Disclaimer:
This is an updated guideline from the Extracorporeal Life Support Organization (ELSO) for the role of extracorporeal membrane oxygenation (ECMO) for patients with severe cardiopulmonary failure due to coronavirus disease 2019 (COVID-19). The great majority of COVID-19 patients (>90%) requiring ECMO have been supported using venovenous (V-V) ECMO for acute respiratory distress syndrome (ARDS). While COVID-19 ECMO run duration may be longer than in non-COVID-19 ECMO patients, published mortality appears to be similar between the two groups. However, data collection is ongoing, and there is a signal that overall mortality may be increasing. Conventional selection criteria for COVID-19–related ECMO should be used; however, when resources become more constrained during a pandemic, more stringent contraindications should be implemented. Formation of regional ECMO referral networks may facilitate communication, resource sharing, expedited patient referral, and mobile ECMO retrieval. There are no data to suggest deviation from conventional ECMO device or patient management when applying ECMO for COVID-19 patients. Rarely, children may require ECMO support for COVID-19–related ARDS, myocarditis, or multisystem inflammatory syndrome in children (MIS-C); conventional selection criteria and management practices should be the standard. We strongly encourage participation in data submission to investigate the optimal use of ECMO for COVID-19.
Keywords: acute respiratory distress syndrome, coronavirus disease 2019, extracorporeal life support organization, extracorporeal life support program, extracorporeal membrane oxygenation, multisystem inflammatory syndrome in children, pandemic
The role of extracorporeal membrane oxygenation (ECMO) support for patients with cardiopulmonary failure due to coronavirus disease 2019 (COVID-19) is evolving. A prominent feature of COVID-19 in critically ill patients is acute respiratory distress syndrome (ARDS). Early in the pandemic, data on ECMO use was limited, and guidance was offered based on best practices at the time.1–4 Very limited case series available at the onset of the pandemic seemed to indicate poor survival for patients with ARDS placed on ECMO.5 However, the role of ECMO for COVID-19–related ARDS and other indications has become more apparent as the pandemic unfolds and evidence is generated.
A multicenter French study of 83 patients with COVID-19–related ARDS managed with ECMO revealed an estimated 60 day mortality of 31%.6 Subsequently, data from the Extracorporeal Life Support Organization (ELSO) Registry reported an estimated cumulative incidence of in-hospital mortality 90 days after ECMO initiation of 37.4%. This report included 1,035 patients with COVID-19 who received ECMO in 36 countries.7 An additional observational study reported 45% mortality for 1,531 patients from 177 centers in Europe and Israel.8
According to prepandemic historical data from the ELSO registry, venovenous (V-V) ECMO results in an approximate mortality of 40%, venoarterial (V-A) 55%, and extracorporeal cardiopulmonary resuscitation (ECPR) 71%. Mean V-V run duration is generally longer (12 days) than V-A (7 days).9 For patients with COVID-19, mortality is similar to historical V-V ECMO mortality; however, mortality is still being determined with ongoing data collection and may be increasing.10 Median (14 days7 and 20 days6) and mean (18 days8) run duration appears to be longer.
In the great majority (>90%) of reported cases, V-V ECMO was utilized for COVID-19.6–8 Some patients with COVID-19 develop myocarditis, massive pulmonary embolism, stress cardiomyopathy, arrhythmias, and acute coronary syndrome,11–13 which may require mechanical circulatory support such as V-A ECMO. Data on V-A ECMO for COVID-19 are limited in the ELSO Registry study and may be found in small case series, making the utility of V-A ECMO for COVID-19–related cardiogenic shock less clear.6–8,14 As a general guide to practice, we recommend the use of ECMO for patients with COVID-19 and severe cardiopulmonary failure who meet traditional criteria and when appropriate resources are available.15
Given the paucity of available data when prior ECMO guidelines were published,1,4 this guideline has been created to summarize currently available literature and offer recommendations to update select areas within the previous guidelines.4 This document will focus on care specific to COVID-19 patients receiving ECMO and recommended alterations in the utilization of ECMO during a pandemic. We recommend referral to existing guidelines for general ECMO practices.2
| Key Recommendations |
|---|
| V-V ECMO may be utilized for patients with COVID-19 and severe respiratory failure with expected outcomes comparable to patients supported with V-V ECMO prepandemic. |
| V-A ECMO may be utilized for patients with COVID-19 and severe cardiac failure; however, the experience is more limited. |
| Mobile ECMO is feasible and may be conducted safely for patients with COVID-19. |
| Organize ECMO centers within geographic regions to coordinate patient referrals, where feasible. |
| Unify patient selection criteria across a geographic region, where feasible. |
| Contraindications for ECMO use should become more stringent as ECMO capacity diminishes. |
| Data submission to facilitate research is essential for our evolving understanding of optimal ECMO care for patients with COVID-19. |
| While some centers have increased their anticoagulation targets, bleeding remains a concern, and there is no data to recommend deviation from conventional anticoagulation goals. |
| There is no data to recommend deviation from conventional ECMO practices, e.g., blood product transfusion thresholds, tracheostomy, endotracheal extubation, rehabilitation, cannulation configuration, or ventilator management. |
| Potential discontinuation of ECMO in the setting of perceived futility should be clearly discussed with patients and their surrogate decision-makers. |
| Rarely, children can require ECMO support for severe ARDS, myocarditis, or multisystem inflammatory disease in children; ECMO patient selection and management should follow conventional guidelines. |
ECMO Program Organization3
International
Centers providing ECMO that are not ELSO member centers are encouraged to join ELSO and contribute to COVID-19–related ECMO cases in the international registry.
We also recommend participation in other key international efforts related to COVID-19 data collection, such as the EuroELSO survey8 and COVID-19 Critical Care Consortium,16,17 to enable a real-time understanding of COVID-19 ECMO practices and to help facilitate crucial research and quality assurance in this area.15
National/Regional
Creating or utilizing existing national and regional ECMO networks is encouraged to coordinate referrals within given geographic areas in which patient transport is possible.18–21
If a patient is referred to an ECMO center that lacks capacity, efforts should be made to redirect the referral to another ECMO center in the region with available capacity, with consideration of availability of mobile ECMO if indicated.
Before ECMO capacity becomes saturated within a given region, we recommend these ECMO networks adapt unified patient exclusion criteria (see below: Patient Selection) at a regional level to promote equitable access to ECMO and to avoid the need for transferring centers to make referrals to multiple ECMO centers.
Mobile ECMO has been safely used to retrieve patients with COVID-19 from referring centers.22–27
Adult and pediatric ECMO centers within a region28 should consider pooling resources, whenever feasible, such as pumps, disposables, or staff, to optimize ECMO capacity from existing resources.
When ECMO equipment resources are constrained, ECMO centers may use ELSO’s Supply Exchange (supplies.elso.org) to improve access to ECMO services when there is a supply disruption, either due to increased demand or an unforeseen limitation in supplies.
ECMO centers and referring centers may use ELSO’s ECMO Availability Map (elso.org) for the purposes of regional coordination of ECMO capacity. This tool is publicly available and updated by ELSO member centers.
Educational webinars and conferences hosted by ELSO and other scientific societies, as well as regional ECMO networks, should be utilized to rapidly disseminate new data to ECMO practitioners as they emerge.
