Abstract
Objectives:
This systematic literature review addressed the use of mandibular cortical index (MCI), assessed by panoramic radiography, for the identification of postmenopausal women at risk of osteoporosis.
Methods:
Databases were searched for original research studies published from September 2010 to September 2020 using the following keywords: “postmenopausal osteoporosis” and synonyms combined with “panoramic radiography” and synonyms. Only English language manuscripts and studies pertaining to the MCI were selected.
Results:
A total of 24 studies were included. The publications were highly heterogeneous in terms of the subject of interest, i.e. the MCI, with some studies comparing the usefulness of the MCI using panoramic radiography and using cone beam computed tomography, and others comparing different radiomorphometric indexes developed for panoramic radiography.
Conclusions:
Based on the literature included in this systematic review, we conclude that the MCI is useful as an auxiliary tool for identifying postmenopausal females at risk of low bone mineral density (BMD), as it correlates with skeletal BMD measured by dual X-ray absorptiometry. Nevertheless, other radiomorphometric indexes obtained from panoramic radiographs, such as panoramic mandibular index, mental index, and mandibular cortical width, are also valuable as auxiliary tools in the identification of postmenopausal females at risk, as they also correlate with BMD. Thus, it is not possible to affirm which index is the most reliable for the identification of postmenopausal females considering the literature screened. PROSPERO registration systematic review CRD42020208152.
Keywords: postmenopausal osteoporosis, panoramic radiography, bone mineral density, postmenopausal women, osteoporosis
Introduction
Osteoporosis is defined as a chronic metabolic disorder that affects bone strength and integrity, resulting in decreased bone mass and predisposing patients to low-energy fractures.1 The disease mostly affects postmenopausal females and strongly correlates with aging.2 It is suggested that changes in mandible cortical morphology appear at the onset of menopause.3 Osteoporotic fractures may lead to significant morbidity or mortality; however, osteoporosis is asymptomatic, making prevention with early diagnosis imperative.
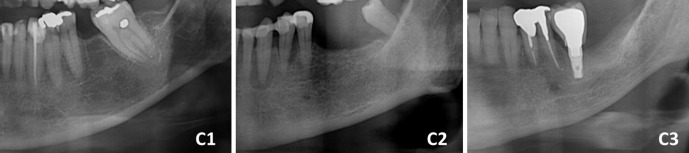
Although dual X-ray absorptiometry (DXA) is the gold-standard imaging technique for the diagnosis of osteoporosis, many screening tools have been created and investigated in order to identify patients at risk of low bone mineral density (BMD). The mandibular cortical index (MCI), developed for panoramic radiography in 1994 by Klemetti and collaborators,4 is a qualitative index that assesses the appearance of the mandibular endosteum. It classifies the mandibular cortex as C1, where the mandibular cortical bone has normal shape, indicating that the patient is not at risk; C2, where the mandibular cortical bone presents few radiolucent areas with semi-circular or linear shape; and C3, where the mandibular cortical bone presents several radiolucent areas, indicating that the patient is at high risk of systemic osteoporosis.4 An example of the aforementioned classification is available on Figure 1.
Figure 1.
An example of mandibular cortical index classification in panoramic radiography. C1: the endosteum of the mandibular cortex is well-demarcated, without radiolucid areas. C2: radiolucid areas are present. C3: the mandibular cortex is will-defined, with the presence of several radiolucid areas.
The main advantage of the MCI is its easy applicability among dentists, given that it constitutes a visual classification. This index was firstly applied as a auxiliary tool for the identification of postmenopausal females using conventional radiographs.4 Since then, a number of researchers have advocated the applicability and usefulness of the MCI as an accurate auxiliary tool for low BMD, particularly in postmenopausal females.2,5,6 Thus, this systematic review addressed the following question: “Is the MCI, assessed by panoramic radiography, effective for the screening of postmenopausal females with low BMD when compared to other indexes or control groups?”
Methods and materials
Protocol and registration
This systematic review was registered at the National Institute for Health Research International Prospective Register of Systematic Reviews (PROSPERO; registration number: CRD42020208152). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was followed.7
Study selection
The selection of eligible studies for inclusion in this systematic review was carried out by searching the following databases: PubMed Central® (United States National Institutes of Health’s National Library of Medicine), Embase® (Excerpta Medica Database), Scopus® (Elsevier), Cochrane Central Register of Controlled Trials, Web of Science® (Institute of Scientific Information – Clarivate Analytics), and Google Scholar® (Google). These databases were searched without implementing any language restrictions, and papers published between September 2010 and September 2020 were included.
The Boolean operator “AND” was used to combine search keywords. Itemized search strategies were established for each database on the basis of the following search keywords: osteoporosis AND panoramic radiography; osteoporosis AND post-menopause AND pantomography; osteoporosis AND post-menopause AND orthopantomography; bone density AND post-menopause AND panoramic radiography; bone density AND post-menopause AND pantomography; bone density AND post-menopause AND orthopantomography; bone content AND post-menopause AND panoramic radiography; bone content AND post-menopause AND pantomography; bone content AND post-menopause AND orthopantomography; bone mineral density AND post-menopause AND panoramic radiography; bone mineral density AND post-menopause AND pantomography; bone mineral density AND post-menopause AND orthopantomography; osteoporosis AND post-menopause AND panoramic radiography; osteoporosis AND post-menopause AND pantomography; osteoporosis AND post-menopause AND orthopantomography; bone density AND post-menopause AND panoramic radiography; bone density AND post-menopause AND pantomography; bone density AND post-menopause AND orthopantomography; bone content AND post-menopause AND panoramic radiography; bone content AND post-menopause AND pantomography; bone content AND post-menopause AND orthopantomography; bone mineral density AND post-menopause AND panoramic radiography; bone mineral density AND post-menopause AND pantomography; bone mineral density AND post-menopause AND orthopantomography; osteoporosis AND post-menopausal period AND panoramic radiography; osteoporosis AND post-menopausal period AND pantomography; osteoporosis AND post-menopausal period AND orthopantomography; bone density AND post-menopausal period AND panoramic radiography; bone density AND post-menopausal period AND pantomography; bone density AND post-menopausal period AND orthopantomography; bone content AND post-menopausal period AND panoramic radiography; bone content AND post-menopausal period AND pantomography; bone content AND post-menopausal period AND orthopantomography; bone mineral density AND post-menopausal period AND panoramic radiography; bone mineral density AND post-menopausal period AND pantomography; bone mineral density AND post-menopausal period AND orthopantomography; postmenopausal osteoporosis AND panoramic radiography; postmenopausal osteoporosis AND pantomography; postmenopausal osteoporosis AND orthopantomography; post-menopausal osteoporosis AND panoramic radiography; post-menopausal osteoporosis AND pantomography; post-menopausal osteoporosis AND orthopantomography; post-menopausal bone loss AND panoramic radiography; post-menopausal bone loss AND pantomography; post-menopausal bone loss AND orthopantomography; post-menopausal bone loss AND panoramic radiography; post-menopausal bone loss AND pantomography; post-menopausal bone loss AND orthopantomography.
