The assessment of professionalism focuses on 3 subcompetencies: professional behavior and ethical principles (PROF-1), accountability and conscientiousness (PROF-2), and self-awareness and help-seeking (PROF-3).1 As a result of harmonizing, Milestones 2.0 provides graduate medical education (GME) programs with a common set of subcompetencies across all specialties, with a developmental progression allowing for longitudinal assessment in training.2 The aim of this article is to provide guidance on assessing professionalism, using this harmonized set of subcompetencies.
A unique challenge for assessing professionalism in the learning and working environment is the overlap of behaviors (eg, showing up late for work) that could be considered misconduct (persistent tardiness despite clear expectations) or a lapse in the core competency of professionalism (late arrival to clinic due to difficulty balancing competing patient priorities). Residents are both employees and learners. This has important implications for remediation of professionalism concerns.
While the focus of this article is on the assessment of the professionalism subcompetencies, medical educators should also consider the outcomes of these assessments as opportunities to improve curricula and faculty development in these professionalism areas. For example, the COVID-19 pandemic has highlighted health disparities in the just distribution of resources. And, if the assessment of professionalism highlights a gap in ethics knowledge, there are resources to address these deficits.3 Program-level analysis of the subcompetency assessments should be used to drive curriculum improvement in these areas.
PROF-1: Professional Behavior and Ethical Principles
The foundational elements of medical professionalism were outlined by the American Board of Internal Medicine Foundation in their landmark article “Medical Professionalism in the New Millennium: A Physician Charter,” and the charter was subsequently adopted by all member boards of the American Board of Medical Specialties.4 These elements are incorporated into the PROF-1 subcompetency and include concepts such as professional conduct, ethical behavior, and professional identity formation (Figure 1). As such, it is a very broad subcompetency; thus, the methods for assessment are equally wide-ranging and include assessment scales, direct observations, multisource evaluations, and patient surveys. One of the most-studied tools is the Professionalism Mini-Evaluation Exercise (P-MEX), which is feasible to use in a GME environment.5,6 Additional selected validated assessment tools are listed in the Table.
Figure 1.
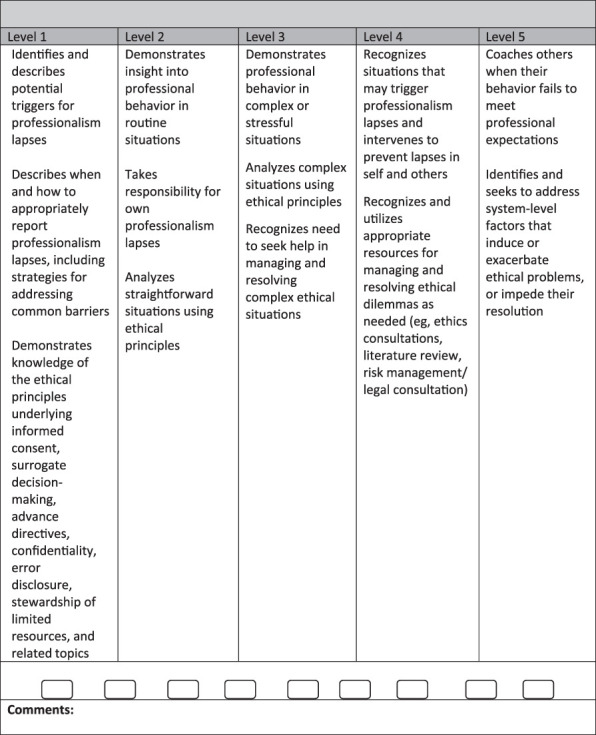
PROF-1: Professional Behavior and Ethical Principles
Table.
Selected Validated Tools to Assess Professionalism
| Tool or Assessment Type | Specialty | Authors |
| Assessment scale | Internal medicine | Arnold et al (1998)15 |
| Critical incident review | Medical students | Hodges et al (2005)16 |
| Encounter card | Obstetrics and gynecology | Brennan and Norman (1997)17 |
| Multisource assessment | Radiology | Wood et al (2004)18 |
| Patient survey | Internal medicine | Abadel and Hattab (2014)19 |
| Professionalism Mini-Evaluation Exercise (P-MEX) | Emergency medicine multiple | Amirhajlou et al (2019)20 Cruess et al (2006)21 |
| Simulation | Surgery | Lifchez et al (2015)22 |
Hodges and colleagues published an extensive review of the assessment of professionalism and highlighted several key points.7 First, a systematic approach to feedback is critical and requires a safe supportive environment, specific behavioral-based feedback that is both reinforcing of positive behaviors and corrective of lapses, and follow-up on behavior change over time. Second, the best assessment systems incorporate multiple measures by various observers over time, with data collected in a variety of settings including complex, challenging, and stressful situations. Third, identification and documentation of professionalism lapses and negative behaviors requires a process that is separate from the more general system that promotes medical professionalism as an academic competency.
