Abstract
Background
The US healthcare settings and staff have been stretched to capacity by the COVID-19 pandemic. While COVID-19 continues to threaten global healthcare delivery systems and populations, its impact on nursing has been profound.
Objectives
This study aimed to document nurses' immediate reactions, major stressors, effective measures to reduce stress, coping strategies, and motivators as they provided care during COVID-19.
Design
Mixed-methods, cross sectional design. Participants responded to objective and open-ended questions on the COVID-19 Nurses' Survey.
Participants
The survey, was sent to nurses employed in health care settings during the pandemic; 110 nurses participated.
Results
Immediate reactions of respondents were nervousness and call of duty; major stressors were uncertainty, inflicting the virus on family, lack of personal protective equipment (PPE), and protocol inconsistencies. Effective measures to reduce stress identified were financial incentives and mental health support. Most frequently used coping strategies were limiting televised news about the virus, talking with family and friends, and information, Motivators to participate in future care included having adequate PPE and sense of duty. Bivariate analysis of outcomes by age group, education, work setting, and marital status was performed. Nurse respondents with higher advanced degrees had significantly less fear than those with BSN-only degrees (p < .05).Of respondents who were married/living with a partner, 85.9% listing “uncertainty about when the pandemic will be under control” as a major stressor (p < .05), while 62.8% of those who were single/divorced/widowed (p = .015) did so. Further, 75% of respondents working in critical care listed “mental health services” as important (p = .054). Four major qualitative themes emerged: What is going on here?; How much worse can this get?; What do I do now?; What motivates me to do future work?
Conclusion
The study found nurses were motivated by ethical duty to care for patients with COVID-19 despite risk to self and family, leaving nurses vulnerable to moral distress and burnout. This research articulates the need for psychological support, self- care initiatives, adequate protection, information, and process improvements in the healthcare systems to reduce the risk of moral distress, injury and burnout among nurses.
Keywords: Nursing, COVID-19, Coronavirus, Pandemic, Moral distress, Fear, Stress, Duty
What is already known about the topic
-
•
Research to date has identified fear of contracting and spreading the coronavirus.
-
•
Lack of preparedness by the healthcare system with policies, processes, and supplies required to address the needs of both patients and frontline nurses during the COVID-19 pandemic were also reported.
What this paper adds
-
•
A mixed-methods approach converges findings from quantitative and qualitative data, a noted gap in currently published COVID research studies.
-
•
Data provide demographic factors and respondents' initial reactions, coping factors to relieve stress, and motivators to continue working with patients during a pandemic.
-
•
Survey tool was adapted from nursing research during the SARS 2003 epidemic in Taiwan and 2012, MERS epidemic in Saudi Arabia, adding a global perspective.
-
•
Demographic characteristics may help nursing administrators identify nurses who may need more support and to serve as advocates to protect the physical and mental well-being of nurses.
-
•
The study highlights the need for nursing educators to better prepare nurses in disaster management, including self-care.
1. Introduction
COVID-19 cases were reported first in Wuhan, Hubei province in China, in December 2019, and the first U.S. case was identified in the state of Washington on January 30, 2020 (World Health Organization [WHO], 2021c). U.S. healthcare providers were demonstrably unprepared and overwhelmed by the increase in patients presenting with infections. By the time this viral infection was identified as having wide-ranging community spread in the U.S., it was apparent that administrators in hospitals and community health systems faced a major public health crisis. Patient care protocols for testing and control of viral spread and reports of its severity changed frequently. Emergency departments and acute and critical care units filled to capacity. Nurses and other healthcare providers were left vulnerable due to shortages of information, personal protective equipment (PPE), ventilators, and other patient care resources.
Frontline nurses faced innumerable challenges, including intense fear of viral transmission to self and others while attending to managing critically ill patients with insufficient amounts and types of PPE. Nurses distanced themselves from friends, family, and colleagues to avoid spreading the virus, and often feared returning home after shifts. At work, nurses often served in family-surrogate roles, as patients were suffering, even dying, isolated from loved ones. This experience left frontline nurses vulnerable to ongoing moral distress due to the ethical considerations in caring for patients and themselves during this unprecedented time.
Scholarly literature detailing the experiences of nurses during the COVID-19 pandemic is rapidly expanding (Digby, Winton-Brown, Finlayson, Dobson, & Bucknall, 2020; Dimino, Horan, & Stephenson, 2020; Lingis, 2020; Sun et al., 2020). Although SARS (WHO, 2021a) and MERS (WHO, 2021b) had epidemic and not pandemic viral spreads, they presented many similarities noted in research surrounding nursing and COVID-19.
In a retrospective study of Taiwanese health care workers who cared for patients during the 2003 SARS epidemic, psychiatric and emergency care providers initially interviewed 26 female nurses who were assigned to a “SARS Team” to care for patients with what was then an unknown virus (Lee et al., 2005). Using narrative analyses, they developed the SARS-Team Questionnaire English Version to survey respondents' initial reactions, stressors, coping strategies, and motivations to care. Also included was a series of open-ended questions. This study reinforced the importance of providing mental health services to prevent secondary traumatization (p. 358) and timely updates to frontline nurses regarding policy and procedural changes. With Dr. S. Lee's permission, researchers modified the SARS-Team Questionnaire English Version with some modifications of terminology for use with U. S. nurses.
Khalid, Khalid, Qabajah, Barnard, and Qushmaq (2016) adapted the SARS-Team questionnaire used by Lee et al. (2005), based on content review by 10 representative staff members, to interview healthcare providers in Saudi Arabia who served during the 2015 MERS viral outbreak in Jeddah, Saudi Arabia. The “MERS CoV Staff Questionnaire,” included the five (5) sections studied by Lee et al. (2005): (a) staff emotions during the outbreak; (b) associated stressors; (c) factors that could have helped reduce stress; (d) coping strategies used, and (e) motivators to work in future outbreaks. The authors reported that personal safety, access to information and equipment, positive attitudes among co-workers, recognition for service, and monetary rewards were of value should future crises arise. (Khalid et al., 2016, p. 13).