Institutional
In select cases, where regional resources exist to support the creation of new ECMO centers, and it is felt essential to meet increased demand due to the pandemic, this should be undertaken utilizing guidance from ELSO and in close collaboration with other experienced centers to optimize patient outcomes.29,30 Telemedicine could be utilized to facilitate this.31
Tracking of available staffing, equipment, and beds should be performed to determine ECMO capacity on a regular basis. Capacity determination should take into consideration other related services that utilize the same resources as ECMO (cardiothoracic surgery, cardiac critical care, medical critical care, transplant, etc.).32,33
Bedside staffing ratios may be altered under contingency and crisis capacity34 to allow a bedside specialist to care for more patients than usual. This may be facilitated using methods for remote monitoring and co-locating patients who are receiving ECMO (including both COVID-19 and non-COVID-19 ECMO patients, as appropriate for the individual hospital).
If surgical procedures involving cardiopulmonary bypass are suspended, perfusionists may be deployed to the bedside to relieve ECMO specialists for other duties, where applicable.
Patient Selection
ECMO is a finite resource and requires the utilization of other finite resources, such as intensive care unit (ICU) beds and staffing. Patient selection must be judicious and equitable and should become more stringent as capacity diminishes.32,35,36
Indications
Indications for ECMO initiation should remain unchanged during a pandemic, and we refer to ELSO guidelines and established literature outlining these indications.1,2,4,15,37–40
Conventional therapies for ARDS should be applied according to the standard algorithm, leading to the use of ECMO after other measures have been attempted, especially prone positioning, unless contraindicated (Figure 1).41 It should be emphasized that low-pressure and low-volume ventilation should be adhered to, with consideration of ECMO if unable to safely mechanically ventilate the patient, even if oxygenation is relatively intact.
While it may be tempting to stretch the use of conventional therapy to avoid placing patients on ECMO due to resource constraints, there is no evidence to support delaying ECMO initiation when it is indicated. We recommend ECMO patient selection as in Figure 1. Outcomes with delayed ECMO initiation may be worse and run duration may be longer, offsetting any potential benefit from attempted conservation of resources.42–44
Patients who are deteriorating in non-ECMO centers should be referred early for ECMO consideration to allow for safe transport or time to organize mobile ECMO rescue in appropriate patients.22
Survival with V-V ECMO for COVID-19–related pneumonia and ARDS6–8 is similar to historical survival data for other causes of acute severe respiratory failure meeting V-V indications in the ELSO Registry.9 This suggests that COVID-19 could be considered similarly to other causes of reversible infectious pulmonary disease, with awareness that COVID-19 patients may require longer run times.6–8,45–47 However, mortality in this population may be increasing over time and updated data should be considered in decision-making (elso.org).
It is currently unknown if COVID-19 patients requiring V-A ECMO have similar survival compared with historical data.
Figure 1.
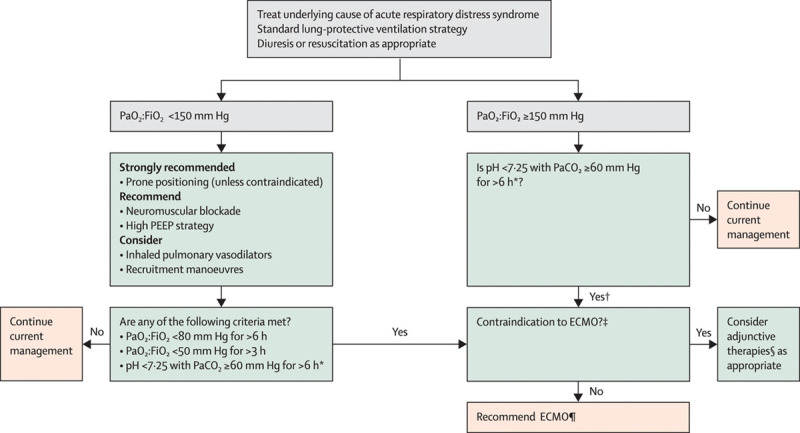
Algorithm for management of acute respiratory distress syndrome, including indications for ECMO. *With respiratory rate increased to 35 breaths per minute and mechanical ventilation settings adjusted to keep a plateau airway pressure of <32 cm H2O. †Consider neuromuscular blockade. ‡There are no absolute contraindications that are agreed upon except end-stage respiratory failure when lung transplantation will not be considered; exclusion used in the EOLIA trial can be taken as a conservative approach to ECMO contraindications. ∫For example, neuromuscular blockade, high PEEP strategy, inhaled pulmonary vasodilators, recruitment maneuvers, and high-frequency oscillatory ventilation. ¶Recommend early ECMO as per EOLIA trial criteria; salvage ECMO, which involves deferral of ECMO initiation until further decompensation (as in the crossovers to ECMO in the EOLIA control group), is not supported by the evidence but might be preferable to not initiating ECMO at all in such patients. Credit: Abrams et al.39. ECMO, extracorporeal membrane oxygenation; EOLIA, Extracorporeal Membrane Oxygenation to Rescue Lung Injury in Severe Acute Respiratory Distress Syndrome; PaCO2, partial pressure of carbon dioxide in arterial blood; PaO2:FiO2, ratio of partial pressure of oxygen in arterial blood to the fractional concentration of oxygen in inspired air; PEEP, positive end-expiratory pressure.
Contraindications
We recommend that ECMO centers establish descriptions for levels of diminishing ECMO capacity,34 and capacity should be tightly linked to exclusion criteria, that is, when capacity diminishes, exclusion criteria become more stringent based on characteristics associated with increased mortality (Figure 2),7,15,32,44,48,49 and longer run duration.50,51 Of note, there is survival and run-time variability depending on the indication for ECMO and individual patient characteristics, and thus each ECMO referral should be considered on a case-by-case basis.
Mortality increases with prolonged exposure to mechanical ventilation before ECMO44; the additional impact of prolonged exposure to high-flow nasal cannula or noninvasive positive-pressure ventilation before mechanical ventilation is currently unknown.
COVID-19 patients receiving ECMO may consume more resources to meet personal protective equipment (PPE) requirements, and this may be a factor in patient selection by necessity when PPE is limited.
Risks and benefits of providing ECPR for patients who have COVID-19 or whose status is unknown, for example, out-of-hospital cardiac arrest, should be carefully considered given the increased potential for PPE breach and lower historical survival with ECPR compared with most other uses of ECMO.49 However, ECPR outcomes also vary considerably according to patient population based on factors that include witnessed or unwitnessed arrest, in-hospital versus out-of-hospital arrest, duration, and etiology of arrest. Thus, context matters in the decision of whether or not to proceed with ECPR, and centers should a priori determine whether or not they will provide ECPR for patients with COVID-19 and patients with unknown COVID-19 status.
Systems should be prepared to rapidly identify changes in capacity and communicate resultant changes in exclusion criteria to their ECMO teams and regional networks to continually optimize the benefit-to-resource utilization ratio.
Figure 2.