Eligibility criteria
Types of studies
Only research studies were considered eligible for inclusion; abstracts, oral presentations, case reports, and literature reviews were excluded. Original investigations that did not consider the MCI as the methodology were not eligible. Additionally, articles that were non-English language and/or used non-human subjects were excluded. The present review did not consider other imaging techniques, such as CT; it only considered panoramic radiography.
Participant groups
Studies involving groups of postmenopausal females, which performed panoramic radiographs for MCI assessment were included.
Data extraction
Data extraction was performed by three independent reviewers who initially screened the titles and abstracts and then evaluated the full text of each selected study. A fourth reviewer checked each study that was considered eligible by the other three reviewers. Disagreements among the reviewers were solved by discussion, and, when an agreement could not be reached, two other collaborators were consulted.
Data analysis–risk of bias
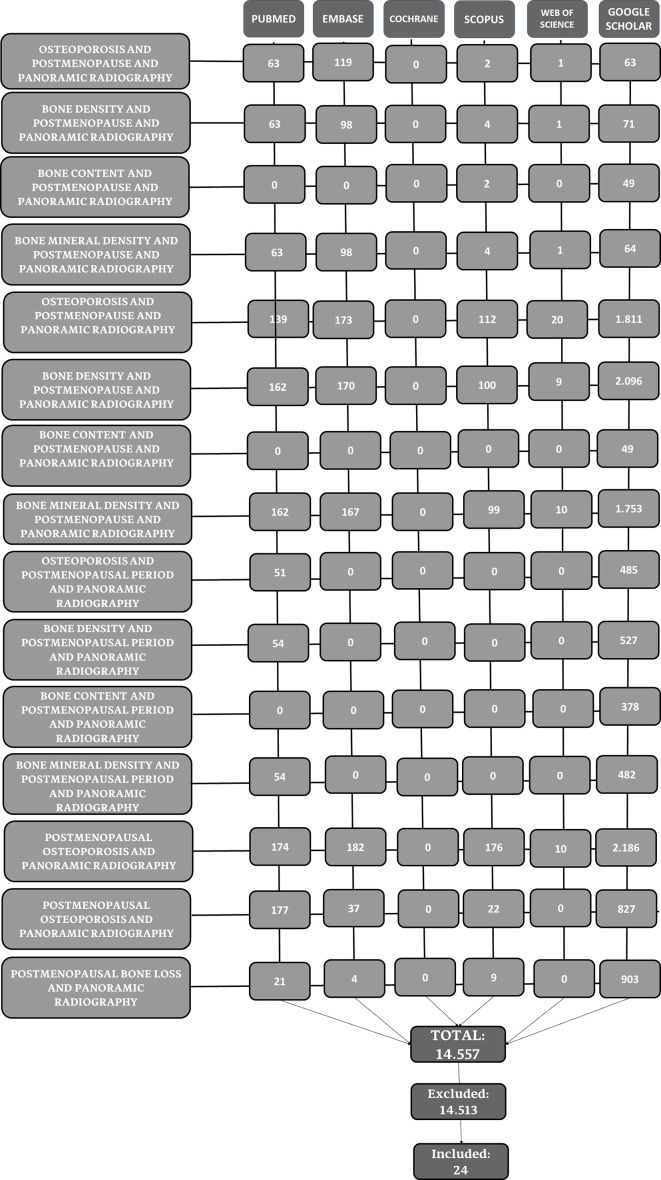
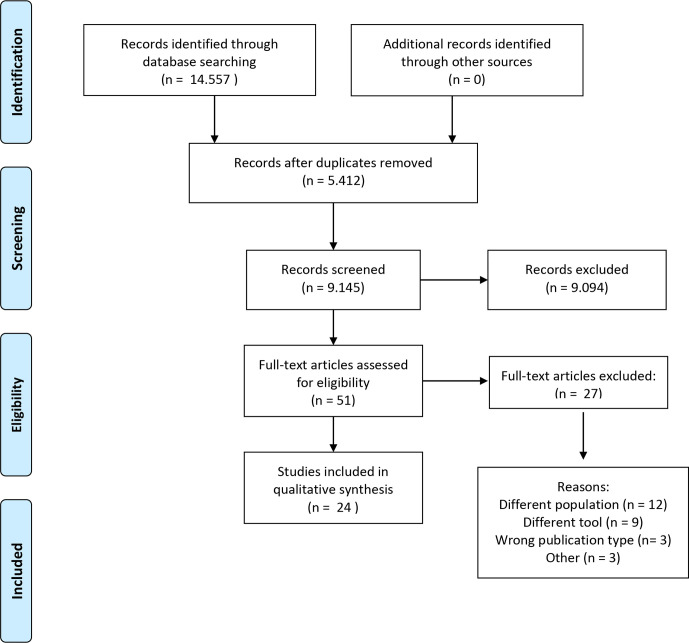
The data search results considering databases and keywords are summarized in a flow chart (Figure 2). The Prisma flow diagram, along with the search results, is available in Figure 3. Data about the included studies are available in Tables 1 and 2.
Figure 2.
Flow chart of study selection. All search results for the words “orthopantomography,” “pantomography,” and “panoramic radiography” were aggregated and expressed as “panoramic radiography” in order to make the flow chart more concise.
Figure 3.
Prisma flow chart of search results.
Table 1.