In 2015, the Saudi health care system in Riyadh was further impacted by MERS outbreaks. Researchers in Riyadh conducted what was believed to be the first qualitative study of the experiences of health care providers affected by MERS (Almutairi, Adlan, Balkhy, Abbas, & Clark, 2018). Using inductive analyses from interviews with 4 nurse and 3 physician participants, they identified the following themes: “caring for others in the defining moments,” “prejudice and stigma,” “moments of traumatic fear and despair,” and “denial and underestimation of the seriousness of the disease” (pp. 188–190). The authors suggested these findings could help organizational leaders support and prepare employees for the immediate and long-term human impacts of public health crises.
In a qualitative study, Lee, Hong, and Park (2020) interviewed 17 nurses who worked with patients during Korea's 2015 MERS epidemic. Analysis yielded seven theme clusters: “Fear of Uncertainty,” “Beyond Hesitation,” “A Scene Like a Battlefield,” “Chaotic Nursing Identity,” “Buttresses for Sustainability,” “Lingering Trauma,” and “Expanded Horizon of Nursing.” Their overall thematic construct as Beyond the Fear of Uncertainty. As with the SARS epidemic, researchers found nurses' fear of contracting the disease often conflicted with their ethics of caring for others as the MERS epidemic unfolded. (Lee et al., 2020, p. 3349).
To date, one year after COVID-19 cases were first reported, the U.S. is experiencing a second wave of COVID-19 infections. Health care settings and staff are again stretched to capacity. The virus continues to pose a global threat to health care delivery systems, nurses, and populations in almost every country, with only a few not reporting epidemiologic statistics. In mid- January approximately 94 million cases of COVID-19 have been confirmed worldwide, with approximately 2 million associated deaths; in the U.S., there were 22,102,069 confirmed cases and 371,084 deaths at that time (World Health Organization, 2021a, World Health Organization, 2021b, World Health Organization, 2021c). The U.S reported 23 million cumulative confirmed cases and 390,809 deaths at that same time. Recent data from the Johns Hopkins Coronavirus Resource Center identifies that the mortality rate in the U. S. has, however, decreased from nearly 4.3% in June 2020 to 1.7% as of January 10th (University of Oxford, 2021).
According to the International Council of Nurses' statistics for October 2020, the number of nurses who have died after contracting the coronavirus is 1500. This figure represents the lost lives of nurses from only 44 of the world's 195 countries and is an underestimation of the total number of deaths of nurses worldwide. Deaths have been attributed to the lack of knowledge about the virus and lack of personal protective equipment (PPE) available as the virus appeared and with its subsequent declaration as pandemic. Despite the decreasing death rates, nurses and their families remain at a higher risk of viral exposure and subsequent disease than the general public and continue to serve (Karlsson & Fraenkel, 2020).
Nurses often report their ethical obligation to provide clinical leadership and direct patient care yet also struggle with self-health concerns and worry about transmitting the virus to family and others (McConnell, 2020). Fear is a frequent phenomenon identified in multiple studies including this research (Akgün, Shamas, Feder, & Schulman-Green, 2020; Hu et al., 2020; Jennings & Yeager, 2020) Nurses reported choosing alternative housing options for fear of bringing the virus home. Jennings and Yeager (2020) noted an association between fear, collaboration, and communication. According to their research, communication between nursing and other members of the healthcare team is essential to achieving the best outcomes for nurses and patients. Collaboration and flexibility when implementing process improvement changes were identified as effective methods to cope with fear and develop strength and resilience. Akgün et al. (2020) noted communication and sharing changes in standards as a key strategy to decrease fear in patients and their families when faced with isolation in the intensive care unit (ICU).
In a descriptive cross-sectional study involving 261 frontline nurses in the Philippines in 2020, Labrague and de Los Santos (2020) demonstrated an inverse relationship between fear and job satisfaction, job turnover, and psychological stress. The study concluded the need for hospital administrators to develop clear guidelines, training, and mental health support in order to keep nurses on the frontlines and to prevent burnout. Yet the impact of COVID-19 on nurses has not been elucidated both qualitatively and quantitatively.
The aim of this study was to document vivid descriptions of nurses' immediate reactions, major stressors, and their measures to manage stress during the first months of the COVID-19 pandemic. In addition, the study sought to identify how frequently nurses used coping strategies and their motivations to care for patients in the future. Understanding nurses' reactions and stressors experienced during COVID-19 is necessary to inform administrators, educators, and point of care providers as they develop strategies and structures that support physical, mental, and emotional health and healing.
2. Methods
2.1. Design
This study is a mixed-methods cross sectional design using an online survey that yielded quantitative data and narrative descriptive data from open-ended questions.
2.2. Participants
Participants were recruited from registered nursing alumni and current MSN students from a college in Pennsylvania, U. S. A total of 119 nurse participants consented; 110 of them responded to questions. Participants were employed during COVID-19; were prepared at either the bachelor or masters level; and worked in various healthcare environments.
2.3. Data collection
The online survey was adapted from the SARS Team Questionnaire, English Version with permission obtained from Dr. S. H. Lee. The COVID-19 Nursing Questionnaire was distributed electronically via QualtricsR survey software in August 2020, five months after the World Health Assembly's declaration of the COVID-19 pandemic in March.
Participants were asked to provide demographic information and respond to objective items in five categories: immediate reactions (18 items), major stressors (23 items), effective measures to reduce stress (16 items), use frequency of coping strategies (12 items), and motivators to participate in the care of patients during future pandemics (5 items). Participants were also asked 6 open-ended questions about what they faced during the pandemic:
Q1. How would you describe your initial reaction to caring for patients with COVID-19?
Q2. Describe major stressors you encountered.
Q3. Describe effective measures you used or could have used to reduce stress.
Q4. How frequently were the listed coping strategies used?
Q5. What would motivate you to participate in healthcare delivery in a repeated pandemic or epidemic?
Q6. Is there anything you have not yet described related to this experience but would like to address?