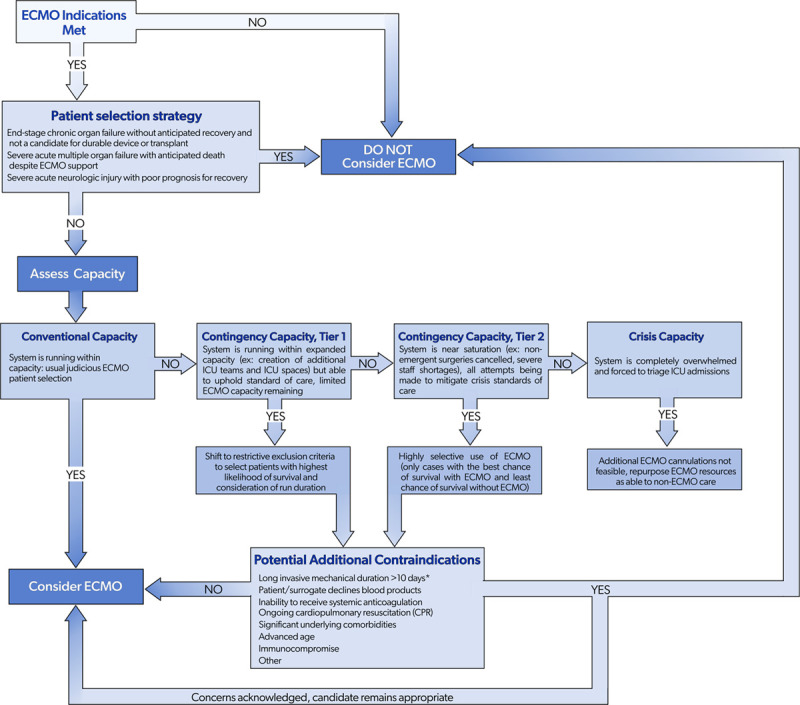
Contraindications algorithm for V-A and V-V ECMO use (COVID-19 and non-COVID-19) during a pandemic based on system capacity. *The impact of duration on high-flow nasal cannula and/or noninvasive mechanical ventilation in addition to invasive mechanical ventilation is unknown. COVID-19, coronavirus disease 2019; CPR, cardiopulmonary resuscitation; ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; PaCO2, partial pressure of carbon dioxide in arterial blood; PaO2:FiO2, ratio of partial pressure of oxygen in arterial blood to the fractional concentration of oxygen in inspired air; PEEP, positive end-expiratory pressure; V-A, venoarterial; V-V, venovenous.
Cannulation Strategies
Conventional two-site (V-A and V-V) and multisite, e.g., veno-arteriovenous (V-AV), cannulation strategies, as well as V-V dual-lumen cannulas, as needed to address the underlying problems, are appropriate for use in patients with COVID-19.
There may be a role for the use of dual-lumen single cannula right ventricular assist device (right atrium to pulmonary artery) in patients with COVID-19 pneumonia; however, the evidence is limited.46,47
Ongoing Care During ECMO
Routine management of the patient receiving ECMO is outside the scope of this guideline, and we refer to previously published guidelines2 and reviews37,52,53 Recommendations on disease modifying agents are also outside of the scope of this guideline, and we refer to published national and international guidelines.54–56 A concise list of COVID-19 ECMO-specific recommendations is provided in Figure 3.
Figure 3.
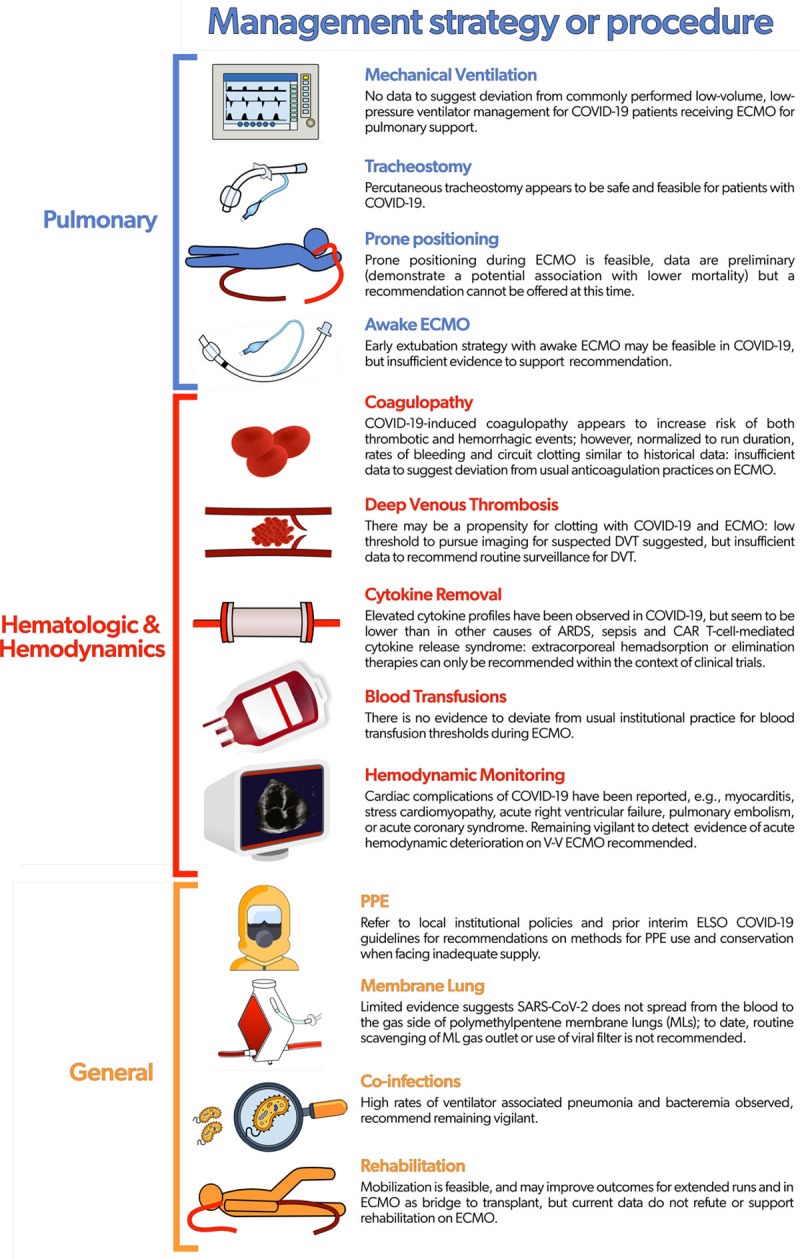
Recommendations for ongoing care for patients with COVID-19 receiving ECMO. ARDS, acute respiratory distress syndrome; CAR, chimeric antigen receptor; COVID-19, coronavirus disease 2019; DVT, deep venous thrombosis; ECMO, extracorporeal membrane oxygenation; ELSO, Extracorporeal Life Support Organization; ML, membrane lung; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; V-V, venovenous.
Pulmonary
There are no data to suggest deviation from commonly performed ventilator management (very low-pressure, low-volume ventilation) for patients receiving V-V ECMO with COVID-19.2,57
Percutaneous tracheostomy appears to be safe and feasible for patients with COVID-19.58–60
Prone positioning during ECMO is feasible61 and 81% of COVID-19 patients in one study were placed in the prone position.6 Preliminary data demonstrate a potential association of prone positioning on ECMO with lower mortality.15,62,63 However, a recommendation cannot be offered at this time.
An early extubation strategy with awake ECMO may be feasible for patients with COVID-19.46,47 However, there is currently no data to support this strategy over one in which the patient remains endotracheally intubated during ECMO.