Research articles selected to the review
| Authors | Year | Country | Main objectives pertaining to MCI |
|---|---|---|---|
| Alam et al.8 | 2020 | Saudi Arabia | To evaluate the relationship between age, body mass index, oral signs, and BMD osteoporosis among postmenopausal females, assessing MCW, PMI, MCI and number of missing teeth in panoramic radiographs. |
| Kato et al.9 | 2019 | Brazil | To assess and compare MCI obtained by digital panoramic radiographs and by panoramic reconstruction of CBCT with three different slice thicknesses for the screening of low BMD in post-menopausal females. |
| Golhar et al.10 | 2019 | India | To evaluate MI and MCI by panoramic radiographs; to assess osteoporosis in post-menopausal females evaluating USG-calcaneus and serum calcium levels in osteoporosis in post-menopausal females. |
| Nasreen et al.11 | 2019 | India | To evaluate alveolar bone mass using radiomorphometric indices (including MCI) in postmenopausal females. To correlate radiomorphometric indices with serum vitamin D3. |
| Grocholewicz et al.12 | 2018 | Poland | To evaluate mandibular morphometric analysis (including MCI) and QUS at the radius and proximal phalanx III finger. |
| Navabi et al.13 | 2018 | Iran | To compare MCW and MCI from digital panoramic radiograph in osteopenic and osteoporotic postmenopausal females. |
| Choi et al.5 | 2018 | Brazil | To assess BMD by peripheral DXA and MCI in Brazilian females, according to age ranges. |
| Munhoz et al.2 | 2018 | Brazil | To compare peripheral BMD alterations among Brazilian postmenopausal females from three ethnic groups considering age and BMI influence; to correlate their BMD with MCI. |
| Munhoz et al.14 | 2017 | Brazil | To analyze the influence of Type 2 BMD and panoramic radiomorphometry in postmenopausal females, comparing with results from nondiabetic postmenopausal females. |
| Pallagatti et al.15 | 2017 | India | To validate the use of MCI on panoramic radiographs so as to detect osteoporosis in the patients at an early disease stage. |
| Carmo et al.16 | 2017 | Brazil | To asess the role of radiomorphometric indices (including MCI) in panoramic radiographs, in the diagnosis of low BMD in postmenopausal females |
| Kolte et al.17 | 2017 | India | To compare the risk of osteoporosis in pre- and postmenopausal periodontally healthy and chronic periodontitis females by digital panoramic radiographs. |
| Grgic et al.18 | 2017 | Serbia | To examine the correlation between dental panoramic indices (MCI and MI) and BMD bone mineral density in these three groups of patients: postmenopausal females with osteoporosis, osteoporosis treated with bisphosphonate therapy and control group. |
| Alonso et al.19 | 2016 | Brazil | To evaluate and compare images from CBCT and panoramic radiographs using MCI. |
| Jagelavičienė et al.20 | 2016 | Lithuania | To determine the relation between MCI and calcaneal BMD among postmenopausal females. |
| Majumder and Harum.21 | 2015 | Bangladesh | Evaluate the alveolar bone changes in osteopenic and osteoporosis condition of postmenopausal females. |
| Kim et al.22 | 2014 | Korea | To assess if MCI, MI and simple visual estimation could be used for osteoporosis diagnosis based on the correlation with BMD. |
| Valerio et al.23 | 2013 | Brazil | To correlate the MCI and MI with BMD, evaluated by the dual-energy X-ray absorptiometry test, in a population of postmenopausal females to identify patients with asymptomatic low BMD. |
| Gaur et al.24 | 2013 | India | To assess and compare the relative efficacy, ease of application and measurement of the various mandibular cortical indices which were obtained on the panoramic radiographs with bone densitometry data of postmenopausal females |
| Martínez – Maestre et al.25 | 2013 | Spain | To evaluate the use of mandibular anatomic indexes on panoramic radiographs as predictors of bone fragility fractures |
| Khojastehpour et al.26 | 2011 | Iran | To assess MCW and MCI in panoramic radiography of postmenopausal females |
| Khatoonabadet al.27 | 2011 | Iran | To evaluate the relationship among the radiomorphometric indices of the mandible, biochemical markers of the bone turnover and hip BMD in a group of post-menopausal females. |
| Mudda et al.3 | 2010 | India | To assess mandibular bone changes in pre and postmenopausal females with chronic generalized periodontitis using different radiomorphometric indices as MCI, MI, PMI in Indian population. |
| Leite et al.28 | 2010 | Brazil | To test correlations of panoramic radiomorphometric indices with lumbar spine and hip BMDs and to test the accuracy of these indices for predicting osteoporosis. |
MCI: mandibular cortical index; MCW: mandibular cortical width; BMD: bone mineral density; QUS: quantitative ultrasound; MI: mental index; PMI: Panoramic mandibular index; CBCT: cone beam computed tomography; USG: ultrasound; DXA: dual X-ray absorptiometry.
Author, year of publication, country of origin, main objective pertaining to the mandibular cortical index.
Table 2.
Population studied, number of participants of each study (n), main results, comparisons performed results (between indexes) and conclusions
| Authors | Population Studied | n | Main results | Comparisons performed | Conclusions |
|---|---|---|---|---|---|
| Alam et al.8 | Postmenopausal females divided in two groups: with osteoporosis and without osteoporosis, according to their DXA results. | 60 | A significant difference in the mandibular cortical shape index between the two groups was observed. | When the postmenopausal females with osteoporosis were compared with postmenopausal females without osteoporosis, the indexes MCW, PMI, M/M ratio and FD did not present any statistically significant results. MCI presented the risk of osteoporosis in the C3 category was 11.36 times higher than that in the C2 category and 10.64 times higher for C2 than for C1; moreover, the risk of osteoporosis in the C3 category was 111.11 times higher than that in the C1 category. | The MCI on panoramic radiographs are effective indicators of osseous changes in postmenopausal females with osteoporosis. |
| Kato et al.9 | Postmenopausal females exclusively, classified according to DXA results. | 54 | The sensitivity and specificity for panoramic radiographs: 52.6 and 56.2%, respectively; for panoramic reconstructions of CBCTs with 5-, 15-, and 25 mm slice thicknesses: 63.1 and 43.7%, 50.0 and 50.0%, and 52.6 and 62.5%, respectively. |
Panoramic reconstructions using CBCT with different slices were compared to panoramic radiographs using MCI. Panoramic reconstructions from CBCTs with 25 mm slice thickness seems to be the most accurate. | The panoramic reconstruction of CBCT with 25 mm slice thicknesses seems to be the most accurate among the examinations evaluated. Panoramic radiographs and CBCT may be useful for the screening of low BMD in post-menopausal females. |
| Golhar et al.10 | Premenopausal (control group) and post-menopausal females (study group). BMD status were classified using phalanx T-score. | 100 | In Pre-menopausal group, 45 (90%) patients belonged to C1 classification, while 5 (10%) patients belonged to C2 classification. In Post-menopausal group, 22 (44%) patients belonged to C1 cortical classification, while 21 (42%) patients belonged to C2 cortical quality and 7 (14%) patients belonged to C3 cortical classification. | Correlations between MCI and the phalanx T-score were observed. Phalanx T-score was not correlated with other indexes relating radiomorphometric measurements PMI, MR and MCW. |
MI and MCI associate well and combining the two may be more helpful rather than using either of them alone. |
