Abstract
The role of extracorporeal membrane oxygenation (ECMO) in the management of severely ill patients with coronavirus disease 2019 (COVID-19) continues to evolve. The purpose of this study is to review a multi-institutional clinical experience in 100 consecutive patients, at 20 hospitals, with confirmed COVID-19 supported with ECMO. This analysis includes our first 100 patients with complete data who had confirmed COVID-19 and were supported with ECMO. The first patient in the cohort was placed on ECMO on March 17, 2020. Differences by the mortality group were assessed using χ2 tests for categorical variables and Kruskal–Wallis rank-sum tests and Welch’s analysis of variance for continuous variables. The median time on ECMO was 12.0 days (IQR = 8–22 days). All 100 patients have since been separated from ECMO: 50 patients survived and 50 patients died. The rate of survival with veno-venous ECMO was 49 of 96 patients (51%), whereas that with veno-arterial ECMO was 1 of 4 patients (25%). Of 50 survivors, 49 have been discharged from the hospital and 1 remains hospitalized at the ECMO-providing hospital. Survivors were generally younger, with a lower median age (47 versus 56.5 years, p = 0.014). In the 50 surviving patients, adjunctive therapies while on ECMO included intravenous steroids (26), anti-interleukin-6 receptor blockers (26), convalescent plasma (22), remdesivir (21), hydroxychloroquine (20), and prostaglandin (15). Extracorporeal membrane oxygenation may facilitate salvage and survival of selected critically ill patients with COVID-19. Survivors tend to be younger. Substantial variation exists in the drug treatment of COVID-19, but ECMO offers a reasonable rescue strategy.
Keywords: extracorporeal membrane oxygenation, coronavirus, COVID-19, pulmonary failure, acute respiratory distress syndrome, heart failure, outcomes, quality
As of October 4, 2020, 34,963,965 patients around the world have been diagnosed with coronavirus disease 2019 (COVID-19), with 1,034,185 associated deaths (2.96% mortality worldwide).1 Meanwhile, in the USA, as of October 4, 2020, 7,385,837 patients have been diagnosed with confirmed COVID-19, with 209,408 associated deaths to date (2.84% mortality in the USA).1 Most deaths in patients with COVID-19 are due to severe respiratory failure, with a small group succumbing to combined pulmonary and cardiac failure.2,3
We previously published an analysis of 32 COVID-19 patients with severe pulmonary compromise supported with extracorporeal membrane oxygenation (ECMO)4 and concluded that “ECMO may play a useful role in salvaging selected critically ill patients with COVID-19. Additional patient experience and associated clinical and laboratory data must be obtained to further define the optimal role of ECMO in patients with COVID-19 and acute respiratory distress syndrome (ARDS). These initial data may provide useful information to help define the best strategies to care for these challenging patients, and may also provide a framework for much-needed future research about the use of ECMO to treat patients with COVID-19.”4
Several recently published analyses describe cohorts of COVID-19 patients supported with ECMO.4–8 Early data from Wuhan, China, reported an alarmingly high rate of mortality of 83% (5 out of 6) in COVID-19 patients supported with ECMO.5,6 More recent data, however, reveal improved survival of COVID-19 ECMO patients.4,7,8 Both recent individual institutional reports,7 as well as recent reports from multi-institutional registries,8 present detailed analyses with promising results and improvements in survival. Our current report from our multi-institutional database4 corroborates these studies from individual institutions7 and multi-institutional registries,8 but additionally provides more granular, detailed information than a large-scale registry and more generalizable information than analysis from a single institution. It is a fact that the role of ECMO in the management of severely ill patients with COVID-19 continues to evolve. The purpose of this study is to review our multi-institutional clinical experience in 100 consecutive patients with confirmed COVID-19 and severe pulmonary compromise supported with ECMO and to document outcomes and trends in management over time.
