, Zhang X. Value of lingual lymph node metastasis in patients with squamous cell carcinoma of the tongue. Laryngoscope 2019; 129: 2527–30. doi: 10.1002/lary.27927 [DOI] [PubMed] [Google Scholar]
- 33.Jia J, Jia M-Q, Zou H-X. Lingual lymph nodes in patients with squamous cell carcinoma of the tongue and the floor of the mouth. Head Neck 2018; 40: 2383–8. doi: 10.1002/hed.25340 [DOI] [PubMed] [Google Scholar]
- 34.Ananian SG, Gvetadze SR, Ilkaev KD, Mochalnikova VV, Zayratiants GO, Mkhitarov VA, et al. Anatomic-histologic study of the floor of the mouth: the lingual lymph nodes. Jpn J Clin Oncol 2015; 45: 547–54. doi: 10.1093/jjco/hyv029 [DOI] [PubMed] [Google Scholar]
- 35.Ando M, Asai M, Ono T, Nakanishi Y, Asakage T, Yamasoba T. Metastases to the lingual nodes in tongue cancer: a pitfall in a conventional neck dissection. Auris Nasus Larynx 2010; 37: 386–9. doi: 10.1016/j.anl.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 36.Ozeki S, Tashiro H, Okamoto M, Matsushima T. Metastasis to the lingual lymph node in carcinoma of the tongue. J Maxillofac Surg 1985; 13: 277–81. doi: 10.1016/S0301-0503(85)80064-3 [DOI] [PubMed] [Google Scholar]
- 37.Dutton JM, Graham SM, Hoffman HT. Metastatic cancer to the floor of mouth: the lingual lymph nodes. Head Neck 2002; 24: 401–5. doi: 10.1002/hed.10026 [DOI] [PubMed] [Google Scholar]
- 38.Umeda M, Minamikawa T, Shigeta T, Oguni A, Kataoka T, Takahashi H, et al. Metastasis to the lingual lymph node in patients with squamous cell carcinoma of the floor of the mouth: a report of two cases. Kobe J Med Sci 2010; 55: E67–72. [PubMed] [Google Scholar]
- 39.Nishio N, Fujimoto Y, Hiramatsu M, Yamamoto Y, Sone M. Sonographic detection of a lingual node metastasis from early squamous cell cancer of the tongue. J. Clin. Ultrasound 2018; 46: 69–72. doi: 10.1002/jcu.22486 [DOI] [PubMed] [Google Scholar]
- 40.Han W, Yang X, Huang X, Hu Q, Wang Z. Metastases to lingual lymph nodes from squamous cell carcinoma of the tongue. Br J Oral Maxillofac Surg 2008; 46: 376–8. doi: 10.1016/j.bjoms.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 41.Shiozawa M, Kobayashi S, Sato Y, Maeshima H, Hozumi Y, Lefor AT, et al. Magnetic resonance lymphography of sentinel lymph nodes in patients with breast cancer using superparamagnetic iron oxide: a feasibility study. Breast Cancer 2014; 21: 394–401. doi: 10.1007/s12282-012-0401-y [DOI] [PubMed] [Google Scholar]
- 42.Li C, Meng S, Yang X, Zhou D, Wang J, Hu J. Sentinel lymph node detection using magnetic resonance lymphography with conventional gadolinium contrast agent in breast cancer: a preliminary clinical study. BMC Cancer 2015; 15: 213. doi: 10.1186/s12885-015-1255-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lu Q, Hua J, Kassir MM, Delproposto Z, Dai Y, Sun J, et al. Imaging lymphatic system in breast cancer patients with magnetic resonance lymphangiography. PLoS One 2013; 8: e69701. doi: 10.1371/journal.pone.0069701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pouw JJ, Grootendorst MR, Bezooijen R, Klazen CAH, De Bruin WI, Klaase JM, et al. Pre-Operative sentinel lymph node localization in breast cancer with superparamagnetic iron oxide MRI: the SentiMAG multicentre trial imaging subprotocol. Br J Radiol 2015; 88: 20150634. doi: 10.1259/bjr.20150634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Motomura K, Izumi T, Tateishi S, Tamaki Y, Ito Y, Horinouchi T, et al. Superparamagnetic iron oxide-enhanced MRI at 3 T for accurate axillary staging in breast cancer. Br J Surg 2016; 103: 60–9. doi: 10.1002/bjs.10040 [DOI] [PubMed] [Google Scholar]
- 46.Bae S, Lee H-J, Nam W, Koh YW, Choi EC, Kim J. Mr lymphography for sentinel lymph node detection in patients with oral cavity cancer: preliminary clinical study. Head Neck 2018; 40: 1483–8. doi: 10.1002/hed.25167 [DOI] [PubMed] [Google Scholar]
- 47.Nishio N, Fujimoto Y, Hiramatsu M, Yamamoto Y, Sone M. Sonographic detection of a lingual node metastasis from early squamous cell cancer of the tongue. J Clin Ultrasound 2018; 46: 69–72. doi: 10.1002/jcu.22486 [DOI] [PubMed] [Google Scholar]
- 48.Rubio IT, Diaz-Botero S, Esgueva A, Rodriguez R, Cortadellas T, Cordoba O, et al. The superparamagnetic iron oxide is equivalent to the Tc99 radiotracer method for identifying the sentinel lymph node in breast cancer. Eur J Surg Oncol 2015; 41: 46–51. doi: 10.1016/j.ejso.2014.11.006 [DOI] [PubMed] [Google Scholar]
- 49.Zada A, Peek MCL, Ahmed M, Anninga B, Baker R, Kusakabe M, et al. Meta-Analysis of sentinel lymph node biopsy in breast cancer using the magnetic technique. Br J Surg 2016; 103: 1409–19. doi: 10.1002/bjs.10283 [DOI] [PubMed] [Google Scholar]
- 50.Alvarado MD, Mittendorf EA, Teshome M, Thompson AM, Bold RJ, Gittleman MA, et al. SentimagIC: a non-inferiority trial comparing superparamagnetic iron oxide versus technetium-99m and blue dye in the detection of axillary sentinel nodes in patients with early-stage breast cancer. Ann Surg Oncol 2019; 26: 3510–6. doi: 10.1245/s10434-019-07577-4 [DOI] [PubMed] [Google Scholar]