Hematologic and Hemodynamic Monitoring
COVID-19–induced coagulopathy appears to include both thrombotic and bleeding events.64–66 Specific ramifications for ECMO include circuit clotting,67,68 higher than previously reported rates of pulmonary embolism,6 and intracranial hemorrhage.69–72 However, when normalized to ECMO run duration, rates of bleeding, and circuit clotting in patients with COVID-19 are similar to historical data, in one observational study.7 Balancing hematologic derangements with ECMO anticoagulation is complex. Many centers have increased their anticoagulation targets but bleeding remains a concern, and there are insufficient data to suggest deviation from usual anticoagulation practices2 for patients with COVID-19 receiving ECMO.
There are insufficient data to recommend routine surveillance for deep venous thrombosis for patients with COVID-1973; however, we recommend a low threshold to pursue imaging for suspected deep venous thrombosis, including after decannulation, given that there may be a propensity for clotting in COVID-19 patients during ECMO.74,75
While elevated cytokine profiles have been observed in patients with COVID-19, these seem to be lower than in non-COVID-19–related ARDS and sepsis and much lower than chimeric antigen receptor (CAR) T-cell-mediated cytokine release syndrome,76 although evidence is needed to provide further insights. Therefore, extracorporeal hemadsorption or elimination therapies can only be recommended within the context of clinical trials.77
There is no evidence to deviate from usual institutional practices for blood transfusion thresholds during ECMO.78
We recommend remaining vigilant for acute hemodynamic deterioration during V-V ECMO. This may occur due to cardiac complications of COVID-19, for example, myocarditis, stress cardiomyopathy, acute right ventricular failure,79,80 pulmonary embolism, or acute coronary syndrome.
General
We refer the reader to local institutional policies and prior interim ELSO COVID-19 guidelines for recommendations on PPE use and conservation methods when facing inadequate supply.3,4
There is no evidence to suggest that virions can travel out of the exhaust of a polymethylpentene membrane lung, and thus routine scavenging is not recommended, although the current evidence is limited.81
Remain vigilant for bacterial coinfection and superinfection given high observed rates of ventilator-associated pneumonia and bacteremia in some studies.6,82–85
Mobilization of patients is feasible while undergoing ECMO46,86–88 and may be necessary to achieve favorable outcomes for patients with extended ECMO runs and those bridging to transplant. However, there are currently insufficient data to refute or support mobilization specifically for patients receiving ECMO for acute COVID-19.
Intra-hospital transport can be safely performed, and thus traveling within the hospital should be pursued when indicated, for example, radiology, unit relocation, etc.89
Weaning and Discontinuation of ECMO
Centers should determine a priori whether they plan to offer lung or heart transplant or durable ventricular assist devices to patients with COVID-19 who are unable to wean from ECMO, as this will have implications for decision making surrounding continuation or discontinuation of ECMO in patients who are not recovering. Regional referral can be considered if transplant or durable device placement is not locally available.
If patients are bridging to recovery, the consent process should include a discussion outlining criteria with family for when ECMO support will be stopped once it is determined to be unlikely to provide further benefit to the patient. In this case, the patient will be returned to conventional therapy or consideration given for withdrawal of life-sustaining therapies (futility and principle of proportionate therapy).35
It is challenging to determine futility in the patient receiving V-V ECMO with single-organ failure awaiting pulmonary recovery. It is important to note that prolonged hospitalization in this cohort may not portend a higher mortality rate: patients hospitalized at 40 days had an estimated 90 day mortality of 14% in the ELSO Registry study.7
Duration on ECMO (>90% V-V) for COVID-19 from three large observational studies was median 13.9 days (interquartile range [IQR], 7.8–23.3 days),7 median 20 days (IQR, 10–40 days),6 and mean 18 days.8 It is important to note that successful native lung recovery has been reported after prolonged (>28 days) V-V ECMO support.90
The role of chest imaging in determining futility while on V-V ECMO is unknown.
Lung transplantation has been successfully pursued for some COVID-19 patients who were receiving ECMO, with single-organ failure, but without recovery of adequate lung function. The timing for when this should be considered, and for when further attempts at awaiting native pulmonary recovery should be abandoned, remain unclear.91–93
ECMO in Children with COVID-19
Acute infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in children is most commonly either asymptomatic or associated with only mild respiratory disease. Occasionally, however, this can lead to life-threatening hypoxemic respiratory failure with ARDS due to severe COVID-19 or, rarely, acute heart failure and cardiogenic shock secondary to myocarditis. Furthermore, a minority can develop multisystem inflammatory syndrome in children (MIS-C) within 4 weeks of exposure to the virus, presenting with clinical and laboratory evidence of systemic inflammation, which can rapidly progress to shock.94 Most children who require intensive care with acute COVID-19 or MIS-C receive targeted therapy, recover and are discharged home.95,96 Rarely, children with severe disease ultimately require ECMO.97–99 While the basic principles of ECMO for COVID-19 in children do not significantly differ from ECMO use for other diseases, there are some special nuances that a pandemic presents that should be considered in the decision-making process.
Candidacy
We recommend applying similar principles currently published in ELSO guidelines2 for patient selection of pediatric COVID-19–associated respiratory failure and MIS-C.
Cannulation
Standard cannulation strategies appropriate for any pediatric ECMO patient should be used. There is no evidence to support alteration of cannulation strategy for patients with COVID-19.
Appropriately sized dual-lumen or two-site cannulation approach is commonly employed for V-V support of pediatric respiratory failure patients without circulatory collapse.
V-A support is indicated for cardiac compromise associated with COVID-19–related myocarditis and MIS-C and for patients with severe respiratory disease where adequately sized V-V cannulation cannot be accomplished.
Management Principles
We recommend the use of standard pediatric institutional ECMO protocols for the management of pediatric patients with COVID-19. There is no evidence to recommend changes in anticoagulation, sedation, or other protocols for patients with COVID-19.
Management of the underlying COVID-19 and MIS-C diseases should follow institutional and national guidelines.100
Conclusions
Patients with COVID-19 initially exhibited similar mortality when supported with V-V ECMO as compared to historical data in patients with other causes of acute severe respiratory failure. However, mortality may be increasing and is still being determined with ongoing data collection. Data are still limited regarding V-A ECMO support in COVID-19. That said, ECMO may be utilized for adult patients with COVID-19 and severe cardiopulmonary failure when resources permit. Children may require ECMO support for severe ARDS, myocarditis or MIS-C, and ECMO patient selection and management should follow conventional guidelines. ECMO centers should consider forming networks within geographic regions to pool resources and coordinate patient referrals for ECMO. Submission of patient data is essential for ongoing research to enhance the care of patients receiving ECMO for COVID-19–related cardiopulmonary failure. When conventional capacity exists, indications and contraindications for ECMO should remain unchanged; however, as hospital system capacity diminishes, contraindications for ECMO use should become more stringent based on characteristics associated with increased mortality and longer run duration. There are no data to recommend deviation from conventional ECMO management for COVID-19 patients during their ECMO run, for example, anticoagulation, blood product transfusion thresholds, tracheostomy, endotracheal extubation, mobility, cannulation configuration, or ventilator management. The criteria surrounding ECMO discontinuation for perceived futility should be clearly discussed with patients and families.