2.4. Validity, reliability, and rigor
The survey tool was assessed for content validity. It had been used previously in two research studies that examined health care workers, and nurses caring for patients during SARS and MERS respectively (Khalid et al., 2016; Lee et al., 2005). An experienced statistician analyzed and interpreted quantitative data. Trustworthiness in the analysis for qualitative data was established as three nurse researchers explored narratives independently and consensually validated the themes and sub themes. To enhance credibility of findings, researchers converged qualitative equivalent data with the quantitative counterparts. (Creswell & Poth, 2018).
2.5. Ethical considerations
Approval to conduct the research was granted by the Institutional Review Board at Moravian College. Informed consent was explained on page one of the survey and implied as respondents chose to begin answering questions. Mental health resources for mental health services were provided to the study participants, and a private email account was available for study participants to contact researchers should additional support be sought during or after taking the survey.
3. Results
3.1. Quantitative analyses
Quantitative data management tasks and analyses were performed using SAS Release 9.4 statistical software (The SAS Institute, 2019, Cary, NC). Frequency distributions with percentages were generated for independent and dependent variables.
3.2. Demographic characteristics
Independent variables are respondent's age group, professional education, work setting, and marital status. Participant characteristic may be found in Table 1 .
Table 1.
Participant characteristics (N = 110).
| Item | Frequency | Percentage (%) |
|---|---|---|
| Age group (years) | ||
| 18–25 | 22 | 20.0 |
| 26–34 | 44 | 40.0 |
| 35–44 | 26 | 23.6 |
| 45+ | 18 | 15.4 |
| Education level | ||
| BSN | 88 | 80.0 |
| MSN | 22 | 20.0 |
| Work settings | ||
| Acute/medical | ||
| Surgical | 36 | 25.0 |
| Critical care | 26 | 18.1 |
| Other | 82 | 56.9 |
| Marital status | ||
| Married/partner | 64 | 58.2 |
| Single/divorced/ | ||
| Widowed | 46 | 41.8 |
3.3. Dependent variables
Five sets of dependent variables were measured: immediate reactions, major stressors, effective measures to relieve stress, usage frequency of coping strategies, and motivators to provide care in the future. For each of these dimensions, researchers identified the most salient responses, i.e., with the highest frequencies of affirmative responses or the highest means where there were multiple response levels. After reviewing all five dimensions, bivariate analyses were completed for all five dimensions by the demographic independent variables, age group, professional education, work site, and marital status.
3.4. Descriptive statistics
Table 2 is a list of the top 5 responses to each of the survey questions.
Table 2.
The top 5 responses.
| Immediate reactions to Covid-19 | ||||
|---|---|---|---|---|
| Item | Total (n) | Moderate (n) | Severe (n) | Moderate/severe % |
| I felt nervous and worried | 92 | 46 | 25 | 77.2 |
| I took it as a call of duty | 84 | 28 | 34 | 73.8 |
| I felt I had no choice | 78 | 26 | 21 | 73.1 |
| I took it as a challenge(n = 95) | 73 | 29 | 20 | 67.1 |
| I felt hatred | 17 | 7 | 4 | 64.7 |
| Major stressors | |||
|---|---|---|---|
| Item | Yes (n) | Moderate/severe (n) | Moderate/severe |
| Uncertainty about when the epidemic will be under control | 90 | 78 | 86.7 |
| Worry about inflicting coronavirus on family members | 83 | 70 | 84.3 |
| Worry about lack of staffing | 75 | 62 | 82.7 |
| Patients' families' emotional reactions | 73 | 60 | 82.2 |
| Conflict between duty and safety | 72 | 57 | 79.2 |
| Effective measures to reduce stress | |||
|---|---|---|---|
| Item | Total (n) | Moderately |
(%) Moderately |
| Very effective(n) | Very effective | ||
| Sharing jokes and humor with co-workers | 74 | 58 | 78.4 |
| Encouragement among co-workers | 71 | 53 | 74.6 |
| Sufficient rest or time off | 64 | 37 | 60.7 |
| Community recognition and support | 66 | 39 | 59.1 |
| Improvements in patient's | 67 | 39 | 58.2 |
| Most frequently used coping strategies | |||
|---|---|---|---|
| Item | Responses (n) | Mean | SD |
| Taking proactive measures (washing hands, Wearing masks, temperature taking) | 87 | 3.89 | 0.32 |
| Limiting oneself from watching too much news about COVID-19 | 85 | 3.22 | 0.85 |
| Actively acquiring knowledge about Covid-19 | 87 | 3.21 | 0.71 |
| Chatting with family and friends by phone or video to share concerns and support | 85 | 3.14 | 0.80 |
| Engaging in recreational activities (shopping, streaming movies, outdoor exercises, internet surfing, social media) | 85 | 3.04 | 0.89 |
| Motivators to care in future epidemics or pandemics | |||
|---|---|---|---|
| Item | Total (n) | Mean | SD |
| Adequate and sufficient protective equipment | 84 | 1.95 | 0.90 |
| Clear information about the disease | 84 | 2.63 | 1.40 |
| Family support | 84 | 3.20 | 1.58 |
| Reasonable staffing/shift | 84 | 3.20 | 0.99 |
| Bonus pay for dangerous work | 84 | 3.98 | 1.21 |
Supplements A through E are complete lists of the responses to each of the survey questions.
3.4.1. Immediate reactions
The percentage of those with moderate and severe reactions were calculated for those who responded “yes” that they had reactions that were, “mild”, “moderate”, or “severe.” Accordingly, the stressors showing the highest levels of severity of those with any reaction were:
-
•
I felt nervous and worried
-
•
I took it as a call of duty
-
•
I felt I had no choice
-
•
I took it as a challenge
-
•
I felt hatred
3.4.2. Major stressors
Participants were asked to identify major stressors they experienced. Respondents were most likely to list the following as stressors.
