Competency-based medical education (CBME) entails the assessment of learner development and a systematic approach to decision-making about learner progress. Decision-making by groups charged with generating valid judgments of progress can ensure learner readiness for advancement and inform feedback to learners. Programmatic assessment, which supports CBME, requires collecting and synthesizing multiple data points about learner performance to generate progress decisions.1
The study of group process and decision-making dates to the 1930s2 and includes theories and approaches that can inform educators' work in a CBME program. The importance of group decision-making in graduate medical education (GME) is highlighted by the Accreditation Council for Graduate Medical Education (ACGME) Next Accreditation System and requirement for clinical competency committees (CCCs).3 CCCs provide opportunities to consider how theories and approaches to group decision-making can be applied to enhance CBME.4–6 Groups tend to generate more ideas than individuals, are more likely to notice and correct errors, have better collective memory, and use more data in drawing conclusions.7,8 Theories and concepts for group decision-making (Table) show how group members influence one another's decisions both positively and negatively9,10; 5 functions (actions a group can take) for better group decisions11; and how large crowds make better decisions.12 However, lack of member diversity, poor data and poor data synthesis, incomplete information sharing,13 and groupthink14,15 threaten group advantages.
Table.
Concepts and Theories Relevant to the Science of Group Process Applicable to Clinical Competency Committees (CCCs)
| Theory or Framework | Description | Problem This Theory/Framework Could Address for a CCC | How Theory/Framework Applies to Improve CCC Group Process |
| Social decision scheme (SDS) theory9 | Based in an input-process-output framework, SDS theory considers how individual preferences, composition of preferences within the group, and patterns of group influence (how the group makes the decision using decision scheme or rules) yield collective decisions.21 | A CCC that lacks structure with regard to membership or defined processes for how information is shared and decisions are made is hoping to reflect on and codify its recruitment and processes. | Establishing diverse membership to ensure a wide range of individual preferences are represented and making clear how decisions will be made promotes consistency and fairness in the committee's work. |
| Functional theory11 | A group must achieve 5 “functions” for effective decision-making:21 1. Analyze problem: for thorough understanding. 2. Establish evaluation criteria: understand standards required to achieve an effective choice. 3. Generate realistic alternative options. 4. Evaluate advantages of potential solution options. 5. Evaluate disadvantages of potential solution options. | CCC members make different judgements about residents due to different understanding of the purpose and role of the committee or the criteria by which they judge residents' performance. For a particular resident, members may be uncertain how to support their learning through usual rotations or supplementary learning opportunities with a mentor or special schedule. | CCC members engage in training regarding the criteria by which they evaluate residents and the options for decisions about individual residents for proceeding in the program, undergoing remediation, or other. |
| Groupthink10 | Group members' desire for group cohesion and unanimity overrides their motivation to consider information carefully and leads them to make poor quality decisions. | Members of a CCC that has included the same membership for many years feel that they function efficiently and harmoniously. However, 2 residents the CCC deemed ready for graduation recently were determined by their fellowship directors to have major gaps in their competence. | Rotating membership enhances the array of viewpoints on the CCC. The chair can invite all members to speak and share dissenting opinions prior to decision-making. Group training and reflection about the risks of groupthink and monitoring their own practice is needed. |
| The Wisdom of Crowds12 | Groups tend to make better decisions than individuals when specific conditions are met: 1. Diverse group membership. 2. Each member makes initial decisions independently without influence of others. 3. Tacit knowledge and experience are acknowledged and integrated. 4. Individual decisions are aggregated into a group decision. | A CCC experiences some member dissatisfaction. Some members of a CCC feel that they are not contributing actively to the CCC, and recently some members have not spoken at all during committee meetings. | The CCC can recruit members with diversity of experiences, backgrounds, and opinions, who are then allowed to make individual judgments based on review of performance data before the group comes together to share opinions and come to consensus. |