Acknowledgment
The authors would like to recognize and thank the team of worldwide extracorporeal membrane oxygenation (ECMO) experts led by Dr. Kiran Shekar who drafted the “Interim ECMO for COVID-19 Guidelines.” Their worldwide collaboration, expertise, and guidance helped the ECMO community during the first year of the pandemic and this manuscript builds on their important work.
ELSO COVID-19 Working Group Members: Kiran Shekar (Adult Intensive Care Services The Prince Charles Hospital, Brisbane, Queensland, Australia); Giles Peek (University of Florida, Shands Hospital for Children, Gainesville, Florida); Jenelle Badulak (University of Washington, Seattle, Washington); Udo Boeken (Department of Cardiac Surgery, University Hospital, Duesseldorf, Germany); Heidi J. Dalton (INOVA Fairfax Medical Center, Falls Church, Virginia); Lovkesh Arora (University of Iowa Hospital & Clinics, Iowa City, Iowa); Bishoy Zakhary (Oregon Health and Science University, Portland, Oregon); Lakshmi Raman (University of Texas Southwestern Medical Center, Dallas, Texas); Kollengode Ramanathan (National University Hospital, Singapore); Joanne Starr (CHOC Children’s Hospital, Orange, California); Abdul Raham al-fares (Al-Amiri and Jaber Al-Ahmed Hospitals, Ministry of Health, Kuwait); Abhishek Jha (St. George’s NHS Foundation Trusts, London, United Kingdom); Alex Bribriesco (Billings, Montana); Ayed Y. Asiri (Prince Mohammed Bin Abdulaziz Hospital, Riyadh, Saudi Arabia); Alwardt Cory (Mayo Clinic Hospital, Phoenix, Arizona); Angela Jarden (Cleveland Clinic Children’s, Cleveland, Ohio); Aparna Hoskote (Great Ormond Street Hospital for Children NHS Foundation Trust, London, United Kingdom); Arpan Chakraborty (Medica Superspecialty Hospital, Kolkata, India); Asif A. Saberi (Medical College of Georgia at Augusta State University, Augusta, Georgia); Bindu Akkanti (UT McGovern Medical School, Houston, Texas); Ayed Asiri (Prince Mohammed Bin Abdulaziz Hospital, Riyadh, Saudi Arabia); Charles McDonald (The Prince Charles Hospital, Brisbane, Queensland, Australia); Chris Harvey (Glenfield Hospital, Leicester, United Kingdom); Chris Wells (University of Maryland Medical Center, Baltimore, Maryland); Daniel Duerschmied (Medical Center, University of Freiburg, Freiburg, Germany); Daniel Loverde (Billings Clinic Hospital, Billings, Montana); Debra Bristow (The Prince Charles Hospital, Brisbane, Queensland, Australia); Donnie Harrington (University of Florida, Shands Hospital, Gainesville, Florida); Emma Haisz (Lady Cilento Hospital, Brisbane, Queensland, Australia); Emma Ridley (The Alfred, Monash University, Melbourne, Victoria, Australia); Eric Sy (University of Saskatchewan, Saskatoon, Saskatchewan, Canada); Erika Dal Checco (S.Orsola-Malpighi University Hospital, Bologna, Italy); Gary Schwartz (Baylor University Medical Center, Dallas, Texas); Grace van Leeuwen (Sidra Medicine, Doha, Qatar); Hiroyuli Tanaka (Kyoto Medical Center, Kyoto, Japan); Jae Seung Jung (Korea University Medicine, Seoul, Republic of Korea); Jason Frischer (Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio); Jayesh Dhanani (Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia); Jeff Dellavolpe (Methodist Hospital, San Antonio, Texas); Ju Zhao (Fuwai Hospital Chinese Association of Medical Science, Beijing, People's Republic of China); Jumana Haji (Aster CMI Hospital, Bangalore, India); Lorenzo Grazioli (Papa Giovanni XXIII Hospital, Bergamo, Italy); Mark Dennis (Royal Prince Alfred Hospital, Sydney, New South Wales, Australia); M. Velia Antonini (1st Intensive Care Unit, University Hospital of Parma, Parma, Italy); Nicolas Brozzi (Cleveland Clinic Florida, Weston, Florida); Omar Alibrahim (Jacob’s School of Medicine, University of Buffalo, Buffalo, New York); Peter Lai (St Mary’s Hospital, Hong Kong); Peter Von Homeyer (University of Washington, Seattle, Washington); Shekhar Raj (Driscoll Children’s Hospital, Corpus Christi, Texas); Sravanthi Nandavaram (University of Kentucky, Lexington, Kentucky); Stephen Keller (Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts); Stephanie Mateev (University of California, Davis, California); Suzanne Bennet (UC Health-University of Cincinnati Medical Center, Cincinnati, Ohio); Thomas Müller (University Hospital Regensburg, Regensburg, Germany); Timothy D. Smith (The Christ Hospital and Lindner Research Center, Cincinnati, Ohio); Usman Asad (Department of Anesthesiology and Critical Care, University of Pennsylvania, Philadelphia, Pennsylvania); and Vincent Pellegrino (The Alfred, Melbourne, Victoria, Australia). ELSO Staff: Elaine Cooley, Peter Rycus, and Christine Stead.
Footnotes
Disclosure: Dr. Stead is a chief executive officer of the Extracorporeal Life Support Organization (ELSO). Dr. Paden is a president of the ELSO. Multiple patents and intellectual property regarding a novel renal replacement device to be used with extracorporeal membrane oxygenation (device not discussed in this article). Dr. Bartlett serves on ELSO’s board of directors. Dr. Barrett received grants from Getinge and ALung. Dr. Combes received grants from Getinge and personal fees from Getinge, Baxter, and Xenios outside the submitted work. Dr. Lorusso is a consultant for Medtronic, LivaNova, and Eurosets (all honoraria paid to the University). Dr. Ogino is a past-president of the ELSO; he serves on ELSO board of directors. Dr. Schmidt receives lecture fees from Getinge, Xenios, and Drager outside the submitted work. Dr. Shekar acknowledges research support from Metro North Hospital and Health Service. Dr. MacLaren serves on ELSO’s board of directors. Dr. Brodie receives research support from ALung Technologies. He has been on the medical advisory boards for Baxter, Abiomed, Xenios, and Hemovent. He is the President-elect of the ELSO. The remaining authors have no conflicts of interest to report.
Drs. MacLaren and Brodie are co-senior authors.
ELSO COVID-19 Working Group Members are listed in acknowledgment section.
Contributor Information
M. Velia Antonini, Email: velian@unimore.it.
Christine M. Stead, Email: cstead@elso.org.
Lara Shekerdemian, Email: lssheker@texaschildrens.org.
Lakshmi Raman, Email: lraman@elso.org.
Matthew L. Paden, Email: mpaden@elso.org.
Cara Agerstrand, Email: ca2264@cumc.columbia.edu.
Robert H. Bartlett, Email: robbar@med.umich.edu.
Nicholas Barrett, Email: Nicholas.Barrett@gstt.nhs.uk.
Alain Combes, Email: combes001@gmail.com.
Roberto Lorusso, Email: roberto.lorussobs@gmail.com.
Mark T. Ogino, Email: mogino@elso.org.