-
•
Uncertainty about when the epidemic will be under control
-
•
Worry about inflicting the coronavirus on family
-
•
Worry about lack of staffing
-
•
Worry about families' emotional reactions
-
•
Conflict between duty and safety
3.4.3. Effective measures to reduce stress
Participants were asked about measures that were effective in reducing stress, and to what extent they were effective. These five measures were identified most often as “moderately” or “very much effective” in reducing stress:
-
•
Sharing jokes and humor with co-workers
-
•
Encouragement among co-workers
-
•
Sufficient rest or time off
-
•
Community recognition and support
-
•
Improvement in patient's condition
3.4.4. Most frequently used coping strategies
Nurse participants were asked how frequently coping strategies were used according to the following Likert scoring: 1 = almost never; 2 = sometimes; 3 = often; 4: almost always. Those measures used with the highest mean scores are:
-
•
Taking protective measures (washing hands, wearing mask, taking own temperature)
-
•
Limiting oneself from watching too much news about COVID-19
-
•
Actively acquiring more knowledge about COVID-19 (symptoms, transmission pathway)
-
•
Chatting with family and friends by phone or video chat to share concerns and support
-
•
Engaging in recreational activity (shopping, streaming movies, outdoor exercises, internet surfing, social media)
3.4.5. Motivators to care in future
Respondents were asked to rank, by importance, five potential motivators to care for patients if another epidemic or pandemic occurs. Mean scores and standard deviations from those who reported how important a motivator is are shown below. Responses were scored in rank order with “1” being of most importance “5” being least important. Respondents were most motivated by adequate and sufficient protective equipment (Mean = 1.95) and least motivated by bonus pay for dangerous work (Mean = 3.98). Rank ordering of motivators is noted.
-
•
Adequate and sufficient protective equipment
-
•
Clear information about the disease
-
•
Family support
-
•
Reasonable staffing/shift
-
•
Bonus pay for dangerous work
3.5. Bivariate analyses of outcomes by demographic variables
3.5.1. Immediate reactions by demographic factors
Researchers ran ANOVAs or t-tests of four of the immediate reactions. Two statistically significant associations were observed. First, respondents with professional education level with MSN degrees had lower mean values (Mean = 1.95) for the item “I felt frightened” than those with a BSN degree (mean = 2.63; t = 2.86, df = 98, p < .005). Similarly, respondents with a MSN degree had lower mean values (mean = 2.62) for the item “I felt nervous and worried” than those with BSN degrees (Mean = 3.01; t = 1.98, df = 98, p = .05). Turning to marital status, while none of the four possible associations examined was statistically significant, marital status approached significance.. Nurse respondents with a spouse or partner living with them had higher mean scores on “Feeling nervous and worried” (mean = 3.03), than those who were single, divorced, or widowed respondents, 2.73 (t = 1.80, df = 99, p = .075).
3.5.2. Major stressors by demographic factors
Crosstabulations, with Chi-square statistics were run for four major stressors (“Uncertainty about when the epidemic will be under control,” “I worry about inflicting coronavirus on family,” “Worry about lack of proper knowledge and equipment,” and Worry about getting infected”) by age group, professional education, work setting, and marital status. None of the associations was found to be statistically significant at p < .05. However, one association was suggestive, that of “Worry about lack of proper knowledge and equipment (e.g., PPE)” by work setting. While 68.1% of respondents who worked in neither acute care nor critical care listed this as most important, 70.4% of those working in acute medical-surgical care listed it as most important and 91.7% of those working in critical care listed it as most important (Chi-square = 4.98, df = 2, p = .083).
Three of the major stressor variables were statistically significantly associated with respondents' marital status, and the fourth was close to significance. First, 85.9% of respondents who were married or living with a partner listed “Uncertainty about when the epidemic will be under control” as a major stressor, while 68.6% of those who were single, divorced, or widowed did so (Chi-square = 4.24, df = 1, p = .040). Also, 84.4% of respondents who were married or living with a partner listed “Yourself displaying coronavirus like symptoms” as a major stressor, while 62.9% did so among those who were single, divorced, or widowed (Chi-square = 5.87, df = 1, p = .015). Whereas 82.8% of those married or living with a partner listed “Worry about inflicting coronavirus on family” as a major stressor, while 57.1% did so among those single, divorced, or widowed (Chi-square = 7.70, df = 1, p = .006). The one result which only approached significance was that 79.7% of those married or living with a partner listed “Worry about lack of staffing” as a major stressor while 64.7% of those single, divorced, or widowed did so (Chi-square = 2.62, df = 1, p = .105).
3.5.3. Effective measures to relieve stress by demographic factors
Cross tabulations were run with Chi-square statistics on effective measures to relieve stress (“Hospital granted additional financial incentives (e.g., bonus pay)” and “Mental health services”) by age group, professional education, work setting, and marital status. Mental health services by work site approached statistical significance with 40.0% of respondents who work in acute care medical-surgical sites listing mental health services as effective measures, 48.9% of those who work in neither acute care nor critical care and 75.0% of respondents who work in critical care listed (Chi-square = 5.86, df = 2, p = .054). Neither of the top two effective measures to relieve stress was significantly associated with marital status: “Hospital granted additional financial incentives (e.g., bonus pay)” nor “Mental health services.”
3.5.4. Coping strategies by demographic factors
Researchers ran ANOVAs and t-tests (as appropriate) of three coping strategies- “Taking protective measures (washing hands, wearing mask, taking own temperature)”, Limiting oneself from watching too much news about COVID-19,” and “Actively acquiring more knowledge about COVID-19 (symptoms, transmission pathway)” – by age group, professional education, work setting, and marital Status.
The strategy of “Limiting oneself from watching too much news about COVID-19” significantly decreased as respondents' age group increased (F = 2.80, p = .045). Respondents' age group of 18–25 had the highest mean score, 3.62; 26–34 had a mean of 3.19; and 35–44 had a similar mean, 3.20. Those 45 and over had the lowest mean, 2.72. Similarly, the strategy of “Actively acquiring more knowledge about COVID-19 (symptoms, transmission pathway)” significantly increased with age (F (3,84) =3.45, p = .020): those 18–25 had the lowest mean, 2.88; 26–34 had a mean of 3.08; 35–44 had the highest mean, 3.60, and 45 and over had a mean of 3.20. None of the top three coping strategies was significantly associated with marital status.