When remediation is needed for a resident with professionalism difficulties, the plan should be specific and developed in conjunction with the resident. It should include further education, readings, and reflections to foster insight into one's behavior; specific measures to monitor for behavior change; and a specific timeline and follow-up. The Alpha Omega Alpha Honor Medical Society has a monograph that addresses remediation plans.8 A number of institutions also have programs to assist physicians with remediation.9,10 Some breaches of professionalism may require notification of hospital administration, specialty boards, state medical boards, or other authorities, and program directors should seek appropriate consultation in this regard.11
Even if a resident never has a lapse in professionalism, Levels 4 and 5 of this subcompetency describe aspirational behavior wherein residents can proactively recognize situations that may lead to lapses in themselves or others and can begin to coach others on professional behaviors. Some specialties have also developed a number of case scenarios that can be used to assess high-performing residents' skills in these areas.12
PROF-2: Accountability and Conscientiousness
Emanuel and Emanuel define professional accountability in health care as the procedures and processes by which physicians take responsibility for the activities related to patients and colleagues.13 The focus of control shifts as physicians take more responsibility for their administrative duties, patient care, and other tasks. Assessing Levels 1–3 of this subcompetency can be done by looking at how much external control is needed to ensure task completion. Multisource evaluations can also be used to gather outside input, especially related to patient care tasks. As with PROF-1, residents at Levels 4 or 5 begin to anticipate situations that may lead to lapses (eg, an upcoming busy rotation) and begin to mentor others to prevent or remediate lapses.
Conscientiousness is one of 4 elements of “trustworthiness” in providing patient care in a progressively autonomous manner.14 In the context of patient care, a resident could be assessed on the comprehensiveness of their data gathering and their reliability in completing or following through on tasks. As with accountability, the locus of control for conscientiousness should shift to the resident as they progress along the Milestones scale. The expectation for a Level 3 resident is the comprehensive completion of all tasks in a timely manner without prompting, and with resident-initiated help-seeking if barriers arise.
Expectations regarding accountability and conscientiousness increase as an individual takes on the role of physician, as they progress through their professional identity formation (Figure 2). While tools to measure professional identity are still limited,23 the use of multisource feedback in conjunction with a coaching model has been shown to be helpful in fostering professional development in this domain.24
Figure 2.
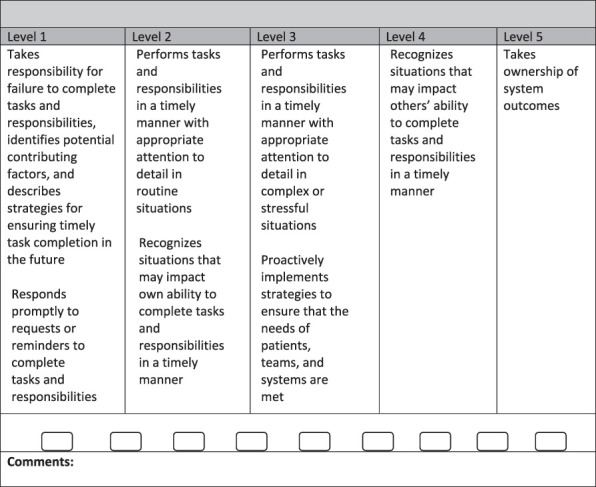
PROF-2: Accountability and Conscientiousness
PROF-3: Self-Awareness and Help-Seeking
This subcompetency highlights the importance of self-awareness and seeking help as components of professional identity formation (Figure 3). While the Milestones in this subcompetency were developed to focus on promoting personal and professional well-being, it is well-recognized that self-awareness, emotional intelligence, and asking for help are an important part of professional development. At the early stages of development, lack of self-awareness often leads to the need for help going unrecognized. Over time, a skilled physician recognizes that asking for help when needed benefits patients and that this benefit supersedes any perceived need to “demonstrate competence.”
Figure 3.