Giles Peek, Email: gilespeek@ufl.edu.
Vincent Pellegrino, Email: succenyl@gmail.com.
Leonardo Salazar, Email: demotucordis@gmail.com.
Matthieu Schmidt, Email: matthieuschmidt@yahoo.fr.
Kiran Shekar, Email: Kiran.Shekar@health.qld.gov.au.
Graeme MacLaren, Email: graeme_maclaren@nuhs.edu.sg.
Daniel Brodie, Email: hdb5@cumc.columbia.edu.
References
- 1.Bartlett RH, Ogino MT, Brodie D, et al. Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J. 2020; 66:472–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Extracorporeal Life Support Organization. ECMO and ECLS > Resources > Guidelines. Available at: https://www.elso.org/Resources/Guidelines.aspx. Accessed December 27, 2019
- 3.Ramanathan K, Antognini D, Combes A, et al. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 2020; 8:518–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shekar K, Badulak J, Peek G, et al. Extracorporeal life support organization COVID-19 interim guidelines: A consensus document from an International Group of Interdisciplinary Extracorporeal Membrane Oxygenation Providers. ASAIO J. 2020; 66:707–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henry BM, Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): Pooled analysis of early reports. J Crit Care. 2020; 58:27–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmidt M, Hajage D, Lebreton G, et al. ; Groupe de Recherche Clinique en REanimation et Soins intensifs du Patient en Insuffisance Respiratoire aiguE (GRC-RESPIRE) Sorbonne Université; Paris-Sorbonne ECMO-COVID investigators. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: A retrospective cohort study. Lancet Respir Med. 2020; 8:1121–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barbaro RP, MacLaren G, Boonstra PS, et al. ; Extracorporeal Life Support Organization. Extracorporeal membrane oxygenation support in COVID-19: An international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020; 396:1071–1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorusso R, Combes A, Lo Coco V, De Piero ME, Belohlavek J; EuroECMO COVID-19 WorkingGroup; Euro-ELSO Steering Committee. ECMO for COVID-19 patients in Europe and Israel [published online ahead of print January 9, 2021]. Intensive Care Med doi: 10.1007/s00134-020-06272-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Extracorporeal Life Support Organization. ECMO and ECLS > Registry > Statistics > International Summary. Available at: https://www.elso.org/Registry/Statistics/InternationalSummary.aspx. Accessed November 18, 2020
- 10.Extracorporeal Life Support Organization. Full COVID-19 Registry Dashboard. Data unpublished. Available at: https://www.elso.org/Registry/FullCOVID19RegistryDashboard.aspx. Accessed December 6, 2020
- 11.Kang Y, Chen T, Mui D, et al. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020; 106:1132–1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shafi AMA, Shaikh SA, Shirke MM, Iddawela S, Harky A. Cardiac manifestations in COVID-19 patients-A systematic review. J Card Surg. 2020; 35:1988–2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 2020; 2019:1648–1655 [DOI] [PubMed] [Google Scholar]
- 14.Fried JA, Ramasubbu K, Bhatt R, et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020; 141:1930–1936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacLaren G, Combes A, Brodie D. What’s new in ECMO for COVID-19? Intensive Care Med. 2021; 47:107–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.COVID-19 Critical Care Consortium. Available at: https://www.covid-critical.com/. Accessed December 17, 2020.
- 17.Li Bassi G, Suen J, Barnett AG, et al. ; COVID-19 Critical Care Consortium Investigators. Design and rationale of the COVID-19 Critical Care Consortium international, multicentre, observational study. BMJ Open. 2020; 10:e041417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warren A, Camporota L, Vuylsteke A. Surge capacity and updated admission criteria: Response of the NHS-commissioned national respiratory extracorporeal membrane oxygenation network to the COVID-19 pandemic. Br J Anaesth. 2020; 125:e282–e283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li C, Hou X, Tong Z, Qiu H, Li Y, Li A; Chinese Society of Extracorporeal Life Support (CSECLS). Extracorporeal membrane oxygenation programs for COVID-19 in China. Crit Care. 2020; 24:317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leow L, Papadimas E, Subbian SK, MacLaren G, Ramanathan K. Organization of extracorporeal membrane oxygenation services for COVID-19 [published online ahead of print September 30, 2020]. Asian Cardiovasc Thorac Ann doi: 10.1177/0218492320962932 [DOI] [PubMed] [Google Scholar]
- 21.Takeda S. Nationwide system to centralize decisions around extracorporeal membranous oxygenation use for severe COVID-19 pneumonia in Japan. Acute Med Surg. 2020; 7:e510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daniela M, Felipe S, Van Nicolette SJ, et al. Mobile ECMO in COVID-19 patient: Case report [published online ahead of print September 19, 2020]. J Artif Organs doi: 10.1007/s10047-020-01209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brozzi N, Hernandez-Montfort J, Noguera E, et al. Successful mobile extracorporeal membrane oxygenator for COVID-19 severe respiratory failure. J Card Surg. 2020; 35:3655–3657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Imaeda T, Hattori N, Abe R, et al. Interhospital transportation of a COVID-19 patient undergoing veno-venous extracorporeal membrane oxygenation by helicopter [published online ahead of print October 3, 2020]. Am J Emerg Med doi: 10.1016/j.ajem.2020.09.089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haye G, Fourdrain A, Abou-Arab O, Berna P, Mahjoub Y. COVID-19 Outbreak in France: Setup and activities of a mobile extracorporeal membrane oxygenation team during the first 3 weeks. J Cardiothorac Vasc Anesth. 2020; 34:3493–3495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salas de Armas IA, Akkanti BH, Janowiak L, et al. Inter-hospital COVID ECMO air transportation [published online ahead of print November 25, 2020]. Perfusion doi: 10.1177/0267659120973843 [DOI] [PubMed] [Google Scholar]
- 27.Rafiq MU, Valchanov K, Vuylsteke A, et al. Regional extracorporeal membrane oxygenation retrieval service during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic: An interdisciplinary team approach to maintain service provision despite increased demand. Eur J Cardiothorac Surg. 2020; 58:875–880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gerall C, Cheung EW, Klein-Cloud R, Kreines E, Brewer M, Middlesworth W. Allocation of resources and development of guidelines for extracorporeal membrane oxygenation (ECMO): Experience from a pediatric center in the epicenter of the COVID-19 pandemic. J Pediatr Surg. 2020; 55:2548–2554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barbaro RP, Odetola FO, Kidwell KM, et al. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015; 191:894–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: The potential role of extracorporeal membrane oxygenation. JAMA. 2020; 323:1245–1246 [DOI] [PubMed] [Google Scholar]
- 31.Lopez-Magallon AJ, Saenz L, Lara Gutierrez J, et al. Telemedicine in pediatric critical care: A retrospective study in an international extracorporeal membrane oxygenation program. Telemed J E Health. 2018; 24:489–496 [DOI] [PubMed] [Google Scholar]
- 32.Abrams D, Lorusso R, Vincent JL, Brodie D. ECMO during the COVID-19 pandemic: When is it unjustified? Crit Care. 2020; 24:507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sromicki J, Schmiady M, Maisano F, Mestres CA. ECMO therapy in COVID-19: An experience from Zurich [published online ahead of print October 30, 2020]. J Card Surg doi: 10.1111/jocs.15147 [DOI] [PubMed] [Google Scholar]