3.5.5. Frequency using motivators by demographic factors
Researchers ran ANOVAs and t-tests (as appropriate) of the most salient motivators to care in a future pandemic by age group, professional education, work setting, and marital status. None of the possible associations were statistically significant.
3.6. Qualitative analysis
Qualitative data were analyzed by the researchers, three doctorally-prepared nurse educators, who reviewed and coded the narrative responses and grouped this data into shared concepts to determine emerging themes and subthemes. Researchers performed this analysis independently, compared and contrasted findings, and achieved consensus. A code book documented major themes, and sub themes identified for each of the open-ended questions in confirming the trustworthiness of data.
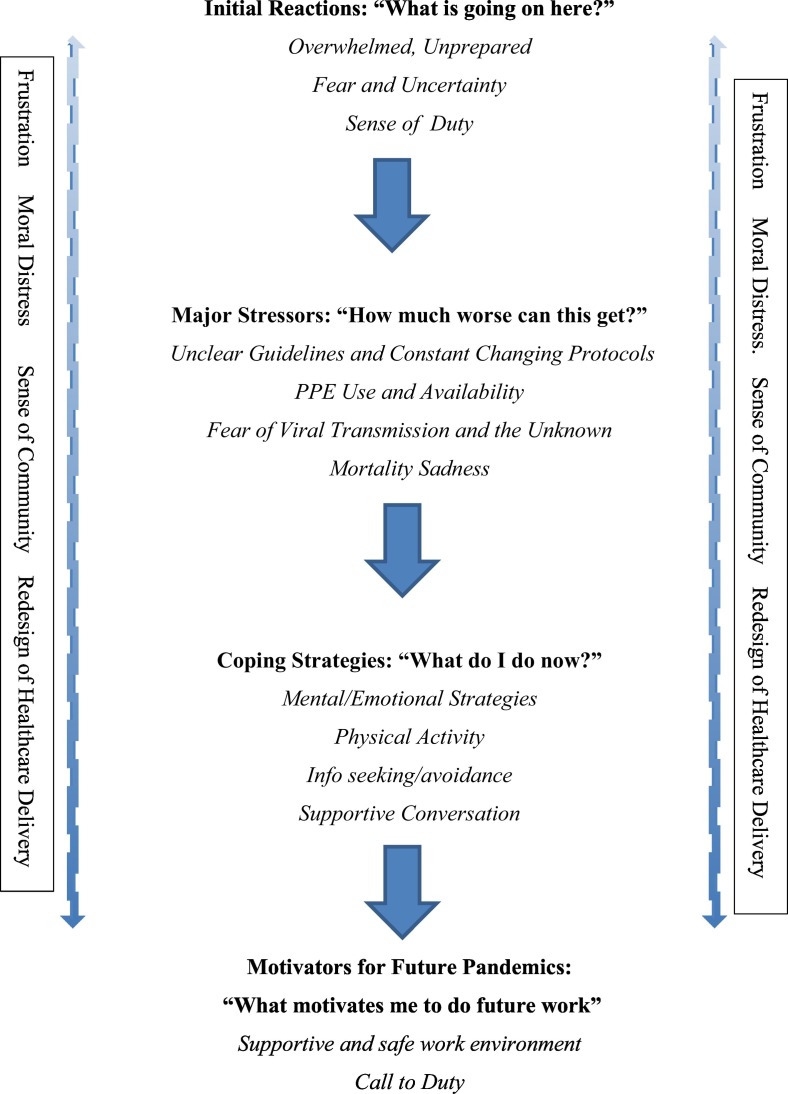
Significant statements were extracted to best represent the themes and subthemes. For each question, researchers determined four emerging themes as: (1) “What is going on here?” (2) “How much worse can this get?” (3) “What do I do now?” and (4) “What motivates me to do future work?” Three additional themes emerged including (5) Lingering frustration, (6) Moral distress, and (7) Sense of community. A diagram of the thematic analysis of nurses' pandemic Lives is depicted in Fig. 1 .
Fig. 1.
Thematic analysis of nurses' pandemic lives.
Table 3 identifies participant's quotations representative of each theme and subthemes.
Table 3.
Nurses' pandemic lives: themes and subthemes.