Materials and Methods
A prospective, multi-institutional cohort study was conducted on all patients with confirmed COVID-19 who were supported with ECMO at 20 hospitals. A multi-institutional database was created and utilized to assess these patients. This database is prospectively maintained on all patients and has been used for data collection and analysis. The database used is a component of the SpecialtyCare Operative Procedural REgistry, (SCOPETM) [https://specialtycareus.com/]. (SpecialtyCare is a United States provider of Allied Health services, and the SCOPETM Registry contains data from over 1 million perfusion procedures in over 40 states at more than 300 hospitals. This manuscript describes the ECMO experience treating a subset of these patients with COVID-19.) Data captured included patient characteristics, pre-COVID-19 risk factors and comorbidities, confirmation of COVID-19 diagnosis, features of ECMO support, specific medications utilized in an attempt to treat COVID-19, and short-term outcomes through hospital discharge.
This analysis includes our first 100 patients with complete data who had confirmed COVID-19 and were supported with ECMO, starting with our first COVID-19 patient who was placed on ECMO on March 17, 2020. These 100 patients include 96 patients supported with veno-venous ECMO and 4 patients supported with veno-arterial ECMO. The initial cohort included our first 104 patients who had confirmed COVID-19 and were supported with ECMO; four patients (one survivor and three nonsurvivors) were excluded from this analysis because of incomplete data. Inclusion in the analysis required complete data in the following fields: ECMO start date, ECMO end date, outcome (alive or dead), pre-COVID comorbidities (asthma, cancer, chronic renal failure, diabetes, heart disease, hypertension, or obesity), and adjunctive therapeutic interventions (antiviral medications, antimalarial medications, convalescent plasma, interleukin-6 blockers, prostaglandin, or steroids).
Criteria for placement on ECMO were determined by the individual patient care team(s) at each of the 20 hospitals submitting data; all patients were placed on ECMO with severe respiratory failure deemed to be refractory to conventional management. The decision to initiate ECMO, the mode of therapy (i.e., veno-venous, veno-arterial, etc.), and the cannulation strategy were each determined by the individual ECMO Teams, in keeping with their respective individual institutional protocols and guidelines.
Descriptive analysis of the entire cohort was performed using mean, standard deviation, median, and interquartile range (IQR), as appropriate. The primary outcome of interest was mortality during the index hospitalization. Potential differences in categorical variables by the mortality group were assessed using χ2 tests, whereas potential differences in continuous variables by the mortality group were assessed using Kruskal–Wallis rank-sum tests and Welch’s analysis of variance.
Institutional Review Board approval and waiver of the need for consent were obtained. The human subjects research protocol for this study was reviewed and approved by an independent Institutional Review Board. Institutional ethics review board approval was obtained for the use of data from the SCOPETM Database (Protocol #012017, ADVARRA Center for IRB Intelligence, 6940 Columbia Gateway Drive, Suite 110, Columbia, Maryland, USA).
Results
One hundred consecutive patients with COVID-19 were placed on ECMO at 20 different hospitals around the USA. All 100 patients have since been separated from ECMO: 50 patients survived and 50 patients died. Of the 50 survivors, 49 patients have been discharged from the hospital to date. Table 1 provides detailed data about all 100 patients with COVID-19 treated with ECMO. Of note, out of 100 patients, 57 were obese, 39 had hypertension, 37 had diabetes, 20 had asthma, 13 had heart disease, 5 had cancer, and 3 had chronic renal failure. The median time on ECMO was 12 days (IQR = 8–22 days).
Table 1.