| Nasreen et al.11 | Postmenopausal females divided in two sub groups: females from urban and rural area. Vitamin D3 levels were measured. | 60 | Urban group: 0.0% of the subjects in the C1 category, 40.0% of the subjects in C2 category and 60.0% of the subjects in the C3 category. Rural group: 46.7% of the subjects in the C1 category, 43.3% of the subjects in the C2 category, and 10% of the subjects in the C3 category. | MCI, MI, PMI and vitamin D3 levels were compared between groups and their correlation with vitamin D3 levels were tested. MI and PMI did not corelate with vitamin D3 levels. The results considering the correlation between MCI and vitamin D levels were not mentioned in the manuscript. | The findings in panoramic radiographs correlates with serum vitamin D3 level and higher significant values were observed in rural females when compared to females from urban areas. |
| Grocholewicz et al.12 | Postmenopausal females exclusively; BMD status assessed by QUS at the radius and proximal phalanx III finger. | 97 | Higher scores of MCI classification were observed in older females. MCI significantly correlated with the skeletal status, distance between lower mandibular borders behind mental foramen and mandibular ratio. | MCI correlates with phalanx T-score. Phalanx T-score was not correlated with PMI, MR and MCW. | MCI can be effectively assessed on panoramic radiographs and could be used as a screening tool osteoporosis. This index is very simple for application. |
| Navabi et al.13 | Postmenopausal females were divided in osteopenic and osteoporotic, according to their DXA results. | 50 | MCW and MCI was significantly correlated with BMD. | The results showed that MCW is an appropriate index of osteoporosis in post-menopausal females. MCI “almost “correlated with BMD, p = 0.07) |
Postmenopausal females with low femoral BMD have thinner mandibular cortex at the mental foramen region. Dental panoramic radiographs are useful screening tools for postmenopausal osteoporotic patients, give sufficient information to make an early diagnosis and prevent from osteoporotic fractures in elderly females. |
| Choi et al.5 | Females divided in eight groups, according to age ranges. Peripheral DXA was applied to classify females BMD. | 252 | It was found different inverse correlations between MCI and the different forearm sites. | This study did not compare MCI with other indices, only verified MCI correlation with age and peripheral DXA. | Age-related bone loss is more evident in the proximal forearm than in the distal forearm. Furthermore, MCI can express a better inverse correlation with peripheral DXA at the proximal forearm than with the distal forearm. |
| Munhoz et al.2 | Brazilian postmenopausal females with three different ethnicities (afrodescendant, Asian, Caucasian). Peripheral DXA was applied to classify females BMD. | 150 | Age is the only variable associated with osteoporotic alterations in the mandible that reflects on MCI. An inverse correlation was found between the MCI and the T-scores from peripheral DXA. | This study did not compare MCI with other indices, only verified MCI correlation with age, body mass index, ethnic group and peripheral DXA. | Patient’s age is associated with BMD and MCI. The MCI is inversely correlated with peripheral DXA. |
| Munhoz et al.14 | Postmenopausal females divided in diabetics and non-diabetics. Peripheral DXA was applied to classify females BMD. | 228 | Mean Z score values were significantly higher in diabetics than in non-diabetics. T and Z score values were significantly correlated with MCI. | This study did not compare MCI with other indices, only verified MCI correlation with peripheral DXA | Type two diabetes may be associated with increased BMD in postmenopausal females. MCI from panoramic radiographs is moderately correlated with DXA in patients with diabetes with osteoporosis. |
| Pallagatti et al.15 | Postmenopausal females exclusively. DXA was applied to classify females BMD. | 60 | The average accuracy in detecting normal bone, osteopenia and osteoporosis was 58.08%, 63.3 and 64.74% respectively. | This study did not compare MCI with other indices. | Panoramic radiographs MCI can be used as a screening tool for the evaluation as well as early detection of osteoporosis. |
| Carmo et al.16 | Brazilian postmenopausal females. Femoral and lumbar spine DXA was applied to classify females BMD. | 198 | MCI and BMD of lumbar spine were correlated (κ = 0.912). The agreement between MCI and the BMD in the femur was moderated (κ = 0.579). | The correlation of MCI and IM with DXA were compared. The higher correlation was found between MCI and lumbar spine DXA when compared to IM and lumbar spine or femoral DXA, and when compared to MCI and femoral DXA. | The radiomorphometric indices are capable of identifying postmenopausal females with low BMD in the mandible. |
| Kolte et al.17 | pre- and postmenopausal periodontally healthy and with chronic periodontitis. | 120 | MCI evaluation showed a high prevalence of C2 and C3 patterns postmenopausal females. MCI presented correlation with MI and age. MI and PMI values in digital panoramic radiographs were reduced in patients affected with periodontitis. | Although MI, PMI, MCI were assessed, these radiomorphometric indexes were not directly compared. MI and PMI were reduced in females affected with periodontitis. Considering MCI, A reduction between the percentage of C1 pattern in pre- and postmenopausal periodontitis patients was also observed, indicating a more severe erosion of the mandibular cortex in the postmenopausal patients. |
A positive association between MCI and chronic periodontitis in postmenopausal females was noticed. Bone density reduces in postmenopausal females, and the positive association between MCI and chronic periodontitis in postmenopausal females confirms the high risk of osteoporosis in them. |
| Grgic et al.18 | Postmenopausal females divided in groups: osteoporosis, osteoporosis treated with bisphosphonates and control group. | 120 | A higher number of patients with C3 classification was found in the MCI were found in the osteoporosis group but the difference was not significant. No significant differences were found in MI or MCI (p = .06) in all the examined groups. |
MCI and MI specificity and sensitivity were compared. For both indexes, authors tried distinct cut-of points; however no optimal values of sensitivity and specificity were found. | MI and MCI are not precise diagnostic tools for diagnosing low BMD in postmenopausal females. (Observation from this review authors: we consider that MCI had significant difference between groups as p = 0.06) |
| Alonso et al.19 | Females over 45 years old | 30 | No differences were found between the diagnostic results based on panoramic radiography and CBCT panoramic reconstruction. | Panoramic reconstructions using CBCT were compared to panoramic radiographs using MCI. Disagreement between the techniques were verified, particularly in the classification C2 and C1. | The MCI is not an adequate means of assessing bone quality with CBCT. The higher values on MCI classification found for the cross-sectional slices could be associated with better visibility of erosions or defects in mandibular cortical bone on the CBCT image. |
| Jagelavičienė et al.20 | Lithuanian postmenopausal females 50–77 years old, classified using calcaneum BMD. |
129 | The differences in BMD were statistically significant between Groups C1 and C3, Groups C2 and C3, and between the calcaneal BMD groups. There was a statistically significant inverse correlation between the MCI and calcaneal BMD. | This study did not compare MCI with other indices. | The analysis of the MCI validity in BMD status showed low sensitivity (69.4%) and specificity (53.9%). |
| Majumder and Harum.21 | Postmenopausal females divided in osteoporotic, osteopenic and normal. DXA was applied to classify females BMD. | 1315 | The changes in the MCI (C2 and C3) were more frequent in osteoporotic condition rather than osteopenic and normal. | MCI pixel intensity and mandibular alveolar bone mass in panoramic radiographs were assessed but not directly compared. | Changes in postmenopausal alveolar bone were strongly correlated with the BMD of systemic skeletal bone. |
