Abstract
A third wave of COVID-19 occurred after Christmas 2020 in Madrid, one of the European pandemic epicenters. We noticed 6 major differential features to previous waves. First, household contacts were a large proportion of cases. Second, access to rapid antigen tests allowed prompt diagnosis and isolation. Third, clinically severe cases and mortality rates were lower. Fourth, the more transmissible B.1.1.7 strain was increasingly found. Fifth, vaccination benefits were seen in healthcare workers and nursing homes. Lastly, reinfections were more common. By Easter 2021, approximately 25% of the population in Madrid had been infected with SARS-CoV-2. Therefore, massive and accelerated vaccination campaigns are warranted to prevent new COVID-19 waves.
Keywords: Coronavirus, Transmission, Mortality, Reinfections, Antigen testing
Introduction
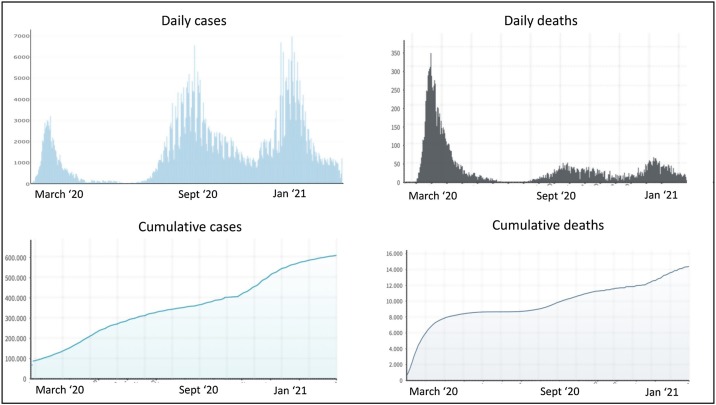
Madrid has been the epicenter of COVID-19 in Spain, primarily due to its high population density and mobility. The city has 3.3 million people, with 6.8 million across the metropolitan area. Up to March 15 2021, roughly 605 000 persons had been diagnosed with SARS-CoV-2 infection and 14 000 had died in the Madrid region (Ministerio de Sanidad, 2021, Instituto Nacional de Estadística, 2021). These figures refer to laboratory-confirmed cases, which underestimate the true number as testing access was limited during the earlier stages of the pandemic (Soriano and Barreiro, 2020).
Two major waves of COVID-19 had occurred in Madrid during 2020. The first, during the spring, peaked in March–April and the second in September–October. Their main features have already been described elsewhere (Soriano et al., 2021a, Pollán et al., 2020, Soriano et al., 2021b). Following holidays and family gatherings during Christmas, a third wave was noticed in January–February 2021. Herein, we report the major differential characteristics of this new surge.
Methods
A nationwide register of SARS-CoV-2 infections and deaths in Spain has existed since March 2020. The regional autonomous communities update the database on a daily basis (Ministerio de Sanidad, 2021, Instituto Nacional de Estadística, 2021). For this study, we analyzed the registers belonging to the Comunidad Autónoma de Madrid from March 1 to 15, 2021.
Results
The first confirmed cases of SARS-CoV-2 infection and deaths due to COVID-19 in Madrid were reported in March 2020. Figure 1 records the evolution of daily reported cases and deaths in Madrid due to SARS-CoV-2 infection since the beginning of the pandemic. The 3 major waves lasted for 1–2 months each. The first wave occurred during the spring of 2020, the second during the fall of 2020, and the third in January–February of 2021.
Figure 1.
SARS-CoV-2 infections and deaths reported in Madrid, Spain.
Discussion
After 2 waves of COVID-19 during the spring and fall of 2020, a third wave emerged in early 2021. This new COVID-19 surge had six major differential features. First, a larger proportion of cases were linked to household contacts, most likely owing to Christmas gatherings as a major trigger of this new wave (Thompson et al., 2021). Second, the widespread use of rapid antigen tests allowed prompt diagnosis and isolation of many positive individuals (Soriano et al., 2020). Third, the proportion of clinically severe cases and mortality rates were lower compared to prior COVID-19 waves. Fourth, the more transmissible virus strain B.1.1.7 was increasingly represented. Fifth, the impact of vaccination was recognized among certain groups, mostly healthcare workers and older people at nursing homes. Lastly, a growing proportion of cases were presumed to be reinfections in people that had already been positive for the virus, indicated by polymerase chain reaction testing and/or being seroreactive for antibodies.
The proportion of clinically severe cases of SARS-CoV-2 infection has declined since the first wave, most likely because diagnoses of asymptomatic or mildly symptomatic individuals have increased over time. In this regard, the widespread use of rapid tests in recent times has allowed more prompt isolation (Soriano et al., 2020) and better clinical monitoring and treatment of carriers (Griffin et al., 2021, Ngo et al., 2021). Indeed, almost all individuals with arterial oxygen saturation values <93% are now treated with corticosteroids. The proportion of hospitalizations and mortality rates in the latest wave have declined compared to the first wave, along with considerable increases in diagnostic capacity. As there are now many survivors following hospital discharge, an out clinic has been established to follow these patients periodically; those meeting the criteria for long-COVID have begun to be closely monitored.