As GME programs have implemented CCCs, some simply followed ACGME requirements to schedule meetings to review learners' assessments. This approach typically focused on residents with performance problems. In contrast to this problem identification approach, CCCs using a developmental approach find added value from the committee process.16 By going beyond minimum requirements, some CCCs have formed dynamic groups to optimize procedures and methods for analyzing learners against the Milestones.17,18
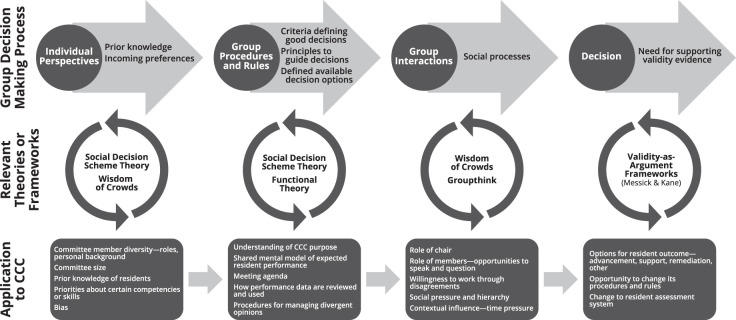
This article presents a model of the CCC group decision-making process (Figure), informed by key theories and ideas relevant to group decision-making. Understanding group decision-making entails consideration of individual members and their initial preferences, rules guiding the group, interactions and relationships among members, and group decisions. The Wisdom of Crowds highlights the importance of these steps and purports that groups usually make more accurate decisions than individuals, but only when they meet certain criteria.12 These criteria include members who bring diverse opinions from decentralized, varied contexts, and maintain their independent opinions until a structured process occurs for aggregating opinions into decisions.12 For CCCs, implications of these requirements are described as follows.
Figure.
Group Decision-Making Framework Relevant for Clinical Competency Committees
Individual Member Perspectives
Individual member perspectives are the opinions, knowledge, and preferences that participants bring. Broad perspectives enhance group work through expansion of information and options that the group considers. Diversity of opinion promotes dissent and invites varied opinions, which help the group consider multiple decision options and avoid premature closure.19 Breadth of individual preferences is fostered through recruiting members with diverse backgrounds, genders, race/ethnicity, experiences, and workplace roles. For CCCs, practical applications of attention to individual member perspectives arise as the committee is populated. For example, one study in pediatrics demonstrated that more experienced members rated residents lower.20 Recruiting members from different clinical services and sites decentralizes representation. Members who are junior and senior, as well as newer and more experienced with resident teaching and assessment, also bring varied perspectives.
Strategies to address individual bias, which can influence group decisions, must address both individual and systemic factors. Individual committee members should participate in training on recognizing and minimizing harmful bias in resident review. Organizational efforts to increase representation of diverse providers among faculty and trainees are needed.22
Group Procedures and Rules
Group procedures and rules are the ways by which a group defines its work and understands its decision-making processes. Social decision scheme (SDS) theory describes how individual members combine their preferences to reach a group decision.23 “Social decision schemes” are rules or procedures by which the group comes to a collective decision (eg, majority vote or consensus). Schemes may be explicitly written, as in bylaws, or implicit.24 Stated and codified rules are ideal to ensure common understanding. However, tacit, unspoken rules may emerge over time and influence decisions through group experience or social pressure within the group.
The CCC chair should ensure that the CCC defines a clear purpose of its work and establishes common understanding of procedures for reviewing resident performance and the available decisions. Functional theory asserts that group decision-making success depends on the group's understanding of the problem it is addressing, criteria for decision-making, and various options for decisions and consequences of each.11 New members will require training in these areas. Efforts to analyze the problem and agree on criteria for determining merits of each decision option shape shared understanding of the group's goal, which is a decision that satisfies the predetermined criteria. The CCC can weigh potential positive and negative consequences of various alternative judgments about a resident and consequences for that resident, thereby maintaining a rational analytic approach. In this way, functional theory draws focus to the task more so than the group members or the way that members influence one another. Sound decision-making according to functional theory depends on group members having access to and sharing information, preconditions to their coming to agreements about decisions, and relative merits compared to alternatives.25
Group Interactions
Interactions within a group involve information sharing and social influence. Members may debate, argue, and defend their positions to influence others.4 CCCs employ variable interactive processes and data interpretation techniques to reach decisions.20,26 Making information available prior to or during meetings enables everyone to contribute to deliberations. Structured procedures for who will speak include inviting the most knowledgeable member to speak first about an individual resident or the most junior person to initiate the discussion, in order to engage those with the most information and those whose voices may not be included.