| Theme | Subthemes | Quotations |
|---|---|---|
| 1. What is going on here? | i. Overwhelmed and Unprepared | “My initial reaction was overwhelming. I was worried more about my family than myself.” “As someone who works in the ER, I knew I would be facing the pandemic head on. It was unsettling at times, but most stress was due to lack of good information…” “My initial reaction to caring for patients was overwhelming. I have never seen such sick patients in most vulnerable and alone state.” |
| ii. Fear, Worry, and Uncertainty | “I was fearful that I would give the infection to family members or other members of the community” “The fear of protecting family members and protecting ourselves and the staff around us made us almost hide from our patients.” “Scared of the unknown and ever-changing information” “I was absolutely terrified” “Constant worry of infecting family members, being forced to isolate from family and being treated like a leper” |
|
| iii. Sense of Duty | “I felt it my duty to help take care of patients with COVID-19 and in a way, it felt empowering to be on the frontline so that I could do something to aid the crisis.” “I felt apprehensive but also knew it was my duty to take care of the patients no matter their diagnosis.” “Stressed but ready to take action as a nurse” |
|
| 2. How much worse can this get? | i. Unclear Guidelines and Constant Changing Protocols | “For weeks on a daily basis our beginning shift huddles consisted of forget what we said yesterday about xxxx, today we are doing xxxx. We were constantly changing protocols which made it difficult to function at work on a daily basis, it was stressful because it was impossible to keep up with the ever-changing protocols in our department.” |
| ii. Personal Protective Equipment (PPE) Use and Availability | “Uncertainty about PPE availability, treatment procedure” “The anxiety in the air was palpable, even though everyone was trying their best, overall, the biggest stressor was what was expected of us – to provide good and safe patient care while the resources were limited.” |
|
| iii. Fear of Viral Transmission and the Unknown | “The unknown: the constant floating to COVID units and constantly changing PPE guidelines. Also not being told about exposures and being told you weren't considered an exposure if you had a surgical mask on.” “Not knowing enough about the disease progression or how the virus works” “Wearing an N95 mask all the time and the unknown of what was truly happening.” |
|
| iv. Mortality Sadness | “Witnessing people's condition deteriorate very quickly and watching them struggle and pass away with no family present.” “…stressors from families calling and holding the iPad so families could video chat and see their dying loved one…” “Major stressor was watching patients die alone with no human touch” |
|
| 3. What do I do now? | i. Mental/Emotional Strategies/ Physical Activities | “Humor and accepting the situation and I made sure to get at least 30 min of exercise outdoor if the weather permitted.” “Coming home to having alone time. Taking a hot shower. Sitting with my family.” “Recognize self-physical and mental health is important and reducing hours worked” |
| ii. Information Seeking or Avoidance (COVID) | “Tried to find as much research and information as I could to ease my anxiety about taking care of these sick patients.” “…trying to avoid constantly watching the news or talking about it.” “Thinking about COVID like the flu. Not thinking about COVID at all.” “I took the opposite approach of many people and I watched updates about the pandemic daily.” |
|
| iii. Supportive Conversation | “Talking with friends and family and venting with coworkers and manager.” “Venting to family, playing and cherishing kids, hugs from my husband, joking with people at work.” “…relationships with my coworkers (worked with the same ‘team’ every shift for 2 months) kept me sane.” |
|
| 4. What motivates me to do future work? | i. Supportive and Safe Work Environment | “More appreciation from the healthcare institution worked. We did not receive bonus pay. Any meals or donations were from the community and not the hospital. Also, adequate information about exposure.” “Increased support from employer by providing clear guidelines, appropriate PPE, enough PPE, hazard pay.” “Having appropriate PPE and staffing. Feeling and appreciated for working through tough times. Not feeling like another number coming into work.” |
| ii. Call to Duty | “The calling and the opportunity to be of service to my community. That's what drew me to nursing initially, and what keeps me in the field.” “I'm a nurse. It's my duty to care for the sick.” “It's my job to care for people. Not a question of motivation.” |
|
| 5. Lingering frustration | i. Lack of PPE ii. Public Restrictions iii. Hospital Environment iv. Sacrifices v. Burnt out vi. Changing policies |
“I had no choice, and I was sick of hearing that I signed up for this. It made me question my career choice because of the amount of weight on nurses with such a lack of support.” “The emotional stressors are far more exhausting than any physical ones. It is important to keep your mental health in check “I do not believe that hospitals are designed well enough to handle pandemics.” “It would seem that if the goal is to reduce transmission, the hospital should have facilities such as showers, laundry, hygiene stations as they do in operating room areas that would help to reduce the number of nurses and healthcare staff tracking possible contaminants home.” |
| 6.Moral distress | i. Tired/Fatigued ii. Patient Death iii. Emotionally iv. Fragile Mental Health Concern v. Moral Anguish |
“My mental health and the mental health of all my co-workers were placed in jeopardy and we need to protect each other from this moral distress if this happens again.” “I still feel emotionally fragile. I question my own emotional strength to continue bedside nursing.” “Watching people die from this virus alone with no family except maybe through FaceTime is not something you forget easily. |
| 7. Sense of community | i. Unity Among Colleagues and Peers ii. Sense of Belonging |
“…It took a whole pandemic for people to truly appreciate nurses.” “My fellow teammates at my workplace were what got me through COVID. Yes it was scary at certain times with the staffing ratios, but we pulled through as a team.” “…We bonded over the issues at work. We became better friends outside of work which only made working together better.” “The whole experience has been enlightening and my team was amazing. Knowing how strong we are when we work together is truly motivating that we can conquer anything thrown at us.’ |
Using a convergence model, quantitative and qualitative data were collected concurrently and analyzed independently for each of the domains. The parallel databases variant was used where the results of the two separate analyses were compared and contrasted, leading to an overall interpretation of results (Creswell & Poth, 2018). See Table 4 : Visual Display of Quantitative and Qualitative Findings.
Table 4.
Visual display of the quantitative and qualitative findings.
| Convergent parallel results | Quantitative Findings | Qualitative Findings | Summary |
|---|---|---|---|
| 1. Immediate reactions | Nervous and worried Call of duty No choice A challenge |
Overwhelmed, unprepared Fear, and uncertainty Sense of duty |
Quantitative and qualitative findings are consistent with regard to worry and call to duty. Additional salient remarks as “no choice” and “a challenge”: were not identified in qualitative analysis. |
| 2. Major stressors | Uncertainty about when the epidemic will be under control Worry about inflicting coronavirus on family, lack of staffing, families' emotional responses. |
Unclear guidelines/ Constant changing protocols PPE use /availability Fear of viral transmission Mortality sadness |
Quantitative findings indicated worry and uncertainty. Qualitative findings reflected additional meaningful statements about mortality sadness |
| 3. Effective Measures to relieve stress | Sharing jokes and humor with co-workers Encouragement among co-workers Sufficient rest or time off Community recognition and support |
Mental/emotional strategies physical activity Information seeking/avoidance Supportive conversation |
Quantitative and qualitative findings are consistent. Mental and emotional strategies encompass quantitative findings such as rest, time off, and humor. |
| 4. Use Frequency of coping strategies | Taking protective measures Limiting oneself from watching too much news about COVID-19 Actively acquiring more knowledge about COVID-19 |
Findings were consistent with effective measures to relieve stress either currently or in the future | Quantitative and qualitative findings are comparable. |
| 5. Motivators | Respondents were most motivated by “Adequate and sufficient protective equipment” | Supportive and safe work environment Call to Duty |
Quantitative and qualitative findings are consistent with a further qualitative emphasis on “call to duty.” |
4. Discussion
To our knowledge, this is the first mixed-methods study to explore the impact of COVID-19 on the lives of nurses during the pandemic.