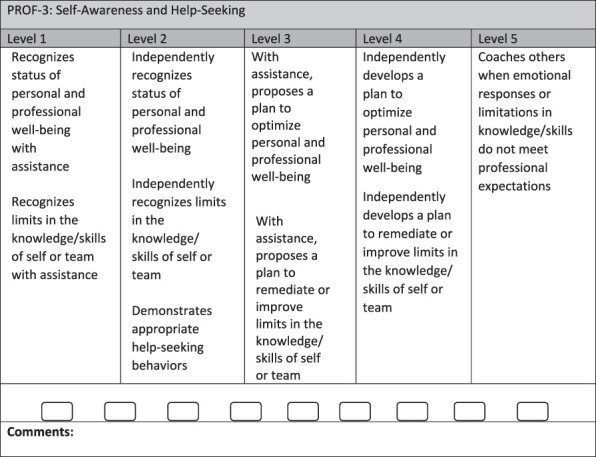
PROF-3: Self-Awareness and Help-Seeking
The focus of this subcompetency is not intended to be on the well-being or resilience of the resident, but rather on the resident's recognition of well-being as an essential element of their professional development and their knowledge of and ability to access resources. The assessment of this subcompetency can be done through direct observations, discussions between residents and faculty mentors, or through an analysis of a resident's individualized goals by the clinical competency committee. At the early levels of development, residents will need assistance in knowing when and how to ask for help, but over time, residents should independently be able to develop a plan to optimize their well-being.
Addressing Professionalism Lapses and Behavioral Misconduct
Program directors and GME leaders often grapple with strategies to remediate learners with behavior difficulties. Part of this challenge arises if lapses in behavior are managed solely as academic professionalism deficiencies, and this dilemma can be complicated further by misunderstanding or a lack of clarity regarding legal recourse and liability for these problems.25 GME leaders often struggle with taking decisive action (eg, suspension, dismissal) allowing the resident an opportunity to remediate, or both.
When a resident behaves inappropriately, the first question to ask is whether this constitutes misconduct. Misconduct includes behaviors where a reasonable person would know the behavior is wrong (eg, drug diversion, lying, cheating, or stealing). In determining how to respond, the program director would evaluate whether or not the resident: (1) should have known the behavior was wrong; (2) has the capacity to learn from their mistake (ie, has insight and remorse); and (3) has the ability to demonstrate proper conduct moving forward. The program director can also weigh other factors, such as the seriousness of any harm resulting from the behavior or the potential for future harm should the behavior reoccur. If a program director concludes that providing an opportunity to remediate creates a real risk of future similar bad behavior or harm resulting from any future bad behavior, it may be necessary to take effective action to prevent recurrence. For example, if a resident commits an intentional privacy breach by looking at a colleague's medical records for curiosity's sake, this is both unprofessional and misconduct. In this case, and particularly if the resident does not recognize that this behavior was wrong or is a serious problem, the employer has an obligation to take effective action to protect the organization, and categorizing this behavior as misconduct allows that to occur most efficiently.
Other behavioral problems may arise when a resident doesn't have the professional or cultural experience to recognize their behavior as problematic. For example, when a new intern tells a nurse to “follow the order,” they may be struggling with how best to communicate among the team in the midst of a stressful day. In this case, being rude is both misconduct and unprofessional. If, following an evaluation of the situation, the program director concludes the resident is amenable to learning from the situation, understands the effect of the actions, and is unlikely to repeat the misconduct, then it may be most appropriate to treat the issue academically, as a deficiency in professionalism, and provide the resident with an opportunity to cure.11,25 Figure 4 provides a framework for identifying when inappropriate behavior may be amenable to remediation as an academic deficiency in professionalism or should be treated as behavioral misconduct with a level of corrective action needed to prevent the behavior from recurring.
Figure 4.

Framework for Considering Behaviors as Deficiency in Academic Professionalism vs Misconduct
Conclusions
Medical professionalism is not inherent; it is not either present or absent. It can and must be taught, developed, and assessed. Harmonization of the professionalism subcompetencies across specialties should facilitate resident teaching, assessment, and coaching as it facilitates development of new tools and approaches.
Acknowledgments
The authors would like to thank Kerry Richard, Esq, Vice President and Senior Deputy General Counsel, MedStar Health Inc, for assistance with the revision of the manuscript.
References
- 1.Edgar L, Roberts S, Holmboe E. Milestones 2.0: a step forward. J Grad Med Educ. 2018;10(3):367–369. doi: 10.4300/JGME-D-18-00372.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edgar L, Roberts S, Yaghmour NA, et al. Competency crosswalk: a multispecialty review of the Accreditation Council for Graduate Medical Education Milestones across four competency domains. Acad Med. 2018;93(7):1035–1041. doi: 10.1097/ACM.0000000000002059. [DOI] [PubMed] [Google Scholar]
- 3.Carrese JA, Malek J, Watson K, et al. The essential role of medical ethics education in achieving professionalism: the Romanell Report. Acad Med. 2015;90(6):744–752. doi: 10.1097/ACM.0000000000000715. [DOI] [PubMed] [Google Scholar]
- 4.Foundation ABIM. American Board of Internal Medicine; ACP-ASIM Foundation. American College of Physicians-American Society of Internal Medicine; European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136(3):243–246. doi: 10.7326/0003-4819-136-3-200202050-00012. [DOI] [PubMed] [Google Scholar]
- 5.Kwan YH, Png K, Phang JK, et al. A systematic review of the quality and utility of observer-based instruments for assessing medical professionalism. J Grad Med Educ. 2018;10(6):629–638. doi: 10.4300/JGME-D-18-00086.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stern DT. Measuring Medical Professionalism. New York, NY: Oxford University Press; 2006. [Google Scholar]
- 7.Hodges BD, Ginsburg S, Cruess R, et al. Assessment of professionalism: recommendations from the Ottawa 2010 Conference. Med Teach. 2011;33(5):354–363. doi: 10.3109/0142159X.2011.577300. [DOI] [PubMed] [Google Scholar]
- 8.Alpha Omega Alpha Honor Medical Society. Byyny RL, Papadakis MA, Paauw DS. Medical Professionalism: Best Practices. 2021 https://alphaomegaalpha.org/medprof2015.html Accessed February 22.