Overview of 100 Patients with COVID-19 Supported with ECMO
| Category | Overall | |
|---|---|---|
| Number of Patients | 100 | |
| Days from COVID diagnosis to intubation (mean [SD]) | 4.85 (5.05) | |
| Days from COVID diagnosis to intubation (median [IQR]) | 3.50 (1.00, 8.00) | |
| Days from intubation to cannulation (mean [SD]) | 4.49 (4.33) | |
| Days from intubation to cannulation (median [IQR]) | 4.00 (1.00, 6.00) | |
| Days on ECMO (mean [SD]) | 16.89 (14.89) | |
| Days on ECMO (median [IQR]) | 12.00 (8.00, 22.00) | |
| Hours on ECMO (mean [SD]) | 395.51 (357.36) | |
| Hours on ECMO (median [IQR]) | 269.00 (170.75, 516.00) | |
| Hours on ECMO (minimum, maximum) | 31.00, 2175.00 | |
| Age (mean [SD]) | 50.10 (12.65) | |
| Age (median [IQR]) | 51.00 (40.75, 60.25) | |
| Gender (count [%]) | Female | 34 (34.0) |
| Male | 66 (66.0) | |
| Asthma (count [%]) | No | 80 (80.0) |
| Yes | 20 (20.0) | |
| Cancer (count [%]) | No | 95 (95.0) |
| Yes | 5 (5.0) | |
| Chronic renal failure (count [%]) | No | 96 (97.0) |
| Yes | 3 (3.0) | |
| Diabetes (count [%]) | No | 63 (63.0) |
| Yes | 37 (37.0) | |
| Heart disease (count [%]) | No | 87 (87.0) |
| Yes | 13 (13.0) | |
| Hypertension (count [%]) | No | 61 (61.0) |
| Yes | 39 (39.0) | |
| Obesity (count [%]) | No | 43 (43.0) |
| Yes | 57 (57.0) | |
| One or more comorbid conditions (count [%]) | No | 20 (20.0) |
| Yes | 80 (80.0) | |
| Proned before ECMO (count [%]) | No | 30 (30.0) |
| Yes | 70 (70.0) | |
| CVVH or CRRT used (count [%]) | No | 71 (71.0) |
| Yes | 29 (29.0) | |
| ECMO Type (count [%]) | Veno-arterial | 4 (4.0) |
| Veno-venous | 96 (96.0) | |
| Anticoagulation type (count [%]) | Argatroban | 10 (10.0) |
| Bivalirudin | 6 (6.0) | |
| Heparin | 84 (84.0) | |
| Antiviral medication (count [%]) | No | 66 (66.0) |
| Yes | 34 (34.0) | |
| Convalescent plasma (count [%]) | No | 48 (52.2) |
| Yes | 44 (47.8) | |
| Hydroxychloroquine (count [%]) | No | 63 (63.0) |
| Yes | 37 (37.0) | |
| Interleukin-6 blocker (count [%]) | No | 53 (54.1) |
| Yes | 45 (45.9) | |
| Prostaglandin (count [%]) | No | 66 (66.7) |
| Yes | 33 (33.3) | |
| Steroids (count [%]) | No | 46 (46.0) |
| Yes | 54 (54.0) |
CRRT, continuous renal replacement therapy; CVVH, continuous veno-venous hemofiltration; ECMO, extracorporeal membrane oxygenation; IQR, interquartile range.
Table 2 provides detailed data comparing the characteristics of 50 survivors with 50 nonsurvivors. Survivors were generally younger, with a lower median age (47 versus 56.5 years, p = 0.014). Although time on ECMO was shorter in survivors than nonsurvivors, this trend was not statistically significant: median time on ECMO in survivors was 10.5 days (IQR = 8–19), whereas median time on ECMO in nonsurvivors was 14 days (IQR = 8–26.25).
Table 2.
Comparison of the 50 Survivors to the 50 Nonsurvivors
| Category | Nonsurvivors | Survivors | p-value | |
|---|---|---|---|---|
| Number of Patients | 50 | 50 | ||
| Days from COVID diagnosis to intubation (mean [SD]) | 5.35 (5.90) | 4.35 (4.06) | 0.44 | |
| Days from COVID diagnosis to intubation (median [IQR]) | 3.00 (1.00, 10.00) | 4.00 (1.00, 7.00) | 0.854 | |