| Kim et al.22 | Korean postmenopausal females with 50 years old or older. DXA was applied to measure BMD. | 194 | BMD at the lumbar spine and total hip were significantly lower in participants with reduction of mandibular width, thinning and resorption of mandibular cortex by the MI and MCI. | Correlations with BMD were assessed using MCI, MC and simple visual estimation. However, comparisons were not performed. | The thickness and morphological changes of mandibular inferior cortical bone are associated with BMD, independent of age, height and weight. |
| Valerio et al.23 | Postmenopausal womens divided in: normal, osteopenic and osteoporosis according to their DXA. | 64 | There were significant differences between the normal and lower bone mineral density groups (osteopenia and osteoporosis) for MCI. | MCI, MI and three indices created by the authors (mental posterior index 1, 2 and 3) were assessed. All the indices were capable of differ females at osteoporosis risk. | The radiomorphometric indices evaluated in panoramic radiographs can be used to identify postmenopausal females with low BMD. |
| Gaur et al.24 | Postmenopausal females exclusively, divided as osteoporotic, osteopaenic and normal according to their DXA results. | 40 | The sensitivity (100%) and specificity (88.88%) of MCI showed good results. | MCI, PMI, MI, antegonial index and gonion index were assessed. Significant reductions of the mean values were observed in the osteoporotic group as compared to normal and osteopaenic groups for all the radiomorphometric indices except for the antegonial index group. | Orthopantomographs may be useful in screening patients with osteoporosis, mainly among postmenopausal females. |
| Martínez – Maestre et al.25 | Spanish postmenopausal females, divided in females that experienced previous fractures (with T-score lower than −2.5) and females without previous fractures (control group). | 120 | C1 group had less cases of females with previous fractures than C2 and C3. C2 has less fractures than C3. | No direct comparisons were performed between indexes. PMI and MI values were significantly lower in cases than in controls. | Panoramic radiomorphometrics mandibular indexes such as MCI, PMI, and MI, may be useful for identifying the population at higher risk for fracture. |
| Khojastehpour et al.26 | Iranian postmenopausal females. DXA was applied to measure BMD and females were grouped in according to DXA results in order to perform comparisons between indexes. | 119 | There were significant associations between BMD and MCI. | Cortical width and shape (MCI) were assessed, and it was observed a significant correlation between age and these indexes. There was also a significant correlation between cortical width and cortical shape of the mandible For both vertebral and femoral BMD, there was a statistically significant difference between the cortical width of normal and osteopenic/osteoporotic groups, however this difference was not significant between the osteopenic and osteoporotic groups. BMD was significantly correlated with cortical shape in both lumbar vertebrae and femoral neck regions. | Postmenopausal females with thin or eroded mandibular inferior cortex may have an increased risk for low BMD or osteoporosis |
| Khatoonabad et al.27 | Postmenopausal females. Hip BMD was measured in order to group females according to T-scores in: osteoporosis, osteopaenic and normal. | 140 | Moderate to severe cortical erosion (C2 and C3) significantly increased the likelihood of osteopenia and osteoporosis. | MCW and M/M ratio showed statistically significant differences between the three groups. No significant difference was found in PMI between the groups. Statistically significant difference in the quality of mandibular cortex (assessed using MCI) between the groups. | Panoramic radiography gives sufficient information to make an early diagnosis regarding osteoporosis in post-menopausal females. Panoramic radiographs may be valuable in the prevention of osteoporotic fractures in elderly females. |
| Mudda et al.3 | Pre and postmenopausal females with generalized periodontitis. | 60 | No association between periodontitis and MCI was found. | MCI, PMI and MI were related to the menopausal status. Patients with C3 category were seen only in post-menopausal group after 54 years of age. | Radiomorphometric indices could be used by general dentists after a little training to detect post-menopausal females at higher risk of osteoporosis. |
| Leite et al.28 | Postmenopausal females exclusively. Hip and lumbar sipne DXA was applied to measure BMD. | 351 | Associations of the MCI and simple visual estimation of the cortical width with BMD, determined at the lumbar spine, femoral neck, and total hip, were significantly lower in patients with thinning and resorption of mandibular cortex identified by the simple visual estimation and MCI, respectively | The qualitative indices (MCI and simple visual estimation) were more convenient than the quantitative indices and demonstrated better association with hip and spinal BMDs. | Antegonial indices and gonial angles cannot be used as osteoporosis predictors. The most accurate indices were the MI, MCI, and visual estimation of cortical width. |
MCI: mandibular cortical index; MCW: mandibular cortical width; BMD: bone mineral density; QUS: quantitative ultrasound; MI: mental index; PMI: Panoramic mandibular index; CBCT: cone beam computed tomography; USG: ultrasound; DXA: dual X-ray absorptiometry; M/M ratio: mandibular alveolar bone resorption degree; FD: fractal dimension; MR: mandibular ratio.
The risk of bias was assessed using the risk of bias in non-randomized studies (ROBINS-I) tool.29 The quality analysis results are available in Table 3.
Table 3.
Quality assessment of each study included according to the ROBINS-I tool.29
| Authors | Confounding | Selection of participants | Deviations from de intended interventions | Missing data | Measurement of outcomes | Selection of reported results | Overal |
|---|---|---|---|---|---|---|---|
| Alam et al.8 | Low | Low | Low | Low | Low | Low | Low |
| Kato et al.9 | Low | Low | Low | Low | Low | Low | Low |
| Golhar et al.10 | Low | Low | Low | Low | Low | Low | Low |
| Nasreen et al.11 | Low | Low | Low | Low | Low | Low | Low |
| Grocholewicz et al.12 | Moderate | Low | Low | Low | Low | Low | Moderate |
| Navabi et al.13 | Low | Low | Low | Low | Low | Low | Low |
| Choi et al.5 | Moderate | Moderate | Moderate | Low | Low | Low | Moderate |
| Munhoz et al.2 | Low | Low | Low | Low | Low | Low | Low |
| Munhoz et al.14 | Low | Low | Low | Low | Low | Low | Low |
| Pallagatti et al.15 | Low | Low | Low | Low | Low | Low | Low |
| Carmo et al.16 | Low | Low | Low | Low | Low | Moderate | Moderate |
| Kolte et al.17 | Moderate | Low | Low | Low | Low | Low | Moderate |
| Grgic et al.18 | Moderate | Low | Low | Low | Low | Low | Moderate |
| Alonso et al.19 | Moderate | Moderate | Low | Low | Low | Low | Moderate |
| Jagelavičienė et al.20 | Low | Low | Low | Low | Low | Low | Low |
| Majumder and Harum.21 | Low | Low | Low | Low | Low | Low | Low |
| Kim et al.22 | Low | Low | Low | Low | Low | Low | Low |
| Valerio et al.23 | Low | Low | Low | Low | Low | Low | Low |
| Gaur et al.24 | Low | Low | Low | Low | Low | Low | Low |
| Martínez – Maestre et al.25 | Low | Moderate | Low | Moderate | Low | Low | Moderate |
| Khojastehpour et al.26 | Low | Low | Low | Low | Low | Low | Low |
| Khatoonabadet al.27 | Low | Low | Low | Low | Low | Low | Low |
| Mudda et al.3 | Low | Low | Low | Low. | Low | Low | Low |
| Leite et al.28 | Low | Low | Low | Low | Low | Low | Low |
Overall risk of bias: equal to the most severe level of bias found in any domain.