- 9.Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med. 2007;82(11):1040–1048. doi: 10.1097/ACM.0b013e31815761ee. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200–1204. doi: 10.1097/ACM.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 11.Padmore JS, Richard KM, Filak AT. Human resources and legal management of residents who fail to progress. In: Stephens KG, editor. Guide to Medical Education in the Teaching Hospital 5th ed. La Vergne, TN: Association for Hospital Medical Education; 2016. pp. 273–295. [Google Scholar]
- 12.American Board of Pediatrics. Education and Training Committee. Teaching, Promoting and Assessing Professionalism Across the Continuum: A Medical Educator's Guide. 2021 https://www.abp.org/professionalism-guide Accessed February 22.
- 13.Emanuel EJ, Emanuel LL. What is accountability in health care? Ann Intern Med. 1996;124(2):229–239. doi: 10.7326/0003-4819-124-2-199601150-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy TJ, Lingard L, Baker GR, Kitchen L, Regehr G. Clinical oversight: conceptualizing the relationship between supervision and safety. J Gen Intern Med. 2007;22(8):1080–1085. doi: 10.1007/s11606-007-0179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arnold EL, Blank LL, Race KE, Cipparrone N. Can professionalism be measured? The development of a scale for use in the medical environment. Acad Med. 1998;73(10):1119–1121. doi: 10.1097/00001888-199810000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Hodges D, McLachlan JC, Finn GM. Exploring reflective “critical incident” documentation of professionalism lapses in a medical undergraduate setting. BMC Med Educ. 2009;9:44. doi: 10.1186/1472-6920-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brennan BG, Norman GR. Use of encounter cards for evaluation of residents in obstetrics. Acad Med. 1997;72(10 suppl 1):43–44. doi: 10.1097/00001888-199710001-00015. [DOI] [PubMed] [Google Scholar]
- 18.Wood J, Collins J, Burnside ES, et al. Patient, faculty, and self-assessment of radiology resident performance: a 360-degree method of measuring professionalism and interpersonal/communication skills. Acad Radiol. 2004;11(8):931–939. doi: 10.1016/j.acra.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Abadel FT, Hattab AS. Patients' assessment of professionalism and communication skills of medical graduates. BMC Med Educ. 2014;14:28. doi: 10.1186/1472-6920-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amirhajlou L, Bidari A, Alipour F, et al. Validity, reliability and acceptability of Professionalism Mini-Evaluation Exercise (P-MEX) for emergency medicine residency training. J Med Ethics Hist Med. 2019;12:12. doi: 10.18502/jmehm.v12i12.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruess R, McIlroy JH, Cruess S, Ginsburg S, Steinert Y. The professionalism mini-evaluation exercise: a preliminary investigation. Acad Med. 2006;81(suppl 10):74–78. doi: 10.1097/00001888-200610001-00019. [DOI] [PubMed] [Google Scholar]
- 22.Lifchez SD, Cooney CM, Redett RJ., 3rd The standardized professional encounter: a new model to assess professionalism and communication skills. J Grad Med Educ. 2015;7(2):230–233. doi: 10.4300/JGME-D-14-00275.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matthews J, Bialocerkowski A, Molineux M. Professional identity measures for student health professionals—a systematic review of psychometric properties. BMC Med Educ. 2019;19(1):308. doi: 10.1186/s12909-019-1660-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sawatsky AP, Huffman BM, Hafferty FW. Coaching versus competency to facilitate professional identity formation. Acad Med. 2020;95(10):1511–1514. doi: 10.1097/ACM.0000000000003144. [DOI] [PubMed] [Google Scholar]
- 25.Padmore JS, Andolsek KM, Iobst WF, Poulin LJ, Hogan SO, Richard KM. Navigating academic law in competency decisions. J Grad Med Educ. 2021;13(suppl 2):102–108. doi: 10.4300/JGME-D-20-00963.1. doi: 10.4300/JGME-D-20-00963.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