| Days from intubation to cannulation (mean [SD]) | 4.33 (4.61) | 4.66 (4.08) | 0.766 | |
| Days from intubation to cannulation (median [IQR]) | 4.00 (1.00, 7.00) | 4.00 (1.75, 6.00) | 0.873 | |
| Days on ECMO (mean [SD]) | 18.58 (17.43) | 15.20 (11.76) | 0.258 | |
| Days on ECMO (median [IQR]) | 14.00 (8.00, 26.25) | 10.50 (8.00, 19.00) | 0.537 | |
| Hours on ECMO (mean [SD]) | 435.44 (418.63) | 355.58 (281.97) | 0.266 | |
| Hours on ECMO (median [IQR]) | 316.00 (170.00, 623.00) | 236.50 (190.00, 444.00) | 0.549 | |
| Hours on ECMO (minimum, maximum) | 31.00, 2175.00 | 61.00, 1344.00 | ||
| Age (mean [SD]) | 53.08 (12.98) | 47.12 (11.69) | 0.018 | |
| Age (median [IQR]) | 56.50 (45.25, 62.00) | 47.00 (40.00, 57.00) | 0.014 | |
| Gender (count [%]) | Female | 15 (30.0) | 19 (38.0) | 0.527 |
| Male | 35 (70.0) | 31 (62.0) | ||
| Asthma (count [%]) | No | 38 (76.0) | 42 (84.0) | 0.453 |
| Yes | 12 (24.0) | 8 (16.0) | ||
| Cancer (count [%]) | No | 47 (94.0) | 48 (96.0) | 1 |
| Yes | 3 (6.0) | 2 (4.0) | ||
| Chronic renal failure (count [%]) | No | 47 (95.9) | 49 (98.0) | 0.986 |
| Yes | 2 (4.1) | 1 (2.0) | ||
| Diabetes (count [%]) | No | 27 (54.0) | 36 (72.0) | 0.098 |
| Yes | 23 (46.0) | 14 (28.0) | ||
| Heart disease (count [%]) | No | 40 (80.0) | 47 (94.0) | 0.074 |
| Yes | 10 (20.0) | 3 (6.0) | ||
| Hypertension (count [%]) | No | 31 (62.0) | 30 (60.0) | 1 |
| Yes | 19 (38.0) | 20 (40.0) | ||
| Obesity (count [%]) | No | 21 (42.0) | 22 (44.0) | 1 |
| Yes | 29 (58.0) | 28 (56.0) | ||
| One or more comorbid conditions (count [%]) | No | 8 (16.0) | 12 (24.0) | 0.453 |
| Yes | 42 (84.0) | 38 (76.0) | ||
| Proned before ECMO (count [%]) | No | 15 (30.0) | 15 (30.0) | 1 |
| Yes | 35 (70.0) | 35 (70.0) | ||
| CVVH or CRRT used (count [%]) | No | 34 (68.0) | 37 (74.0) | 0.659 |
| Yes | 16 (32.0) | 13 (26.0) | ||
| ECMO type (count [%]) | Veno-Arterial | 3 (6.0) | 1 (2.0) | 0.610 |
| Veno-Venous | 47 (94.0) | 49 (98.0) | ||
| Anticoagulation type (count [%]) | Argatroban | 5 (10.0) | 5 (10.0) | 1 |
| Bivalirudin | 3 (6.0) | 3 (6.0) | ||
| Heparin | 42 (84.0) | 42 (84.0) | ||
| Antiviral medication (count [%]) | No | 37 (74.0) | 29 (58.0) | 0.139 |
| Yes | 13 (26.0) | 21 (42.0) | ||
| Convalescent plasma (count [%]) | No | 22 (50.0) | 26 (54.2) | 0.849 |
| Yes | 22 (50.0) | 22 (45.8) | ||
| Hydroxychloroquine (count [%]) | No | 33 (66.0) | 30 (60.0) | 0.679 |
| Yes | 17 (34.0) | 20 (40.0) | ||
| Interleukin-6 blocker (count [%]) | No | 29 (60.4) | 24 (48.0) | 0.303 |
| Yes | 19 (39.6) | 26 (52.0) | ||
| Prostaglandin (count [%]) | No | 31 (63.3) | 35 (70.0) | 0.619 |
| Yes | 18 (36.7) | 15 (30.0) | ||
| Steroids (count [%]) | No | 22 (44.0) | 24 (48.0) | 0.841 |
| Yes | 28 (56.0) | 26 (52.0) |
CRRT, continuous renal replacement therapy; CVVH, continuous veno-venous hemofiltration; ECMO, extracorporeal membrane oxygenation; IQR, interquartile range.
In the 50 surviving patients, adjunctive therapies received while on ECMO were: intravenous steroids (26/50), anti-interleukin-6 receptor monoclonal antibodies – Tocilizumab or Sarilumab – (26/50), convalescent plasma (22/50), antiviral medications – remdesivir – (21/50), hydroxychloroquine (20/50), and prostaglandin (15/50).