Psychological safety is important to maximize each member's contributions to the group's output.27 In a psychologically safe environment, members feel respected and comfortable sharing within the group, and trust other members to listen and share productively. Members should feel able to make initial judgments independently without influence before sharing their opinions and potentially modifying their opinions in light of group deliberations to reach a consensus decision. Social influences within a group can undermine the wisdom of crowd effect when individuals feel prevented from thinking independently.28
Groupthink refers to the tendency of groups to prioritize agreement and group cohesion to the point that they suppress contradictory or discrepant thoughts.10 Desire to maintain group harmony overrides consideration of alternatives and critical viewpoints. Groupthink can afflict well-intended and seemingly high functioning groups. Rather than being probed, silence is inferred to mean assent. Some may presume that decisions are fair and ethical because they derive from a group.
High workload and time pressure within CCCs can create conditions for groupthink. Recent evidence suggests that CCCs may conflate their own performance with experience, hallmarks of groupthink.29,30 Directive leaders, high cohesion, poor decision-making methods, and time constraints all promote groupthink.31,32 Groupthink draws focus to the desire or social pressure to achieve consensus, and contrasts with functional theory, which emphasizes the group's careful understanding and weighing of various alternatives. However, CCCs can employ strategies to guard against groupthink, beginning with group leaders who encourage deliberation and invite sharing of new opinions. One study elaborated how CCC members engaged in effortful discussion to reconcile contradictory performance information rather than rush to a decision.33 Membership turnover or appointed “devil's advocates” may improve consideration of alternatives and enhance decision-making.10,30 Frequent assessment of and reflection on the group's decisions encourage more thorough deliberations.34
Decision Outcomes
Desired outcomes of CCC work include defensible decisions, accurate reporting on trainee performance to the ACGME, and useful formative learning plans for trainees. Unfortunately, few if any studies show whether CCC decisions are accurate, correct, or helpful, and the need to measure CCC outcomes presents a significant challenge. To date, most CCC literature describes group structure or process without examples of Messick's consequences validity35 or Kane's extrapolation or implications evidence.36 Studies correlating Milestone ratings with performance on medical knowledge examinations offer a starting point for this validity work.37–40 Future work is needed to examine whether CCCs can validate decisions with learning and patient care outcomes data. Defining ideal CCC outcomes and how to achieve them will require deep understanding of group dynamics, data infrastructure, and learning analytics to describe, characterize, predict, and influence behavior in medical training.41
Conclusions
Evidence across fields showing how groups outperform individuals on decision-making under certain conditions can bolster the productive use of CCCs in medical education.7 The many group decision-making foibles studied in fields outside of medicine likely also occur within CCCs. A CCC in one institution may look very different than a CCC in another, even within the same specialty, and certainly across specialties. However, standardization of core CCC functions (based on the figure), along with chair and member training on group purpose and procedures, can contribute to highest-yield group communication processes and standardize CCC outcomes. Further research on group decision-making in GME can elucidate ways for group process to empower faculty and CCCs to benefit learners.
Acknowledgments
The authors would like to thank Alisa N. Strauss, PhD, for her assistance with the Figure.
References
- 1.van der Vleuten CPM, Schuwirth LWT, Driessen EW, et al. A model for programmatic assessment fit for purpose. Med Teach. 2012;34(3):205–214. doi: 10.3109/0142159X.2012.652239. [DOI] [PubMed] [Google Scholar]
- 2.Gurnee H. A comparison of collective and individual judgments of fact. J Exper Psychol. 1937;21(1):106–112. doi: 10.1037/h0057058. [DOI] [Google Scholar]
- 3.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 4.Chahine S, Cristancho S, Padgett J, Lingard L. How do small groups make decisions?: A theoretical framework to inform the implementation and study of clinical competency committees. Perspect Med Educ. 2017;6(3):192–198. doi: 10.1007/s40037-017-0357-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hauer KE, Cate OT, Boscardin CK, et al. Ensuring resident competence: a narrative review of the literature on group decision making to inform the work of clinical competency committees. J Grad Med Educ. 2016;8(2):156–164. doi: 10.4300/JGME-D-15-00144.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dickey CC, Thomas C, Feroze U, Nakshabandi F, Cannon B. Cognitive demands and bias: challenges facing clinical competency committees. J Grad Med Educ. 2017;9(2):162–164. doi: 10.4300/JGME-D-16-00411.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stangor C. Principles of Social Psychology—1st International Edition. Jhangiani R, Tarry H, editors. BCcampus Open Education. 2021 eds. https://opentextbc.ca/socialpsychology/ Accessed February 22.