Nurses are faced with the complexities of caring for patients in an overwhelming and unsafe environment. When COVID-19 first appeared in the U.S. healthcare systems were ill-prepared for an emergent pandemic and insufficiently equipped with the infection control measures, protocol, and practices to protect and inform nurses and other healthcare workers.
Frontline nurses can either burn-out or be empowered to cope with the profound stressors posed by the COVID-19 pandemic, and the inevitability of future assaults on public health. Our study found initial reactions were fear, nervousness and worry, a call of duty, and a challenge. Notwithstanding, nurses rose to the challenge, using their education and training to battle the pandemic.
Initial major stressors related to lack of knowledge, frequent policy and procedural changes, lack of PPE and other supplies required to protect nurses and patients from contracting the virus were not unfounded since nurses did get the virus and, in some cases, died, as noted by the ICN (2020) statistics. Nursing administrators have an ethical obligation to protect nurses during crises situations as noted by Hofmeyer & Taylor, 2020.
The COVID-19 pandemic posed several ethical issues for nurses such as working in a critical care unit without proper training, caring for an unprecedented number of people dying alone, and a reported conflict between duty and their own safety as noted by respondents in this study. According to multiple authors, the COVID-19 pandemic has left nurses at the frontline of patient care at risk for moral distress and subsequent moral injury due to traumatic situations, uncertainties, and onerous ethical decisions faced in these times (Digby et al., 2020; Dimino et al., 2020; Lingis, 2020; Sun et al., 2020).
Rushton, Caldwell, and Kurtz (2016) examined moral distress and viewed it as an opportunity for “growth, empowerment, and increased moral resilience” (p. 40). Cacchione, in a 2020 editorial, discussed the risk of nurses developing moral distress when caring for patients with COVID-19 (Cacchione, 2020). Mental health resources and emotional support for nurses caring for patients with COVID-19 were defined as essential to sustaining moral integrity. Gujral, Rushton, & Rosa, 2020, in a Guest Editorial, discuss the need for nurses to “identify a plan for well-being and self-preservation” (p.2).
Awano et al., 2020, examined the rate of anxiety, depression and resilience in healthcare workers in Japan during the COVID-19 pandemic. The researchers surveyed medical healthcare workers at the Japanese Red Cross Medical Center in Tokyo, Japan Their research concluded that psychiatric symptoms occurred and therefore, there is a great need for mental health support. The use of “reflective listening, clarification, reassessment of perceptions” can be beneficial to the mental health of nurses and physicians working on the frontline (Viswanathan, Myers, & Fanous, 2020, p. 541). Hossain and Clatty (2020) investigated the concepts of moral distress and moral injury as they relate to the ethical dilemmas health care providers faced during the pandemic. They noted that “ health care professionals are likely to experience post-traumatic stress as a consequence of serving during the COVID-19 crisis” (p. 5). The authors note that self-care techniques are required to build moral resilience which “allows one to maintain perspective, keep a situation in context, and understand that some conditions are out of one's control” (p.5). The nurse respondents in our study listed sharing jokes and humor with coworkers, sufficient rest and time off, community recognition and support, taking protective measures, recreational activities such as shopping, streaming movies, outdoor exercising and social media as effective self-care techniques and measures to cope and reduce stress.
Furthermore, Sperling (2020) examined how nurses in Israel responded to ethical dilemmas and stress during the coronavirus pandemic. They rated their perceived risk of contracting the virus as high, feared coming to work, and preferred to care for patients with other medical or surgical diagnoses than patients with the coronavirus. Their research also examined nurses' responses to various ethical dilemmas that reflect values such as professional autonomy, beneficence, non-maleficence, equality, and justice” (p. 7). Nurses believed that it was the right of all patients to receive treatment. In cases of shortages of life-sustaining resources, the respondents did not believe that their medical team was qualified to make ethical decisions related to who should or should not receive treatment.
4.1. Strengths and limitations
Respondents were limited to current and graduate nurses from a single institution so expanding the population may strengthen the results. Nonetheless, a strength was the varied respondents' ages and alumni who were practicing in different areas of the U.S. A one-time survey of nurses caring for patients with COVID-19 lacks longitudinal data which could capture the changes that have occurred in the past year. Qualitative data were limited to open-ended questions, but individual semi-structured interviews or focus groups could enable richer narratives.
4.2. Conclusions and implications
Respondents in this study noted a high level of burnout, anxiety, depression, and fear during the COVID-19 pandemic. As the pandemic continues to overwhelm nurses on the frontline, its long-term effects remain to be exposed. Research findings during the SARS and MERS epidemics before March of 2020 foreshadowed the impending healthcare crisis caused by COVID-19 and its effect on nurses and other healthcare providers. Going forward, nurse educators and nursing administrators must use these lessons to protect nurses with appropriate training in self-care techniques, ethics, and moral resilience when faced with current and future major healthcare crises.
Funding
The authors did not receive any external funding.
Declaration of competing interest
The authors do not have any conflict of interest to report.