Low: Comparable to a well-performed randomized trial;
Moderate: sound for a non-randomized study but not comparable to a rigorous randomized trial;
Serious: presence of important problems;
Critical: too problematic… to provide anu useful evidence on the effects of intervention
Results
A total 14,557 studies were identified through database searching and 14,533 studies were excluded; 24 studies were selected.2,3,5,8–28 The following data were extracted: year of publication, country of the study selected, subject pertaining to the MCI, population studied, number of participants included in each study, mains results, and conclusions.
The most recent study was from 20208 and the oldest from 2010.28 Eight publications were from Brazil2,5,9,14,16,19,23,28 and six were from India.3,10,11,15,17,24 The publications were highly heterogeneous in terms of the subject pertaining to the MCI. Some studies compared the MCI using panoramic radiographs and using specifics slices from cone beam computed tomography (CBCT)9,19; others compared different radiomorphometric indexes developed for panoramic radiographs3,8,13,24,26,28; one study evaluated the use of MCI in fracture prediction25; one study assessed if the applicability of MCI was easy for the professionals24; and three studies examined the usefulness of MCI itself (Table 1).15,17,22 Additionally, some studies assessed the correlations between the MCI and bone biomarkers, vitamin D3, and serum calcium,10,11,27 as well as with other BMD examinations, such as DXA or quantitative ultrasound.2,5,10,12,18,20,23,27,28
The participants of the studies selected were grouped according to ethnicity,2 the presence or absence of periodontal disease,3,17 Type 2 diabetes,14 the use of bisphosphonates for osteoporosis treatment,18 pre- and post-menopause period,3,10,17 and distinct age ranges.5 Studies often grouped postmenopausal females in groups of osteoporotic and non-osteoporotic females,8,13,21,23 whereas some studies considered the residence of the females (urban or rural)11 or included females who had experienced previous fractures.25
The number of participants included in the studies ranged from 3019 to 1315.21 The MCI was studied or compared along with a broad number of other quantitative or qualitative radiomorphometric indexes, such as the mandibular cortical width (MCW),8,10,12,26,27 panoramic mandibular index (PMI),3,8,10,11,17,24,27 mental index (MI),3,11,16–18,22–24 mandibular ratio,12 mandibular alveolar bone resorption degree,8,27 pixel intensity,21 fractal dimension,8 simple visual estimation,22,28 and antegonial index and gonion index,24 whereas some researchers only investigated the MCI.2,5,14,15,20 Details about the main results and conclusions pertaining to the MCI based on the data selected are available in Table 2 and are debated in the “Discussion” section.
Discussion
Since panoramic radiographs are often requested at the beginning of dental treatments, their application as auxiliary tools for the identification of patients at risk of low BMD offer several advantages, including better accessibility, low cost, and low radiation exposure.30
The introduction of the technology of digital panoramic radiographs has increased the efficiency of radiographic investigations, as structures and their alterations can be observed in greater detail that that obtained by film-based radiographs. Qualitative image assessments, such as those using the MCI, allow analyses of minimal details of the mandibular cortex in order to identify patients at risk of low BMD. Furthermore, the MCI is an easy-application index that can be broadly implemented by dentists.12
In the present systematic review, we concluded that researchers agree on the usefulness of the MCI as an auxiliary imaging tool for identifying patients at risk of low BMD,2,3,5,8–12,14–28 which could be useful for osteoporosis and, consequently, for preventing low-energy fractures,25 provided that dentists refer the patient for proper diagnosis and treatment. Furthermore, several of the included studies consistently demonstrated the correlation of the MCI with systemic BMD.2,5,10,12,18,20,23,28
When the MCI was compared with other indexes obtained based on panoramic radiographs, such as the MI, MCW, PMI, simple visual estimation, antegonial indexes, and gonial angle measurement, diverse observations were made in terms of their usefulness in screening for low BMD. Briefly, the MI is obtained by drawing a line parallel to the long axis of the mandible and tangential to the inferior border of the mandible and a line perpendicular to this tangent intersecting the inferior border of the mental foramen, along which the MCW is measured.28 The MCW and PMI are also measured using the mental foramen and mandible base.13,31 Simple visual estimation classifies the mandibular cortex based on its width.28 Antegonial indexes measure the cortical width in the region anterior to the gonion or the distance along a perpendicular line from the deepest point of the antegonial notch concavity to a line parallel to the inferior cortical border of the mandible.28,32,33 The gonial angle is evaluated by tracing a line tangential to the mandible’s lower border and another line tangential to the posterior border of the ramus on each side.28,34
Leite et al28 verified that the MCI, MI, and simple visual estimation of the cortical width are accurate for screening for low BMD; however, antegonial indexes and gonial angle measurement could not be applied as predictors of low BMD. Alam et al8 mentioned that the cortical width and PMI are not statistically different between osteoporotic and non-osteoporotic postmenopausal females; however, the MCI was significantly different between these groups. Moreover, authors verified that postmenopausal females with a C3 MCI classification were 11 times more likely to develop osteoporosis than were those with other MCI classifications.8
Navabi et al13 concluded that the MCW is relatively superior to the MCI, because the latter “almost” correlated with low BMD, as assessed by DXA. Nevertheless, the statistical p-value demonstrated by the researchers (p = 0.07)13 would have been considered significant according to other statisticians.35 The same affirmation was made by Grgic et al,18 who indicated a p-value of 0.06 for the correlation of MCI to BMD.
In terms of the correlation between MCI classification and age, we observed a consensus among investigators: as the age increases, the number of postmenopausal females classified as MCI C2 and C3 also increases.3,5,8,26 This correlation is expected, as the risk for osteoporosis increases with age, and systemic BMD alterations due to osteoporosis affect the mandible, similar to how they affect other major bones.
The literature screened for this review did not provide sufficient information to determine which index is the most reliable as an auxiliary tool for the identification of females at risk of low BMD. Previous multicenter studies, such as those related to OSTEODENT project,36,37 including postmenopausal females among others, have tried to answer this question by comparing the sensitivity and specificity of distinct indexes. They have verified that radiomorphometric assessments have a rather small influence on the diagnosis of low BMD, and that measuring the cortical width is superior to MCI in detecting patients with osteoporosis.36 However, Calciolari et al38 argued that qualitative indexes such as the MCI that evaluate any kind of cortical erosion can be considered as convenient indicators of reduced BMD, which is associated with at least osteopenia in approximately 80% of the cases.38 Nevertheless, Devlin et al, agreed on and emphasized the importance of this radiographic evidence, associated to a clinical index, as the dentists’ first alert to the risk for osteoporosis, ensuring proper patient reference to DXA examination.36
Oral conditions such as periodontal disease and absence of teeth and their relationship to radiomorphometric indexes were also examined in the included studies.3,17 Since osteoporosis and periodontal disease result in bone resorption, it is speculated that the two diseases may be linked and that osteoporosis could worsen periodontal disease.39 Although such a link seems reasonable, it has not been demonstrated,17 and it is possible that the onset and progression of periodontal disease are more connected to microbial deposits. Notably, no association was found between MCI status and periodontitis.3 Regarding missing teeth, it was hypothesized that, since the teeth are attached in the jaws, osteoporotic modifications could lead to changes in alveolar bone and, as a result, to tooth loss.8 Nevertheless, no correlation between the MCI and the number of missing teeth was found,2 nor was a difference in the number of teeth between osteoporotic and non-osteoporotic postmenopausal females demonstrated.8
Other health alterations such as Type 2 diabetes and their association with the MCI were also investigated.14 Although patients with Type 2 diabetes often present normal or increased BMD, they have a higher risk for fractures, which is attributed to diabetes outcomes, such as neuropathy or impaired vision.40 The authors of the included studies concluded that the MCI correlates with T- and Z-scores obtained from postmenopausal females with Type 2 diabetes,14 suggesting that this index reflects changes in BMD. The MCI has also been shown to correlate with biomarkers, serum calcium levels, and vitamin D3 levels,10,11,27 which are directly associated to modifications in the bone turnover that are inherent to osteoporosis.