- 8.Johnson DH, Johnson FP. Joining Together Group Theory and Group Skills 11th ed. London, UK: Pearson; 2012. [Google Scholar]
- 9.Stasser G. A Primer of Social Decision Scheme Theory: models of group influence, competitive model-testing, and prospective modeling. Organ Behav Hum Decis Processes. 1999;80(1):3–20. doi: 10.1006/obhd.1999.2851. [DOI] [PubMed] [Google Scholar]
- 10.Janis IL. Groupthink. Psychol Today. 1971;5:43–46. [Google Scholar]
- 11.Orlitzky M, Hirokawa RY. To err is human, to correct for it divine: a meta-analysis of research testing the functional theory of group decision-making effectiveness. Small Group Res. 2001 doi: 10.1177/104649640103200303. 32(3) [DOI]
- 12.Surowiecki J. The Wisdom of Crowds. New York, NY: Anchor Books; 2005. [Google Scholar]
- 13.Faulmüller N, Kerschreiter R, Mojzisch A, Schulz-Hardt S. Beyond group-level explanations for the failure of groups to solve hidden profiles: the individual preference effect revisited. Group Processes Intergroup Relations. 2010;13(5):653–671. doi: 10.1177/1368430210369143. [DOI] [Google Scholar]
- 14.Janis IL. Groupthink Psychological Studies of Policy Decisions and Fiascoes. Boston, MA: Wadsworth, Cengage Learning; 1982. [Google Scholar]
- 15.Baron RS. So right it's wrong: groupthink and the ubiquitous nature of polarized group decision making. Adv Exper Soc Psychol. 2005;37:219–253. doi: 10.1016/S0065-2601(05)37004-3. [DOI] [Google Scholar]
- 16.Hauer KE, Chesluk B, Iobst W, et al. Reviewing residents' competence: a qualitative study of the role of clinical competency committees in performance assessment. Acad Med. 2015;90(8):1084–1092. doi: 10.1097/ACM.0000000000000736. [DOI] [PubMed] [Google Scholar]
- 17.Ketteler ER, Auyang ED, Beard KE, et al. Competency champions in the clinical competency committee: a successful strategy to implement milestone evaluations and competency coaching. J Surg Educ. 2014;71(1):36–38. doi: 10.1016/j.jsurg.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Nabors C, Forman L, Peterson SJ, et al. Milestones: a rapid assessment method for the clinical competency committee. Arch Med Sci. 2017;13(1):201–209. doi: 10.5114/aoms.2016.64045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dai P. The conceptual model of influencing factors and influencing mechanism on team decision-making quality mediated by information sharing. IB. 2013;5(4):119–125. doi: 10.4236/ib.2013.54015. [DOI] [Google Scholar]
- 20.Schumacher DJ, King B, Barnes MM, et al. Influence of clinical competency committee review process on summative resident assessment decisions. J Grad Med Educ. 2018;10(4):429–437. doi: 10.4300/JGME-D-17-00762.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wittenbaum GM, Hollingshead AB, Paulus PB, et al. The functional perspective as a lens for understanding groups. Small Group Res. 2004;35(1):17–43. doi: 10.1177/1046496403259459. [DOI] [Google Scholar]
- 22.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118(4):293–302. doi: 10.1093/phr/118.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davis JH. Group decision and social interaction: a theory of social decision schemes. Psychol Rev. 1973;80(2):97–125. doi: 10.1037/h0033951. [DOI] [Google Scholar]
- 24.Laughlin PR. Social choice theory, social decision scheme theory, and group decision-making. Group Processes Intergroup Relation. 2011;14(1):63–79. doi: 10.1177/1368430210372524. [DOI] [Google Scholar]
- 25.Gouran DS, Hirokawa RY, Julian KM, Leatham GB. The evolution and current status of the functional perspective on communication in decision-making and problem-solving groups. Annal Int Comm Assoc. 1993;16(1):573–600. doi: 10.1080/23808985.1993.11678870. [DOI] [Google Scholar]