The role of a smaller inoculum size as a cause of less severe clinical presentations and lower mortality rates during the third wave is an alternative explanation (Guallar et al., 2020). It indirectly reflects the benefits of universal social distancing, including wearing face masks, encouraging outdoor activities and restricting gatherings.
Since Christmas, a growing proportion of new SARS-CoV-2 infections in Madrid have been due to the B.1.1.7 strain; these now account for more than one-third of infections. A combination of mutations in the B.1.1.7 strain makes it especially contagious, whereas the B.1.351 variant can evade antibodies because of E484K (Soriano and Fernández-Montero, 2021). History tells us that viruses can evolve rapidly to evade barriers to transmission, especially when infections remain numerous. The more infections there are, the more chance mutations will occur, and those that best help the virus to survive will proliferate.
By Easter, approximately 25% of Madrid’s population had been infected with SARS-CoV-2. This infection rate is a slight increase on estimates for the first and second waves (15% and 20%, respectively) (Soriano et al., 2021a, Pollán et al., 2020, Soriano et al., 2021b). Since a large proportion of the population does not have immunity, massive and accelerated vaccination campaigns are warranted for preventing new COVID-19 waves.
By mid-March 2021, vaccines had been administered to approximately 850 000 people in Madrid. Almost all healthcare workers and most residents at nursing homes have been vaccinated. In order to maximize clinical protection, reduce transmission and minimize the risk for selection of vaccine-escape mutants, the COVID-19 vaccination campaign needs to be accelerated.
Author contributions
V.S. and P.B. designed the study. V.S., P.B., F.G.-G., O.C. and C.d.M. analyzed the data. V.S. wrote the first draft. All authors provided input to the final manuscript.
Ethical approval
The study was approved by the UNIR Ethics Committee (ref. 021/2020 and 022/2020).
Funding source
This work was funded in part by UNIR grants TRAPES and SEVERITYGEN, as well as EU projects EASI-Genomics and ‘Cure to Care’.
Conflicts of interest
All authors reported no conflicts of interest. All authors have submitted the ICMJE form for disclosure of potential conflicts of interest.
Acknowledgments
The authors thank the staff of the UNIR Medical Centre and of Consejería de Sanidad de Madrid for providing access to information recorded by the regional public health system.
References
- Griffin D., Brennan-Rieder D., Ngo B., Kory P., Confalonieri M., Shapiro L., et al. The importance of understanding the stages of COVID-19 in treatment and trials. AIDS Rev. 2021;(February) doi: 10.24875/AIDSRev.200001261. [DOI] [PubMed] [Google Scholar]
- Guallar M.P., Meiriño R., Donat-Vargas C., Corral O., Jouvé N., Soriano V. Inoculum at the time of SARS-CoV-2 exposure and risk of disease severity. Int J Infect Dis. 2020;97:290–292. doi: 10.1016/j.ijid.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Estadística. Available at: https://www.ine.es/covid/covid_inicio.htm. [Accessed 19 March 2021].
- Ministerio de Sanidad, Servicios Sociales e Igualdad. https://www.epdata.es/datos/evolucion-coronavirus-cada-comunidad/518/madrid/304. [Accessed 19 March 2021].
- Ngo B., Marik P., Kory P., Shapiro L., Thomadsen R., Iglesias J., et al. The time to offer treatments for COVID-19. Expert Opin Investig Drugs. 2021;(March) doi: 10.1080/13543784.2021.1901883. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollán M., Pérez-Gómez B., Pastor-Barriuso R., Oteo J., Hernán M.A., Pérez-Olmeda M., et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535–544. doi: 10.1016/S0140-6736(20)31483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., Barreiro P. Why such excess of mortality for COVID-19 in Spain? Ther Adv Infect Dis. 2020;7 doi: 10.1177/2049936120932755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., Sánchez-Santos M., Barreiro P. Rapid antigen testing and mask wearing while waiting for COVID-19 vaccines. AIDS Rev. 2020;22:168–172. doi: 10.24875/AIDSRev.M20000038. [DOI] [PubMed] [Google Scholar]
- Soriano V., Meiriño R., Corral O., Guallar M.P. Severe acute respiratory syndrome coronavirus 2 antibodies in adults in Madrid, Spain. Clin Infect Dis. 2021;72:1101–1102. doi: 10.1093/cid/ciaa769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., Ganado-Pinilla P., Sánchez-Santos M., Gómez-Gallego F., Barreiro P., de Mendoza C., et al. Main differences between the first and second waves of COVID-19 in Madrid, Spain. Int J Infect Dis. 2021;(March) doi: 10.1016/j.ijid.2021.02.115. S1201-9712(21)00201-0. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano V., Fernández-Montero J.V. New SARS-CoV-2 variants challenge vaccines protection. AIDS Rev. 2021;23:57–58. doi: 10.24875/AIDSRev.M21000040. [DOI] [PubMed] [Google Scholar]
- Thompson H., Mousa A., Dighe A., Fu H., Arnedo-Pena A., Barrett P., et al. SARS-CoV-2 setting-specific transmission rates: a systematic review and meta-analysis. Clin Infect Dis. 2021;(February) doi: 10.1093/cid/ciab100. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]