Finally, the feasibility of MCI classification using CBCT was also studied. Considering the applicability of MCI classification using CBCT panoramic reconstruction images, Alonso et al19 argued that CBCT is not an adequate imaging modality to apply the MCI classification. The authors explained that MCI classification tends to provide higher values than those expected based on the defects’ visibility in CBCT.19 In contrast, Kato et al9 mentioned that CBCT with 25 mm slice thicknesses seems to be useful for MCI assessment and osteoporosis screening. As the number of cases evaluated in these two studies was relatively small (3019 and 54,9 respectively), further studies with larger samples are required to elucidate these findings.
Conclusions
Considering the literature screened and included in this systematic review, we conclude that MCI is useful as an auxiliary tool for identifying postmenopausal females at risk of low BMD, as it is correlated with skeletal BMD measured by DXA. Other radiomorphometric indexes obtained based on panoramic radiographs, such as the PMI, MI, and MCW, are also valuable as auxiliary tools for this purpose. However, considering the current evidence available in literature, it is not possible to determine which index is the most reliable for identifying postmenopausal females at risk of osteoporosis.
Footnotes
Conflicts of interest: Luciana Munhoz, Lucas Morita, Aline Yukai Nagai, Julia Moreira Santos and Emiko Saito Arita declares no conflicts of interest.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Luciana Munhoz, Email: dra.lucimunhoz@usp.br.
Lucas Morita, Email: lucas.morita@usp.br.
Julia Moreira, Email: jm445629@gmail.com.
Emiko Saito Arita, Email: esarita@usp.br.
REFERENCES
- 1.Levin VA, Jiang X, Kagan R. Estrogen therapy for osteoporosis in the modern era. Osteoporos Int 2018; 29: 1049–55. doi: 10.1007/s00198-018-4414-z [DOI] [PubMed] [Google Scholar]
- 2.Munhoz L, Aoki EM, Cortes ARG, de Freitas CF, Arita ES. Osteoporotic alterations in a group of different ethnicity Brazilian postmenopausal women: an observational study. Gerodontology 2018; 35: 101–9. doi: 10.1111/ger.12322 [DOI] [PubMed] [Google Scholar]
- 3.Mudda JA, Bajaj M, Patil VA. A radiographic comparison of mandibular bone quality in pre- and post-menopausal women in Indian population. J Indian Soc Periodontol 2010; 14: 121–5. doi: 10.4103/0972-124X.70833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res 1994; 102: 68–72. doi: 10.1111/j.1600-0722.1994.tb01156.x [DOI] [PubMed] [Google Scholar]
- 5.Choi IGG, Munhoz L, Arita ES. Assessment of osteoporotic alterations in Brazilian postmenopausal women: a retrospective study. JCDR 2018; 12: ZC34–7. doi: 10.7860/JCDR/2018/34529.11566 [DOI] [Google Scholar]
- 6.White SC. Oral radiographic predictors of osteoporosis. Dentomaxillofac Radiol 2002; 31: 84–92. doi: 10.1038/sj.dmfr.4600674 [DOI] [PubMed] [Google Scholar]
- 7.Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg 2011; 39: 91–2. doi: 10.1016/j.jcms.2010.11.001 [DOI] [PubMed] [Google Scholar]
- 8.Alam T, AlShahrani I, Assiri KI, Almoammar S, Togoo RA, Luqman M. Evaluation of clinical and radiographic parameters as dental indicators for postmenopausal osteoporosis. Oral Health Prev Dent 2020; 18: 499–504. doi: 10.3290/j.ohpd.a44688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kato CN, Tavares NP, Barra SG, Amaral TM, Brasileiro CB, Abreu LG, et al. Digital panoramic radiography and cone-beam CT as ancillary tools to detect low bone mineral density in post-menopausal women. Dentomaxillofac Radiol 2019; 48: 20180254. doi: 10.1259/dmfr.20180254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Golhar SR Motwani M, Khator AD. Panoramic Radiographs vs. Calcaneus Ultrasonography in Diagnosis of Osteoporosis in Postmenopausal Women. Journal of Clinical and Dental Research 2019; 13: ZC38–43. [Google Scholar]
- 11.Nasreen S, Ramesh DNSV, Thriveni R, Bayatnal A, Chowdhury RM, Kattimani S, et al. Assessment of alveolar bone mass using radio morphometric indices in urban and rural postmenopausal women and their correlation with serum vitamin D3 level. Indian J Dent Res 2019; 30: 722–30. doi: 10.4103/ijdr.IJDR_369_18 [DOI] [PubMed] [Google Scholar]
- 12.Grocholewicz K, Janiszewska-Olszowska J, Aniko-Włodarczyk M, Preuss O, Trybek G, Sobolewska E, et al. Panoramic radiographs and quantitative ultrasound of the radius and phalanx III to assess bone mineral status in postmenopausal women. BMC Oral Health 2018; 18: 127. doi: 10.1186/s12903-018-0593-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navabi N, Motaghi R, Rezazadeh M, Balooch H. Relationship between two panoramic radiography indices and bone mineral density of postmenopausal women with osteopenia and osteoporosis. J Dent 2018; 19: 181–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Munhoz L, Cortes ARG, Arita ES. Assessment of osteoporotic alterations in type 2 diabetes: a retrospective study. Dentomaxillofac Radiol 2017; 46: 20160414. doi: 10.1259/dmfr.20160414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pallagatti S, Parnami P, Sheikh S, Gupta D. Efficacy of panoramic radiography in the detection of osteoporosis in post-menopausal women when compared to dual energy X-ray absorptiometry. Open Dent J 2017; 11: 350–9. doi: 10.2174/1874210601711010350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carmo JZB, Medeiros SFde. Mandibular inferior cortex erosion on dental panoramic radiograph as a sign of low bone mineral density in postmenopausal women. Rev Bras Ginecol Obstet 2017; 39: 663–9. doi: 10.1055/s-0037-1606622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kolte RA, Kolte AP, Potey AM. Risk assessment of osteoporosis in pre- and postmenopausal periodontally healthy and chronic periodontitis women with digital panoramic radiographs. J Indian Soc Periodontol 2017; 21: 461–5. doi: 10.4103/jisp.jisp_238_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grgić O, Kovačev-Zavišić B, Veljović T, Novaković-Paro J, Maravić T, Bajkin B. The influence of bone mineral density and bisphosphonate therapy on the determinants of oral health and changes on dental panoramic radiographs in postmenopausal women. Clin Oral Investig 2017; 21: 151–7. doi: 10.1007/s00784-016-1767-6 [DOI] [PubMed] [Google Scholar]