- 26.Schumacher DJ, Michelson C, Poynter S, et al. Thresholds and interpretations: how clinical competency committees identify pediatric residents with performance concerns. Med Teach. 2018;40(1):70–79. doi: 10.1080/0142159X.2017.1394576. [DOI] [PubMed] [Google Scholar]
- 27.Edmondson AC. The Fearless Organization Creating Psychological Safety in the Workplace for Learning Innovation and Growth. Hoboken, NJ: John Wiley & Sons; 2018. [Google Scholar]
- 28.Lorenz J, Rauhut H, Schweitzer F, Helbing D. How social influence can undermine the wisdom of crowd effect. Proc Natl Acad Sci U S A. 2011;108(22):9020–9025. doi: 10.1073/pnas.1008636108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schumacher DJ, Poynter S, Burman N, et al. Justifications for discrepancies between competency committee and program director recommended resident supervisory roles. Acad Pediatr. 2019;19(5):561–565. doi: 10.1016/j.acap.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Schumacher DJ, Martini A, Bartlett KW, et al. Key factors in clinical competency committee members' decisions regarding residents' readiness to serve as supervisors: a national study. Acad Med. 2019;94(2):251–258. doi: 10.1097/ACM.0000000000002469. [DOI] [PubMed] [Google Scholar]
- 31.Riordan D, Riordan M. Guarding against groupthink in the professional work environment: A checklist. J Acad Bus Ethics. 2013;7:1–8. [Google Scholar]
- 32.Chen Z, Lawson RB, Gordon LR, McIntosh B. Groupthink: deciding with the leader and the devil. Psychol Rec. 1996;46(4):581–590. doi: 10.1007/BF03395186. [DOI] [Google Scholar]
- 33.Pack R, Lingard L, Watling CJ, Chahine S, Cristancho SM. Some assembly required: tracing the interpretative work of clinical competency committees. Med Educ. 2019;53(7):723–734. doi: 10.1111/medu.13884. [DOI] [PubMed] [Google Scholar]
- 34.Kaba A, Wishart I, Fraser K, Coderre S, McLaughlin K. Are we at risk of groupthink in our approach to teamwork interventions in health care? Med Educ. 2016;50(4):400–408. doi: 10.1111/medu.12943. [DOI] [PubMed] [Google Scholar]
- 35.Cook DA, Beckman TJ. Current concepts in validity and reliability for psychometric instruments: theory and application. Am J Med. 2006;119(2):166.e7–e16. doi: 10.1016/j.amjmed.2005.10.036. [DOI] [PubMed] [Google Scholar]
- 36.Kane MT. Current concerns in validity theory. J Educ Measure. 2001;38(4):319–342. doi: 10.1111/j.1745-3984.2001.tb01130.x. [DOI] [Google Scholar]
- 37.Hamstra SJ, Yamazaki K, Barton MA, Santen SA, Beeson MS, Holmboe ES. A national study of longitudinal consistency in ACGME milestone ratings by clinical competency committees: exploring an aspect of validity in the assessment of residents' competence. Acad Med. 2019;94(10):1522–1531. doi: 10.1097/ACM.0000000000002820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hauer KE, Vandergrift J, Lipner RS, Holmboe ES, Hood S, McDonald FS. National internal medicine milestone ratings: validity evidence from longitudinal three-year follow-up. Acad Med. 2018;93(8):1189–1204. doi: 10.1097/ACM.0000000000002234. [DOI] [PubMed] [Google Scholar]
- 39.Hauer KE, Vandergrift J, Hess B, et al. Correlations between ratings on the resident annual evaluation summary and the internal medicine milestones and association with ABIM certification examination scores among US internal medicine residents, 2013–2014. JAMA. 2016;316(21):2253–2262. doi: 10.1001/jama.2016.17357. [DOI] [PubMed] [Google Scholar]
- 40.Mainous AG, Fang B, Peterson LE. Competency assessment in family medicine residency: observations, knowledge-based examinations, and advancement. J Grad Med Educ. 2017;9(6):730–734. doi: 10.4300/JGME-D-17-00212.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chan T, Sebok-Syer S, Thoma B, Wise A, Sherbino J, Pusic M. Learning analytics in medical education assessment: the past, the present, and the future. AEM Educ Train. 2018;2(2):178–187. doi: 10.1002/aet2.10087. [DOI] [PMC free article] [PubMed] [Google Scholar]