This analysis includes all COVID-19 patients placed on ECMO at the 20 hospitals participating in this study during the period of this analysis. None of these 100 patients were placed on ECMO during cardiopulmonary resuscitation (CPR). Extracorporeal CPR (ECPR) was not utilized for COVID-19 patients at these 20 hospitals. Of 50 survivors, 49 were supported only with veno-venous ECMO (98%). Furthermore, only one out of four patients supported with veno-arterial ECMO survived. In the 50 patients who died, documented causes of death were: respiratory failure (26/50), multisystem organ failure including acute kidney injury (7/50), sepsis (5/50), disseminated intravascular coagulation (5/50), cerebral bleeding while on ECMO (4/50) cardiac arrest (2/50), and pneumothorax (1/50).
Figure 1 depicts the distribution of all 100 patients by category of outcomes. Figure 2 depicts the distribution of the age of the patients, comparing the survivors with the nonsurvivors. Figure 3 depicts the distribution of hours on ECMO, comparing the survivors with the nonsurvivors. Figure 4 depicts the monthly trends over time in the utilization of these adjunctive therapies in patients with COVID-19 while on ECMO during the 5 months of this analysis.
Figure 1.
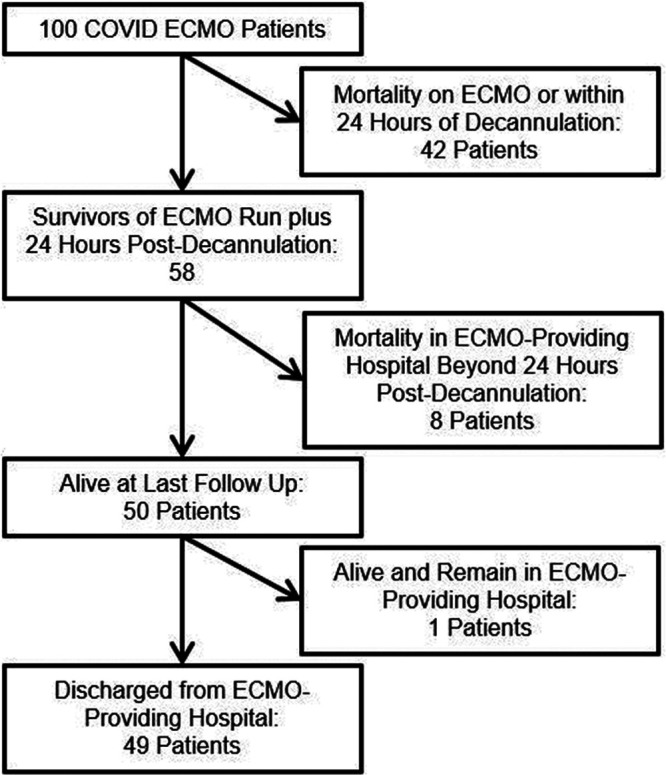
Patient status flowchart: the distribution of all 100 patients by category of outcome.
Figure 2.

Distribution of age – survivors versus nonsurvivors: the distribution of the age of the patients, comparing the survivors with the nonsurvivors.
Figure 3.
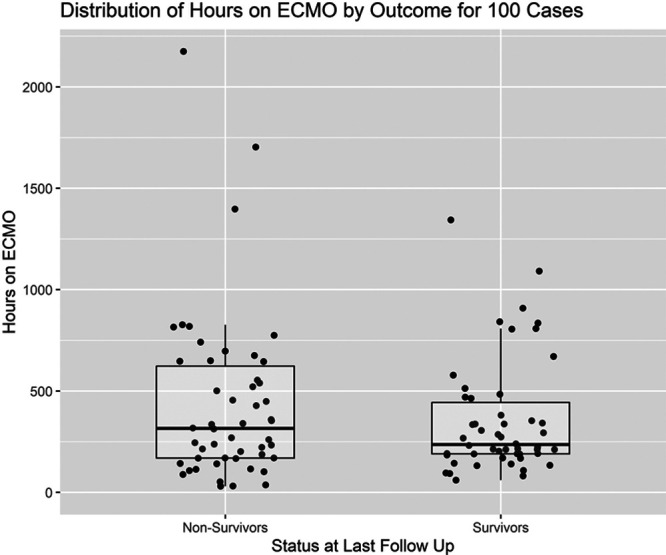
Distribution of hours on ECMO – survivors versus nonsurvivors: the distribution of hours on ECMO, comparing the survivors with the nonsurvivors.
Figure 4.
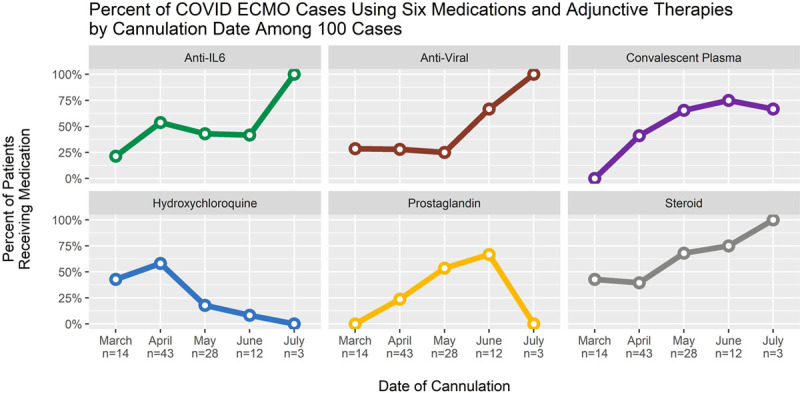
Percent of COVID-19 ECMO patients receiving six adjunctive therapies stratified by month of cannulation. This figure depicts the monthly trends over time in the utilization of six adjunctive therapies in patients with COVID-19 while on ECMO during the 5 months of this analysis: 1.Green line = anti-interleukin-6-receptor monoclonal antibodies (Tocilizumab or Sarilumab). 2. Brown line = antiviral medications (remdesivir). 3. Purple line = convalescent plasma. 4. Blue line = hydroxychloroquine. 5. Yellow line = prostaglandin (Flonan). 6. Gray line = intravenous steroids.
Discussion
Our multi-institutional analysis of 100 consecutive COVID-19 patients who were supported with ECMO and subsequently decannulated provides clear evidence that ECMO facilitates salvage and survival of selected critically ill patients with COVID-19. Survivors tend to be younger. Survival of patients supported only with veno-venous ECMO is 51% (49 out of 96) in our series. Substantial variation exists in the use of adjunctive drugs and therapies in the treatment of COVID-19, but ECMO offers a reasonable rescue strategy.
Clinical guidelines for the management of patients with COVID-19 have been released by the World Health Organization 9 and the Centers for Disease Control and Prevention of the USA.10 Additionally, the Extracorporeal Life Support Organization (ELSO)11 and the American Society for Artificial Internal Organs12 have published guidelines regarding the role of ECMO in treating patients with COVID-19. Nevertheless, the role of ECMO in the management of these challenging patients remains unclear.
Kon et al.7 reported a retrospective analysis of all patients with COVID-19 admitted to New York University Langone Health Manhattan campus from March 10, 2020, to April 24, 2020 who were evaluated for ECMO support. Among 321 patients intubated for COVID-19, 77 patients (24%) were evaluated for ECMO support, and 27 patients (8.4%) were placed on veno-venous ECMO. Zero patients were supported with veno-arterial ECMO. At the time of publication of their study, survival was 96.3%, with only one death to date in more than 350 days of total ECMO support. Thirteen patients (48.1%) remained on ECMO support, and 13 patients (48.1%) were successfully decannulated. Of the 13 decannulated patients, seven patients (25.9%) were discharged from the hospital and six patients (22.2%) remained in the hospital, with four on room air. The authors concluded that “The early outcomes presented here suggest that the judicious use of ECMO support in severe COVID-19 may be clinically beneficial”.7
In contrast, the use of veno-arterial ECMO in patients with COVID-19 has been associated with poor survival. Indeed, in patients with COVID-19, if the extent of end organ damage necessitates veno-arterial ECMO, then the prognosis is poor in comparison to patients with isolated respiratory dysfunction requiring only veno-venous ECMO. Furthermore, if the disease is so severe that the patient has a cardiac arrest refractory to CPR without ECMO, the patient is unlikely to survive and the use of veno-arterial ECMO is likely to be futile.