- 34.Christian MD, Devereaux AV, Dichter JR, Rubinson L, Kissoon N. Introduction and executive summary: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014; 146:8S–34S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Di Nardo M, Dalle Ore A, Starr J, Cecchetti C, Amodeo A, Testa G. Ethics and extracorporeal membrane oxygenation during coronavirus disease 2019 outbreak. Perfusion. 2020; 35:562–564 [DOI] [PubMed] [Google Scholar]
- 36.Supady A, Curtis JR, Abrams D, et al. ; Allocating scarce intensive care resources during the COVID-19 pandemic: practical challenges to theoretical frameworks. . Lancet Respir Med. 2021:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brodie D, Slutsky AS, Combes A. Extracorporeal life support for adults with respiratory failure and related indications: A review. JAMA. 2019; 322:557–568 [DOI] [PubMed] [Google Scholar]
- 38.Abrams D, Garan AR, Abdelbary A, et al. ; International ECMO Network (ECMONet) and The Extracorporeal Life Support Organization (ELSO). Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med. 2018; 44:717–729 [DOI] [PubMed] [Google Scholar]
- 39.Abrams D, Ferguson ND, Brochard L, et al. ECMO for ARDS: From salvage to standard of care? Lancet Respir Med. 2019; 7:108–110 [DOI] [PubMed] [Google Scholar]
- 40.Camporota L, Meadows C, Ledot S, et al. ; NHS England ECMO Service. Consensus on the referral and admission of patients with severe respiratory failure to the NHS ECMO service. Lancet Respir Med. 2021; 9:e16–e17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fan E, Beitler JR, Brochard L, et al. COVID-19-associated acute respiratory distress syndrome: Is a different approach to management warranted? Lancet Respir Med. 2020; 8:816–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Combes A, Hajage D, Capellier G, et al. ; EOLIA Trial Group, REVA, and ECMONet. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018; 378:1965–1975 [DOI] [PubMed] [Google Scholar]
- 43.MacLaren G, Combes A, Brodie D. Saying no until the moment is right: Initiating ECMO in the EOLIA era. Intensive Care Med. 2020; 46:1894–1896 [DOI] [PubMed] [Google Scholar]
- 44.Schmidt M, Bailey M, Sheldrake J, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med. 2014; 189:1374–1382 [DOI] [PubMed] [Google Scholar]
- 45.Jäckel M, Rilinger J, Lang CN, et al. Outcome of acute respiratory distress syndrome requiring extracorporeal membrane oxygenation in Covid-19 or influenza: A single-center registry study [published online ahead of print November 14, 2020]. Artif Organs. doi: 10.1111/aor.13865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mustafa AK, Alexander PJ, Joshi DJ, et al. Extracorporeal membrane oxygenation for patients with COVID-19 in severe respiratory failure. JAMA Surg. 2020; 155:990–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mustafa AK, Tatooles AJ. Reply to Letters to the Editor for “Extracorporeal membrane oxygenation for patients with Covid-19 in severe respiratory failure.” JAMA Surg. 2020E1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schmidt M, Burrell A, Roberts L, et al. Predicting survival after ECMO for refractory cardiogenic shock: The survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J. 2015; 36:2246–2256 [DOI] [PubMed] [Google Scholar]
- 49.Worku E, Gill D, Brodie D, Lorusso R, Combes A, Shekar K. Provision of ECPR during COVID-19: Evidence, equity, and ethical dilemmas. Crit Care. 2020; 24:462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Prekker ME, Brunsvold ME, Bohman JK, et al. Regional planning for extracorporeal membrane oxygenation allocation during coronavirus disease 2019. Chest. 2020; 158:603–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.White DB, Angus DC. A Proposed lottery system to allocate scarce COVID-19 medications: Promoting fairness and generating knowledge. JAMA. 2020; 324:329–330 [DOI] [PubMed] [Google Scholar]
- 52.Combes A, Schmidt M, Hodgson CL, et al. Extracorporeal life support for adults with acute respiratory distress syndrome. Intensive Care Med. 2020; 46:2464–2476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Combes A, Price S, Slutsky AS, Brodie D. Temporary circulatory support for cardiogenic shock. Lancet. 2020; 396:199–212 [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization. COVID-19 Technical Guidance Publications. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications. Accessed November 21, 2020
- 55.Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020; 46:854–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.National Institutes of Health. COVID-19 Treatment Guidelines. 2020. Available at: https://www.covid19treatmentguidelines.nih.gov/. Accessed December 24, 2020 [PubMed]
- 57.Abrams D, Schmidt M, Pham T, et al. Mechanical ventilation for acute respiratory distress syndrome during extracorporeal life support. Research and practice. Am J Respir Crit Care Med. 2020; 201:514–525 [DOI] [PubMed] [Google Scholar]
- 58.Rosano A, Martinelli E, Fusina F, et al. Early percutaneous tracheostomy in coronavirus disease 2019: Association with hospital mortality and factors associated with removal of tracheostomy tube at ICU discharge. A cohort study on 121 patients. Crit Care Med. 2021; 49:261–270 [DOI] [PubMed] [Google Scholar]
- 59.Krishnamoorthy S, Polanco A, Coleman N, et al. The safety and efficacy of tracheostomy in patients diagnosed with COVID-19: An analysis of 143 patients at a Major NYC Medical Center [published online ahead of print November 17, 2020]. Ann Surg. doi: 10.1097/SLA.0000000000004612 [DOI] [PubMed] [Google Scholar]
- 60.Long SM, Chern A, Feit NZ, et al. Percutaneous and open tracheostomy in patients with COVID-19: Comparison and outcomes of an institutional series in New York City. Ann Surg. 2021; 273:403–409 [DOI] [PubMed] [Google Scholar]
- 61.Garcia B, Cousin N, Bourel C, Jourdain M, Poissy J, Duburcq T; Lille Intensive Care COVID-19 group. Prone positioning under VV-ECMO in SARS-CoV-2-induced acute respiratory distress syndrome. Crit Care. 2020; 24:428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guervilly C, Prud’homme E, Pauly V, et al. Prone positioning and extracorporeal membrane oxygenation for severe acute respiratory distress syndrome: Time for a randomized trial? Intensive Care Med. 2019; 45:1040–1042 [DOI] [PubMed] [Google Scholar]
- 63.Giani M, Martucci G, Madotto F, et al. Prone positioning during venovenous extracorporeal membrane oxygenation in acute respiratory distress syndrome: A multicentre cohort study and propensity-matched analysis [published online ahead of print September 17, 2020]. Ann Am Thorac Soc doi: 10.1513/AnnalsATS.202006-625OC. [DOI] [PubMed] [Google Scholar]