References
- Akgün K.M., Shamas T.L., Feder S.L., Schulman-Green D. Communication strategies to mitigate fear and suffering among COVID-19 patients isolated in the ICU and their families [editorial] The Journal of Cardiopulmonary and Acute Care. 2020;49(4):344–345. doi: 10.1016/j.hrtlng.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almutairi A.F., Adlan A.A., Balkhy H.H., Abbas O.A., Clark A.M. “It feels like I’m the dirtiest person in the world.”: Exploring the experiences of healthcare providers who survived MERS-CoV in Saudi Arabia. Journal of Infection and Public Health. 2018;11(2):187–191. doi: 10.1016/j.jiph.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awano N., Oyama N., Akiyama K., Inomata M., Kuse N., Tone M.…Izumo T. Anxiety, depression, and resilience of healthcare workers in Japan during the coronavirus disease 2019 outbreak. The Journal of Internal Medicine. 2020;20:293–299. doi: 10.2169/internalmedicine.5694-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacchione P.Z. Moral distress in the midst of the COVID-19 pandemic [editorial] Clinical Nursing Research. 2020;29(14):215–216. doi: 10.1177/1054773820920385. [DOI] [PubMed] [Google Scholar]
- Creswell, Poth . In: Qualitative inquiry and research design: Choosing among five approaches. 4th ed. Salmon H., Scappino J., editors. SAGE Publications; 2018. Standards of validation and evaluation. [Google Scholar]
- Digby R., Winton-Brown T., Finlayson F., Dobson H., Bucknall T. Hospital staff well-being during the first wave of COVID-19: Staff perspectives. International Journal of Mental Health Nursing. 2020 doi: 10.1111/inm.12804. [DOI] [PubMed] [Google Scholar]
- Dimino K., Horan K.M., Stephenson C. Leading our frontline HEROES through times of crisis with a sense of hope, efficacy, resilience, and optimism. Nurse Leader. 2020;1-5 doi: 10.1016/j.mnl.2020.05.011. , July 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gujral H., Rushton C.H., Rosa W.E. Action steps toward a culture of moral resilience in the face of COVID-19 [guest editorial] Journal of Psychosocial Nursing and Mental Health Services. 2020;58(7):2–4. doi: 10.3928/02793695-20200617-01. [DOI] [PubMed] [Google Scholar]
- Hofmeyer A., Taylor R. Strategies and resources for nurse leaders to use to lead with empathy and prudence so they understand and address sources of anxiety among nurses practicing in the era of COVID-19. Journal of Clinical Nursing. 2020;1-8 doi: 10.1111/jocn.15520. , October 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain F., Clatty A. Self-care strategies in response to nurses' moral injury during COVID-19 pandemic. Nursing Ethics. 2020;1-10 doi: 10.1177/0969733020961825. , October 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu D., Kong Y.W., Han Q., Zhang X., Xai Zhu L., Wei Wan S.…Zhu J. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study [eclinical medicine]. The Lancet. EClinicalMedicine. 2020;1-10 doi: 10.1016/j.eclinm.2020.100424. , June 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Council of Nurses (2020). ICN confirms 1,500 nurses have died from COVID-19 in 44 countries and estimates that healthcare worker COVID-19 fatalities worldwide could be more than 20,000. Retrieved December 5, 2020 from https://www.icn.ch/news/icn-confirms-1500-nurses-have-died-covid-19-44-countries-and-estimates-healthcare-worker-covid.
- Jennings B.M., Yeager K.A. From fear to fortitude: Using the power within the nursing profession to fight COVID-19. Nursing Outlook. 2020, May 3;68(2020):391–392. doi: 10.1016/j.outlook.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson U., Fraenkel C.-J. Covid-19: Risks to healthcare workers and their families: Mistakes made in the first wave must not be repeated in the second [editorial] British Medical Journal. 2020;371:m3944. doi: 10.1136/bmj.m3944. [DOI] [PubMed] [Google Scholar]
- Khalid I., Khalid T.J., Qabajah M.R., Barnard A.G., Qushmaq I.A. Healthcare workers perceived stressors and coping strategies during a MERS-CoV outbreak. Clinical Medicine and Research. 2016;14(1):7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague L.J., de Los Santos J.A.A. Fear of COVID-19, psychological distress, work satisfaction, and turnover intention among frontline nurses. Journal of Nursing Management. 2020;1-9 doi: 10.1111/jonm.13168. , September. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.Y., Hong J.H., Park E.Y. Beyond the fear: Nurses’ experiences caring for patients with Middle East Respiratory Syndrome: A phenomenological study. Journal of Clinical Nursing. 2020;29(3349–3362) doi: 10.1111/jocn.15366. [DOI] [PubMed] [Google Scholar]
- Lee S.H., Juang Y., Su Y., Lee H., Lin Y., Chao C. Facing SARS: Psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. General Hospital Psychiatry. 2005;27(5):352–358. doi: 10.1016/j.genhosppsych.2005.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingis A. The new fear of one another. Journal of Bioethical Inquiry. 2020, August doi: 10.1007/s11673-020-10035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell D. Balancing the duty to treat with the duty to family in the context of the COVID-19 pandemic. Journal of Medical Ethics. 2020;46:360–363. doi: 10.1136/medethics-2020-106250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushton C.H., Caldwell M., Kurtz M. CE: Moral distress: A catalyst in building moral resilience. American Journal of Nursing. 2016;116(7):40–49. doi: 10.1097/01.NAJ.0000484933.40476.5b. [DOI] [PubMed] [Google Scholar]
- Sperling, D. (2020, October). Ethical dilemmas, perceived risk, and motivation among nurse during the COVID-19 pandemic. Nursing Ethics. Retrieved December 5, 2020 from doi: 10.1177/0969733020956376. [DOI] [PMC free article] [PubMed]
- Sun N., Wei L., Shi S., Jiao D., Song R., Ma L.…Wang H. A qualitative study on the psychological experiences of caregivers of COVID-19 patients. American Journal of Infection Control. 2020;48(2020):592–598. doi: 10.1016/j.ajic.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Oxford. (2021). Our World in Data: Mortality risk of COVID chart. Retrieved January 10, 2021 from https://ourworldindata.org.
- Viswanathan, R., Myers, M. F., & Fanous, A. H. (2020). Support groups and individual mental health care via video conferencing for frontline clinicians during the COVID-19 pandemic. Psychosomatics, 61(5), 538–533. doi: 10.1016/j.psym.2020.06.014. [DOI] [PMC free article] [PubMed]
- World Health Organization. (2021a). Severe acute respiratory syndrome. Retrieved January 10, 2021 from https://www.who.int/health-topics/severe-acute-respiratory-syndrome#tab=tab_1.
- World Health Organization (2021b) Middle east respiratory syndrome. Retrieved January 10, 2021 from http://www.emro.who.int/health-topics/mers-cov/index.html.
- World Health Organization (2021c). Timeline: WHO's COVID response. Retrieved January 10, 2021, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline.