Abstract
After a medical student prompted medical faculty to tell their stories of depression and related mental health issues, the author wrote this article with the aim of decreasing the stigma of mental illness and encouraging treatment, as needed, in the medical profession. The professional culture of the house of medicine not only mimics society in attributing stigma to people with mental health issues but may also contribute to high rates of suicide in the ranks of health care professionals by leading to a delay in seeking treatment. Acculturation accelerates in the first year of medical school such that medical students experience an increase in burnout and depressive symptoms from prematriculation levels. It follows that faculty have a responsibility to improve the learning environment. Survey data from medical faculty at the author’s institution showed that depression decreased respondents’ willingness to seek mental health treatment because of the stigma and issues of access to help. Faculty attitudes toward mental health issues, including reluctance to admit having such issues, may be conveyed to medical students in the hidden curriculum that teaches them to keep depression hidden. Moreover, the fear of mental disorders is manifested in licensing and privileging applications under the guise of patient safety, contributing to a culture of shame and silence. As creators and guardians of this professional culture, medical faculty and other physicians must be the ones who change it. The same faculty who play a part in causing and perpetuating stigma related to mental health issues have the power to derive and enact some of the solutions. In addition to giving voice to a personal experience of mental health issues, this article offers suggestions for normalizing moderate to severe depression as a medical disorder, decreasing the stigma of mental health issues, and encouraging faculty to seek treatment.
After I spoke on a panel about physician burnout in my organization, a medical student commented that faculty leaders who were willing to tell their own stories about depression might help to normalize mental disorders, reduce the stigma associated with mental health issues, and enable health professionals to seek treatment. As the chief wellness officer at a large academic health system, I have written this article with the intent of sharing my story and making it safer for others to tell their stories and seek help when needed.
A Physician’s Experience and the Prevalence of Depression
Medical students and residents are particularly vulnerable to depression, starting in medical school. One study found that matriculating medical students have fewer symptoms of burnout and depression than their college graduate peers. 1 Longitudinal studies have shown that medical students’ depressive symptoms increase by an average of 14% during medical school compared with their baseline before they started medical school. 2 A meta-analytic study of medical students found a depression rate of 18% 2 as measured by a score of 10 or greater on the Patient Health Questionnaire-9 (PHQ-9), a screening threshold for a diagnosis of major depression. 3 Similarly, another meta-analytic review found that 21% of residents had at least moderate depressive symptoms 4 as measured by the PHQ-9. 3 By comparison, the 12-month prevalence of major depression in the general population for people aged 18 to 29 is 13% and decreases with age. 5 Of particular concern with the advent of the COVID-19 pandemic is early evidence suggesting that the rate of depression in physicians across age groups is 25%. 6
I vividly remember my first rotation in general internal medicine as a first-year psychiatry resident in California during the 1980s. I summoned the courage to tell my second-year resident that I needed to be away at the same time weekly to attend visits with my psychiatrist. Before he could say anything, I said, “You really don’t want to see what I look like if I don’t go!” I felt surprise and relief that he agreed to my absences, and I started my first course of psychotherapy. Perhaps he thought that psychiatrists choose their specialty because they are trying to solve their own problems. Maybe he was just an understanding person, had someone with mental illness in his own family, or was in therapy himself. I will never know. What I do know is that there is nothing inappropriate about wanting to take care of our problems and seeking help to do so. We could be harming ourselves not to.
During residency, I could hide my shame by telling myself and others a convenient truth: Engaging in psychotherapy was especially encouraged then as a necessity of psychiatric training. We needed to learn how our personal histories and psychological makeup could affect the work we do with patients—to become aware of our unconscious biases. 7 Our own therapy also allowed us to understand the patient experience of psychotherapy. Although this truth provided a good cover story, I really needed to process my grief after my brother’s suicide 10 years earlier, when I was 17. His suicide was a daily, intrusive memory and a source of guilt and shame, which I had rarely discussed with anyone until much later in my career. 8
I learned in my first course of psychotherapy that I had already suffered 2 depressive episodes—the first during the aftermath of my brother’s death and the second in medical school after an unexpected breakup. Although I did not think of these episodes as depression at the time, I experienced intense psychic pain, especially during the second episode. On a nightly basis for numerous weeks, I sat on my bed for what seemed like hours holding my head and rocking when I could no longer concentrate on my medical studies. I felt terribly alone and told no one. Otherwise, I appeared well and “passed for normal” during class, on clinical rotations, or with friends. Although friends and acquaintances saw that outwardly I performed well and graduated with honors, my internal struggle with fear and shame caused me to delay treatment for many years.
After completing residency and moving across the country to start my academic career, I told my next therapist, a clinical psychologist, about several childhood events. He described them as “abusive,” which surprised me. I had treated many patients with abusive childhoods—but my own? Apparently, my medical knowledge did not translate into insight. Later, when my mood worsened, my wife suggested that I consider medication. I was reluctant to see a psychiatrist, arguing that I knew them all in our community.
Barriers to Seeking Treatment
Reluctance to seek mental health treatment among physicians is common. In an anonymous survey of 1,048 academic physicians (response rate 40%), 9 12% endorsed moderate to severe depressive symptoms in the 2 weeks before the survey, as measured by a score of 10 or more on the PHQ-9. Of those, fewer than half reported that they were likely to seek treatment for a mental health concern. Stigma and access to treatment were major concerns related to seeking treatment. More than half of the physicians surveyed endorsed survey items pertaining to stigma, and 70% of physicians with moderate to severe depression reported “getting an appointment that fits my schedule” as a major concern.
In a study of medical students, those with moderate to severe depression were significantly more likely to endorse statements about stigma than those with minimal or mild symptoms. 10 In another study of medical students, 62% agreed that if they were to receive treatment for an emotional/mental health problem, they would hide it from other people. Furthermore, half agreed that if a residency director was aware that a student applying for a residency had an emotional/mental health problem, then the director would pass over that student. 11
When medical interns were asked about factors that might affect their decision to receive mental health treatment for depression, 57% and 52% reported concerns about confidentiality and what others would think, respectively. Of those who screened positive for depression, fewer than a quarter reported starting treatment during their internship. 12 Other research found residents across different specialties expressed moderate to high levels of concern that their supervisors or program directors might become aware that they had depression or alcohol or other drug problems. 13 Overall, such concerns about stigma among medical students, residents, and faculty physicians contribute to reluctance to seek treatment, which has the effect of delaying treatment, especially among those with the most severe symptoms.
Despite my reluctance to see a psychiatrist, I agreed to a visit with my primary care physician (PCP) who started me on an antidepressant. I did well. Unfortunately, the severity of my symptoms increased with the next depressive episode when, for the first time, I had suicidal thoughts. My PCP appropriately wanted me to see a psychiatrist. I initially resisted his advice. I did not want to admit how serious my illness was, yet I could intellectually acknowledge my risk factors for suicide: male gender, family history, traumatic childhood, major mood disorder, and now suicidal thoughts. 14–17 I finally appreciated, with the support of my wife and PCP, that I could not ignore my risk for suicide any more than if I had a potentially fatal physical illness. Only then did I see a trusted psychiatric colleague, albeit in a different city from the one where I lived, one where no one knew me. The sad truth is that suicide is one of our profession’s occupational hazards, with disproportionately higher rates in female than in male physicians (2.3 times and 1.4 times higher than rates in the general population, respectively). 18
Our fears as a society feed stigma, stoked in part by media coverage linking mass shootings to mental illness. 19 Most violent acts are committed by people without mental illness, yet 30% of Americans believe that people with major depression are likely to be violent toward others. 20 In the general population, fear of seeking treatment is fueled by indelible visual images of patients harmed by anachronistic treatments like lobotomy and indiscriminate use of electroconvulsive therapy without modern anesthesia. 21,22 Another fear, particularly for people with mental illness, is involuntary hospitalization. 23 In short, our societal biases associate mental illness with unpredictable violence, punishment, and loss of autonomy.
Physicians are also members of society, with a major difference from nonphysicians. During medical school, we are trained in the contemporary biology of mental disorders, safe and effective treatments, and the compassionate care of all patients. So, what causes our reluctance to seek mental health treatment for ourselves? We do.
We judge each other too frequently for having mental health issues. 24,25 We fear that if we disclose illness to our colleagues and seek help, they will judge us as weak and less capable of doing our work. They may betray our confidentiality and use the information against us. Our greatest fear is putting our careers in jeopardy, especially with licensing boards. 26–28 Ironically, we put our lives in jeopardy to save our careers—even though suicide is career ending. Moreover, we are the ones who sit on medical boards and credentialing committees. We decide who gets accepted or not to medical school and residency programs and who gets promoted or not. We are the ones who perpetuate stigma associated with mental illness through our judgments of peers, residents, and medical students. 24,25
Some of the supplemental application forms I filled out when I applied to medical school in the mid-1970s required responses to all questions, including one about a family history of mental illness. I felt morally distressed by this yes/no question, which was followed by, “Please explain if yes,” because I had to choose between the values of truth and personal privacy. After wrestling with my conscience, I allowed my shame to answer. Unfortunately, we still unnecessarily challenge our medical students, residents, and colleagues with similar questions. 26,28
Of course, impaired colleagues who provide unsafe care should be removed from practice. However, medical leave can accomplish this necessary step without public disclosure in many, if not most, cases. Early diagnosis and treatment—unhindered by stigma—provide the key to preventing impairment and mitigating the risk of suicide. 29–31
Solutions
The good news is that our professional culture is ours to change. 32 If we cause and perpetuate stigma, then we control the solutions. Where do we start?
First, we can speak up and tell our stories, as suggested by the medical student who prompted me and by the courageous examples of others. 33,34 I can share my experience with those who are reluctant to seek treatment because I know how it feels to struggle with feelings that inhibited treatment seeking even as I suffered with suicidal thoughts. Nevertheless, I did take some actions during my illness that helped me to create a safety net when those thoughts surfaced. I started treatment for depression many years before having suicidal thoughts, and therapy taught me to manage my shame and internalized stigma. I also established a trusting relationship with my PCP over many years, so I could more easily call on him when I was ready to discuss medication. Lastly, I had one person, my wife, with whom I could share anything, and I relied on her to have my best interests in her heart. Overall, I’ve had the professional career I wanted despite a history of depression, which I attribute in large part to obtaining the treatment I needed with the help of others.
Second, we can advocate with our state governing bodies, medical boards, and hospital credentialing committees, which still ask inappropriate questions about our mental health, to adopt this question that is recommended by the Federation of State Medical Boards 35 and endorsed by other professional organizations, such as the American Medical Association 36 and the American Psychiatric Association 37:
Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner?
The question focuses on current impairment, encourages treatment, and does not distinguish between psychological and physical conditions. It also does not inquire about the history of a condition and recognizes that a mental health diagnosis does not mean that an individual is impaired.
Third, we can expand our perspective of mental health disorders. Narrow perspectives lend themselves to unidimensional statements, such as mental illness is a weakness or mental disorders are brain disorders. Unfortunately, reductionist thinking or models of illness can contribute to misunderstanding and stigma. 38 Similar to the approach taken with many disorders in medicine, recognizing the complexity of risk factors and implications for treatment may better serve our patients and profession. 39,40 Members of our profession, of all professions, should be able to stop equating illness with weakness. Fourth, we can adapt evidence-based practices for decreasing mental illness stigma and discrimination in the workplace. 41–43
Fifth, we can change our use of stigmatizing language. Labeling people as having mental disorders may unintentionally categorize them as a social out-group, subject to discrimination and disadvantage rather than to inclusiveness and equity. 38 Instead of categorizing people, we can view mental health and mental illness as part of a continuum. The World Health Organization describes mental health as more than the absence of a mental disorder or illness. 44 It emphasizes mental health as a state of well-being in which individuals realize their own abilities, cope with the normal stresses of life, work productively, and contribute to their community. A colleague suggested that we start talking about emotional health rather than mental health, because we all have emotions, whereas we do not all have mental disorders. Feeling stressed or having emotional distress may sound more acceptable than having a mental disorder.
Language is also important when physicians struggle with substance use disorders, which frequently co-occur with depression. 45 Referring to individuals as substance abusers or addicts is especially stigmatizing because these terms can imply a moral weakness resulting in willful misconduct and deserving of punishment. 46–49 Accordingly, substance abuse was removed from the American Psychiatric Association’s diagnostic nomenclature in 2013 and replaced with substance use disorder. 50 Nevertheless, the term abuse remains ingrained in the names of addiction journals 46,49 and federal government agencies 46 as well as in hospital-based policies on drug use and testing. The terms addict and alcoholic are labels that some people who affiliate with Narcotics Anonymous or Alcoholics Anonymous apply to themselves to reinforce a positive identity of being in recovery. However, these are not diagnostic terms, and the value of self-labeling during professional treatment for facilitating recovery is unknown. 51 The preferred phrase is a person with a substance (or alcohol) use disorder. 46–49
Burnout refers to a syndrome caused by chronic workplace-related stressors, characterized by feeling exhausted, disconnected from patients and work, and ineffective at what used to be meaningful work. 52 Many studies find considerable overlap between burnout and depression, but controversy exists about whether the 2 are distinct entities. 9,53 Regardless, some medical students and physicians may find it less stigmatizing to think of themselves as burned-out rather than depressed. Whether identifying oneself as burned-out has value for depression screening is a fruitful area for research. Language can be modified with respect to suicide as well: We can replace the phrase “committed suicide,” which connotes committing a crime or a sin, with “died by suicide.” 54
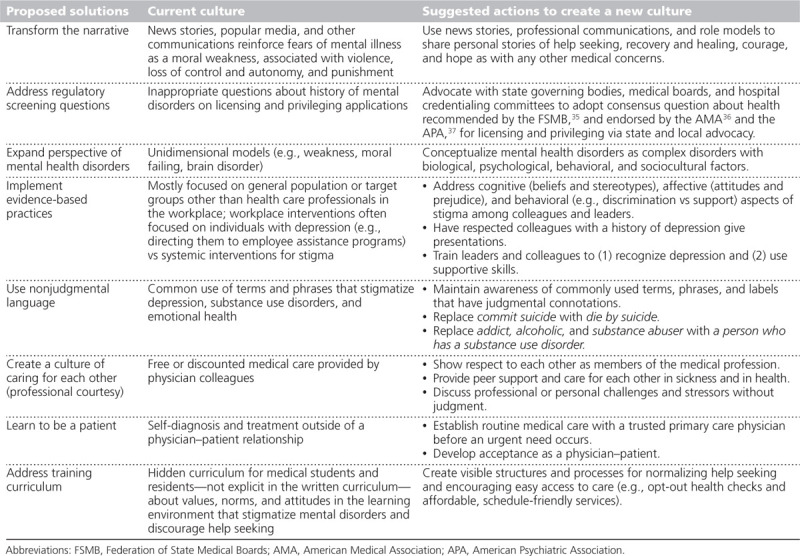
Sixth, we can create a professional culture of caring for each other within our medical schools, hospitals and clinics, and professional associations and societies. We can show support for each other in sickness and in health because we will all be patients someday for one reason or another. 55 We can encourage each other to establish routine medical care for health maintenance with a PCP before an urgent need arises. Seventh, diagnosing and treating ourselves or asking colleagues to order tests and prescribe medications outside the physician–patient relationship is not a substitute for proper primary care. 56 Finally, as faculty, we can address the hidden curriculum of medical students and residents, which subverts seeking treatment by teaching that mental disorders should remain hidden. 57 We can design mechanisms to encourage well-being—defined as an optimal experience and quality of life in the learning and work environment—as well as facilitate confidential access to treatment. 11,58 We owe each other these new norms of professional courtesy. (See Table 1 for a summary of the suggested actions to take us from the current culture to an improved one.)
Table 1.
Proposed Solutions and Suggested Actions for Changing the Current Culture in the Medical Profession to Decrease the Stigma and Discrimination Associated With Mental Illness
Until we do what is in our power as physicians to change our culture, there is little hope for reducing the stigma of mental illness in our profession, which—if unaddressed—can end in suicide. And if we do not reduce the stigma associated with mental disorders in our own profession and serve as examples, then how will we advocate to reduce stigma in society at large?
Acknowledgments:
The author thanks various colleagues who provided helpful comments after reviewing earlier versions of this article.
Footnotes
Editor’s Note: An Invited Commentary by W.E. Bynum IV and J. Sukhera appears on pages XXX–XXX.
Funding/Support: None reported.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
References
- 1.Brazeau CM, Shanafelt T, Durning SJ, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014;89:1520–1525. [DOI] [PubMed] [Google Scholar]
- 2.Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA. 2016;316:2214–2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA. 2015;314:2373–2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75:336–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brenner AM. The role of personal psychodynamic psychotherapy in becoming a competent psychiatrist. Harv Rev Psychiatry. 2006;14:268–272. [DOI] [PubMed] [Google Scholar]
- 8.Brower KJ. The legacy of suicide. Psychiatr Times. 2017;34:1–2. [Google Scholar]
- 9.Zivin K, Brower KJ, Sen S, Brownlee RM, Gold KJ. Relationship between faculty characteristics and emotional exhaustion in a large academic medical center. J Occup Environ Med. 2020;62:611–617. [DOI] [PubMed] [Google Scholar]
- 10.Schwenk TL, Davis L, Wimsatt LA. Depression, stigma, and suicidal ideation in medical students. JAMA. 2010;304:1181–1190. [DOI] [PubMed] [Google Scholar]
- 11.Dyrbye LN, Eacker A, Durning SJ, et al. The impact of stigma and personal experiences on the help-seeking behaviors of medical students with burnout. Acad Med. 2015;90:961–969. [DOI] [PubMed] [Google Scholar]
- 12.Guille C, Speller H, Laff R, Epperson CN, Sen S. Utilization and barriers to mental health services among depressed medical interns: A prospective multisite study. J Grad Med Educ. 2010;2:210–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunn LB, Green Hammond KA, Roberts LW. Delaying care, avoiding stigma: Residents’ attitudes toward obtaining personal health care. Acad Med. 2009;84:242–250. [DOI] [PubMed] [Google Scholar]
- 14.Hawton K, Casanas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: A systematic review. J Affect Disord. 2013;147:17–28. [DOI] [PubMed] [Google Scholar]
- 15.Hubers AAM, Moaddine S, Peersmann SHM, et al. Suicidal ideation and subsequent completed suicide in both psychiatric and non-psychiatric populations: A meta-analysis. Epidemiol Psychiatr Sci. 2018;27:186–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: A meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353–358. [DOI] [PubMed] [Google Scholar]
- 17.Roy A. Combination of family history of suicidal behavior and childhood trauma may represent correlate of increased suicide risk. J Affect Disord. 2011;130:205–208. [DOI] [PubMed] [Google Scholar]
- 18.Schernhammer ES, Colditz GA. Suicide rates among physicians: A quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161:2295–2302. [DOI] [PubMed] [Google Scholar]
- 19.Wilson LC, Ballman AD, Buczek TJ. News content about mass shootings and attitudes toward mental illness. Journalism Mass Commun Q. 2016;93:644–658. [Google Scholar]
- 20.Pescosolido BA, Manago B, Monahan J. Evolving public views on the likelihood of violence from people with mental illness: Stigma and its consequences. Health Aff (Millwood). 2019;38:1735–1743. [DOI] [PubMed] [Google Scholar]
- 21.Caruso JP, Sheehan JP. Psychosurgery, ethics, and media: A history of Walter Freeman and the lobotomy. Neurosurg Focus. 2017;43:E6. [DOI] [PubMed] [Google Scholar]
- 22.McDonald A, Walter G. Hollywood and ECT. Int Rev Psychiatry. 2009;21:200–206. [DOI] [PubMed] [Google Scholar]
- 23.Sweeney A, Gillard S, Wykes T, Rose D. The role of fear in mental health service users’ experiences: A qualitative exploration. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallace JE. Mental health and stigma in the medical profession. Health (London). 2012;16:3–18. [DOI] [PubMed] [Google Scholar]
- 25.Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthc Manage Forum. 2017;30:111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dyrbye LN, West CP, Sinsky CA, Goeders LE, Satele DV, Shanafelt TD. Medical licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92:1486–1493. [DOI] [PubMed] [Google Scholar]
- 27.Gold KJ, Andrew LB, Goldman EB, Schwenk TL. “I would never want to have a mental health diagnosis on my record”: A survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51–57. [DOI] [PubMed] [Google Scholar]
- 28.Mehta SS, Edwards ML. Suffering in silence: Mental health stigma and physicians’ licensing fears. Am J Psychiatry Residents’ J. 2018;13:2–4. [Google Scholar]
- 29.Ghio L, Gotelli S, Cervetti A, et al. Duration of untreated depression influences clinical outcomes and disability. J Affect Disord. 2015;175:224–228. [DOI] [PubMed] [Google Scholar]
- 30.Ghio L, Gotelli S, Marcenaro M, Amore M, Natta W. Duration of untreated illness and outcomes in unipolar depression: A systematic review and meta-analysis. J Affect Disord. 2014;152154:45–51. [DOI] [PubMed] [Google Scholar]
- 31.Hung CI, Liu CY, Yang CH. Untreated duration predicted the severity of depression at the two-year follow-up point. PLoS One. 2017;12:e0185119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shanafelt TD, Schein E, Minor LB, Trockel M, Schein P, Kirch D. Healing the professional culture of medicine. Mayo Clin Proc. 2019;94:1556–1566. [DOI] [PubMed] [Google Scholar]
- 33.Hill AB. Breaking the stigma—A physician’s perspective on self-care and recovery. N Engl J Med. 2017;376:1103–1105. [DOI] [PubMed] [Google Scholar]
- 34.Gupta R. I solemnly share. JAMA. 2018;319:549–550. [DOI] [PubMed] [Google Scholar]
- 35.Federation of State Medical Boards Workgroup on Physician Wellness and Burnout. Physician wellness and burnout: Report and recommendations. J Med Regul. 2018;104:37–48. [Google Scholar]
- 36.Murphy B. Medical boards must avoid contributing to mental health stigma. American Medical Association. https://www.ama-assn.org/residents-students/transition-practice/medical-boards-must-avoid-contributing-mental-health-stigma. Published 2018. Accessed February 2, 2021.
- 37.Council on Psychiatry and the Law. Position statement on inquiries about diagnosis and treatment of mental disorders in connection with professional credentialing and licensing. American Psychiatric Association. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2018-Inquiries-about-Diagnosis-and-Treatment-of-Mental-Disorders-in-Connection-with-Professional-Credentialing-and-Licensing.pdf. Published 2018. Accessed February 2, 2021.
- 38.Lebowitz MS, Appelbaum PS. Biomedical explanations of psychopathology and their implications for attitudes and beliefs about mental disorders. Annu Rev Clin Psychol. 2019;15:555–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wade DT, Halligan PW. The biopsychosocial model of illness: A model whose time has come. Clin Rehabil. 2017;31:995–1004. [DOI] [PubMed] [Google Scholar]
- 40.Vollmer-Conna U, Beilharz JE, Cvejic E, et al. The well-being of medical students: A biopsychosocial approach. Aust N Z J Psychiatry. 2020;54:997–1006. [DOI] [PubMed] [Google Scholar]
- 41.Hanisch SE, Twomey CD, Szeto AC, Birner UW, Nowak D, Sabariego C. The effectiveness of interventions targeting the stigma of mental illness at the workplace: A systematic review. BMC Psychiatry. 2016;16:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shann C, Martin A, Chester A, Ruddock S. Effectiveness and application of an online leadership intervention to promote mental health and reduce depression-related stigma in organizations. J Occup Health Psychol. 2019;24:20–35. [DOI] [PubMed] [Google Scholar]
- 43.Thornicroft G, Mehta N, Clement S, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387:1123–1132. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organization (WHO). Promoting Mental Health: Concepts, Emerging Evidence, Practice. 2004.Geneva, Switzerland: WHO; [Google Scholar]
- 45.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. [DOI] [PubMed] [Google Scholar]
- 46.Botticelli MP, Koh HK. Changing the language of addiction. JAMA. 2016;316:1361–1362. [DOI] [PubMed] [Google Scholar]
- 47.Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21:202–207. [DOI] [PubMed] [Google Scholar]
- 48.Kelly JF, Dow SJ, Westerhoff C. Does our choice of substance-related terms influence perceptions of treatment need? An empirical investigation with two commonly used terms. J Drug Issues. 2010;40:805–818. [Google Scholar]
- 49.Robinson SM. “Alcoholic” or “Person with alcohol use disorder”? Applying person-first diagnostic terminology in the clinical domain. Subst Abus. 2017;38:9–14. [DOI] [PubMed] [Google Scholar]
- 50.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 2013.Arlington, VA: American Psychiatric Publishing; [Google Scholar]
- 51.Tkach MJ. A psychosocial linguistic exploration of the use of alcoholic as a social label of self-identity in AA and 12-step programs. Alcohol Treat Q. 2018;36:101–114. [Google Scholar]
- 52.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. [DOI] [PubMed] [Google Scholar]
- 53.Oquendo MA, Bernstein CA, Mayer LES. A key differential diagnosis for physicians—Major depression or burnout? JAMA Psychiatry. 2019;76:1111–1112. [DOI] [PubMed] [Google Scholar]
- 54.Linn-Gust M, Peters J. A Winding Road: A Handbook for Those Supporting the Suicide Bereaved. 2010.Albuquerque, NM: Chellehead Works; [Google Scholar]
- 55.Klitzman R. When Doctors Become Patients. 2008.New York, NY: Oxford University Press; [Google Scholar]
- 56.Montgomery AJ, Bradley C, Rochfort A, Panagopoulou E. A review of self-medication in physicians and medical students. Occup Med (Lond). 2011;61:490–497. [DOI] [PubMed] [Google Scholar]
- 57.Mulder H, Ter Braak E, Chen HC, ten Cate O. Addressing the hidden curriculum in the clinical workplace: A practical tool for trainees and faculty. Med Teach. 2019;41:36–43. [DOI] [PubMed] [Google Scholar]
- 58.Mortali M, Moutier C. Facilitating help-seeking behavior among medical trainees and physicians using the interactive screening program. J Med Regul. 2018;104:27–36. [Google Scholar]