- 64.Barnes GD, Burnett A, Allen A, et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: Interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020; 50:72–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yusuff H, Zochios V, Brodie D. Thrombosis and coagulopathy in COVID-19 patients requiring extracorporeal membrane oxygenation. ASAIO J. 2020; 66:844–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kowalewski M, Fina D, Słomka A, et al. COVID-19 and ECMO: The interplay between coagulation and inflammation-a narrative review. Crit Care. 2020; 24:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bemtgen X, Zotzmann V, Benk C, et al. Thrombotic circuit complications during venovenous extracorporeal membrane oxygenation in COVID-19. J Thromb Thrombolysis. 2021; 51:301–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guo Z, Sun L, Li B, et al. Anticoagulation management in severe coronavirus disease 2019 patients on extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2021; 35:389–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Masur J, Freeman CW, Mohan S. A double-edged sword: Neurologic complications and mortality in extracorporeal membrane oxygenation therapy for COVID-19–related severe acute respiratory distress syndrome at a tertiary care center. AJNR Am J Neuroradiol. 2020; 41:2009–2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Usman AA, Han J, Acker A, et al. A case series of devastating intracranial hemorrhage during venovenous extracorporeal membrane oxygenation for COVID-19. J Cardiothorac Vasc Anesth. 2020; 34:3006–3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zahid MJ, Baig A, Galvez-Jimenez N, Martinez N. Hemorrhagic stroke in setting of severe COVID-19 infection requiring extracorporeal membrane oxygenation (ECMO). J Stroke Cerebrovasc Dis. 2020; 29:105016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Heman-Ackah SM, Su YS, Spadola M, et al. Neurologically devastating intraparenchymal hemorrhage in COVID-19 patients on extracorporeal membrane oxygenation: A case series. Neurosurgery. 2020; 87:E147–E151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moores LK, Tritschler T, Brosnahan S, et al. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report. Chest. 2020; 158:1143–1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parzy G, Daviet F, Persico N, et al. Prevalence and risk factors for thrombotic complications following venovenous extracorporeal membrane oxygenation: A CT scan study. Crit Care Med. 2020; 48:192–199 [DOI] [PubMed] [Google Scholar]
- 75.Beyls C, Huette P, Abou-Arab O, Berna P, Mahjoub Y. Extracorporeal membrane oxygenation for COVID-19-associated severe acute respiratory distress syndrome and risk of thrombosis. Br J Anaesth. 2020; 125:e260–e262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leisman DE, Ronner L, Pinotti R, et al. Cytokine elevation in severe and critical COVID-19: A rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir Med. 2020; 8:1233–1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stockmann H, Keller T, Büttner S, et al. ; CytoResc Trial Investigators. CytoResc - “CytoSorb” rescue for critically ill patients undergoing the COVID-19 Cytokine Storm: A structured summary of a study protocol for a randomized controlled trial. Trials. 2020; 21:577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ramanathan K, Maclaren G, Combes A, Brodie D, Shekar K. Blood transfusion strategies and ECMO during the COVID-19 pandemic. Lancet. 2020; 8:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Borczuk AC, Salvatore SP, Seshan SV, et al. COVID-19 pulmonary pathology: A multi-institutional autopsy cohort from Italy and New York City. Mod Pathol. 2020; 33:2156–2168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Creel-Bulos C, Hockstein M, Amin N, Melhem S, Truong A, Sharifpour M. Acute cor pulmonale in critically ill patients with Covid-19. NEJM. 2020; 382:e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dres M, Burrel S, Boutolleau D, et al. SARS-CoV-2 does not spread through extracorporeal membrane oxygenation or dialysis membranes. Am J Respir Crit Care Med. 2020; 202:458–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Luyt CE, Sahnoun T, Gautier M, et al. Ventilator-associated pneumonia in patients with SARS-CoV-2-associated acute respiratory distress syndrome requiring ECMO: A retrospective cohort study. Ann Intensive Care. 2020; 10:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Buetti N, Ruckly S, De Montmollin E, et al. COVID-19 increased the risk of ICU-acquired bloodstream infections: A case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med. 2021; 47:180–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rouzé A, Martin-Loeches I, Povoa P, et al. ; coVAPid study Group. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: A European multicenter cohort study. Intensive Care Med. 2021; 47:188–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kreitmann L, Monard C, Dauwalder O, Simon M, Argaud L. Early bacterial co-infection in ARDS related to COVID-19. Intensive Care Med. 2020; 46:1787–1789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wells CL, Forrester J, Vogel J, Rector R, Tabatabai A, Herr D. Safety and feasibility of early physical therapy for patients on extracorporeal membrane oxygenator: University of Maryland Medical Center Experience. Crit Care Med. 2018; 46:53–59 [DOI] [PubMed] [Google Scholar]
- 87.Abrams D, Javidfar J, Farrand E, et al. Early mobilization of patients receiving extracorporeal membrane oxygenation: A retrospective cohort study. Crit Care. 2014; 18:R38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tipograf Y, Salna M, Minko E, et al. Outcomes of extracorporeal membrane oxygenation as a bridge to lung transplantation. Ann Thorac Surg. 2019; 107:1456–1463 [DOI] [PubMed] [Google Scholar]
- 89.Liew MF, Siow WT, Yau YW, See KC. Safe patient transport for COVID-19. Crit Care. 2020; 24:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dreier E, Malfertheiner MV, Dienemann T, et al. ECMO in COVID-19—prolonged therapy needed? A retrospective analysis of outcome and prognostic factors. Perfusion. 2021. doi: 10.1177/0267659121995997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lang C, Jaksch P, Hoda MA, et al. Lung transplantation for COVID-19-associated acute respiratory distress syndrome in a PCR-positive patient. Lancet Respir Med. 2020; 8:1057–1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cypel M, Keshavjee S. When to consider lung transplantation for COVID-19. Lancet Respir Med. 2020; 8:944–946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen JY, Qiao K, Liu F, et al. Lung transplantation as therapeutic option in acute respiratory distress syndrome for coronavirus disease 2019-related pulmonary fibrosis. Chin Med J (Engl). 2020; 133:1390–1396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Feldstein LR, Rose EB, Horwitz SM, et al. ; Overcoming COVID-19 Investigators; CDC COVID-19 Response Team. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020; 383:334–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shekerdemian LS, Mahmood NR, Wolfe KK, et al. ; International COVID-19 PICU Collaborative. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020; 174:868–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ahmed M, Advani S, Moreira A, et al. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020; 26:100527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Di Nardo M, Hoskote A, Thiruchelvam T, et al. Extracorporeal membrane oxygenation in children with coronavirus disease 2019: Preliminary report from the Collaborative European Chapter of the Extracorporeal Life Support Organization Prospective Survey. ASAIO J. 2021; 67:121–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schwartz SP, Walker TC, Kihlstrom M, et al. Extracorporeal membrane oxygenation for COVID-19-associated multisystem inflammatory syndrome in a 5-year-old [published online ahead of print December 29, 2020]. Am Surg doi: 10.1177/0003134820983198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yasuhara J, Watanabe K, Takagi H, Sumitomo N, Kuno T. COVID-19 and multisystem inflammatory syndrome in children: A systematic review and meta-analysis [published online ahead of print January 11, 2021]. Pediatr Pulmonol doi: 10.1002/ppul.25245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rimensberger PC, Kneyber MCJ, Deep A, et al. ; European Society of Pediatric and Neonatal Intensive Care (ESPNIC) Scientific Sections’ Collaborative Group. Caring for critically ill children with suspected or proven coronavirus disease 2019 infection: Recommendations by the Scientific Sections’ Collaborative of the European Society of Pediatric and Neonatal Intensive Care. Pediatr Crit Care Med. 2021; 22:56–67 [DOI] [PMC free article] [PubMed] [Google Scholar]