- 19.Alonso MBCC, Vasconcelos TV, Lopes LJ, Watanabe PCA, Freitas DQ. Validation of cone-beam computed tomography as a predictor of osteoporosis using the Klemetti classification. Braz Oral Res 2016; 3031 May 2016. doi: 10.1590/1807-3107BOR-2016.vol30.0073 [DOI] [PubMed] [Google Scholar]
- 20.Jagelavičienė E, Krasauskienė A, Žalinkevičius R, Vaitkevičienė I, Kubilius R. Relationship between the mandibular cortical index and calcaneal bone mineral density in postmenopausal women. Medicina 2016; 52: 125–31. doi: 10.1016/j.medici.2016.02.005 [DOI] [PubMed] [Google Scholar]
- 21.Majumder MI, Harun MASI. Alveolar bone changes in post-menopausal osteopenic and osteoporosis women: an original research. International Journal of Dental and Medical Specialty 2015; 2: 9–14. doi: 10.5958/2394-4196.2015.00010.2 [DOI] [Google Scholar]
- 22.Kim O-S, Shin M-H, Song I-H, Lim I-G, Yoon S-J, Kim O-J, et al. Digital panoramic radiographs are useful for diagnosis of osteoporosis in Korean postmenopausal women. Gerodontology 2016; 33: 185–92. doi: 10.1111/ger.12134 [DOI] [PubMed] [Google Scholar]
- 23.Valerio CS, Trindade AM, Mazzieiro ET, Amaral TP, Manzi FR. Use of digital panoramic radiography as an auxiliary means of low bone mineral density detection in post-menopausal women. Dentomaxillofac Radiol 2013; 42: 20120059. doi: 10.1259/dmfr.20120059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gaur B, Chaudhary A, Wanjari PV, Sunil M, Basavaraj P. Evaluation of panoramic radiographs as a screening tool of osteoporosis in post menopausal women: a cross sectional study. J Clin Diagn Res 2013; 7: 2051–5. doi: 10.7860/JCDR/2013/5853.3403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martínez-Maestre María Ángeles, Corcuera Flores JR, Machuca G, González-Cejudo C, Torrejón R, Castelo-Branco C. Panoramic radiomorphometry and vertebral fractures in Spanish postmenopausal women. Maturitas 2013; 76: 364–9. doi: 10.1016/j.maturitas.2013.08.011 [DOI] [PubMed] [Google Scholar]
- 26.Khojastehpour L, Afsa M, Dabbaghmanesh MH. Evaluation of correlation between width and morphology of mandibular inferior cortex in digital panoramic radiography and postmenopausal osteoporosis. Iran Red Crescent Med J 2011; 13: 181–6. [PMC free article] [PubMed] [Google Scholar]
- 27.Johari Khatoonabad M, Aghamohammadzade N, Taghilu H, Esmaeili F, Jabbari Khamnei H. Relationship among panoramic radiography findings, biochemical markers of bone turnover and hip BMD in the diagnosis of postmenopausal osteoporosis. Iran J Radiol 2011; 8: 23–8. [PMC free article] [PubMed] [Google Scholar]
- 28.Leite AF, Figueiredo PTdeS, Guia CM, Melo NS, de Paula AP. Correlations between seven panoramic radiomorphometric indices and bone mineral density in postmenopausal women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 449–56. doi: 10.1016/j.tripleo.2009.02.028 [DOI] [PubMed] [Google Scholar]
- 29.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. The selection of patients for dental radiographic examinations. Vol 2017: American dental association / U. S. Department of Health and Human Services 2012;. [Google Scholar]
- 31.Benson BW, Prihoda TJ, Glass BJ. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol 1991; 71: 349–56. doi: 10.1016/0030-4220(91)90314-3 [DOI] [PubMed] [Google Scholar]
- 32.Ledgerton D, Horner K, Devlin H, Worthington H. Radiomorphometric indices of the mandible in a British female population. Dentomaxillofac Radiol 1999; 28: 173–81. doi: 10.1038/sj.dmfr.4600435 [DOI] [PubMed] [Google Scholar]
- 33.Dutra V, Devlin H, Susin C, Yang J, Horner K, Fernandes ARC. Mandibular morphological changes in low bone mass edentulous females: evaluation of panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: 663–8. doi: 10.1016/j.tripleo.2006.02.023 [DOI] [PubMed] [Google Scholar]
- 34.Xie Q-F, Ainamo A. Correlation of gonial angle size with cortical thickness, height of the mandibular residual body, and duration of edentulism. J Prosthet Dent 2004; 91: 477–82. doi: 10.1016/j.prosdent.2004.02.020 [DOI] [PubMed] [Google Scholar]
- 35.Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature 2019; 567: 305–7. doi: 10.1038/d41586-019-00857-9 [DOI] [PubMed] [Google Scholar]
- 36.Devlin H, Karayianni K, Mitsea A, Jacobs R, Lindh C, van der Stelt P, et al. Diagnosing osteoporosis by using dental panoramic radiographs: the OSTEODENT project. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 821–8. doi: 10.1016/j.tripleo.2006.12.027 [DOI] [PubMed] [Google Scholar]
- 37.Horner K, Karayianni K, Mitsea A, Berkas L, Mastoris M, Jacobs R, et al. The mandibular cortex on radiographs as a tool for osteoporosis risk assessment: the OSTEODENT project. J Clin Densitom 2007; 10: 138–46. doi: 10.1016/j.jocd.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 38.Calciolari E, Donos N, Park JC, Petrie A, Mardas N. Panoramic measures for oral bone mass in detecting osteoporosis: a systematic review and meta-analysis. J Dent Res 2015; 94(3 Suppl): 17S–27. doi: 10.1177/0022034514554949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Braga V, Morita L, Munhoz L, Lourenço S, Arita E. Periodontal disease defects and mandibular cortical index in lupus patients. Braz Dent Sci 2019; 22: 506–12. doi: 10.14295/bds.2019.v22i4.1808 [DOI] [Google Scholar]
- 40.Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos Int 2007; 18: 427–44. doi: 10.1007/s00198-006-0253-4 [DOI] [PubMed] [Google Scholar]