Barbaro et al.8 reported a cohort study of 1035 patients aged 16 years or older with confirmed COVID-19 who had ECMO support initiated between Jan 16, 2020, and May 1, 2020, at 213 hospitals in 36 countries, using data from the ELSO Registry. At the time of publication, of these 1035 patients, 67 (6%) remained hospitalized, 311 (30%) were discharged home or to an acute rehabilitation center, 101 (10%) were discharged to a long-term acute care center or unspecified location, 176 (17%) were discharged to another hospital, and 380 (37%) died. The estimated cumulative incidence of in-hospital mortality 90 days after the initiation of ECMO was 37.4% (95% CI, 34.4–40.4). Mortality was 39% (380 of 968) in patients with a final disposition of death or hospital discharge. In the subset of patients receiving veno-venous ECMO and characterized as having ARDS, estimated in-hospital mortality 90 days after the initiation of ECMO was 38.0% (95% CI, 34.6–41.5). The ECMO for circulatory support was independently associated with higher in-hospital mortality (hazard ratio 1.89, 95% CI, 1.20–2.97).
The Value of This Analysis
Our study adds to the body of knowledge and the literature by providing more granular multi-institutional data about our cohort of 100 COVID-19 patients supported with ECMO at 20 hospitals. As described in the third paragraph of the Introduction, several previously published analyses have studied the outcomes of ECMO in patients with COVID-19, and these outcomes have been quite heterogenous.4–8 Our analysis of the SpecialtyCare SCOPETM Registry adds another dataset of multi-institutional data to the growing body of literature about the use of ECMO in patients with COVID-19 and demonstrates that support with ECMO facilitates salvage and survival of selected critically ill patients with COVID-19.
In our analysis, survival of patients supported with only veno-venous ECMO was 51% (49 out of 96). Survival in patients requiring veno-arterial ECMO was poor (1 out of 4 = 25%). Our finding of higher survival with veno-venous ECMO in comparison to veno-arterial ECMO in patients with COVID-19 is consistent with the published literature. It is likely that if the extent of end-organ damage necessitates veno-arterial ECMO in patients with COVID-19, then the prognosis is poor in comparison to patients with isolated respiratory dysfunction requiring only veno-venous ECMO. Our study also reveals that, not surprisingly, survivors were younger than non-survivors (median age = 47 in survivors versus 56.5 years in nonsurvivors, P = 0.014). This finding corroborates with the study from Barbaro et al.8 where patients >40 years of age had an increasing risk of mortality compared to those 16–39 years of age.
Finally, our study also documents the previously unpublished finding that substantial variation exists in the use of adjunctive therapies in the treatment of COVID-19. The use of these various adjunctive medications and treatments has changed over time as more information has been learned regarding the role and potential success of these medications.
In patients with COVID-19 supported with ECMO, outcomes are likely largely governed by the viral burden, the extent of inflammatory cascade, and the response of the patients to the different drugs utilized to address this viremia and inflammation. ECMO is acting as a supportive technology, but may not, as such, in and of itself, be the primary driver of mortality or recovery.
Future Directions
Much remains to be learned about the role of ECMO in these patients. From our analysis, no specific demographic, clinical, or laboratory data, to date, is predictive of outcome with ECMO in patients with COVID-19, with the exception of younger age. Similarly, the role of multiple medications in the treatment of COVID-19 remains unclear.
Important additional potential future research projects that will provide valuable information include the following analyses:
An analysis of the variation in processes of care and outcomes across hospitals.
An analysis of the relationship between programmatic ECMO volume and outcome.
An analysis of survival trends over time, from March 2020 to later.
A multivariable analysis of risk factors for survival.
A multivariable analysis of the influence of various medications and adjunctive therapies on survival.
Limitations
This analysis is based on the available data in our database. Additional follow-up is required on all surviving patients. Further patient accrual will enhance continued analysis of outcomes. We plan to continue gathering data to provide additional insight as to guideposts for patient selection and predictors of outcomes. It is our hope that by sharing our experience, other centers and patients may benefit.
Conclusions
Our experience and analysis of 100 consecutive patients at 20 hospitals reveal that ECMO facilitates salvage and survival of selected critically ill patients with COVID-19. Survivors tend to be younger. Survival of patients supported with only veno-venous ECMO is 51% in our cohort. Substantial variation exists in the drug treatment of COVID-19, but ECMO offers a reasonable rescue strategy. Additional gathering and analysis of data will inform appropriate selection of patients and provide guidance as to best use of ECMO in terms of timing, implementation, duration of support, and best criteria for discontinuation. Expansion of studies such as the current analysis presented here will provide a means to further define the role of ECMO in the management of severely compromised patients with COVID-19 and will serve to refine the optimal use of ECMO in these patients, with the goal of continuing to enhance survival.
Footnotes
Disclosure: Dr. Jacobs has received funds from SpecialtyCare. Dr. Firstenberg has received funds from Maquet Cardiovascular and Medtronic. Mr. Stammers, Ms. Mongero, Dr. Tesdahl, Mr. Patel, Mr. Coley, and Dr. Sestokas are paid employees of SpecialtyCare, Inc. The remaining authors have no conflicts of interest to report.
Contributor Information
Jeffrey p. Jacobs, Email: JeffJacobs@msn.com.
Alfred H. Stammers, Email: Al.Stammers@specialtycare.net.
J.W. Awori Hayanga, Email: jeremiah.hayanga@wvumedicine.org.
Michael S. Firstenberg, Email: msfirst@gmail.com.
Linda B. Mongero, Email: Linda.Mongero@specialtycare.net.
Eric A. Tesdahl, Email: Eric.Tesdahl@specialtycare.net.
Keshava Rajagopal, Email: keshava.rajagopal@gmail.com.
Faisal H. Cheema, Email: Faisal.Cheema@hcahealthcare.com.
Kirti Patel, Email: Kirti.Patel@specialtycare.net.
Feriel Esseghir, Email: Feriel.Esseghir@surgery.ufl.edu.
Tom Coley, Email: Tom.Coley@specialtycare.net.
Anthony K. Sestokas, Email: Anthony.Sestokas@specialtycare.net.
Marvin J. Slepian, Email: chairman.syns@gmail.com.
Vinay Badhwar, Email: vinay.badhwar@wvumedicine.org.
References
- 1.John Hopkins Research Center. Coronavirus COVID-19 global cases by the Center for Systems Science and Engineering (CSSE). Available at: https://coronavirus.jhu.edu/map.html. Accessed October 4, 2020
- 2.Clerkin KJ, Fried JA, Raikhelkar J, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020; 141:1648–1655 [DOI] [PubMed] [Google Scholar]
- 3.Madjid M, Safavi-Naeini P, Solomon SD, et al. Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020; 5:831–840 [DOI] [PubMed] [Google Scholar]
- 4.Jacobs JP, Stammers AH, St Louis J, et al. Extracorporeal Membrane Oxygenation in the treatment of severe pulmonary and cardiac compromise in coronavirus disease 2019: Experience with 32 patients. ASAIO J. 2020; 66:722–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8:475–481. Erratum in: Lancet Respir Med 8: e26, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henry BM. COVID-19, ECMO, and lymphopenia: A word of caution. Lancet Respir Med. 2020; 8:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kon ZN, Smith DE, Chang SH, et al. Extracorporeal Membrane Oxygenation Support in severe COVID-19. Ann Thorac Surg. 2021; 111:537–543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barbaro RP, MacLaren G, Boonstra PS, et al. ; Extracorporeal Life Support Organization. Extracorporeal membrane oxygenation support in COVID-19: An international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020; 396:1071–1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. Interim guidance. 3 March 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf. Accessed April 7, 2020
- 10.Centers for Disease Control and Prevention. Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html. Accessed April 7, 2020
- 11.Bartlett RH, Ogino MT, Brodie D, et al. Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J. 2020; 66:472–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajagopal K, Keller S, Akhanti B, et al. Advanced pulmonary and cardiac support of COVID-19 patients: Emerging recommendations from ASAIO - a “living working document.” ASAIO J. 2020; 66:588–598 [DOI] [PMC free article] [PubMed] [Google Scholar]


